- Institute of Nutritional Medicine, University of Luebeck, Luebeck, Germany
Background: There is increasing evidence that certain dietary factors affect the course of acne vulgaris.
Objectives: The primary aim of this exploratory survey was to reveal patients' perceptions of a possible link between acne and diet. Secondary, patients' perceptions of the quality of nutritional communication, sources of dietary information, and a dietary information gap, have been investigated.
Methods: An online survey is conducted on Instagram using a structured questionnaire in German. Data is analyzed quantitatively and qualitatively, and chi-square tests are performed.
Results: Most of the 1,040 participants believe that there is a connection between acne and diet (75%). However, due to a frequent lack of nutritional consultation by dermatologists (87%), participants' nutritional information needs are not met. Therefore, they seek additional sources of information, mainly Instagram(63%), online forums(54%), and textbooks (46%). However, the participants feel that their nutritional interventions are unsuccessful and believe that an information gap exists.
Conclusion: This study draws attention to the existence of an information gap regarding the topic of acne and nutrition. Adequate patient education on currently available data and its limitations is urgently needed to counteract patients' long-held beliefs in diet and acne myths.
Introduction
Acne vulgaris is a multifactorial inflammatory skin disease with an overall global prevalence of ~9% (Eichenfield et al., 2021). Its prevalence varies substantially for different countries and age groups and is highest for adolescents in Westernized countries (Stathakis et al., 1997). Acne vulgaris usually has its onset in preadolescence and often resolves once early adulthood is reached (Heng and Chew, 2020; Eichenfield et al., 2021). Predominantly the pilosebaceous units of the face, back, and trunk are affected, showing comedones, papules, and pustules (Dréno, 2017; Heng and Chew, 2020). The severity of the disease may be influenced by certain external aspects like psychological and lifestyle factors, occupational factors, medication, pollutants, climatic factors, and nutrition (Dréno et al., 2018; Eichenfield et al., 2021). Although acne is very often considered only an aesthetic problem, it is a serious disease that potentially generates not just low self-esteem, poor perception of one's body, social withdrawal, and relevant impairments of quality of life (de Vries et al., 2022), but also psychiatric comorbidities as depression, and social anxiety disorders (Claudel et al., 2020; Eichenfield et al., 2021).
Dietary restrictions have been part of acne treatments since the nineteenth century, and a direct link between acne and dietary factors like carbohydrates, fat, and high-fat dairy products has been postulated (Dall'Oglio et al., 2021). In the 1960s, the hypothesis of acne being a diet-originated disease was rejected due to the absence of convincing evidence (Anderson, 1971). Current data demonstrate associations between the consumption of milk, sugary beverages, and fatty and sugary products with current acne (Penso et al., 2020). It remains controversial, however, if these associations result from a causal relationship or even reverse causality (Dall'Oglio et al., 2021).
Accordingly, many acne patients try to modify their habitual diet by avoiding certain foods (mostly milk, dairy, and chocolate) or increase the intake of others (mostly food products rich in omega-3 fatty acids) (Bungau et al., 2022).
Data on the sources that acne patients use to inform themselves about dietary interventions are very rare. In a survey including 50 acne patients (Houston, Texas, USA), Nguyen et al. found that acne patients obtained their information from Google searches (49.0%), dermatologists (43%), family members and TV (41.0%), and medical websites (31.0%) (Nguyen et al., 2016). However, the number of participants was very limited, and due to changes in social media usage these results are outdated. A more recent study from Turkey investigating the social media use in 1,489 acne patients found that 46.3% regularly and 28.8% sometimes referred to social media sources to make inquiries about acne (Kayiran et al., 2021). In this study, social media usage for acne-related content was higher in women than in men. The most used social media were Google (67.0%), Instagram (54.0%), and Youtube (49.0%).
It has been suggested earlier that there is a positive correlation between disease burden and online search interest (Khanna et al., 2018). Therefore, the impact of these online searches and the validity of social media search results are topics worth considering.
In the current German guideline for acne management, no diet-specific statement is provided at all (Nast et al., 2011). This guideline, however, has not been updated since 2011. Remarkably, this assessment of available data does not seem to be obsolete, since even the most recent National Institute for Health and Care Excellence (NICE) guideline for the management of acne states that there is not enough evidence to support specific diets for treating acne (National Institute for Health and Care Excellence (NICE), 2021). Consistently, in the current guidelines of the American Academy of Dermatology, no specific dietary changes are recommended in the management of acne (Zaenglein et al., 2016). However, it is stated that high glycemic index diets may be associated with acne and that limited evidence suggests an effect of dairy on acne.
According to the present state of knowledge, study results support the idea that certain dietary factors do not cause but rather aggravate or influence acne to some degree (Dall'Oglio et al., 2021). However, several studies demonstrated that acne symptoms could be improved by a low glycemic index (GI) or a low glycemic load (GL) diet (Burris et al., 2018). Clinical data on the effect of milk, dairy, and chocolate on acne symptoms still remain controversial (Dai et al., 2018; Juhl et al., 2018; Dall'Oglio et al., 2021).
Other dietary factors may also contribute to the improvement of acne are foods rich in omega-3 fatty acids (Thomsen et al., 2020), omega-6 fatty acids (Balić et al., 2020), probiotics (Sinha et al., 2021), and putative effects of vegetarian, vegan, or ketogenic diets on acne symptoms (Baldwin and Tan, 2021). To date, however, no definitive conclusions can be drawn (Dall'Oglio et al., 2021).
Due to the lack of evidence regarding the efficacy of dietary interventions in treating acne vulgaris, advising patients on dietary topics remains challenging for dermatologists. This state of uncertainty, being defined as a meta-cognition and a self-reflective mental state in which one is subjectively aware of one's ignorance, is pervasive in medicine (Han et al., 2011). Nutritional research and technological developments have yielded detailed knowledge, but also overly complex information that is difficult to translate into clinical recommendations (Gärtner et al., 2020).
Paradoxically, the rise of evidence-based medicine has increased the awareness of professionals that their knowledge is very limited and subject to rapid obsolescence (Han et al., 2019; Pomare et al., 2019).
Regarding communication psychology, dermatologists may use different strategies to address this scientific uncertainty (Pomare et al., 2019; Medendorp et al., 2021): On the one hand, dermatologists can strictly eliminate all dietary topics from their medical consultations, which will leave many patients disappointed and intensify the perception of a pre-existing information gap. On the other hand, dermatologist can unequivocally clarify the current lack of knowledge/evidence, thereby avoiding both potentially unhealthy dietary restrictions and unjustified hopes for a “dietary cure” (Bansback et al., 2017). Depending on how the uncertainty is communicated, it can affect patients in completely different ways (Medendorp et al., 2021).
In Germany, this complex situation is even complicated since no established treatment pathway exists that would integrate the specific expertise of general practitioners, dermatologists, and nutritionists. Despite an existing referral system between general practitioners and specialists, acne patients are free to without further ado contact any dermatologist, gynecologist, or nutritionist for medical or dietary advice.
Of note, detrimental effects of rigid and over-restrictive dietary interventions may explain the associations of acne, unfavorable body composition, and eating disorders as described in previous studies (Barrea et al., 2021; Öner and Hacinecipoglu, 2021).
Therefore, the primary aim of this exploratory survey was to reveal patients' perceptions of a possible link between acne and diet. Secondary, patients' perceptions of the quality of nutritional communication and sources of dietary information have been investigated.
Materials and Methods
Data Collection
An online survey on acne and nutrition was conducted using a structured questionnaire in the German language. The design of the questionnaire, the administration of the survey, and the collection of data have been based on the well-established methodology of empirical research (Brenner, 2020).
Acne patients of all ages were recruited using social media—predominantly Instagram channels dealing with the topics of skin diseases, nutrition, and a healthy lifestyle, or a combination thereof. Participant consent was collected when participants started the questionnaire.
Data were collected using the online tool SurveyMonkey. The survey was administered for 27 days in August 2021 and comprised 24 questions. Of these, ten questions were closed questions with predetermined responses, four questions were open-ended questions with text fields of unlimited characters, six questions were designed as mixed questions containing the additional option “other,” and four questions asked for ratings on a scale ranging from 0 to 100 points.
The questionnaire addressed participants' demographic data, their perceptions regarding the role of diet in acne, the quality of their dermatologists' dietary consultations, and whether they were looking for information on this topic themselves. If participants were looking for information on these topics themselves, they were asked which sources they had consulted and what information they had received as well as their perceptions of the existence of an information gap.
Data Analysis
Descriptive statistics, including frequencies, means, standard deviations, and quantiles, were applied using Microsoft Excel 2019 to characterize the study population. Open-ended questions were analyzed qualitatively. To determine whether statistically differences between the expected frequencies of answers and the observed frequencies, chi-square tests were performed using IBM SPSS Statistics Version 28.0. The chi-square test is the valid statistical hypothesis test for statistics been chi-square distributed under the null hypothesis. P-values ≤ 0.05 were considered statistically significant. The quantitative variable age was categorized into four different age cohorts (≤ 20; 21–30, 31–40, and >40), while the remaining quantitative variables addressing participants' ratings and the existence of an information gap were categorized into quintiles.
Results
Demographic Characteristics
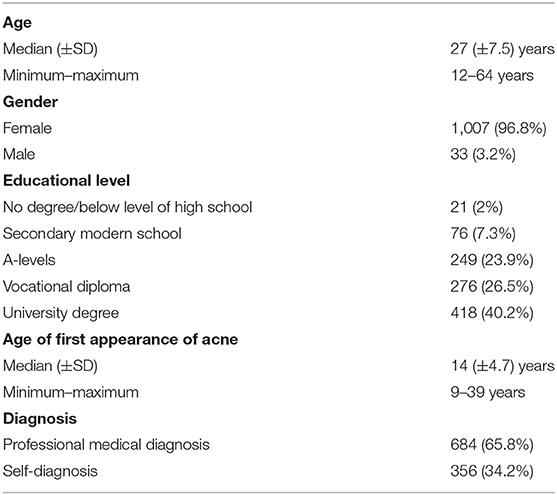
In total, 1,040 participants completed the online survey. Detailed demographic characteristics of the study population are given in Table 1. To treat their acne, participants had tried, on average, eight different methods (Figure 1). The most frequently utilized methods were cosmetic products from drugstores (83.9%), followed by cosmetic products from pharmacies (78.0%) and the administration of dry mud masks (70.9%). Furthermore, 66.2% of the participants had changed their diets to improve their acne.
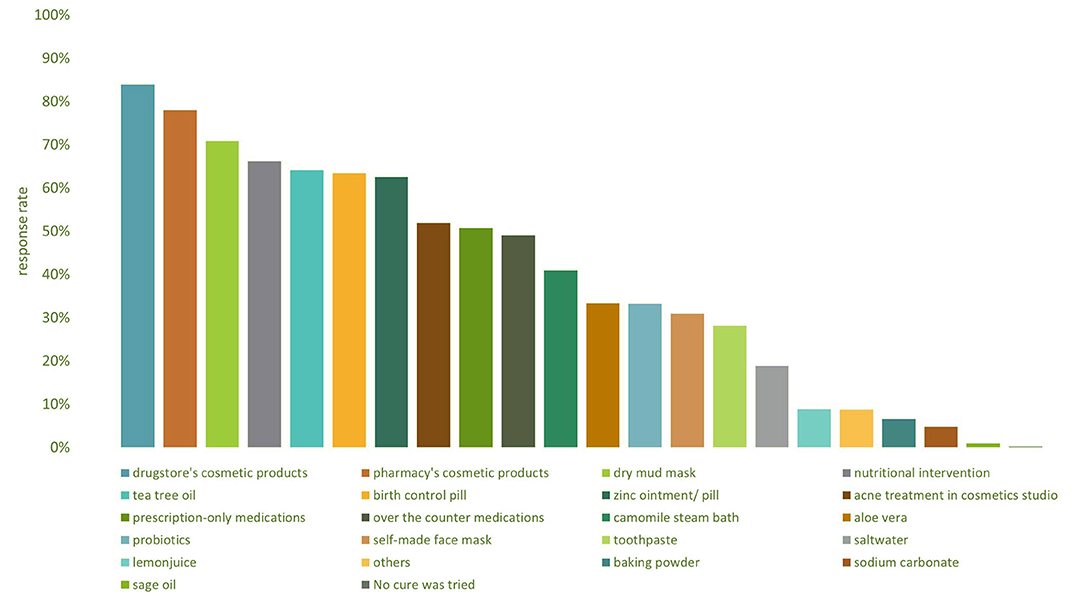
Figure 1. Bar chart showing the distribution of acne treatment methods participants used. Multiple answers were possible; the option “others” offered an open-ended response field.
Perception of the Connection Between Acne and Nutrition
Of the participants, 65.3% reported that 1 year or longer had passed after their acne onset since they first came across the topic “acne and nutrition” Moreover, 15.2% first heard about the topic after a few months and 5.6% after a few days, while only 13.9% of the participants were immediately aware of the connection. Only 10.0% of the study population claimed to have paid attention to their nutrition prior to the onset of their acne. As shown in Figure 2, of the professionally diagnosed participants, 87.4% reported that nutritional aspects were not discussed at all by their dermatologists. In addition, 3.3% of the participants received consultations only on demand. Only 1.1% of the participants were provided with detailed nutritional consultations.
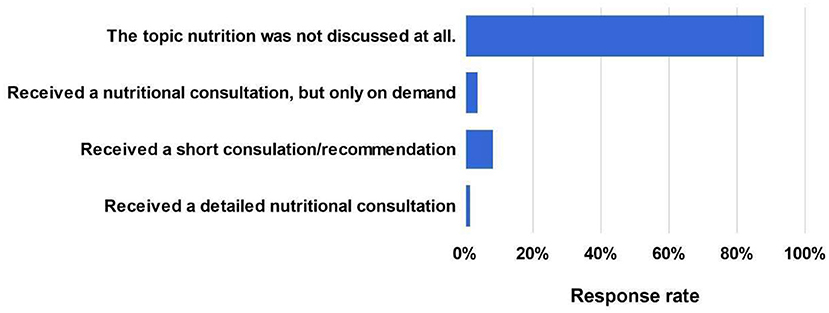
Figure 2. Responses to the question of whether participants received nutritional consultations from their dermatologists.
Regarding the participants' needs and expectations, 66.8% claimed that they did not receive any nutritional consultations but would have liked to, and 20.1% reported that their dermatologists' consultations were not sufficient (Figure 3). On the contrary, only 2.2% of the participants stated that they had been well-advised by their dermatologists. Furthermore, 10.9% did not receive nutritional consultations but did not want them. Half of the participants (50.5%) were convinced that an individual, detailed nutritional consultation had or would have positively affected their outcomes, whereas 41.6% hypothesized that this had or would have probably been the case. Only 7.1% shared the opinion that there would have been probably no effect, and <1% believed that there would have been no effect at all on the outcome.
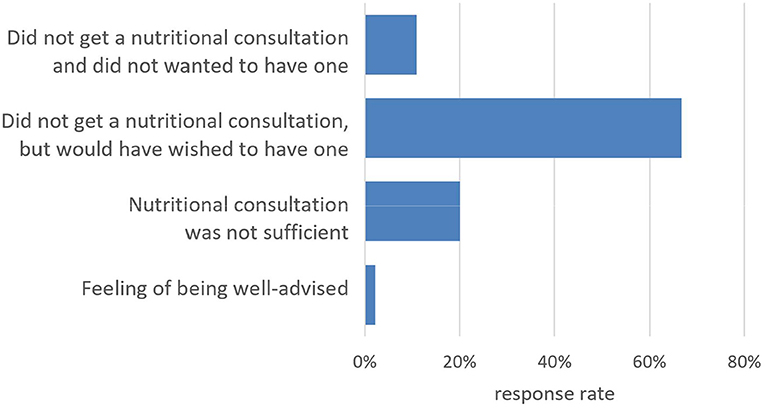
Figure 3. Responses to the question of whether or not participants felt sufficiently advised about the connection between acne and nutrition after their diagnoses.
Of the participants, 75.3% believed that there was a connection between acne and nutrition, whereas 22.5% thought that there might be a connection. Among the study population, only 2.2% said that there is no connection” or “probably no connection.” As indicated in Table 2, a chi-square of independence showed no significant associations between the belief that there is a connection between acne and nutrition and the variables gender, age, and educational degree.
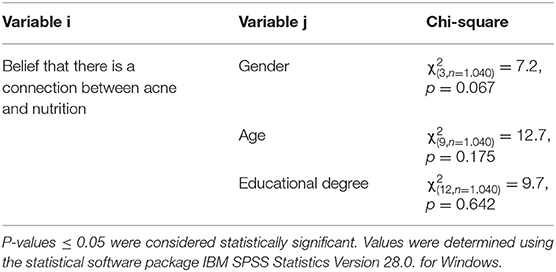
Table 2. Results of chi-square test of independence of different variables, indicated as the variables i and j.
93.1% of the participants reported that they had informed themselves about the link between acne and nutrition. A chi-square test of independence showed a significant relationship between the participants' beliefs that there is a connection between acne and nutrition and the motivation to inform oneself about this relationship (χ2 = 29.7, p < 0.001). Another chi-square test of independence showed no significant association between a dermatologist consultation and participants' motivations to inform themselves about the connection between acne and nutrition (χ2 = 1.5, p = 0.819). The distribution of the answers is provided in Table A1 in the appendix.
Utilized Sources
A multiple-choice question was included in the questionnaire to investigate the sources used for self-education regarding possible links between acne and nutrition. The responses were sorted into age cohorts (<20, 21–30, 31–40, and >41 years) (Figure 4). While participants younger than 20 most often used YouTube (24.2%) followed by Instagram (22.2%) and online forums (20.5%), the older cohorts most often used Instagram (21.7%) followed by online forums (18.9%) and textbooks (16.9%). Of all the age cohorts, 15.0% provided additional heterogeneous sources in an open-ended response field. Here, participants reported listening to podcasts, visiting a non-medical practitioner or nutritionist, using traditional Chinese medicine (TCM) interventions, searching pubmed.com to find original scientific papers, taking part in coaching and lectures, or gaining knowledge from their university studies.
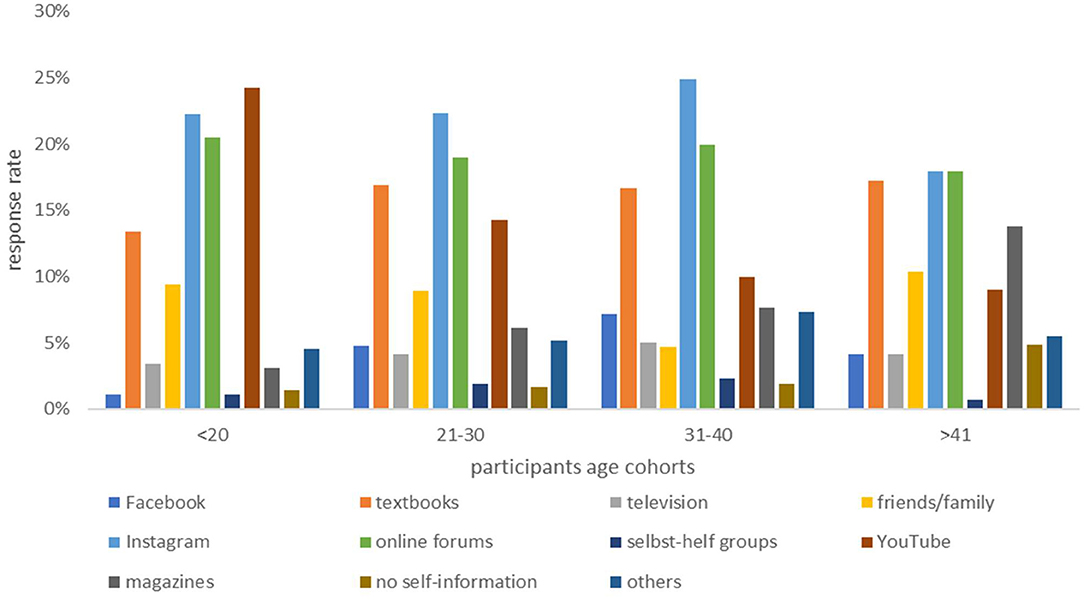
Figure 4. Bar chart showing sources that participants used to educate themselves regarding the of topic acne and nutrition, sorted by age cohort (<20, 21–30, 31–40, and >41 years). Multiple answers were possible.
Nutritional Interventions
The participants who educated themselves were asked about the nutritional recommendations they found during their research. Most often, the participants received the information to refrain from consuming sugar (86.4%), dairy products (82%), fast food (80.4%), sweets (78%), and milk (77.4%). The recommendations that were most frequently adopted in practice were abstaining from milk (66.7%), dairy products (58.7%), fast food (54.6%), and sugar (50.3%).
The participants also found the recommendations of drinking plenty of water (89.8%) and increasing their consumption of vegetables (75.0%) and fruits (53.2%). Additionally, 45.0% received the advice to increase their intake of foods rich in omega-3 fatty acids. The advice that a vegan or vegetarian diet may improve acne symptoms was found by 42.4% and 26.0% of the participants, respectively. The recommendations most often followed in practice were drinking plenty of water (84.5%), followed by eating plenty of vegetables (69.5%) and fruits (46.9%). The intake of foods containing omega-3 fatty acids was controlled by 34.2% of the participants (Figure 5). There was no significant association between receiving a dermatologist consultation and translating recommendations into practice (χ2 = 14.9, p = 0.247). On the contrary, there was a significant association between educating oneself and translating recommendations into practice (χ2 = 55.5, p < 0.001).
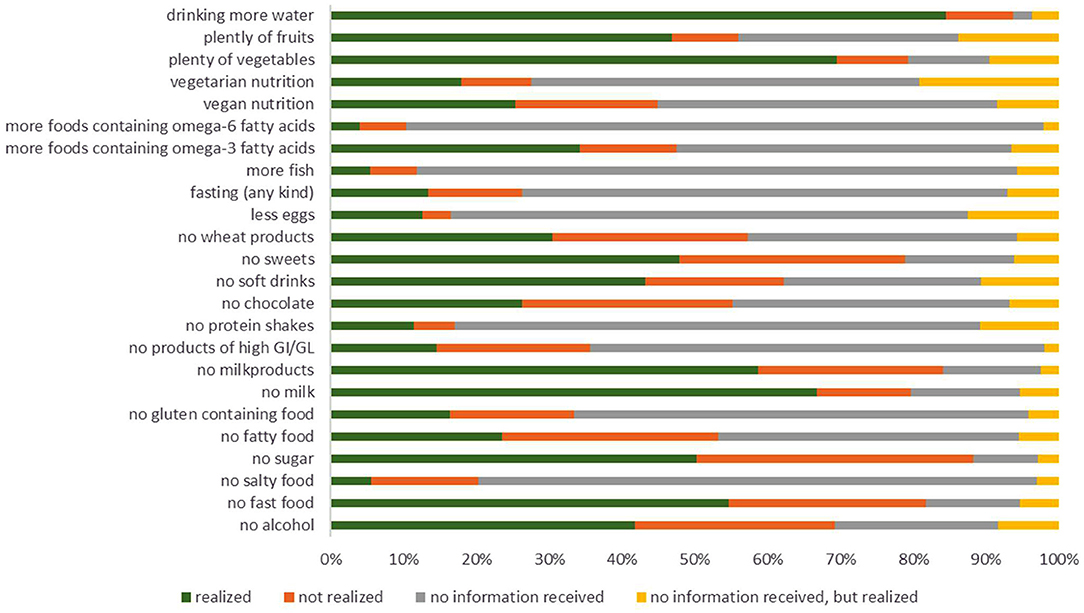
Figure 5. Bar chart of the translation of recommendations into practice by the participants. The participants matched the category “realized” when they gained information and translated it into practice, “not realized” when gained information but did not translate it into practice, “no information received” when they did not gain information and also did not translate it into practice, and “no information received, but realized” when they did not gain information but followed a specific eating behavior anyways.
Compared to their pre-diagnostic diets, awareness of nutritional and dietary topics increased for 75.1% of participants. Nutritional awareness after diagnosis was significantly associated with the variable of educating oneself (χ2 = 65, p < 0.001).
Perceptions of Success and the Existence of an Information Gap
The participants were asked to rate their personal success regarding the effects of dietary interventions on the course of their acne using a scale ranging from 0 to 100 points (100 points = highly successful). They rated their success with a median value of 54 points, whereas the first and third quartiles were 32 and 73 points, respectively. The quality of the dermatologist consultation regarding the topic of acne and nutrition had no impact on the success of the nutritional interventions (χ2 = 23.4, p = 0.104). However, there was a significant association between educating oneself and the success of the nutritional interventions (χ2 = 63, p < 0.001). Furthermore, a significant association was found between nutritional awareness after diagnosis and the success of the nutritional interventions (χ2 = 203.1, p < 0.001).
Moreover, the participants rated the existence of an information gap regarding the topic of acne and nutrition using a 100-point scale (100 points = existence of a large information gap). The median rating was 91 points, and the first and third quartiles were 75 and 100 points, respectively. This indicates that most of the participants shared the opinion that there is an information gap. The association between receiving a dermatologist consultation and the perception of the existence of an information gap was significant (χ2 = 53.6, p < 0.001). Furthermore, informing oneself was not significantly associated with a belief in the existence of an information gap (χ2 = 2, p = 0.744). However, there was a significant association between successful dietary interventions and the belief in the existence of an information gap (χ2 = 100.7, p < 0.001).
Finally, the participants rated their feelings of being affected by the information gap a median value of 72 points. Half of the participants gave ratings within the range of 49 to 90 points, representing the first and third quartiles, respectively. The feeling of being affected was significantly associated with personal success regarding nutritional interventions (χ2 = 58.6, p < 0.001).
Discussion
There is increasing evidence that nutrition plays an important role in the pathogenesis of acne vulgaris. This exploratory survey study aimed to investigate acne patients' perceptions of a link between acne and diet, the quality of their dermatologists' nutritional consultations, and their motivation to search for information from additional sources. Furthermore, we investigated the perception of an information gap regarding nutrition in acne patients.
The role of nutrition in the development of acne is complex and has not yet been completely elucidated. Nevertheless, 98.0% of the participants reported believing that a link between acne and nutrition (probably) exists. In contrast, only 1.0% received detailed nutritional consultations from their dermatologists. For 87.0% of participants, the topic of nutrition was not addressed at all, indicating that it still plays a minor role in acne treatment and medical patient counseling. As current guidelines do not recommend specific dietary changes for acne patients and the current evidence for specific dietary interventions is still insufficient, dermatologists may feel restricted in their nutritional consultations (Hauk, 2017). Nevertheless, most participants desired more detailed nutritional consultations, as they believed that these would improve their outcomes.
However, these results may be subject to an inclusion bias, as presumably most participants answering the questionnaire were of the opinion that dietary factors directly affected their disease.
Participants' perceptions of a possible link between acne and nutrition were significantly associated with the motivation to search for information from additional sources. Most frequently, and irrespective of the patients' ages, Instagram, online forums, and textbooks were used for research. According to results from Khanna et al. (2018), who investigated Google search results for dermatological conditions, including acne, most of the information online is “unfounded and/or misleading.” Although studies often have critical flaws in their research designs and are unconfirmed, they are presented as true by self-proclaimed experts withholding decisive information. There are also educational web pages and influencers with medical backgrounds communicating high-quality, relevant, and evidence-based information, including study limitations. However, it remains unknown whether patients without medical expertise use these educational web pages, which often contain difficult-to-understand information (Khanna et al., 2018). The multitude of information may be overtaxing and provoke further myths regarding acne and diet.
Nguyen et al. (2016) performed an exploratory survey study investigating patients' beliefs regarding acne and diet. They reported that most of the patients (n = 49) believed that fried/greasy food (73.0%) and chocolate (53.0%) were the main triggers of acne. In contrast, refined carbohydrates and sugar were perceived as less important in acne onset (Nguyen et al., 2016). Our study showed that the most commonly received recommendations were not translated into practice at the same frequency. Although the information to forego sugar was obtained by most of the participants (86.4%), only 50.3% tried to translate this recommendation into practice. In comparison, fewer people got the information to forego milk (77.4%) and milk products (82.0%), but the translation of these recommendations into practice was higher than that of sugar (milk: 66.7%; milk products: 58.7%). This inconsistency may be due to personal obstacles in translating certain dietary recommendations into practice or the strength of long-held beliefs that may differ from the gathered information.
Participants who informed themselves regarding dietary interventions showed significantly increased nutritional awareness after their diagnoses, which was indicative of the patients' high intrinsic motivation and suffering. Nevertheless, the information gap affects patients' perceptions of their success with dietary changes (median value of 54 out of 100 points). Unrealistic expectations lead to dissatisfaction regarding their achievements. The lack of success, the lack of consultations with a dermatologist, and the feeling of not being well-advised or of being overtaxed by the gathered information leads to the perception of an information gap (median value of 91 out of 100 points) and the feeling of being affected by it (median value of 72 out of 100 points). An open-ended question addressing the participants' thoughts and opinions regarding the topic of acne and nutrition uncovered participants' feelings of being desperate due to many ineffective drug prescriptions and the feeling of being neglected by their dermatologists. Since the study population was mainly recruited via social media channels dealing with skin diseases, nutrition, or a healthy lifestyle, indicating a general interest and expertise in this field, these results are biased and cannot necessarily be applied to the general population of those with acne in Germany.
It cannot be overlooked that acne is a multifactorial disease that requires a holistic treatment approach (Eichenfield et al., 2021). Unfortunately, currently, drug prescription is the first-line treatment, rather than considering exposome factors like nutrition (Dréno et al., 2018). The identification and controlling of these factors offer the possibility of adjuvant interventions, which could improve therapeutic outcomes and prevent the risk of relapse, thereby increasing patients' quality of life [National Institute for Health and Care Excellence (NICE) (2021)].
These findings indicate the need for dermatologists to implement adequate consultations on the impact of diet on acne to meet patients' medical and nutritional expectations. Nutrition counseling of acne patients should clarify the current lack of knowledge and should prevent potentially unhealthy dietary restrictions. If patients aim to search for dietary trigger factors, the use of validated digital applications (apps) and tracking technologies should be encouraged. Patients sticking to possibly harmful dietary restrictions should be advised to contact a licensed nutritionist for professional support. On the other hand, almost any specific diet has the potential to improve the feeling of self-efficacy in many patients, thereby contributing to efficient coping strategies (Sawyer et al., 2019).
Therefore, uncritical dietary interventions should not be dismissed out of hand just because of a lack of evidence, if these interventions appear crucial for the patient's coping strategy. Regarding current communicational research, this approach to address the scientific uncertainty should be communicated clearly and transparently with patients (Medendorp et al., 2021). It is important to advise patients that many results of online searches for medical conditions are unconfirmed and not necessarily supported by robust data (Khanna et al., 2018).
It is a peculiarity of the German health care system that acne patients (like all patients) are free to contact a specialist, even before or without consulting any general practitioner. Therefore, evidence-based knowledge regarding dietary recommendations for acne patients must be available not only for general practitioners, but for all specialties (esp. gynecologists, dermatologists, nutritionist/licensed dietitians). To enable those specialists to provide nutrition-related information, the expired German guideline for the management of acne needs to be updated; in this process, dietary recommendations should be addressed sufficiently.
Moreover, the resulting information gap means that acne patients search for information on social media, which is often not educational or evidence-based but rather promotional or stated by self-proclaimed experts (Khanna et al., 2018). This may lead to incorrect assumptions, unhealthy diets, unnecessary dietary restrictions, and spending on ineffective dietary supplements (Pomare et al., 2019). Therefore, diets should be checked primarily for potential risks and adverse effects first rather than for their efficacy. This principle of non-maleficence deserves special attention in the professional communication, since detrimental effects of rigid and over-restrictive dietary interventions may impair the nutritional status and pose a significant health risk in acne patients (Pomare et al., 2019; Barrea et al., 2021; Öner and Hacinecipoglu, 2021).
We do acknowledge some limitations of our study. Representing an exploratory survey, the questionnaire has been developed for this survey without being validated before. However, this fact is a result of lack of previous studies on this respective topic of research. Nevertheless, data provided here can serve as the basis of future reproduction and validation. Being limited to acne patients in Germany, the transferability of the results to other countries is not necessarily given, since the German health care system includes some special features (esp. regarding the referral system). Finally, study participants are subject to a selection bias as being exclusively recruited via social media. However, this method can be justified by the fact that social media like Instagram, Facebook, and Twitter, are prevalent sources of health information today and are commonly used for health purposes (Chen and Wang, 2021). Moreover, our social media-based approach is backed by previous analyses demonstrating the growing relevance of social media for dermatological research in particular (Geist et al., 2021).
Since there are remaining controversies, further research is required before finally implementing nutrition into clinical therapy and establishing medical nutritional guidelines. Therefore, upcoming research needs to identify causal effects of dietary interventions on acne by setting up appropriately designed randomized-controlled trials. Furthermore, personalized dietary approaches must be developed that adequately take into account the individual metabolism, microbiome, and genetic background. And finally, the relevance and differential effects of different communication strategies to address scientific uncertainty in the context of dietary recommendations for acne patients require substantial clarification.
Data Availability Statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found at: https://doi.org/10.6084/m9.figshare.17111375.v3.
Ethics Statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the participants' legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author Contributions
MS and LT contributed equally to conception and design of the study. LT recruited the participants, performed the statistical analysis, and wrote the first draft of the manuscript. MS contributed to manuscript revision, read, and approved the submitted version. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcomm.2022.842443/full#supplementary-material
References
Baldwin, H., and Tan, J. (2021). Effects of diet on acne and its response to treatment. Am. J. Clin. Dermatol. 22, 55–65. doi: 10.1007/s40257-020-00542-y
Balić, A., Vlašić, D., ŽuŽul, K., Marinović, B., and Mokos, Z. B. (2020). Omega-3 versus Omega-6 polyunsaturated fatty acids in the prevention and treatment of inflammatory skin diseases. Int. J. Mol. Sci. 21, 741. doi: 10.3390/ijms21030741
Bansback, N, Bell, M, Spooner, L, Pompeo, A, Han, P. K. J, and Harrison, M. (2017) Communicating uncertainty in benefits harms: a review of patient decision support interventions. Patient 10 311–319. doi: 10.1007/s40271-016-0210-z
Barrea, L., Donnarumma, M., Cacciapuoti, S., Muscogiuri, G., De Gregorio, L., et al. (2021). Phase angle and Mediterranean diet in patients with acne: Two easy tools for assessing the clinical severity of disease. J. Transl. Med. 19, 171. doi: 10.1186/s12967-021-02826-1
Brenner, P. S., (ed.). (2020). Understanding Survey Methodology: Sociological Theory and Applications. New York, NY: Springer.
Bungau, S. G., Tit, D. M., Vesa, C. M., Abid, A., Szilagyi, D.-V., Radu, A.-F., et al. (2022). Non-conventional therapeutical approaches to acne vulgaris related to its association with metabolic disorders. Eur. J. Pharmacol. 923, 174936. doi: 10.1016/j.ejphar.2022.174936
Burris, J., Shikany, J. M., Rietkerk, W., and Woolf, K. (2018). A low glycemic index and glycemic load diet decreases insulin-like growth factor-1 among adults with moderate and severe acne: a short-duration, 2-week randomized controlled trial. J. Acad. Nutr. Diet. 118, 1874–1885. doi: 10.1016/j.jand.2018.02.009
Chen, J., and Wang, Y. (2021). Social media use for health purposes: systematic review. J. Med. Internet Res. 23, e17917. doi: 10.2196/17917
Claudel, J. P., Auffret, N., Leccia, M. T., Poli, F., and Dréno, B. (2020). Acne from the young patient's perspective. J. Eur. Acad. Dermatol. Venereol. 34, 942–947. doi: 10.1111/jdv.16067
Dai, R., Hua, W., Chen, W., Xiong, L., and Li, L. (2018). The effect of milk consumption on acne: a meta-analysis of observational studies. J. Eur. Acad. Dermatol. Venereol. 32, 2244–2253. doi: 10.1111/jdv.15204
Dall'Oglio, F., Nasca, M. R., Fiorentini, F., and Micali, G. (2021). Diet and acne: review of the evidence from 2009 to 2020. Int. J. Dermatol. 60, 672–685. doi: 10.1111/ijd.15390
de Vries, F., Driessen, R., Tjin, E., Westenberg, A., Vehof, H., and van de Kerkhof, P. (2022). The association between acne care provision and quality of life: a cross-sectional survey. Health Sci. Rep. 5, e487. doi: 10.1002/hsr2.487
Dréno, B. (2017). What is new in the pathophysiology of acne, an overview. J. Eur. Acad. Dermatology Venereol. 31, 8–12. doi: 10.1111/jdv.14374
Dréno, B., Bettoli, V., Araviiskaia, E., Sanchez Viera, M., and Bouloc, A. (2018). The influence of exposome on acne. J. Eur. Acad. Dermatol. Venereol. 32, 812–819. doi: 10.1111/jdv.14820
Eichenfield, D. Z., Sprague, J., and Eichenfield, L. F. (2021). Management of acne vulgaris. J. Am. Med. Assoc. 326, 2055–2067. doi: 10.1001/jama.2021.17633
Gärtner, J., Berberat, P. O., Kadmon, M., and Harendza, S. (2020). Implicit expression of uncertainty – suggestion of an empirically derived framework. BMC Med. Educ. 20, 83. doi: 10.1186/s12909-020-1990-3
Geist, R., Militello, M., Albrecht, J. M., Presley, C. L., Anderson, J. B., Laughter, M., et al. (2021). Social media and clinical research in dermatology. Curr. Dermatol. Rep. 10, 105–111. doi: 10.1007/s13671-021-00350-5
Han, P. K., Babrow, A., Hillen, M. A., Gulbrandsen, P., Smets, E. M., and Ofstad, E. H. (2019). Uncertainty in health care: towards a more systematic program of research. Patient Educ. Couns. 102, 1756–1766. doi: 10.1016/j.pec.2019.06.012
Han, P. K., Klein, W. M., and Arora, N. K. (2011). Varieties of uncertainty in health care: a conceptual taxonomy. Med. Decis. Making. 31, 828–838. doi: 10.1177/0272989X11393976
Heng, A. H. S., and Chew, F. T. (2020). Systematic review of the epidemiology of acne vulgaris. Sci. Rep. 10, 5754. doi: 10.1038/s41598-020-62715-3
Juhl, C. R., Bergholdt, H. K. M., Miller, I. M., Jemec, G. B. E., Kanters, J. K., Ellervik, C., et al. (2018). Lactase persistence, milk intake, and adult acne: a mendelian randomization study of 20,416 Danish adults. Nutrients 10, 1041. doi: 10.3390/nu10081041
Kayiran, M. A., Karadag, A. S., Alyamaç, G., Cemil, B. Ç., Demirseren, D. D., Aksoy, H., et al. (2021). Social media use in patients with acne vulgaris: what do patients expect from social media? J. Cosmet. Dermatol. 20, 2556–2564. doi: 10.1111/jocd.14272
Khanna, R., Shifrin, N., Nektalova, T., and Goldenberg, G. (2018). Diet and dermatology: Google search results for acne, psoriasis, and eczema. Cutis. 102, 44.
Medendorp, N. M., Stiggelbout, A. M., Aalfs, C. M., Han, P. K. J., Smets, M. A., and Hillen, M. A. (2021). A scoping review of practice recommendations for clinicians' communication of uncertainty. Health Expert 24, 1025–1043. doi: 10.1111/hex.13255
Nast, A., Bayerl, C., Borelli, C., Degitz, K., Dirschka, T., Erdmann, R., et al. (2011). Behandlung der Akne. AWMF 013-017. Avaialble online at: https://www.awmf.org/uploads/tx_szleitlinien/013-017l_S2k_Behandlung_der_Akne_2011-abgelaufen.pdf
National Institute for Health Care Excellence (NICE) (2021). NG198. Avaialble online at: https://www.nice.org.uk/guidance/ng198/resources/acne-vulgaris-management-pdf-66142088866501
Nguyen, Q.-G., Markus, R., and Katta, R. (2016). Diet and acne: an exploratory survey study of patient beliefs. Dermatol. Pract. Concept. 6, 21–27. doi: 10.5826/dpc.0602a05
Öner, Ü., and Hacinecipoglu, F. (2021). Could acne be a risk factor for devoloping eating disorders? Acne vulgaris and eating disorders. J. Cosmet. Dermatol. doi: 10.1111/jocd.14330 [Epub ahead of print].
Penso, L., Touvier, M., Deschasaux, M., Szabo de edelenyi, F., Hercberg, S., Ezzedine, K., et al. (2020). Association between adult acne and dietary behaviors: findings from the nutrinet-santé prospective cohort study. JAMA Dermatol. 156, 854–862. doi: 10.1001/jamadermatol.2020.1602
Pomare, C., Churruca, K., Ellis, L. A., Long, J. C., and Braithwaite, J. (2019). A revised model of uncertainty in complex healthcare settings: a scoping review. J. Eval. Clin. Pract. 25, 176–182. doi: 10.1111/jep.13079
Sawyer, A. T., Harris, S. L., and Koenig, H. G. (2019). Illness perception and high readmission health outcomes. Health Psychol. Open 6, 2055102919844504. doi: 10.1177/2055102919844504
Sinha, S., Lin, G., and Ferenczi, K. (2021). The skin microbiome and the gut-skin axis. Clin. Dermatol. 39, 829–839. doi: 10.1016/j.clindermatol.2021.08.021
Stathakis, V, Kilkenny, M, and Marks, R. (1997). Descriptive epidemiology of acne vulgaris in the community. Australas. J. Dermatol. 38, 115–123. doi: 10.1111/j.1440-0960.1997.tb01126.x
Thomsen, B. J., Chow, E. Y., and Sapijaszko, M. J. (2020). The potential uses of omega-3 fatty acids in dermatology. J. Cutan. Med. Surg. 24, 481–494. doi: 10.1177/1203475420929925
Keywords: acne vulgaris, diet, nutritional intervention, information gap, acne myths, dermatology, Instagram, social media
Citation: Smollich M and Tischner L (2022) Patient Perceptions About Acne, Nutrition, and a Dietary Information Gap. Front. Commun. 7:842443. doi: 10.3389/fcomm.2022.842443
Received: 23 December 2021; Accepted: 12 April 2022;
Published: 02 May 2022.
Edited by:
Victoria Team, Monash University, AustraliaReviewed by:
Alison Layton, University of York, United KingdomJennifer K. Ptacek, University of Dayton, United States
Copyright © 2022 Smollich and Tischner. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Martin Smollich, bWFydGluLnNtb2xsaWNoQHVrc2guZGU=
 Martin Smollich
Martin Smollich Lea Tischner
Lea Tischner