
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Commun. , 28 April 2021
Sec. Health Communication
Volume 6 - 2021 | https://doi.org/10.3389/fcomm.2021.638031
The role of media use on mental health distress is particularly concerning during the COVID-19 global pandemic. The vulnerabilities to and experiences of the COVID-19 pandemic in the United States are greatly influenced by racial/ethnic inequalities. The COVID-19 pandemic may present unique mental health challenges for Asian Americans because of racial targeting and limited access to and engagement with mental health care. This present investigation examines whether the association between media use and mental health distress is more pronounced for Asian Americans for whom media messages that document and promote anti-Asian racism are likely to be especially salient and influential. Using a national survey of Asian (n = 524) and White (n = 527) American participants, our findings reveal that racial/ethnic identity interacted with the negative effect of media use on mental health for Asian Americans, but not for White Americans. We also explored whether the effect of media use on mental health was mediated by social and health risk perceptions. Results revealed that even though imagined stigma was associated with mental health distress, it did not mediate the effect of media use on mental health. Health risk perceptions mediated the negative effect of media use on both psychosocial distress and loneliness. Implications for health communication, media studies, and anti-Asian racism are discussed, especially in the context of health crises.
Communication scholars have long recognized that health crises enhance the public's need for accurate and reliable health information and the motivation to engage in information-seeking behaviors (Kahlor, 2010; Austin et al., 2012). The role of media use on mental health distress is particularly concerning during the COVID-19 global pandemic. A growing body of evidence suggests that media portrayals of the pandemic (e.g., employment interruption and loss, infringements on personal freedoms, etc.) is linked with emotional distress and mental illness; for many people, this is a time of psychological vulnerability and uncertainty (Pfefferbaum and North, 2020; Rajkumar, 2020; Xiong et al., 2020). To mitigate harmful media effects during health crises, scholars must better understand the psychological processes underlying the relationships between media use and mental health distress (Holmes et al., 2020).
The vulnerabilities to and experiences of the COVID-19 pandemic in the United States are greatly influenced by racial/ethnic inequalities (Chowkwanyun and Reed, 2020; Kantamneni, 2020). Indeed, the psychosocial effects of the pandemic in the United States are best understood in the context of the current and historical mistreatment of Asian Americans, who have been blamed for the cause and spread of COVID-19 virus (Misra et al., 2020). The COVID-19 pandemic may especially present unique mental health challenges for Asian Americans, because of racial targeting as well as due to limited access to and engagement with mental health care due to various sociocultural factors. The potential for media use to exacerbate mental health distress might be particularly pronounced for Asian Americans, for whom the pandemic has heightened the incidence of racial targeting, discrimination, and violence (Gover et al., 2020; Reny and Barreto, 2020). This present investigation examines whether the association between media use and mental health distress is more pronounced for Asian Americans for whom media messages that document and promote anti-Asian racism are likely to be especially salient and influential.
The present study makes several significant contributions to health communication, media studies, and racial/ethnic studies. First, it explores the theoretical mechanisms through which media use during the COVID-19 pandemic influences mental health distress. Second, it investigates the extent to which Asian Americans, compared to White Americans, are particularly vulnerable to this effect due to heightened anti-Asian racism during the pandemic. Third, it contributes to a better understanding of the role of racism in mental health outcomes, an understudied topic within communication, especially in the context of Asian American experiences. Fourth, this study expands our understanding of the negative effects of stigmatization by incorporating more subtle forms such as “imagined stigma,” which examines if the mere expectation or anticipation of being discriminated against can have negative health outcomes on stigmatized individuals. Finally, this study provides important methodological insights about conducting national level survey-based research on Asian Americans, considering the overall paucity of health communication and media effects scholarship on this racial/ethnic minority group.
Global and local disasters and health crises often lead to increases in information-seeking and media use (Xu, 2020). The public’s dependency on media sources was heightened during the pandemic, which in turn became more influential in shaping public beliefs, attitude, and behaviors (Ball-Rokeach and Jung, 2009). While media use can help communicate about virus-related health risks and preventive behaviors, it can also exacerbate psychological distress about the pandemic (Chao et al., 2020; Gao et al., 2020). Research reveals a complicated relationship between media use during times of crises and psychological distress. In certain conditions, media use can facilitate a reduction in uncertainty and engagement in protective health behaviors, both of which can foster feelings of empowerment and agency (Sakurai and Murayama, 2019). Yet, media use during health crises and other disasters has also been linked to increases in stress, anxiety, and impairments in social and work activities (Vasterman et al., 2005; Thompson et al., 2019).
Evidence suggests that during the COVID-19 pandemic, the use of both traditional and social media platforms is associated with unintended mental health consequences including stress, anxiety, panic, and depression symptoms (Ahmad and Murad, 2020; Chao et al., 2020; Gao, 2020; Ni et al., 2020; Zhao and Zhou, 2020). The uniqueness of this particular health crisis, which has led to state-mandated and/or self-imposed quarantines, may be particularly likely to amplify the effect of media use on psychological distress. Ongoing exposure to news and social media messages about the health crisis can intensify threat perceptions and activate a prolonged stress response, all of which creates a heightened vulnerability to mental health distress.
In the present study, we explore the influence of media use on three measures of mental health particularly relevant to the COVID-19 context: subjective wellbeing, loneliness, and psychosocial distress. Conceptually, mental health distress is defined by both the symptoms related to a particular stressor (e.g., anxiety about being infected by the virus) and the effect of managing that particular stressor to maintain psychosocial functioning (e.g., sadness from prolonged period of social isolation during mandated quarantine) (Terluin et al., 2004). Mental health is more than the presence or absence of distressing symptoms. Researchers have noted the importance of subjective wellbeing, which includes a global evaluation of one’s overall life (e.g., life satisfaction), experiences of mental states (e.g., happiness), and eudaimonia (e.g., feelings of purposefulness) (Dolan and Metcalfe, 2012). Psychosocial distress includes dimensions of stress related to both psychological states (e.g., anxiety, sadness, hopelessness) and social factors (e.g., relationship problems).
The long history of xenophobic treatment of Asian-American communities in the United States, which tend to be treated similarly despite considerable diversity with respect to ethnicity, language use, and country of origin, has contributed to well-documented disparities in mental health and treatment-seeking (Gee et al., 2009). Evidence suggests that there are higher levels of mental health distress in some Asian-American communities, which may be attributed, in part, to lower levels of mental health help-seeking (Nagayama Hall and Yee, 2012). Reluctance to seek mental health treatment is influenced by a variety of factors including access to affordable, culturally competent mental health care, cultural stigma related to help-seeking behaviors, and concerns about conformity to the “model minority” stereotype that suggest that Asian Americans are economically and socially successful and therefore not in need of mental health treatment (Leong and Lau, 2001; Jang et al., 2019).
Additionally, the media have perpetuated racism by framing Asian immigrants as “dirty” and “sickly” (Chou and Feagin, 2008). Even before the global health crisis caused by COVID-19, Asian Americans have long been blamed for various public health threats caused by known or newly discovered diseases and illnesses (Tessler et al., 2020). Contemporary media platforms, including traditional news media and social media, are plagued with misleading and racist messages that blame Asian Americans for the COVID-19 pandemic (Darling-Hammond et al., 2020; Le et al., 2020). President Trump’s repeated use of the terms such as “China virus” and “Chinese virus” further racialized the COVID-19 pandemic and intensified the anti-Asian sentiment (Li and Nicholson, 2021). In an investigation of the prevalence of anti-Asian sentiment on Twitter before and during the COVID-19 pandemic, Nguyen and colleagues (2020) found that there was a 68.4% increase in negative tweets referring to Asians following the emergence of the virus. Stop AAPI Hate (2021) reported that between March and December 2020 there were over 2,800 reported anti-Asian hate crimes throughout the nation. Evidence is now emerging that social media use during the COVID-19 pandemic is associated with prejudice toward Chinese Americans (Croucher et al., 2020) although more research is needed about the influence of media use on the perpetuation of racism toward Asian Americans.
Media use can exacerbate threat perceptions about the COVID-19 pandemic by activating concerns about the potential to experience social risk. One particularly relevant form of social risk is the experience of being stigmatized for real or imagined association with the COVID-19 virus. Although considerable attention has been paid to the role that media play in constructing and perpetuating stigma about social groups (Ramasubramanian and Yadlin-Segal, 2017; Dixon, 2020) and health conditions (Smith, 2007), we also need to study the effect of media on concerns about the possibility of experiencing stigma in the public sphere.
The particularities of any social stigma are dependent on the target of the stigma (i.e., the social group) but researchers generally agree that the stigma is enacted by the social avoidance and/or exclusion of, the use of derogatory and demeaning labels to describe, the endorsement of negative beliefs about and attitudes toward, and discriminatory behaviors that affect targeted group members (Link and Phelan, 2001). Of course, the absence of any of these stigma indicators does not negate the potential threat of experiencing stigma for vulnerable individuals and groups. Central to our interest in the present study is an investigation of how media use during the COVID-19 pandemic leads to imagined stigma.
The experience of imagined or anticipatory stigma is called “symbolic interaction stigma” and can be differentiated from public stigma and self-stigma, which relate to the stereotypes, prejudice, and discrimination toward a targeted group that are enacted in the public sphere and/or internalized and integrated into one’s self-concept, respectively (Link et al., 2015; Quinn et al., 2015). Symbolic interaction stigma (referred to hereafter as “imagined stigma”) occurs when a person imagines how other people will respond to a stigmatized status (e.g., a targeted racial/ethnic identity), anticipates the effect of stigmatized identity on interactions with others, and mentally rehearses how to negotiate encounters with imagined stigmatizing behaviors (Link et al., 2015). Like experiences of public and self-stigma, imagined stigma is associated with mental health distress and social isolation (Link et al., 2015; Soghoyan and Gasparyan, 2017).
To better understand the growing body of evidence that shows media use during the COVID-19 pandemic is associated with mental health distress, we suggest that it may be helpful to consider the degree to which media use affects concerns about the potential to experience stigma. Of course, concerns about vulnerability to stigma is likely more pronounced for people who are perceived to be associated with the cause and/or spread of the virus. For Asian Americans, exposure to news and social media reports about the increased anti-Asian sentiment in the United States (much of which is related to the falsehoods about the role that Asian Americans have played in the COVID-19 pandemic) may be especially likely to heighten a sense of vulnerability to stigmatizing experiences. As media use exacerbates concerns about the social risk of experiencing stigma, the intensification of mental health distress is also likely to occur. Although mental health distress can manifest in a variety of ways, we are concerned largely with the effect of media on one’s sense of subjective wellbeing and an increase in symptoms of both psychological and social (i.e., psychosocial) distress as well as feelings of social isolation (e.g., loneliness).
Just as media use has the potential to amplify concerns about the social risks related to the COVID-19 pandemic, media consumers are also likely to experience heightened concerns about the health risks of COVID-19. Indeed, it is difficult for media consumers to avoid messages about the health risks associated with COVID-19; the current information environmental is saturated with health messages aimed at educating the public about the health risks of COVID-19 and motivating preventive health behaviors to curb the spread of the virus (Garrett, 2020; Malecki et al., 2020).
Efforts to understand and document the role that media play in shaping public health behavior have focused on how media influence people’s risk perception. Both the Health Belief Model (Becker and Rosenstock, 1984) and the Extended Parallel Processing Model (the EPPM; Witte, 1992) point out that the perceived severity and susceptibility influenced the level of perceived risks and fear, which in turn affect people’s response to the risk and whether they will adopt recommended health behaviors. Indeed, a sizable corpus of research points to the integral role that media play in shaping public beliefs about the severity of and susceptibility to health risks (Wahlberg and Sjoberg, 2000). In the context of the COVID-19 pandemic, Nowak et al. (2020) found that health beliefs about severity and susceptibility predicted both preventative behaviors and also hoarding. Research conducted in different countries also shows the perceived severity and susceptibility influence individual’s intention to receive COVID-19 vaccine (Cavazos-Arroyo and de Celis-Herrero, 2020; Wong et al., 2020).
Even as current public health efforts to enhance risk perceptions about COVID-19 are important to motivate preventive behaviors that curb the spread of the virus, constant exposure to messages that heighten awareness of health risks might also have the unintentional effect of exacerbating mental health distress. Although health risk perceptions are an important determinant of health behaviors (Ferrer and Klein, 2015), there is some evidence that perceived health risks can also exacerbate psychological distress (Gibbons and Groarke, 2016). The potential for health risk perceptions to negatively affect mental health might be especially pronounced for people who feel vulnerable to the COVID-19 virus and its effects. For Asian Americans, health risk perceptions may be exacerbated by fears about the spread of the virus in Asian American communities and evidence that Asian Americans are high risk for both virus transmission and virus-related morbidity and mortality (Wang et al., 2020).
To better understand the psychological mechanisms that underlie the effects of media use on mental health distress during the COVID-19 pandemic, we propose that it is necessary to 1) investigate the relationships between media use, social and health risk perceptions, and mental health distress, and 2) to examine how racial/ethnic identity influences the negative influence of media use on both the social and health risk perceptions and mental health distress of Asian Americans. Thus, we propose the following hypotheses:
H1: Media use will be positively associated with imagined stigma (a) and health risk perceptions (b).
H2: Racial/ethnic identity will significantly affect social and health risk perceptions such that Asian Americans will report significantly higher levels of imagined stigma (a) and health risk perceptions (b) than White Americans.
H3: Racial/ethnic identity will interact with media use such that media use will be associated significantly higher levels of imagined stigma (a) and health risk perceptions (b) for Asian Americans but not White Americans.
H4: Media use will be significantly associated with mental health distress. Specifically, media use will be significantly associated with lower subjective wellbeing (a), higher psychosocial distress (b), and higher levels of loneliness (c).
H5: Racial/ethnic identity will significantly affect mental health distress such that Asian Americans will report significantly lower levels of subjective wellbeing (a), and higher levels of psychosocial distress (b), as well as loneliness (c) than White Americans.
H6: Racial/ethnic identity will significantly interact with media use such that media use will be associated with significantly lower levels of subjective wellbeing (a), more psychosocial distress (b), and more loneliness (c) for Asian Americans but not White Americans.
H7: Imagined stigma (a) and health risk perceptions (b) will mediate the effect of media use on mental health distress.
Asian (n = 524) and White (n = 527) American participants were recruited online through a Qualtrics panel (see Table 1 for demographics). The Asian Americans participants self-identified as Chinese (n = 191), South Asian (n = 103), Japanese (n = 75), Filipino (n = 69), Vietnamese (n = 49), Korean (n = 18), and Other (n = 19). White Americans in our sample were significantly younger, more liberal, and wealthier than Asian Americans. White Americans were also more likely to reside in urban areas whereas Asian Americans were more likely to reside in rural areas.
After consenting to an electronic consent form, participants completed an online survey through the Qualtrics platform. Data were collected for a 1 week period in May of 2020. Although the survey asked a range of questions, we used the following measures in the current study.
Participants were asked to what extent they “typically consume” six types of media: print, TV, internet, social, entertainment, and news media on a 1 = never and 6 = always response scale. A composite scale was created averaging the six items (M = 3.45 SD = 0.67, alpha = 0.66), which follows the tradition of existing studies that have used self-reported global estimates of media use (Vandewater and Lee, 2009).
Four items adapted from Cho and Lee (2015) assessed perceived severity of and susceptibility to COVID-19 pandemic (e.g., “Contracting COVID-19 is a very serious issue to me” and “I believe I am at risk for contracting COVID-19”) on a 1 (strongly disagree) to 5 (strongly agree) rating scale (M = 3.75, SD = 0.80, α = 0.77).
Eight items were adapted from Link et al. (2015) to assess how often individuals experienced discrimination during the COVID-19 pandemic due to their racial or ethnic identity (e.g., “Others reacting to you as if they were afraid or intimidated?” and “I received unfair treatment in a variety of contexts”). Participants responded on a 1 (never) to 5 (always) rating scale (M = 1.40, SD = 0.68, α = 0.96).
Eight items were adapted from Link et al. (2015) to assess concerns about imagined stigma during the COVID-19 pandemic (e.g., “How often do you feel people would look down on you?” and “Worry that people think of you as different from everyone else”) on a 1 (never) to 5 (always) rating scale (M = 1.64, SD = 0.81, α = 0.94).
Based on recommendations of Dolan and Metcalfe’s (2012) review of best practices for measuring subjective wellbeing, a single item measure of the evaluative dimension of subjective wellbeing was used (“Overall, how satisfied are you with your life nowadays?”), with a 1 (not at all) to 5 (very) rating scale (M = 3.29, SD = 1.06).
An eight item scale, adapted from Hyun et al. (2006) was used to assess symptoms of psychosocial distress during the COVID-19 pandemic (e.g., “How often do you experience hopelessness?” and “How often do you experience relationship problems?”), with a 1 (never) to 5 (always) response scale (M = 2.04, SD = 0.89, α = 0.93).
A three item-scale from Hughes et al. (2004) was used to measure loneliness (e.g., “How often do you lack companionship?” and “How often do you feel isolated from others?”), with a 1 (never) to 5 (always) rating scale (M = 2.13, SD = 0.97, α = 0.88).
Two items from Cornwell and Waite (2009) were used to assess and control for participants’ physical and mental health ratings (e.g., “Would you say your physical/mental health is excellent, good, average, poor, very poor?”). Responses were recoded so higher scores represent better physical/mental health (Ms = 3.81, 3.94, SDs = 0.79, 0.88, respectively).
We analyzed H1–H6 through a series of general linear models. Standardized estimates of slopes are reported below (see Table 2 for correlations among main variables and Table 3 for GLM models). To answer H7, which pertains to the mediation effects of imagined stigma and health risk perceptions, we used the PROCESS 4 Model (Hayes, 2017). Within these analyses, standard errors, indirect effects, and confidence intervals are based on 1,000 bootstrap samples. Consistent with the recommendations of Hayes (2017), unstandardized coefficients are reported for mediation analyses. Individual differences in mental and physical health and direct stigma experiences were controlled for in all analyses.
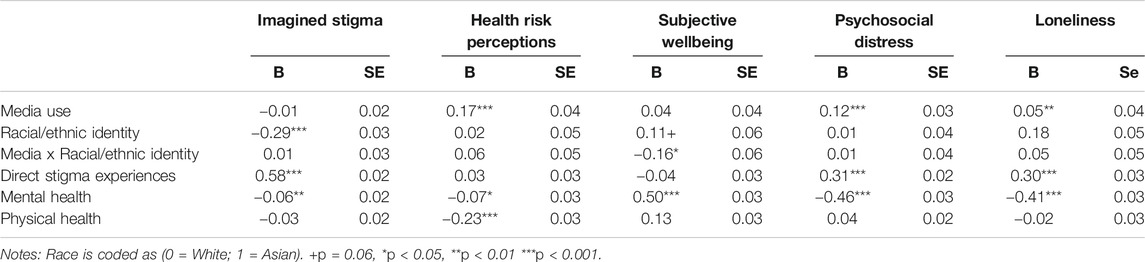
TABLE 3. General linear models results testing H1–H6 controlling for direct stigma experiences, mental health, and physical health.
The first set of analyses determined whether media use was a significant predictor of imagined stigma and health risk perceptions, the degree to which social and health risk perceptions were affected by racial/ethnic identity, and whether racial/ethnic identity interacted with media use on these social and health risk perceptions.
Media use did not significantly predict imagined stigma; therefore H1a was not supported. Racial/ethnic identity did significantly influence imagined stigma, although in the unexpected direction, F (1, 994) = 81.03, p < 0.01. Contrary to prediction, White Americans (M = 1.93, SD = 0.88) reported greater imagined stigma than Asian Americans (M = 1.35, SD = 0.62). Therefore, H2a was not supported. Racial/ethnic identity did not interact with media use; therefore, H3a was not supported.
Media use was significantly and positively associated with health risk perceptions, F (1, 994) = 69.89, b = 0.17, p < 0.001; therefore, H1b was supported. Racial/ethnic identity did not yield a significant main effect on health risk perceptions; therefore, H2b was not supported. Racial/ethnic identity did not yield an interactive effect with media use on health risk perceptions; therefore, H3b was not supported.
The next set of analyses tested whether media use was a significant predictor of mental health distress, the degree to which mental health distress was affected by racial/ethnic identity, and whether racial/ethnic identity interacted with media use to influence mental health distress.
Contrary to prediction, media use was not a significant predictor of subjective wellbeing; therefore, H4a was not supported. As expected, racial/ethnic identity yielded a marginally significant main effect, F (1, 994) = 3.42, p =0.06; however, contrary to prediction, Asian Americans reported higher subjective wellbeing (M = 3.40, SD = 1.05) than White Americans (M = 3.18, SD = 1.07). Therefore, H5a was not supported. As we predicted, there was a significant interaction between media use and racial/ethnic identity, F (1, 994) = 7.88, p < 0.01. Simple slope analyses revealed that media use was significantly and inversely associated with subjective wellbeing for Asian Americans, F (1, 495) = 9.08, b = -0.11, p < 0.01, but not White Americans, F (1, 496) = 0.95, b = 0.04, p =0.33 (see Figure 1); therefore, H6a was supported.
Media use significantly and positively predicted psychosocial distress, F (1, 994) = 32.56, b = 0.12, p < 0.01; therefore, H4b was supported. The main effect of racial/ethnic identity on psychosocial distress was not significant; therefore, H5b was not supported. Contrary to prediction, there was no interaction between racial/ethnic identity and media use; therefore, H6b was not supported.
Media use significantly and positively influenced loneliness, F (1, 994) = 9.93, b = 0.05, p < 0.01; therefore, H4c was supported. Neither the main effect of racial/ethnic identity nor its interaction with media use was significant in this model; H5c and H6c were not supported.
The final set of analyses were conducted to explore whether imagined stigma and health risk perceptions mediated the effects of media use on mental health distress (see Table 4 for indirect effects of each mediator on three mental health distress measures).
Contrary to prediction, imagined stigma did not significantly mediate the effect of media use on any of the three measures of mental health distress; therefore, H7a was not supported.
Contrary to prediction, health risk perceptions did not significantly mediate the influence of media use on subjective wellbeing. However, the results indicated that health risk perceptions significantly mediated the effect of media use on both psychosocial distress and loneliness. Therefore, H7b received partial support.
As media users rely more heavily on media sources for information about and distraction from the health crisis (Koeze and Popper, 2020; Liu et al., 2020), it is critical to understand both the underlying mechanisms through which media use influences mental health and the extent to which particular identity characteristics, like race and ethnicity, make certain people more vulnerable to such influences. The purpose of this study was to investigate the influence of media use during the COVID-19 pandemic on the mental health distress of Asian Americans and White Americans. To better understand the psychological processes underlying the relationship between media use and mental health, we examined the effect of media use on perceptions about both the social and health risks related to the COVID-19 pandemic. Central to the goal of this investigation is our interest in exploring whether the relationship between media use and mental health distress is more pronounced for Asian Americans, for whom the increased presence of anti-Asian public discourse, racism, and discriminatory behavior is likely to have deleterious effects.
The results indicate that the relationship between media use and mental health distress is more complex than originally predicted. Media use had a significant direct effect on two of the three measures of mental health distress: media use was positively associated with psychosocial distress and loneliness but it was not a significant predictor of subjective wellbeing. These findings may be a function of measurement differences in the mental health constructs of interest. Whereas the measures of psychosocial distress and loneliness assess the presence of ego-dystonic mental health (e.g., hopelessness, loneliness, sadness), the measure of subjective wellbeing assesses an ego-syntonic facet of mental health (i.e., general life satisfaction). For scholars who seek to better understand the effect of media use on mental health, these findings point the importance of using different measures to capture the various dimensions of psychosocial wellbeing. Further exploration of how media use might differentially impact the positive (i.e., ego-syntonic) and negative (i.e., ego-dystonic) dimensions of mental health is warranted.
The results also revealed surprising findings about how racial/ethnic identity influenced the effect of media use on mental health distress. Although racial/ethnic identity did not influence the effect of media on psychosocial distress or loneliness, the results indicated that media use had a negative effect on subjective wellbeing for Asian Americans, but not White Americans. Even as the Asian Americans in our sample reported higher subjective wellbeing than White Americans, it appears that media use might reverse whatever buffering effect racial/ethnic identification may have on wellbeing. Our findings confirm that Asian Americans are particularly vulnerable to the negative mental health effects of media use. Coupled with the unique identity experiences of Asian Americans who are presently experiencing heightened levels of anti-Asian sentiment, media use appears to exacerbate mental health distress. These findings are consistent with other work in which frequent social identity threats, experienced via interpersonal discrimination and exposure to negative media images of one’s in-group members, lead to adverse social psychological outcomes for racial/ethnic minorities (Saleem et al., 2019; Saleem and Ramasubramanian, 2019).
The findings reveal that even as media use had a direct influence on mental health distress, this influence was partially mediated by risk perceptions. In the current investigation, we explored the effect of media use on one particular kind of social risk: imagined stigma, which is conceptualized by the anticipatory effect of one’s stigmatized status on interactions with others (Link et al., 2015). The findings show imagined stigma was directly associated with all three measures of mental health distress (i.e., less subjective wellbeing, more psychosocial distress, and loneliness); however, contrary to prediction, media use did not directly predict imagined stigma. Therefore, imagined stigma did not mediate the effect of media use on mental health distress and there was no significant interaction between media use and racial/ethnic identity on imagined stigma. It may be that the nature of media consumption, rather than the totality of time spent with media (as was measured in this study), is a better predictor of the effect of media on the anticipation of stigmatizing experiences. One can imagine how exposure to specific genres (e.g., news content) or social media content (e.g., a trending story about yet another act of racist, anti-Asian behavior) might be more likely to prime ruminations and fear about the possibility of experiencing stigma.
One unexpected finding was that White Americans reported higher levels of imagined stigma than Asian Americans. We suggest that these findings may be a function of the effect of fears about both social and health risks related to the COVID-19 pandemic faced by all racial and ethnic identity groups. It is reasonable to expect heightened concerns and even fears about social interactions during a time of great global uncertainty. Even though general media use was not a predictor of imagined stigma, it is possible that exposure to disturbing news and social media stories about the public shaming of people who fail (or are perceived to fail) to take recommended actions to protect themselves or other from the virus (e.g., not wearing a mask) might prime fears about experiencing COVID-19-related discrimination. The effect of the COVID-19 pandemic on imagined stigma might have been worse for White Americans for whom racial/ethnic identity has often afforded protections against real or imagined stigmatizing experiences. These findings point to the importance of continuing to explore environmental, social, and identity factors that facilitate imagined stigma and its influence on mental health.
Unlike imagined stigma, health risk perceptions did mediate the influence of media use on mental health distress. Media use had a direct effect on health risk perceptions about the severity of and susceptibility to the COVID-19 pandemic. Health risk perceptions mediated the effect of media use on both psychosocial distress and loneliness but not subjective wellbeing. Contrary to expectation, racial/ethnic identity did not have a direct on health risk perceptions, nor was there was there an interaction between identity, media use, and health risk perceptions. It seems that for Asian and White Americans alike, the effect of media use on mental health distress was mediated by concerns about susceptibility to and the severity of the COVID-19 pandemic. The effect of racial/ethnic identity on media use might function differently when the media landscape, regardless of genre and platform, is full of health information and warnings about health risks associated with the coronavirus. The finding that health risk perceptions mediate the negative effect of media use on mental health distress for all media consumers points to the need for further exploration of why, and under what conditions, health risk perceptions have useful or deleterious effects on mental wellbeing.
The findings from this study have theoretical implications for health communication scholarship, media psychology, and Asian American studies. They provide insights into the theoretical mechanisms underlying the ways in which media use during COVID-19 shape mental health distress through imagined stigma and heightened health risk perceptions. By comparing Asian Americans to White Americans, these findings have implications for ethnic/race studies scholars to understand the psychosocial vulnerabilities for racial and ethnic minorities during the COVID-19 pandemic.
There is very little scholarship about Asian American media use and effects within the media psychology literature (Ramasubramanian, 2011; Ramasubramanian et al., 2017). This study adds significantly to this sparse literature by providing a better understanding of how and why racist media portrayals lead to negative health outcomes for racial/ethnic audiences. This is an especially understudied topic in the context of Asian American media use. Another theoretical contribution of this paper is its emphasis on imagined stigma. Previous studies on stigma and prejudice within media effects and health communication have typically included actual discrimination experiences. However, our study shows that it is also important to consider the negative health outcomes of anticipated stigma experiences on marginalized individuals. Indeed, the finding that imagined stigma was negatively associated with all three measures of mental health distress points to the importance of understanding how imagined stigma by itself functions as a mental health risk factor. By incorporating these subtle and indirect forms of stigma in our measures, health communication scholars can better understand the ways in which media stereotypes influence minoritized populations. Even as this study illuminates our understanding of the mental health influence of media use during a particularly vulnerable historical moment (i.e., the COVID-19 pandemic), the findings reported here contribute to the growing corpus of research that seeks to address the important role of racial/ethnic identity in media effects scholarship (Ramasubramanian and Banjo, 2020). The fact that media use differentially affects the mental health distress of racially/ethnically distinct groups is both theoretically and practically significant and invites further exploration of how racial/ethnic identity moderates media effects related to other facets of mental health and wellbeing.
In terms of practical implications, our study findings have relevance to media practitioners, journalists, and content creators. Even as there is some history of scholarly inquiry about how media frame racial minorities, like Asian Americans, the results of this study point to the need to continue to actively investigate the effects of media framing and use during the COVID-19 pandemic. During this time when media dependency is particularly heightened for media consumers who wish to learn about the pandemic, journalists and media producers need to be extra attentive to the ways in which framing of COVID-19 news stories, especially about health risks, could lead to greater imagined stigma and heightened sense of vulnerability for Asian American viewers.
These findings also have implications for health care practitioners such as mental health professionals and physicians. Given the role of media in shaping mental health distress and affecting subjective wellbeing and psychosocial distress, care providers should include and explicitly address media use as a way to buffer oneself from mental health distress, especially during the COVID-19 pandemic and particularly for people who belong to racial/ethnic minority communities. Even as there is growing scholarly interest in how media use impacts mental health and illness experiences, far less attention has been given to specific psychological mechanisms, such as imagined stigma, that can be targeted in psychotherapeutic treatments aimed at correcting the negative influence of media on mental health. The present study offers some evidence that the development of tools designed to both assess the impact of and offer treatment interventions for media use in mental health treatment may be warranted.
The finding that media use mediates risk perceptions, which can function as important predictors of psychosocial distress and loneliness, demonstrates the importance diversifying theoretical and methodological approaches to understanding how media use influences mental health. Efforts to understand the direct effect of media use on mental health outcomes have the potential to neglect how media use activates important psychological processes and perceptions that mediate the effect of media use on mental health distress; future studies should continue to explore both direct and indirect media effects on mental health.
These findings also have implications for ongoing efforts aimed at developing culturally sensitive mental health care; given the historic difficulty with access to and engagement with mental health care in the United States, it might be beneficial to understand how culturally appropriate media messaging about media use can be used to address and improve mental health in Asian American communities. Although our interest in exploring the negative effect of media use during a time when mental health vulnerabilities are particularly heightened because of the COVID-19 pandemic, future research should also explore whether media content (e.g., entertainment vs. news content), attentional processes (e.g., passive vs. active use), and motivations (e.g., escapism or social support) buffer media consumers from these and other mental health outcomes. Our findings illustrate the important role that this and future media effects studies can play in multidisciplinary efforts aimed at helping media consumers and mental healthcare professionals to understand and correct the processes through which media use exacerbate mental health vulnerabilities.
The study is not without limitations. For one, a cross-sectional survey like this, even with a national sample of participants, only provides a snapshot of how media use influences mental health. Future research needs to look at longitudinal studies and experimental research in order to ascertain the intervening variables and theoretical mechanisms. In the present study, we measured how much time respondents spent with various kinds of media in order to ascertain a global estimate of media use. The use of self-reported global estimates of media use are common, in part, because they are inexpensive, easy to administer, and, most importantly, because they reflect the normative tradition of media measurement in major, nationally representative surveys (e.g., the National Health and Nutrition Examination Surveys, the Kaiser Family Foundation Surveys, the National Institute of Child Health and Human Development Study, etc.) that have played a critical role in shaping scholarship and public discourse about media effects (Vandewater and Lee, 2009). However, the treatment of media use as a single item (i.e., a composite average) fails to capture the complexity of media exposure conditions and important content characteristics that may influence the observed relationships (De Vreese and Neijens, 2016). Nonetheless, the findings reported in this study offer a snapshot about the direct and mediating effect of media use on psychosocial wellbeing. Future research should consider alternative measurement approaches to explore the direct and indirect effects of media use on mental health; knowing more precisely how attentional and content exposure experiences impact mental wellbeing would be especially useful for mental health care treatment.
These data were collected in late spring 2020, when anti-Asian hate crimes had increased tremendously. Later in the summer, with the Black Lives Matter movement, the largest uprising in the history of the United States, we saw a greater awareness about racism, especially anti-Black racism, in the United States Therefore, it is possible that the negative effects of media use on minoritized populations’ mental health will decrease as media framing of protests and racism changes. Another important point is that Asian Americans are a diverse group consisting of multiple nationalities, sub- and co-cultures, and life experiences; this diversity is not captured in our treatment of all Asian Americans as a single racial/ethnic group. Even as we recognize that this categorization of complex identity groups has the potential to reify an overly simplistic social construction of Asian racial and ethnic identities, we believe our interest in comparing the experiences of people who self-identify as Asian Americans with people who self-identify as White Americans justifies this approach. Of course, it is possible that some Asian Americans who were feeling especially vulnerable may have decided not to participate in studies such as this. Despite these limitations, our findings offer important and significant insights about how media use affects the mental health of Asian Americans as compared to White Americans.
In sum, these findings reveal the complexity of the relationship between media use and social and health risk perceptions. Although conventional wisdom suggests that the power of media to heighten public attention to health crises and amplify health risk perceptions is beneficial, our findings suggest that the effect of media use on health risk perception might have the unintended effect of intensifying mental health distress, especially for Asian Americans. The power of the media to amplify concerns about social and health risks and exacerbate mental health vulnerabilities is particularly concerning during this time when uncertainty about the nature and trajectory of COVID-19 global health pandemic remains uncertain. It is important to consider the ways in which racial/ethnic minorities such as Asian Americans can regulate their media use as a way to buffer themselves from the negative mental health outcomes caused by heightened sense of vulnerability and stigma experiences.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by University of Massachusetts Boston Institutional Review Board. The patients/participants provided their written informed consent to participate in this study.
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ahmad, A. R., and Murad, H. R. (2020). The Impact of Social Media on Panic during the COVID-19 Pandemic in Iraqi Kurdistan: Online Questionnaire Study. J. Med. Internet Res. 22 (5), e19556. doi:10.2196/19556
Austin, L., Fisher Liu, B., and Jin, Y. (2012). How Audiences Seek Out Crisis Information: Exploring the Social-Mediated Crisis Communication Model. J. Appl. Commun. Res. 40 (2), 188–207. doi:10.1080/00909882.2012.654498
Ball-Rokeach, S. J., and Jung, J. Y. (2009). “The Evolution of Media System Dependency Theory,” in The Sage Handbook of Media Processes and Effects. Editors R. Nabi, and M. B. Oliver (Los Angeles, CA: Sage Publications), 531–544.
Becker, M. H., and Rosenstock, I. M. (1984). “Compliance with Medical Advice,” in Health Care and Human Behavior. Editors A. Steptoe, and A. Matthews (Academic Press), 135–152.
Cavazos-Arroyo, J., and de Celis-Herrero, P. (2020). Severidad, susceptibilidad y normas sociales percibidas como antecedentes de la intención de vacunarse contra coviD-19. Revista de Salud Pública 22 (2), 1–7. doi:10.15446/rsap.v22n2.86877
Chao, M., Xue, D., Liu, T., Yang, H., and Hall, B. J. (2020). Media Use and Acute Psychological Outcomes during COVID-19 Outbreak in China. J. Anxiety Disord. 74, 102248. doi:10.1016/j.janxdis.2020.102248
Cho, H., and Lee, J.-S. (2015). The Influence of Self-Efficacy, Subjective Norms, and Risk Perception on Behavioral Intentions Related to the H1N1 Flu Pandemic: A Comparison between Korea and the US. Asian J. Soc. Psychol. 18, 311–324. doi:10.1111/ajsp.12104
Chou, R., and Feagin, J. R. (2008). The Myth of the Model Minority: Asian Americans Facing Racism. Boulder, CO: Paradigm Publishers.
Chowkwanyun, M., and Reed, A. L. (2020). Racial Health Disparities and Covid-19 - Caution and Context. N. Engl. J. Med. 383, 201–203. doi:10.1056/NEJMp2012910
Cornwell, E. Y., and Waite, L. J. (2009). Social Disconnectedness, Perceived Isolation, and Health Among Older Adults. J. Health Soc. Behav. 50 (1), 31–48. doi:10.1177/002214650905000103
Croucher, S. M., Nguyen, T., and Rahmani, D. (2020). Prejudice toward Asian Americans in the COVID-19 Pandemic: the Effects of Social Media Use in the United States. Front. Commun. 5, 39. doi:10.3389/fcomm.2020.00039
Darling-Hammond, S., Michaels, E. K., Allen, A. M., Chae, D. H., Thomas, M. D., Nguyen, T. T., et al. (2020). After “The China Virus” Went Viral: Racially Charged Coronavirus Coverage and Trends in Bias against Asian Americans. Health Educ. Behav. 47, 870–879. doi:10.1177/1090198120957949
de Vreese, C. H., and Neijens, P. (2016). Measuring Media Exposure in a Changing Communications Environment. Commun. Methods Measures 10 (2-3), 69–80. doi:10.1080/19312458.2016.1150441
Dixon, T. L. (2020). “Media Stereotypes: Content, Effects, and Theory,” in Media Effects: Advances in Theory and Research. Editors M. B. Oliver, A. A. Raney, and J. Bryant 4th Edn. (Routledge), 243–257.
Dolan, P., and Metcalfe, R. (2012). Measuring Subjective Wellbeing: Recommendations on Measures for Use by National Governments. J. Soc. Pol. 41 (2), 409–427. doi:10.1017/s0047279411000833
Ferrer, R. A., and Klein, W. M. (2015). Risk Perceptions and Health Behavior. Curr. Opin. Psychol. 5, 85–89. doi:10.1016/j.copsyc.2015.03.012
Frohlich, K. L., and Potvin, L. (2008). Transcending the Known in Public Health Practice. Am. J. Public Health 98 (2), 216–221. doi:10.2105/ajph.2007.114777
Gao, J., Zheng, P., Jia, Y., Chen, H., Mao, Y., Chen, S., et al. (2020). Mental Health Problems and Social Media Exposure during COVID-19 Outbreak. PLoS One 15 (4), e0231924. doi:10.1371/journal.pone.0231924
Garrett, L. (2020). COVID-19: the Medium Is the Message. Lancet. 395 (10228), 942-943. doi:10.1371/journal.pone.0231924
Gee, G. C., Ro, A., Shariff-Marco, S., and Chae, D. (2009). Racial Discrimination and Health Among Asian Americans: Evidence, Assessment, and Directions for Future Research. Epidemiologic Rev. 31 (1), 130–151. doi:10.1093/epirev/mxp009
Gibbons, A., and Groarke, A. (2016). Can Risk and Illness Perceptions Predict Breast Cancer Worry in Healthy Women? J. Health Psychol. 21 (9), 2052–2062. doi:10.1177/1359105315570984
Gover, A. R., Harper, S. B., and Langton, L. (2020). Anti-Asian Hate Crime during the CoViD-19 Pandemic: Exploring the Reproduction of Inequality. Am. J. Crim Just 45 (4), 647–667. doi:10.1007/s12103-020-09545-1
Hayes, A. F. (2017). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York, NY: Guilford publications.
Holmes, E. A., O'Connor, R. C., Perry, V. H., Tracey, I., Wessely, S., Arseneault, L., et al. (2020). Multidisciplinary Research Priorities for the COVID-19 Pandemic: a Call for Action for Mental Health Science. Lancet Psychiatry 7 (6), 547–560. doi:10.1016/s2215-0366(20)30168-1
Hughes, M. E., Waite, L. J., Hawkley, L. C., and Cacioppo, J. T. (2004). A Short Scale for Measuring Loneliness in Large Surveys. Res. Aging 26 (6), 655–672. doi:10.1177/0164027504268574
Hyun, J. K., Quinn, B. C., Madon, T., and Lustig, S. (2006). Graduate Student Mental Health: Needs Assessment and Utilization of Counseling Services. J. Coll. Student Development 47 (3), 247–266. doi:10.1353/csd.2006.0030
Jang, Y., Yoon, H., Park, N. S., Rhee, M.-K., and Chiriboga, D. A. (2019). Mental Health Service Use and Perceived Unmet Needs for Mental Health Care in Asian Americans. Community Ment. Health J. 55 (2), 241–248. doi:10.1007/s10597-018-0348-3
Kahlor, L. (2010). PRISM: A Planned Risk Information Seeking Model. Health Commun. 25 (4), 345–356. doi:10.1080/10410231003775172
Kantamneni, N. (2020). The Impact of the COVID-19 Pandemic on Marginalized Populations in the United States: A Research Agenda. J. Vocational Behav. 119, 103439. doi:10.1016/j.jvb.2020.103439
Koeze, E., and Popper, N. (2020). The Virus Changed the Way We Internet. The New York Times. https://www.nytimes.com/interactive/2020/04/07/technology/coronavirus-internet-use.html.
Le, T. K., Cha, L., Han, H.-R., and Tseng, W. (2020). Anti-Asian Xenophobia and Asian American COVID-19 Disparities. Am. J. Public Health 110 (9), 1371–1373. doi:10.2105/ajph.2020.305846
Leong, F. T. L., and Lau, A. S. L. (2001). Barriers to Providing Effective Mental Health Services to Asian Americans. Ment. Health Serv. Res. 3 (4), 201–214. doi:10.1023/a:1013177014788
Li, Y., and Nicholson, H. (2021). When “Model Minorities” Become “Yellow Peril” – Othering and the Racialization of Asian Americans in the COVID-19 Pandemic. Sociol. Compass. 15 (2), e12849. doi:10.1111/soc4.12849
Link, B. G., and Phelan, J. C. (2001). Conceptualizing Stigma. Annu. Rev. Sociol. 27 (1), 363–385. doi:10.1146/annurev.soc.27.1.363
Link, B. G., Wells, J., Phelan, J. C., and Yang, L. (2015). Understanding the Importance of “symbolic Interaction Stigma”: How Expectations about the Reactions of Others Adds to the Burden of Mental Illness Stigma. Psychiatr. Rehabil. J. 38 (2), 117–124. doi:10.1037/prj0000142
Liu, P. L. (2020). COVID-19 Information Seeking on Digital Media and Preventive Behaviors: The Mediation Role of Worry. Cyberpsychology, Behav. Soc. Networking. 23 (10), 677–682. doi:10.1089/cyber.2020.0250
Malecki, K., Keating, J. A., and Safdar, N. (2020). Crisis Communication and Public Perception of COVID-19 Risk in the Era of Social Media. Clin. Infect. Dis. 72 (4), 697–702. doi:10.1093/cid/ciaa758
Misra, S., Le, P. D., Goldmann, E., and Yang, L. H. (2020). Psychological Impact of Anti-asian Stigma Due to the COVID-19 Pandemic: A Call for Research, Practice, and Policy Responses. Psychol. Trauma Theor. Res. Pract. Pol. 12 (5), 461–464. doi:10.1037/tra0000821
Nagayama Hall, G. C., and Yee, A. H. (2012). U.S. Mental Health Policy: Addressing the Neglect of Asian Americans. Asian Am. J. Psychol. 3 (3), 181–193. doi:10.1037/a0029950
Nguyen, T. T., Criss, S., Dwivedi, P., Huang, D., Keralis, J., Hsu, E., et al. (2020). Exploring U.S. Shifts in Anti-asian Sentiment with the Emergence of COVID-19. Int J Environ Res Public Health. 17 (19), 7032. doi:10.3390/ijerph17197032
Nowak, B., Brzóska, P., Piotrowski, J., Sedikides, C., Żemojtel-Piotrowska, M., and Jonason, P. K. (2020). Adaptive and Maladaptive Behavior during the COVID-19 Pandemic: The Roles of Dark Triad Traits, Collective Narcissism, and Health Beliefs. Personal. Individual Differences 167, 110232. doi:10.1016/j.paid.2020.110232
Pfefferbaum, B., and North, C. S. (2020). Mental Health and the Covid-19 Pandemic. N. Engl. J. Med. 383 (6), 510–512. doi:10.1056/nejmp2008017
Phan, M. Y., Yang, L., Leung, C. M., Li, N., Yao, X. I., and Wang, Y (2020). Mental Health, Risk Factors, and Social Media Use during the COVID-19 Epidemic and Cordon Sanitaire Among the Community and Health Professionals in Wuhan, China: Cross-Sectional Survey. JMIR Ment. Health. 7 (5), e19009. doi:10.2196/19009
Quinn, D. M., Williams, M. K., and Weisz, B. M. (2015). From Discrimination to Internalized Mental Illness Stigma: The Mediating Roles of Anticipated Discrimination and Anticipated Stigma. Psychiatr. Rehabil. J. 38 (2), 103–108. doi:10.1037/prj0000136
Rajkumar, R. P. (2020). COVID-19 and Mental Health: A Review of the Existing Literature. Asian J. Psychiatry. 52, 102066–102070. doi:10.1016/j.ajp.2020.102066
Ramasubramanian, S., and Banjo, O. O. (2020). Critical Media Effects Framework: Bridging Critical Cultural Communication and Media Effects through Power, Intersectionality, Context, and Agency. J. Commun. 70 (3), 379–400. doi:10.1093/joc/jqaa014
Ramasubramanian, S., Doshi, M., and Saleem, M. (2017). Mainstream versus Ethnic Media: How They Shape Self-Esteem and Ethnic Pride Among Ethnic Minority Audiences. Int. J. Commun. 11, 1879–1899.
Ramasubramanian, S. (2011). Television Exposure, Model Minority Portrayals, and Asian-American Stereotypes: An Exploratory Study. J. Intercultural Commun. 26. http://www.immi.se/intercultural/nr26/ramasubramanian.htm
Ramasubramanian, S., and Yadlin‐Segal, A. (2017). “Stigma: Media Influence on,” in The International Encyclopedia of Media Effects. Editors P. Rössler, C. A. Hoffner, and L. Zoonen doi:10.1002/9781118783764.wbieme0159
Reny, T. T., and Barreto, M. A. (2020). Xenophobia in the Time of Pandemic: Othering, Anti-asian Attitudes, and COVID-19. Politics, Groups, and Identities, 1–24. doi:10.1080/21565503.2020.1769693
Sakurai, M., and Murayama, Y. (2019). Information Technologies and Disaster Management - Benefits and Issues -. Prog. Disaster Sci. 2, 100012. doi:10.1016/j.pdisas.2019.100012
Saleem, M., and Ramasubramanian, S. (2019). Muslim Americans' Responses to Social Identity Threats: Effects of Media Representations and Experiences of Discrimination. Media Psychol. 22 (3), 373–393. doi:10.1080/15213269.2017.1302345
Saleem, M., Wojcieszak, M. E., Hawkins, I., Hawkins, I., Li, M., and Ramasubramanian, S. (2019). Social Identity Threats: How Media and Discrimination Affect Muslim Americans' Identification as Americans and Trust in the U.S. Government. J. Commun. 69 (2), 214–236. doi:10.1093/joc/jqz001
Smith, R. (2007). Media Depictions of Health Topics: Challenge and Stigma Formats. J. Health Commun. 12 (3), 233–249. doi:10.1080/10810730701266273
Soghoyan, A., and Gasparyan, K. (2017). “Mental Health and Stigma,” in Global Mental Health. Editors S. Bährer-Kohler, and F. Carod-Artal (Gewerbestrasse: Springer Nature), 61–69. doi:10.1007/978-3-319-59123-0_6
Stop AAPI Hate (2021). Stop AAPI Hate: New Data on Anti-asian Hate Incidents against Elderly and Total National Incidents in 2020. https://stopaapihate.org/reportsreleases/
Terluin, B., Rhenen, W. V., Schaufeli, W. B., and De Haan, M. (2004). The Four-Dimensional Symptom Questionnaire (4DSQ): Measuring Distress and Other Mental Health Problems in a Working Population. Work & Stress 18 (3), 187–207. doi:10.1080/0267837042000297535
Tessler, H., Choi, M., and Kao, G. (2020). The Anxiety of Being Asian American: Hate Crimes and Negative Biases during the COVID-19 Pandemic. Am. J. Crim Justice, 1–11. doi:10.1007/s12103-020-09541-5
Thompson, R. R., Jones, N. M., Holman, E. A., and Silver, R. C. (2019). Media Exposure to Mass Violence Events Can Fuel a Cycle of Distress. Sci. Adv. 5 (4), eaav3502. doi:10.1126/sciadv.aav3502
Vandewater, E. A., and Lee, S.-J. (2009). Measuring Children's Media Use in the Digital Age. Am. Behav. Scientist 52 (8), 1152–1176. doi:10.1177/0002764209331539
Vasterman, P., Yzermans, C. J., and Dirkzwager, A. J. E. (2005). The Role of the Media and Media Hypes in the Aftermath of Disasters. Epidemiologic Rev. 27 (1), 107–114. doi:10.1093/epirev/mxi002
Wahlberg, A. A. F., and Sjoberg, L. (2000). Risk Perception and the Media. J. Risk Res. 3 (1), 31–50. doi:10.1080/136698700376699
Wang, D., Gee, G. C., Bahiru, E., Yang, E. H., and Hsu, J. J. (2020). Asian-Americans and Pacific Islanders in COVID-19: Emerging Disparities amid Discrimination. J. Gen. Intern. Med. (12), 353685–353688. doi:10.1007/s11606-020-06264-5
Witte, K. (1992). Putting the Fear Back into Fear Appeals: The Extended Parallel Process Model. Commun. Monogr. 59 (4), 329–349. doi:10.1080/10410236.2012.708633
Wong, L. P., Alias, H., Wong, P.-F., Lee, H. Y., and AbuBakar, S. (2020). The Use of the Health Belief Model to Assess Predictors of Intent to Receive the COVID-19 Vaccine and Willingness to Pay. Hum. Vaccin. Immunother. 16 (9), 2204–2214. doi:10.1080/21645515.2020.1790279
Xiong, J., Lipsitz, O., Nasri, F., Lui, L. M. W., Gill, H., Phan, L., et al. (2020). Impact of COVID-19 Pandemic on Mental Health in the General Population: A Systematic Review. J. Affective Disord. 277, 55–64. doi:10.1016/j.jad.2020.08.001
Xu, J. (2020). Does the Medium Matter? A Meta-Analysis on Using Social Media vs. Traditional Media in Crisis Communication. Public Relations Rev. 46 (4), 101947. doi:10.1016/j.pubrev.2020.101947
Keywords: mental health, Asian Americans, media use, stigma, risk perceptions
Citation: Quintero Johnson JM, Saleem M, Tang L, Ramasubramanian S and Riewestahl E (2021) Media Use During COVID-19: An Investigation of Negative Effects on the Mental Health of Asian Versus White Americans. Front. Commun. 6:638031. doi: 10.3389/fcomm.2021.638031
Received: 04 December 2020; Accepted: 15 April 2021;
Published: 28 April 2021.
Edited by:
Iccha Basnyat, James Madison University, United StatesReviewed by:
Rafael Obregon, UNICEF United Nations International Children's Emergency Fund, United StatesCopyright © 2021 Quintero Johnson, Saleem, Tang, Ramasubramanian and Riewestahl. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jessie M. Quintero Johnson, SmVzc2llLnF1aW50ZXJvQHVtYi5lZHU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.