- 1Department of Psychology, Michigan State University, East Lansing, MI, United States
- 2Department of Psychology, University of Waterloo, Waterloo, ON, Canada
When the 2019 novel coronavirus disease (COVID-19) was rapidly spreading in China in early 2020, China's National Health Commission quickly responded to the psychological crisis by issuing guidelines for establishing mental health intervention systems, including providing psychological assistance hotlines. However, recent critiques have emphasized China's lack of pre-established mental health interventions which resulted in an inefficient response. This is the first empirical study to systematically examine mental health service use in China during the COVID-19 outbreak. The current study focused on the use of mental health hotlines in a Northern Chinese region. This region originally had a regional level hotline. During the outbreak, 12 out of its 16 sub-regional juridical areas started providing their own hotlines. Data regarding the regional level hotline and the 12 sub-regional level hotlines were obtained, including daily number of calls received, strategies for disseminating hotline services, and callers' expressed concerns. Confirmed COVID-19 cases in China, in the region, and in each of the sub-regional juridical area were also recorded daily during China's peak period of COVID-19. Analyses of these data revealed that the mental health hotlines tended to have low usage overall. Hotlines that merely provided their numbers to community centers and quarantine centers tended to receive few calls. Hotlines that encouraged individuals to advertise the service on personal social media accounts tended to receive more calls. The daily number of confirmed COVID-19 cases in the country was closely related the number of phone calls received at the regional hotline. Sub-regional hotline operators reported that a significant proportion of callers had concerns about contracting COVID-19, negative emotions from prolonged social isolation, and family conflicts while stay-at-home policies were implemented. It was also observed that the sub-regional level hotlines did not start until COVID-19 cases in the country started to decline. Overall, the psychological assistance hotlines provided during COVID-19 satisfied some mental health needs. However, consistent with recent commentaries, the hotline services were not established during the time that demand likely peaked. Future studies are warranted to determine the best strategies to improve the accessibility of mental health hotline services.
Introduction
In 2019, China was the first country to be affected by the novel coronavirus disease (COVID-19), which would eventually become a worldwide pandemic. The initial COVID-19 outbreak occurred in the city of Wuhan, located in Central China, in December 2019. In January 2020, the number of confirmed cases and deaths due to COVID-19 rapidly increased in China. There were then significant concerns regarding the impact of COVID-19 on the mental health of the Chinese public (e.g., Dong and Bouey, 2020; Liu et al., 2020). Several studies have since reported emotional distress and symptoms of anxiety and depression experienced by people in China (Wang et al., 2020; Xiang et al., 2020; Zhou, 2020). A national study of 52,730 Chinese individuals revealed that 35% experienced psychological distress during the COVID-19 pandemic (Qiu et al., 2020). Soon after COVID-19 started to rapidly spread in China, on January 27th, 2020, The National Health Commission of the People's Republic of China (NHCC) issued guidelines for responding to the psychological crisis and distress created by the disease (National Health Commission of China, 2020c).
However, recent commentaries suggested that the country's organization and management models for psychological interventions still had much to improve (e.g., Dong and Bouey, 2020; Duan and Zhu, 2020; Xiang et al., 2020). Commentaries indicated that the guidelines issued by the NHCC were overly general, providing no specification about how different resources should be delivered to which group of individuals (Dong and Bouey, 2020). Additionally, the practical implementation of mental health services was challenged by unestablished intervention systems and the inadequacy of authoritative mental health organizations (Duan and Zhu, 2020). China lacked a pre-existing and well-established organization and management models for mental health interventions. Therefore, it was relatively difficult for China to efficiently respond to the sudden need for psychological services brought by the COVID-19 crisis. The commentaries provided general directions for establishing and improving mental health response systems in China. For instance, Dong and Bouey (2020) emphasized the importance of proactively establishing community resources, planning for psychological interventions, and implementing preventative strategies before the occurrence of emergency events.
Despite these general recommendations, no empirical studies have systematically examined any type of mental health service in any area of China during the COVID-19 outbreak. Therefore, there are neither specific points of intervention nor steps toward resolution available for Chinese mental health service providers. Chinese mental health service providers are then unable to consider, establish, or improve the system, particularly in the context of crisis response. The service providers are left with the same issue they had faced while responding to the psychological crisis associated with the COVID-19 pandemic, namely, not having specific guidance for a potential next step of implementation.
Psychological assistance hotlines can quickly connect a person in need with a provider. Their implementation formed an important part of the mental health strategy in China during COVID-19 (National Health Commission of China, 2020a,b). The first mental health intervention guidelines issued by the NHCC on January 27th specified that interventions, including psychological assistance hotlines, should be organized at each juridical level (National Health Commission of China, 2020c). On February 2nd, 2020, the NHCC issued a notice for the provinces of China to establish the psychological assistance hotlines (National Health Commission of China, 2020b). The particular guidelines for the establishment followed soon on February 7th, 2020 (National Health Commission of China, 2020a).
Psychological Assistance Hotlines in China
The first psychological assistance hotlines were established in China in the late 1980s (Zhang et al., 1995) (Zhang et al., 1 when it became increasingly common for families to own telephones (e.g.,0.4% of families in Shanghai owned telephones in 1984 compared to 30.3% in 1994; Ji, 1995). The Shanghai Mental Health Hotline (Shanghai is an Eastern-Central Chinese area, within Southern China) was one of the first general psychological assistance hotlines in China. From 1990 to 1992, it received 14,667 calls from all over the country (Ji, 1995). Of these calls, 8,214 had complete records available. An analysis of these records revealed that the majority of calls were concerning intimate or family relationships (Ji, 1995). A significant proportion (12.4%) of the 8,214 calls sought assistance about emotional issues such as depression and anxiety (Ji, 1995). Over the next years, this hotline witnessed an increasing proportion of calls that presented emotional concerns, from 20.3% in 1995 to 31.5% in 1999 (Cheng et al., 2000). An analysis of the Shanghai hotline data over the decade from 1990 to 2000 concluded that hotline counseling provided effective mental health intervention (Zhu et al., 2005).
In addition to general psychological assistance hotlines, the Nanjing Crisis Intervention Center (located in an Eastern-Central Chinese area within Southern China) set up the first crisis intervention hotline in China in 1991 (Xie et al., 1996). This hotline was primarily aimed at suicide prevention. Over the first 4 years of operation, this crisis intervention hotline received over 4,000 calls (Xie et al., 1996).
Few records are available regarding hotline operations in Northern China until early 2000. In 2003, China was faced with the severe acute respiratory syndrome (SARS) epidemic, a viral respiratory illness also caused by a coronavirus. The SARS outbreak was associated with high levels of anxiety and depression among the Chinese public (Liang, 2003), those who were ill with SARS at the time of the study (Cheng and Wong, 2005), and the survivors (Cheng and Wong, 2005; Mak et al., 2009; Moldofsky and Patcai, 2011; Fang et al., 2019). An analysis of a general psychological assistance hotline that mainly received calls from Beijing showed that the hotline provided effective mental health support during the SARS epidemic (Wang et al., 2003). The current study examined psychological assistance hotlines in a Northern Chinese region that operated during the COVID-19 crisis, as directed by relevant NHCC guidelines (National Health Commission of China, 2020a,b,c).
Psychological Assistance Hotlines at the Time of the COVID-19 Outbreak
The geographic region of interest in this study is located in Northern China and is home to ~16 million people. This Northern Chinese region has 16 sub-regional juridical areas. The specific details of this region (e.g., name of the region, the specific juridical level, dates of its first and last reported COVID-19 case, the precise number of accumulated cases) are omitted to protect the identities of the individuals involved in the original data collection. In this article, “regional level hotline” refers to a hotline established by an organization governed by the regional jurisdiction. A “sub-regional hotline” refers to a hotline established by one of the sub-regional juridical areas within this region. This Northern Chinese region only had one major hotline available at the regional level before the spread of COVID-191, which had been available for about 10 years.
This region began to see its first cases of COVID-19 during the last week of January 2020. Following guidelines provided by the NHCC (National Health Commission of China, 2020a,b), 12 out of the 16 sub-regional juridical areas in this region implemented individual hotline services on the same day within the first week of February. The psychological interventions used in this region during the peak of the COVID-19 were typical of similar areas in China (e.g., on February 6th, 2020, Sichuan, a Southwestern Chinese province, started to provide several psychological assistance hotlines to the public; Zhou, 2020). These hotlines were available to address general mental health concerns, not limited to COVID-19 related issues. Operators would provide referrals (e.g., contact information for hospitals) for callers with concerns beyond the hotlines' capacity to support. The hotlines did not offer follow-up calls to the callers. Since these hotlines were not established before the spread of COVID-19 in China, this period provided a unique opportunity to examine factors that may have contributed to the utilization of hotlines at their outset.
Aim and Objectives
The goal of the current study was to characterize usage rates of the hotlines (i.e., number of calls received) in the Northern Chinese region, and to examine factors that may be associated with the usage, such as dissemination strategies and the number of confirmed COVID-19 cases. The first objective of this study was to analyze the amount of usage at these hotlines. Because the sub-regional hotlines were introduced during COVID-19 and needed to be promoted to the public, we predicted that rates of utilization of these hotlines would be low relative to the pre-existing regional hotline. We anticipated that the regional level hotline, which had been established before COVID-19, would receive a greater number of calls.
The second objective of the study was to describe how the hotlines disseminated their services. Approachability is one factor that may contribute to health service utilization. It relates to the extent to which a health resource is identifiable to people facing health needs (Levesque et al., 2013). One way to increase service approachability is for the services to make themselves known to the people in need. Therefore, this study described how each of the hotlines available in this region advertised its services to the public. We also explored whether and how different methods of service dissemination used by the hotlines might have contributed to their different usage rates.
The third objective of the study was to examine whether the daily number of calls received at the hotlines were related to the daily confirmed number of COVID-19 cases. As a fourth objective, callers' characteristics and concerns raised during the hotline calls were briefly explored. This exploration was to complement the understanding of people who responded to outreach from the hotlines. Understanding hotline users would help target future service outreach and provision.
Methods
Ethical Considerations
Secondary data obtainment and analyses involved in the current study received ethics clearance through the Institutional Ethics Review Board at the University of Waterloo.
Data Collection
Twelve of the 16 sub-regional juridical areas within the examined region established psychological assistance hotlines during COVID-19. Since the names of the sub-regional areas were not specified in this study to protect the identities of the individuals who provided the information, the areas were randomly numbered and presented as Areas 1–12.
Hotline Service Information and Dissemination Methods
The hours of operation of each hotline was publicly available. All the hotline host organizations were contacted by phone to obtain their organization type (e.g., hospital, counseling service center) and qualification of their hotline operators. The regional level host organization and 10 out of the 12 sub-regional hotline host organizations were able to provide a list of methods used to advertise their own hotline numbers.
Daily Number of Calls Received
The 12 sub-regional hotline host organizations reported the daily number of calls received to the regional hotline host. The regional hotline host was contacted to provide these numbers to the researchers. The number of daily calls obtained was from the date that the sub-regional hotlines were established in the first week of February, till ~1 week after COVID-19 cases stopped increasing in this entire region. In total, 32 days of data of the daily number of calls received at the 12 sub-regional hotlines were obtained. Since the regional level hotline was previously established, the daily number of calls received was obtained from January 1st, 2020, till April 8th, 2020, for a total of 98 days.
Daily Number of Confirmed COVID-19 Cases
Since January 21, 2020, the confirmed COVID-19 cases were reported and updated daily for the public. The research team documented the number of daily confirmed cases for 104 days (from January 21st to May 4th). The daily number of cases at the national level, the region of interest of this study, and the sub-regional areas were noted and used for analyses in the current study.
Content of Phone Calls and Caller Characteristics
In mid-March of 2020, the Area 6 hotline host organization interviewed operators at the regional hotline and at hotlines of Area 1–12 that meet the inclusion criteria described below. The interviews asked (1) about notable demographic characteristics (e.g., age, sex-at-birth) of the people who called, (2) whether the calls received were mostly related to COVID-19, and, (3) what concerns about COVID-19 were raised. Answers to (1) and (2) were noted during the interviews and summarized in writing immediately after the interview. Answers to (3) were transcribed (typed) verbatim during the interviews. The written summaries and interview transcripts were obtained from the Area 6 hotline host to explore the characteristics of people who used the hotlines.
Inclusion and Exclusion Criteria
Only the hotlines that had received a total of more than 10 calls before the end of the first week of March were contacted. Out of the 12 sub-regional hotlines, nine sub-regional hotlines had satisfied the criterion of having received more than 10 calls and were included in the study. Area 5 was excluded because the operator informed the interviewer that the hotline operated mainly by making out-going calls to people at high risk of contracting COVID-19 (see Note 3 of Table 1). Area 9 and Area 12 could not be reached and were excluded from this analysis. Two operators at the regional level hotline were interviewed. Therefore, data of caller characteristics and content of calls received were originally collected from nine hotline operators from eight hotlines, including the regional level hotline and seven out of the 12 sub-regional hotlines.
Analyses
Objective 1: Analyzing the Number of Calls Received by the Hotlines During COVID-19
For each of the regional level hotline and the 12 sub-regional hotlines, the calls received at the hotlines were summed across the 32 days during which data of the sub-regional hotlines were obtained. To examine the number of calls in proportion to population size, the sums were then divided into the populations of the areas (i.e., the total number of calls at the regional hotline was divided into the total population of the region; the total number of calls at each sub-regional hotline was divided into the population size of the respective sub-regional area).
Objective 2: Describing Dissemination Strategies of the Hotlines
Descriptions of the dissemination methods were summarized for each hotline. Methods of hotline service dissemination were categorized according to the level of populations reached (e.g., community, individuals).
Objective 3: Examining the Association Between the Number of Calls and the Number of Confirmed COVID-19 Cases
Correlations were calculated between the number of calls received at each hotline and the daily confirmed number of COVID-19 cases in the local area, the entire region, and China overall. The situation in Hubei and China overall was salient on media and affected policies (e.g., stay-at-home orders, mental health interventions) implemented in regions outside of Hubei. Thus, people's psychological state was likely affected by the severity of COVID-19 both in Hubei locally and in the country overall. The correlational analyses were only done for the regional level hotline and three sub-regional hotlines (i.e., hotlines of Areas 1, 3, and 11). The other sub-regional hotlines received too few calls during the 32 days of hotline operation examined for any correlational results to be interpretable.
Additionally, confirmed cases of COVID-19 were reported since January 21st, 2020, at the national level, before this region saw any COVID-19 cases. The daily number of phone calls received at the regional hotline was obtained until April 8th, 2020. A non-parametric Spearman correlation was calculated for these two variables between these two dates (for a total of 79 days). We also found the period during which calls at the regional hotline peaked, and compared it with the period during which the national daily confirmed COVID-19 cases peaked. To identify the period during which phone calls peaked, we calculated 5-day running averages for the number of phone calls and then subtracted each resulting data point from the next one. The results of the subtractions indicated the change in the number of phone calls from day-to-day. A positive change value indicated an increase in the number of calls from the previous day, whereas a negative change value indicated a decrease. We flagged change values whose absolute values were one standard deviation away from the mean. The period between the day with the first flagged positive change and the day with the last negative change was the peak period. When finding the peak period of daily confirmed COVID-19 in the country, two outliers (data from February 12th and 13th) were first removed. The rest of the process of finding the peak was the same as that used for finding the peak period of the regional hotline calls.
Objective 4: Exploring Callers' Characteristics and Concerns Raised During the Calls
The basic characteristics of the callers and their expressed concerns, as described by the hotline operators, were analyzed. The researchers coded the descriptions by categories of concerns (e.g., COVID-19 illness-related anxiety, mental health issues due to prolonged social isolation). Major themes of concerns were summarized.
Results
Representativeness of the Region Studied
The Northern Chinese region studied in the current analyses had a total of ~150 accumulated COVID-19 cases (0.00087% of the population), with its last confirmed case of COVID-19 reported at the end of February 2020. This total confirmed number was relatively low compared to other areas of the world affected by the COVID-19 pandemic. However, this number is representative of reported COVID-19 cases in areas of China outside of Hubei (the province where Wuhan is located). Specifically, as of the date that this Northern Chinese region saw its last COVID-19 increase, China had accumulated 78,959 COVID-19 cases. Of these cases, 83.48% (65,914 cases;0.11% of the population) were reported within Hubei. The other provincial jurisdictions of China (n = 33) had an average number of 395.30 (SD = 403.4426) accumulated COVID-19 cases (M = 0.00092% of population; SD = 0.00062%). Therefore, although the accumulated COVID-19 cases in the region studied appears low compared to other areas of the world, this number is representative of Chinese regions outside of Hubei.
Calls Received at Each Hotline
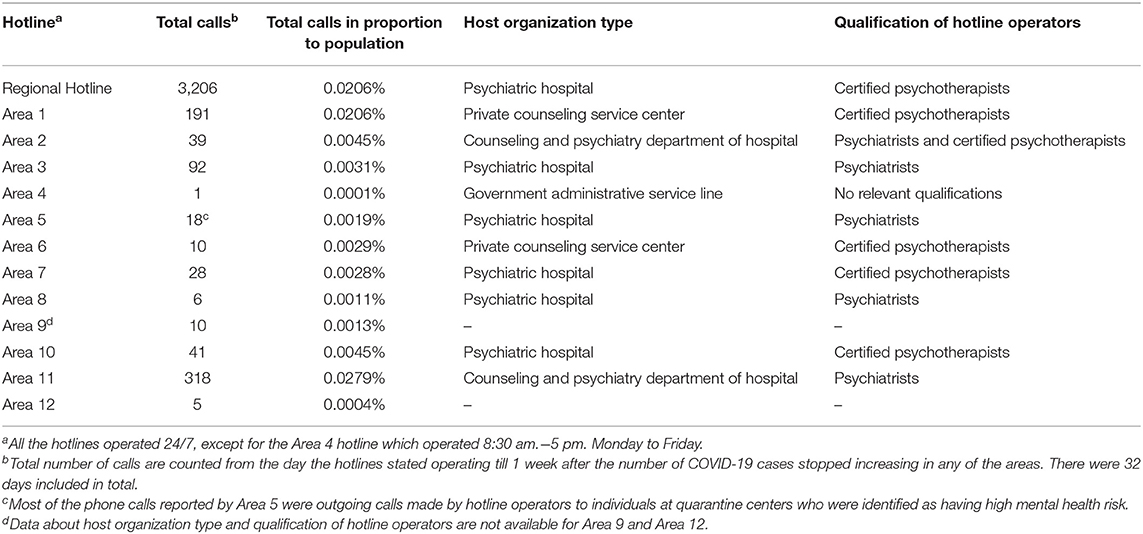
Characteristics of the hotlines examined (e.g., type of host organization, service hours) are presented in Table 1.
Across the 32 days during which data for the sub-regional hotlines were obtained, the number of calls received at the regional level hotline (n = 3,206) was 0.021% of the population of the region. At the 12 sub-regional level hotlines, the proportion of the number of calls (M = 63.25, SD = 96.59) to the population size (M = 1047.91 thousand, SD = 651.49 thousand) in each area ranged from 0.00011 to 0.028%. Table 1 shows the total number of calls received at each hotline and their proportion to the population. Area 1 (0.021%), Area 11 (0.028%), and the regional level hotline (0.021%) received the highest number of calls in proportion to population size. Although the number of calls (n = 91) in Area 3 might seem relatively higher than hotlines in most other areas, its number of calls in proportion to population size (0.0031%) was not as high in rank (e.g., Areas 10 had 41 calls but 0.0045% in proportion to the population size of the area).
Summary
Consistent with prediction, the sub-regional hotlines had low usage. The regional hotline received a relatively large number of calls overall but the usage rate in proportion to population size was still low.
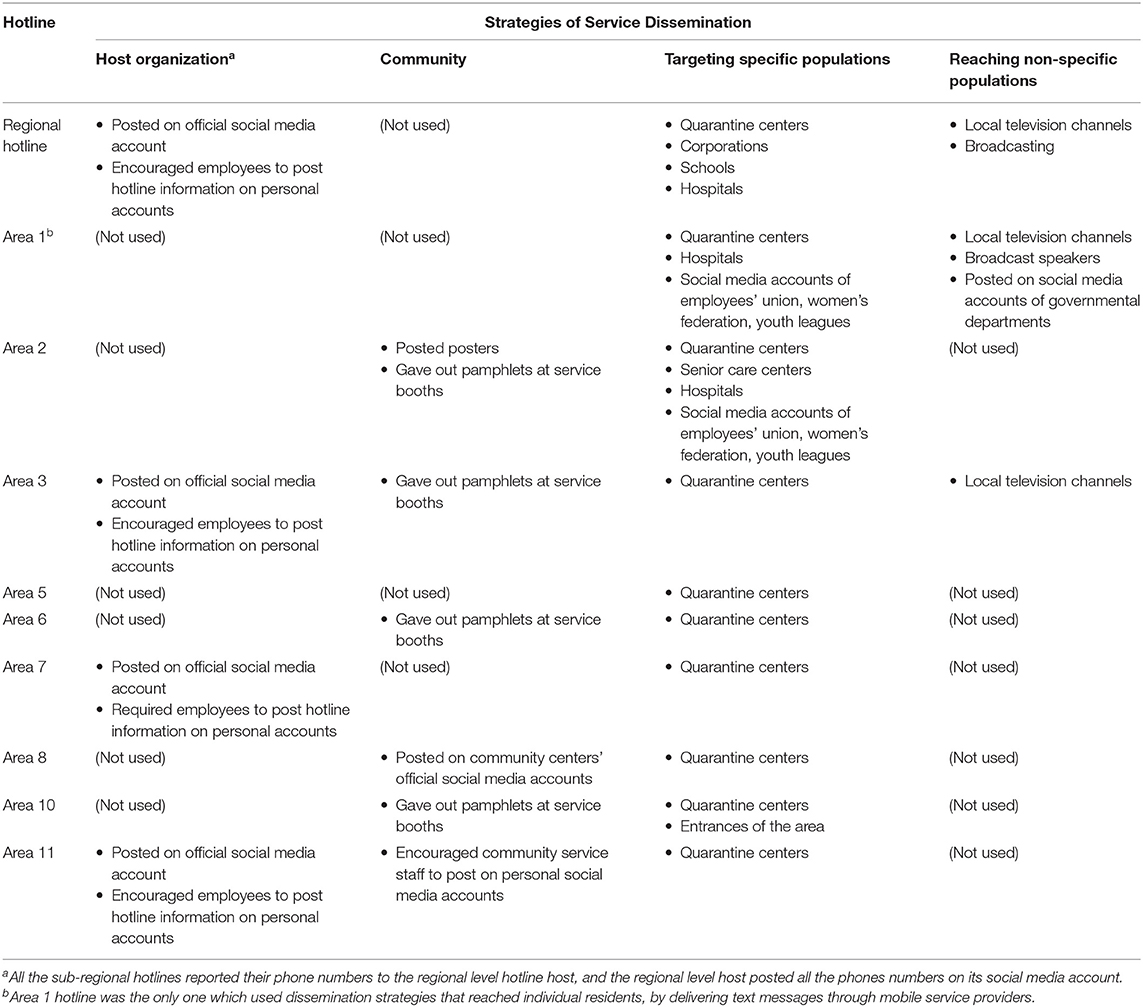
Dissemination Methods of Hotline Service
Dissemination strategies of the hotlines are presented below according to whether the method was through (1) channels owned by the host organization, (2) community channels, (3) targeting specific populations (e.g., people at quarantine centers), (4) reaching individual residents, and (5) methods with non-specific targets. Summaries of these methods are presented in Table 2.
Host Organization Channels
The hosts of the regional hotline and the hotlines in Areas 3, 7, and 11 all advertised their hotline numbers through their own official social medial accounts. These hosts also encouraged employees at the organization to re-post the hotline information on their personal accounts. Area 7 host made the re-posting task a requirement for its employees.
All the sub-regional hotline host organizations were also required to submit their hotline numbers to the regional hotline host. On the third day following the start of the sub-regional hotline operations, the regional hotline host posted these numbers along with its own on its official social media account.
Community Channels
Each sub-regional area had residential communities under its governance. Areas 2, 3, 6, 8, 10, and 11 all advertised their hotline service through community resources. Specifically, posters were posted in the communities of Area 2. Pamphlets were given out at community service booths in Areas 2, 3, 6, and 10. These service booths were operated by volunteers during the COVID-19 to provide body temperature checks. Area 8 had community centers post the hotline number on their official social media accounts. Area 11 encouraged community service staff to post the hotline number on their personal social media accounts.
Targeting Specific Populations
All the hotlines, except for Area 4, provided their numbers to local quarantine centers, where people who had close contact with those who contracted COVID-19 temporarily stayed. The regional hotline additionally provided its number to corporations and schools so they can distribute to individual employees and students. Area 2 provided its numbers to senior care centers. Hotline numbers at the regional level and Areas 1 and 2 were also provided to hospitals under their respective juridical governance. Additionally, Areas 1 and 2 had their hotline numbers posted on social media accounts of the Employees' Union, Women's Federation, and Youth Leagues. Area 10 provided its hotline information to people at entrances of the area to incoming travelers.
Reaching Individuals
Area 1 had all the major mobile service providers forward its hotline number to individual residents through text messages.
Channels Reaching Non-specific Targets
The number of the regional level hotline and those of Area 1 and 3 were disseminated through local television channels and local newspapers. The regional level hotline was also advertised through broadcasting. Additionally, Area 1 uniquely had broadcast speakers installed throughout the area, and its hotline number was cast to its residents through this channel. Area 1 also had governmental departments post the hotline information on their departmental social media accounts.
Summary
Patterns between methods of service dissemination and hotline usage could be observed. Area 1 used methods that ensure reaching each resident and had relatively high hotline usage. Area 11 received the most phone calls and had the highest number in proportion to population, compared with other sub-regional hotlines. The relatively high usage rate of the Area 11 hotline may be related to its method of service dissemination, as it relied the most heavily on dissemination through individuals' personal social media. Merely relying on dissemination through community centers and/or providing the number to quarantine centers appeared to be inadequate for reaching consumers, as can be seen from Areas 5, 6, and 8. Area 4 did not use any method to advertise its service other than submitting its number to the regional host organization, and hotline at this area had the least number of phone calls. Overall, encouraging individuals to post the hotline service on their social media accounts appeared to be an effective way of service outreach.
Relationship Between Daily Number of Calls and Daily Number of Confirmed COVID-19 Cases
We first observed that Area 1 is the area where COVID-19 cases were concentrated in the region, with 44% of total COVID-19 cases from Area 1 and the rest from the other 16 areas of the region.
Results of the correlational analyses are presented in Table 3. Non-parametric Spearman correlations revealed that the calls received at the Area 1 hotline had an increasing trend over time (r = 0.34, df = 30, p = 0.058). The number of calls were negatively correlated with the daily increase of COVID-19 cases in the area (r = −0.41, df = 30, p = 0.019) and in the region overall (r = −0.44, p = 0.013), but not with the daily increase in the country (r = 0.31, df = 30, p = 0.087).
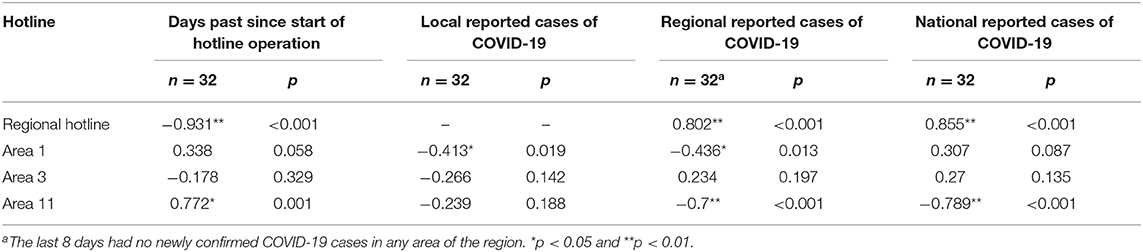
Table 3. Correlations between numbers of calls received at selected hotlines and number of days past since their operation, daily confirmed COVID-19 cases in the sub-regional local area, in the region, and in the country.
On the other hand, the number of calls received at the Area 11 hotline significantly increased over time (r = 0.77, df = 30, p < 0.001). The number of calls did not correlate with increases of COVID-19 in this area but had significantly negative correlations with the daily reported of COVID-19 cases in the overall region (r = −0.70, df = 30, p < 0.001) and the country (r = −0.79, df = 30, p < 0.001).
Area 3 saw no trend of the phone calls received at its hotline over time. There was also no relationship between the number of phone calls and the daily confirmed number of COVID-19 in the area, in the region, or the country. As noted previously, although Area 3 received a high number of phone calls that allowed the correlational analysis, the area had a larger population size and the number of phone calls in proportion to population size was low.
At the regional level hotline, the number of phone calls received decreased (r = −0.93, df = 30, p < 0.001) over the 32 days since the sub-regional hotlines started operating. Contrasting the patterns seen in Areas 1 and 3, the number of calls received at the regional hotline positively correlated with daily increase of COVID-19 in the region (r = 0.80, df = 30, p < 0.001) and in the country (r = 0.86, df = 30, p < 0.001). During the 79 days between January 21st and April 8th, the calls at the regional hotline were again significantly positively correlated with the national daily confirmed COVID-19 cases (r = 0.68, df = 30, p < 0.001).
Peak Period of Phone Calls at the Regional Level Hotline
As can be seen in Figure 1, the number of phone calls at the regional hotline had a peak period. The beginning of the peak period (i.e., first flagged positive change) occurred on the day after the first day that the region saw its first COVID-19 case. In the following 10 days, the calls showed flagged increases on 9 days, before reaching the absolute peak point and starting to show a decrease in the number of calls (i.e., flagged negative values). We observed that the peak point (i.e., the point whose change from its previous point is positive and whose change to its next point is negative) occurred on the day that the sub-regional hotlines started to operate. There were 16 days between this day of peak and the end of the peak period (i.e., the last flagged change). Six of the 16 days had a flagged decrease of phone calls and none indicated a flagged increase of calls. The last flagged decrease occurred ~1 week before the region saw its last COVID-19 increase.
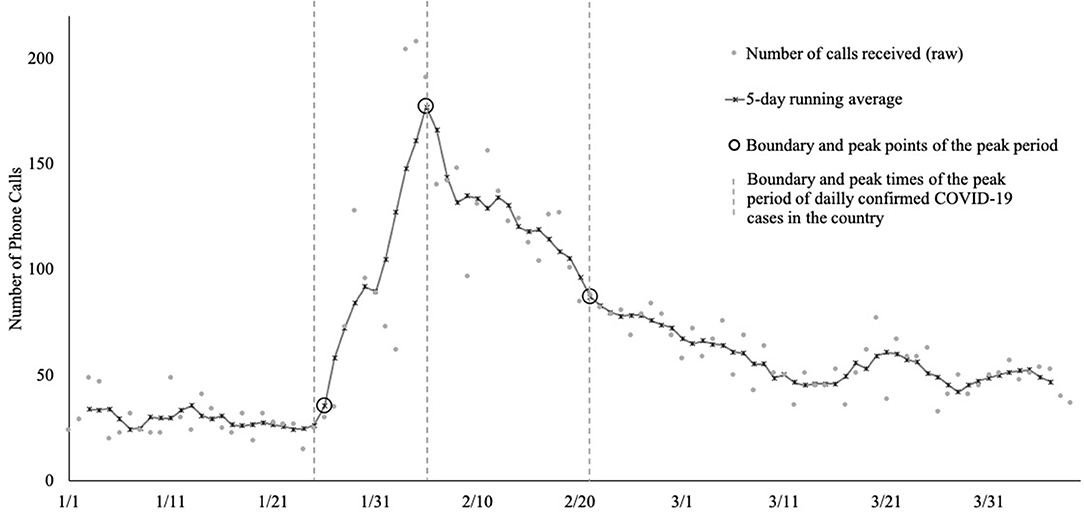
Figure 1. The daily number of phone calls received at the regional hotline from January 1st, 2020, till April 8th, 2020, and 5-day running averages. The number of phone calls showed a monotonic increase since the day COVID-19 cases were reported in this region, peaked on the day the sub-regional hotlines started to operate, and started to show monotonic decrease afterward. The peak period spanned 27 out of the 79 days.
Summary
Taken together, phone calls received at the regional hotline showed a monotonic increase since the day COVID-19 cases were reported in this region, peaked on the day the sub-regional hotlines started to operate, and started to show monotonic decrease afterward. In total, the peak period spanned 27 days. Notably, the number of phone calls received at the regional level hotline appeared to show decreasing trend over time when only examining the calls from the day when the sub-regional hotlines started operation (as described above). However, examining the number of phone calls over a longer period revealed that the number of phone calls changed over time in a non-linear manner.
Peak Period of National COVID-19 Cases
Since the number of COVID-19 cases at the national level correlated with the number of calls received at the regional level hotline, as described above, we also identified the peak period of COVID-19 in China. We observed that the daily increase of COVID-19 cases showed a monotonic increase between January 25th and February 3rd. Changes were not flagged between February 4th and February 6th, and there is a monotonic decrease between February 7th and February 21st, with 10 of the days having flagged negative change values.
We observed that the day on which the regional level hotline calls peaked fell within the days during which the daily confirmed cases of COVID-19 peaked in China, February 3rd to 7th. Interestingly, the day that increase of COVID-19 started to slow down (February 7th) was also the day on which the NHCC issued a specific guideline for establishing mental health hotlines (National Health Commission of China, 2020a). Overall, the peak period of the regional level hotline calls coincided almost perfectly with the peak period of national daily confirmed COVID-19 cases.
Concerns Raised During the Hotline Calls
According to the operators' recollection, callers' ages ranged from seven to over 80 years old, with most individuals between 20 and 50 years old. There were slightly more female callers than males. Major themes of concerns included anxiety about contracting COVID-19, mental health issues associated with social isolation, and conflict with family members due to extended time of staying at home. Quotations illustrating these themes and some other concerns are presented below.
Illness-Related Anxiety
Most calls received during the peak of COVID-19 were related to the crisis. One major theme of concerns revealed was fear of contracting COVID-19:
Many people were anxious about getting sick, getting the coronavirus. They reported lots of somatized symptoms. It's common to hear reduced appetite and difficulty falling asleep. Also, heart palpitation, increased blood pressure, sweating. People checked their body temperature multiple times a day, staring at the body thermometer all day long. There were also people who repeatedly checked themselves against the coronavirus symptoms.
Social Isolation
Aside from concerns directly related to becoming sick, one major theme of issues was related to long-term isolation. As the hotline operators recalled, many concerns were about not being able to have social interactions and living with the same home routine every day for a prolonged period of time. People started to have feelings of boredom, fatigue, and associated anxiety. For instance, one operator recalled:
A lot of people were calling because they had to stay at home for this prolonged period. They were in a very different psychological state. Some people used to like playing online games, but then they had this time to play all day long. It became boring and tiring very quickly. Got rid of any gaming addiction right there. Similar to those who watched TV series all day long. There was a lot of anxiety. Anxiety from isolation and not having much to do.
Family Conflict
Another major issue raised was family conflict due to spending extended time with family during isolation at home. As reported by a hotline operator:
One common issue is family conflict. Before the pandemic, people were busy at work, at school, and family didn't spend so much time together. Now family members were stuck together all day long. Issues that used to be glossed over created explicit conflicts. There were also family conflicts surrounding the coronavirus itself. I remember, to give you an example, one person talked about her mother believing herself being sick and complaining to the rest of the family about not taking her to the hospital. That created a lot of fights.
Other Concerns
The hotline operators also highlighted some issues related to COVID-19 even though they did not form themes as the ones discussed above. For instance, one operator received a call from a 7-year-old child. The child felt helpless because both of the child's parents were working at the medical frontline and the grandparents were quarantined. An elderly caller expressed re-triggered traumatic memories. This caller survived a major earthquake in the 1970s, and the pandemic was triggering anxiety and worry about natural disasters. The hotline operator at Area 1 also highlighted that some callers were survivors of COVID-19 but they felt guilty about having made others sick:
[Area 1 to this region] is like Wuhan to China. It's where the coronavirus was the worst. Most people got the virus because they went to this one place. Some people who went to this place and then later got tested positive felt very guilty. They felt guilty about having passed the virus to others.
Summary
Overall, hotline operators reported that a significant proportion of hotline callers had concerns directly or indirectly related to COVID-19. However, many calls were about general psychological concerns, not related to COVID-19 per se. The issues related to COVID-19 were grouped into themes including illness-related anxiety, a psychological difficulty about prolonged home isolation, and family discord due to spending more time at home.
Discussion
Despite China's unprecedented emphasis on and speed of response to the psychological crisis when COVID-19 spread in the country, its mental health solutions were criticized as inadequate, primarily due to lack of pre-established organization and management (Dong and Bouey, 2020; Duan and Zhu, 2020). The current study is the first to examine a specific provision of mental health intervention, namely, psychological assistance hotlines, in China during COVID-19. The results revealed the low usage of mental health hotlines during COVID-19. The hotline usage appeared to be related both to ways of service promotion and the number of confirmed COVID-19 cases in the local area and the country. Results from this study suggest specific directions for the improvement of hotline service establishment in China to meet the mental health needs of the public and to prepare for future crises.
Number of Calls Is Associated With Service Dissemination Strategies
The hotline services were used by only a small proportion of the population but some patterns between usage and methods of service dissemination were observed. Hotlines that only relied on disseminating services through community centers (e.g., social media accounts of community centers, community service booths), and/or providing its numbers to local quarantine centers did not receive many calls. The sub-regional hotline that received the highest number of calls relied heavily on advertising its service through personal social media. This hotline encouraged individuals to re-post information about the service on their personal social media accounts. Interestingly, this area was the only one that received a significant increase in phone calls over time. It is possible that this pattern was related to its reliance on social media for service dissemination. It may be that this method allows individuals to directly and quickly share information with others on a platform they are familiar with, rather than relying on the mass public to continuously be aware of and seek out resources provided by community centers. Because individuals continued posting and re-posting the hotline service information within their mutual social circles, the information would be expected to become more widely known as more time passed. This result suggests that where it is consistent with the societal and work culture, using personal social media may be an effective, efficient, and more relatable way of mental health service outreach, reflecting modern forms of communication.
The hotline that reached each individual resident in its service dissemination received a relatively high number of phone calls. However, this area also had the highest number of confirmed COVID-19 cases compared to other sub-regional areas examined. Without another area that experienced a similar impact of COVID-19 but used different service dissemination approaches, it is difficult to dissect the influence of COVID-19 severity from the effectiveness of service outreach.
Notably, although the strategies of service dissemination appeared to be related to the hotline service usage, it is difficult to determine the extent of their causal relationship from the current study. For instance, the area that had the lowest hotline usage barely engaged in service dissemination. The only way it promoted its service to the public was by submitting it to the regional hotline host so the regional host could post it on its social media account, along with phone numbers of the other hotlines. However, this limitation in outreach was not the only downside of the service provided by this hotline. This hotline had the shortest operation hours. It was also the only hotline whose operators did not have training or qualifications to provide psychological interventions. Therefore, although variation in dissemination strategies appeared to be related to variation in hotline usage, this association may be merely a reflection of the general service quality that contributed to service use overall. Future studies are required to determine how different aspects of hotline service provision may influence the number of calls it receives, besides dissemination strategies.
Association of Number of Calls With Confirmed COVID-19 Cases
No consistent patterns were observed across the sub-regional hotlines when comparing the number of calls they received and the number of confirmed COVID-19 cases. However, the number of calls received at the regional level hotline was closely related to the daily confirmed COVID-19 cases reported in the country. The examination of this relationship was possible because the regional level hotline operated prior to the peak of COVID-19 cases in China. The daily number of calls received at the regional level hotline positively correlated with daily confirmed cases reported in the nation. Moreover, the period during which the regional hotline calls peaked coincided almost perfectly with the period during which daily confirmed cases of COVID-19 peaked in China.
Notably, this observed relationship between the number of regional hotline calls and national COVID-19 cases does not preclude the influence of service dissemination on the use of the hotlines. It is possible that dissemination efforts changed over time according to the number of confirmed COVID-19 cases. Specifically, the hotline hosts might have engaged in more outreach when more COVID-19 cases occurred. The effort of service outreach and COVID-19 severity would then affect the number of calls at the same time. Although COVID-19 will become a unique historical event, future studies can experiment with the impact of different service dissemination strategies on the utilization of mental health hotlines in order to better assess causal relationships between dissemination and the utilization of hotline services.
Need for Established Mental Health Systems for Public Crisis Response
Interestingly, the days when the regional level hotline reached its absolute usage peak coincided not only with the days of the absolute peak of daily confirmed COVID-19 in China but also the time when sub-regional hotlines started operating. That is, after the sub-regional hotlines became available, the regional level hotline started to see a decline in the number of phone calls received. It is possible that phone calls that would have been made to the regional hotline were directed to the sub-regional hotlines when these hotlines became available, thus resulting in the decrease in the number of calls to the regional hotline. It would suggest that the sub-regional hotlines did effectively share the service demand that would have been directed to the regional hotline.
The coincidence between the peak of COVID-19 in the country and the beginning of the sub-regional hotline operations revealed potential delays of the hotline service provision. Specifically, the sub-regional hotlines only became available when COVID-19 cases in the country already started to decrease. The services were not established when COVID-19 started to become an increasing concern and when the regional hotline saw increasing usage. This observation is consistent with opinions expressed in the commentaries that criticized the lack of pre-established psychological intervention systems in China, which limited the country's ability to respond effectively when facing crises (Dong and Bouey, 2020; Duan and Zhu, 2020). COVID-19 may be an opportunity for mental health service providers in China to learn from the limitations of the current systems and better prepare for future needs.
Future Development of Hotline Services in China
Over the past decades, psychological assistance hotlines in China have become more available and increasingly accessed (Ji, 1995; Zhu et al., 2005). Even though the public mental health crisis brought by COVID-19 revealed some limitations of the mental health systems in China, the development of mental health systems is a work in progress in every country. In fact, the establishment of psychological assistance hotlines in China during COVID-19 was extremely rapid. The lowest juridical levels set up their hotlines (e.g., the ones examined in the current study) within 2 weeks after the issuance of NHCC's psychological crisis response guidelines (National Health Commission of China, 2020c) and within 1 week after the national notification for hotline establishment (National Health Commission of China, 2020b). Despite such rapid response, service provision still lagged behind the public's service demand (as discussed above). This observation suggests that disaster/crisis response simply cannot rely on the ad hoc creation of intervention systems. Mental health systems need to be established in a proactive manner and well-disseminated beforehand, with staff already trained for crisis intervention, in order to effectively serve the need of the pubic when a disaster/crisis occurs.
As mental health service providers continue to improve the quality and accessibility of psychological assistance hotlines, some options may be considered. For instance, the hotlines examined in this study were all general counseling hotlines. The development of hotlines that address specific concerns for specific populations may help improve the efficiency and quality of service provision. As seen from the themes of COVID-19 related concerns found in this study (i.e., anxiety about disease contraction, the psychological impact of prolonged isolation at home, and family conflicts due to spending more time at home with family), people at different ages experienced a variety of difficulties. The hotline operators, however, might not have been trained to provide services that would suit the diverse needs of the callers. To provide more targeted services, it may be valuable to create hotlines based on the type of issues raised by different populations (e.g., sexual assault; Finn and Hughes, 2008; child abuse; Ngoc, 2005; suicidal ideation; Ohtaki et al., 2016). It should be noted that in countries (e.g., the U.S.) where a variety of hotlines are usually available, it may be difficult for the people in need to identify the hotline that best suits their needs. As hotline providers in China establish their services, it may be beneficial to plan for providing targeted services that are also easily accessible. Future studies could examine how specialty needs are currently addressed and determine whether systematic changes would be required to improve current services.
In addition, the provision of hotline counseling services should be considered in the context of other mental health services available. In some Western countries, hotlines are mainly available for crisis interventions. General counseling services are usually provided by psychotherapists in the community and many consumers have insurance coverage when using these services. The hotlines examined in the current study, similar to many others in China, provide general counseling; in-person consultation from therapists is not always accessible or affordable. Therefore, the establishment of hotline service systems in China may face unique challenges. Chinese mental health providers may need to establish standards suitable for the circumstance of the society, in addition to learning from countries with a longer history of mental health system development.
Challenges in Achieving Service Accessibility
Service dissemination is only one of the many steps involved in translating the needs of mental health care to the actual use of services and attaining desirable health outcomes. Many factors from both the suppliers' and the consumers' side play a role (Ecob and Macintyre, 2000; Andersen, 2008; Andersen et al., 2013; Levesque et al., 2013). For example, Levesque et al. (2013) conceptualized five dimensions that health service providers need to accomplish in order to make the service accessible. These five dimensions included approachability (i.e., the extent to which the service is known and identifiable), acceptability (i.e., the extent to which the service is appropriate for a particular individual in the cultural and social environment), availability and accommodation (i.e., the extent to which the service can be reached in time), affordability (i.e., the extent to which prices and opportunity costs of the service can be covered by one's income) and appropriateness (i.e., the extent to which the service fits the service seeker's needs; Levesque et al., 2013). In reflection to the dimensions presented by Levesque et al. (2013), each sub-regional hotline in the current study made various efforts to increase their approachability by distributing information regarding hotline services.
Corresponding to the five dimensions of accessible service are the five abilities of individuals that would enable their needs to be translated into outcome (Levesque et al., 2013). Namely, these are people's abilities to perceive, seek, reach, pay for, and engage in services. Consumers' ability to perceive the need for care is complementary to approachability of the service provider. For instance, someone who is experiencing anxiety about having COVID-19 may be aware of the hotline resource, but they may not recognize this anxiety as a psychological issue and have no desire to call a mental health hotline. Therefore, it is necessary to increase the mental health literacy of the public so individuals with service needs are able to self-identify and respond to the outreach efforts of the service providers.
Notably, among all the challenges that China needs to overcome for mental health hotlines and other psychological interventions to function adequately, improving service quality may take the longest time and require the most investment. China is currently under a severe shortage of mental healthcare providers (Liang et al., 2018). This shortage was indicated in commentaries about China's mental health provision during COVID-19 (Dong and Bouey, 2020) and is also evident from the varying degree of qualification of mental health hotline operators seen in the current study. The shortage of professionals renders the fast establishment of psychological interventions during crises infeasible (Duan and Zhu, 2020). Consequently, to become effective in mental health service provision, especially when facing unexpected events of crises, China would likely have to engage in long-term commitment and investment in establishing mental health systems.
Limitations
Several limitations should be noted when interpreting the findings. First, the results of the current study were obtained from the data of one Northern Chinese region. The results may not generalize to other regions, especially those that were geographically further from this region and had different demographics. However, other regions may still be informed by this study because the severity of COVID-19 in this region was on par with most regions in China and the mental health solutions it used were representative of other regions during COVID-19.
Second, observations about mental health hotline usage from this study were made from the limited time period of COVID-19 in China, as the sub-regional hotlines were previously not available. It may inform hotline service usage during a public health crisis. However, before the findings from this study can be used to inform changes to dissemination strategies of mental health hotline services in general, more studies should be done to understand hotline usage outside of the time of a pandemic. For instance, although the operators reported that most individuals who called the hotlines tended to be between ages 20 and 50, it is unknown whether this age group is also more likely to use hotlines in general.
Third, many factors in addition to service outreach can affect mental health resource utilization. Future studies are warranted to determine to what extent service dissemination can affect usage of mental health hotlines, and what other factors are significant contributors to mental health service use in China, in general, and in response to crises.
Fourth, the qualitative analysis of concerns people expressed during the hotline calls was not systematic or in-depth in this study, due to the limitations of the secondary data that were available. To better understand the issues raised during these calls, future studies should collect systematic records for each call. Finally, the current study did not include information about how various issues were approached by the hotline operators during the calls. As dissemination is only one step in ensuring service use, future studies should examine details of the service provision and understand how it may impact the use of the hotline services. If future studies examine hotline usage post-COVID-19, it may be especially important to accounting for service provision during the crisis, as current service may impact people's trust of the service and therefore future usage.
Data Availability Statement
The data analyzed in this study is subject to the following licenses/restrictions: Hotline usage data used in the study are not shared.
Ethics Statement
Secondary data obtainment and analyses involved in the current study received ethics clearance through the Institutional Ethics Review Board at the University of Waterloo.
Author Contributions
RM conducted the analyses and took the lead in writing the manuscript. JO contributed to conceptualizing study analyses. JO and RN reviewed and provided critical feedback on the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank Dr. Amy Drahota for helpful discussions about the idea of the study.
Footnote
1. ^The only other hotline available in this region before COVID-19 was one offered by the Women's Federation. Data from this hotline were not available for analysis in the current study. However, private communication with the director of this hotline revealed that daily number of phone calls received, before and during COVID-19, were much fewer than the number received by the regional level hotline examined in this study. Not including data from this hotline therefore would unlikely change the results of this study.
References
Andersen, R. M. (2008). National health surveys and the behavioral model of health services use. Med. Care 46, 647–653. doi: 10.1097/MLR.0b013e31817a835d
Andersen, R. M., Davidson, P. L., and Baumeister, S. E. (2013). “Improving access to care,” in Changing the U.S. Health Care System: Key Issues in Health Services, Policy, and Management, ed G. F. Kominski (San Francisco, CA: John Wiley & Sons), 33–69.
Cheng, H., Ji, J. L., and Wen, S. M. (2000). Mental health hotline services in Shanghai between 1995. Chinese J. Clin. Psychol. 3. Available online at: http://clinicalpsychojournal.yywkt.cn
Cheng, S. K. W., and Wong, C. W. (2005). Psychological intervention with sufferers from severe acute respiratory syndrome (SARS): lessons learnt from empirical findings. Clin. Psychol. Psychother. 12, 80–86. doi: 10.1002/cpp.429
Dong, L., and Bouey, J. (2020). Public mental health crisis during COVID-19 pandemic. Emerging Infect. Dis. 26, 1616–1618. doi: 10.3201/eid2607.200407
Duan, L., and Zhu, G. (2020). Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiatry 7, 300–302. doi: 10.1016/S2215-0366(20)30073-0
Ecob, R., and Macintyre, S. (2000). Small area variations in health related behaviours; do these depend on the behaviour itself, its measurement, or on personal characteristics? Health Place 6, 261–274. doi: 10.1016/S1353-8292(00)00008-3
Fang, S., Wang, X. Q., Yang, B. X., Liu, X. J., Morris, D. L., and Yu, S. H. (2019). Survey of Chinese persons managing depressive symptoms: help-seeking behaviours and their influencing factors. Compr. Psychiatry, 95, 1–9. doi: 10.1016/j.comppsych.2019.152127
Finn, J., and Hughes, P. (2008). Evaluation of the RAINN national sexual assault online hotline. J. Technol Human Serv. 26, 203–222. doi: 10.1080/15228830802094783
Ji, J. (1995). Hotline for mental health in Shanghai, China. Crisis, 16, 116–120. doi: 10.1027/0227-5910.16.3.116
Levesque, J. F., Harris, M. F., and Russell, G. (2013). Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int. J. Equity Health 12:18. doi: 10.1186/1475-9276-12-18
Liang, B. (2003). Common psychological stress responses and psycholoigcal interventions during the SARS epidemic in China. Studies Psychol. Behav. 3. Available online at: http://psybeh.tjnu.edu.cn/CN/volumn/current.shtml
Liang, D., Mays, V. M., and Hwang, W. C. (2018). Integrated mental health services in China: Challenges and planning for the future. Health Policy Plan. 33, 107–122. doi: 10.1093/heapol/czx137
Liu, S., Yang, L., Zhang, C., Xiang, Y. T., Liu, Z., Hu, S., et al. (2020). Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry 7, e17–e18. doi: 10.1016/S2215-0366(20)30077-8
Mak, I. W. C., Chu, C. M., Pan, P. C., Yiu, M. G. C., and Chan, V. L. (2009). Long-term psychiatric morbidities among SARS survivors. Gen. Hosp. Psychiatry, 31, 318–326. doi: 10.1016/j.genhosppsych.2009.03.001
Moldofsky, H., and Patcai, J. (2011). Chronic widespread musculoskeletal pain, fatigue, depression, and disordered sleep in chronic post-SARS syndrome: a case-controlled study. BMC Neurol. 11:37. doi: 10.1186/1471-2377-11-37
National Health Commission of China (2020a). Guidelines for Psychological Assistance Hotlines During 2019-nCoV Pneumonia Epidemic. Hanoi.
National Health Commission of China (2020b). Notification for Establishing Psychological Assistance Hotlines in Response to 2019-N-Cov Pneumonia Epidemic.
National Health Commission of China (2020c). Principles of the Emergency Psychological Crisis Interventions for the New Coronavirus Pneumonia.
Ohtaki, Y., Oi, Y., Doki, S., Kaneko, H., Usami, K., Sasahara, S., et al. (2016). Characteristics of telephone crisis hotline callers with suicidal ideation in Japan. Suicide Life-Threat. Behav. 47, 54–66. doi: 10.1111/sltb.12264
Qiu, J., Shen, B., Zhao, M., Wang, Z., Xie, B., and Xu, Y. (2020). A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. General Psychiatry 33, 1–3. doi: 10.1136/gpsych-2020-100213
Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L., McIntyre, R. S., et al. (2020). A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 87, 40–48. doi: 10.1016/j.bbi.2020.04.028
Wang, Y. N., Gao, W., Bin, and Yang, X. D. (2003). Application assessment of psychological counseling through hotline during the SARS epidemic period. Chinese J. Behav. Med. Sci. 5. Available online at: http://zhxwyxynkxzz.yiigle.com
Xiang, Y. T., Yang, Y., Li, W., Zhang, L., Zhang, Q., Cheung, T., et al. (2020). Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 7, 228–229. doi: 10.1016/S2215-0366(20)30046-8
Xie, X., Weinstein, L., and Meredith, W. (1996). Hotline in China: one way to help Chinese people. Psychol. Rep. 78:90. doi: 10.2466/pr0.1996.78.1.90
Zhang, M., Ji, J., and Chu, Z. (1995). Assessment of Shanghai mental health hotline 上海心理健康热线电话心理咨询应用评估I [In chinese]. 临床精神医学杂志, 5. 195–197.
Zhou, X. (2020). Psychological crisis interventions in Sichuan province during the 2019 novel coronavirus outbreak. Psychiatry Res. 286:112895. doi: 10.1016/j.psychres.2020.112895
Zhu, X., Chen, H., and Ji, J. (2005). The analysis of hotline data for mental illness. Clin. Med. J. China 2. Available online at: http://www.c-jcm.com/zglcyx/ch/index.aspx
Keywords: COVID-19, mental health, dissemination, hotline, service utilization
Citation: Ma R, Nguyen R and Oakman JM (2020) Dissemination Strategies and Usage of Psychological Assistance Hotlines During the COVID-19 Outbreak in China. Front. Commun. 5:60. doi: 10.3389/fcomm.2020.00060
Received: 10 May 2020; Accepted: 09 July 2020;
Published: 23 July 2020.
Edited by:
Mohan Jyoti Dutta, Massey University, New ZealandReviewed by:
Ravindra Kumar Vemula, English and Foreign Languages University, IndiaVictoria Team, Monash University, Australia
Copyright © 2020 Ma, Nguyen and Oakman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ruofan Ma, cjI4bWFAdXdhdGVybG9vLmNh
 Ruofan Ma
Ruofan Ma Rin Nguyen
Rin Nguyen Jonathan M. Oakman2
Jonathan M. Oakman2