
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Commun., 22 April 2020
Sec. Health Communication
Volume 5 - 2020 | https://doi.org/10.3389/fcomm.2020.00020
Reflecting Japan's growing elderly population, communication between dementia patients and their family caregivers has become as much of an issue as ageism in neo-gerontology, nursing, and social work. The details of communication in dementia care are best described through the perspective of discourse analysis: theoretical concepts borrowed from applied linguistics and communication studies offer practical tools for monitoring how dementia patients experience communication with others, either domestically or professionally. Ochs (2002), e.g., adopted the theory of stance-taking to describe the interaction between an autistic child and other “normal” pupils. This discourse and the underlying power issue is analogous to the typical view of Alzheimer patients. In the field of social work, Feil (1993) defined the concept of a validation scale to gauge caregiver attitudes toward patients based on theories of individual schema, frame, and patient subjectivity. There are reciprocal versions of this concept in nursing, such as the invalidation scale suggested by Van Wheert et al. (2008). This study positions these concepts of validation and invalidation within the theoretical framework of discourse analysis, and uses them to analyze the illocutionary act or linguistic formula in communication between physicians, caregivers, and dementia patients, based on data recorded in a Japanese hospital examination room in 2016 (16 occasions; N = 58). The acts were found to correspond to: (1) psychological representation; (2) orientation and testing; (3) accusing and blaming; and (4) disruption and intruding on a patient's frame. Further analysis found an overuse of psychological verbs, which represent patients' thoughts, emotions, perceptions, and sensory status, with 50% unaccompanied by hedge as a modal marker to avoid strong subjectivity. In testing a dementia patient's cognitive status, 50% of the data contained questions that asked patients directly to report their cognitive status, requiring them to have a metacognitive awareness, or by infantilizing the patient through simple orientation. As for acts of accusation and claims about a patient's current symptoms, these included: a caregiver's extra intention as “voice” in forms of constructed speech (Tannen, 1986), deviation from the maxim of quantity (Grice, 1975), and poking fun at the patient. The results suggest that those subjectivities in caregiver and patient can be explained in relation to a social and structural power issue, which positions patients automatically as “the normal deviant” (Goffman, 1963), and positions caregivers themselves as an authority, as “the normal,” and as “representative.” From a practitioner's perspective, this framework suggests a need for introspection to acknowledge frame and subjectivity, as well as a need for compassion for the experiences of a patient's life.
Communication with dementia patients has been analyzed primarily using an approach that seeks to identify so-called problems in discourse. Williams et al. (2009) examined the problematic behavior of elderly individuals, such as agitation, withdrawal, and refusal of care, when caregivers use infantilizing elder speech. Similarly, in an analysis of caregiver communication strategies, Magai et al. (2002) also found the presence of infantilizing speech in addition to disabling, invalidating, and imposition acts.
Van Wheert et al. (2008) proposed the invalidation scale to measure patient subjectivity as constructed by caregivers. This construct can be observed as (1) representations of a patient's thoughts, emotions, or sensory status; (2) representations of intention by some utterance or action; (3) requests for reorientation toward reality; (4) accusations of misunderstanding related to memory loss; and (5) testing of cognitive elements. This framework suggests that the need to separate caregiver interpretations from those of patients is the key to understanding functional communication in dementia discourse.
The invalidation scale is based on the quality of working life among certified nursing assistants by using the MSP scale of negative communication, in which several behavioral guidelines are provided. Measures in the MSP scale include (a) invalidation (failing to acknowledge another's subjective reality), (b) accusation (blaming a person for actions or failures that arise from a lack of ability or misunderstanding), (c) disruption (strongly intruding on a person's action or inaction, thereby breaking the patient's frame of reference), and (d) knowledge testing (asking questions about facts instead of trying to accommodate the patient's environment).
In contrast, validation in dementia care has been described as including (a) recognition of the uniqueness and individuality of each patient, (b) recognition of the reasons behind acts and utterances, (c) recognition of the need for unconditional and unbiased acceptance, and (d) compassion and acceptance to reduce patient anxiety and preserve patient dignity (Feil, 1993).
Though the concepts of invalidation and validation seem to be quite opposite, standards based on these concepts seem to share a recognition of differences in personal schemas and backgrounds, as well as differences in subjectivity between patients and caregivers.
Moreover, each act on the scale of invalidation, MSP, and validation resembles a speech act in the sense that each word carries a pragmatic meaning that is intended to achieve an activity directed toward a certain purpose. For example, the utterance, “Please close the window,” has the same function as the utterance, “Don't you feel chilly?,” followed by a gaze to the window, in the sense that both utterances are used to achieve the same purpose; i.e., requesting others to close a window. More broadly, the term formula, which is used to tag the categories of each speech occasion, refers to the superordinate function of each speech act. For example, the sound and utterance “ha ha ha” can be categorized as laughter as a speech act in Japanese, but at the same time this utterance could have a superordinate purpose such as “insulting” according to the linguistic formula. This structural relationship between speech act and other superordinate linguistic categories can be found in Sinclair and Coulthard (1975), where Lesson, Transaction, Exchange, and Move are positioned above 20 sorts of acts.
Following this concept of superordinate and broader categories, the term speech act is also a subordinate category to the level called illocutionary acts (Searle, 1975). Typical examples of speech acts are expressed by a minimized function such as requesting, rejecting, asserting, inviting, greeting, and questioning. However, the categorization of a speech act varies depending on its propositional position. Searle (1975) discusses the variety of pragmatic functions and difficulty in forming systematic criteria for what are potentially thousands of illocutionary acts and psychological states. The definition of validation is a broader concept than a summary of speech act as function. In this paper, the concepts of invalidation and validation are analyzed in accordance with the term formula as describing the broader pragmatic concept.
The concepts of invalidation and validation in dementia care communication described above are related to theories of discourse analysis—particularly in terms of how visible/auditory patient communication tends to depend on the complex world of the caregiver. More broadly, these concepts have their origins in philosophy. Matsuda (1984) describes the framework of subjectivity and intersubjectivity in the field of philosophy that Husserl developed his theory of intersubjectivity by noticing and being aware of individual perspectives restricted to individual experience (Husserliana III.S108–109). This restriction of perspective should be overcome by negotiating self and other's “window of monad” to escape the ethno-centrism of each subject as well as the subjectivity of each act of recognition (Husserliana 1.S125). In intellectuality defined by Husserl, our restricted perspective and other perspective can be integrated together, through our portability earned by experience by asking how we experience ourselves and the world (Husserliana 1.S146).
In the field of discourse analysis, the construction of subjectivity employs terminology such as stance-taking, as defined in Du Bois (2007). According to Du Bois (2007), the interactional mechanism consists of the following three elements: object (the message in terms of utterances, non-linguistic expressions, and written text), subject (recipient of the message), and alignment (managed relationship between parties). The subject takes a stance and evaluates an object through their stance or background. The subject can provide numerous evaluations of an object, so long as an entity is present to interpret someone's utterance or gesture as an object. It almost seems as though the same word can have numerous meanings, depending on the pragmatic context. These subjective statuses of the subject are positioned by evaluating the object in the stance-taking triangle, as seen in Figure 1.
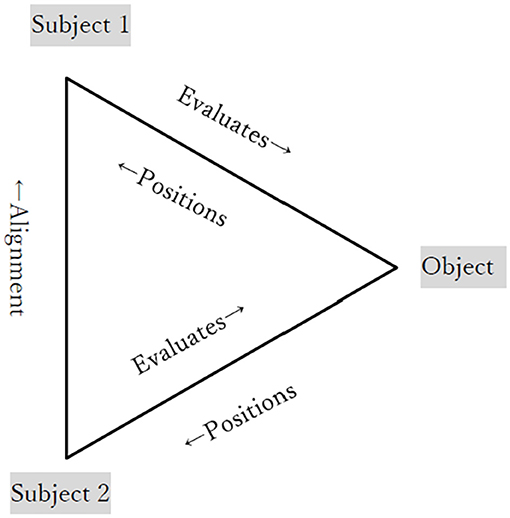
Figure 1. Stance-taking triangle by Du Bois (2007).
In considering the deconstruction of subjectivity as it relates to intersubjectivity, there must be more than two subjects, whereby the evaluation and interpretation by the first subject are also related and evaluated by a cooperative interpretation of the message. Through interactive negotiation between the subjects, intersubjectivity is constructed logically. This interaction becomes aligned and is usually achieved not only through verbal expressions but also through non-linguistic inputs. This phenomenon is called alignment of the stance of agreement or disagreement toward each subject's subjectivity.
However, this alignment can sometimes be used to construct the wrong “fact,” under the assumption that a positioning by Subject 1 is strongly believed for a certain reason and agreed by other subjects. For example, Ochs (2002) reports the example of ethnomethodological data, where an autistic pupil's successful activity in playing softball is minimized by her teacher and other teammates in their subjective judgments about her committing a foul. Though a catcher who took the nearest position to the pupil as a batter insists that she wasn't touching the ball at all, others' judgments from a subjective view aligned together, finally constructing the wrong fact that she committed a foul. This process of aligning interpretation to construct a “fact” is structured under the teacher's assumption that the pupil is disabled, who is subsequently misjudged under this assumption. In other words, the teacher's credibility is assured by the decision sustained by the majority, which gradually produces a “fact” despite evidence to the contrary. When the concept of stance-taking is applied to this data, the structure of stance-taking in the frame of Du Bois (2007) would resemble Figure 2.

Figure 2. Stance-taking triangle applied to Ochs' observation (Ochs, 2002).
The difficulty in forming systematic categories for the variety of pragmatic functions was noted above. Similarly, the definition of validation is also a broader concept when dealing with data than simply counting the number of functional speech acts. Regarding intersubjectivity and stance-taking, each utterance can be placed into a pragmatic and/or functional category depending on its formula or illocutionary act. Examples include assessment and appraisal, which are identified using adjectives, such as horrible, ideal, and nasty. However, there are no established criteria for the categorization of such intersubjectivity (Englebretson, 2007). By focusing on subjectivity and intersubjectivity and examining the pragmatics and functional aspects of speech acts in the caregiver–patient domain, this paper argues that caregivers frequently commit acts of invalidation. Intersubjectivity as a concept related to validation and invalidation in discourse analysis will be clarified, followed by a discussion of how these theories can be adopted for data analysis.
As discussed above, the concepts of validation (Feil, 1993) and invalidation (Van Wheert et al., 2008), as well as the MSP scale in dementia care communication, share a common theoretical basis with discourse analysis theories. Here, linguistic formulae and functions are proposed that can be identified using concepts like validation and invalidation frames. When merging each concept in relation to validation, invalidation, and MSP, some concepts belong to the same categories, as shown in Table 1.

Table 1. Categories of invalidation, from Van Wheert et al. (2008) and Feil (1993).
This merging of concepts seems to have the organization and structure illustrated in Figure 3.
Since invalidation has these organizational elements, discourses and narratives related to accusation and blaming, disruption, and knowledge testing were extracted from data in the initial stage to clarify how patient, caregiver, and doctor's subjectivities are constructed. Specifically, discourse and utterances that contain the formula or illocutionary act indicated in Figure 3 were extracted and then analyzed using discourse analysis to obtain a sense of patient individuality and reality beyond superficial utterances and acts.
This study used audio-based data from recordings made in some hospital examination rooms between January and June 2016. All data were audiotaped with the approval of patients or their family caregivers at the request of their regular doctor. As the recruitment strategy, the scope of the study was limited to senior dementia patients who were relatively at the early stages of the disease and could visit the hospital for their treatment sessions, sometimes accompanied by their family members. The data for this research scope may be designated as second use because the recordings were originally collected for the purpose of marketing research conducted by Verilogue Inc., via a local Japanese marketing company. The participants in this dataset included doctors, patients, caregivers, and sometimes nurses. The details of the age, gender, and level of dementia severity of the patients are presented in Table 2.
Discourse patterns related to invalidation, MSP, and validation, as shown in Table 1 and Figure 3, were classified by illocutionary content and formulae and were analyzed by the author, under four categories: (1) representations of a patient's thoughts, emotions, or senses; (2) requests for reorientation or testing knowledge; (3) accusation or blaming a patient for a misunderstanding related to memory loss; and (4) disruption, thereby breaking the patient's frame of reference. These categories were identified by sentences as well as contexts. In subsequent analysis, the details of linguistic and pragmatic elements were specified in relation to psychological verbs or modal markers, types of queries, the discourse condition surrounding accusation, strategies to soften impoliteness, and notable interaction related to disruption or intersubjectivity. As this study focuses on how caregivers interpret patient acts and utterances, caregiver utterances were the primary focus of the analysis. Utterances by patients and doctors were also helpful in identifying context.
Constructions of reorientation, accusation, and disruption were further analyzed as interactional elements using the theoretical frame of stance-taking (Du Bois, 2007), investigating how theory can be adopted when analyzing actual validation and invalidation settings in the data. Other theoretical linguistic frameworks, such as modal markers, theme and lemma, the meaning of laughter, and feedback are occasionally employed to clarify interactions between formulae.
The data analysis revealed the following four devices in the construction of subjectivity and invalidation patterns: (a) the overuse of psychological state indicators representing the patient's inner feelings without modal markers; (b) the testing of metacognitive faculties, which required patients to have more complicated cognitive skills, or unnatural testing, which disabled patients by asking simple questions like name or age; (c) accusations of patient memory loss that threaten the patient's identity; and (d) the construction of intersubjectivity regarding problematic patient behaviors, and the high credibility attributed to caregivers for their own subjectivities. All these cases indicate ultimately a failure on the caregiver's part to acknowledge the patient's subjective reality.
Additionally, phenomena that could belong to the validation scale were found in utterances by doctors. These included: (a) softening the impoliteness of orientation by merging it with other daily conversation including topics such as New Year celebrations or moving home; and (b) interpreting a patient's utterance by considering their frame and schema, instead of believing all of what is reported by the caregiver.
Accusations of diminished patient ability were frequently found in the examination room in the presence of a physician. This led to counter-accusations by the patients whose sense of identity was damaged. Other invalidation discourse included caregivers providing interpretations of problematic patient behavior, attributing it to patient idiosyncrasies that were reflections of the caregivers' own stances toward the patient.
Acts of invalidation frequently represent patient emotional and epistemic stances using psychological state verbs. According to Sugimura (2007), psychological state verbs include those related to thoughts, emotions, perceptions, and sensations in verbs or adjectives. Caregivers employed these strategies as linguistic devices to represent patient cognitive and emotional states. In addition, psychological state verbs used to express invalidation share pragmatic properties with MSP in terms of accusation, in the sense that they were frequently used to blame patients for actions or failures.
These psychological state verbs are usually restricted to the first-person pronoun or speaker in Japanese grammar, since it is unnatural in Japanese to assume the psychological state of another person (Sotozaki, 2006; Ohso, 2007). Yet, caregivers frequently represented a patient's psychological state as if they were the patient themselves, which coincided with acts of invalidation. In this study, all caregiver utterances related to psychological states were first extracted, and subsequently classified in terms of psychological categories and detailed formulae. Table 3 summarizes the expressions used to assert patient states through psychological state terms found in the data, following Sugimura's (2007) categorization of verbs and adjectives. These psychological states are usually expressed in the form of adjectives in English, whereas verbs are usually used in Japanese.
Of the 82 cases summarized in Table 3, the psychological categories break down as follows: (1) thought: 49 (56.1%); (2) emotion: 14 (17.1%); (3) perception: 6 (7.3%); and (4) sensory: 13 (15.9%). The first two examples also contain acts of accusation via claims of diminished cognitive function. In detail, most of the verbs related to thought refer to a PT's cognitive status, such as forgetting or remembering. As for emotional categories, statements of a PT's negative feelings such as hating, being depressed, being sad, or being irritated are reported by the CGs instead of the PTs themselves. In perception categories, there are two ways to refer to a PT's hearing and vision: one is expressed by simple verbs, while the other uses verbs accompanied with a modal to denote ability, such as “be able to.” The detail of sensory verbs shows various formulae, ranging from hurting to being calm.
In summary, the detailed features of those verbs could imply that the cognitive states of forgetting and remembering, for instance, are quite personal and hard to represent by a third person. However, some family members try to focus on suggesting how a patient feels, who they are hating, or whether they are enjoying life or not; the credibility of their suggestions from visible or audible keys is limited to a certain degree. Additionally, the suggestions about a patient's ability to see and hear are very personal, which cannot be understood by a person in a different physical condition, as shown in the following example.
Example 1. Thinking (Data #6)
01 DR: PT's forgetfulness isn't severe, but… She sometimes loses concentration; or rather, it's hard to maintain recollection. It is happening. [PT is referred to by name.]
02 CG: But (PT) is sometimes reminded of it later. (omoidasu)
03 DR: Sometimes (PT) can recall; yeah. If it were true dementia… (omoidasu)
In this example, the physician and the caregiver are discussing the patient's cognitive state, and frequently using “omoidasu” (remember/recall). In lines 01–03, the caregiver and doctor use the word without clearly stating the subject, i.e., the person recalling something. However, omitting the subject does not alter the context because it is implied that the patient is the subject.
As Merleau-Ponty (1962) notes on the connection between consciousness and sensations, individuals who experience phantom pain caused by a personal history of lost limbs doubt whether the pain can be a fact or not. Perception as an integrated common-sense concept and the result of scientific thought tends to cut out actual feelings from the personal experience of perception. Thus, the representation of psychological and physical perception itself, through its philosophical origins in the separation of mind and body, contains a philosophical basis for the neglect of a patient's real sensations and failing to acknowledge another's subjective reality. As such, “thinking” verbs to indicate cognitive states are frequently found in dementia discourse, while caregiver subjectivity and confidence in reporting patient recall are taken for granted.
Example 2. Emotional state (Data #6)
01 DR: I guess that her uneasiness could be a side effect of the medication.
02 CG: (She) has been irritable for a long time. (iraira shite-ta)
03 DR: That's the medication.
In this example, the physician and the caregiver are discussing possible side effects when the caregiver describes the patient as “continuously irritated” in line 02 without clarifying the circumstances. The caregiver displays strong subjectivity and authority in representing the patient's emotions without providing an example of an utterance or act to support the presumed irritability.
The psychological state verbs and adjectives listed in Table 2 that imply patient cognitive or emotional state frequently appear in the data. In each appearance, the subject is not explicitly stated. However, it is clearly implied that the subject is the patient, given contextual cues such as the physician asking about the patient. This representative mode frequently appears in the data, implying strong assumed credibility/subjectivity on the part of the caregiver while risking the invalidation of patient autonomy. Conversely, some psychological state terms accompanied by modal auxiliary verbs, citations, or sentence endings can be markers that represent the caregiver's objectified stance in parallel to the patient's subjectivity.
The following example introduces the citation marker “-to” as an expression of caregiver modality.
Example 3. Citation marker “-to” (Data #1)
01 CG: I think (she) seems a bit depressed.
Chotto utu-ppoi-na to omou -n-desu-yo-ne
02 DR: She is not cheerful today.
03 CG: She has been like this.
04 DR: Yeah, she is blunt.
05 CG: Anyway, (she) has a totally negative outlook.
In Example 3, the subjective claim that the patient is depressed is softened by a triple hedge in the form of the suffix (-ppoi) in line 01 as well as a citation clause used with, I think. The term “n-desu,” the combination of nominalizer and copula, is used to add the speaker's subjective comment, after objectifying the content of the proposition (Maynard, 1997).
These psychological verbs, which occur with modality markers to objectify their degree of credibility in representing a patient's emotional state, are used by caregivers in almost 50% of the recorded cases. The details of these modal markers for objectifying psychological representation are shown in Table 4.
These modal expressions emphasize the caregiver's perceptions and serve as an objectivity marker. Furthermore, such modality differs from direct psychological state terms that represent the subjective reality of the patient. While these pragmatic functions appeared in the data, so too did psychological state expressions without any modal hedging. Out of all 83 cases of psychological verbs recorded in the data, 42 were accompanied with modal markers to objectify their representation, and 41 omitted any modal markers to provide an objective stance.
Another integrated speech act proposed by invalidation and MSP is knowledge testing. This activity can be attributed to the institutional characteristic of dementia care in which the physician needs to know the patient's current symptoms, necessarily intruding on the patient's actions or utterances and breaking the patient's frame of reference. In the data, expressions of knowledge testing can be classified under two categories: (1) metacognitive requests, in which patients are asked directly to judge their current cognitive status; and (2) orientation, in which doctors ask patients to answer some simple questions to assist their judgment of the patient's cognitive status. This latter type of test can be divided further into two categories: (a) simple questions about a patient's name or age; and (b) cognitive testing, which is included naturally in normal conversation in the examination room, where a main topic progresses toward several lemmas (subtopics) during the natural conversational flow. From a functional sentence perspective, Daneš (1974) suggested a thematic progression pattern to the natural flow of conversation, in which the theme, which has already been introduced into a discourse, plays an important role as a hub in the conversational cohesion between lemmas, which conversely sustain the theme.
In order to examine the types of cognitive status tests, doctors' utterances related to orientation and testing were extracted and subsequently categorized as either metacognitive requests (questions such as “Do you think you forget things easily?”) or orientation. As for orientation, the expressions were further classified as simple questions (such as “What is your name?” or “How old are you?”) or orientation mingled with ordinary conversation to find out about a patient's current situation (including questions such as “Who did you go with to celebrate New Year?” and “Where is your son living now?”). In either case, whether testing cognition by direct questions or indirectly by asking questions about the patient's birthday or age, the doctors' utterances broke the natural flow of conversation. Some of these tests followed a hedge, such as an introductory remark like “I think you have already understood this is just a cognitive test, but…,” or simple modal markers attached to the sentence, such as “I feel like (the patient's cognitive status is).” Some also used a rephrasing of face-threatening words such as “forget” to more indirect words such as “be in trouble.” Table 5 shows the occurrences of each of these testing categories.
The results show that, of all the examination occasions from Data 1 to 16, seven occasions contained direct questions asking patients about metacognition. In five of these cases, the questions followed a hedge to soften the unnatural flow of the conversation. However, two cases out of seven did not show any hedge or introduction to a metacognitive request. As for orientation, doctors employed this type of testing in almost 50% of the occasions (8 out of 16), most of which constituted conversational orientation, which ensures a more natural flow of conversation. Typical orientation in the form of simple questions occurred on two occasions. Of the eight conversational cases, six show a form of hedge, whereas two show a total lack of hedge. The following examples help to explain how these cognitive tests are a potential threat to a patient's face and show how hedges are utilized to soften unnatural conversation flow.
The following are two examples of metacognitive requests, in which patients are asked directly to recognize their memory status.
Example 4. Metacognitive request (Data #5)
01 PT: They just stand there waving for a while.
02 DR: So, you can't recall what [NAME OF OTHER] was looking like this year.
03 PT: I can't see that clearly. I think watching them on TV is the best.
04 DR: Ah, the footage on TV is better, huh? I guess that is true.
05 PT: I thought I might remember more but it was such a quick glance, I can't really picture them anymore.
06 DR: I see, but you remember going there, though?
07 PT: Yes. [LAUGHING]
08 DR: Then you are okay.
In this example, a doctor asks a patient to judge her memory in relation to a previous topic (New Year celebration). Though the object to be recalled is pointed out in the conversation and could make it easy for the patient to reply, the doctor's questions in lines 02 and 06 ask the patient directly to recognize their own cognition. This kind of metacognitive request is more complicated than a simple question, such as “What did she look like?” or “You did go there, didn't you?” The complexity arises as the patient initially must objectify themselves from a third-person perspective and then needs to qualify that objectivity by a subjective judgment. As well as the politeness issue, this kind of questioning gives the impression that the patient is positioned not as a complete adult but is rather infantilized or rendered incapable. This positioning by the doctor is followed by laughter on the patient's side in line 07, as a sign of “feeling embarrassed” (Morreall, 1981). This embarrassed laughter is specific to the testing of cognitive status, including metacognitive, conversational, and orientation tests, and was found in 9 out of 16 data.
Example 5. Metacognitive request (Data #8)
01 DR: How about her memory? How's her forgetfulness? Do you remember anything about recent news? Anything interesting that caught your attention? Could you talk about it a little?
02 PT: I've been watching the parliamentary proceedings on TV.
In this example, a doctor asks a patient if she remembers something or not. This kind of metacognitive test fails to protect the patient's dignity as a complete adult and is harmful mainly for two reasons: (1) its unsuitability as an examination of a patient's cognitive situation; and (2) the politeness issue due to unnatural and blunt questioning, while positioning patients as incapable.
Orientation aims to detect whether patients recognize the relations between themselves and outside factors involving time, space, or interpersonal relationships. These simple questions are often employed in dementia examinations. However, they also have the same potential to harm the patient's sense of politeness or cause embarrassment and could still position the patient as being as incapable as a child or pet, especially in cases of patients at the early stage of dementia.
Example 6. Request for orientation (Data #3)
01 CG: One time, she couldn't pay the karaoke fee because she lost her money.
02 DR: So, that kind of stuff has been happening… I got it. How old are you?
03 PT: 79 years old. Born in the eighth year [of the Showa era].
04 DR: What's the date again, today?
05 PT: Today is [LAUGHTER] January.
06 DR: What day of the week is it?
07 PT: Tuesday.
08 DR: That's right. Tuesday.
Here, typical examples of orientation are shown in lines 02 and 04, in which the doctor asks simple questions about the patient's age and date. These questions can also be interpreted as impolite, because they are simply excessive diagnostics in a case of mild cognitive impairment (MCI). At this instance, typical examples of orientation are shown in lines 02 and 04, in which the doctor asks simple questions about the patient's age and the date. These questions may also be interpreted as impolite because they denote excessive diagnostics in cases of MCI. The cognitive decline of MCI patients would be obvious in comparison to their counterparts of similar age and educational backgrounds without MCI (Gauthier et al., 2006). Nonetheless, patients with MCI can lead their daily lives in a relatively normal manner in comparison to those presenting the type of dementia seen in Alzheimer's disease. At this instance, typical examples of orientation are shown in lines 02 and 04, in which the doctor asks simple questions about the patient's age and the date. These questions may also be interpreted as impolite because they denote excessive diagnostics in cases of MCI. The cognitive decline of MCI patients would be obvious in comparison to their counterparts of similar age and educational backgrounds without MCI (Gauthier et al., 2006). Nonetheless, patients with MCI can lead their daily lives in a relatively normal manner in comparison to those presenting the type of dementia seen in Alzheimer's disease. As for breaking the natural flow of conversation, the physician suddenly changes the topic from managing money to the patient's date of birth in line 02 and the current date in line 04. This topic shift is unnatural in the sense that this kind of conversation would only take place in an examination room. Moreover, the patient seems accustomed to this kind of testing as evidenced by her immediate recognition that the impromptu questions were directed toward her, while she can still feel some embarrassment as shown in the laughter in line 05. This example shows that testing is an act of disruption that forces the patient into the physician's frame of reference.
The details of the results summarized in Table 5 show that several types of hedge are used to soften the potential harm associated with cognitive testing. The types of hedge can be categorized as follows: (1) grammatical expression (two occurrences); (2) rephrasing (three occurrences); (3) showing a boundary (one occurrence); (4) introduction and initiation (seven occurrences); and (5) camouflage as ordinary conversation (three occurrences). The strategies of 1 and 2 focus on small elements in an utterance, such as a modal marker (“I feel like that”), or turning harmful phrases (such as those involving forgetting) to indirect expressions (“remembering must be hard”), as noted above. The strategies of 3–5, in which the doctor indicates a shift of topic toward cognitive testing, are linguistic devices inserted before the cognitive test utterances. The following example is a case of introduction in advance of cognitive testing.
Example 7. Hedging by introduction/initiation (Data #5)
01 DR: How about making an appointment for the liver exam for the 15th of November? What time would be good?
02 PT: How about around the same time as today?
03 DR: Okay, it will be on the 15th.
04 PT: Thank you.
05 DR: Well, I think you understand what is going on, but I'd still like to ask you a few questions. How old are you?
07 PT: 79 years old.
08 DR: Good. And when is your birthday?
09 PT: May 20th.
In this unnatural exchange, the physician makes a meta-discourse comment by stating in line 05, “Well, I think you understand what is going on, but I'd still like to ask you a few questions,” which marks a register shift toward testing, albeit hedged to mitigate intrusiveness. The physician seems to recognize that knowledge testing is a face-threatening act, but nonetheless proceeds in line with the authority granted to physicians. This excerpt illustrates therefore both a test of knowledge and an act of disruption according to the MSP scale, since the physician maintains their own frame of reference without attempting to accommodate the patient's frame of reference.
The next example is a hedge that is mingled with natural conversation during the examination. This strategy is effective in not making patients feel that they are being tested.
Example 8. Hedging by camouflage as ordinary conversation
01 DR: Do you watch news on the TV? You take a rest, too. Well, in terms of the news about the governor of Tokyo.
02 PT: Yes, I do. [PT names the governor of Tokyo] That's terrible.
03 DR: What did he do? Why is he blamed?
04 PT: He is mixing up official business with personal affairs.
[…omitted material…]
05 DR: An investigation committee won't be held.
06 PT: Yes, why not. It would be obvious if he is guilty or not.
07 DR: I see. I wonder.
08 PT: It is not good to mix official business with personal affairs, because he uses our tax.
09 DR: Yes. You remember a lot and have a good memory. (CG/PT: [LAUGHING])
10 PT: These topics are easy to remember. I cannot remember difficult topics.
Here, it seems as if the doctor is just asking about the PT's ordinary life, not focusing solely on dementia symptoms, but integrated with other elements such as lifestyle. The TV news topic is very vague in its relation to cognitive testing and to the previous topic, in which the PT claimed that she needs a break from housework, for example, by watching TV. However, it is clarified at the end of this topic, where the doctor reveals in line 09 that he is checking her cognitive status by commenting, “You remember a lot.” Following this sequence, CG and PT burst into laughter in line 09; the patient then explains the humor in the evaluation of her own cognitive status by commenting in line 10, “These topics are easy to remember.”
In this conversational exchange, the doctor uses the strategy of developing the conversation and subtopic (lemma) based on the main topic provided at the beginning. In contrast to testing knowledge directly, this strategy requires doctors to be more skilled in discourse structure, particularly in how to introduce cognitive checks without committing too much impoliteness and avoiding giving the impression that the patient is incapable.
Utterances and contexts where caregivers accused or blamed patients for their actions, failures, misunderstandings, or lack of ability were also extracted from the data. The formulae and illocutionary acts found in those extracts were then divided into five categories, based on the degree or directness of each accusation: (1) contrasting (statement of idea and matter opposing what patients said); (2) claiming patient's symptoms as a cause, addressed toward patient (statement of event or situation, which is attributed to patient's bad behavior or cognitive state); (3) claiming patient's symptoms as a cause, addressed toward doctor (statement of event or situation, which is attributed to patient's bad behavior or cognitive state); (4) constructed speech, which cites a patient's thoughts or feelings; and (5) poking fun or joking about a patient's utterance or situation. The degree of accusation would be highest in 1 and diminishes through 2–5. The results of this analysis are shown in Table 6.
In considering these results, the category of claiming or blaming should be considered first. Clearly stated accusations (such as “No, you don't remember”; or, “You are stupid”), which could be used with strong negative or insulting words, were not found in the data. The most frequent form of accusation was speaking ill about patients addressed toward doctors. In this case, it was difficult to judge whether an individual utterance could be categorized as “accusation/blaming” or simply as reporting the situation. Whether a person takes an utterance as accusing or reporting can depend on the person's perception. In the case of contrasting, clues are relatively easy to find by examining the logical connection between a PT utterance and a CG utterance, as shown in the next example.
Example 9. Accusation: contrasting ideas
01 DR: Oh, so you kind of exercise during housework.
02 PT: I do everything.
03 DR: All the housework?
04 CG: She lives with her husband.
05 DR: I see, I see.
06 PT: That's why I have to do it by myself.
07 DR: He helps you a lot?
08 PT: No way.
09 CG: He does wash the dishes at night.
10 PT: No, no. Only because I eat earlier than him.
In this conversation about who does the housework in the patient's home, controversy is evoked among the PT and CG in lines 06–10 because the patient insists that she does it all, which is contradicted by the caregiver's utterance in line 09: “He does wash the dishes at night.” Whether this is making a false claim or just reporting a fact, it evokes further patient opposition with strong negation in line 10 because it insulted her identity or frame. If the caregiver's utterance were addressed to the patient herself, this would place the statement in the broader category of blaming.
Other examples in the claiming symptoms categories 2 and 3 also provide difficulties in distinguishing accusation from reporting fact, as the statements are vague on whether the caregiver intends a blame. This is particularly the case when a statement toward doctors is vague about patient memory loss or a bad situation, because they can be said to be just reporting a patient's current situation as representative. However, there may be clues. For example, there is an element of “common sense” to conveying certain utterances, following pragmatic theories about conversation. For example, Grice's Cooperative Principles (Grice, 1975), which include Quantity, Quality, Relation, and Manner, could indicate whether those utterances stating a patient's current symptoms belong to unmarked conversation or a marked one, which includes extra “conversational implicature.”
Following this maxim, the next example seems to violate some of the principles of marked discourse, which include the patient's manner of “accusation.”
Example 10. Accusation: claiming PT's symptoms, addressed to DR (Data #4)
01 DR: How's everything going? She looked a bit grumpy the whole time.
02 CG: Yes, she's been like that.
03 DR: I see. We were talking about driving a car earlier and he tells me she hasn't been near the key for three, four years.
04 CG: Ah, is that right.
05 DR: It was this year, wasn't it?
06 CG: Yes. She forgets everything like that. For example, she would say she hasn't had anything to eat right after she finishes a meal.
07 DR: She says that?
08 CG: Yes. We just stopped at her brother's grave for a visit, but she said to me that I hadn't taken her there for 6 months.
09 DR: Oh, I see, she wants to visit there more often?
10 CG: No, what I mean is that I take her there quite a lot. She forgets, then when we get there, she sees the live flowers there and realizes that we have been there recently. She thinks I am lying to her.
As seen in this example, almost all the caregiver's utterances are related to claims about the patient's memory loss. It seems to be normal, especially at the beginning of the session, because of the caregiver's responsibility in representing the patient's current symptoms and situation. The purpose of the doctor in checking her cognitive status could be because they need some supporting evidence before concluding her treatment plan. However, the caregiver's claims about the patient's bad cognitive situation continue until the end of this examination session.
Example 11. Accusation: claiming PT symptoms, addressed to DR (maxim of quantity)
01 DR: I see. Let's try the new medication and tell me how that goes next time.
02 CG: Okay.
03 DR: Not too significantly but her attention has declined and there is a slight issue with apathy, the decrease of self- motivation. From what you have told me today, her memory seems to be not so good either, though?
04 CG: Her memory is not good at all.
05 DR: I understand. Her mind is somewhere else.
06 CG: I have asked her what day it is today before we came here. I ask her who came and visited her, and it is only on Thursdays that we have a visitor, so she says, oh, it was Thursday yesterday, then it must be Friday today. There are times when she asks herself, is it nineteen fifty what now?
07 DR: She's off the mark that much? That is strange as the test results show she got the dates right, ah, except for the year.
08 CG: Of course, because we went through that before we came here.
09 DR: Really. [LAUGHING] I see now.
10 CG: She gets my daughter's age wrong every time too.
11 DR: Her grandchild's age? I see. Well, let's continue with the treatment and let me know how things are again next time.
12 CG: Yes, thank you very much.
13 DR: Thank you, take care.
In this coda to a discourse, the doctor indicated the treatment plan in line 01 and checked the situation with the CG, by which he concluded the treatment plan in line 05 and then tried to close the conversation in line 11. However, somehow the CG could not stop making claims about the patient's cognitive status and tried to give new and more detailed information about the patient's inability to memorize things. This caregiver's attitude of claiming continues for 8 min and 8 s out of a total recording time of 11 min and 13 s. This kind of conversational flow deviates from the maxim of Quantity: one should state the required amount of information; and should not state more information than required.
Those conversations that belong to “accusing” rather than “reporting” are recorded in a total of 42 cases, which are pragmatically obvious underneath the linguistic surface. This intention of the caregiver to accuse or blame can also be found in the ways of making fun of a patient, such as by citing patient utterances, as seen in the following examples.
Example 12. Accusation: constructed speech (Data #11)
01 CG: I can't tell if she's really listening to me or not. Just that she's so dazed. But she also shows a sense of victimization. She tells me that I haven't been visiting her for a long time. But I have. I must keep reminding her that I have been here two days earlier, we have gone to see a movie together. I don't think she remembers it but when I tell her, she says “Huh!”, she insisted she remembers it. But I suspect she really can't remember.
[…omitted material…]
02 CG: It's so challenging to deal with her as she interprets everything negatively. She keeps asking the same questions too. Say, I have explained something five seconds ago, she interrupts me saying, “I have heard enough, are you stupid?”, but she hasn't listened to what I have just said. So, she repeatedly asks me about it over and over.
In the above data, this patient as a persona reported in the caregiver's narrative gives an impression of a violent and strong-tempered woman. However, the patient herself, who appeared previously in Data #4, sounds like a silent and ladylike woman. All of the citations that represent PT utterances are expressed as direct citations and use an exclamation mark as a terminator. This is characteristic of the “demonstration” type of citation (Clark and Gerrig, 1990), which includes extra implication of the speaker themselves. This type of speech is also categorized as “constructed speech” in Tannen (1986), exemplified in a narrative case, where the speaker uses constructed speech in order to enhance his fear and surprise in witnessing a tragedy in an emergency center in a hospital. Following this angle, the caregiver's narrative in this example could also be categorized as constructed speech, which could not really have been uttered by the patient but reflects her feeling toward this event. In this case, her utterance in 01 and 02 could belong to the “accusation/blaming” category rather than just reporting a patient's memory loss.
The next example shows another type of caregiver subjectivity reflected in conversation in the examination room.
Example 13. Poking fun, joking (Data #10)
01 DR: How old are you?
02 PT: [AGE].
03 DR: What's your date of birth?
04 DR: What day is today?
05 PT: Tuesday.
06 DR: Tuesday, yes. This calendar shows March, therefore you answered like Tuesday. Nearly correct.
07 PT: Oh, is that so? I misunderstood it.
08 CG: You made a hit then. (DR: [LAUGHTER])
In this example, the PT is oriented toward the doctor's questioning. Seemingly, the CG utterance in line 08 is praising the PT's mistake in line 06 because the evidence of the calendar led her to the answer. However, the utterance, “You made a hit,” is actually a response to the previous PT utterance, “I misunderstood it.” Given the doctor's laughter that follows, the CG utterance, “You made a hit,” could be interpreted as a speech act that pokes fun at the patient. Such accusations attributed to poking fun or joking were seen five times in the entire data.
Expressions related to disruption and intruding were examined qualitatively, because the concept of disruption and intruding on a patient's frame is actually a superordinate category to all of the other analytical categories, including psychological representation, orientation and testing, and accusation and blaming, as indicated in Figure 3.
Moreover, the subject of disruption and intruding on a patient's frame will be discussed together with subjectivity and intersubjectivity in the discussion below. Disruption and intruding are defined as acts that neglect a patient's own perspective and cognitive frame. Here, “frame” can be interpreted as schema or individual standards for understanding and positioning each personal interaction. Tannen (2006) observed how a pediatric doctor changed their ways of speaking to fit the schema of an infant patient, the infant's mother, and a group of interns. Additionally, Tannen (2006) indicated that different frames about sharing housework between wife and husband are reframed by that of their child.
Thus, the examination of disruption and intruding focuses on utterances in contexts where a patient's frame is neglected or not well-understood. The impressive utterance, which could symbolize the problem in dementia communication related to subjectivity and intersubjectivity, is also extracted for qualitative analysis. In this case, extracts are taken from utterances by all the participants, as well as from the range of illocutionary acts. Analysis of the results revealed four categories of disruption and intruding, as shown in Table 7.
The first notable element related to a patient's frame is that patients themselves show a humble attitude toward their judgment or subjectivity, which may be due to their understanding of how the outside world would see them as “senile.” The following examples include impressive utterances on a patient's low opinion of their own subjectivity, and of how the world views them.
Example 14. Patient's low opinion of their own subjectivity (Data #3)
[PT is asked the address of her son's place.]
01 PT: Ehh…, where is it? [detailed address]? It is [detailed address] in my head.
In this acknowledgment, it seems as if the patient has already been notified that her cognitive status is vague, which could have influenced her faith in her ability to make an objective judgment.
Example 15. Patient's Low Opinion of Their Own Subjectivity (Data #11)
[PT is notified that DR plans to increase the dose of anti- dementia medication, through the result of MRT.]
01 PT: I myself don't have any need like that (necessity to increase a dose).
In this example, the patient tried to decline the doctor's plan for medication, which contrasts with the PT's good result in MRT. The DR however takes a careful approach, which considers the possibility that the PT may be unable to understand the dosage measurements.
These utterances imply that there are some patients who consider that they should not place too much trust in their thought, judgment, memory, feeling, sensations, and even consciousness. This humble attitude of the patient is in stark contrast to that of the caregivers in the next examples, in which patients are positioned as “deviants.”
Example 16. Positioning patient as deviant: comparison to “natural” (Data #8)
[Talking about the issue of overeating.]
01 DR: But she remembers eating them, doesn't she?
02 CG: She remembers eating them, but she ends up looking sheepish as she knows that she will be scolded.
03 DR: Oh, I see. What does she do when you tell her off?
04 CG: She thinks it over.
In this example, the caregiver fixes the standard to her frame (the PT is a victim of her overeating) and assumes that it is natural to scold the PT when she commits an act of overeating. Moreover, even her emotional reflections, such as “sheepish” or “thinking it over,” are assumed to be natural consequences. In some cases of dementia, overeating is widely recognized as a symptom due to the patient's feeling of being hungry. Hence, the symptom can be “natural.” In other words, scolding this natural symptom, which is due to the extraordinary feeling of hunger and is experienced as real by the patient, can be defined as “unnatural.” Such failures to realize a patient's frame, due to the PT's low opinion of their own subjectivity, are also found in the next examples.
Example 17. Positioning patient as deviant: Patient's defense as “natural” (Data #10)
01 DR: Does she lose something or forgets where she puts it?
02 CG: She sometimes forgets where she puts things.
03 PT: Yes, I do.
04 DR: You cannot find that?
05 CG: No, it was lost.
06 PT: But, you know, I am [AGE].
In this example, the assumptions and standards of “normal” and “natural” become controversial. For example, whether the PT forgets things is discussed here among three participants, and the CG gives a negative view in both lines 02 and 05. In this case, all the observations related to the PT's cognitive status seem to be positioned as symptoms associated with dementia. However, by defending her stance, this patient casts doubt on drawing the line between forgetfulness associated with the natural situation of aging and dementia. It also stands in contrast to the CG's strong belief in her own subjective judgment.
Example 18. Judgment, based on assumption of deviation (Data #12)
01 PT: After I came here, she also started throwing bowls. She poured hot water on me when she was in a bad temper.
02 DR: If she started those acts, then it can be called a fight…
03 PT: She was angry.
04 DR: Well, you have become calmer, I suppose. That's why she doesn't get angry and throw things.
In this example, the doctor seems to be on the side of the patient's wife, who the PT insists started this fighting to abuse him. The logical connection of the utterance in line 02 seems to lack integrity, if a “fight” is defined by the activity, not by someone's claim. Moreover, it is difficult to make a clear judgment that the reason why the PT's wife is not committing violent acts anymore is because the PT has become calm. This discourse seems to be based on a certain assumption that symptoms due to the patient's dementia would cause this incident, while positioning the patient as the cause of bad behavior and “stigmatizing” the family.
The next example shows that a CG can have a high opinion of her own subjectivity and judgment, and that these views, when aligned with a doctor's, can turn subjectivity to objective fact.
Example 19. Construction of “objectivity” by alignment of subjectivities (Data #14)
01 DR: Please separate her a bit from the others. She has been known to strike out a bit.
02 CG: Well, I have a sister, and she (PT) really hates her. She deeply hated my sister (DR: hum…), and this is where her violence comes from.
03 DR: So, this is the source of her problem behavior?
04 CG: Yes, it is.
05 DR: She has such a discord with your sister?
06 CG: Yes.
07 DR: Oh, that why. I've been considering why she hates especially women, who they could resemble.
In this example, the doctor advises that the patient be isolated from other residents at the facility in order to avoid potential violence. The caregiver then proposes a reason for the violence, cooperating with the physician to align their subjectivity as fact and ignoring alternatives. The boundary between the necessary representation and over-representation of patient intention is an obstacle that requires regular monitoring, and the avoidance of high opinions of her own judgment on the part of the caregiver.
Those strong assumptions, shown in Examples 16–19, originated by a third party's strong subjectivity and high opinion of their judgment and at the same time position patients as the deviant and as unnatural. This patient's attitude contrasts with that of the patient in Example 15, who is humble and calm and takes the third party's view of themselves for granted.
This paper has analyzed how illocutionary acts in dementia discourse can be categorized according to the concepts of invalidation, MSP, and validation. A variety of functional speech acts, such as psychological verbs, requests for orientation, and accusation and blaming, were classed as subordinate categories under the superordinate category of disruption and intruding on a patient's frame, as shown in Figure 3. However, these categories are components of another broader concept related to how patient, caregiver, and doctor take stances in terms of their subjectivities and intersubjectivities. This is the most significant characteristic in analyzing dementia discourse in Japanese. In this discussion, the integrated concept of subjectivity and intersubjectivities is situated in the frame of an axis of “the normal” and “the normal deviant” (Goffman, 1963).
Observing each utterance related to validation and invalidation, it seems that the positioning of patients as the deviant against the concept of normal and healthy others plays an important role in distinguishing the characteristics of this institutional talk, in which patients are obliged to accept their stigmatized status and are not allowed to have a high level of credibility regarding their cognitive state. Since individuals are restricted in the world due to ties to their own perspective and experience (Merleau-Ponty, 1962), patients facing this vulnerability are accustomed to doubt their subjectivity. Meanwhile, under this social structure, caregivers maintain a high level of confidence in their ability to be the normal and as the voice of authority.
This confidence in the subjectivity of the caregiver is reflected in testing and orientation. If we were to be tested with questions such as “How are you?” or “Do you find it easy to forget things recently?,” we would tend to feel insulted, with resentment over the fact that we are not mad. However, dementia patients accept this impoliteness, responding at most with embarrassed laughter. This acceptance of impoliteness might originate in their understanding of their institutional role as a “dementia patient,” together with an acceptance of the label of normal deviant. In other words, they are tailored into the frame that “the normal” requires them to adopt. This power structure can also affect patient recognition of the vulnerability of their subjective stance, as apparent in expressions such as “in my head” (Example 14) and “I myself don't have any need like that” (Example 15), which distinguish their uniqueness, and this sense of uniqueness becomes a sense of “the normal deviant” under this institutional structure.
However, not all parties in this structure follow this egoistic approach to requests. As shown by the examples of conversational testing, some doctors employ camouflage, in which the boundary between testing and ordinary conversation is vague and the potential for impoliteness is avoided. In Goffman's terminology (Goffman, 1963), they play the role of “the wise” who understand the patient's standing through their numerous experiences of tracking the patient's development. Conversational testing also coincides with the concept of “validation,” either by recognizing the reasons behind acts and utterances, or by recognizing the patient's need for unconditional and unbiased acceptance. This recognition of reasons seems to underline the alignment of subjectivities in Example 19, where the caregiver proposes a reason for the patient's violence. Here, the possible reasons, the need for recognition, and the subsequent alignment are the prominent features of the discourse. The bias and direction of bias are key, in the sense that the caregiver is required to find some bias toward the patient, while retaining her own authority.
The egoistic orientation to the patient as “the normal deviant” is also found in acts of accusation and insulting. In Example 16, the caregiver assumed that scolding the symptom of dementia (overeating) is natural. However, punishing the patient will not have consequences for the patient's subsequent action, because this is part of the disease. The caregiver seems to liken the patient to a child in considering that punishment would serve to improve their behavior, but the situations of patient and child are not the same for many reasons. Example 11, in which the caregiver continues to report on the patient's poor cognitive status, also reflects this egoism of “the normal.” The overstated report deviates from the maxim of quantity but includes extra “conversational implicature” regarding the intention of the speaker. In Example 18, the caregiver's high credibility is supported by the doctor, who assumes that the origin of the married couple's fight must be the patient as the stigmatized, rather than the wife as the normal.
It is the institutional structure and the roles within it that makes such an alignment possible. As discussed earlier, the interactional mechanism consists of the object, the subject, and the alignment, as exemplified in the case of the autistic pupil in Ochs (2002). The false conclusion arrived at in that case, achieved by the interaction and alignment of subjectivities, occurs under a similar mechanism. The fact that the pupil did not commit a foul is treated as false by agreement among the other (“normal”) teammates. Similarly, in Example 18, the doctor agrees with the caregiver's subjectivity in identifying the cause of the patient's violent act. Here, the power issue of the normal vs. the stigmatized also enables this discourse feature.
Thus, patient and caregiver take an opposite stance in their attitudes toward their own subjectivity. However, not all patients accept an institutional structure that positions them as the deviant. Some patients protect themselves by denying the institutional norm of “passing,” insisting for instance that not all cases of forgetting things belong to the symptoms of developing dementia. In Example 17, the patient casts some doubt on the caregiver's interpretation of her forgetting where she puts things, as this, she suggests, can also happen to others without dementia. Thus, she undermines the distinction between “the normal” and “the deviant,” and refuses to obey the institutional norm.
As mentioned above, some doctors play the role of “the wise,” who understands the personal situation of dementia patients through their experience. This type of doctor utilizes their representation of patient's though not as invalidation, but as validation, by recognizing the reasons behind acts and utterance without bias or assumptions about their role as “the stigmatized” under the institutional structure. We return to Example 10, which illustrates the stance of validation. In this example, the stance of the doctor reveals an attempt to understand the reasoning behind a patient's utterances without bias.
01 CG: Yes. We just stopped at her brother's grave for a visit, but she said to me that I hadn't taken her there for 6 months.
02 DR: Oh, I see, she wants to visit there more often?
03 CG: No, what I mean is that I actually take her there quite a lot…
In this example, the accusation about a patient's cognitive status has been stated continuously, but the doctor suggests a way to interpret the patient's utterance, instead of focusing on incidents that she forgot. Whereas, the caregiver's claim is focused mainly on the proposition of “forgetting,” the doctor shifts the focus by providing another subjectivity: the patient's forgetfulness about her visits to the grave actually reflects her eagerness to visit there more often. In other words, the focus is not on whether she was taken there, but how many times she was taken there.
We now return to Example 9, which provides another example of validation and intersubjectivity toward a patient's utterance:
01 PT: I do all the housework.
02 DR: Oh, so you kind of exercise during housework.
03 PT: I do everything.
04 DR: All the housework?
05 CG: She lives with her husband.
06 DR: I see, I see.
07 PT: That's why I have to do it by myself.
07 DR: He helps you a lot?
08 PT: No way.
09 CG: He does wash the dishes at night.
10 PT: No, no. Only because I eat earlier than him.
11 DR: Does he help you sometimes?
12 PT: Yes, he does.
13 CG: He is a good man.
14 DR: I do the housework, though the husband assists me.
In this example, the statements concerning housework differ between patient and caregiver, though the doctor's question in line 07 is somehow accepted by the patient. The conversational flow does not appear to show any agreement. However, the doctor succeeds in detecting the facts when the patient says in line 14, “I do the housework, though the husband assists me.” This suggests a consistency on the part of the patient in insisting that she is the housewife who is responsible for the work, and the husband is just assisting. Thus, the doctor succeeds on the validation scale in “recognizing the reasons behind acts and utterances.” In contrast, the caregivers in the recorded data limit their perspectives to their own frames. The practice of “the wise” can be a sophisticated form of validation, based on an understanding of a patient's struggle and how their situation can be improved. Such an understanding is the source of validation and acts ultimately to protect a patient's dignity.
This study has explored the concept of invalidation through an examination of dementia care discourse, with each occurrence conforming to the criteria of the invalidation and MSP scales from the perspective of intersubjectivity and stance-taking. First, psychological state verbs and adjectives, categorized into thoughts, emotions, perceptions, and sensations, were used to represent patient subjectivity. Such verbs, such as forgetting and remembering, were mostly related to thought and referred to a patient's cognitive status. Third-party speakers tended to represent the subjective realities of patients without modal markers for objectifying their subjective judgment in almost 50% of the recorded cases, thereby neglecting the patient's subjectivity toward her/his own acts and utterances while favoring the caregiver's and doctor's interpretations.
As for the illocutionary acts that reflect invalidation in knowledge testing and orientation, almost 50% of the data contained metacognitive questions that ask patients directly to report their cognitive status, and thereby embarrass patients at the early stage of cognitive impairment. Though most of the cases were accompanied with a hedge or introduction to avoid impoliteness, these acts still have the potential to intrude on a patient's frame. The exceptional cases include those questions that are camouflaged with ordinary conversation, in which the strategy of developing conversation by maintaining cohesion between theme and lemma was observed.
Accusing and blaming acts, in which claims were made about a patient's cognitive symptoms, were frequently found in the data. In these cases, linguistic devices, such as constructed speech and the maxim of quantity, are the key to detecting the speaker's “voice” and for distinguishing between claiming and reporting. Other illocutionary acts of accusation and blaming included the contrasting of ideas and poking fun at a patient.
The final category in the invalidation scale is the overarching category of disruption and intruding on a patient's frame. Qualitative observation shows that dementia patients tend to have a low opinion of their subjectivity, in contrast to the high opinion of the caregiver, who positions the patient as a deviant, often utilizing the frame of natural vs. unnatural. This frame of natural vs. unnatural is the basis of the assumption that patients are the cause of any trouble with others and affects the caregiver's and doctor's judgments through the alignment of subjectivities among the two parties.
This study attributes the intersubjectivity and subjectivity reflected in these illocutionary acts to a certain power issue, which is only enabled under this institutional structure of dementia discourse. In an axis suggested by Goffman (1963), patients are automatically labeled as “the normal deviant” in contrast to others who are positioned as “the normal.” The institutional structure tends to lower a patient's self-confidence in their abilities, whereas caregivers can represent a patient's thoughts and feelings through their institutional role. Moreover, these representations become “facts” through the alignment of subjectivities and can potentially lead to a false judgment. Some patients are accustomed to the strategy of “passing,” recognizing how they are socially labeled and avoiding possible interactional conflict. In this situation, the patient needs to retain a wider perspective to consider several subjectivities, whereas the caregiver can maintain the same perspective, which is limited to their own subjectivity.
However, some patients opposed the egoistic approach under the institutional norm of “passing” and declined to be wholly positioned as “the deviant,” using strategies such as casting doubt on the boundary between dementia and forgetfulness due to normal aging. Moreover, some doctors are aware that there is a role for “the wise” besides “the normal” and “the normal deviant” in this institutional structure and suggest alternative interpretations of a patient's utterance. Recognition of the reasons behind acts and utterances fits into the frame of validation and could also work to avoid potential hurt to the patient and paternalism in the examination room.
Feil's framework of validation (Feil, 1993) shares some elements with frames in linguistics and discourse analysis and also accords with theories of intersubjectivities, such as wrongly constructed alignment in Ochs (2002), voice and dialogic in Bakhtin (1986), intersubjectivity in Husserl (1973), and the subjectivity of personal sensations in Merleau-Ponty (1962). The various illocutionary acts and linguistic formulae are employed to achieve intersubjectivity and subjectivity in institutional dementia discourse.
Feil (1993) proposes that validation in dementia care should involve a respect for individuality, which is achieved through an awareness of patient uniqueness as well as an avoidance of personal bias. Feil's framework goes on to promote caregiver objectivity independent of subjective preconceptions. Validation is a principle of sociolinguistic and discourse analysis that can improve the care of those living with dementia by helping caregivers and physicians better understand the impact of their speech on the autonomy and dignity of the patient.
Some acts of validation and invalidation may appear superficial. However, the existence of bias toward the patient is an element that should be monitored. Additionally, caregivers should be aware of the potential harm to patients in dementia care and should be sensitive to their own bias and assumptions.
The data used in this study are based on previously collected audio data recorded in Japanese dementia patient examination rooms from January to June 2016 by Verilogue Inc. and provided to the author in an anonymized form. Verilogue adheres to a strict privacy and data security policy in accordance with CASRO's Code of Standards and Ethics for Survey Research. This policy can be found on the Verilogue website (http://verilogue.com/privacy).
Written informed consent was obtained from all participants prior to recording. Thus, an ethics approval was not required for this study according to applicable institutional and national guidelines and regulations.
The author confirms being the sole contributor of this work and has approved it for publication.
This work was supported by JSPS KAKENHI Grant Number JP16KT0010.
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Bakhtin, M. (1986). “The problem of speech genres,” in Speech Genres and Other Late Essays, eds C. Emerson and M. Holquist, M (Austin: University of Texas Press), 60–102.
Clark, H. H., and Gerrig, R. J. (1990). Quotations as demonstrations. Language 66, 764–805. doi: 10.2307/414729
Daneš, F. (1974). “Functional sentence perspective and the organization of the text,” in Papers on Functional Sentence Perspective, ed F. Daneš (Prague: Academia, The Hague and Paris: Mouton), 106–128. doi: 10.1515/9783111676524
Du Bois, J. W. (2007). “The stance triangle.” in Stancetaking in Discourse: Subjectivity, Evaluation, Interaction, ed R. Englebretson (Amsterdam: John Benjamins), 139–182. doi: 10.1075/pbns.164.07du
Englebretson, R. (2007). Stancetaking in Discourse: Subjectivity, Evaluation, Interaction. Pragmatics and Beyond New Series, 164. Amsterdam: John Benjamins. doi: 10.1075/pbns.164
Feil, N. (1993). The Validation Breakthrough: Simple Techniques for Communicating with People with “Alzheimer's-type Dementia.” Baltimore: Health Professions Press; Japanese translation published by arrangement with Health Professions Press, Tusui Shobou.
Gauthier, S., Reisberg, B., Zaudig, M., Petersen, R. C., Ritchie, K., Broich, K., et al. (2006). Mild cognitive impairment. Lancet 367, 1262–1270. doi: 10.1016/S0140-6736(06)68542-5
Grice, P. H. (1975). “Logic and Conversation.” in Syntax and Semantics, eds P. Cole and J. Morgan (New York, NY: Academic Press), 183–198.
Husserl, E. (1973). “Cartesianiscshe Meditationen und Pariser Vorträge,” in Cartesian Meditations and the Paris Lectures, ed S. Strasser (Hague: Martinus Nijhoff).
Magai, C., Coshen, C. I., and Gomberg, D. (2002). Impact of training dementia caregivers in sensitivity to nonverbal emotion signals. Int. Psycho. 14, 25–38. doi: 10.1017/S1041610202008256
Matsuda, T. (1984). Phänomenologie der Intersubjektivitat bei Husserl. Jahrb. Philosop. Tet. Ronso 11, 43–54.
Maynard, S. (1997). Danwa bunseki no kanosei: Riron, hoho, Nihongo no hyogensei. (Discourse Analysis: Theory, Method and Japanese Expressivity.) (Japanese Edition). Tokyo: Kuroshio Shuppan.
Ochs, E. (2002). “Becoming a speaker of culture.” in Language Acquisition and Language Socialization: Ecological Perspectives, ed C. Kramsch (New York, NY: Continuum), 99–120.
Ohso, M. (2007). Verbs and adjectives of emotion in Japanese. Studies in Language and Culture. Nagoya Univ. Grad. School Lang. Cult. 22, 21–30. doi: 10.18999/stulc.22.2.21
Searle, J. R. (1975). “Indirect speech acts.” in Syntax and Semantics Vol. 3: Speech Acts, eds P. Cole and J. Morgan (New York, NY: Academic Press), 168–182. doi: 10.1163/9789004368811_004
Sinclair, J. M., and Coulthard, R. M. (1975). Towards an Analysis of Discourse: The English Used by Teachers and Pupils. London: Oxford University Press.
Sotozaki, Y. (2006). Restriction on personal pronoun of Japanese subject: Japanese main text phenomenon and syntactic structure. Scient. Approach. Lang. 5, 149–160.
Sugimura, Y. (2007). Re-Categorization of Japanese Psychological Verb With Collocation With Compound Verbs. Studies in Language and Culture. Nagoya University Graduate School of Languages and Cultures. Available online at: https://www.lang.nagoya-u.ac.jp/~sugimura/achivement/pdf/symposium/017.pdf
Tannen, D. (1986). “Introducing constructed dialogue in Greek and American conversational and literary narrative.” in Direct and Indirect Speech, ed F. Coulmas (Berlin: Mouton de Gruyter), 311–332. doi: 10.1515/9783110871968.311
Tannen, D. (2006). Intertextuality in Interaction: Reframing Family Arguments in Public and Private. Text Talk 26, 597–617. doi: 10.1515/TEXT.2006.024
Van Wheert, J. C. M., Dulmen, A. M., and Bensing, J. M. (2008). “What factors affect caregiver communication in psychogeriatric care?” in Alzheimer's Disease: New Research, ed A. M. Visser (New York, NY: Nova Science Publishers), 87–117.
Keywords: dementia discourse, validation, invalidation, subjectivity, intersubjectivity, orientation, alignment
Citation: Amino K (2020) Validation, Invalidation, and Negative Speech Acts in Dementia Care Discourse. Front. Commun. 5:20. doi: 10.3389/fcomm.2020.00020
Received: 09 January 2019; Accepted: 13 March 2020;
Published: 22 April 2020.
Edited by:
Iccha Basnyat, James Madison University, United StatesReviewed by:
Vinita Agarwal, Salisbury University, United StatesCopyright © 2020 Amino. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kaoru Amino, YW1pbm8ua2FvcnUuNTQ0QG0ua3l1c2h1LXUuYWMuanA=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.