
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Commun. , 13 December 2019
Sec. Health Communication
Volume 4 - 2019 | https://doi.org/10.3389/fcomm.2019.00074
Background: Although the vaccination against influenza has been found to be an impactful and cost-effective protection against the disease, coverage is incomplete. This draws attention to the factors of people's flu vaccination decisions. The article contributes to understanding the effect of social factors on vaccination behavior. Social factors comprise the ways people may be affected by their peers and the mass media or by healthcare providers and health institutions.
Method: Samples of some 200 senior citizens were interviewed by write-in questionnaire in Taiwan, South Korea and the Swiss canton Ticino.
Results: Encouragement by the family physician and a combination of the frequency of contact with vaccination subjects in interpersonal and traditional mass communication and perceived concern with vaccination there increased vaccination rates in the two Asian countries, and model behavior and experience strongly affected vaccination in South Korea, all in bivariate analyses. Multivariate regression in Taiwan and Korea loses the impact of mass media. Perceived concern in sources showed complete mediation by frequency of interpersonal communication in Taiwan and partial mediation in Korea.
Conclusion: There is indeed a relationship between social factors and individual vaccination behavior, which, however, is far from being pervasive. There's hardly any result with direct relevance for the hypotheses that shows up in all three countries, and a meaningful and clear pattern in the differences between the Swiss sample on the one hand and the two Asian countries emerges.
Health protection messages reach consumers from health authorities, from their physicians and their peers, and via communication media. They refer to lifestyle matters such as a healthy diet and sufficient physical activity (Edelman et al., 2018), and also to vaccination.
Our study is concerned with the recommendation to receive vaccination against influenza annually. This recommendation is typically issued to elderly persons and persons at risk, e.g., health care staff (Costantino and Vitale, 2016). Although the vaccination against influenza has been found to be an impactful and cost-effective protection against the disease (Jefferson et al., 2005; Maciosek et al., 2006; Restivo et al., 2018), coverage is incomplete. This draws attention to the factors of people's flu vaccination decisions (Schmid et al., 2017) and the communication channels they use for coming to a decision. Traditional channels can be sorted along a continuum of how secure consumers can be to find expertise. Interpersonal communication with one's friends and family would rank lowest, followed by traditional mass media, where you find highly competent experts and much less competent others. Health authorities and physicians will be at the top of the continuum. The age of digital communication has added the Internet and its appliances to the available channels. Its position on the expertise continuum is 2-fold: information content on the Internet would rank close to traditional mass media, and social media content close to interpersonal communication (Naheed et al., 2018). The relationships of interest are (1) which channels communicate pro- and anti-vaccination information, (2) how intensively are they used by people, and (3) how are these use and contact patterns correlated with vaccination behavior.
Cognitive factors figuring in risk calculation (Galvani et al., 2007; Xia and Liu, 2013; Commodari, 2017; Ling et al., 2018) are well established predictors of vaccination behavior [e.g., for the swine flu pandemic of 2009: (Eastwood et al., 2010; Liao et al., 2011; Myers and Goodwin, 2011); for different vaccinations at once: (Streefland, 2001; Francois et al., 2005); for influenza: (Chapman and Coups, 1999, 2006), and for immunizing Taiwanese children against influenza: (Chen et al., 2015)]. A recent systematic review pertaining to all of Asia singled out safety concerns and concerns about efficacy of the flu vaccination as important predictors (Sheldenkar et al., 2019), but concentrating on them misses an important point. Medical lay persons cannot be expected to undertake a comprehensive and well-founded risk calculation based on established evidence about the efficacy and risks of vaccination. Even registered nurses were found to enter misconceptions in their own decision-making about whether to get vaccinated against the flu or not (Ofstead et al., 2008; Hollmeyer et al., 2009). Rather than doing risk calculation by themselves, people may listen to the information and opinions of others, which may or may not be based on their risk and benefit calculations.
A study based on group interviews found that people do not follow blindly the imminent advice present in media presentations of the MMR vaccination (Tabacchi et al., 2017), but are turning to these media for information. They are willing to accept the recommendations given by their peers, mainly for reinforcing their own views (Ditsungnoen et al., 2016), and they prefer getting personal advice issued by their physicians (Petts and Niemeyer, 2004; Tabacchi et al., 2016).
Another factor is the advice people receive from their physician about the annual flu vaccination. Literature has called upon physicians to advise health care customers to get vaccinated against the flu (Zimmerman et al., 2004), but in all likelihood, this will not shift flu vaccination coverage to higher levels. Providers can only advise when patients seek consultation during the period when the influenza vaccination is to be applied, or they might not care or forget to mention the flu shot. This leaves room for processes of communication from less qualified sources.
A review study covering research published between 1996 and 2005 found that, among citizens aged 65 or older, influenza vaccination was more frequent in men than women, in married persons compared to single or widowed, and increased with education and age up to a point. As to social influences, vaccination behavior depended on a person's experience and was affected by professional advice, actually from the nurses more than from the GPs (Ward and Draper, 2008).
That people talk to their peers, friends and relatives about influenza vaccination is not very likely to cause problems as people are not likely to mistake their peers for medical authority. That might be different for media messages on vaccination that will reach the health care customer by any of the classical mass media or by the Internet. Studies on communication effects on vaccination decisions, and from there onto infections have employed simulation models (Tchuenche et al., 2011). Other work uses media content surveillance instruments to provide warning of an increase in vaccination hesitancy or resistance (Larson et al., 2013). Web 2.0 applications are considered a device to broaden vaccination coverage by some, and as a channel that spreads skepticism by others (Betsch et al., 2012; Odone et al., 2015).
The influenza vaccination is a special case for studying communication influences. First it is required to be repeated annually, which makes it a somewhat everyday health issue to be decided on, whereas most other vaccinations protect a person for many a year. Secondly, it is among the vaccinations most talked about. Thirdly it has a certain potential to be misjudged because the condition of influenza might be mistaken for the common cold (Chiu, 2018), leaving people wondering why someone caught a cold in spite of having been vaccinated. Given the easy mixing up the two, there might also be a dissonance between the alleged harmlessness of the condition and the expense for protection against the disease. On the other hand, as an earlier survey of the adult South Korean population shows, the hope of also preventing a cold by receiving the influenza vaccination can be a motive for the vaccination (Kee et al., 2007).
The general assumption of this research is that patients will be more likely to get themselves vaccinated against influenza if they receive messages supportive of vaccination from their physicians, their peers or the media. In fact, Lee and Kim (2015) have shown, for South Korea, that the use of different channels of information about vaccination messages was linked with different vaccination behavior. Among U.S. adults, frequent users of digital social media were more likely to be vaccinated against the flu than light users (Naheed et al., 2018). For another case, the 2015 MERS outbreak, a association between use if mass media and protective measure emerged among residents of Hong Kong (Ludolph et al., 2018). Vaccination advice might be explicitly communicated to people, but can also originate from observing model behavior and experiencing an infection with influenza or vaccination effects in oneself or significant others. Observations and experience have a potential to implicitly communicate the necessity or futility and the benefits or risks associated with vaccination. Vaccination-supportive information includes statements on the seriousness and fast diffusion of influenza or other concerns about the dangers associated with it, and also statements on the efficacy or harmlessness of the vaccine. Beliefs about risks such as these are the major concern of research into the antecedents of vaccination decision (Weinstein et al., 2007).
Our general assumption is that vaccination skepticism is fostered by persons without medical training rather than by experts. The stance of vaccination messages is therefore hypothesized to be more positive among physicians than in traditional media and in Internet information content, and still more positive there than in peer (interpersonal) communication and social media on the web. We do not aim at grasping the objective content available on these channels, but are rather interested in people's subjective assessments of this content. And as the use of specific digital health communication channels depends on the general use of digital these channels, which is contingent on age, we compare the use of these separately. Consequentially, that separation is also applied to the perceived concern about the flu in the channel. We deduct these hypotheses:
Health care consumers will perceive a higher concern about influenza in traditional mass media than among their peers (H1.1) and on Internet information sites than in social media on the Web (H1.2).
The general assumption is that consumers select those channels that they expect will give them what they want: a distanced view on the flu vaccination. Thus, for the case that H1 is supported, we hypothesize:
Health care consumers will expose themselves more to influenza content in the communication with peers than in traditional mass media (H2.1), and more to influenza content in social media than in information web pages (H2.2).
The product of use and perceived stance can be considered a factor in a consumer's own vaccination decision. The higher the perceived concern about influenza in a channel and the higher the use of this channel, the more will consumers get vaccinated (H3).
The combined stance/use measure can be considered the independent variable in communication effects analysis. To assess the magnitude of such effects, other factors have to be considered along with the communication factors. Among the other factors, there are the sociodemographic variables (Ibuka et al., 2010; Lee, 2015; Commodari, 2017) and the perception of the disease and peer model behavior with regard to vaccination.
Consumers will get themselves vaccinated more frequently if they experienced infection with influenza themselves (H4.1) or among their close friends and family (H4.2) and if a larger share of their friends and family receives their own immunization against influenza (H4.3).
These hypotheses are tested in three different cultures, Taiwan, South Korea, and the Italian-speaking part of Switzerland. This choice, especially of the two Asian countries, was guided by the observation that most research in the area covers North American and European countries. As the arguments above are so general, however, that they are expected to pertain similarly in all three countries, we do not hypothesize specific cultural differences. Doing the same analyses in three countries, however, yields observations on differences between these countries more or less automatically. Therefore, we also pose the research question, are there any cultural differences between Korea, Taiwan and Switzerland with regard to social influences on vaccination decisions?
Small surveys were conducted among elderly citizens in Taiwan, South Korea and the Italian speaking part of Switzerland, almost perfectly coinciding with the Canton of Ticino.
A total of 217 older adults were interviewed in Seoul, Korea. The face-to-face interviews were conducted from January 23 to February 28, 2017 at various locations where the elderly population often congregate to socialize. Three graduate students were trained as interviewers and visited senior centers, community culture centers, and churches. When a person agreed to participate in the survey, the interviewer read the questions and recorded their answers on a paper questionnaire.
Participants in the Chinese convenience sample in this study were over age 65 years of age or older and came from some communities in the Taipei area. A total of 204 older adults were recruited from March to May 2017. The study trained 25 graduate students as interviewers. A questionnaire was distributed for personal interviews, and informed consent was asked of each of the recruited elders.
Swiss respondents were contacted in January and February 2017 in bars or other meeting points frequented by senior citizens. The study was restricted to the canton of Ticino, the Italian-speaking part of Switzerland. To be eligible, participants had to be 65 or older. Persons interested in the survey were handed a paper printout to be filled in. Questionnaires were collected on the premises. Participants were invited to a coffee as a way of saying thank you. The sample comprised 206 participants.
Ethics approval and consent to participate The study was approved by the ethical committees of Fu Jen Catholic University, Taiwan (No. FJU-IRB NO: C105073, Febr 10th, 2017) and of Ewha Womans University, Seoul, South Korea (No. IRB 129–7, Jan 16th 2017). The survey was conducted following the guidelines of the Declaration of Helsinki. Since participation was anonymous and voluntary, consent was implicitly obtained by completing the survey.
The general dependent variable is last season's vaccination behavior, coded as a yes/no/cannot remember answer to the question, “This winter season, did you get vaccinated against the flu?” The Taiwanese and the Korean data included answers to the effect that the respondents “cannot remember.”
Perceived stance of a channel toward influenza vaccination and use of this channel were measured for four channels, traditional mass media, friends and family, the Internet, and online social media. For each of the channels the frequency of use with regard to the subject of vaccination and the perceived concern conveyed by the channels (if the respondent used it at all) were inquired about. For mass media, the questions were formulated as “This winter season, how often have you read, seen or heard anything about the flu in the mass media such as newspapers, TV, and radio?” Frequency of use was measured on 7-digit scales with 1 = “not at all” and 7 = “very often.” Concern was measured by respondents' subjective perception: “On a scale from 1 to 7, where 1 means not concerned at all and 7 means very concerned, what would you say how concerned about the flu are the mass media these days?” The questions about friends and family, the Internet and social media were similar to these.
In addition, respondents were asked whether (if at all) a communication channel encouraged or discouraged the respondent to get vaccinated. The encouragement question included a fifth source, the family physician, and is understood to combine use and perceived stance in one composite measure. The questions were explicitly directed at the experiences the winter before and can therefore only be related to vaccination then, not to likelihood of future vaccination behavior, which was also measured in the same survey. Encouragement was measured by questions covering which channels gave advice in which direction, encouraging or discouraging participation in the flu vaccination. For the answers, a scale was used reaching from 1 = strongly encouraged to 7 = strongly warned against. Respondents were also offered to check that they had not received advice from the source. For group comparisons analyzing both the presence of advice and its direction, scale points 1 to 3 and 5 to 7 were taken together, indicating persons who had received encouragement and discouragement, respectively. For inclusion of this variable in the regression, scales were used that added persons who had not received advice at the midpoint of the scale.
Experience was measured by a single question, “Have you been diagnosed with influenza in the last 2 years?”. Friends' and families' experience was measured by “Has any one in your family been diagnosed in the last 2 years?” Model behavior was asked about in a single question also, running “How do most of your family and friends handle influenza vaccination? Do most get vaccinated or not?”
For technical reasons, the frequency scale was recoded from 1 to 7 to 0 to 6. The indicator for the amount of vaccination-supportive information is the product of the two scales, ranging from 0 to 42. For respondents who indicated they did not use a source for vaccination information the product is 0; in fact they were not asked for perceived concern. Missing cases for frequency of use were excluded (almost exclusively in the South Korea data pertaining to Internet and social media), while missing cases for perceived concern among those who did use the source were replaced by the mode, 5 in case of talking with family and friends, and 4 in case of the other three sources.
For a vivid presentation of the correlation between vaccination behavior and amount of vaccination-supportive information, the 0-42 product scale was grouped into five ordinal categories so that the scale value zero was a separate category and the other four produced groups of approximately equal size in the complete sample. The ordinal scale used these categories and cut-off points:
0 no vaccination-supportive information communicated;
1–4 very little vaccination-supportive information communicated;
5–10 little vaccination-supportive information communicated;
11–20 some vaccination-supportive information communicated;
21–42 highly vaccination-supportive information behavior.
It turned out that too few respondents used the Internet or social media at all to apply these ordinal categories to these two sources. In order to analyze these two sources, the categories used for them were:
0 no motivation communicated (applied to about 2/3 of the samples);
1–10 (very) little vaccination-supportive information communicated;
11–42 some vaccination-supportive information communicated.
Frequency counts will show which communication channels are used, how the users perceive the pro- or anti-vaccination stance, and—combining use and content perception—describe the dosage of pro- and anti-vaccination information respondents were exposed to. Paired sample t-test were computed for testing Hypotheses 1 and 2. Second, the dosage of vaccination information will be related to vaccination behavior. Analysis first employed cross tabulations and later uses bivariate non-parametric correlations and binary logistic regression to determine the relative weight of the various predictors and to gain an assessment of significance. Finally, mediation analysis was performed with vaccination behavior in the last season as the dependent variable, the measure of the intensity of concern perceived in media as independent variable, and the frequency of conversations with friends and family on influenza as the mediator.
Slightly more than 200 persons in each country participated in the survey, 204 from Taiwan, 217 from South Korea, and 206 from the Italian-speaking part of Switzerland. The South Korean sample was split equally between men and women, while in Taiwan female (57%) and in Switzerland male respondents (60%) were over-represented. Secondary or high school was the mode in a question for highest educational degree in all three countries (39% in Taiwan, 41% in South Korea, 77% in Switzerland), but in the two Asian cultures the lowest category of primary school or less was reported more frequently than in Switzerland (23% in Taiwan, 22% in South Korea but only 10% in Switzerland). Similarly, the two Asian samples claimed a university degree more frequently than the respondents from the Swiss sample (38% in South Korea, 20% in Taiwan and only 9% in Switzerland). In Taiwan, 19% indicated college or apprenticeship as highest education, a category that was not used in the other two countries. At 76 years of age on average (SD = 6.9), the Swiss respondents were considerably older than their South Korean and Taiwanese counterparts (both 71 years of age on average, SD = 5.9 in Taiwan and SD = 5.1 in South Korea). Health status, in contrast, was rather similar: 3.2 (SD = 0.79) on average in Taiwan, 3.4 (SD = 1.02) in South Korea and 3.1 (SD = 0.76) in Switzerland, on a worded 5-digit scale.
South Korean participants were the most eager vaccinators, 60% of them reported they had been immunized in the most recent season, while only 45% of the Swiss and 42% of the Taiwanese participants reported the same. More than half of the Swiss (55%) and the Taiwanese (51%) respondents indicated they had not been immunized, while only 28% of the South Koreans said that. Twelve percent of the South Korean and 7% of the Taiwanese could not remember. A χ2-test finds these overall differences highly significant (χ2 = 52.939, df = 4, p < 0.001). The higher level of vaccination coverage in South Korea may have to do with the fact that influenza vaccination in this country is free for everybody over 65 years of age, whereas in Switzerland persons who have no special risk for complications or infection and have not reached the franchise of their health insurance and work for an employer who does not cover the cost have to pay for the vaccination themselves. In Taiwan, adults over 50 and adolescents in children under 18 as well as a number of high-risk groups receive a subsidy for the vaccination, but have to cover the rest themselves.
By far most respondents received communication about influenza vaccination from the traditional mass media, 83% of the South Koreans, 88% of the Swiss, and 96% of the Taiwanese. When the intensity of contact is measured by the scale average (1 = no contact to 7 = very often), Swiss seniors emerge as the group with most frequent contacts (5.2 vs. 4.7 in Taiwan and 3.7 in South Korea). Large majorities of respondents also reported to have talked with friends and family about influenza vaccination: 88% in Taiwan, 85% in South Korea and 62% in Switzerland. In terms of averages, South Koreans report the highest level of contacts (4.0), followed by the Taiwanese (3.7), and the Swiss came in last (3.3). The situation is fundamentally different for contacts on the Internet and social media. Only very few of the Swiss respondents reported to have had contact with the Internet (4%) or social media (2%) about influenza vaccination, while among the Taiwanese 49% had had contact with the Internet and 60% with social media, and among the South Koreans 47% with the Internet and 39% with social media. This is also reflected in the scale averages which were practically identical with the starting point of the scale (1.1 for both Internet and social media) in Switzerland, while the Taiwanese sample reached 2.3, respectively, 2.7 and the South Koreans 2.3, respectively, 2.0. The data reveal a clearly different pattern for the Swiss respondents. Compared to the other two countries they had contact with traditional media more often but talked to friends and family less often, and more or less ignored the potential of the Internet (that is websites) and electronic social media as an information source for vaccination information. That might have to do with the fact that the Swiss sample was considerably older than the samples from the two Asian countries. Hypothesis 2.1 was confirmed in South Korea (t = −2.300, df = 216, p < 0.02), while the other two countries showed highly significant differences against the direction hypothesized (Taiwan t = 7.927, df = 203, p < 0.001, Switzerland (t = 10.612 =, df = 205, p < 0.001). Hypothesis 2.2 was confirmed for Taiwan (t = −3.619, df = 203, p < 0.001), and in South Korea the differences were against the direction of the hypothesis (t = 3.010, df = 174, p < 0.01). It is not true that the respondents prefer using peer channels more than institutional, more expert ones.
The respondents from Taiwan perceived a comparable amount of concern in all four information sources: 4.6 in traditional media, 4.4 for friends and family, 4.1 for the Internet 4.0 for social media. The South Korean respondents reached averages 0.4 points lower for traditional media, the Internet and social media and 0.4 points higher for friends and family (4.2, 4.8, 3.8, and 3.7 in the same order). Again, Switzerland stands out. The Swiss respondents perceived much less concern in the traditional media (2.2) and among friends and family (2.3), while the very few respondents who had had contact with the Internet and social media roughly saw them as concerned as their Taiwanese and Korean counterparts.
Hypothesis 1.1 was confirmed in Taiwan (t = 2.238, df = 176, p < 0.05), but a highly significant difference against expectations emerged in the South Korean data (t = −4.946, df = 165, p < 0.001). Both Swiss comparisons and the tests of Hypothesis 1.2 in all three countries failed to show significant differences. As with use, the respondents from the three countries did not perceive a higher concern over influenza in the institutional as compared to the peer communication channels. Figure 1 illustrates the means that were analyzed above.
If Figure 1 is looked at with some more abstraction, and in terms of aggregation of data on the level of country, it appears that the more often a channel is used, the less concern about influenza the Swiss perceive there. And less concern can be expected to be related with high vaccination skepticism. It is indeed the more skeptical channels that are looked at more often for vaccination information. In contrast, the slopes of the imaginary trendlines for Taiwan and South Korea move up, indicating that the more frequently used communication channels convey more concern over the flu and thus run against vaccination skepticism. It thus can be stated that, paradoxically, the basic assumption, from which the hypotheses were deduced, is not necessarily correct for the two Asian countries, although some of the hypotheses are supported there; for Switzerland, in contrast, the assumption appears to apply, but none of the hypotheses derived from it was supported.
Reception of vaccination-supportive communication content was hypothesized, as the major independent variable, to be positively related with decisions in favor of influenza vaccination. The level of reception, as a product term of frequency of use and perceived concern, can be described by average values on a scale reaching from 0 to 42, which are given in the second column of Table 1. Respondents in the two Asian countries throughout received more vaccination-supportive communication than their Swiss counterparts. Taiwanese respondents received it mostly from traditional media, South Koreans from friends and family. The low dose of vaccination-supportive information in Switzerland is caused by a low perception of concern in traditional media and among friends and family, and a very low frequency of use close to zero of online information sources.
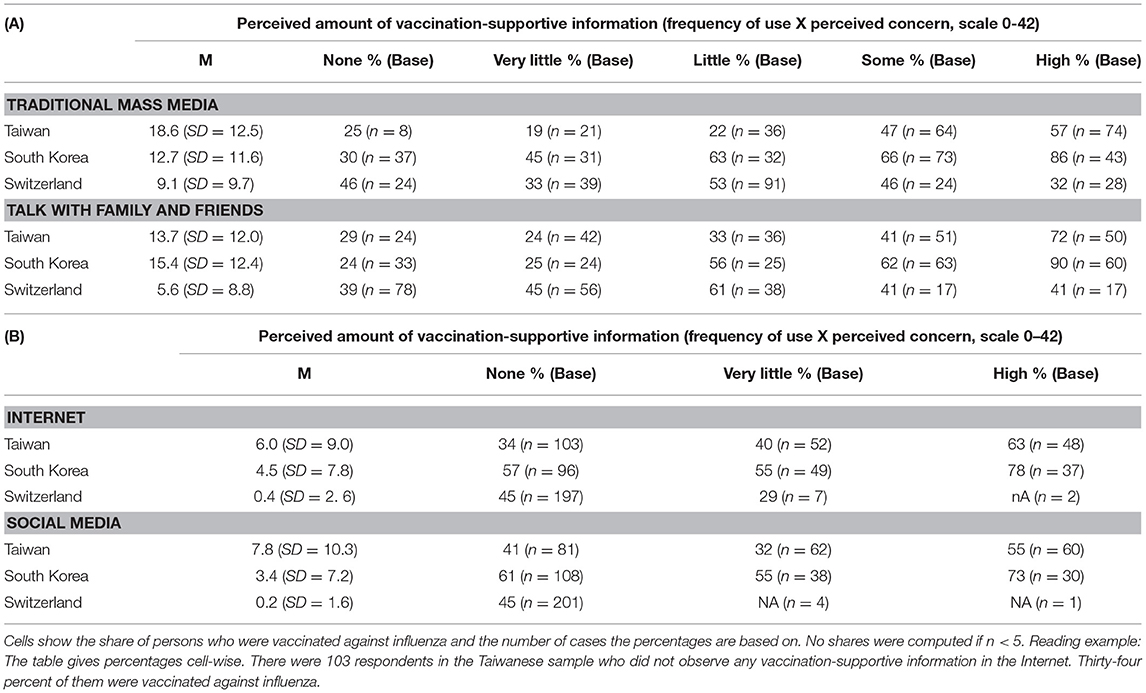
Table 1. Percentage of respondents vaccinated by sources, country, and perceived amount of vaccination-supportive information.
The first testing of Hypothesis 3 was done by comparing the frequency of actual immunization in ordered categories of reception of vaccination-supportive information. Rising shares in the rows in Table 1 are expected as reception increases. The results are very straightforward for the traditional media and for talking with friends and family. The more supportive of vaccination a person's received communication was, the more likely this person is vaccinated. This is very pronounced for Taiwan and South Korea, but completely absent in the Ticino data. For Internet and social media as sources for vaccination information, the relationship is less clear. There is an unsteady increase in vaccination rate as the potentially motivating media contacts grew, again restricted to the two Asian countries. The Ticino respondents in this case have hardly had any contact with vaccination content on the Internet or in social media; nothing can be said about the relationship between communication behavior and vaccination rate for the electronic media as used by the Swiss elderly respondents.
Hypothesis 3 thus receives strong support for the Taiwanese and South Korean samples as far as peer communication and traditional mass media are concerned and weak support for the digital channels. South Korean appear to be more susceptible to the influences, and taking the span of the trends as indicator, friends and family do more for vaccination than mass media. No support was found for Switzerland, again. Table 1 shows the results.
Similar to the analysis above on the influence of combined measures of channel use and perceived stance, the next step looks into the effects of the encouragement measure that is already a combination of use and stance. The elderly citizens in the three countries have different perceptions of what their physician suggested. Almost every second respondent from Ticino (46%), every third from Taiwan (37%) and every fourth in South Korea (26%) had not received advice from the family doctor. South Koreans were comparatively often discouraged (14%), which happened much less often to respondents from Taiwan (5%) and hardly ever to those from Ticino (1%). On the other end, the respondents who indicated their physician encouraged them to take the shot, followed that advice to 62% in Switzerland, 61% in Taiwan and 88% in South Korea. The relative frequent discouraging from vaccination that occurred in South Korea, along with the infrequent passing of advice was balanced out by an extraordinarily high sense of adherence among those who were told otherwise.
Comparing adherence between those who were discouraged and those who were encouraged shows an increase of 17 percentage points (from 44 to 61%) in Taiwan and 46 percentage points (42 to 88%) in South Korea. As only two respondents reported discouragement from the family physician, no meaningful difference can be reported to Ticino. In summary: these results can be interpreted as evidence of a positive effect of doctoral recommendations on influenza vaccination behavior in the two Asian countries.
Among Taiwanese who felt encouraged by the traditional media, the share of those vaccinated was slightly higher than among persons who felt discouraged (60 vs. 44%). Again this same difference was larger in South Korea (85 vs. 54%). Encouragement by friends and family followed the same pattern: a somewhat higher vaccination rate for the encouraged as compared to the discouraged in Taiwan (60 vs. 52%), and much higher in South Korea (89 vs. 39%). Here a value can be computed for the Swiss respondents, at a medium difference (70 vs. 44%). The two remaining agents of encouragement, Internet information and social media, do not follow the pattern. Encouragement by Internet information goes along with higher vaccination rate in Taiwan (72 vs. 46%), but not in South Korea (75 vs. 75%). Encouragement by social media goes along with higher vaccination rate in South Korea (69 vs. 56%), but not in Taiwan (58 vs. 54%; Table 2).
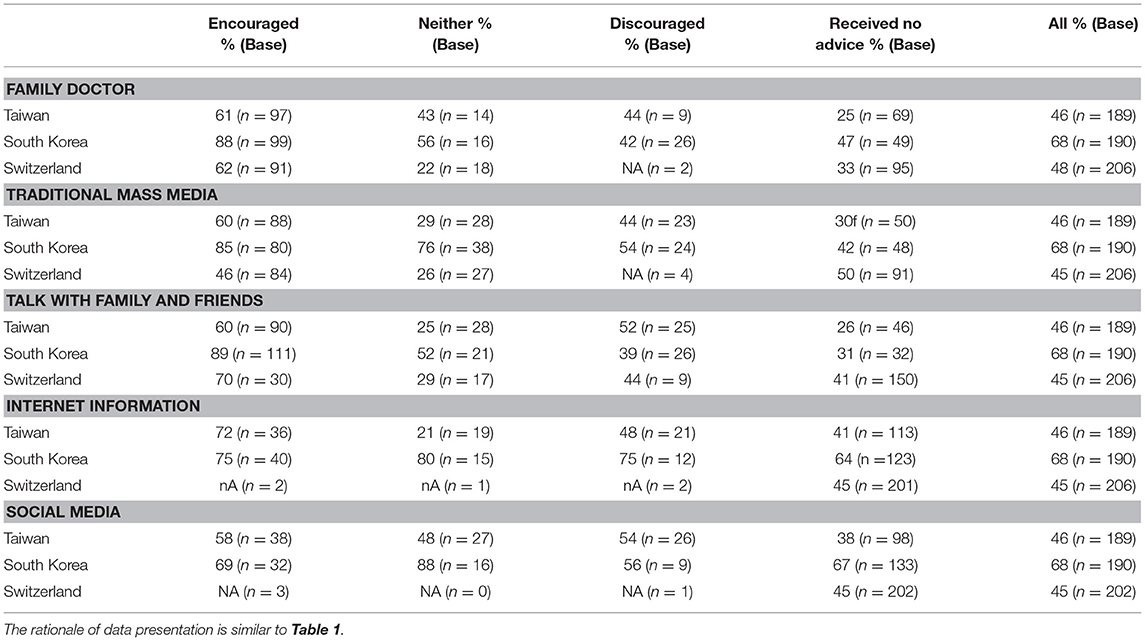
Table 2. Percentage of respondents vaccinated by encouragement and discouragement from different communication channels by country.
No advice, that is no communication about the subject goes along with low vaccination rates in case of the communication with one's doctor more or less in all three countries and from mass media channels in the Asian ones. Receiving no advice often is followed by the lowest vaccination rates.
Receiving ambiguous advice is sometimes followed by vaccination rates similar to the level among persons who feel discouraged by a channel: family doctor in Taiwan, Internet information in South Korea. In some cases, ambiguous advice leads to more vaccination than discouragement: family doctor, mass media, friends and family, and social media in South Korea. Interestingly, there are quite a few cases where discouragement leads to more vaccinations than ambiguous advice: mass media, family and friends, and Internet information in Taiwan, family and friends in Switzerland.
The analyses above serve the purpose of making the link between the vaccination last season and its predictor variables vivid. In order to account for possible inter-correlation between the predictors, binary logistic regressions were computed, treating respondents who could not remember their vaccination decision last season as missing cases and using the scale values for reception of vaccination-supportive information (0–42) as independent variables. Gender, age and subjective health status were entered as controls in a first block, physician advice as a second, experience and model behavior as the third and finally concluding with vaccination-supportive information as a fourth block.
The regression models explain a fair amount of the variance in vaccination behavior, the highest in South Korea (58%) and the lowest in Switzerland (22%; in Taiwan 45%; Nagelkerke's R2). The three countries share a high contribution of physician advice to vaccination behavior. They also share a lacking influence of recent experience of being diagnosed with influenza oneself, or having a family member diagnosed. The model behavior of one's family with regard to vaccination, however, affects respondents' own vaccination behavior in the two Asian countries, but not in Switzerland. The communication of vaccination-supportive information impacts vaccination behavior only when it comes from friends and family, and only in the two Asian countries. South Korean respondents also reported an influence of Internet-communicated information (Table 3). This leads to the conclusion that there is absolutely no support for Hypothesis 3 as it pertains to traditional mass media and digital social media, but some support from the two Asian countries (respectively one of them; South Korea, almost at p = 0.052) as it pertains to peer communication and Internet information sites.
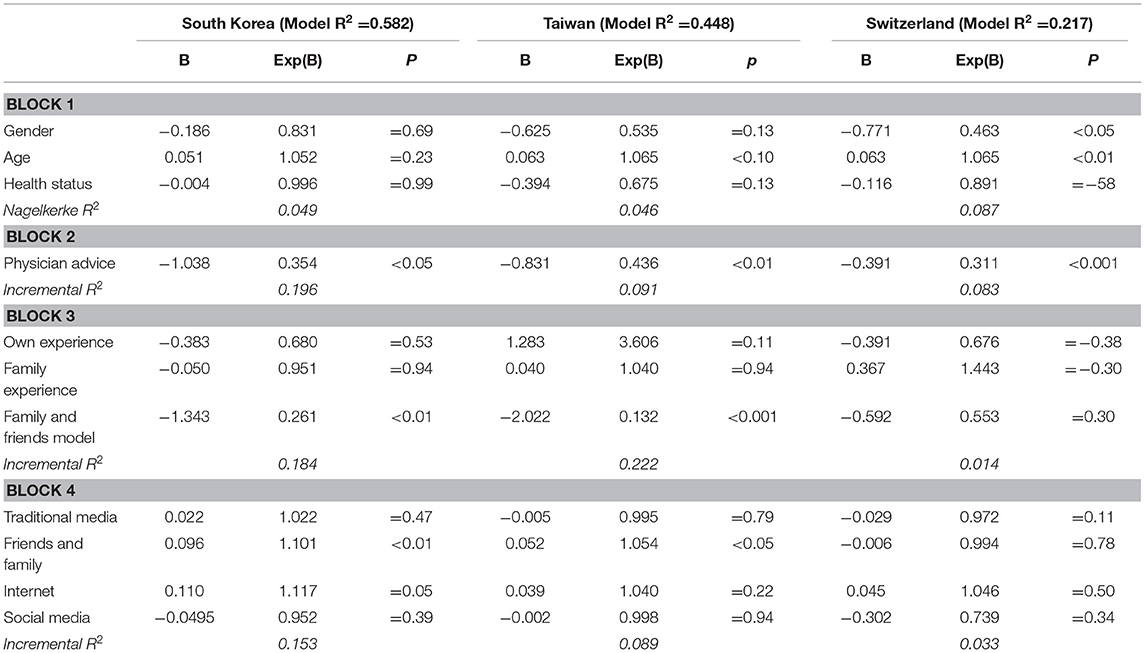
Table 3. Prediction of vaccination behavior by physician advice, experience, and reception of vaccination-supportive information from different sources (binary logistic regression).
Cross tabulations showed that a diagnosis of influenza in a participant in the last 2 years against expectations decreased vaccination in the most recent season by 8 percentage points from 43 to 35% (χ2 = 0.468, df = 2, ns) in Taiwan, increased it by 31 percentage points from 52 to 83% (χ2 = 16.763, df = 2, p < 0.001) in South Korea and by 5 percentage points from 44 to 49% in Switzerland (χ2 = 0.199, df = 1, ns). Having a family member being diagnosed with influenza in the last 2 years decreased vaccination in the most recent season by 5 percentage points from 43 to 38% (χ2 = 0.413, df = 2, ns) in Taiwan, increased it by 39 percentage points the from 45 to 84% (χ2 = 34.279, df = 2, p < 0.001) in South Korea and decreased it by 8 percentage points from 47 to 39% in Switzerland (χ2 = 1.361, df = 1, ns). Having one's own family being vaccinated against influenza increased vaccination rate in the most recent season by 38 percentage points from 28 to 66% (χ2 = 34.159, df = 2, p < 0.001) in Taiwan, by 45 percentage points from 31 to 76% (χ2 = 40.801, df = 2, p < 0.05) in South Korea, and by 15 percentage points from 43 to 58% in Switzerland (χ2 = 1.547, df = 1, ns). Thus, Hypothesis 4.2 is clearly confirmed by the results of bivariate analysis from South Korea and not supported by the results from the other two countries. Hypothesis 4.1 is also clearly supported by South Korea and not supported by Taiwan and Switzerland. In fact, the results from these two countries run against expectations as do the Taiwanese results with regard to Hypothesis 2, although none of these adverse results reached significance. Hypothesis 4.3, in deviation from the pattern, is confirmed by the results from Taiwan, South Korea and partly, though not reaching significance, from Switzerland also. Thus, both model behavior and experience strongly affect vaccination behavior in South Korea, while in Taiwan only model behavior has that effect while experience does not affect vaccination behavior, or, if anything, does so in the unexpected direction. The lack of impact of experience is confirmed in the regression analysis for all three countries, as is the influence of the perception of model behavior in the two Asian countries. The Swiss data do not show any significant relationship of vaccination behavior with the three indicator questions. One can conclude that the implicit messages contained in the experiences and the model behavior of one's family does not impact vaccination behavior in this country.
The two bivariate results from Taiwan that ran against expectations moreover showed low case numbers in the hypothesized vaccination-supportive condition (n = 17 for being diagnosed oneself, n = 37 for having a family member diagnosed). This of course affects the significance tests reported above and means that it is rather likely that these two results are the product of chance. The result from Taiwan that was in line with the hypotheses (family model behavior; n = 77) had many more cases in the vaccination-supportive group. In contrast, the Swiss results that ran contrary to expectations had the highest number of cases in that condition (n = 72, compared to n = 35 and n = 19 in the other two analyses). In other words: the adverse results for Taiwan are possibly the product of low case numbers, while this is not so in Switzerland.
A possible interaction between media and interpersonal communication is suggested by three observations: (1) the fact that, at least in the two Asian countries, vaccination-supportive information is received from friends and family, (2) that friends and family act as models seeking vaccination themselves, and (3) that vaccination-supportive information in mass media channels remained without effects. That shall be investigated more deeply. For that purpose, the perception of concern in media channels respondents used for acquiring vaccination information was merged in a single scale (Cronbach's alpha = 0.68), comprising traditional mass media, Internet information and social media. An ANOVA showed there were highly significant differences between the three countries in that measure (F = 95.448, df = 2, 558, p < 0.001), which is due to the difference between Switzerland and the two Asian countries, as post-hoc Scheffe tests revealed. The scale averages were 4.2 for Taiwan, 3.9 for South Korea and 2.2 for Switzerland.
The models yielded for the three countries are different. The total effect of perceived concern in media channels is outstanding in South Korea, fairly large in Taiwan, and not existent in Switzerland. The Taiwanese model shows complete mediation in that the direct effect of concern in the media drops to an insignificant level. In contrast, mediation in the South Korean model is partial only; in fact the direct effect is still stronger than the indirect one. For Switzerland, there is neither a direct nor an indirect effect; the only significant path runs from the mediator variable, frequency of talk, to the outcome, receiving the influenza vaccination. Table 4 lists the relevant coefficients for three countries.
The study yields rather diverse results, which at a first glance, are not so easily accommodated. The most noteworthy finding in general is that, despite such claims in the literature, communication channels are not the predominate source for vaccination skepticism. Secondly, the conceptual considerations at the beginning of this article play different roles in different countries. And the third general finding is that the factors considered in this study together contribute quite a lot to vaccination decisions, in some cases mediated by frequency of conversations. The ensuing discussion of the results will look at this in a more detailed way. With regard to the use of more institutional and peer communication channels, the perception of concern over influenza in these channels, as well as model behavior in one's social environment the three countries yield very different results. This pertains to the level of the independent variables as well as to the magnitude of their possible effect on vaccination behavior. The evidence that supports the hypotheses is therefore far from being pervasive. There's hardly any result with direct relevance for the hypotheses that shows up in all three countries.
Beginning with vaccination coverage itself, the higher level in South Korea may have to do with the fact that influenza vaccination in this country is free for everybody over 65 years of age, whereas in Switzerland persons have to pay for the vaccination themselves unless they have a special risk for complications or infection, have reached the franchise of their health insurance or work for an employer who covers the cost. In Taiwan, adults over 50 and adolescents in children under 18 as well as a number of high-risk groups receive a subsidy for the vaccination, but have to cover the rest themselves.
The diversity of the results between countries does not appear to be at random. Rather, there seems to be a meaningful and clear pattern in the differences between the Swiss sample on the one hand and the other two countries on the other, and also some systematic difference between the other two.
Swiss respondents, in comparison with the two Asian cultures, use the traditional media more for vaccination information than their Asian counterparts, but they talk less with friends and family about vaccination. They more or less completely ignore the Internet and the social media as sources of vaccination information. They perceived less concern about influenza in the traditional media and among their friends and family. The amount of vaccination-supportive information they encounter is lower than in the two Asian countries, due to lower perceived concern in the traditional mass media and among friends and family and to a much lower use of digital media. On the individual level of analysis there's no link among the Swiss respondents between the amount of vaccination-supportive information they receive and the likelihood that they get vaccinated against the influenza. This also means that none of the hypotheses receive any substantial support from the Swiss survey.
The respondents from the two Asian cultures use for vaccination information channels they perceive as supporting vaccination. The more they do both (using the channels and perceiving them as supportive of vaccination), the more they reported to have received the flu shot last season. Possible gaps in coverage of the vaccine cannot be explained by communication failure. In Switzerland, in contrast, vaccine coverage is unrelated to the use of vaccination-supportive communication channels.
Swiss citizens thus present themselves as quite independent of social influences when it comes to a personal medical decision, and they themselves as well as their possible sources for vaccination information appeared to be quite calm and unexcited. Their independence, in comparison with the two East Asian cultures studied here, is reminiscent of the polarity between individualistic culture as found in Western European nations and collectivist culture considered typical of Eastern Asia (Hofstede, 1980), the former being concerned with how much an individual profits from collectives he or she belongs to, and the latter focusing on how well an individual fits in (e.g., Oyserman and Lee, 2008).
It is as if the Swiss respondents were immune against influences of communication with regard to vaccination. The lower frequency of communication with peers, the very low level of use of the Internet and the perception of media and peers as being relatively unconcerned about influenza all might contribute to the relative invulnerability. It is unlikely that communication content is to blame because the immunity is observed in both the traditional mass media and the personal communication with friends and family. Still, content analysis of media depictions of influenza and the vaccination against influenza are needed to clarify the potential contribution of media content to the vaccination decision as well as to test whether the mass media in the country are indeed as unconcerned (in relative terms) as they see them.
The importance of culture for communication about vaccination has recently been highlighted by a study that finds people in two holistic Asian cultures (South Korea and Hong Kong) put more trust in experienced-based communication content, and use this type of content more, while respondents in an analytic Western culture (the U.S) trusted expertise-based content more, and also use this type of content more (Song et al., 2016). Intensity of use and trust in content can be considered conditions of communication effects. Therefore, this study is of direct relevance to our findings on relationships between perceived stance of communication content in different communication channels and recipients' position or behavior on it, more precisely: of direct relevance to the differences between the two Asian and the European culture in our study. In particular the lack of a relationship between user perception of the stance to vaccination on one side and respondents' position on the other for talks with friends and family and for the social media on the Internet, as well as the model behavior of one's family with regard to vaccination in Switzerland are closely connected to these findings, in so much as these communication channels focus on experience-based more than expertise-based content.
The mediation model presented in this analysis is very but not completely similar to a model developed and tested for the case of the 2013 threat of a MERS pandemic in Hong Kong. The Hong Kong study conceptualized media use as the independent variable and precautions taken as the dependent one, and frequency of personal communication as well as perception of concern in one's social environment as possible mediators. Fitting the data to the model yielded three indirect paths: the first from media use via interpersonal communication to precautions taken, the second from media use via perceived concern in the media and among one's friends to precautions, and finally from media use via interpersonal communication via perceived concern to precautions. The adapted model in the present study replaced the dependent variable of precautions by vaccination behavior, completely deleted the independent variable of media use and replaced it by perceived concern in different communication channels, effectively reversing the causal paths from interpersonal communication to concern from the Hong Kong study into one from concern to frequency of talks in the present vaccination study. The model describes, as shown, the Taiwan data very well, the South Korean data partially, and the Swiss data not at all.
As far as Korea is concerned, the finding relates to a general feature of its culture: Social emulation and bandwagon effects are very strong in Korea, reflecting collectivistic culture. Such cultural differences need to be further studied.
Consistency as a potential expression of culture was also observed for the differences between Taiwan and South Korea. The strongest support for hypotheses came from the South Korean sample, meaning that the contribution of social factors to making vaccination decisions is strongest in this country. The South Koreans also are the most eager vaccinators this study. Neither of the two Asian nations appeared to be much impressed by experience, either their own or their family's, when making a vaccination decision, but observing model behavior in their family with regard to vaccination may have led to imitation; at least there's a relationship between model behavior and their own decision. In addition, vaccination-supportive information the elderly in South Korea receive from talking to friends and family appears to be of special importance. It is the only source that South Koreans perceive as more concerned than their Taiwanese counterparts do, and the correlation with vaccination decision behavior is the strongest. Conversations with friends and family, moreover, is the way that some of the concern perceived in media (traditional and digital) may reach people eligible for the influenza vaccination. Perceived concern in the media, so our models suggest, makes people in South Korea and Taiwan talk to friends and family, and this talking increases the likelihood of seeking the vaccination. The Swiss do nothing like this. They perceive the media as much less concerned about influenza, and even when they do, this does not make them seek the advice of their friends and family. The observation that the Taiwanese tend to stay away from medical practices for vaccination purposes when the stance of communication media on vaccination is ambiguous may be linked with their inclination to converse with their family and friends when concern over influenza gets more discernible.
Abstracting from cultural differences, the evidence provided in this study suggests that among elderly citizens in the three countries under study the major sources for vaccination information are traditional mass media and friends and family. Use and perception of concern in these sources combined were related to vaccination behavior in the two Asian countries at least in bivariate analysis. In addition, observing model behavior among family and friends appears to be more consequential than recent experience with influenza. Or taken together, the findings underscore the importance of interpersonal communication as a source for vaccination information that counts. New digital media, in contrast, play a minor part only. That may have to do with the fact that all sampled persons were in retirement age.
Generally, much fewer respondents report to feel discouraged than encouraged by the vaccination information they receive. Especially in Switzerland, discouragement does not appear to occur at all. South Korean respondents appear to be much more susceptible to encouragement than the Taiwanese, no matter whether it comes from the family doctor, mass media, friends, and family or social media. An earlier survey of the adult South Korean population, already identifies encouragement as one of the factors that might increase influenza vaccination coverage (Hollmeyer et al., 2009). In Taiwan, ambiguous advice creates low vaccination rates. No communication about vaccination can be a sign of disinterest and consequently result in low vaccination rates.
Can the blame for low flu vaccination coverage be put on communication? Not in general terms that would pertain to all three countries. The question “peers or pundits,” shorthand for the inquiry of who has the stronger (detrimental) effect on vaccination behavior, friends and family or communication institutions, may have “physician” as a new answer, and it may have to be answered differently in different countries. And finally the “or” in the question may have to be replaced by “and” as the interaction of both forces turns out to be efficacious. It does not appear that the information and advice given with regard to vaccination is ineptly communicated, or that there are actors who systematically discredit the recommendation for vaccination against the flu. Neither is there a tendency in health care consumers to actively seek anti-vaccination communication.
Among the major limitations of this study is the quality of sampling. Convenience samples were drawn in all three countries, and the procedures and targets varied between the three. Therefore, no claim of representativeness can be made. But the major conclusions we make do not require a representative sample of citizens at age 65+. Sampling the elderly is a difficult problem in survey research in general due to difficulties in reaching them, especially if they are institutionalized instead of living in communities. Cognitive decline and high refusal are two more obstacles. In addition, some of our interpretations on cultural differences and the fact that hypotheses are better confirmed in countries where their basis is challenged by our data makes us optimistic that the samples are not too far off the mark.
The datasets generated for this study are available on request to the corresponding author.
The studies involving human participants were reviewed and approved by Ethical committees of Fu Jen Catholic University, Taiwan (No. FJU-IRB NO: C105073, Febr 10th, 2017) and of Ewha Womans University, Seoul, South Korea (No. IRB 129–7, Jan 16th 2017). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
PS, SA, and Y-CW: conceptualization. PS and SA: formal analysis. PS: writing—original draft preparation. SA, Y-CW, and F-LC: writing—review and editing. All authors: methodology.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Betsch, C., Brewer, N. T., Brocard, P., Davies, P., Gaissmaier, W., Haase, N., et al. (2012). Opportunities and challenges of Web 2.0 for vaccination decisions. Vaccine 30, 3727–3733. doi: 10.1016/j.vaccine.2012.02.025
Chapman, G. B., and Coups, E. J. (1999). Predictors of influenza vaccine acceptance among healthy adults. Prevent. Med. 29, 249–262. doi: 10.1006/pmed.1999.0535
Chapman, G. B., and Coups, E. J. (2006). Emotions and preventive health behavior: worry, regret, and influenza vaccination. Health Psychol. 25, 82–90. doi: 10.1037/0278-6133.25.1.82
Chen, C.-H., Chiu, P.-J., Chih, Y.-C., and Yeh, G.-L. (2015). Determinants of influenza vaccination among young Taiwanese children. Vaccine 33, 1993–1998. doi: 10.1016/j.vaccine.2015.01.032
Chiu, M. (2018). Colds and flu: Understanding. PS Post Script. Availabe online at: https://search.informit.com.au/documentSummary;dn=555553429069954;res=IELHEA (accessed May 17, 2019).
Commodari, E. (2017). The role of sociodemographic and psychological variables on risk perception of the flu. SAGE Open 7, 1–10. doi: 10.1177/2158244017718890
Costantino, C., and Vitale, F. (2016). Influenza vaccination in high-risk groups: a revision of existing guidelines and rationale for an evidence-based preventive strategy. J. Prev. Med. Hyg. 57, E13–E18.
Ditsungnoen, D., Greenbaum, A., Praphasiri, P., Dawood, F. S., Thompson, M. G, Yoocharoen, P., et al. (2016). Knowledge, attitudes and beliefs related to seasonal influenza vaccine among pregnant women in Thailand. Vaccine 34, 2141–2146. doi: 10.1016/j.vaccine.2016.01.056
Eastwood, K., Durrheim, D. N., Jones, A., and Butler, M. (2010). Acceptance of pandemic (H1N1) 2009 influenza vaccination by the Australian public. Med. J. Aust. 192, 33–36. doi: 10.5694/j.1326-5377.2010.tb03399.x
Edelman, C. L., Mandle, C. L., and Kudzma, E. C., (eds.). (2018). Health Promotion Throughout the Life Span - E-Book, 9th ed. St. Louis, MO: Elsevier.
Francois, G., Duclos, P. D., Margolis, H., Lavanchy, D., Siegrist, C. A., Meheus, A., et al. (2005). Vaccine safety controversies and the future of vaccination programs. Pediatr Infect. Dis. J. 24, 953–961. doi: 10.1097/01.inf.0000183853.16113.a6
Galvani, A. P., Reluga, T. C., and Chapman, G. B. (2007). Long-standing influenza vaccination policy is in accord with individual self-interest but not with the utilitarian optimum. Proc. Natl. Acad. Sci. U.S.A. 104, 5692–5697. doi: 10.1073/pnas.0606774104
Hofstede, G. (1980), Culture's Consequences: International Differences in Work-Related Values. Beverly Hills, CA: Sage.
Hollmeyer, H. G., Hayden, F., Poland, G., and Buchholz, U. (2009). Influenza vaccination of health care workers in hospitals—A review of studies on attitudes and predictors. Vaccine 27, 3935–3944. doi: 10.1016/j.vaccine.2009.03.056
Ibuka, Y., Chapman, G. B., Meyers, L. A., Li, M., and Galvani, A.P. (2010). The dynamics of risk perceptions and precautionary behavior in response to 2009 (H1N1) pandemic influenza. BMC Infect. Dis. 10:296. doi: 10.1186/1471-2334-10-296
Jefferson, T., Rivetti, D., Rivetti, A., Rudin, M., Di Pietrantonj, C., and Demicheli, V. (2005). Efficacy and effectiveness of influenza vaccines in elderly people: a systematic review. Lancet 366, 1165–1174. doi: 10.1016/S0140-6736(05)67339-4
Kee, S. Y., Lee, S., Cheong, H. J., Chun, B. C., Song, J. Y., Choi, W. S., et al. (2007). Influenza vaccine coverage rates and perceptions on vaccination in South Korea. J. Infect. 55, 273–281. doi: 10.1016/j.jinf.2007.04.354
Larson, H. J., Smith, D. M. D., Paterson, P., Cumming, M., Eckersberger, E., Freifeld, C. C., et al. (2013). Measuring vaccine confidence: analysis of data obtained by a media surveillance system used to analyse public concerns about vaccines. Lancet Infect. Dis. 13, 606–613. doi: 10.1016/S1473-3099(13)70108-7
Lee, H. O., and Kim, S. Y. (2015). Linking health information seeking to behavioral outcomes: antecedents and outcomes of childhood vaccination information seeking in South Korea. J. Health Commun. 20, 285–296. doi: 10.1080/10810730.2014.927035
Lee, K-C, Han, K, Kim, JY, Nam, GE, Han, B-D, Shin, K-E. (2015). socioeconomic status and other related factors of seasonal influenza vaccination in the South KoreanaAdult population based on a nationwide cross-sectional study. PLoS ONE 10:e0117305. doi: 10.1371/journal.pone.0117305
Liao, Q., Cowling, B. J., Lam, W. W. T., and Fielding, R. (2011). Factors affecting intention to receive and self-reported receipt of 2009 pandemic (H1N1) vaccine in Hong Kong: a longitudinal study. PLoS ONE 6:e17713. doi: 10.1371/journal.pone.0017713
Ling, M., Kothe, E. J., and Mullan, B. (2018). Predicting intention to receive a seasonal influenza vaccination using Protection Motivation Theory. Soc Sci Med. 233, 87–92. doi: 10.1016/j.socscimed.2019.06.002
Ludolph, R., Schulz, P. J., and Chen, L. (2018). Investigating the effects of mass media exposure on the uptake of preventive measures by Hong Kong residents during the 2015 MERS outbreak: the mediating role of interpersonal communication and the perception of concern. J. Health Commun. 23, 1–8. doi: 10.1080/10810730.2017.1388455
Maciosek, M. V., Solberg, L. I., Coffield, A. B., Edwards, N. M., and Goodman, M. J. (2006). Influenza vaccination. Health impact and cost effectiveness among adults aged 50 to 64 and 65 and older. Am. J. Prev. Med. 31, 72–79. doi: 10.1016/j.amepre.2006.03.008
Myers, L. B, and Goodwin, R. (2011). Determinants of adults' intention to vaccinate against pandemic swine flu. BMC Public Health 11, 11–15. doi: 10.1186/1471-2458-11-15
Naheed, A., Quinn, S. C., Hancock, G. R., Freimuth, V.S., and Jamison, A. (2018). Social media use and influenza vaccine uptake among White and African American adults. Vaccine 36, 7556–7561. doi: 10.1016/j.vaccine.2018.10.049
Odone, A., Ferrari, A. F., Visciarelli, S., Shefer, A., Pasquarella, C., and Signorelli, C. (2015). Effectiveness of interventions that apply new media to improve vaccine uptake and vaccine coverage: a systematic review. Hum. Vaccin. Immunother. 11, 72–82. doi: 10.4161/hv.34313
Ofstead, C L., Tucker, S. T., Beebe, T. J, and Poland, G. A. (2008). Influenza vaccination among registered nurses: information receipt, knowledge, and decision-making at an institution with a multifaceted educational program. Infect. Control Hospit. Epidemiol. 29, 170–173. doi: 10.1086/526431
Oyserman, D., and Lee, S. W. S. (2008). Does culture influence what and how we think? Effects of priming individualism and collectivism. Psychol. Bull. 134, 311–342. doi: 10.1037/0033-2909.134.2.311
Petts, J., and Niemeyer, S. (2004). Health risk communication and amplification: Learning from the MMR vaccination controversy. Health Risk Soc. 6, 7–23. doi: 10.1080/13698570410001678284
Restivo, V., Costantino, C., Bono, S., Maniglia, M., Marchese, V., Ventura, G., et al. (2018). Influenza vaccine effectiveness among high-risk groups: a systematic literature review and meta-analysis of case-control and cohort studies. Hum. Vaccin. Immunother. 14, 724–735. doi: 10.1080/21645515.2017.1321722
Schmid, P., Rauber, D, Betsch, C., Lidolt, G., and Denker, M-L. (2017). Barriers of influenza vaccination intention and behavior – A systematic review of influenza vaccine hesitancy, 2005 – 2016. PLoS ONE 12:e0170550. doi: 10.1371/journal.pone.0170550
Sheldenkar, A., Lim, F., Yung, C. F., and Lwin, M. O. (2019). Acceptance and uptake of influenza vaccines in Asia: a systematic review. Vaccine 37, 4896–4905. doi: 10.1016/j.vaccine.2019.07.011
Song, H., Omori, K., Kim, J., Tenzek, K. E., Morey Hawkins, J., Lin, W.-Y., et al. (2016). Trusting social media as a source of health information: online surveys comparing the United States, Korea, and Hong Kong. J. Med. Internet. Res. 18:e25. doi: 10.2196/jmir.4193
Streefland, P. H. (2001). Public doubts about vaccination safety and resistance against vaccination. Health Policy 55, 159–172. doi: 10.1016/S0168-8510(00)00132-9
Tabacchi, G., Costantino, C., Cracchiolo, M., Ferro, A., Marchese, V., Napoli, G., et al. (2017). Information sources and knowledge on vaccination in a population from southern Italy: the ESCULAPIO project. Hum. Vaccin. Immunother. 13, 339–345. doi: 10.1080/21645515.2017.1264733
Tabacchi, G., Costantino, C., Napoli, G., Marchese, V., Cracchiolo, M., Casuccio, A., et al. (2016). Determinants of European parents' decision on the vaccination of their children against measles, mumps and rubella: a systematic review and meta-analysis. Hum. Vaccin. Immunother. 12, 1909–1923. doi: 10.1080/21645515.2016.1151990
Tchuenche, J. M., Dube, N., Bhunu, C. P., Smith, R. J., and Bauch, C. T. (2011). The impact of media coverage on the transmission dynamics of human influenza. BMC Public Health 11(Suppl. 1):S5. doi: 10.1186/1471-2458-11-S4-S5
Ward, L., and Draper, J. (2008). A review of the factors involved in older people's decision making with regard to influenza vaccination: a literature review. J. Clin. Nurs. 17, 5–16. doi: 10.1111/j.1365-2702.2006.01861.x
Weinstein, N. D., Kwitel, A., McCaul, K. D., Magnan, R. E., Gerrard, M., and Gibbons, F. X. (2007). Risk perceptions: assessment and relationship to influenza vaccination. Health Psychol. 26, 146–151. doi: 10.1037/0278-6133.26.2.146
Xia, S., and Liu, J. (2013). A computational approach to characterizing the impact of social influence on individuals' vaccination decision making. PLoS ONE 8:e60373. doi: 10.1371/journal.pone.0060373
Keywords: influenza vaccination decision, social factors, senior citizens, Taiwan, South Korea, Switzerland
Citation: Schulz PJ, Wu Y-C, An S and Chen F-L (2019) Social Influences on Influenza Vaccination Decision Among Senior Citizens in Taiwan, South Korea, and Switzerland. Front. Commun. 4:74. doi: 10.3389/fcomm.2019.00074
Received: 21 October 2019; Accepted: 29 November 2019;
Published: 13 December 2019.
Edited by:
Rukhsana Ahmed, University at Albany, United StatesReviewed by:
Elena Commodari, University of Catania, ItalyCopyright © 2019 Schulz, Wu, An and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Peter Johannes Schulz, c2NodWx6cEB1c2kuY2g=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.