- 1Faculty of Kinesiology and Physical Education, University of Toronto, Toronto, ON, Canada
- 2Department of Psychiatry, University of Toronto, Toronto, ON, Canada
- 3Department of Supportive Care, Princess Margaret Cancer Centre, University Health Network, Toronto, ON, Canada
Background: Cancer-related cognitive impairment (CRCI) is a common, persistent quality of life complaint among breast cancer survivors (BCS), however there remain no proven treatments. There is emerging evidence that aerobic exercise and yoga may improve CRCI. There remains limited research on the safety and feasibility of virtually-supervised, remotely-delivered yoga interventions among cancer survivors, and no yoga studies to date have assessed cognitive function as a primary outcome in BCS. The purpose of this study was to explore the feasibility of an 8-week, remotely-delivered yoga intervention and examine its impact on cognitive function, fatigue, and exercise levels in BCS using a concurrent mixed-methods design.
Methods: Participants completed objective and self-report cognitive function measures (NIH Toolbox remote cognitive battery, PsyToolkit Task Switch test, Functional Assessment of Cancer Therapy-Cognitive Function [FACT-Cog3]); fatigue (Revised-Piper Fatigue Scale); and exercise activity level (modified Godin Leisure Time Exercise Questionnaire) before and after the yoga intervention. Semi-structured qualitative interviews were conducted post-intervention to understand participants' experiences with the yoga intervention, CRCI, and fatigue.
Results: The intervention surpassed a priori feasibility indicators (adherence rate = 83.7%, attrition rate = 5.4%, no adverse events). Participants (n = 18, Mage= 52.2 ± 10.1) had significant improvements in objective memory, fatigue, and weekly minutes of moderate-to-vigorous exercise post-intervention. Qualitative themes indicated that participants found the remote intervention to be enjoyable and beneficial.
Conclusions: In this small proof-of-concept study, remotely-delivered yoga appears safe and effective at improving CRCI. Future randomized controlled trials examining the impact of remotely-delivered yoga interventions on cognitive function in BCS are warranted.
Background
Cancer-related cognitive impairment (CRCI)—sometimes referred to as “chemobrain”—is a common treatment-related side effect associated with numerous breast cancer treatments including chemotherapy, surgery, and hormone therapy (Ahles et al., 2012; Wefel and Schagen, 2012; Bernstein et al., 2017; Dijkshoorn et al., 2021; Jebahi et al., 2021). CRCI is characterized by difficulties with learning, memory, attention, processing speed, executive function, and intra-individual variability, all of which may contribute to worse quality of life (QoL) and reduced survival (Ahles et al., 2012; Wefel and Schagen, 2012; Yao et al., 2016, 2017b). Studies have demonstrated that up to 75% of breast cancer survivors (BCS) may experiences CRCI, persisting for up to 20 years following treatment (Koppelmans et al., 2012; Ahles and Root, 2018). Despite the prevalence and significance, there are no proven pharmacological treatments, highlighting the need for behavioral interventions that can mitigate the debilitating effects of CRCI for BCS (Argyriou et al., 2011; Bernstein et al., 2018).
Emerging evidence from small RCTs suggests that exercise interventions (i.e., aerobic, combined aerobic-resistance, and mind-body) may be a potential strategy to mitigate or improve cognitive impairments in cancer survivors (Campbell et al., 2019, 2020). Some studies have demonstrated that exercise, including yoga, may improve cognitive impairments related to memory and processing speed in BCS (Derry et al., 2015; Janelsins et al., 2016; Galiano-Castillo et al., 2017; Campbell et al., 2018; Hartman et al., 2018). However, the evidence remains mixed and more research is needed to understand the optimal exercise dose that may mitigate CRCI.
Several studies and reviews have deemed in-person, supervised yoga to be safe and feasible for breast cancer patients and survivors with reported adherence rates to yoga interventions between 75 and 82% (Speed-Andrews et al., 2010; Buffart et al., 2012; Levine and Balk, 2012; Danhauer et al., 2015; Derry et al., 2015; Komatsu et al., 2016). There is limited research exploring the impact of yoga on CRCI, however, preliminary evidence suggests that 4-week and 24-week in-person yoga interventions may improve self-reported memory impairments and cognitive problems in BCS (Derry et al., 2015; Janelsins et al., 2016). However, these studies were limited in that they did not explore cognitive function as a primary outcome and only used a single self-report measure to assess cognitive function. Self-reported cognitive dysfunction is more highly correlated with mood and fatigue than with objective cognitive dysfunction, and the International Cognition and Cancer Task Force (ICCTF) recommends objective tests, which assess processing speed, memory, and executive function domains as the gold standard for measuring cognitive function (Wefel et al., 2011). The literature in older adults has demonstrated that yoga is beneficial to improve memory function for older adults with and without cognitive impairments (Bhattacharyya et al., 2020), yet there are too few yoga studies among cancer survivors to make conclusions about its impact on CRCI. Furthermore, little is known about yoga via remotely-delivered options as previous studies have been conducted in-person.
The evaluation of remote interventions is timely, given that several exercise and yoga programs shifted to virtual platforms and remote delivery during the COVID-19 pandemic and continue to offer online programming (Newton et al., 2020). In addition, frequently cited barriers to in-person yoga and exercise programs have been travel to the fitness center, bad weather, and lack of time (Speed-Andrews et al., 2010; Brunet et al., 2013). Remotely-delivered yoga programs have the potential to reduce these barriers and overall burden for cancer survivors. One pilot study, which adapted its 8-week yoga intervention for BCS to Zoom during the pandemic, reported average adherence to be 87.5% (Knoerl et al., 2021). Further, a feasibility study that examined the impact of a self-directed, at-home yoga program in breast cancer patients undergoing chemotherapy reported a high adherence rate of 94.4% (Komatsu et al., 2016). Although studies have reported generally high adherence and satisfaction rates, more research is needed to determine the delivery and type of remote yoga intervention that BCS will adhere to and benefit from. To our knowledge, this is the first study to evaluate the feasibility of a virtually-supervised, remotely-delivered yoga intervention and assess its impact on both objective and self-reported cognitive function as secondary outcomes. This highlights the need for a pilot feasibility study, which will inform future randomized controlled trials that are adequately powered to assess differences in cognitive function.
The primary purpose of this study was to use a mixed-methods design to assess the feasibility (e.g., enrolment, adherence, attrition, adverse events, satisfaction, participant feedback) of a remotely-delivered yoga intervention for BCS. The secondary objectives were to examine changes in: (1) objectively-assessed cognitive function (i.e., immediate, episodic, and working memory, verbal learning, language/vocabulary knowledge, and shifting and updating) via neuropsychological tests; (2) self-reported cognitive function; (3) self-reported cancer-specific fatigue; and (4) self-reported exercise levels. Qualitative interviews were used to support quantitative findings and gain a deeper understanding of primary and secondary outcomes.
It was hypothesized that the study would meet the following a priori feasibility indicators: adherence rate ≥70%, attrition rate < 30%, and that no adverse events or major injuries would occur as a result of the yoga intervention (Speed-Andrews et al., 2010; Levine and Balk, 2012; Ross Zahavich et al., 2012; Komatsu et al., 2016). It was anticipated that the qualitative feedback would provide insights into facilitators and barriers of the intervention (Galantino et al., 2012b; Levine and Balk, 2012).
Methods
Study design and participants
This study was a concurrent nested mixed-methods single-arm design (ClinicalTrials.gov identifier: NCT05180656). The quantitative and qualitative data were collected in parallel, with the quantitative data being the dominant method and the qualitative data used to complement the quantitative feasibility data and exploratory secondary outcomes (Kroll and Neri, 2009). The study was approved by the University of Toronto Research Ethics Board (REB) (REB Number: 41494). Participants were recruited Canada-wide through social media platforms (e.g., Twitter, Instagram, Facebook) and through local agencies and programs that serve BCS (e.g., Canadian Cancer Society and their Cancer Connection Forum, Gilda's Club Toronto, Wellspring Canada). Inclusion criteria were: (1) ≥18 years of age; (2) males or females with a primary diagnosis of Stage I-IIIa breast cancer; (3) completed primary treatments including surgery, radiation, and/or chemotherapy; (4) proficient in written and spoken English; and (5) access to the Internet and a computer with videoconferencing capabilities. Exclusion criteria were: (1) scheduled to receive primary treatments such as surgery, radiation, or chemotherapy in the future; (2) color-blind since the objective cognitive tests required participants to distinguish between colors; (3) current regular yoga practice defined as ≥2 times/week; and (4) major cognitive disorder(s) or impairment(s) (score ≤ 21 on the Telephone Interview of Cognitive Status) (Bentvelzen et al., 2019). Those who currently practiced yoga two or more times per week were excluded so that feasibility outcomes and potential changes in secondary outcomes could be attributed to the twice-weekly classes during the 8-week yoga intervention, rather than to previous yoga practice.
Yoga intervention
The yoga intervention consisted of two virtually-supervised, one-hour yoga classes per week led by a certified yoga instructor for 8 weeks. The intervention was conducted over a period of 13 weeks with four separate cohorts of participants, each completing the 8-week intervention. If there were two or more interested and eligible participants on a given week, they were enrolled in the intervention in a small cohort and began their 8-week intervention at that time point. The yoga instructor was informed when new participants joined the intervention and had them introduce themselves to the class. She offered simpler poses with detailed explanations for new participants and more advanced pose progressions for the rest of the group.
The instructor was a 200-h Yoga Alliance certified yoga instructor, had completed the “Yoga Thrive: Therapeutic Yoga for Cancer Survivors” certificate, and had several years of experience teaching yoga to cancer patients and survivors. All classes were delivered live through the videoconferencing platform, Zoom, and took place on Tuesday and Thursday evenings. Each Zoom class was opened 15 min before the start time, and participants were told that this was optional informal time that they could use to socialize, which was intended to help foster community in the virtual environment. During the classes, the yoga instructor kept her video on and led the class by demonstrating the poses and providing verbal prompts and live feedback to participants. The primary author also attended and observed all classes to monitor participants' safety, flag participants' questions to the yoga instructor, and record attendance and potential adverse events. Participants were strongly encouraged to have their videos on so that the yoga instructor and primary author could monitor them and provide modifications to the poses as necessary.
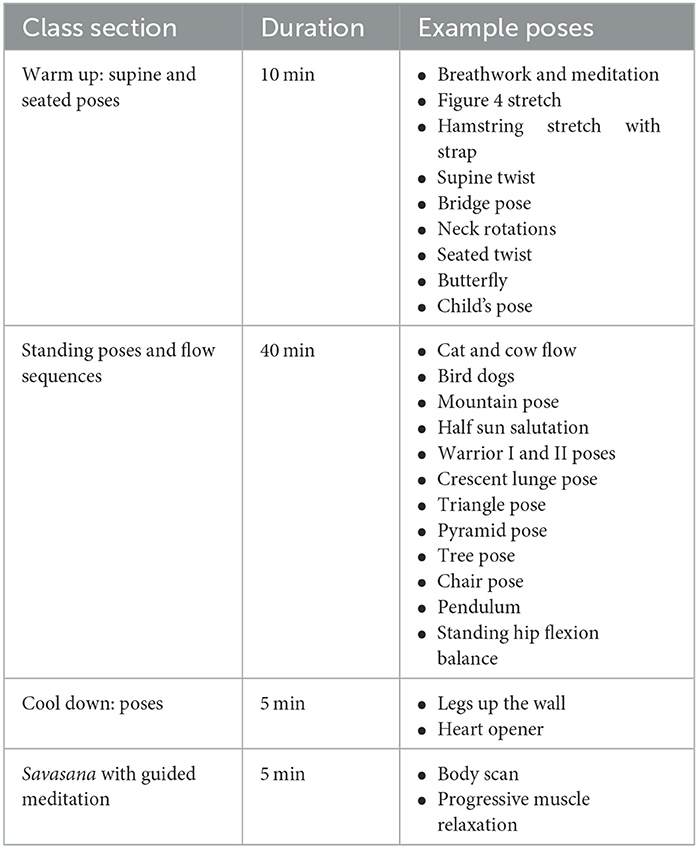
The program was based primarily in Hatha yoga but also incorporated aspects of Iyengar and Vinyasa yoga, as well as breast cancer-specific yoga movements. Participants were encouraged to use props in the form of household items (e.g., chair, belt). Each class consisted of a series of poses paired with breathwork, meditation practices, and themes focused on visualization, affirmations, and self-compassion (Derry et al., 2015). Each class began with a 5–10 min warm-up of supine and seated poses and was followed by 40 min of standing poses (e.g., sun salutation sequence, warrior I and II pose, tree pose, pendulum) paired with flow sequences. Each class concluded with 5 min of cool-down poses and a 5 min focused meditation in Savasana (corpse pose) that incorporated body scans and progressive muscle relaxation (Cramer et al., 2015). A more detailed outline of the class is provided in Table 1.
The classes were designed to have participants work at a moderate intensity (Rating of Perceived Exertion [RPE] = 12–14), with the goal of increasing participants' moderate-vigorous physical activity (MVPA) and improving their cognitive function upon completion of the program (Derry et al., 2015; Ehlers et al., 2017; Biazus-Sehn et al., 2020). The classes progressed in difficulty and variation over the 8 weeks, where the instructor introduced advanced poses and more rapid transitions between the poses every week to each appropriate cohort.
Measures
Demographic and clinical information
Demographic (e.g., age, race, marital status, education level) and clinical (e.g., cancer stage, time since diagnosis, cancer treatments received) variables were collected at baseline via self-report.
Feasibility
Feasibility was assessed through enrolment, adherence, and attrition rates, as well as adverse events and participant burden and satisfaction scores (Craig et al., 2008; Song et al., 2015; Trinh et al., 2021). Enrolment was calculated as the number of participants who enrolled in the intervention, divided by the total number of participants assessed for study eligibility. Adherence was calculated as the number of classes participants attended, divided by the 16 classes offered throughout the intervention. Attrition was based on participant dropout, calculated as the number of participants who did not complete the intervention, divided by the number of participants who remained enrolled at the 8-week post-intervention mark. During the yoga classes, the primary author monitored for any potential adverse events, defined as an unfavorable change in the health of a participant, including abnormal laboratory findings, that occurs during the study. This change may or may not be caused by the intervention/treatment being studied (National Library of Medicine, 2023). Following the intervention, participants filled out a satisfaction survey that assessed their overall impression of the program, including usefulness of the program and burden related to the classes and the assessments (Trinh et al., 2021). Participants rated their responses using a 5-point Likert scale. Participants also indicated their perceived exertion after each class using the Borg RPE scale ranging from 6 to 20, where 6 indicated “no exertion” and 20 indicated “maximal exertion” (Borg, 1982). Average RPE scores across the 16 classes were assessed post-intervention to determine if it was being delivered at a moderate intensity.
Objective cognitive function
Cognitive function was assessed objectively using four tests from the remote NIH Toolbox Cognitive Battery (Heaton et al., 2014; Hook et al., 2021). The NIH Toolbox practice effects are minimal and comparable to other widely used gold-standard cognitive measures (Heaton et al., 2014). The NIH Toolbox Battery was administered at baseline and post-intervention via a shared iPad screen through Zoom and took ~45 min to complete. The tests included the Picture Vocabulary Test to assess language/vocabulary knowledge, the Picture Sequence Memory Test to assess episodic memory, the List Sort Working Memory Test to assess working memory and the executive function updating, and the Auditory Verbal Learning Test to assess immediate memory and verbal learning (Heaton et al., 2014; Hook et al., 2021). Since the remote NIH Toolbox Battery does not include a measure of the executive function shifting, which is commonly impaired in BCS treated with chemotherapy (Bernstein et al., 2017; Yao et al., 2017a), the PsyToolkit Task Switch cognitive test was administered to supplement the NIH Toolbox Battery (Stoet, 2010, 2017).
Self-reported cognitive function
The Functional Assessment of Cancer Therapy-Cognitive Function Version 3 (FACT-Cog3) was used to assess self-reported cognitive function at baseline and post-intervention. Participants were asked to rate 37 items related to perceived cognitive complaints on a 5-point Likert scale (0 = “not at all” or “never” and 4 = “very much” or “several times/day”) where higher scores reflect fewer cognitive problems and better QoL (Von Ah and Tallman, 2015). The FACT-Cog3 has demonstrated good validity and reliability with Cronbach alphas of 0.86 for the total score and between 0.77 and 0.86 for subscale scores (Von Ah and Tallman, 2015).
Self-reported fatigue
The Revised-Piper Fatigue Scale (PFS) is a 22-item questionnaire that was used to assess behavioral/severity, affective meaning, sensory, and cognitive/mood dimensions of fatigue (0–10 point Likert scale) at baseline and post-intervention (Piper et al., 1998). The Revised-PFS has an excellent total reliability score of 0.97 (Piper et al., 1998). Lower scores represent better overall levels of fatigue.
Self-reported exercise
A modified version of the Godin Leisure-Time Exercise Questionnaire (GLTEQ) was used to assess self-reported exercise at baseline and post-intervention. The questionnaire was modified to have participants report the number of times per week and the average duration (minutes/session) that they engaged in resistance exercise, as well as light, moderate, or vigorous leisure-time exercise in a typical week (Godin et al., 1986). Total weekly minutes of MVPA were calculated as the sum of the number of moderate exercise minutes per week, plus 2 times the number of vigorous exercise minutes per week. The GLTEQ has a good reliability coefficient of 0.64 for assessing physical activity (PA) (Godin et al., 1986). It has been employed to assess exercise in oncology populations (Amireault et al., 2015), including in yoga-based intervention studies with BCS (Speed-Andrews et al., 2010).
Qualitative interviews
Qualitative, semi-structured interviews were conducted to further inform the primary outcome of feasibility. Questions addressed what participants enjoyed and did not enjoy about the intervention, program preferences, and barriers or challenges faced, as well as questions related to perceptions of fatigue, mental and physical wellbeing, and cognitive function, which provided additional insight into the secondary outcomes. An 11-question interview guide (Appendix A) was developed based on the primary and secondary study objectives. It was informed by the research team's expertise in exercise oncology and mixed-methods delivery, as well as from previous feasibility and yoga intervention studies that used qualitative and mixed-methods approaches (Carson et al., 2007; Galantino et al., 2012a). Interviews were conducted by the primary author with all participants individually over Zoom within 1 week of them completing the intervention. The interviews were audio-recorded and transcribed via a University of Toronto Zoom for Mac Account (Version: 5.11.1; Account type: education).
Data analysis
Quantitative data analyses were conducted using IBM SPSS Statistics Version 26. Descriptive statistics and frequencies were used to characterize the sample for demographic and clinical variables, as well as for the feasibility outcomes of enrolment, adherence, and attrition rates, RPE values, and satisfaction scores. Secondary outcome data, including scores on the NIH Toolbox Cognitive Battery, PsyToolkit Task Switching Test, FACT-Cog3, Revised-PFS, and GLTEQ, were assessed for skewness and kurtosis (< ±1.0) to determine if they met normality assumptions. For normally distributed data, paired sample t-tests were run to compare pre- and post-scores, and means, standard deviations, and confidence intervals were reported. For non-normally distributed data, Wilcoxon signed-rank tests were run, and medians, interquartile ranges (IQRs), and Z-scores were reported (Field, 2009). Statistical significance was set at p < 0.05. Because of the small sample size and pilot nature of the study, effect sizes (i.e., Cohen's d for t-tests; Pearson's correlation coefficient r for Wilcoxon signed-rank tests) were calculated to determine the magnitude of the difference between scores (Field, 2009). For the FACT-Cog3 and Revised-PFS, clinical minimally important differences (MIDs) were also examined (Stover et al., 2013; Bell et al., 2018).
The interview recordings were transcribed verbatim via Zoom and then formatted and cleaned for correctness. The transcripts were analyzed using Braun and Clarke's six phases of thematic analysis (Braun and Clarke, 2006). The primary author assumed a relativist ontology and subjectivist epistemology by acknowledging that participants' realities were shaped through their lived experiences, while recognizing her own positionality and the co-creation of knowledge with participants during the interview.
Qualitative analyses were done using NVivo Software (Version 12). The primary author (ARN) first became familiar with the transcripts (i.e., re-listening to interviews, re-reading transcripts) while making short analytic notes. Second, the author identified codes (i.e., repeating units of meaning) deductively by coding all text relevant to the concept of feasibility (e.g., enjoyment, barriers, facilitators, future suggestions, satisfaction). The author then coded inductively, generating codes based on repeating words or notions, which allowed unexpected concepts to be accounted for. After the initial coding, two research assistants (GG, MH) each coded a subset of two transcripts and a collaborative approach was used to refine codes and uncover a richer understanding of the data (Braun and Clarke, 2019). After codes were finalized, the primary author searched for themes across the codes and refined theme names with the last author (LT) to ensure that they were representative of the data. NVivo was used to record the number of participants that discussed each theme to uncover the most prominent themes across the dataset. Specific participant quotes were selected, reviewed by the last author, and used to write up the findings.
Rigor in the qualitative data was established in several ways. Transcripts were re-read at the start of the analysis process to ensure familiarity. The primary author refined the initial codes while integrating independent codes generated by two additional research assistants (GG, MH) to ensure that the process was data-driven. Rigor was further established by maintaining the stated subjectivist epistemological stance and acknowledging all authors' positionality. We acknowledge our various backgrounds on exercise oncology, neuropsychology, cancer rehabilitation, and breast cancer survivorship, and consider exercise to be an important part of cancer treatment and rehabilitation. These factors contributed to and shaped the interpretation of the qualitative data.
A concurrent nested mixed-methods design was used with the quantitative and qualitative data collected in parallel and analyzed simultaneously (Kroll and Neri, 2009). The qualitative findings assisted with the interpretation of quantitative feasibility findings and participants' perceptions regarding the quantitative secondary outcomes. Integration of the quantitative and qualitative data occurred in the methods, results, and discussion sections. Merging took place during the methods phase, where the interview guide was designed to support the primary and secondary quantitative outcomes (Fetters et al., 2013). A narrative contiguous approach was used with quantitative and qualitative findings presented separately in the results, and a narrative weaving approach was implemented in the discussion, where both quantitative and qualitative data were presented together (Fetters et al., 2013).
Results
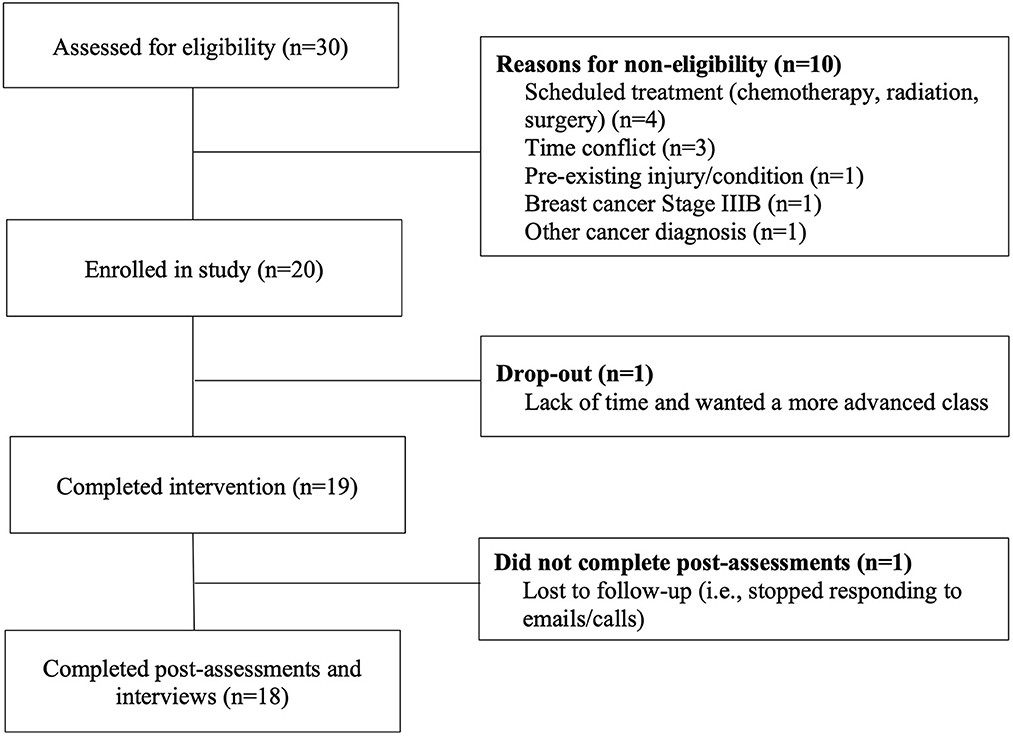
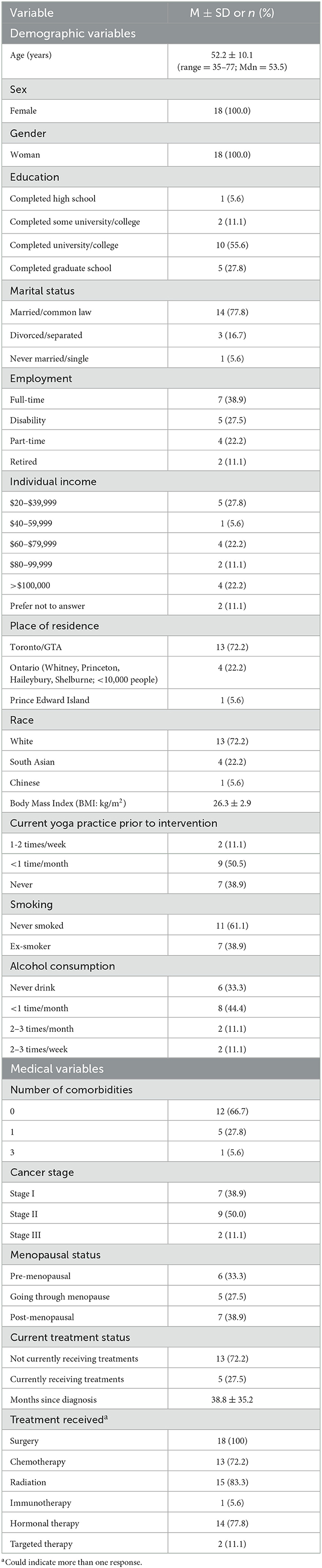
Twenty breast cancer survivors were recruited and enrolled in the 8-week yoga program in four separate cohorts (i.e., n = 12 in the first cohort at week 1, n = 2 in the second cohort at week 2, n = 3 in the third cohort at week 3, and n = 3 in the fourth cohort at week 6). Of the 20 participants enrolled, 19 completed the 8-week yoga intervention and 18 completed all post-program follow-up measures (i.e., cognitive tests, questionnaires, individual semi-structured interview). Participant flow through the study is outlined in Figure 1. The reported results are based on the 18 participants who completed all follow-up measures. Demographic and medical characteristics of the sample are reported in Table 2. All participants were female, identified as women, and were an average age of 52.2 ± 10.1 years. The majority were White (73%), married (78%), resided in Toronto/the Greater Toronto Area (GTA) (72%) and had completed university, college, or graduate studies (83%). Participants were on average 3.25 years post-breast cancer diagnosis. All participants had received surgery (100%) and the majority had also received radiation treatment (82%), hormonal therapy (78%), and/or chemotherapy treatment (72%).
Quantitative findings
Feasibility
The feasibility indicators of enrolment, adherence, attrition, and adverse events were calculated with the entire sample (n = 20), including participants who dropped out. The enrolment rate was 66.7% with 30 participants screened for eligibility and 20 participants enrolled in the study (Figure 1). Participants attended an average of 14 of the 16 classes over the 8-week period, resulting in an adherence rate of 83.7%. One participant dropped out after attending 3 of 8 weeks of the intervention (6 classes) due to lack of time and wanting a more advanced class, which resulted in an attrition rate of 5.3%. No adverse events occurred. Thus, the study met the a priori feasibility indicators of adherence rate ≥70%, attrition rate < 30%, and no adverse events (Speed-Andrews et al., 2010; Levine and Balk, 2012; Ross Zahavich et al., 2012; Komatsu et al., 2016).
The average participant-reported RPE across classes was 12 (range = 7.4–16.1), which was calculated as the mean of each participant's reported RPE across the 16 classes. Participants' average RPE fell in the lower end of the moderate intensity range (RPE range = 12–14). Based on average RPE scores, 50% of participants were working at or above a perceived moderate intensity (RPE≥12) and 50% were working below the intensity (RPE < 12).
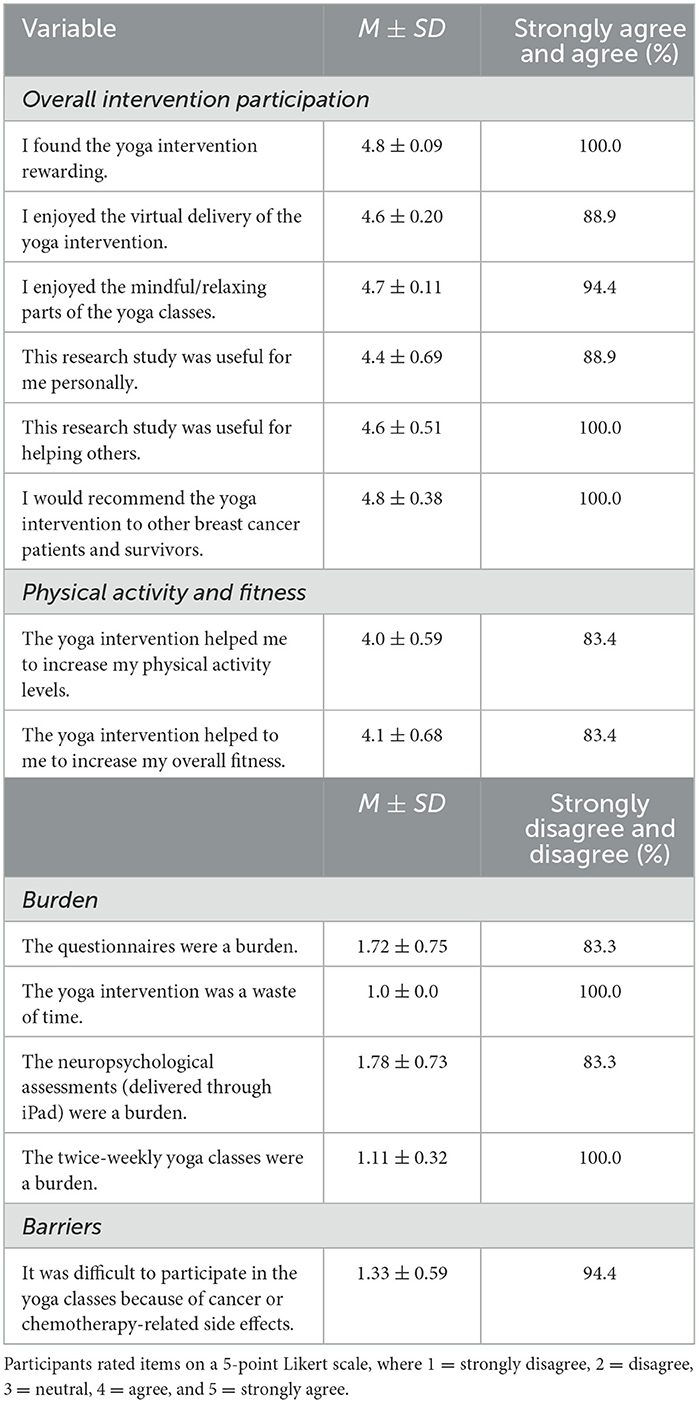
Participant responses on the satisfaction questionnaire revealed high overall satisfaction and low overall burden with respect to both the yoga intervention and study. Average scores and percentages for items are reported in Table 3. Briefly, all participants found the yoga intervention to be rewarding and would recommend it to others, and 88.9% enjoyed the virtual delivery of the intervention. Participants did not find the yoga intervention or study assessments burdensome.
Objective cognitive function
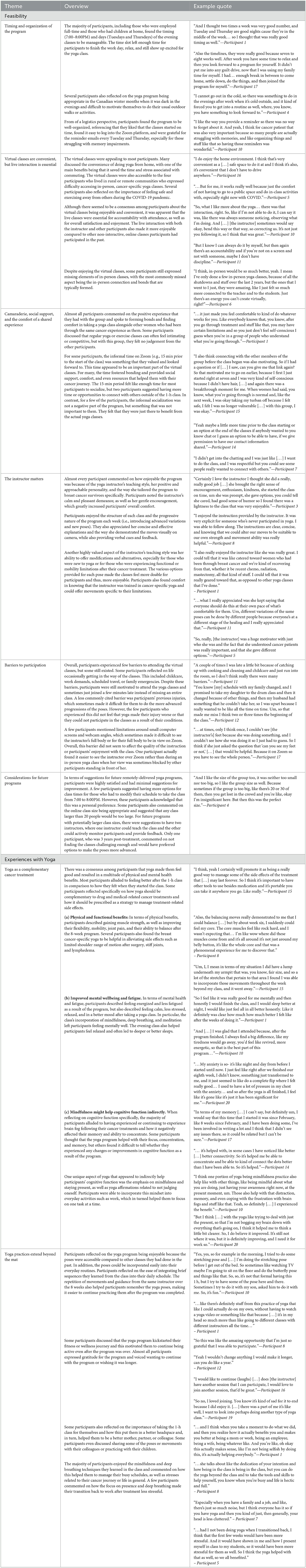
Pre- and post-intervention scores on the objective cognitive function tests are reported in Table 4. Following the yoga intervention, participants demonstrated significant improvements in episodic memory via the Picture Sequence Memory Test (Z = −2.612, p = 0.009, r = −0.44), and trend for improvement in immediate memory and verbal learning via the Auditory Verbal Learning Test (Z = −1.842, p = 0.07, r = −0.31). For the Picture Sequence Memory Test, participants had a mean percentile of 56.0% pre-intervention (range = 2.0–99.0%), which improved to 71.2% post-intervention (range = 17.0–99.0%). Percentile ranks are not calculated for the Auditory Verbal Learning Test. As expected, no significant improvements were observed in language/vocabulary knowledge via the Picture Vocabulary Test, which is considered an index of pre-morbid ability (Z = −0.780, p = 0.44, r = −0.13). However, participants' mean percentile rank on this test was 47.6% pre-intervention (range = 2.0–88.0%), and improved to 55.1% post-intervention (range = 14.0–93.0%). No changes were observed in either working memory or updating via the List Sort Working Memory Test [Mdiff ± SE = −3.22± 2.31; 95% CI = −8.10–1.66; t(17) = −1.39, p = 0.18; dz = −0.33]. On this test, participants had a mean percentile rank of 49.8% pre-intervention (range = 16.0–90.0%), which improved to 60.7% post-intervention (range = 9.0–96.0%).
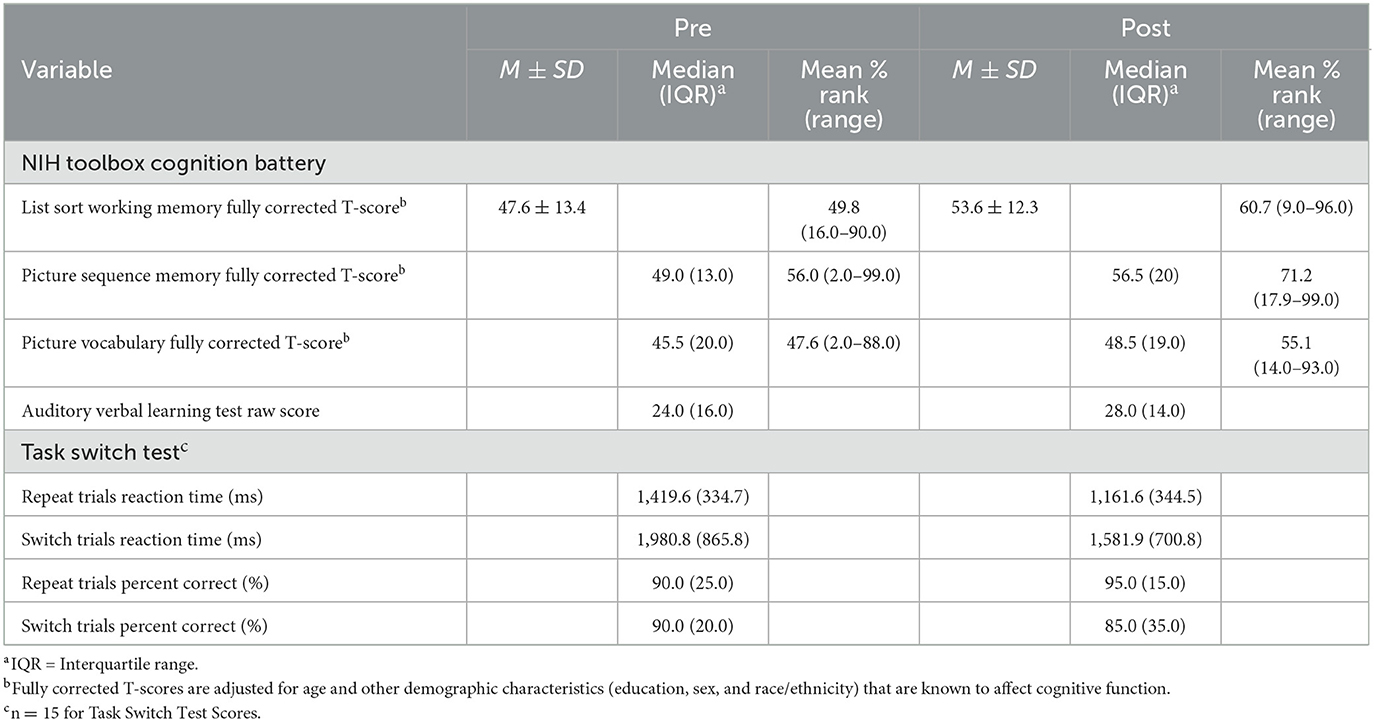
Table 4. Objective cognitive function test scores among breast cancer survivors (n = 18) pre- and post-yoga intervention.
Fifteen participants had complete data on the Task Switching Test. In the mixed block of the test post-intervention, participants had significant improvements in reaction time on non-switch/repeat trials (Z = −2.613, p = 0.009, r = −0.48), and a trend toward significant improvements on switch trials (Z = −1.817, p = 0.07, r = −0.33), but no significant differences in the percentage (%) of correct responses for non-switch (Z = −1.025, p = 0.31, r = −0.19) or switch trials (Z = −0.625, p = 0.532, r = −0.11).
Self-report outcomes
All self-report outcome scores are reported in Table 5. There were no significant or clinically meaningful differences in participants' self-reported cognitive function scores, including comments from others (Z = −0.543, p = 0.59, r = −0.12) and perceived cognitive abilities (PCA) (Z = −0.701, p = 0.48, r = −0.09). There was a trend for improvement in perceived cognitive impairment (PCI) (Z = −1.940, p = 0.052, r = −0.32) and the impact of perceived cognitive impairments on quality of life (Z = −1.860, p = 0.063, r = −0.3) post-intervention.
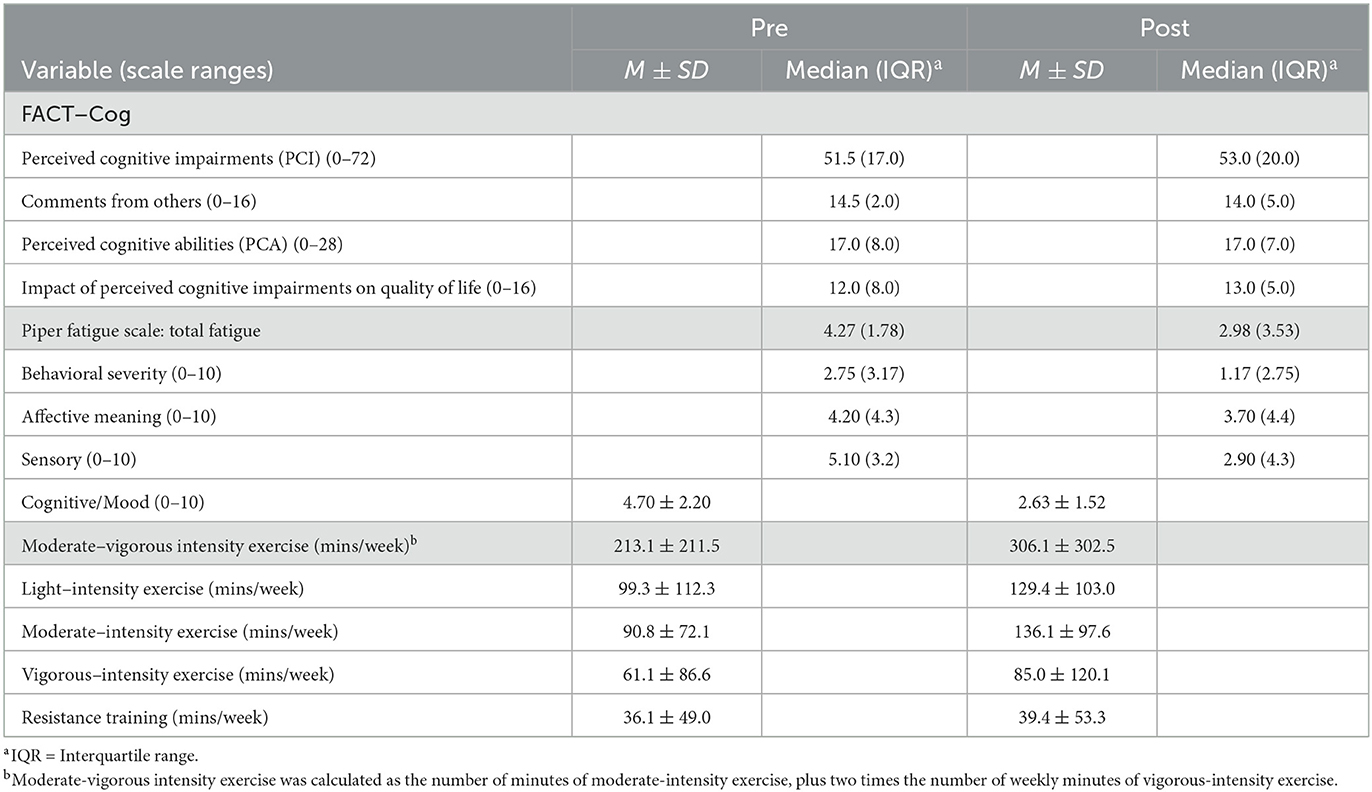
Table 5. Self-reported secondary outcomes of cognitive function, fatigue, and exercise levels among breast cancer survivors (n = 18) pre- and post-yoga intervention.
Participants had significant improvements in total fatigue assessed via the PFS-Revised (Z = −2.831, p = 0.005, r = −0.47) post-intervention, which was also clinically meaningful (MID = 1 point). Participants went from experiencing moderate fatigue (Wefel and Schagen, 2012; Bernstein et al., 2017; Yao et al., 2017b) pre-intervention to mild fatigue (Ahles et al., 2012; Dijkshoorn et al., 2021; Jebahi et al., 2021) post-intervention (Stover et al., 2013). Participants experienced significant improvements on the sensory fatigue subscale (Z = −2.701, p = 0.007, r = −0.45) and the cognitive/mood subscale after the yoga intervention [Mdiff ± SE = 2.07± 2.32; 95% CI = 0.91 – 3.21; t(17) = 3.78, p = 0.002; dz = 0.89], but no significant improvements on the behavioral/severity subscale (Z = −1.140, p = 0.254, r = −0.19) or on the affective meaning subscale (Z = −1.327, p = 0.185, r = −0.22).
Participants significantly increased their weekly MVPA (minutes) post-intervention [Mdiff ± SE = 93.1± 38.8; 95% CI = −174.9 –−11.2; t(17) = −2.40, p = 0.03; dz = −0.57]. The same percentage of participants (55.6%) were meeting guidelines of 150 min/week of MVPA before and after the yoga intervention.
Qualitative findings
Feasibility and experiences with yoga
The following six themes that related to the broader concept of feasibility were identified deductively: (1) Timing and organization of the program; (2) Virtual delivery of classes are convenient, but live interaction is essential; (3) Camaraderie, social support, and the comfort of a shared cancer experience; (4) The instructor matters; (5) Barriers to participation; and (6) Considerations for future programs. Participants found the evening classes to be feasible and manageable, even with the demands of work and childcare. The live classes helped to facilitate adherence and fostered bonding and a sense of community among participants. Most participants valued the informal time to connect with other women ahead of each class, but this was not essential for all participants. The instructor's personality, knowledge on breast cancer, and her ability to offer pose modifications further contributed to adherence and enjoyment. The virtual classes helped to remove barriers to participation such as travel, but barriers for some included busy schedules and challenges with following the instructor's movements on a small screen. Participants had few suggestions regarding changes for future programs, but offering multiple class times and having an additional instructor for classes with more than 20 participants were common suggestions. While participants seemed to greatly enjoy the remote yoga program as a whole, participants voiced different preferences around timing of the classes, the option to socialize, and aspects of in-person classes that cannot be substituted by virtual classes. This demonstrates the importance of designing and individualizing yoga interventions based on participants' unique preferences when possible.
Under the larger concept of experiences with yoga, the following two themes were identified using an inductive approach: 1) Yoga as a complementary cancer treatment; and 2) Yoga practices extend beyond the mat. Within theme 1, three sub-themes were conceptualized including: a) Physical and functional benefits; b) Improved mental well-being and fatigue; and c) Mindfulness may help cognitive function indirectly. Participants discussed feeling better physically and emotionally after the yoga classes, as well as the benefits of yoga after experiencing cancer and treatment-related side effects such as impaired cognitive function. It was also evident that participants valued the yoga poses and mindful practices that they learned during the program and discussed incorporating these practices into their everyday lives. A detailed overview of each theme with relevant participant quotes is outlined in Table 6.
Discussion
The purpose of this study was to evaluate the feasibility of a virtually-supervised, remotely-delivered yoga intervention among BCS using a mixed-methods approach. This study was feasible and exceeded the a priori feasibility indicators of adherence rate ≥70%, attrition rate < 30%, and no adverse events as a result of the yoga intervention. Overall, the intervention was well-received and the majority of BCS enjoyed the program components and expressed positive feedback.
Feasibility
The study enrolment rate over the 3-month recruitment period was 66.7%, which was higher than other remote and hybrid yoga feasibility studies with documented enrolment rates between 34 and 59% (Komatsu et al., 2016; Porter et al., 2019; Faravel et al., 2021; Gothe and Erlenbach, 2022). The adherence rate for this study was 83.3%, which was higher than previously published adherence rates for in-person yoga interventions (45–79%) (Speed-Andrews et al., 2010; Levine and Balk, 2012; Danhauer et al., 2015; Derry et al., 2015), but in line with adherence rates for remotely-delivered yoga interventions (78–94%) among BCS (Komatsu et al., 2016; Knoerl et al., 2021; Gothe and Erlenbach, 2022). One study which adapted its 8-week yoga intervention to Zoom because of the COVID-19 pandemic, found that adherence among cancer survivors increased from 33% to 87.5% when the intervention was moved from in-person to Zoom (Knoerl et al., 2021). These findings, along with the high adherence rate reported in our study, suggest that remotely-delivered interventions have the potential to increase participant adherence due to the removal of barriers such as commuting and lack of time. In our study, Zoom functioned well and there were minimal technology-related disruptions experienced by the instructor or participants. Muting participants, “pinning” the yoga instructor's video, and sending reminder emails with the Zoom link were all aspects that facilitated smooth virtual delivery.
The overall study attrition rate of 5.3% was below the a priori indicator of < 30%. Participants expressed that the difficulty level of the class was appropriate, and greatly valued the modifications offered for the poses, including the option to tailor their yoga practice to their physical needs/limitations. These findings suggest that options for pose modifications contributed to high adherence and thus, future yoga programs should consider the importance of providing options in the poses. There were no adverse events and participants who had pre-existing injuries or mobility limitations (e.g., back pain, frozen shoulder, lymphedema) reported that the yoga classes were appropriate with modifications and did not exacerbate their conditions. Based on the qualitative findings, the instructor's knowledge and teaching style was evidently one of the most positive parts of the program for participants and an important consideration for future yoga studies and programs when selecting a yoga instructor. These findings suggest that virtually-supervised yoga classes, taught by an instructor who has knowledge, training, and previous experience teaching yoga to cancer survivors, are potentially safe for BCS with various conditions at different time points post-treatment.
BCS were highly satisfied with the yoga intervention and did not find the twice-weekly, one-hour yoga classes or the study assessments (i.e., questionnaires, cognitive tests) to be burdensome. Qualitative research conducted with adults and cancer survivors during the pandemic suggests that remote exercise interventions are acceptable and appealing because of the technology, accountability, and social support formed with virtual groups (Brannon et al., 2022). Our qualitative themes highlighted that the timing (i.e., evenings) and the frequency (two times/week) of the classes were feasible, even for those who worked or had children at home. Yoga was a particularly enjoyable form of exercise in the evenings as it helped participants to relax before bedtime. Thus, future studies should consider offering evening yoga classes. A few participations suggested having more options for class times, so it might be important for future programs to consider hosting numerous class times.
Other reasons for high attendance and enjoyment were attributed to the well-organized program structure, the instructor's teaching style and modifications offered, the live classes which helped with accountability and convenience, and the social support and comfort of attending with other women who had experienced breast cancer. In previous studies that evaluated in-person yoga interventions, the social environment was an important positive element of the interventions (Speed-Andrews et al., 2010; Levine and Balk, 2012) and our findings suggest that social support can still be fostered in a virtual class environment. In our study, social support was fostered by opening the Zoom class 15 min early, which provided participants with the option to socialize with others in an informal manner. Future studies should consider including a designated time before and after the virtual class for participants to connect and potentially time for just participants to bond (i.e., no yoga instructor or researcher).
Qualitatively, participants experienced few barriers to attending the virtual classes. Although some participants discussed that daily responsibilities such as work, family emergencies, or childcare, would sometimes result in being late to or missing a class, the virtual classes helped to remove these barriers. Several participants discussed feeling fatigued before attending class but were motivated to attend because of the ease of joining from their homes. Previous studies have highlighted that travel to in-person classes, illness or fatigue, and scheduling conflicts are some of the main barriers to attending in-person yoga interventions (Speed-Andrews et al., 2010; Danhauer et al., 2015). Our findings suggest that virtual classes can remove barriers such as travel and fatigue. Offering virtual or hybrid in-person/virtual classes may increase adherence rates and reduce barriers to future exercise programming for cancer survivors.
Secondary outcomes
The secondary outcomes of cognitive function, fatigue, and exercise levels were exploratory. The study sample was underpowered to examine significant changes in these outcomes, but had a sensitivity to predict medium-large effects (dz ≥ 0.70). Thus, changes in secondary outcomes were interpreted with caution and MIDs were examined where possible. Participants had significant improvements in episodic memory scores after the intervention with a medium-large effect size, however, it was below what our sample size (n = 18) could reliably detect. There is limited literature examining the impact of yoga on objectively-assessed memory in cancer survivors, however, our findings are in line with a meta-analysis that reported yoga and mind-body therapies to be beneficial to improve memory function in older adults (Bhattacharyya et al., 2020). The studies in the meta-analysis delivered mainly in-person classes, highlighting the need for more studies evaluating the effect of virtual yoga interventions on cognitive function. One study reported improvements in cancer survivors' self-reported memory after a 4-week yoga intervention (Janelsins et al., 2016). Our findings add to this literature and suggest that BCS may experience improvements in memory after a moderate-intensity yoga intervention, however, this needs to be replicated with a control group to determine whether improvements were due to the intervention. It should be noted that only half of the participants in our study were achieving a moderate-intensity RPE, which may not have been sufficient to observe changes in cognitive function (Ehlers et al., 2017). Future research should examine participants' cognitive function scores in relation to their RPE scores to determine if achieving a higher intensity of exercise is correlated with changes in cognitive function.
Objective measures of working memory, immediate memory, verbal learning, and the executive function updating improved after the yoga intervention, but these improvements were not significant. However, participants were not required to have a pre-determined level of cognitive impairment to be considered eligible for the study. As a result, participants' baseline level of cognitive function may have been better than expected, which could explain why larger improvements in cognitive function were not seen post-intervention. Small RCTs that have examined the impact of aerobic exercise interventions on cognitive function in BCS reported significant improvements in processing speed in the exercise group, but similar to our study, did not report consistent improvements across all measures of cognitive function (Campbell et al., 2018; Hartman et al., 2018). An RCT with a larger sample size is needed to make definitive conclusions on whether yoga has the potential to improve objective measures of cognitive function. There is also limited research on best practices to deliver cognitive function assessments remotely. We followed the remote administration guidelines to deliver the NIH Toolbox Remote Cognitive Battery to participants via Zoom (Hook et al., 2021). However, no studies to date have used the Remote NIH Toolbox Battery to assess cognitive function in BCS after a yoga intervention, making it challenging to compare our cognitive function results.
There were no significant or clinically meaningful improvements in self-perceived cognitive function post-yoga intervention, however there was a trend for improvement in PCI and the impact of PCI on quality of life. The effect size for the PCI subscale was medium (0.32), which was larger than an effect size for PCI (0.04) in BCS following a 24-week aerobic exercise intervention (Campbell et al., 2018). The lack of significant improvements can be attributed to several aspects including participants overestimating their baseline level of self-perceived cognitive function, the small sample size being underpowered to detect differences, two participants having prior, somewhat regular yoga experience (1–2 times/week), and the intervention being too short and/or not delivered at a sufficient enough exercise intensity to see improvements. Although not significant, a novel qualitative finding was that yoga's focus on mindfulness, presence, and deep breathing appeared to indirectly help participants with their concentration and memory, with mindful practices helping participants focus on daily tasks. A meta-analysis of functional MRI studies demonstrated that cancer survivors treated with chemotherapy had lower activation in two clusters of the brain's frontoparietal attention network, an area important for controlled attention (Bernstein et al., 2021). One theory suggests that the controlled breathing and meditative practices in yoga that focus on mind-wandering, memory consolidation, and self-reflective thinking are associated with activation in a network of brain regions called the Default Mode Network, which has been associated with improved working memory in adults (Voss et al., 2010; Gothe and Mcauley, 2015). Thus, there may be implications that mindfulness and breathing in yoga, separate from the physical effects of MVPA, play a unique role in improving cancer survivors' self-perceived cognitive function. Future studies should consider exploring changes in mindfulness as a potential mediator in the relationship between yoga and cognitive function.
Participants experienced significant and clinically meaningful improvements in self-perceived cancer-related fatigue, with a medium-large effect size following the yoga intervention. Of particular note, participants' fatigue improved from the moderate to mild range post-intervention (Stover et al., 2013). This finding was further supported by the qualitative findings where participants described an ongoing struggle with fatigue after their diagnosis, but described feeling more energized after the yoga classes. The literature supports these findings, reporting a small-moderate beneficial effect of yoga on cancer-related fatigue (O'Neill et al., 2020). Given that fatigue is a frequently cited complaint among BCS, our study shows that cancer-related fatigue may improve following an 8-week yoga intervention.
Participants experienced significant improvements on the cognitive/mood domain of fatigue and the large effect size (0.89) was in line with what a sample size of 18 could detect. This is somewhat unsurprising given that one of the predicted mechanisms through which exercise may improve CRCI is through reductions in fatigue (Ehlers et al., 2017). Among BCS, research has shown that greater daily MVPA is associated with less fatigue and that fewer fatigue symptoms are associated with better scores on objective assessments of executive function, memory, and attention (Ehlers et al., 2017; Salerno et al., 2021). Although more research is needed, our study adds to evidence that MVPA, as well as cancer-related fatigue, cognitive-specific fatigue, and objectively-assessed memory may improve after a yoga intervention.
The qualitative themes also revealed that some of the benefits of the yoga program were reductions in stress, improvements in sleep, and positive social interactions and bonds formed with others. Future studies may consider measuring some of these variables to determine how they might affect the relationship between yoga and cognitive function.
Lessons learned and modifications
Twice-weekly, one-hour evening classes were feasible for BCS and study assessments were not burdensome, suggesting that few adjustments need to be made to the intervention or the study design before implementing a future RCT. Thus, the next step for this work is to conduct an RCT that is powered to examine the impact of a remotely-delivered yoga intervention on self-reported and objective cognitive function in BCS.
In our study, the primary author attended and observed all classes to monitor participant safety and to assist the yoga instructor in managing the virtual environment. This was beneficial to both the instructor and the participants and future remotely-delivered interventions may wish to make use of a second instructor or exercise specialist. The yoga instructor's personality and teaching style, as well as the approachability of the researcher and instructor for participant feedback and questions, played an important role in enjoyability and feasibility for participants. Future yoga studies should strongly consider employing a yoga instructor who has cancer-specific training and is able to offer modified movements for participants with limitations/injuries. Another consideration for future interventions would be to provide participants with at least 15 minutes of optional time before or after each class to interact for overall class enjoyment, accountability, and to help foster a sense of community. Given that participants expressed wanting a longer intervention, future studies could consider evaluating a 12-week or 16-week yoga program to determine whether a longer program might produce greater improvements in cognitive function.
Finally, the qualitative findings demonstrated that BCS have various preferences for remotely-delivered yoga, including preferences for socialization and the timing of the classes. This highlights the importance of tailoring future yoga interventions to the individual preferences and needs of BCS. BCS in this study appeared to unanimously appreciate the live instruction, options/modifications offered for the poses, and being able to take the class at their own pace. These are unique aspects of yoga that may make it particularly appealing for BCS compared to other types of exercise, and an important consideration for any future exercise oncology study.
Strengths and limitations
The evaluation of a remotely-delivered yoga intervention was timely due to the COVID-19 pandemic, given that several exercise and yoga programs for cancer survivors were adapted to remote delivery and the effectiveness of these programs remains unknown. Remote interventions offer convenience, comfort, and increased access for rural communities. Another strength was employing a yoga instructor who had breast-cancer specific training, knowledge, and teaching experience. Live instruction and feedback from the instructor increased participants' comfort levels and reduced fears of injury or exacerbating treatment-related limitations. The use of a standardized, well-validated battery of cognitive tests via the NIH Toolbox was another strength and in line with the ICCTF's recommendation to use objective cognitive measures that assess processing speed, memory, and executive function domains (Wefel et al., 2011). Future studies assessing cognitive function should refer to the ICCTF's recommendations when selecting cognitive function measures (Wefel et al., 2011). Finally, the use of mixed-methods to examine the feasibility of a remotely-delivered yoga intervention was a strength. Using a concurrent nested design, the qualitative findings assisted with a deeper interpretation of the quantitative findings and were used to understand which aspects of the intervention were especially valuable and why.
A limitation of the study was the single-group design and the lack of a control group, which may have masked the true effect of the yoga intervention. With a small sample size and no control group, we are unable to definitively conclude whether improvements in cognitive function and fatigue were due to the yoga intervention itself or other factors (i.e., practice effects, general improvements in side effects over time, other exercise outside of the yoga intervention). Another limitation was that the majority of the sample was highly educated and predominantly White and therefore, not representative of all BCS. Homogenous samples (e.g., White, young, and highly educated) are a common limitation across distance-based exercise oncology trials (Groen et al., 2018). In our study, seven participants of the original 20 enrolled identified as South Asian or Chinese, but greater efforts need to be made to recruit a more racially diverse sample. Recruitment strategies and partnerships with organizations that serve minority racial groups and lower socio-economic status groups of cancer survivors forged ahead of time may aid with recruitment.
Conclusion
This study used a mixed-methods approach to evaluate the feasibility of a remotely-delivered yoga intervention in BCS. To our knowledge, this is the first yoga study to do so while also assessing cognitive function via both self-report and objective measures. The quantitative feasibility results, in addition to the qualitative findings, indicated that the intervention was feasible, safe, and enjoyable for participants. Improvements were noted in the secondary outcomes of cognitive function, fatigue, and MVPA levels, however, due to the small sample size and single-group design, these improvements should be interpreted with caution. The findings are novel in that they highlighted that virtually-supervised yoga classes delivered through videoconferencing are convenient, enjoyable, and result in high adherence rates. For BCS, yoga may potentially help to manage treatment-related side effects such as fatigue and CRCI. Overall, the design of both the study and intervention should be replicated in future RCTs that are adequately powered to assess changes in self-reported and objective cognitive function.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by University of Toronto Research Ethics Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
AN: Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Writing—original draft. LB: Conceptualization, Writing—review & editing. CS: Writing—review & editing, Conceptualization. JJ: Conceptualization, Writing—review & editing. LT: Conceptualization, Methodology, Supervision, Writing—review & editing, Resources.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. AN was supported by the Canadian Institutes of Health Research Canada Graduate Scholarship-Master's program.
Acknowledgments
We would like to acknowledge and greatly thank the study's yoga instructor, Patricia (Trish) Blinn (Princess Margaret Cancer Center, Toronto, ON, Canada), who designed and conceptualized the yoga program with the support of the primary author and taught all of the classes over the course of the intervention. This study would not have been possible without her expertise and dedication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcogn.2023.1286844/full#supplementary-material
References
Ahles, T. A., and Root, J. C. (2018). Cognitive effects of cancer and cancer treatments. Annu. Rev. Clin. Psychol. 14, 425–451. doi: 10.1146/annurev-clinpsy-050817-084903
Ahles, T. A., Root, J. C., and Ryan, E. L. (2012). Cancer- and cancer treatment-associated cognitive change: An update on the state of the science. J. Clin. Oncol. 30, 3675–3686. doi: 10.1200/JCO.2012.43.0116
Amireault, S., Godin, G., Lacombe, J., and Sabiston, C. M. (2015). The use of the Godin-Shephard Leisure-Time Physical Activity Questionnaire in oncology research: a systematic review. BMC Med. Res. Methodol. 15, 1–11. doi: 10.1186/s12874-015-0045-7
Argyriou, A. A., Assimakopoulos, K., Iconomou, G., Giannakopoulou, F., and Kalofonos, H. P. (2011). Either called “chemobrain” or “chemofog,” the long-term chemotherapy-induced cognitive decline in cancer survivors is real. J. Pain Symptom Manage. 41, 126–139. doi: 10.1016/j.jpainsymman.2010.04.021
Bell, M. L., Dhillon, H. M., Bray, V. J., and Vardy, J. L. (2018). Important differences and meaningful changes for the functional assessment of cancer therapy-cognitive function (FACT-COG). J. Patient-Report. Outcom. 48, 2. doi: 10.1186/s41687-018-0071-4
Bentvelzen, A. C., Crawford, J. D., Theobald, A., Maston, K., Slavin, M. J., Reppermund, S., et al. (2019). Validation and normative data for the modified telephone interview for cognitive status: the sydney memory and ageing study. J. Am. Geriatr. Soc. 67, 2108–2115. doi: 10.1111/jgs.16033
Bernstein, L. J., Edelstein, K., Sharma, A., and Alain, C. (2021). Chemo-brain: an activation likelihood estimation meta-analysis of functional magnetic resonance imaging studies. Neurosci Biobehav Rev. 130, 314–25. doi: 10.1016/j.neubiorev.2021.08.024
Bernstein, L. J., McCreath, G. A., Komeylian, Z., and Rich, J. B. (2017). Cognitive impairment in breast cancer survivors treated with chemotherapy depends on control group type and cognitive domains assessed: a multilevel meta-analysis. Neurosci Biobehav Rev. 83, 417–28. doi: 10.1016/j.neubiorev.2017.10.028
Bernstein, L. J., McCreath, G. A., Nyhof-Young, J., Dissanayake, D., and Rich, J. B. A. (2018). brief psychoeducational intervention improves memory contentment in breast cancer survivors with cognitive concerns: results of a single-arm prospective study. Support. Care Cancer 26, 2851–2859. doi: 10.1007/s00520-018-4135-z
Bhattacharyya, K. K., Andel, R., and Small, B. J. (2020). Effects of yoga-related mind-body therapies on cognitive function in older adults: a systematic review with meta-analysis. Arch. Gerontol. Geriatr. 93, 104319. doi: 10.1016/j.archger.2020.104319
Biazus-Sehn, L. F., Schuch, F. B., Firth, J., and Stigger, F. S. (2020). Effects of physical exercise on cognitive function of older adults with mild cognitive impairment: a systematic review, and meta-analysis. Arch. Gerontol. Geriatr. 89, 104048. doi: 10.1016/j.archger.2020.104048
Borg, G. A. V. (1982). Psychophysical bases of perceived exertion. Med. Sci. Sport Exerc. 14, 377–381. doi: 10.1249/00005768-198205000-00012
Brannon, G. E., Mitchell, S., Ray, M. A., Bhai, S., Beg, M. S., Basen-Engquist, K. M., et al. (2022). A qualitative examination of COVID-19′s impacts on physical activity and perceptions of remote delivery interventions. Am J Heal Promot. 36, 472–476. doi: 10.1177/08901171211053845
Braun, V., and Clarke, V. (2006). Using thematic analysis in psychology. Qual. Res. Psychol. 3, 77–101. doi: 10.1191/1478088706qp063oa
Braun, V., and Clarke, V. (2019). Reflecting on reflexive thematic analysis. Qual. Res. Sport Exerc. Heal. 11, 589–97. doi: 10.1080/2159676X.2019.1628806
Brunet, J., Taran, S., Burke, S., and Sabiston, C. M. A. (2013). qualitative exploration of barriers and motivators to physical activity participation in women treated for breast cancer. Disabil. Rehabil. 35, 2038–2045. doi: 10.3109/09638288.2013.802378
Buffart, L. M., van Uffelen, J. G. Z., Riphagen, I. I., Brug, J., Mechelen, W., van Brown, WJ, et al. (2012). Physical and psychosocial benefits of yoga in cancer patients and survivors, a systematic review and meta-analysis of randomized controlled trials. BMC Cancer. 12, 1–21. doi: 10.1186/1471-2407-12-559
Campbell, K., Kam, J. W. Y., Neil-Sztramko, S. E., Liu Ambrose, T., Handy, T. C., Lim, H. J., et al. (2018). Effect of aerobic exercise on cancer-associated cognitive impairment: a proof-of-concept RCT. Psychooncology 27, 53–60. doi: 10.1002/pon.4370
Campbell, K., Zadravec, K., Bland, K. A., Chesley, E., Wolf, F., Janelsins, M. C., et al. (2020). The effect of exercise on cancer-related cognitive impairment and applications for physical therapy: systematic review of randomized controlled trials. Phys. Ther. 100, 523–542. doi: 10.1093/ptj/pzz090
Campbell, K. L., Winters-Stone, K. M., Wiskemann, J., May, A. M., Schwartz, A. L., Courneya, K. S., et al. (2019). Exercise guidelines for cancer survivors: consensus statement from international multidisciplinary roundtable. Med. Sci. Sports Exerc. 51, 2375–2390. doi: 10.1249/MSS.0000000000002116
Carson, J. W., Carson, K. M., Porter, L. S., Keefe, F. J., Shaw, H., Miller, J. M., et al. (2007). Yoga for women with metastatic breast cancer: results from a pilot study. J. Pain Symptom Manage. 33, 331–341. doi: 10.1016/j.jpainsymman.2006.08.009
Craig, P., Dieppe, P., Macintyre, S., Mitchie, S., Nazareth, I., Petticrew, M., et al. (2008). Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ. 337, 979–83. doi: 10.1136/bmj.a1655
Cramer, H., Rabsilber, S., Lauche, R., Kümmel, S., and Dobos, G. (2015). Yoga and meditation for menopausal symptoms in breast cancer survivors - a randomized controlled trial. Cancer 121, 2175–2184. doi: 10.1002/cncr.29330
Danhauer, S. C., Griffin, L., Avis, N., Sohl, S., Jesse, M., Addington, E., et al. (2015). Feasibility of implementing a community-based randomized trial of yoga for women undergoing chemotherapy for breast cancer. J. Commu. Support Oncol. 13, 139–147. doi: 10.12788/jcso.0125
Derry, H. M., Jaremka, L. M., Bennett, J. M., Peng, J., Andridge, R., Shapiro, C., et al. (2015). Yoga and self-reported cognitive problems in breast cancer survivors: a randomized controlled trial. Psychooncology 24, 958–966. doi: 10.1002/pon.3707
Dijkshoorn, A. B. C., van Stralen, H. E., Sloots, M., Schagen, S. B., Visser-Meily, J. M. A., Schepers, V. P. M., et al. (2021). Prevalence of cognitive impairment and change in patients with breast cancer: a systematic review of longitudinal studies. Psychooncology 30, 635–648. doi: 10.1002/pon.5623
Ehlers, D. K., Aguiñaga, S., Cosman, J., Severson, J., Kramer, A. F., McAuley, E., et al. (2017). The effects of physical activity and fatigue on cognitive performance in breast cancer survivors. Breast Cancer Res. Treat. 165, 699–707. doi: 10.1007/s10549-017-4363-9
Faravel, K., Huteau, M. E., Jarlier, M., de Forges, H., Meignant, L., Senesse, P., et al. (2021). Importance of patient education for at-home yoga practice in women with hormonal therapy-induced pain during adjuvant breast cancer treatment: a feasibility study. Integr. Cancer Ther. 20, 15347354211063791. doi: 10.1177/15347354211063791
Fetters, M. D., Curry, L. A., and Creswell, J. W. (2013). Achieving integration in mixed methods designs - principles and practices. Health Serv. Res. 48, 2134–2156. doi: 10.1111/1475-6773.12117
Field, A. (2009). Discovering Statistics Using SPSS. London; Thousand Oaks, CA; New Delhi; Singapore: SAGE Publications Ltd.
Galantino, M., Greene, L., Archetto, B., Baumgartner, M., Hassall, P., Murphy, J. K., et al. (2012a). A qualitative exploration of the impact of yoga on breast cancer survivors with aromatase inhibitor-associated arthralgias. Explor J. Sci. Heal. 8, 40–47. doi: 10.1016/j.explore.2011.10.002
Galantino, M., Lou, G. L., Daniels, L., Dooley, B., Muscatello, L., and O'Donnell, L. (2012b). Longitudinal impact of yoga on chemotherapy-related cognitive impairment and quality of life in women with early stage breast cancer: a case series. Explor J. Sci. Heal. 8, 127–35. doi: 10.1016/j.explore.2011.12.001
Galiano-Castillo, N., Arroyo-Morales, M., Lozano-Lozano, M., Fernández-Lao, C., Martín-Martín, L., Del-Moral-Ávila, R., et al. (2017). Effect of an Internet-based telehealth system on functional capacity and cognition in breast cancer survivors: a secondary analysis of a randomized controlled trial. Support. Care Cancer 25, 3551–3559. doi: 10.1007/s00520-017-3782-9
Godin, G., Jobin, J., and Bouillon, J. (1986). Assessment of leisure time exercise behavior by self-report: a concurrent validity study. Med. Sci. Sport Exerc. 77, 359–362.
Gothe, N. P., and Erlenbach, E. (2022). Feasibility of a yoga, aerobic and stretching-toning exercise program for adult cancer survivors: the STAYFit trial. J. Cancer Surviv. 16, 1107–1116. doi: 10.1007/s11764-021-01101-y
Gothe, N. P., and Mcauley, E. (2015). Yoga and cognition: a meta-analysis of chronic and acute effects. Psychosom. Med. 77, 784–797. doi: 10.1097/PSY.0000000000000218
Groen, W. G., van Harten, W. H., and Vallance, J. K. (2018). Systematic review and meta-analysis of distance-based physical activity interventions for cancer survivors (2013–2018): we still haven't found what we're looking for. Cancer Treat Rev. 69, 188–203. doi: 10.1016/j.ctrv.2018.07.012
Hartman, S. J., Nelson, S. H., Myers, E., Natarajan, L., Sears, D. D., Palmer, B. W., et al. (2018). Randomized controlled trial of increasing physical activity on objectively measured and self-reported cognitive functioning among breast cancer survivors: the memory and motion study. Cancer 124, 192–202. doi: 10.1002/cncr.30987
Heaton, R. K., Akshoomoff, N., Tulsky, D., Mungas, D., Weintraub, S., Dikmen, S., et al. (2014). Reliability and validity of composite scores from the NIH Toolbox cognition battery in adults. J. Int. Neuropsychol. Soc. 20, 588–598. doi: 10.1017/S1355617714000241
Hook, J., Sivan, A., Nowinski, C., and Gershon, R. (2021). Remote Administration Guidelines for the NIH Toolbox®: Response to COVID-19.
Janelsins, M. C., Peppone, L. J., Heckler, C. E., Kesler, S. R., Sprod, L. K., Atkins, J., et al. (2016). YOCAS©® yoga reduces self-reported memory difficulty in cancer survivors in a nationwide randomized clinical trial: Investigating relationships between memory and sleep. Integr. Cancer Ther. 15, 263–271. doi: 10.1177/1534735415617021
Jebahi, F., Sharma, S., Bloss, J. E., and Wright, H. H. (2021). Effects of tamoxifen on cognition and language in women with breast cancer: a systematic search and a scoping review. Psychooncology 30, 1262–1277. doi: 10.1002/pon.5696
Knoerl, R., Giobbie-Hurder, A., Berfield, J., Berry, D., Meyerhardt, J. A., Wright, A. A., et al. (2021). Yoga for chronic chemotherapy-induced peripheral neuropathy pain: a pilot, randomized controlled trial. J. Cancer Surviv. 2021, 0123456789. doi: 10.1007/s11764-021-01081-z
Komatsu, H., Yagasaki, K., Yamauchi, H., Yamauchi, T., and Takebayashi, T. A. (2016). self-directed home yoga programme for women with breast cancer during chemotherapy: a feasibility study. Int. J. Nurs. Pract. 22, 258–266. doi: 10.1111/ijn.12419
Koppelmans, V., Breteler, M. M. B., Boogerd, W., Seynaeve, C., Gundy, C., Schagen, S. B., et al. (2012). Neuropsychological performance in survivors of breast cancer more than 20 years after adjuvant chemotherapy. J. Clin. Oncol. 30, 1080–1086. doi: 10.1200/JCO.2011.37.0189
Kroll, T., and Neri, M. (2009). Designs for mixed methods research. Mix Methods Res. Nurs. Heal. Sci. 2009, 31–49. doi: 10.1002/9781444316490.ch3
Levine, A. S., and Balk, J. L. (2012). Pilot study of yoga for breast cancer survivors with poor quality of life. Complement Ther. Clin. Pract. 18, 241–5. doi: 10.1016/j.ctcp.2012.06.007
National Library of Medicine (2023). ClinicalTrials.gov Glossary Terms. Available online at: https://www.clinicaltrials.gov/study-basics/glossary (accessed September 15, 2023).
Newton, R. U., Hart, N. H., and Clay, T. (2020). Keeping patients with cancer exercising in the age of COVID-19. JCO Oncol Pract. 16, 656–664. doi: 10.1200/OP.20.00210
O'Neill, M., Samaroo, D., Lopez, C., Tomlinson, G., Santa Mina, D., Sabiston, C., et al. (2020). The effect of yoga interventions on cancer-related fatigue and quality of life for women with breast cancer: A systematic review and meta-analysis of randomized controlled trials. Integr. Cancer Ther. 19, 882. doi: 10.1177/1534735420959882
Piper, B. F., Dibble, S. L., Dodd, M. J., Weiss, M. C., Slaughter, R. E., Paul, S. M., et al. (1998). The revised Piper Fatigue Scale: psychometric evaluation in women with breast cancer. Oncol. Nurs. Forum. 25, 677–684. doi: 10.1037/t18854-000
Porter, L. S., Carson, J. W., Olsen, M., Carson, K. M., Sanders, L., Jones, L., et al. (2019). Feasibility of a mindful yoga program for women with metastatic breast cancer: results of a randomized pilot study. Support. Care Cancer. 27, 4307–4316. doi: 10.1007/s00520-019-04710-7
Ross Zahavich, A. N., Robinson, J. A., Paskevich, D., and Culos-Reed, S. N. (2012). Examining a therapeutic yoga program for prostate cancer survivors. Integr. Cancer Ther. 12, 113–25. doi: 10.1177/1534735412446862
Salerno, E. A., Culakova, E., Kleckner, A. S., Heckler, C. E., Lin, P. J., Matthews, C. E., et al. (2021). Physical activity patterns and relationships with cognitive function in patients with breast cancer before, during, and after chemotherapy in a prospective, nationwide study. J. Clin. Oncol. 39, 3283–3292. doi: 10.1200/JCO.20.03514
Song, M. K., Sandelowski, M., and Happ, M. B. (2015). “Current practices and emerging trends in conducting mixed methods intervention studies in the health sciences,” in SAGE Handbook of Mixed Methods in Social and Behavioral Research, eds. Tashakkori, A., and Teddlie, C. Thousand Oaks: Sage Publications, 725–48.
Speed-Andrews, A. E., Stevinson, C., Belanger, L. J., Mirus, J. J., and Courneya, K. S. (2010). Pilot evaluation of an Iyengar yoga program for breast cancer survivors. Cancer Nurs. 33, 369–381. doi: 10.1097/NCC.0b013e3181cfb55a
Stoet, G. (2010). PsyToolkit: A software package for programming psychological experiments using Linux. Behav. Res. Methods. 42, 1096–1104. doi: 10.3758/BRM.42.4.1096
Stoet, G. (2017). PsyToolkit: a novel web-based method for running online questionnaires and reaction-time experiments. Teach. Psychol. 44, 24–31. doi: 10.1177/0098628316677643
Stover, A. M., Reeve, B. B., Piper, B. F., Alfano, C. M., Smith, A. W., Mitchell, S. A., et al. (2013). Deriving clinically meaningful cut-scores for fatigue in a cohort of breast cancer survivors: A Health, Eating, Activity, and Lifestyle (HEAL) study. Qual. Life Res. 22, 2279–2292. doi: 10.1007/s11136-013-0360-6
Trinh, L., Kramer, A. F., Rowland, K., Strom, D. A., Wong, J. N., McAuley, E. A., et al. (2021). Pilot feasibility randomized controlled trial adding behavioral counseling to supervised physical activity in prostate cancer survivors: behavior change in prostate cancer survivors trial (BOOST). J. Behav. Med. 44, 172–86. doi: 10.1007/s10865-020-00185-8
Von Ah, D., and Tallman, E. F. (2015). Perceived cognitive function in breast cancer survivors: evaluating relationships with objective cognitive performance and other symptoms using the functional assessment of cancer therapy - cognitive function instrument. J. Pain Symptom Manage. 49, 697–706. doi: 10.1016/j.jpainsymman.2014.08.012
Voss, M. W., Prakash, R. S., Erickson, K. I., Basak, C., Chaddock, L., Kim, J. S., et al. (2010). Plasticity of brain networks in a randomized intervention trial of exercise training in older adults. Front. Aging Neurosci. (2010) 2, 1–17. doi: 10.3389/fnagi.2010.00032
Wefel, J. S., and Schagen, S. B. (2012). Chemotherapy-related cognitive dysfunction. Curr. Neurol. Neurosci. Rep. 12, 267–275. doi: 10.1007/s11910-012-0264-9
Wefel, J. S., Vardy, J., Ahles, T., and Schagen, S. B. (2011). International Cognition and Cancer Task Force recommendations to harmonise studies of cognitive function in patients with cancer. Lancet Oncol. 12, 703–708. doi: 10.1016/S1470-2045(10)70294-1
Yao, C., Bernstein, L. J., and Rich, J. B. (2017a). Executive functioning impairment in women treated with chemotherapy for breast cancer: a systematic review. Breast Cancer Res. Treat. 166, 15–28. doi: 10.1007/s10549-017-4376-4
Yao, C., Rich, J. B., Tannock, I. F., Seruga, B., Tirona, K., Bernstein, L. J., et al. (2016). Pretreatment differences in intraindividual variability in reaction time between women diagnosed with breast cancer and healthy controls. J. Int. Neuropsychol. Soc. 22, 530–539. doi: 10.1017/S1355617716000126
Keywords: exercise oncology, breast cancer, yoga, cancer-related cognitive impairment (CRCI), remotely-delivered intervention, feasibility, mixed-methods
Citation: Neville AR, Bernstein LJ, Sabiston CM, Jones JM and Trinh L (2023) Feasibility of a remotely-delivered yoga intervention on cognitive function in breast cancer survivors: a mixed-methods study. Front. Cognit. 2:1286844. doi: 10.3389/fcogn.2023.1286844
Received: 31 August 2023; Accepted: 16 October 2023;
Published: 02 November 2023.
Edited by:
Keita Kamijo, Chukyo University, JapanReviewed by:
Mohamed Aly, Assiut University, EgyptElizabeth Ann Salerno, Washington University in St. Louis, United States
Copyright © 2023 Neville, Bernstein, Sabiston, Jones and Trinh. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Linda Trinh, bGluZGEudHJpbmhAdXRvcm9udG8uY2E=
 Alyssa R. Neville
Alyssa R. Neville Lori J. Bernstein
Lori J. Bernstein Catherine M. Sabiston
Catherine M. Sabiston Jennifer M. Jones2,3
Jennifer M. Jones2,3 Linda Trinh
Linda Trinh