- 1Department of Public and Environmental Wellness, Oakland University, Rochester, MI, United States
- 2Department of Curriculum Development & Delivery, Kilgore Academy, Halfway, MO, United States
- 3Kinesiology & Health Science, Louisiana State University Shreveport, Shreveport, LA, United States
- 4Department of Exercise Science, California Lutheran University, Thousand Oaks, CA, United States
- 5Department of Human Movement Science, Oakland University, Rochester, MI, United States
Type 2 diabetes can result in debilitating vascular complications, and resistance training (RT) is an effective therapy for improving cardiovascular outcomes. However, only 10–30% of adults meet the public health guidance for RT. While current RT guidelines focus on targeting major muscle groups, guidance specific to simplified movement categorization may augment understanding of RT programming and improve uptake and outcomes. Current movement pattern definitions and descriptions lack clarity, accuracy, and consistency. This paper proposes movement definitions and descriptions to be used for RT intervention design and prescription, and includes the following categories: hip, knee, ankle, vertebral column, vertical push, horizontal push, vertical pull, and horizontal pull. These categories are intended to aid clinicians, researchers, and trainers in RT surveillance and RT intervention design for improving vascular complications in type 2 diabetes. Simplified RT program design using these categories may also facilitate greater RT program understanding and adherence for patients.
Introduction
Type 2 diabetes (T2D) is a metabolic condition of impaired insulin uptake and sometimes production (1). From 1980 to 2014, diabetes prevalence increased four-fold from 108 to 422 million adults, and the majority of cases were T2D (2). Increased prevalence is concerning as micro- and macrovascular complications accompany this condition, including retinopathy, neuropathy, and nephropathy (3). Common macrovascular complications include cardiovascular, cerebrovascular, and peripheral vascular disease.
Chronic resistance training (RT) reduces vascular comorbidities and cardiometabolic risk factors in T2D (4–6), and some benefits manifest after a single session (4). Despite these benefits, only 10–30% of adults in the USA, Scotland, Australia, and Finland meet RT public health guidance (7–10). RT is “a category of exercises intended to increase muscular strength; most commonly the applied resistance takes the form of a barbell, dumbbell, weight machine, or simple gravity (bodyweight exercise)” ( (11), p. 166). This form of exercise drives unique structural and metabolic adaptations, including increased muscular strength, power, muscle cross-sectional area, muscle activation, neural drive (12), bone mineral density, basal metabolic rate (13), and anabolic hormone secretion (14).
RT additionally improves endothelial function, hypertension, glycosylated hemoglobin concentrations, blood lipid levels, and body fat % in prediabetes and T2D (4, 15, 16), although these effects vary by race, ethnicity (17), sex (18), and age (19). RT intervention characteristics such as frequency, intensity, and use of single- or multi-joint exercises also influence intervention effectiveness (15). RT protocols often lack key component descriptions such as rest periods, movement speed, implements utilized (e.g., barbell or weight machine) (20–22), and included exercises (23, 24). This heterogeneity across studies makes replication and dosage determination difficult. In order to optimize health benefits for people with T2D, accurate and consistent RT definitions are warranted.
When selecting exercises to include in interventions, a focus on physical function rather than muscle groupings may be beneficial. Qadir et al. (15) found that most RT interventions that reduced cardiometabolic risk in this population primarily incorporated multi-joint exercises. Previous studies using combinations of multi- and single-joint RT improved endothelial function (16, 25), cardiac autonomic function, and inflammation in T2D (25). Furthermore, multi-joint exercises mimic natural movements performed in everyday life better than single-joint isolation exercises.
Activities of Daily Living (ADL) are often listed in exemplar form: moving a table, loading a washing machine, toilet use, and self-hygiene (26). While these activities are understandable in terms of outcome, in a functional context they involve pushing, pulling, bending, and twisting movements. Some research suggests that diabetes impairs real-world physical function by reducing capacity to perform ADL (27). Conversely, RT replicating ADL movement patterns may improve ADL competency (28, 29).
Research is currently underway to test modification of the Muscle-Strengthening Exercise Questionnaire using movement patterns instead of muscle groupings (data not published) (30). Thus, the present paper will explore publicly used nomenclature and proposes movement definitions and descriptions intended to enable uniform understanding and consistent application for RT interventions to reduce cardiovascular comorbidities in T2D.
Issues in RT exercise categories
Training muscles in isolation, using single-joint exercises, is a prominent characteristic of bodybuilding programs as competitors are assessed for muscularity, definition, size, shape, proportion, symmetry, and balance of whole-body development. In the general population, such training is generally performed intending to alter physical appearance by increasing muscle hypertrophy (31). Isolation training appears prominently in public health guidelines. The 2018 Physical Activity Guidelines for Americans (32) recommended performing muscle-strengthening activities (i.e., RT) working all major muscle groups at least twice a week (32). When major muscle groups are defined as the legs, hips, back, abdomen, chest, shoulders, and arms, such presentation may be interpreted as a RT isolation exercise approach. Most of the public can likely identify generic body segments, but the public’s understanding of anatomy is limited (33–35). Additionally, it is unclear if the public can identify exercises specific to body parts or muscle groups. Alarmingly, the vast majority of U.S. physical education teacher education programs do not offer RT principles and methods coursework (36). A similar circumstance exists in medical education (37–40). If two primary sources of health and fitness information are unfamiliar with RT fundamentals, any expectation of the public understanding and applying RT principles and methods to their lives may be unfounded.
It is generally assumed that physical education or sports science graduates will have mastered fitness delivery methods. However, in a study examining the knowledge of RT principles and methods in high school physical education teachers and coaches, neither group demonstrated minimum competencies to design and implement safe RT programs (41). More recently it was reported that less than 18% of teachers took courses in resistance training techniques, weight room safety, and resistance training programming during their Physical Education Teacher Education (42). These findings indicate a fundamental knowledge gap in the primary professionals who are tasked with educating the public on physical literacy. Furthermore, low levels of anatomical knowledge in the public is of concern (33–35), as an inability to identify anatomical structures (e.g., muscles and bones) may hamper the ability of the public to understand RT concepts. Classifying and describing resistance exercises objectively and uniformly may enable more effective conveyance of information from fitness and health professionals to the public.
An example of an exercise often misclassified in effect is the Bent Row (Figure 1 2A, B). Here, the hands grasp a barbell, while the hips flex forward until the vertebral column is at or slightly above parallel to the floor. Once the “bent” position is achieved, the body remains isometrically contracted, and the barbell is pulled up from the floor toward the vertebral column until the bar contacts it at about the level of the xiphoid process of the sternum. It is common to see this exercise described as only affecting the latissimus dorsi, trapezius, and posterior deltoids, as only the arms moving at the shoulder are considered (43). This approach omits the contribution of elbow flexors and ignores the roles of other muscles in providing isometric postural stability and movement control. A system of simple movement categorizations accessible to a general audience may improve RT uptake and outcomes.
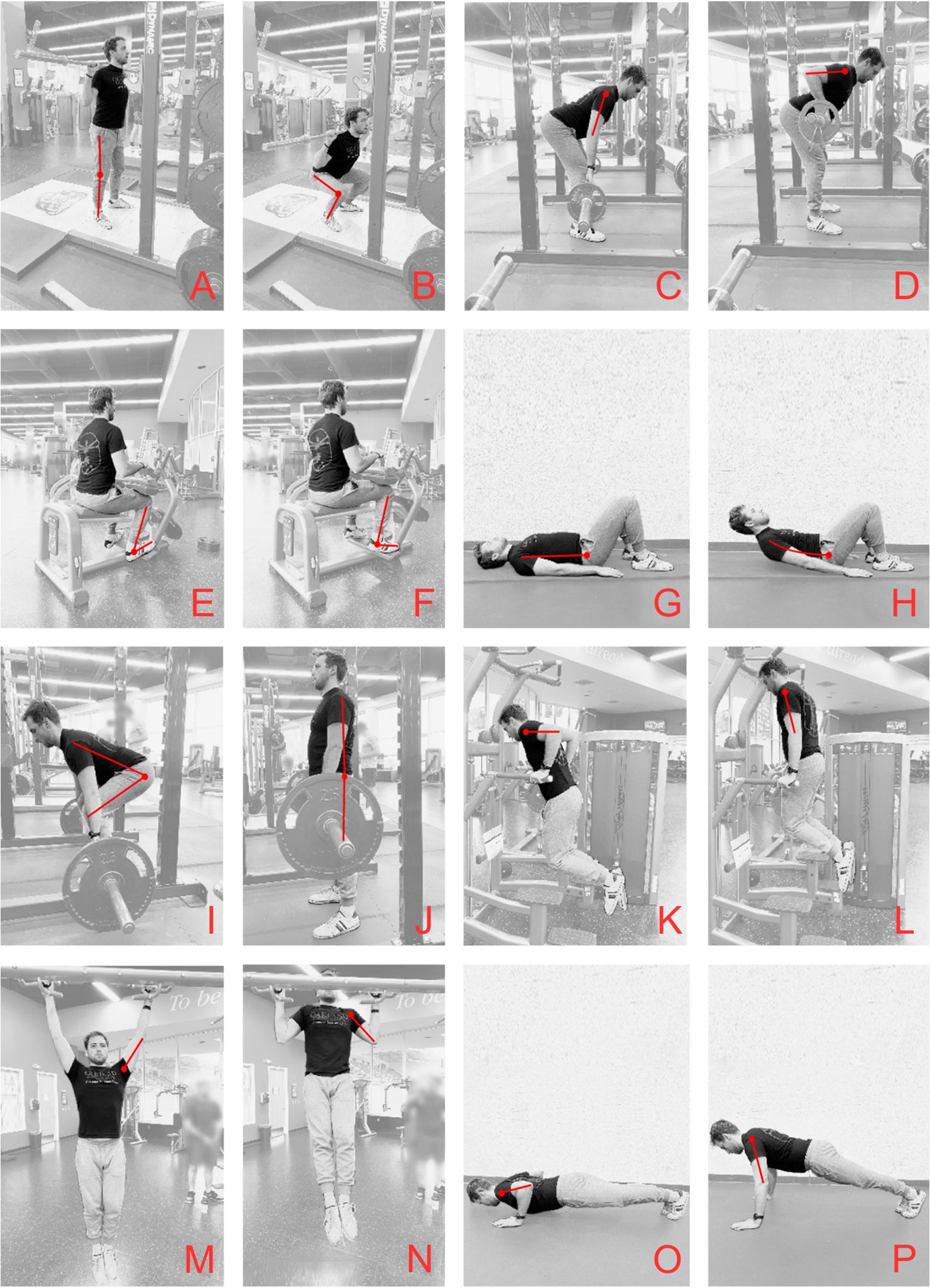
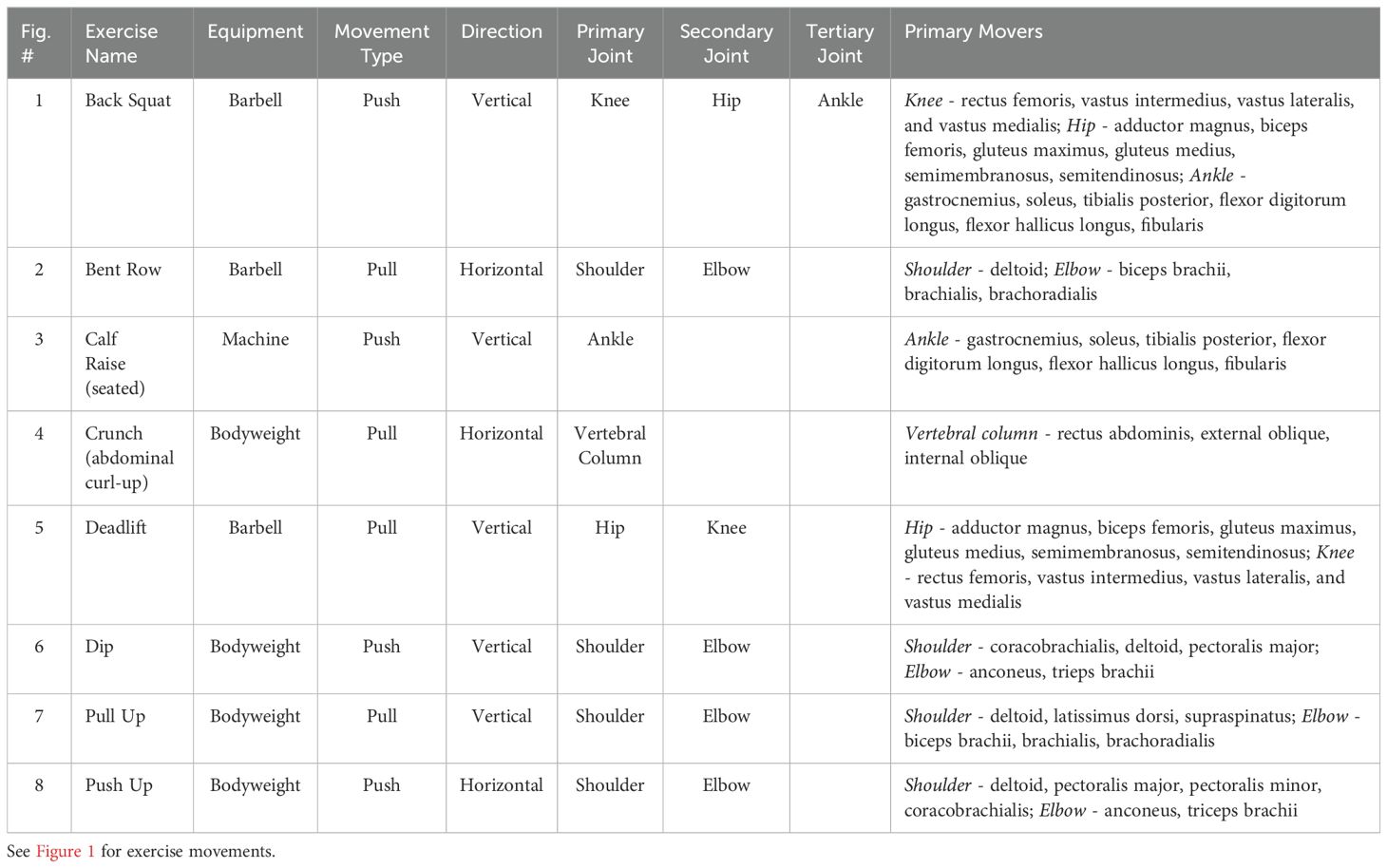
Figure 1. Exercise examples for each movement category; (A) Back Squat start, (B) Back Squat finish, (C) Bent Row start, (D) Bent Row finish, (E) Calf Raise start, (F) Calf Raise finish, (G) Crunch start, (H) Crunch finish, (I) Deadlift start, (J) Deadlift finish, (K) Dip start, (L) Dip finish, (M) Pull Up start, (N) Pull Up finish, (O) Push Up start, (P) Push Up finish. For categoric assignment see Table 1.
Movement occurs when muscles provide force at moveable joints, and basic motor patterns are learned in childhood from formal and informal physical experiences (44). Movement pattern categories currently in use are variable, but generally describe the application of force around the primary joint most moved during an exercise. “Pushing” moves segments away from the center of gravity of the body, while “pulling” moves segments toward the center of gravity (45). Although a push or pull can be generated by any muscled joint of the body, description and categorization of these terms can be confusing. When considering pushing or pulling involving the arms, pushing is generally characterized by elbow extension, while pulling is characterized by elbow flexion. This simplicity becomes inaccurate if used with compound movements.
Over the past two decades, several non-scientists have proposed movement pattern categories for RT exercises (46–48). Push-pull sequencing of exercises is common in RT programs created for athletes (49–51), military personnel (48), and first responders (48, 52, 53). Despite its popularity, objective definitions for these commonly used terms are sparse in the literature (54, 55). Castanheira et al. (55) defined the term, push-pull, as exercises that work non-synergist muscles in the upper body. In 2003, Boyle (47) proposed seven categories for sports performance exercises (1): hinge hip-dominant (2), knee-dominant (3), rotational (4), horizontal push (5), horizontal pull (6), vertical push, and (7) vertical pull movements. In 2018, Mullins (46) proposed three additional categories specific to general fitness exercise movements as follows: stability, gait, and cross-pollination (i.e., combination of movement patterns). Lastly, in 2021, Tumminello (48) proposed eight exercise movement categories for the training of military personnel and first responders (1): jumping and landing (2), throwing and striking (3), locomotion (4), rotation (5), pushing (6), pulling (7), knee bending, and (8) hip hinging. In a clinical setting, Rosenberg et al. (54) categorized movement patterns as (1) push (2), pull (3), hinge (4), squat, and (5) core. All of these proposed categorizations suffer from inconsistency, weak and inaccurate descriptors, gaps in applicability, and lack of consensus.
Commonly, patients with T2D are referred to fitness facilities that are equipped primarily with RT machines (56). RT machines focus on primary movers and minimize recruitment of motor and isometric stabilizing musculature (43). A simple and logical system of categorization and description that is useful for trainers, and understandable by patients, may improve RT prescription quality, uptake, and outcomes.
Movement patterns for public health
Some RT exercises, such as isolation machine exercises, fit into categories intuitively. Other exercises, such as compound exercises, need careful consideration in terms of direction of body or object movement(s), movement planes, and joint(s) moved by active musculature. Every RT movement requires recruitment of specific muscle groups (57), and this specificity makes categorization difficult to create and apply universally as exercises may fit into multiple movement categories in current systems.
Practical movement patterns for RT proposed here include Vertical Push (VPush), Horizontal Push (HPush), Vertical Pull (VPull), and Horizontal Pull (HPull). These patterns occur at the ankle, knee, hip, vertebral column, shoulders, and wrists. Choosing the joint and muscles most dominant in the target exercise (i.e., primary movers) as categorical components, rather than identifying every minor synergist, motor stabilizer, and isometric stabilizer active at every joint, creates a less informationally-dense system that may be easier for patients to understand. Exercise examples for these terms along with primary movement patterns, joints, and muscles involved are presented in Table 1. Images of exemplar exercises are presented in Figure 1.
Hip movements refers to lower body actions directly involving muscles moving the hip joint. The Deadlift (i.e., free weight) and Back Extension (i.e., weight machine) are exercises included in this category. Both exercises are used under the premise that they recruit the gluteals and hamstrings. The machine exercise fits this idea well. However, the Deadlift, while meeting hip movement criteria, carries additional accessory functions. There are a few centimeters of knee extension in the movement along with recruitment of motor and isometric stabilizers (i.e., hip adductors, abductors, and flexors). The Deadlift also invokes isometric vertebral muscle contraction during hip extension and this further affects the posterior muscles attached to the glenohumeral joint and shoulder girdle (58). Thus, while Deadlift prime movers place it in this category, Deadlifts are often included in training for their knee or vertebral column developing capacity. Exercises within this category are single-joint (e.g., Back extension) but may include multi-joint exercises (e.g., Deadlift) with primary movers functioning at the hip.
Knee movements refers to lower body actions directly involving muscles moving the knee joint. The Leg Extension and Squat both involve knee extension, and this is commonly considered the primary joint involved and musculature developed. The Leg Extension fits this concept well, but the Squat involves multiple joints, the hip very profoundly, and the ankle to a lesser degree (59). Isometric contraction of the vertebral musculature adds motor stability and control. Exercises within this category are single-joint (e.g., Leg Extension) and multi-joint (e.g., Squat) with primary movers also at the hip.
Ankle movements refers to lower body actions directly involving muscles moving the ankle joint. Calf Raises are an example of an ankle movement. Ankle movements included in common exercises are plantar- and dorsiflexion. Eversion and inversion are more common in rehabilitative settings (60). While often assumed that exercises in this category will be single joint movements, in every exercise where the patient is standing and there is movement at the knee and hips, ankle muscles are also involved as synergists or stabilizers (61).
Vertebral column movements refers to upper body actions directly involving muscles that move the torso. Exercises in this category are restricted to those acting to move the vertebral column without direct hip and shoulder involvement, the most familiar of which may be the Crunch. Many exercises that are stated to target muscles of the torso may also involve movements of the hips. Such is the case for the Leg Raise, which involves lying supine, flexing the hip, and moving the extended legs upward. The only movement that occurs here is hip flexion via the hip flexors. However, it also requires the isometric contractions of the rectus abdominus to stabilize the torso (62). In such cases, as movement only occurs at the hip, it should be classified as a hip movement.
Vertical Push (VPush) movements are actions applying force to an object that subsequently moves away from the body in an upward or downward direction, relative to the body’s center of gravity and postural alignment. Vertical pushing can occur at almost any joint, and exercises in this category include the Dip (VPush - shoulder), Calf Raise (VPush - ankle), and Back Squat (VPush - knee, hip, and ankle).
Horizontal Push (HPush) movements are actions applying force to an object that subsequently moves away from the body in a forward or rearward direction relative to the body’s center of gravity and postural alignment. Horizontal pushing can occur at almost any joint, and exercises in this category include the Bench Press (HPush - shoulder and elbow), Leg Press (HPush - hip, knee, and elbow), and Push Up (HPush - shoulder and elbow).
Vertical Pull (VPull) movements are actions applying force to an object that subsequently moves in an upward or downward direction toward the body’s center of gravity and postural alignment. Vertical pulling can occur at almost any joint and exercises in this category include the Pull Up (VPull - shoulder and elbow), Upright Row (VPull - shoulder and elbow), and Deadlift (VPull - the hip, knee, and ankle).
Horizontal Pull (HPull) movements are actions applying force to an object which subsequently moves toward the body in a forward or rearward direction relative to the body’s center of gravity and postural alignment. Horizontal pulling occurs at almost any joint and exercises in this category include the Bent Row (HPull - shoulder and elbow) and Leg Curl (HPull - knee).
Discussion
This paper proposes an organization of RT movements for use in public health, specifically for reducing vascular comorbidities in T2D. To ensure that all major muscle groups are trained, public health messaging could include ‘do exercises that push and pull each major joint at least twice a week, with most exercises involving more than one joint.’ Human movement largely occurs in a multi-joint manner. An organized approach to description and categorization can ensure that machine isolation exercises included comprehensively provide whole-body training. However, multi-joint RT exercises that mimic these movements are more likely to improve physical function, increase muscle activation and strength, and, consequently, reduce metabolic stress and injury risk compared to single-joint exercises (63, 64). The descriptors presented here provide a structure ensuring programming balance across body segments and muscle groups. Further, the descriptors may enhance understanding of which exercises to work what body part and for what purpose. This is especially important as previous research shows that a stronger understanding of exercise correlates to improved compliance and adherence (65).
Classifying resistance exercises by movement pattern rather than muscle group may help patients better conceptualize exercise technique and programmatic outcomes compared to naming muscle groups. If an RT program balances pushing and pulling movements, this approach should aid in correcting muscle imbalances and reduce injury risk (66, 67).
Movement pattern classification may improve training status assessment, critical for RT prescription (68). Commonly, training status is assessed by self-report of uninterrupted time that the trainee has been performing RT in years and months. Technique and strength level are additional methods of assessing training status (68, 69). Testing one upper body push, one upper body pull, one squat variation, and one hip hinge movement have been recommended, and categories proposed in the current paper may be preferential (68).
Movement pattern categorization may simplify program design. Movement pattern categorization may facilitate improvement of a specific ADL or understanding of other exercises similar to ADL. Patients/practitioners can use categories to select exercises within the same category to add to the training stimulus, choose replacement exercises per individual needs, or strength can be appropriately balanced in functional outcome.
Populations with T2D require considerations of their pathological status when making exercise selections. For example, when foot ulcers are present, resulting from peripheral neuropathy, non-weight bearing exercise is recommended (70). Use of devices such as a forefoot offloading shoe may complicate standing exercise selection further (71). In these situations, seated machine weights exercises provide less aggravation of lesions, as pressure applied to the feet is not required.
Despite the benefits of movement categorization, limitations exist. First, any system of categorization of movements faces challenges when considering exercises that clearly involve more than one movement pattern and joint. An example is the Snatch (i.e., weightlifting competition lift) includes a modified Deadlift (VPull, hip 1°, knee 2°, ankle 3°), Shrug (VPull, shoulder 1°), and Overhead Squat (VPush, knee 1°, hip 2°, ankle 3°). Categorizing resistance exercises into individual joint movement patterns for health surveillance purposes and exercise prescription may effective with machine-based RT, as the complex nature of many free-weight exercises requires considered placement of some exercises into multiple categories. Another challenge may be variations of an exercise it designated category. For example, the barbell moves vertically in the Bench Press, yet the supine body position on the bench leads to the movement categorized as a horizontal push away from the anterior surface of the torso (HPush, shoulder 1°, elbow 2°). This categorization applies to low positive and negative angles of the Incline and Decline Bench Presses, however, more vertical equipment settings create close resemblances to a VPush. It is tempting to suggest that above a 45° angle setting be considered vertical and less than 45°considered horizontal, but more consideration is needed. Lastly, the forces applied across body weight, free weights, resistance bands, machines, and cables vary substantially, and may change the exercise categorization (72).
When selecting exercises for a RT program and communicating them to patients, using movement types, direction of movement, and utilized joints rather than muscle groups may simplify the programming process and improve patient understanding and adherence. The system presented here may result in improvements in strength, leading to enhanced ADL function, and better vascular health in those suffering from T2D by making RT seem less intimidating.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
EB: Conceptualization, Investigation, Methodology, Project administration, Supervision, Visualization, Writing – original draft, Writing – review & editing. LK: Conceptualization, Investigation, Writing – review & editing, Visualization. KP: Writing – review & editing, Conceptualization, Investigation. AK: Writing – review & editing. JH: Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We would like to thank Christian Maron for serving as our fitness model in the resistance training photos.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
VPush, vertical push; HPush, horizontal push; VPull, vertical pull; HPull, horizontal pull
References
1. Sapra A, Bhandari P. Diabetes. In: StatPearls. StatPearls Publishing, Treasure Island (FL (2024). Available at: http://www.ncbi.nlm.nih.gov/books/NBK551501/.
2. Global report on diabetes (2024). Available online at: https://www.who.int/publications-detail-redirect/9789241565257.
3. Harding JL, Pavkov ME, Magliano DJ, Shaw JE, Gregg EW. Global trends in diabetes complications: a review of current evidence. Diabetologia. (2019) 62:3–16. doi: 10.1007/s00125-018-4711-2
4. Brown EC, Franklin BA, Regensteiner JG, Stewart KJ. Effects of single bout resistance exercise on glucose levels, insulin action, and cardiovascular risk in type 2 diabetes: A narrative review. J. Diabetes Complications. (2020) 34:107610. doi: 10.1016/j.jdiacomp.2020.107610
5. Gholami F, Khaki R, Mirzaei B, Howatson G. Resistance training improves nerve conduction and arterial stiffness in older adults with diabetic distal symmetrical polyneuropathy: A randomized controlled trial. Exp. Gerontol. (2021) 153:111481. doi: 10.1016/j.exger.2021.111481
6. Dos Santos Araujo JE, Nunes Macedo F, Sales Barreto A, Viana dos Santos MR, Antoniolli AR, Quintans-Junior LJ. Effects of resistance and combined training on vascular function in type 2 diabetes: A systematic review of randomized controlled trials. Rev. Diabetes Stud. (2019) 15:16–25. doi: 10.1900/RDS.2019.15.16
7. Bennie JA, Pedisic Z, van Uffelen JGZ, Charity MJ, Harvey JT, Banting LK, et al. Pumping iron in Australia: prevalence, trends and sociodemographic correlates of muscle strengthening activity participation from a national sample of 195,926 adults. PloS One. (2016) 11:e0153225. doi: 10.1371/journal.pone.0153225
8. Bennie JA, Pedisic Z, Suni JH, Tokola K, Husu P, Biddle SJH, et al. Self-reported health-enhancing physical activity recommendation adherence among 64,380 finnish adults. Scand. J. Med. Sci. Sports. (2017) 27:1842–53. doi: 10.1111/sms.12863
9. Strain T, Fitzsimons C, Kelly P, Mutrie N. The forgotten guidelines: cross-sectional analysis of participation in muscle strengthening and balance & co-ordination activities by adults and older adults in Scotland. BMC Public Health. (2016) 16:1108. doi: 10.1186/s12889-016-3774-6
10. Bennie JA, Lee DC, Khan A, Wiesner GH, Bauman AE, Stamatakis E, et al. Muscle-strengthening exercise among 397,423 U.S. Adults: prevalence, correlates, and associations with health conditions. Am. J. Prev. Med. (2018) 55:864–74. doi: 10.1016/j.amepre.2018.07.022
11. Kilgore L. Kilgore academy abridged dictionary for fitness trainers & Coaches: book 1 - fitness concepts and terms Vol. 1. Halfway, MO: Kilgore Academy (2024).
12. Hughes DC, Ellefsen S, Baar K. Adaptations to endurance and strength training. Cold Spring Harb. Perspect. Med. (2018) 8:a029769. doi: 10.1101/cshperspect.a029769
13. Physiological adaptations of skeletal muscle and bone to resistance training and its applications in orthopedics: A review. - Document - Gale OneFile: Health and Medicine (2024). Available online at: https://go-gale-com.huaryu.kl.oakland.edu/ps/i.do?id=GALE%7CA757705816&sid=googleScholar&v=2.1&it=r&linkaccess=abs&issn=09717986&p=HRCA&sw=w&userGroupName=bigbendcc&aty=ip.
14. Kraemer WJ, Ratamess NA. Hormonal responses and adaptations to resistance exercise and training. Sports Med. Auckl NZ. (2005) 35:339–61. doi: 10.2165/00007256-200535040-00004
15. Qadir R, Sculthorpe NF, Todd T, Brown EC. Effectiveness of resistance training and associated program characteristics in patients at risk for type 2 diabetes: a systematic review and meta-analysis. Sports Med. - Open. (2021) 7:38. doi: 10.1186/s40798-021-00321-x
16. Cohen ND, Dunstan DW, Robinson C, Vulikh E, Zimmet PZ, Shaw JE. Improved endothelial function following a 14-month resistance exercise training program in adults with type 2 diabetes. Diabetes Res. Clin. Pract. (2008) 79:405–11. doi: 10.1016/j.diabres.2007.09.020
17. Tarar BI, Knox A, Dean CA, Brown EC. Resistance training responses across race and ethnicity: a narrative review. Ethn Health. (2023) 28(8):1–17. doi: 10.1080/13557858.2023.2212147
18. Roberts BM, Nuckols G, Krieger JW. Sex differences in resistance training: A systematic review and meta-analysis. J. Strength Cond Res. (2020) 34:1448. doi: 10.1519/JSC.0000000000003521
19. Ahtiainen JP, Walker S, Peltonen H, Holviala J, Sillanpää E, Karavirta L, et al. Heterogeneity in resistance training-induced muscle strength and mass responses in men and women of different ages. Age. (2016) 38:10. doi: 10.1007/s11357-015-9870-1
20. Pavlova AV, Shim JSC, Moss R, Maclean C, Brandie D, Mitchell L, et al. Effect of resistance exercise dose components for tendinopathy management: a systematic review with meta-analysis. Br. J. Sports Med. (2023) 57:1327–34. doi: 10.1136/bjsports-2022-105754
21. Wollesen B, Herden M, Lamberti N, Giannaki CD. Defining and reporting exercise intensity in interventions for older adults: a modified Delphi process. Eur. Rev. Aging Phys. Act. (2024) 21:3. doi: 10.1186/s11556-024-00337-8
22. Slade SC, Dionne CE, Underwood M, Buchbinder R. Consensus on exercise reporting template (CERT): explanation and elaboration statement. Br. J. Sports Med. (2016) 50:1428–37. doi: 10.1136/bjsports-2016-096651
23. Huffman KM, Koves TR, Hubal MJ, Abouassi H, Beri N, Bateman LA, et al. Metabolite signatures of exercise training in human skeletal muscle relate to mitochondrial remodelling and cardiometabolic fitness. Diabetologia. (2014) 57:2282–95. doi: 10.1007/s00125-014-3343-4
24. Mager U, Kolehmainen M, de Mello VDF, Schwab U, Laaksonen DE, Rauramaa R, et al. Expression of ghrelin gene in peripheral blood mononuclear cells and plasma ghrelin concentrations in patients with metabolic syndrome. Eur. J. Endocrinol. (2008) 158:499–510. doi: 10.1530/EJE-07-0862
25. Bhati P, Shenoy S, Hussain ME. Exercise training and cardiac autonomic function in type 2 diabetes mellitus: A systematic review. Diabetes Metab. Syndr. Clin. Res. Rev. (2018) 12:69–78. doi: 10.1016/j.dsx.2017.08.015
26. Edemekong PF, Bomgaars DL, Sukumaran S, Schoo C. Activities of daily living. In: StatPearls. StatPearls Publishing, Treasure Island (FL (2024). Available at: http://www.ncbi.nlm.nih.gov/books/NBK470404/.
27. Win MMTM, Fukai K, Nyunt HH, Hyodo Y, Linn KZ. Prevalence of peripheral neuropathy and its impact on activities of daily living in people with type 2 diabetes mellitus. Nurs. Health Sci. (2019) 21:445–53. doi: 10.1111/nhs.12618"10.1111/nhs.12618
28. Adams J, Cline MJ, Hubbard M, McCullough T, Hartman J. A new paradigm for post-cardiac event resistance exercise guidelines. Am. J. Cardiol. (2006) 97:281–6. doi: 10.1016/j.amjcard.2005.08.035
29. Ribeiro AS, Nunes JP, Schoenfeld BJ. Selection of resistance exercises for older individuals: the forgotten variable. Sports Med. (2020) 50:1051–7. doi: 10.1007/s40279-020-01260-5
30. Shakespear-Druery J, Cocker KD, Biddle SJH, Bennie J. Muscle-Strengthening Exercise Questionnaire (MSEQ): an assessment of concurrent validity and test–retest reliability. BMJ Open Sport Exerc Med. (2022) 8:e001225. doi: 10.1136/bmjsem-2021-001225
31. Strong J. The language of bodybuilding. Paragraph. (2003) 26:163–74. doi: 10.3366/para.2003.26.1-2.163
32. U.S. Department of Health and Human Services. Physical activity guidelines for americans. 2nd Edition. Washington, DC: U.S. Department of Health and Human Services (2018).
33. Taylor AM, Diggle P, Wessels Q. What do the public know about anatomy? Anatomy education to the public and the implications. Anat Sci. Educ. (2018) 11:117–23. doi: 10.1002/ase.1746
34. Weinman J, Yusuf G, Berks R, Rayner S, Petrie KJ. How accurate is patients’ anatomical knowledge: a cross-sectional, questionnaire study of six patient groups and a general public sample. BMC Fam Pract. (2009) 10:43. doi: 10.1186/1471-2296-10-43
35. Ramanayake BS, Liyanagoda NE, Dahanayake PK, Hemachandra MAD. Do patients understand medical communication? Patients’ knowledge on anatomical location of organs in human body. (2014). Scientific Research Journal (SCIRJ)
36. Ayers SF, Housner LD. A descriptive analysis of undergraduate PETE programs. J. Teach Phys. Educ. (2008) 27:51–67. doi: 10.1123/jtpe.27.1.51
37. Hernández López M, Puentes Gutiérrez AB, García Bascones M, Fernández García L, Pérez Novales D, Marquina Valero MA. Strength training education for physicians increases its prescription. Rehabilitacion. (2022) 56:274–8. doi: 10.1016/j.rh.2021.10.003
38. Cardinal BJ, Park EA, Kim M, Cardinal MK. If exercise is medicine, where is exercise in medicine? Review of U.S. Medical education curricula for physical activity-related content. J. Phys. Act Health. (2015) 12:1336–43. doi: 10.1123/jpah.2014-0316
39. Thompson WR, Sallis R, Joy E, Jaworski CA, Stuhr RM, Trilk JL. Exercise is medicine. Am. J. Lifestyle Med. (2020) 14:511–23. doi: 10.1177/1559827620912192
40. Tao D, Awan-Scully R, Ash GI, Gu Y, Pei Z, Gao Y, et al. Health policy considerations for combining exercise prescription into noncommunicable diseases treatment: a narrative literature review. Front. Public Health. (2023) 11:1219676/full. doi: 10.3389/fpubh.2023.1219676/full
41. McGladrey BW, Hannon JC, Faigenbaum AD, Shultz BB, Shaw JM. High school physical educators’ and sport coaches’ Knowledge of resistance training principles and methods. J. Strength Cond Res. (2014) 28:1433. doi: 10.1519/JSC.0000000000000265
42. Kern BD, Bellar D, Wilson WJ. Examining the knowledge and training of secondary school physical educators providing strength and conditioning programming (2023). Available online at: https://journals-humankinetics-com.huaryu.kl.oakland.edu/view/journals/jtpe/43/1/article-p102.xml. doi: 10.1123/jtpe.2022-0291
43. Human Kinetics. Essentials of strength training and conditioning 4th edition with HKPropel access (2024). Available online at: https://us.humankinetics.com/products/essentials-of-strength-training-and-conditioning-4th-edition-with-hkpropel-access.
44. Vosniadou S. On the nature of naïve physics. In: Limón M, Mason L, editors. Reconsidering conceptual change: issues in theory and practice. Springer Netherlands, Dordrecht (2002). doi: 10.1007/0-306-47637-1_3
45. Informa Healthcare, Karwowsk W. Pushing and pulling strengths. In: International encyclopedia of ergonomics and human factors - 3 volume set, 2nd ed. Boca Raton: CRC Press (2006).
46. Jr KM. Programming the general population for optimal fitness (2018). Available online at: https://www.nsca.com/education/articles/ptq/programing-the-general-population-for-optimal-fitness10-important-movement-patterns/.
48. NSCA-CPT NT. The 8 main movement patterns – A programming framework for tactical strength and conditioning (2021). Available online at: https://www.nsca.com/education/articles/tsac-report/the-8-main-movement-patterns/.
49. Nevin J, Smith P, Waldron M, Patterson S, Price M, Hunt A, et al. Efficacy of an 8-week concurrent strength and endurance training program on hand cycling performance. J. Strength Cond Res. (2018) 32:1861. doi: 10.1519/JSC.0000000000002569
50. Yildiz S, Pinar S, Gelen E. Effects of 8-week functional vs. Traditional training on athletic performance and functional movement on prepubertal tennis players. J. Strength Cond Res. (2019) 33:651. doi: 10.1519/JSC.0000000000002956
51. Appleby B, Newton RU, Cormie P. Changes in strength over a 2-year period in professional rugby union players. J. Strength Cond Res. (2012) 26:2538. doi: 10.1519/JSC.0b013e31823f8b86
52. Hatfield GL, Lesser IA. Does body size impact muscle recruitment during law enforcement physical control simulator use? Ergonomics. (2020) 63:1551–60. doi: 10.1080/00140139.2020.1808247
53. Mason MR, Heebner NR, Abt JP, Bergstrom HC, Shapiro R, Langford EL, et al. The acute effect of high-intensity resistance training on subsequent firefighter performance. J. Strength Cond Res. (2023) 37:1507. doi: 10.1519/JSC.0000000000004417
54. Rosenberg J, Hyde PN, Yancy WSJ, Ford KM, Champ CE. Quantity of resistance exercise for breast cancer patients: does the dose match the objective? J. Strength Cond Res. (2021) 35:1467. doi: 10.1519/JSC.0000000000003996
55. Castanheira RPM, Ferreira-Junior JB, Celes RS, Rocha-Junior VA, Cadore EL, Izquierdo M, et al. Effects of synergist vs. NonSynergist split resistance training routines on acute neuromuscular performance in resistance-trained men. J. Strength Cond Res. (2017) 31:3482. doi: 10.1519/JSC.0000000000001762
56. Morgan F, Battersby A, Weightman AL, Searchfield L, Turley R, Morgan H, et al. Adherence to exercise referral schemes by participants – what do providers and commissioners need to know? A systematic review of barriers and facilitators. BMC Public Health. (2016) 16:227. doi: 10.1186/s12889-016-2882-7
57. Manual of structural kinesiology (2020). Available online at: https://www.mheducation.com/highered/product/manual-structural-kinesiology-floyd/M9781260237757.html.
58. Martín-Fuentes I, Oliva-Lozano JM, Muyor JM. Electromyographic activity in deadlift exercise and its variants. A systematic review. PloS One. (2020) 15:e0229507. doi: 10.1371/journal.pone.0229507
59. Schoenfeld BJ. Squatting kinematics and kinetics and their application to exercise performance. J. Strength Cond Res. (2010) 24:3497. doi: 10.1519/JSC.0b013e3181bac2d7
60. Postle K, Pak D, Smith TO. Effectiveness of proprioceptive exercises for ankle ligament injury in adults: A systematic literature and meta-analysis. Man Ther. (2012) 17:285–91. doi: 10.1016/j.math.2012.02.016
61. Nalam V, Adjei E, Lee H. Quantification and modeling of ankle stiffness during standing balance. IEEE Trans. BioMed. Eng. (2021) 68:1828–37. doi: 10.1109/TBME.2020.3023328
62. Monfort-Pañego M, Vera-García FJ, Sánchez-Zuriaga D, Sarti-Martínez MÁ. Electromyographic studies in abdominal exercises: A literature synthesis. J. Manipulative Physiol. Ther. (2009) 32:232–44. doi: 10.1016/j.jmpt.2009.02.007
63. American College of Sports Medicine. American College of Sports Medicine position stand. Progression models in resistance training for healthy adults. Med. Sci. Sports Exerc. (2009) 41:687–708. doi: 10.1249/MSS.0b013e3181915670
64. Paoli A, Gentil P, Moro T, Marcolin G, Bianco A. Resistance Training with Single vs. Multi-joint Exercises at Equal Total Load Volume: Effects on Body Composition, Cardiorespiratory Fitness, and Muscle Strength. Front. Physiol. (2017) 8:1105. doi: 10.3389/fphys.2017.01105
65. Zhu Y, Cheng K, Wang H, Xu Z, Zhang R, Cheng W, et al. Exercise adherence and compliance and its related factors among elderly patients with type 2 diabetes in China: A cross-sectional study. Patient Prefer Adherence. (2022) 16:3329–39. doi: 10.2147/PPA.S374120
66. Baker DG, Newton RU. An analysis of the ratio and relationship between upper body pressing and pulling strength. J. Strength Cond Res. (2004) 18:594. doi: 10.1519/R-12382.1
67. Kolber MJ, Beekhuizen KS, Cheng MSS, Hellman MA. Shoulder injuries attributed to resistance training: A brief review. J. Strength Cond Res. (2010) 24:1696. doi: 10.1519/JSC.0b013e3181dc4330
68. Santos Junior ERT, de Salles BF, Dias I, Ribeiro AS, Simão R, Willardson JM. Classification and determination model of resistance training status. Strength Cond J. (2021) 43:77. doi: 10.1519/SSC.0000000000000627
69. Kritz M, Cronin J, Hume P. Screening the upper-body push and pull patterns using body weight exercises. Strength Cond J. (2010) 32:72. doi: 10.1519/SSC.0b013e3181df5cfe
70. Tran MM, Haley MN. Does exercise improve healing of diabetic foot ulcers? A systematic review. J. Foot Ankle Res. (2021) 14:19. doi: 10.1186/s13047-021-00456-w
71. Bus SA, Armstrong DG, Gooday C, Jarl G, Caravaggi C, Viswanathan V, et al. Guidelines on offloading foot ulcers in persons with diabetes (IWGDF 2019 update). Diabetes Metab. Res. Rev. (2020) 36:e3274. doi: 10.1002/dmrr.3274
Keywords: diabetes mellitus, type 2, resistance training, health communication, activities of daily living, measurement, public health, health education
Citation: Brown EC, Kilgore LJ, Pierce K, Knox A and Haworth JL (2024) Movement pattern definitions for resistance training behavior measurement in diabetes. Front. Clin. Diabetes Healthc. 5:1447595. doi: 10.3389/fcdhc.2024.1447595
Received: 11 June 2024; Accepted: 29 July 2024;
Published: 27 August 2024.
Edited by:
Yun Shen, Pennington Biomedical Research Center, United StatesReviewed by:
Jiayan Zhang, University of California, Los Angeles, United StatesFei Shao, Capital Medical University, China
Yi Mu, ClinChoice Inc., United States
Copyright © 2024 Brown, Kilgore, Pierce, Knox and Haworth. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Elise C. Brown, ZWxpc2Vicm93bkBvYWtsYW5kLmVkdQ==
 Elise C. Brown
Elise C. Brown Lon J. Kilgore2
Lon J. Kilgore2 Kyle Pierce
Kyle Pierce Allan Knox
Allan Knox Joshua L. Haworth
Joshua L. Haworth