- Cambridge Centre for Sport and Exercise Sciences, Anglia Ruskin University, Cambridge, United Kingdom
Introduction: Increased physical activity is recommended as a cost-effective measure to tackle long-term management of people with diabetes, but research on interventions lacks consistency in terms of effective duration and modality.
Methods: The aim of this study was to evaluate expert consensus on exercise and physical activity prescription via a three-round Delphi study conducted with 45 UK-based health and fitness professionals experienced in prescribing exercise or physical activity to people with diabetes.
Results: The majority of items put forward to the panel reached consensus with 70% or above voting these items as important, but the details of the type, duration and/or modality of exercise or physical activity prescription within these items often contradicted each other, suggesting that patients are receiving inconsistent advice. The range of different exercise prescription found in this study suggests that patients are being given inconsistent and potentially confusing advice, which may affect their participation in exercise and long-term lifestyle change.
Conclusion: More consistent promotion of advice from healthcare and fitness professionals may help with increasing physical activity in this participant group and achieving long term behavior change, reducing patient symptoms as well as reducing the cost to the National Health Service (NHS).
1 Introduction
Diabetes affects 4.7 million people in the UK (1) and costs the NHS approximately £10 billion per year (2). Diabetes is recognized as a global epidemic (3) and is increasing year on year (4).
Increases in exercise and physical activity are commonly used in people with type 2 diabetes as an initial method for those newly diagnosed (5), in addition to maintenance and control of symptoms (3),and also have notable health benefits for people with type 1 diabetes (6). Yet despite this intervention being cost effective and potentially easy to implement, there is a lack of consensus in appropriate prescription of physical activity or exercise for patients with diabetes, and research on exercise interventions lacks consistency in terms of exercise modality and duration (3, 7). While patients may be encouraged to be more active by their healthcare provider, detailed and condition-specific advice to support this is limited (8) which may lead to ineffective prescription of exercise and reduce the likelihood of the patient making long-term lifestyle changes. In addition to having a limited impact on the progression of the condition, this also implies an associated cost in terms of medication and health care for the long-term management of the patient with diabetes, as well as potentially limiting their quality of life (3).
The aims of this research are to evaluate the goals and outcomes for providing exercise interventions for people with diabetes, and to establish which type of intervention(s) is considered most beneficial.
2 Methods
2.1 Rationale
A Delphi study is a method for attempting to obtain consensus between experts and stakeholders using a series of ‘rounds’ of questions. Delphi studies gain information from a wide range of stakeholders in an iterative and anonymous way (9).
People with diabetes may be provided with physical activity recommendations from pre-diagnosis through to managing advanced symptoms such as peripheral neuropathy, by healthcare professionals as well as fitness professionals, so a Delphi study to attempt to establish consensus within this range of professions is appropriate to gather opinion from a diverse group.
2.2 Study design and development
Informed consent was obtained prior to participation, and ethical approval was granted by Anglia Ruskin University research ethics panel. A three-round approach was adopted as this is considered optimal to generate consensus (10). The surveys were delivered online (www.onlinesurveys.ac.uk) with links sent to participants via email, and data was gathered between April and September 2021.
This study has been reported considering the methodological considerations presented in the CREDES checklist (11) which is included in the Supplementary Material.
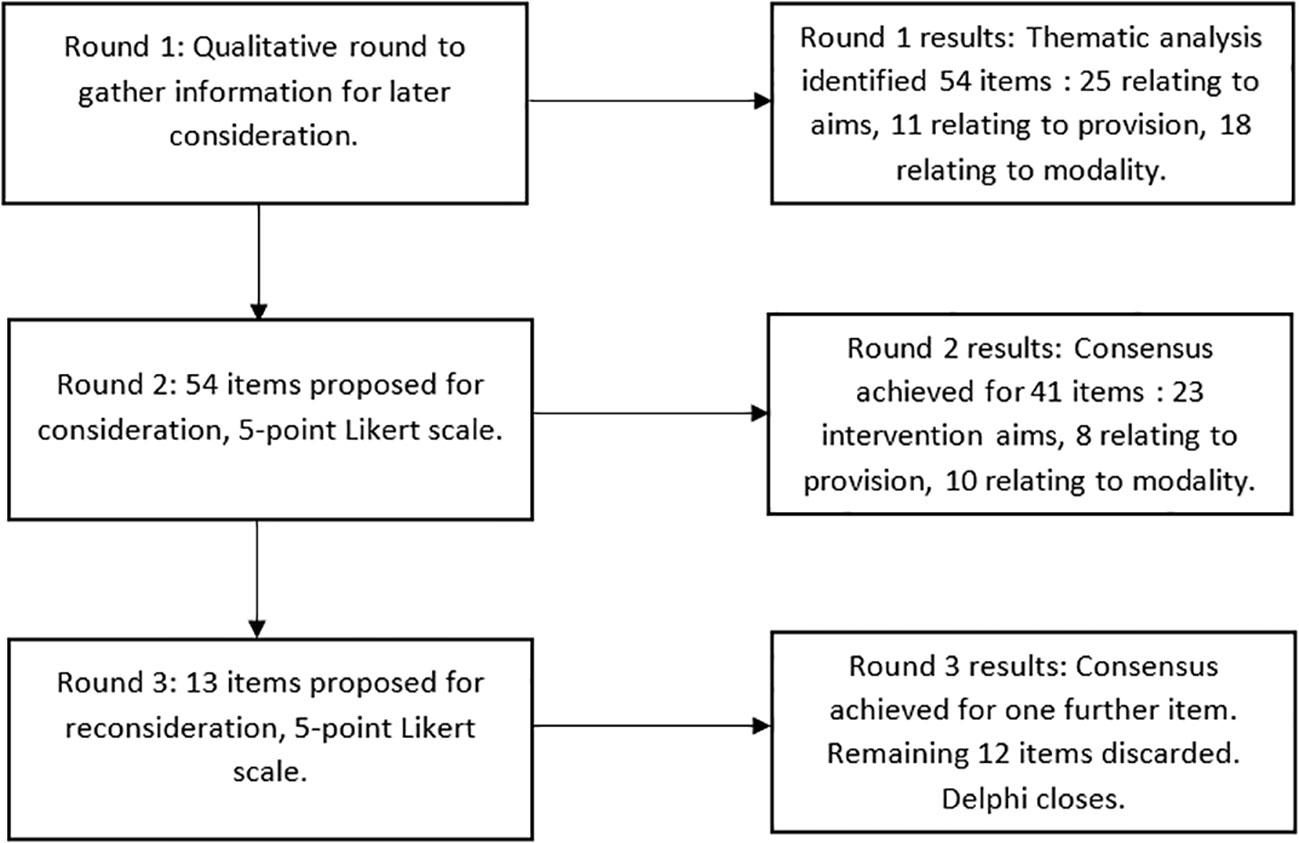
2.3 Qualitative round
A classical approach was used for the first round of the Delphi study. As previously noted, research on exercise interventions in people with diabetes lacks clear consensus, so using a literature review to establish the initial topics would be likely to miss key factors from the participants’ professional experience. To ensure that this was fully represented, free-text responses were gathered on the aims of intervention and type of exercise that would be most appropriate (12). In addition, participants were asked for any general comments. These responses were then collated following an inductive thematic analysis (13) to identify key themes from the panel to present for consensus.
All suggestions were retained to ensure a breadth of response and to reduce bias due to over representation of any specific group. Specific themes for future rounds were kept in the participants own words where possible to prevent ambiguity or confusion, and to help with readability for the participants of these questions in future rounds.
2.4 Quantitative rounds
Each survey was pilot tested using both healthcare and fitness professionals to improve the structure of the survey and to ensure that the statements were understandable by the target audience. As a result of this pilot testing, a ‘Don’t know’ option was added to each item to account for various levels of experience and technical knowledge that may exist between different professions. This also prevented any attrition due to the participants perceived lack of knowledge or due to more dominant individuals (14). During each survey, participants were encouraged to add comments if they wanted to revise the subsequent questions in later rounds to avoid any ambiguity.
The second round presented the themes established in the first round with a five-item Likert scale to rate the perceived importance of each aspect. Consensus was defined at 70% of all participants stating ‘Strongly Agree’ or ‘Agree’, which is consistent with other Delphi studies (15).
Any items that had not reached consensus following the second round were presented to the participants again in round three, alongside a summary of how previous voting had rated each aspect to allow each participant to consider the overall view before providing a new rating (16). Previous voting was presented in simple percentage values so that participants did not need any specific knowledge to interpret any measures of central tendency or variance, making this accessible and easy to understand (17). If consensus for an item was already achieved in round two, then this item was removed from rescoring. Participants were blinded to each other’s responses other than in this collective summary to reduce any bias (15).
Participants were given six weeks to complete each round, and regular reminders were sent via email to encourage ongoing participation. The estimated time to complete each round was 15 minutes for round one, and 10 minutes for rounds two and three. There were no incentives provided for participation. All participants that took part in the original round were asked to complete subsequent rounds to attempt to gain a complete reflection from the original panel and to avoid invalid consensus due to drop out or attrition (18).
2.5 Expert panel
Participants were included if they were UK-based healthcare or exercise professionals that considered themselves experienced in prescribing exercise interventions for people with diabetes. Participants were purposively sampled to ensure a range of different experience on the panel, and included physiotherapists, podiatrists, yoga teachers, GP referral exercise instructors, endocrinology consultants and diabetes specialist nurses to gain a wide representation across a number of specialist areas (16). Recruitment of panelists was done via social media, personal contacts and using snowball sampling to increase the diversity of the included sample population (19).
No limitations were placed on what level of qualification or years of experience would denote an ‘expert’ to ensure that anyone with any relevant contribution could participate (20). The choice to include both healthcare and fitness professionals was made to ensure that intervention advice given early in diagnosis (for example via GPs or practice nurses) was included rather than just considering those patients that are advised via physiotherapy or referral interventions (21). This breadth of participant roles ensures advice at each stage of diagnosis and treatment is represented in the panel where possible. Participants were limited to UK-practicing professionals to limit any impact of discrepancy in healthcare that may exist in other countries, and to ensure consistency of responses.
It has been suggested that a sample size of 12 is valid to ensure consensus within a Delphi study, with larger sample sizes leading to diminishing returns (22). Attrition within Delphi studies has been found to be variable with as low as 45% response rates recorded in some studies (23). This level of attrition was also expected to be impacted by the COVID pandemic. An initial sample size of 45 participants was selected for use in this study, to allow for a comparable sample to previous Delphi studies, whilst anticipating the possibility of 50% attrition in later rounds (22). The responses of both healthcare and fitness professionals were monitored to ensure that the participation of each group remained consistent, and to reduce attrition bias if those with minority opinions withdrew from the study (23).
3 Results
3.1 Participant demographics
Of the 45 participants recruited, thirty provided demographic information. The majority of participants in the study were female (77%). In addition, most of the participants that offered demographic information were educated to degree standard or above (67% of fitness professionals, 81% of healthcare professionals). In each round there was a consistent split between healthcare and fitness professionals, which suggests that the results are appropriately representative of each sector.
3.2 Attrition
Of the 45 participants that contributed to the initial round, 26 (58%) agreed to participate in further rounds. Participants did not always provide a reason for drop out, but the ongoing COVID situation in the UK during the time that the surveys were open accounted for some attrition due to redeployment of healthcare and fitness professionals resulting from lockdown and the vaccine rollout. Of these 26 participants, 21 participated in round 2 (47%) and 19 in round 3 (42%).
3.3 Survey development
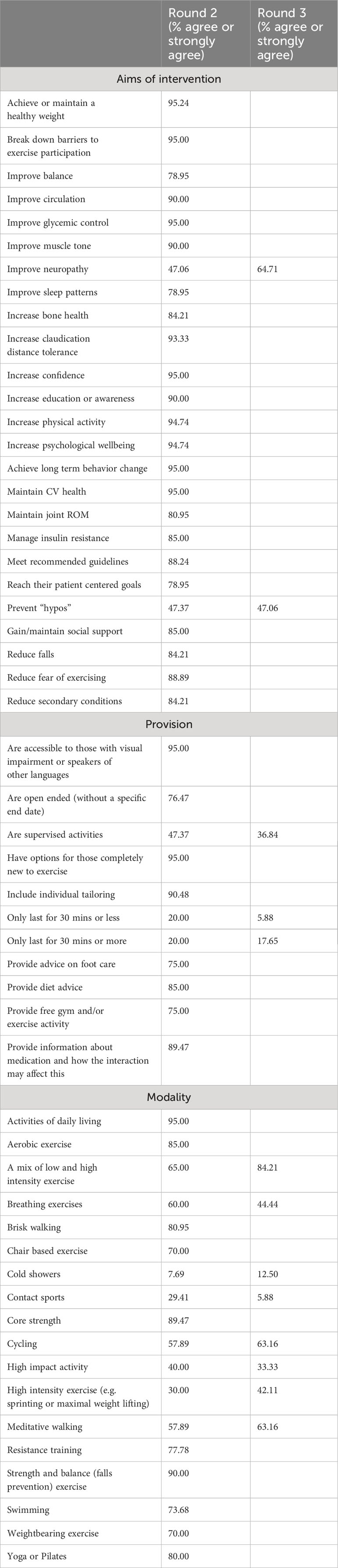
An inductive thematic analysis of the free text responses resulted in 25 statements relating to the goals and aims of exercise interventions, 11 statements relating to provision (for example statements on cost or accompanying services) and 18 statements on the exercise modality. These statements can be found in Table 1. These statements were all presented in the surveys in alphabetical order to avoid any leading questions or biased responses based on the order in which this was viewed by participants. In addition, healthcare professionals are less motivated to respond to surveys where clinical items dominated (23), so using alphabetical order ensured that these were potentially spread throughout the presented options. Participants could respond with ‘don’t know’ in each case if they were unsure or the concept was outside their scope of practice or experience.
3.4 Round 2 results
In round 2, the majority of items (89%, n=16) relating to goals and aims reached the 70% consensus limit. No items were removed, revised or added as a result of the participants’ comments. The two items that failed to reach the 70% consensus level were the aim of the intervention to improve neuropathy and to prevent “hypos” (hypoglycemia or low blood sugar) both achieving 47% consensus.
Within the section on provision, consensus was not achieved when considering whether activities should be supervised (47% agree or strongly agree) and when considering duration. Within the qualitative round, there was a difference of opinion on duration with some participants stating that only less than 30 minutes duration was appropriate, while others stated it had to be over 30 minutes to be effective, so both options were presented in round 2 to attempt to achieve consensus. In each case, most participants stated ‘Neither agree nor disagree’.
When considering exercise modality, the majority of participants agreed that both aerobic (85%) and resistance exercise (78%) were important activities for a person with diabetes. In addition, some specific exercise modalities such as swimming, yoga and Pilates, brisk walking, core strength and strength and balance (falls prevention) exercises also reached consensus from the panel. Eight other modalities failed to reach the prescribed consensus level and were therefore presented to the panel again in round 3.
3.5 Round 3 results
One item, to include a mix of high and low impact activity, reached consensus following round 3. The remaining items were discarded at this point due to not reaching consensus.
The progression through the different rounds and consensus reached is presented in Figure 1.
The statements and responses from each round are presented in Table 1.
4 Discussion
The aim of this study was to evaluate the level of consensus in exercise prescription for people with diabetes. Previous evidence suggested that people with diabetes may struggle to get reliable recommendations from their healthcare professionals (24). In this study, we gathered data about the exercise and physical activity prescription within healthcare and fitness settings in the UK to show specific similarities or differences in practice. Although most of the items achieved consensus, these are often contradictory and include many different modalities. This supports the aims of the intervention as being patient-led and tailored, as different exercise modalities may be appropriate at different stages of the diagnosis.
Despite finding a lack of consistent recommendation between health and fitness professionals in providing advice and exercise prescription, the use of physical activity to manage diabetes symptoms and improve the overall health of people with diabetes is recommended as part of a multifactorial approach to treating the condition (25). In particular the American College of Sports Medicine have recently adapted their recommendations for people with diabetes to specifically include physical activity, focusing on reducing sedentary time and moving more rather than advocating participation in planned, structured exercise (26). This is especially important in managing diabetes due to a high level of inactivity (27) with this patient population being disproportionately sedentary (28). While healthcare professionals may be familiar with providing general diet and medication advice, they may lack confidence when promoting physical activity and exercise (29).
Of the original 25 items presented in round 2 to establish the aims of the interventions, the majority reached consensus. Where consensus was not achieved this may be a lack of shared knowledge and understanding within the participants, as preventing hypoglycemia may not be a concern for those patients prescribed metformin, for example, and it may not be possible to ‘improve neuropathy’ rather than alleviate the symptoms (30).
When considering aspects of provision that could be useful, consensus was achieved on most options that related to increasing accessibility, such as reduced cost and options for those new to exercise. The lack of consensus on duration of activity, with no specific time for activity being preferred more than others may relate to the aim for a ‘person centered’ approach, with some durations being more appropriate for those new to exercise or older, and others being more applicable to other demographics (31). The need for supervised activity did not reach consensus, which may relate to the prescription of general physical activity rather than exercise interventions. However, a recent study has suggested that the presence of an instructor caused increased adherence and long-term behavior change in overweight adults (32) so this may be an area requiring further consideration.
When selecting an expert panel for the Delphi study, any professional with experience of prescribing exercise or physical activity were included, as this would represent a range of ability and knowledge that could contribute to our attempts to reach consensus. However, professionals within this group may see people with diabetes at different stages of their condition. As mentioned previously, nurses are likely to advise patients with diabetes from diagnosis onwards, whereas physiotherapists may not become involved until patients are referred with comorbidities (21). When considering interventions, cost also becomes a factor with healthcare professionals providing their services for free via the NHS, whereas a personal trainer is associated with an additional cost that may not be accessible. Similarly, there is an additional cost associated with yoga teachers and gym instructors represented on the panel, which may influence their recommendations by needing to provide ‘value for money’ with specific exercise prescription. This difference of opinion between professionals that a person with diabetes may approach for advice is inevitably confusing and frustrating (24) and may discourage patients from becoming more active.
The lack of identification of a small group of preferred exercise modality found in this study is supported by the aims of the interventions provided by the participants, with some of the additional free-text comments suggesting that the type of exercise intervention is less important than creating an overall long-term behavior change and ongoing increased activity. While some participants were very specific in their recommendations and content, this was not the case for the whole cohort. One of the key ideas mentioned in the first round was the idea of tailored, patient specific interventions which would override the need for a “one-size-fits-all” diabetes intervention. Diabetes affects a wide range of ages, and this can also affect the appropriateness of prescribed interventions. In addition, comorbidities and complications as a result of having diabetes can also restrict the interventions that could be considered appropriate. Although advocating long term behavior change as an important factor, it is not clear how this will be delivered in practice, with available schemes such as exercise referral lacking clear focus on behavior change (33), and practitioners lacking both leadership and self-awareness to deliver interventions supporting behavior change (34). While compliance with recommended levels of physical activity is a factor in managing long term change (35) ensuring this is achieved in practice is problematic. In particular, structured provision only provides marginal benefit over other interventions (such as providing basic advice) (36) supporting the overall emphasis on unstructured physical activity via activities of daily living found within this Delphi study. This is also supported by recent advice from the ACSM advocating reducing sedentary behavior to manage symptoms and slow progression of diabetes (26).
4.1 Strengths and limitations
A key strength of this research is the breadth of participant experience within the expert panel, to ensure a diverse range of opinion was gathered to attempt to achieve consensus. Despite attrition, an appropriately sized panel was retained for all three rounds.
Due to recruitment being via social media and snowballing, there may be some sampling bias due to the participants already having an interest in non-medical interventions to treat people with diabetes. In addition, due to the constructivist nature of Delphi studies (11) and the lack of consistency and consensus within existing literature it is possible that this study contains information that is not present in existing literature, or that existing literature presents features not considered in the results of this study.
4.2 Clinical implications
The lack of consistent preference for exercise aim and modality found in this study suggests that exercise prescription may be inconsistent, and the lack of clear recommendations may discourage patients to become more active. Lack of knowledge or experience in exercise prescription can be overcome by providing general physical activity advice, and signposting to relevant resources such as the ACSM statement (26) and Diabetes UK resources (37). In this way, clear, unambiguous guidelines from both fitness and health professionals can encourage people with diabetes to make long term changes to their health behavior, managing their condition and reducing cost to the National Health Service.
5 Conclusion
While the benefits of increased physical activity within this population group are widely advocated, the current advice provided may be confusing and contradictory. The large amount of consensus on different intervention methods achieved in this study supports this, and more research is required on the consistent and specific promotion of physical activity advice from healthcare and fitness professionals and how to achieve long term behavior change in this participant group.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by School of Psychology and Sport Sciences ethics committee at Anglia Ruskin University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
CS: Conceptualization, Formal analysis, Investigation, Methodology, Validation, Visualization, Writing – original draft. FC: Writing – review & editing. MAT: Writing – review & editing. AM: Conceptualization, Methodology, Supervision, Visualization, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcdhc.2023.1278597/full#supplementary-material
References
1. Diabetes UK. Number of people with diabetes reaches 4.7 million (2019). Available at: https://www.diabetes.org.uk/about_us/news/new-stats-people-living-with-diabetes (Accessed 1st March 2022).
2. Williams R, Karuranga S, Malanda B, Saeedi P, Basit A, Besançon S, et al. Global and regional estimates and projections of diabetes-related health expenditure: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract (2020) 162(5):108072. doi: 10.1016/j.diabres.2020.108072
3. Shawahna R, Batta A, Asa’ad M, Jomaah M, Abdelhaq I, et al. Exercise as a complementary medicine intervention in type 2 diabetes mellitus: A systematic review with narrative and qualitative synthesis of evidence. Diabetes Metab Syndr (2021) 15(1):273–86. doi: 10.1016/j.dsx.2021.01.008
4. Tabish SA. Is diabetes becoming the biggest epidemic of the twenty-first century? Int. J. Health Sci (2007) 1(2):V–VIII.
5. Kirwan JP, Sacks J, Nieuwoudt S. The essential role of exercise in the management of type 2 diabetes. Cleve Clin J Med (2017) 84(7 Suppl 1):S15–21. doi: 10.3949/ccjm.84.s1.03
6. Colberg SR, Laan R, Dassau E, Kerr D. Physical activity and type 1 diabetes: time for a rewire? J. Diabetes Sci Technol (2015) 9(3):609–18. doi: 10.1177/1932296814566231
7. Thomas D, Elliot EJ, Naughton GA. Exercise for type 2 diabetes mellitus. Cochrane Database Syst Rev (2006) 3. doi: 10.1002/14651858.CD002968.pub2
8. Vas PRJ, Pafili K, Papanas N. Exercise to improve diabetic peripheral neuropathy: An additional option? Clin Neurophysiol (2018) 48(4):191–3. doi: 10.1016/j.neucli.2018.05.001
9. Schmaltz U, Spinler S, Ringbeck J. Lessons learned from a two-round Delphi-based scenario study. MethodsX (2021) 8. doi: 10.1016/j.mex.2020.101179
11. Jünger S, Payne SA, Brine J, Radbruch L, Brearley SG. Guidance on Conducting and REporting DElphi Studies (CREDES) in palliative care: Recommendations based on a methodological systematic review. Palliat Med (2017) 31(8):684–706. doi: 10.1177/0269216317690685
12. Riiskjær E, Ammentorp J, Kofoed P-E. The value of open-ended questions in surveys on patient experience: number of comments and perceived usefulness from a hospital perspective. Int J Qual Health Care (2012) 24:509–16. doi: 10.1093/intqhc/mzs039
14. Hall DA, Smith H, Heffernan E, Fackrell K, Core Outcome Measures in Tinnitus International Delphi (COMiT’ID) Research Steering Group, et al. Recruiting and retaining participants in e-Delphi surveys for core outcome set development: Evaluating the COMiT’ID study. PloS One (2018) 13(7):e0201378. doi: 10.1371/journal.pone.0201378
15. Vernon W. The Delphi technique: A review. Int J Ther Rehabil (2013) 16(2). doi: 10.12968/ijtr.2009.16.2.38892
16. Humphrey-Murto S, de Wit M. The Delphi method-more research please. J Clin Epidemiol (2018) 106:136–9. doi: 10.1016/j.jclinepi.2018.10.011
17. Keeney S, Hasson F, McKenna H. Consulting the oracle: ten lessons from using the Delphi technique in nursing research. J Advanced Nurs (2006) 53(2):205–12. doi: 10.1111/j.1365-2648.2006.03716.x
18. Boel A, Navarro-Compán V, Landewé R, van der Heijde D. Two different invitation approaches for consecutive rounds of a Delphi survey led to comparable final outcome. J Clin Epidemiol (2021) 129:31–9. doi: 10.1016/j.jclinepi.2020.09.034
19. Morgan DL. Snowball sampling. In: Given LM, editor. The SAGE Encyclopedia of Qualitative Research Methods. Los Angeles: SAGE Publications (2018).
20. Mullen PM. Delphi: myths and reality. J. Health Organ. Manage (2003) 17(1):37–52. doi: 10.1108/14777260310469319
21. National Institute for Health and Care Excellence. Type 2 diabetes in adults: management (2022). Available at: https://www.nice.org.uk/guidance/ng28 (Accessed 1st March 2022).
22. Murphy MK, Black NA, Lamping DL, McKee CM, Sanderson CFB, Askham J, et al. Consensus development methods, and their use in clinical guideline development. Health Technol Assess (1998) 2(3):1–88. doi: 10.3310/hta2030
23. Gargon E, Crew R, Burnsid G, Williamson PR. Higher number of items associated with significantly lower response rates in COS Delphi surveys. J Clin Epidemiol (2019) 108:110–20. doi: 10.1016/j.jclinepi.2018.12.010
24. Kime N, Pringle A. Physical activity and healthcare professionals: a cornerstone of diabetes care? Perspect Public Health (2019) 139(2). doi: 10.1177/1757913918823430
25. Colberg S, Sigal R, Yardley J, Riddell MC, Dunstan DW, Dempsey PC, et al. Physical activity/exercise and diabetes: A position statement of the American diabetes association. Diabetes Care (2016) 39(11):2065–79. doi: 10.2337/dc16-1728
26. Kanaley J, Colberg S, Corcoran M, Malin SK, Rodriguez NR. Exercise/physical activity in individuals with type 2 diabetes: A consensus statement from the American college of sports medicine. Med Sci Sports Exercise (2022) 54(2):353–68. doi: 10.1249/MSS.0000000000002800
27. Abushamat LA, McClatchey PM, Scalzo RL, et al. The role of exercise in diabetes, in: “Endotext” (2019). Available at: https://www.ncbi.nlm.nih.gov/sites/books/NBK549946/ (Accessed 1st March 2022).
28. Kennerly A, Kirk A. Physical activity and sedentary behaviour of adults with type 2 diabetes: a systematic review. Pract Diabetes (2018) 35(3):86–9. doi: 10.1002/pdi.2169
29. Din NU, Moore GF, Murphy S, Wilkinson C, Williams NH. Health professionals’ perspectives on exercise referral and physical activity promotion in primary care: Findings from a process evaluation of the National Exercise Referral Scheme in Wales. Health Educ J (2015) 74(6):743–57. doi: 10.1177/0017896914559785
30. Dobson JL, McMillan J, Li L. Benefits of exercise intervention in reducing neuropathic pain. Front Cell Neurosci (2014) 8(102). doi: 10.3389/fncel.2014.00102
31. Izquierdo M, Merchant RA, Morley JE, Anker SD, Aprahamian I, Arai H, et al. International exercise recommendations in older adults (ICFSR): expert consensus guidelines. J Nutr Health Aging (2021) 25:824–53. doi: 10.1007/s12603-021-1665-8
32. Muollo V, Rossi AP, Milanese C, Zamboni M, Rosa R, Schena F, et al. Prolonged unsupervised Nordic walking and walking exercise following six months of supervision in adults with overweight and obesity: A randomised clinical trial. Nutr Metab Cardiovasc Dis (2021) 31(4):1247–56. doi: 10.1016/j.numecd.2020.12.012
33. Campbell F, Holmes M, Everson-Hock E, Davis S, Buckley Woods H, Anokye N, et al. A systematic review and economic evaluation of exercise referral schemes in primary care: a short report. Health Technol Assess (2015) 19(60):1–110. doi: 10.3310/hta19600
34. Downey J, Shearn K, Brown N, Wadey R, Breckon J. Behaviour change practices in exercise referral schemes: developing realist programme theory of implementation. BMC Health Serv Res (2021) 21(335). doi: 10.1186/s12913-021-06349-9
35. Thomas N, Alder E, Leese G. Barriers to physical activity in patients with diabetes. J Postgrad Med (2004) 80:287–91. doi: 10.1136/pgmj.2003.010553
36. National Institute for Health and Care Excellence. Physical activity: exercise referral schemes (2014). Available at: https://www.nice.org.uk/guidance/PH54/ (Accessed 1st March 2022).
37. Diabetes UK. Diabetes and Exercise (2022). Available at: https://www.diabetes.org.uk/guide-to-diabetes/managing-your-diabetes/exercise (Accessed 1st March 2022).
Keywords: diabetes, exercise, physical activity, public health, Delphi study
Citation: Strongman C, Cavallerio F, Timmis MA and Morrison A (2023) Evaluating consistency of physical activity and exercise prescription in the UK for people with diabetes – a Delphi study. Front. Clin. Diabetes Healthc. 4:1278597. doi: 10.3389/fcdhc.2023.1278597
Received: 16 August 2023; Accepted: 17 November 2023;
Published: 07 December 2023.
Edited by:
Norbert Hermanns, Research Institute of the Diabetes Academy Mergentheim (FIDAM), GermanyReviewed by:
Roberta Lamptey, Korle Bu Teaching Hospital, GhanaTimm Roos, Research Institute of the Diabetes Academy Mergentheim (FIDAM), Germany
Copyright © 2023 Strongman, Cavallerio, Timmis and Morrison. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Clare Strongman, Y3NzMTM5QHBnci5hcnUuYWMudWs=
 Clare Strongman
Clare Strongman Francesca Cavallerio
Francesca Cavallerio Matthew A. Timmis
Matthew A. Timmis