- 1Human Potential Translational Research Program, Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore
- 2Centre for Sleep and Cognition, Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore
- 3Singapore Institute for Clinical Sciences, Agency for Science, Technology and Research (A*STAR), Singapore, Singapore
- 4Department of Obstetrics and Gynecology, Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore
- 5Folkhälsan Research Center, Helsinki, Finland
Background: Gestational Diabetes Mellitus (GDM) exposes women to future risk of Type 2 Diabetes. Previous studies focused on diet and physical activity, less emphasis was given to tackle intertwined risk factors such as sleep and stress. Knowledge remains scarce in multi-ethnic Asian communities. This study explored the: (1) feasibility of a holistic digital intervention on improving diet, physical activity (PA), sleep and stress of Asian women with a history of GDM, and (2) preliminary efficacy of the holistic intervention on women’s physical and mental well-being via a pilot randomized controlled trial.
Methods: Female volunteers with a history of GDM but without pre-existing diabetes were recruited from multi-ethnic Singaporean community. Each eligible woman was given a self-monitoring opportunity using Oura Ring that provided daily feedback on step counts, PA, sleep and bedtime heart rate. Intervention group additionally received personalized recommendations aimed to reinforce healthy behaviors holistically (diet, PA, sleep and stress). Dietary intake was evaluated by a research dietitian, while step counts, PA, sleep and bedtime heart rate were evaluated by health coaches based on Oura Ring data. Perceived physical and mental health and well-being were self-reported. Clinical outcomes included glycemic status determined by HbA1c and OGTT tests, body mass index, blood pressures and lipid profile.
Results: Of 196 women from the community, 72 women completed diabetes screening, 61 women were eligible and 56 women completed the study. The 56 completers had mean age of 35.8 ± 3.7 years, predominantly Chinese, majority had their first GDM diagnosed at least 2 years ago and had two GDM-affected pregnancies. After intervention period, more women in the Intervention group achieved at least 8,000 steps/day and had at least 6 hours of sleep per night. Noticeable reduction of added sugar in their food and beverages were observed after the dietary intervention. Changes in body weight and mental well-being were observed but group differences were not statistically significant.
Conclusions: The holistic approach appeared feasible for personalizing lifestyle recommendations to promote physical and mental well-being among women with a history of GDM. Larger studies with sufficient assessment timepoints and follow-up duration are warranted to improve the evaluation of intervention effects on clinical outcomes.
Clinical trial registration number: https://clinicaltrials.gov/show/NCT05512871, NCT05512871.
1 Introduction
Women with a history of Gestational Diabetes Mellitus (GDM) have an increased risk for Type 2 Diabetes (T2D) and other noncommunicable diseases than women who had normoglycemic pregnancy (1 ; 2–5). On a global scale, the prevalence of T2D including GDM was estimated to change at different rates in different regions (6). The age-adjusted hyperglycemia in pregnancy rate was projected to be around 15.8-16.0% between 2019 and 2045 contingent on other characteristics and the use of diagnostic criteria specific to the regions (7).
GDM is defined as glucose intolerance with first onset during pregnancy. While GDM may resolve following pregnancy, compared to women who had a normoglycemic pregnancy, women with a history of GDM are at a 10-fold risk of developing T2D (8). Risk factors for GDM are largely similar to those for T2D (e.g. family history of T2D, ethnicity, advanced age and overweight or obesity) (9). Pregnancy related risk factors (e.g. increased age in pregnancy, insulin therapy, multiparity, hypertensive disorders and preterm delivery) and risk factors after pregnancy (e.g. weight gain and physical inactivity) were also associated with future development of T2D (4, 9). The risk of T2D is elevated with the increasing length of GDM history. Accordingly, women with recent GDM could benefit from early intervention to help them prevent T2D or delay the progression to T2D (10–12).
Mobile health (mHealth) and digital interventions have emerged and played a transformative role in facilitating lifestyle changes by supplementing face-to-face interventions and bringing convenience to the users. A multitude of smartphone Applications (App), wireless mobile technologies, virtual communication tools and activity tracking wearable devices have been introduced to the space of health promotion, care delivery, disease prevention and management (13). While mHealth is beginning to gain traction among relevant stakeholders in the healthcare industry, it is of our interest to explore the possibility of leveraging a mHealth strategy to address the health needs of women with a history of GDM in a holistic manner.
Previous prevention studies have largely been focusing on promoting healthy diet and physical activity and less emphasis was given to tackle the intertwined risk factors for T2D such as sleep and stress. Furthermore, evidence of lifestyle intervention on preventing T2D in women with a history of GDM remains scarce in the context of multi-ethnic Asian community and this calls for further exploration. Therefore, this study aimed to: 1a) examine the feasibility of using smartphone Apps and activity wearable device to collect data (diet, PA, sleep and stress) necessary for a multi-disciplinary team of health coaches to deliver holistic lifestyle interventions that can be personalized and tailored to the needs of women at an individual level; 1b) explore whether the lifestyle data collected within a short time window (10 weeks) can provide meaningful information for understanding lifestyle behavior in a holistic manner and facilitate health coaching, and 2) explore preliminary efficacy of the proposed lifestyle intervention on clinical health and well-being outcomes (blood glucose concentrations, body weight, blood pressures, lipid profile, mental well-being and perceived general well-being) among women with a history of GDM via a pilot randomized controlled trial (RCT) study design.
2 Materials and methods
2.1 Study characteristics
2.1.1 Study design
This was a feasibility and pilot study conducted among Asian women with a history of GDM. The feasibility study lasted for 10 weeks in total. The study design included a 2-week baseline observation phase followed by a 8-week pilot study that comprised a 4-week RCT (parallel two-arm, single-center, non-blinded) and a 4-week follow-up period.
2.1.2 Eligibility criteria
Inclusion criteria were Asian women residing in Singapore during the study period, aged between 21-45 years who self-reported a history of GDM of not more than 10 years ago, without pre-existing diabetes, and able to provide a written informed consent in English language. Exclusion criteria were current or previous diagnosis of diabetes mellitus (except GDM), currently pregnant or anticipate becoming pregnant, performing full breastfeeding during study period, within 12 weeks postpartum, following special diet or dietary restrictions, experiencing severely limited mobility, diagnosed with malnutrition, eating disorders, severe insomnia or major diseases (cancers, unstable heart diseases, severe kidney diseases, unstable mental illness, dementia or cognitive impairment), experiencing alcohol or drug abuse, taking medications known to influence glucose metabolism, did not own a smartphone (Android version 10 or above) compatible with the mobile Apps used in this study, and participating in concurrent clinical trial, lifestyle intervention or fitness and wellness program.
2.1.3 Participants and settings
Recruitment was conducted from September 2022 to March 2023 through advertising the study on social media platforms (Instagram, Facebook advertisements, LinkedIn, Telegram), dissemination of electronic study flyers through corporate E-mails (National University Health System (NUHS) and Agency for Science, Technology and Research (A*STAR)), by word of mouth (among family and friends), advertising the study on the CrowdTaskSG online portal initiated by the Singapore government for engaging the citizens, and through collaborating with polyclinics in the West region of Singapore. Interested individuals contacted the study team via phone or E-mail. Recruitment was also conducted on-site in polyclinics located at the West region of Singapore to identify potential women. A two-step screening procedure was adopted. First, women who expressed interest in participating in this study were pre-screened for eligibility via phone. Second, women who met the study criteria (except diabetes status) and provided informed consent were invited to attend a diabetes screening conducted at the study site (Human Development Research Centre (HDRC), National University of Singapore).
2.2 Study procedures
2.2.1 Screening procedures
Women were reminded to fast for at least 10 hours before attending the screening visit. Two diabetes screening tests, i.e. a glycated hemoglobin (HbA1c) finger prick test followed by a 75g Oral Glucose Tolerance Test (OGTT), were conducted in succession to determine women’s diabetes status before enrolling them to the study. At the screening visit, women first underwent a HbA1c finger prick test (DCA Vantage® Analyzer, Siemens) and provided basic information about their demographics and general health. Women who demonstrated HbA1c ≥ 6.5% at screening visit were excluded from the study and advised to consult their medical doctors. Each woman who had HbA1c < 6.5% was then given an oral glucose solution containing 75g of sugar. After 120 minutes, blood sample was drawn again. The collected blood samples were analysed to measure fasting 0-min plasma glucose (FPG) and 120-min or 2-hour plasma glucose (2hPG) concentrations. Women who had non-diabetic glucose concentrations determined by the OGTT results, i.e. FPG < 7.0 mmol/L and 2hPG < 11.1 mmol/L, were finally included in the study. Otherwise, women were excluded from the study and advised to consult their medical doctors.
2.2.2 Baseline procedures
Demographics were self-reported and baseline anthropometric measures (body weight and height) were recorded. Women were also requested to self-report their general physical and mental health and well-being using self-administered questionnaires (as described in Section 2.6). At baseline visit, after an overnight fasting of at least 10 hours, blood samples were drawn for additional biochemical analyses (i.e, HbA1c, full blood count, insulin, blood markers of inflammation (hsCRP), lipid and liver function tests).
2.2.3 Wearable devices
A continuous glucose monitoring system (CGMS) wearable device (FreeStyle Libre Pro iQ, Abbott Laboratories Limited) was applied to monitor individuals’ subcutaneous glycemic variability for 14 days and women were blinded to the CGMS readings. Each woman was also given an Oura Ring (Ōura Health Ltd.) paired with the Oura proprietary mobile App to collect continuous lifestyle data (physical activity, sleep duration, bedtime heart rate and heart rate variability) throughout the study period (as described in Section 2.6).
2.3 Study groups
2.3.1 Randomization
Randomization was performed after baseline assessments and procedures. The randomization strategy (block size of 4) was developed independently by a statistician. Eligible women were randomized to either the Control group or Intervention group based on a 1:1 allocation ratio.
2.3.2 Control group
Women randomized to the Control group received a standard mHealth package that comprised:
1. an Oura Ring paired with Oura mobile App:
to monitor PA, sleep and bedtime heart rate throughout study period
2. an electronic diary (e-Diary):
to log dietary information and report perceived stress level (if any) over 14 days from baseline
2.3.3 Intervention group
Women randomized to the Intervention group received an mHealth package that comprised:
1. the standard mHealth package received by the Control group, and
2. a purpose-built study mobile App:
i. to upload photos of food and beverages for review by a research dietitian,
ii. to self-report perceived stress level on a 7-point Likert scale, and
iii. to receive 2 sessions of personalized, messaging-based lifestyle recommendations delivered by a team of health coaches through a virtual chatroom
2.4 Intervention
2.4.1 Review of lifestyle behavior
A team of health coaches from multi-disciplinary domains (diet, PA, nursing and public health) reviewed women’s lifestyle data (dietary intake, step count, time spent being sedentary, sleep duration, self-reported stress level). Women were encouraged to wear the Oura Rings and upload photos of food and beverages if lifestyle data was deemed insufficient for evaluation by the health coaches. Health coaching lasted for 4 weeks per woman, and personalized recommendations were delivered via the study mobile App once every 2 weeks to address the lifestyle needs of the individuals.
2.4.2 Personalized lifestyle recommendations
Lifestyle recommendations were guided by the information available on the publicly accessible website of the Singapore Health Promotion Board (14) and the HealthHub website (15). Personalized recommendations were delivered by the health coaches if any of the following conditions was met: (1) the women did not follow the My Healthy Plate recommendations (Singapore Health Promotion Board My Healthy Plate), their diets lacked a decent portion size of healthy food (i.e. fruits, vegetables, protein, wholegrain, less than 2 servings of fish per week) or were high in refined carbohydrates, saturated fat or added sugar (based on the research dietitian’s review of women’s dietary information), (2) weekly average of steps count was below 7,000 steps per day (based on Oura Ring data), (3) weekly average of sleep score was below 80 (based on Oura Ring data), and (4) weekly stress levels were deemed extreme that require intervention by the health coaches (based on women’s self-rating).
2.4.3 Virtual incentives
Virtual incentives in the form of congratulatory messages (e.g. “keep up the good work!”) were delivered to the women who made improvements over time as well as those who maintained satisfactory performance and did not require health recommendations.
2.5 Primary outcomes
2.5.1 Feasibility
Feasibility measures included the access to participants, rate of recruitment and retention, proportion of women who met the inclusion criteria, use of mHealth packages, completion of assessments at baseline and endpoint visits, adherence to study duration and procedures, and data completeness. For the Intervention group, we additionally examined the availability of photos of food and beverages needed for dietary assessments, and the feasibility of delivering personalized recommendations by the health coach using the virtual chatroom offered by the study mobile App.
2.5.2 Preliminary efficacy
The preliminary efficacy of the pilot RCT was determined by comparing between the Intervention and Control groups on the mean change from baseline in clinical health and well-being outcomes associated with T2D, i.e. FPG, 2hPG following a 75g of oral glucose load, body weight, blood pressures, lipid profile, perceived general well-being and mental well-being as determined by: (1) depression: based on the Beck’s Depression Inventory (BDI)-II measures (16)), and (2) anxiety: based on the State-Trait Anxiety Inventory (STAI) measures (17).
2.6 Explanatory variables
2.6.1 Baseline characteristics
Baseline data included age, marital status, occupation, highest education level, monthly household income, household members, time since the first diagnosis of GDM, number of pregnancies affected by GDM, medical history, history of cigarettes smoking and alcohol drinking and past experience in using mobile Apps and wearable devices for self-monitoring of lifestyle behaviours.
2.6.2 Anthropometrics
Body weight (kg) was measured without shoes using a calibrated digital scale (SECA GmbH & Co. KG). Two measures were recorded to the nearest 0.1 kg, and a third measure was obtained if the first and the second measures differed by > 0.2 kg. The average of the measures was reported.
Body height (cm) was measured without shoes using an automatic weighing scale (SECA GmbH & Co. KG). Two measures were recorded to the nearest 0.1 cm, and a third measure was obtained if the first and the second measures differed by > 1.0 cm. The average of the measures was reported.
Body Mass Index (BMI) was calculated as body weight (in kilograms) divided by height (in meters squared) and categorized based on the Asian cut-off points (underweight: < 18.5 kg/m2; normal weight: 18.5-22.9 kg/m2; overweight: 23.0-24.9 kg/m2; pre-obese: 25.0-29.9 kg/m2, and obese: ≥ 30.0 kg/m2) (18). Body fat mass (kg) and lean body mass (kg) were assessed using a bioimpedance analysis instrument (SFB7, ImpediMed Ltd.).
2.6.3 Blood pressures
Women were asked to rest for 5 minutes, then systolic blood pressure and diastolic blood pressure were measured twice using an automated digital monitor (HBP 1320, Omron Corp.). A third measure was obtained if the first and the second measures differed by > 10 mmHg. The mean of the measures was reported.
2.6.4 Biomarkers
Blood samples were collected following a minimum 10 hours of overnight fast by a trained phlebotomist using a standardized procedure, and the biochemistry analyses were conducted by the National University Hospital Referral Laboratories. In this study, the following blood biomarkers were analyzed and reported: HbA1c (% and mmol/L), FPG and 2hPG concentrations following a 75g of oral glucose load (mmol/L), Triglycerides (mmol/L), LDL (low-density lipoprotein) cholesterol (mmol/L) and HDL (high-density lipoprotein) cholesterol (mmol/L).
2.6.5 Dietary intake
Each woman was requested to self-report their intake of meals including snacks (i.e. photos of food and beverages, date, time, main ingredients of their food and beverages, place, home-cook vs dine out, companion) via the e-Diary for 14 days from baseline.
During the intervention period, women randomized to the Intervention group were additionally requested to continue uploading photos of food and beverages to the study mobile App for the research dietitian to review the women’s dietary intake and deliver personalized dietary recommendations through the virtual chatroom.
2.6.6 Physical activity, sleep duration and bedtime heart rate
The Oura Ring (Ōura Health Ltd) is a novel wearable that detects body movement, sleep or wake states using multiple sensors (accelerometer, temperature). The Oura Ring has been validated against medical grade actigraphy and polysomnography (19–21). Each ring was paired with Oura’s proprietary mobile App to provide continuous and objectively measured lifestyle data, i.e. step counts, time spent on intensity-based physical activity, time spent being sedentary, sleep duration, bedtime heart rate and heart rate variability. Each woman was encouraged to wear her Oura Ring throughout the study period.
During the intervention period, Oura Ring data contributed by the Intervention group were reviewed by the health coaches to offer lifestyle recommendations through the virtual chatroom. Recommendations were personalized and tailored to the needs of the women.
2.6.7 Perceived stress
Each woman was requested to self-report any stressful events (if any) that they encountered during the first 14 days of the study. They were asked to share information about the date and time of the reported stressful events, reasons for feeling stressful, and rate their stressfulness on a 7-point Likert scale.
During the intervention period, women randomized to the Intervention group were additionally prompted to rate their stress level via the virtual chatroom for review by the health coaches.
2.6.8 Perceived well-being
A 36-item Short Form Survey (22) that consists of a set of generic, coherent, and easily self-administered questionnaire was used to measure health-related quality-of-life. A Subjective Happiness Scale (23) which is a simple 4-item tool was self-administered to assess an individual’s global subjective happiness.
2.7 Data analyses
2.7.1 Data processing
The Oura Ring data were collected on a daily basis. In the context of this study, “Baseline Oura Ring data” was defined as data collected within the first 14 days from the date women made in-person baseline visit to the study site. Data for step count and time spent being sedentary were summarized after removing data points when daily step counts were < 1,800 steps/day (i.e. the lowest 5th percentile) and when women were not contributing data for more than 870 minutes (i.e. the largest 5th percentile). Sleep duration and bedtime heart rate were summarized based on data captured during women’s bedtime (night time) when long sleep periods (≥ 3 hours) as well as intermittent short sleep periods (between 15 mins and 3 hours) were recognized by the Oura Rings. Periods of sleep and naps during day time were not considered in this study.
The photos of food and beverages and other description about meal intake (ingredients, place, companion) submitted by the Intervention group were analyzed by a research dietitian. Similarly, “Baseline diet data” referred to dietary information collected within the first 14 days from the date of baseline visit. Subsequently, the Intervention group continued sharing information about food and beverages throughout the 4-week intervention period. The quality of diet was assessed by the research dietitian to determine whether or not women’s diet was meeting the My Healthy Plate recommendations, whether women were consuming sufficient intake of vegetables, fruits, wholegrain, protein and fish, consuming food or beverages which were high in added sugar, choosing low fat option and avoiding high intake of saturated fat in their diets.
2.7.2 Statistical analysis
Frequencies (percentages), means (standard deviations) or medians (interquartile ranges) were used to summarize the data (questionnaire, surveys, laboratory biochemistry analysis, Oura Ring and study mobile App) collected from women who completed both baseline and endpoint assessments. Statistical tests were performed, e.g. Chi-square or Fisher’s exact test for categorical variables, and two independent sample t-tests or ANOVA for continuous variables. Nonparametric tests were used as appropriate.
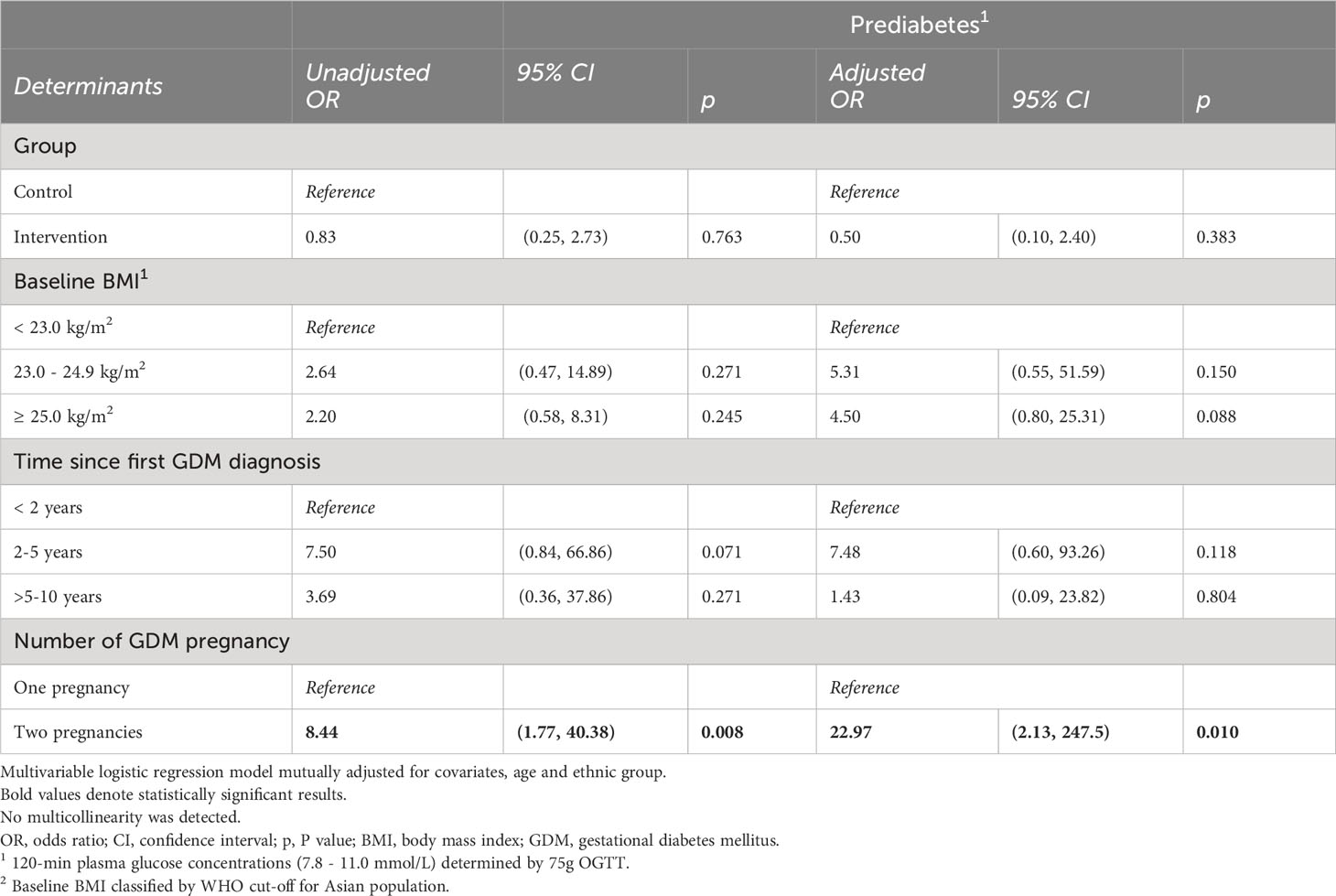
Preliminary efficacy was examined by comparing the differences between the two study groups on the change in the interested clinical health and well-being outcomes between study baseline and endpoint. Additional analyses were conducted to only focus on 3 main ethnic groups in the Singaporean population (i.e. Chinese, Malay and Indian) to identify factors associated with the interested clinical outcomes at the end of the study (i.e. glucose concentrations following 75g OGTT, body weight and mental well-being). Associations were assessed using multivariate linear regressions adjusted for potential confounders. A sensitivity analysis was performed to determine if there was any significant discrepancy in the direction and magnitude of associations by including all completers in the multivariate regressions model. Further, multivariable logistic regression models with adjustment for potential confounders were conducted to explore factors associated with prediabetes which was determined by the 75g OGTT values between 7.8 and 11.0 mmol/L. A p-value of <0.05 was considered statistically significant. All statistical analyses were conducted using STATA SE version 18 for Windows (StataCorp LLC). Since this was a pilot study, a sample size calculation was not performed. A minimum pragmatic target of 30 women for each study group was set prior to the study.
2.8 Ethical approval
Ethical approval was granted by the National Healthcare Group (NHG) Domain Specific Review Board (DSRB) (Ref: 2021/00843). The design, conduct and reporting of the pilot RCT were in accordance with the Consolidated Standards of Reporting Trials (CONSORT) guidelines.
3 Results
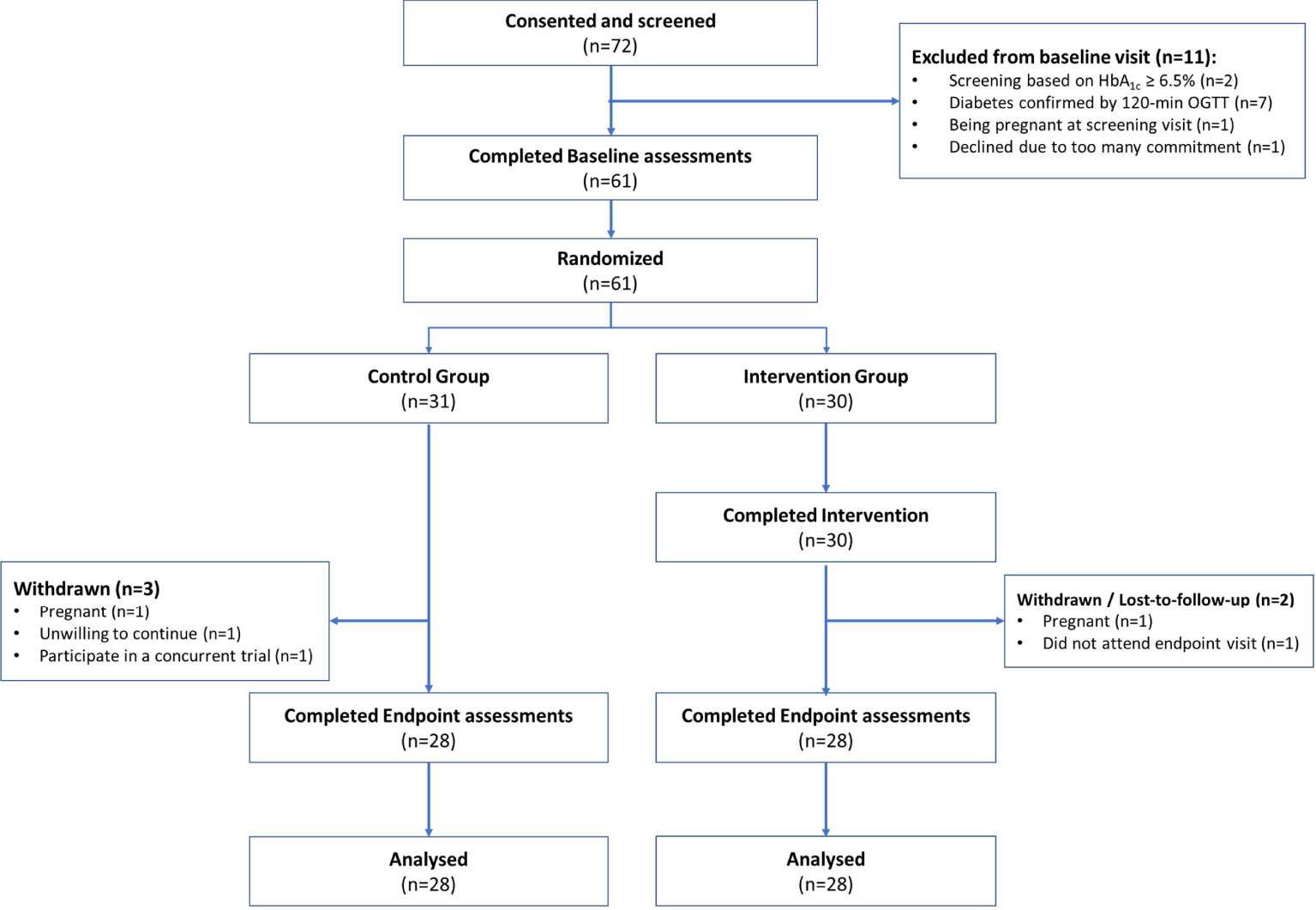
In total, 196 women from the community expressed interest in this study. 72 (36%) consented for eligibility assessments. Figure 1 summarizes the flow of participants through the stages of the pilot RCT. Outreach was most successful through advertising the study via NUHS and A*STAR corporate E-mails (38.9%), followed by advertising by word of mouth among family members, friends and relatives (29.2%), social media platforms such as Instagram, Telegram, Facebook advertisement and LinkedIn (25%), CrowdTaskSG online portal (5.6%) and polyclinic in the West region of Singapore (1%). Of the 72 women who attended screening, 61 (84%) were eligible and completed baseline assessments. All of them were randomized at baseline to the Control (n=31) or Intervention (n=30) group, respectively. 56 (92%) completed the study and provided data for analyses. 5 (8%) did not complete the study and the reasons for withdrawal or dropout were self-reported pregnancy (n=2), participating in a concurrent trial (n=1), unwilling to continue (n=1) and did not attend endpoint study visit (n=1).
Figure 2 provides an indication of women’s participation and contribution across various dimensions of the study. Of the 61 women included in the study, all of them (100%) completed baseline assessments, 56 (92%) remain engaged in the study and completed endpoint assessments. Of the 56 completers, 55 (98%) contributed sufficient device data for the subsequent analyses of step count, sedentary time, sleep duration and bedtime heart rate variability, and 48 (85%) actively used the Oura Ring for at least 60 days (of the total 70 days of study period).
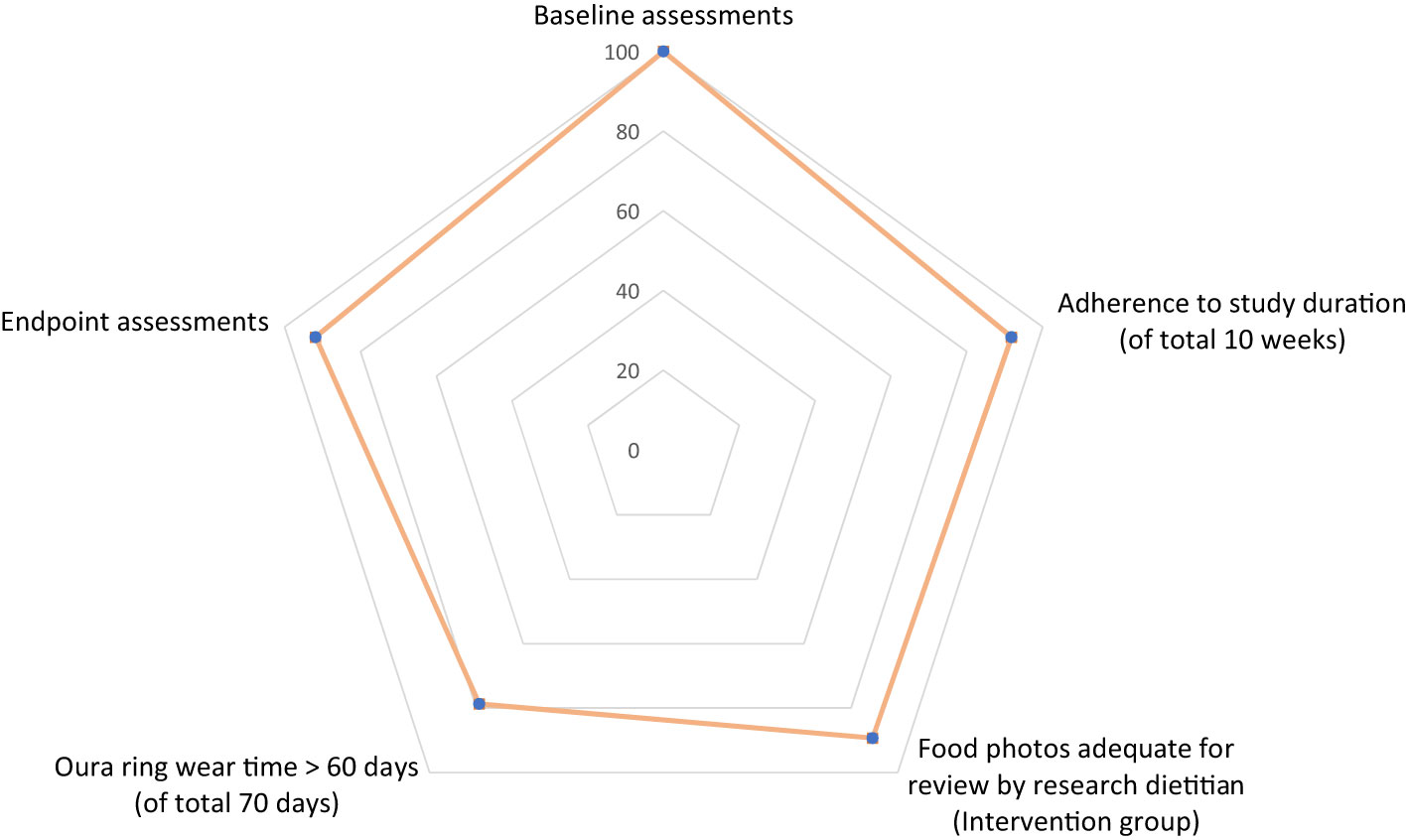
Figure 2 Percentage of women (among 61 eligible women) contributed to various dimensions of the study.
For the Intervention group, additional information about dietary intake (photos of food and beverages) were collected in addition to Oura Ring data. 25/28 (89%) women in the Intervention group submitted photos of food and beverages that were deemed adequate for the research dietitian to make assessments and deliver dietary recommendations through the App. Holistic lifestyle data (diet, physical activity, sleep and heart rate) were made available for the health coach to review, make informed feedback and recommendations.
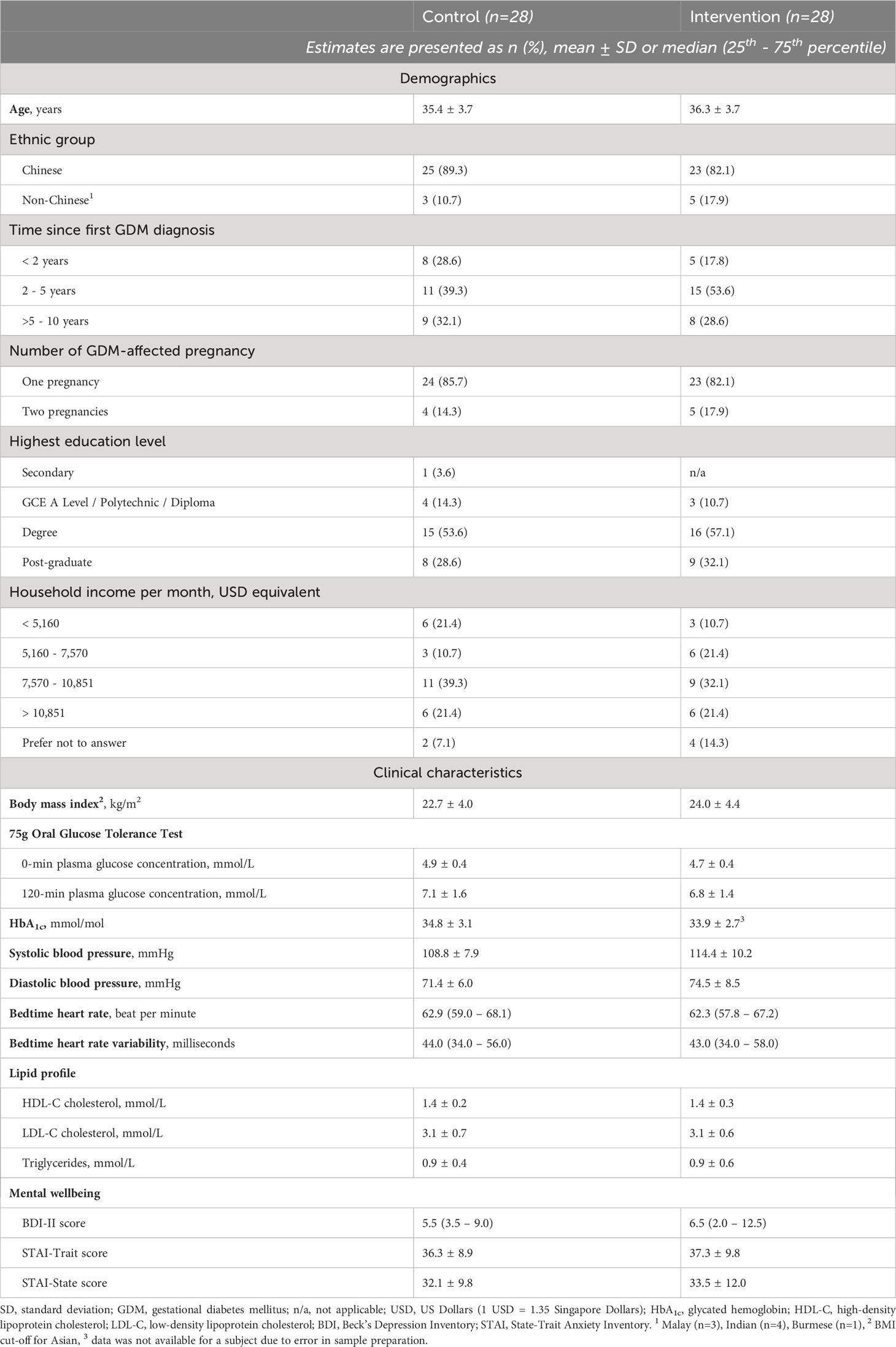
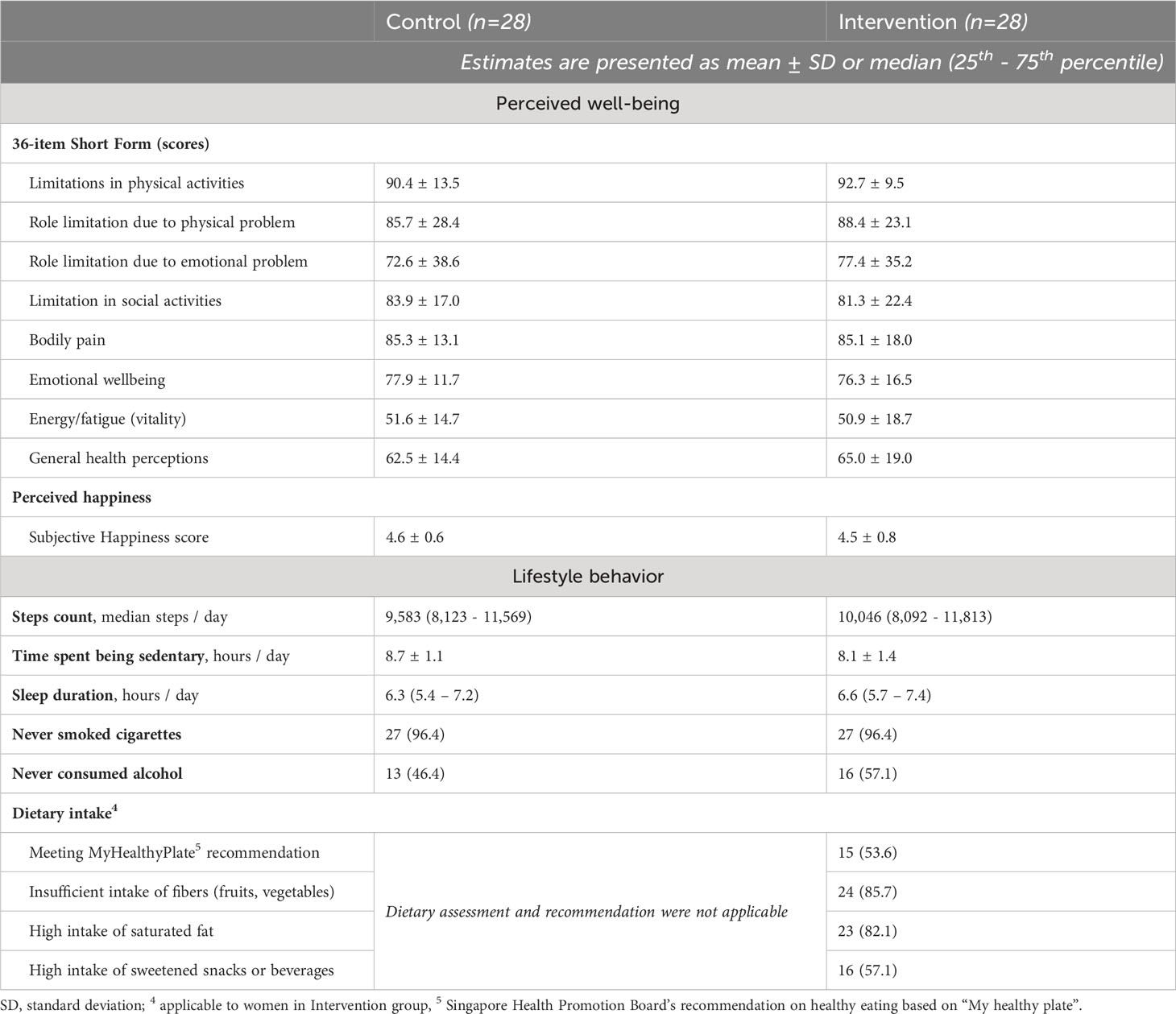
3.1 Baseline characteristics
Tables 1A, 1B describe the demographics, clinical characteristics, perceived well-being and lifestyle behaviours of the women randomized to the Control and Intervention groups at baseline. Women in the study (Intervention vs. Control) had mean age (36.3 ± 3.7 vs. 35.4 ± 3.7 years), predominantly Chinese (82% vs. 89%), had their first GDM diagnosed at least 2 years ago (82% vs. 71%) and less than 20% had two GDM-affected pregnancies (18% vs. 14%). Majority of them received tertiary education or above (89% vs. 82%) and had household income of more than USD 7,570 per month (54% vs. 61%).
Majority of the clinical characteristics of the women were within healthy ranges. A small number of the women in both groups were found to have prediabetes (18% vs. 32%), slightly elevated systolic blood pressures (14% vs. 29%), LDL-C > 3.3 mmol/L (39% vs. 29%) and Triglycerides > 1.7 mmol/L (4% vs. 7%). The women’s mental well-being was generally satisfactory with only one woman demonstrating a borderline moderate depression (BDI-II score of 30) and a small number of them indicating probable high-state anxiety: STAI-State score ≥ 46 (7% vs. 14%) or STAI-Trait score of ≥ 52 (7% vs. 14%).
The perceived well-being of the women in both groups were largely similar across the examined domains and no significant difference between the two groups was observed at baseline (Table 1B). In terms of baseline lifestyle behaviour, women in the Intervention group (vs. Control) achieved median 10,046 (vs. 9,583) steps per day, spent 8.1 (vs. 8.7) hours per day being sedentary and had mean sleep duration of 6.6 (vs. 6.3) hours per day. Almost half of the women in the Intervention group (vs. 46% in the Control group) had never consumed alcoholic drinks. 96% of the women in this study had never smoked cigarettes. Women randomized to the Intervention group were requested to share photos of food and beverages through the study App and had their baseline dietary intake assessed by the research dietitian. Of 28 women, 53% met the My Healthy Plate recommendations, 75% had decent amount of protein intake, 53% had at least 2 servings of fish per week, and only a quarter of them had decent portion sizes of fruits, vegetables and wholegrain in their diet. While 4% of the women had high consumption of refined carbohydrates, 82% and 57% consumed food that were high in saturated fat and added sugar, respectively.
3.2 Preliminary efficacy of intervention
Figures 3, 4 summarize the changes in lifestyle behaviors from baseline to post-intervention. Among the 56 completers, a higher proportion of women in the Intervention group achieved daily step counts of at least 8,000 steps per day and reduced sedentary time (or inactive time) as classified by the Oura Ring, but no noticeable improvement was observed for sleep duration (Figure 3). Among 25 women who provided adequate number of photos for dietary assessments, none of them demonstrated high consumption of refined carbohydrates after the intervention (Figure 4). Slight improvements were observed as women added protein, fruits and vegetables to their diets and reduced the consumption of saturated fat. More noticeable change was observed as the women reduced the consumption of added sugar in their food after the dietary intervention. However, the intake of wholegrain and fish remained inadequate. Table 2 presents the mean change of clinical health and well-being outcomes from baseline to the end of the study and the observed differences between the study groups were not statistically significant.
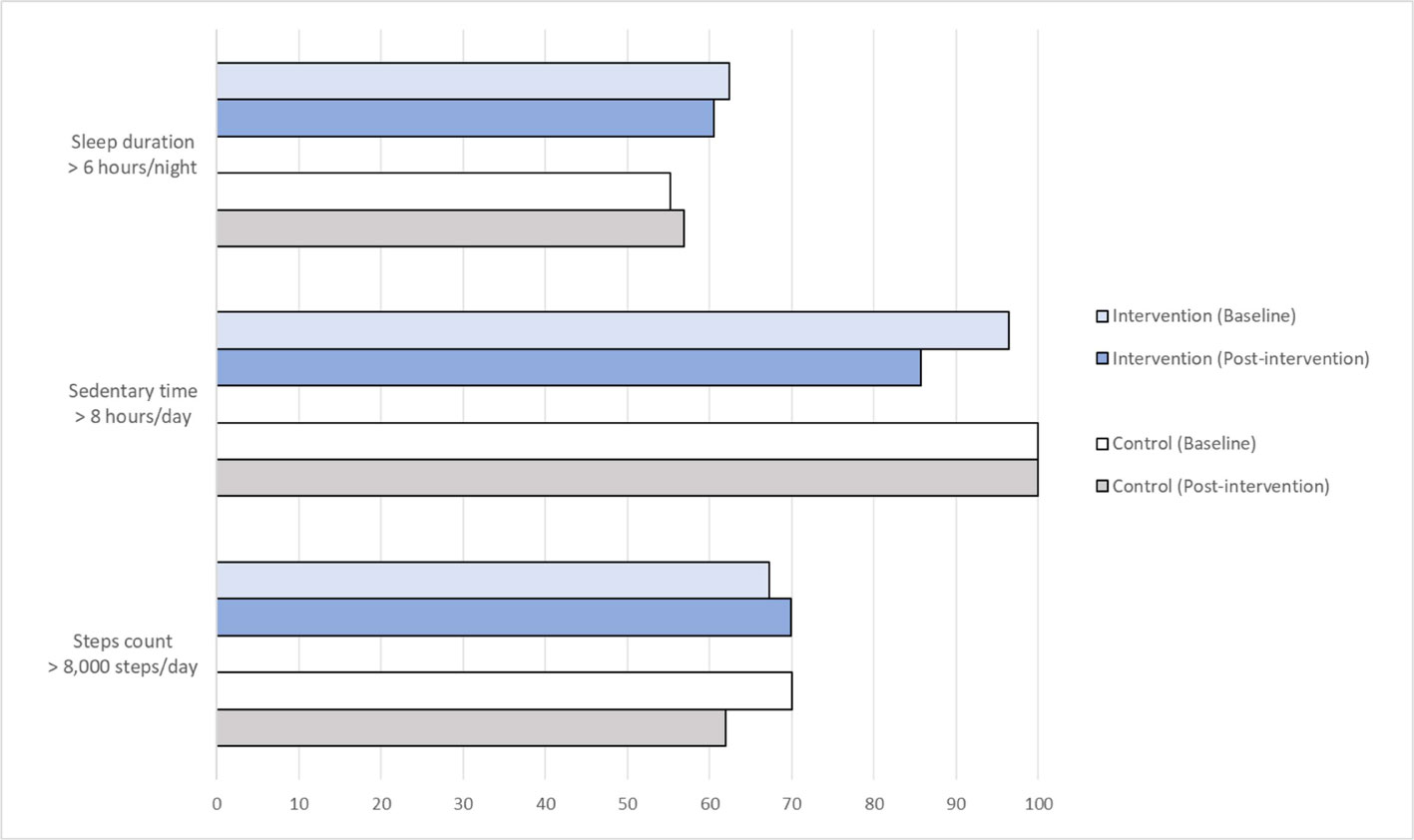
Figure 3 Percentage of women (among 56 completers) and their PA and sleep duration at Baseline and Post-intervention.
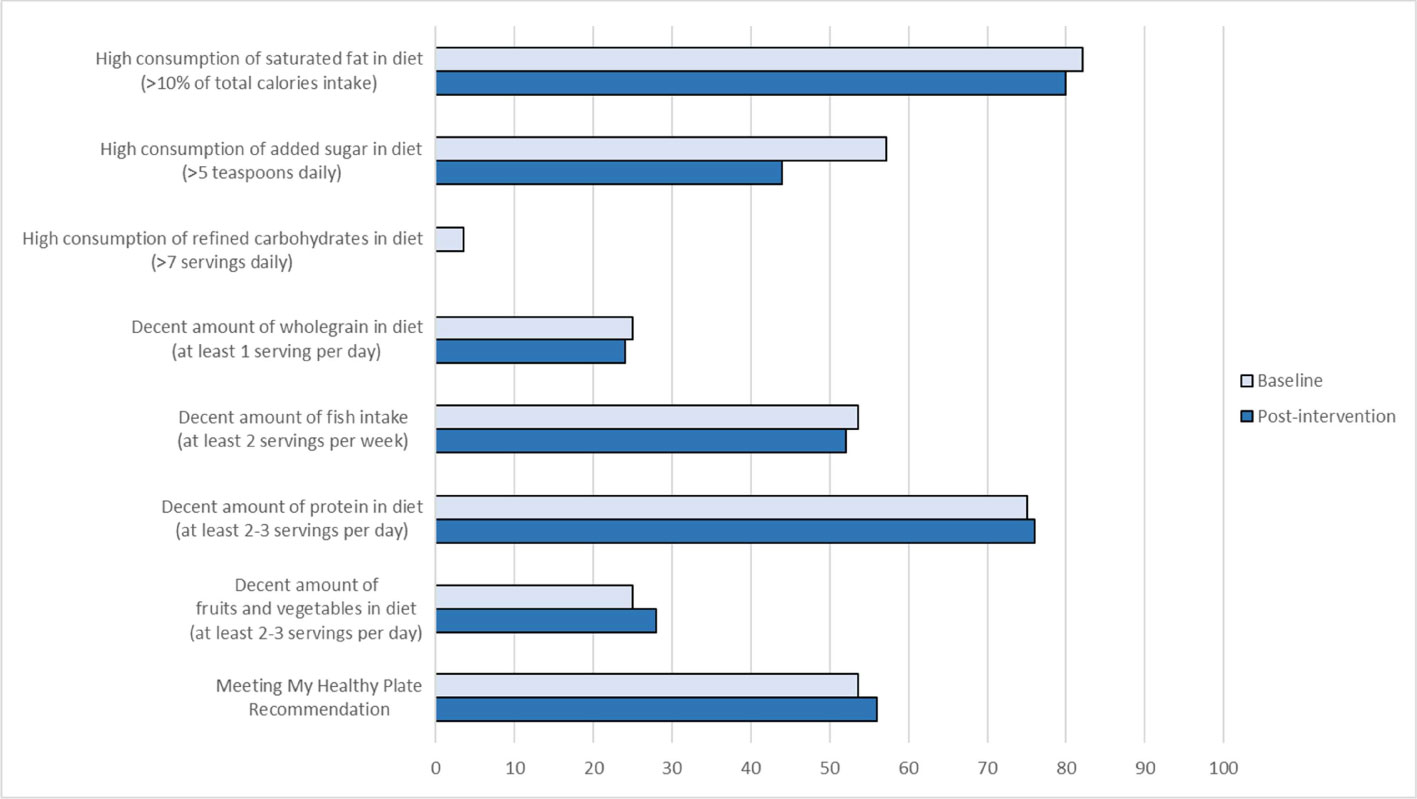
Figure 4 Percentage of women in the Intervention Group (among 25 women) and their dietary intake at Baseline and Post-intervention.
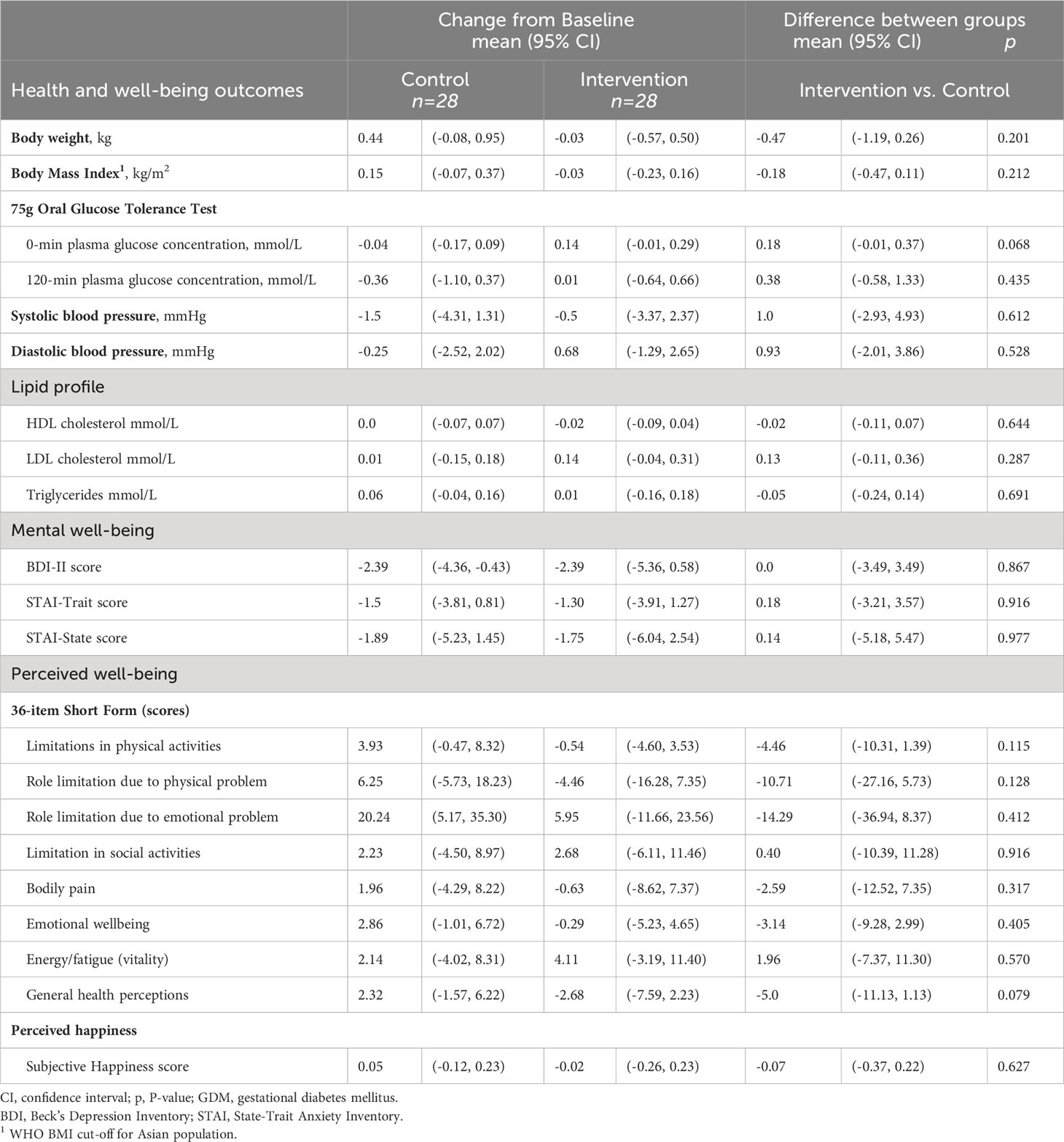
Table 2 Mean change in preliminary efficacy health and wellbeing outcomes between Intervention and Control groups.
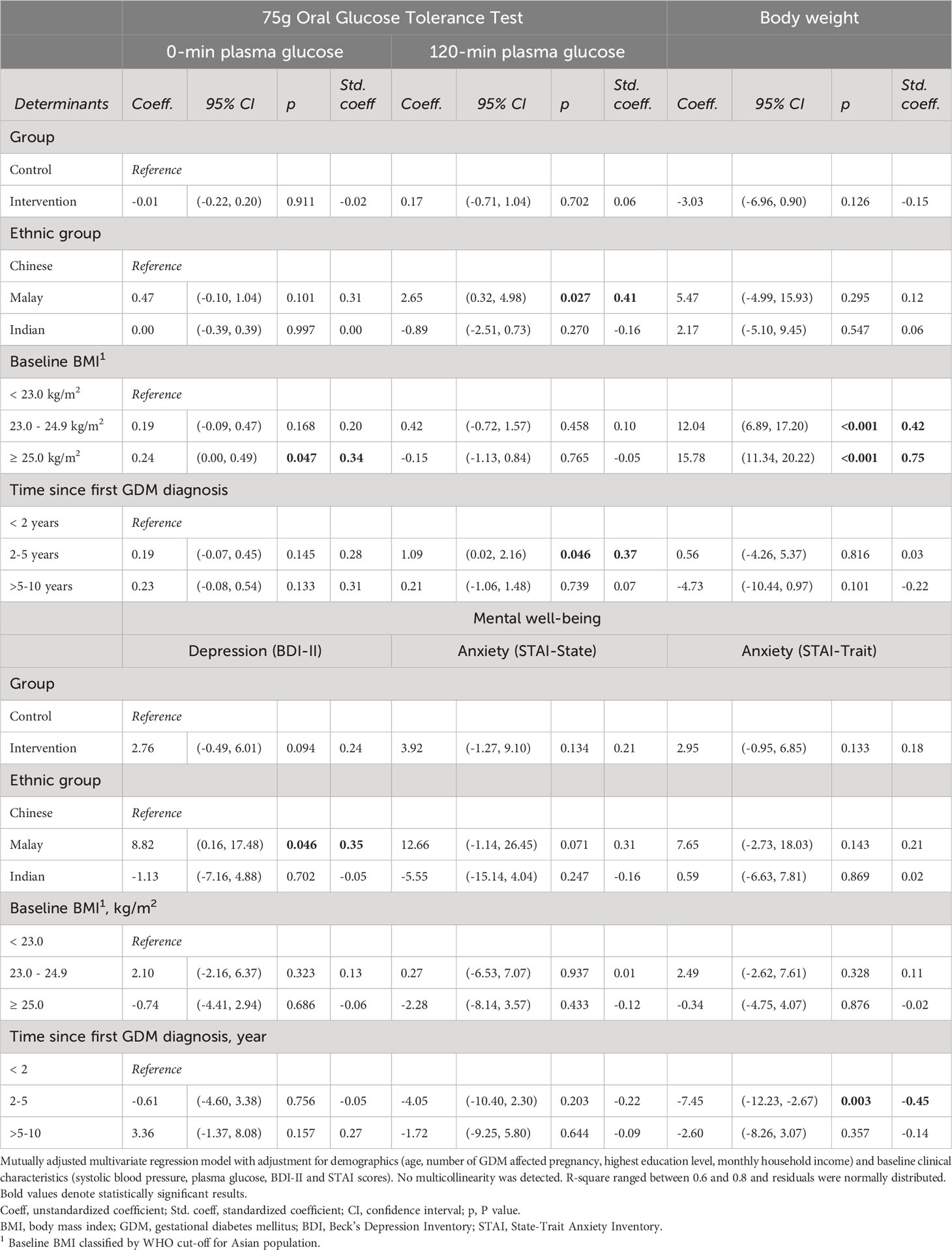
3.3 Factors associated with clinical outcomes
3.3.1 Plasma glucose concentrations
Women with higher BMI had higher 0-min plasma glucose concentrations (or FPG) when compared to women with lower BMI (Table 3), however, this positive relationship did not exist for the 120-min plasma glucose concentrations (or 2hPG). Instead, being in the Malay ethnic group was associated with higher 120-min plasma glucose concentrations when compared to their Chinese counterpart. Similar positive relationship was observed in women who had their first GDM diagnosed between 2-5 years ago when compared to women who had their GDM first diagnosed in less than 2 years.
3.3.2 Body weight
Women who were being overweight and obese at baseline were associated with higher body weight at the end of the study (Table 3). A noticeable magnitude of intervention effect on body weight favoring the Intervention group was observed, however, the effect was not statistically significant.
3.3.3 Mental well-being
When compared to Chinese women who constantly maintained mental well-being within the healthy ranges, Malay women had higher BDI-II scores but none of them demonstrated probable clinical depression at the endpoint assessment. The findings further suggest that women with their GDM diagnosed 2-5 years ago had lower anxiety (STAI-Trait) level than women who had their GDM diagnosed more recently in less than 2 years ago.
3.3.4 Prediabetes
Prediabetes was more common among women who had 2 GDM-affected pregnancies (67%) as compared to women who had only 1 GDM-affected pregnancy (19%). The results of multivariable logistic regression suggest that the odds of prediabetes were significantly associated with higher number of GDM pregnancy after accounting for potential confounders (Table 4). Figure 5 shows the changes in women’s blood glucose status (i.e. normal glucose tolerance (NGT) vs. prediabetes) from study baseline to endpoint in relation to the changes in their body weight between the two timepoints. Initial observations suggested that a small number of the women who had NGT at baseline were found to have prediabetes at the end of the study and this was common among the individuals who gained weight over the two timepoints.
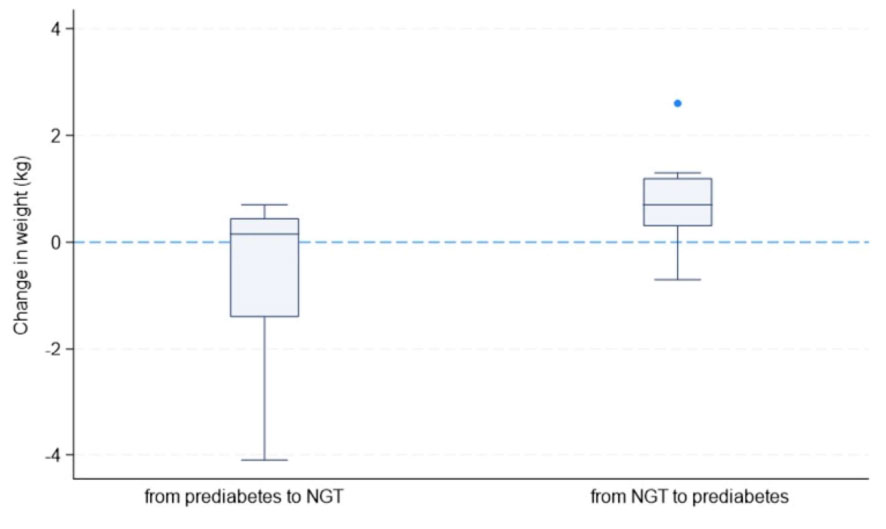
Figure 5 Changes in women’s blood glucose status and body weight between study Baseline and Endpoint (NGT, normal glucose tolerance).
4 Discussions
This study identified that the mHealth-enabled holistic approach was acceptable among women with a history of GDM as 91.8% of the 61 enrolled women completed the study, and 78.7% wore the Oura Ring for at least 90% of the study duration. Among the women in the Intervention group, 89.3% provided adequate number of photos of food and beverages for dietary assessments. The collection of holistic lifestyle data from multiple sources was feasible, and the delivery of personalized lifestyle recommendations through the study mobile App was feasible. A more integrated solution could potentially streamline the process and improve the women’s uptake of mHealth strategies.
4.1 Recruitment and participant characteristics
Eligible women of this study were mainly recruited through corporate E-mails, among family and friends, and advertising the study on social media platforms. Of the 196 women who expressed interest in this study, 36% were screened and 31% were finally included in the study. Among the women who had a GDM history of 5-10 years, more than 90% were excluded due to T2D and were advised to consult with their doctors for further assessment. Women in the study were predominantly from the Chinese ethnic group, highly educated, had medium-to-high household income and potentially more affluent in relation to the use of social media and technology. The apparent low uptake from the minority ethnic groups and women from low socioeconomic status deserve attention since studies have suggested that economic, socio-cultural and societal factors were associated with risk of GDM and T2D in Asia regions (24, 25). Therefore, improving the recruitment strategy to reach out to these groups of women is warranted.
4.2 Preliminary efficacy of lifestyle modifications
Preliminary findings of the present study suggest that the observed difference between groups on the body weight outcome was mainly attributable to weight gain among women with BMI of 25 kg/m2 or more in the Control group who did not receive health coaching. Suppressing weight gain could be a practical challenge for women with pre-obesity and obesity in the absence of lifestyle intervention. Therefore, introducing women to lifestyle intervention after GDM might confer clinically important benefits in some individuals although the difference between study groups was not statistically significant (26–28).
In line with the current knowledge, interventions focusing on managing weight or BMI have not been effective in preventing glycemic deterioration after GDM (28). The possible explanation could be that the frequency and intensity of the proposed intervention was not optimal for a subgroup of individuals who are at higher risk of T2D (29). Further, the observed higher odds of prediabetes among women with their first GDM diagnosed 2-5 years ago may be attributable to insufficient or neglected health management as compared to women with more recent GDM diagnosis.
Both study groups demonstrated improvement in mental well-being outcomes at the study endpoint, although the intervention effect was not statistically significant. Preliminary findings of this study suggest that women’s exposure to self-monitoring of physical activity and lifestyle behavior may have improved their mental well-being over time (30). In addition, health concerns related to glucose intolerance are often attributable to physiological and psychological stressors. Sleep deprivation and disturbances increase cortisol levels whereas elevated oxidative stress results in insulin resistance, influencing blood glucose levels which in turn increase an individual’s risk of T2D and other metabolic diseases (31–33). Accordingly, giving attention to reducing anxiety and improving mental well-being may help prevent future risk of T2D.
The incidence rate of T2D after GDM is highly variable across countries and it is relatively higher among Asian populations than among Western populations (34, 35). Furthermore, T2D in Asian populations is characterized by a younger age and lower BMI of onset than in the Western populations (36). Possible explanation for such phenomenon in Asia is that the Asian populations are undergoing rapid socio-economic transformation, creating an environment that can induce obesity and maladaptive inflammatory responses that exacerbate β-cell dysfunction in these regions (37). Singapore is no exception with a GDM prevalence around 23.5% in 2019 (IDF Diabetes Atlas 9th edition Singapore Diabetes Report). The Singaporean GUSTO (Growing Up in Singapore Towards healthy Outcomes) study demonstrated that the risk of developing T2D was 12-fold in Singaporean women 4-6 years after their GDM diagnoses (38).
Asian women could benefit from lifestyle modifications following GDM. Initial improvements in metabolic health and lifestyle behaviors following one year of dietary and physical activity interventions were reported (39). Although group difference was not observed, the incidence of T2D within 3 years postpartum was lowered when Asian women were exposed to diet and exercise interventions (40). Results from observational studies further demonstrated that integrating psychosocial well-being (i.e. offering social support and improving self-efficacy) in lifestyle interventions were positively associated with adopting healthy lifestyle (i.e. increased physical activity, improved diet) and lower stress perception. Similar interventions also reduced BMI and postpartum diabetes status and improved metabolic outcomes (41). The current body of knowledge, taken together, support a holistic approach to improving diet, physical activity and psychosocial well-being for preventing T2D in women with a history of GDM.
4.3 Strengths and limitations
The present study demonstrates that it was feasible to identify and recruit women with a history of GDM from the larger community settings. Infrastructures were available to collect holistic lifestyle data including sleep and heart rate variability beyond the conventional focus on diet and PA. Regular feedback offered by the Oura Ring may have increased women’s health awareness and enabled them make actionable goals to increase their daily steps count and reduce time spent on being sedentary. The human-technology interface adopted in the present study was feasible for the health coaches to review individuals’ needs in a holistic manner, and allowed them to tailor their recommendations to improve physical health and mental well-being at an individual level. Recommendations delivered in a personalized and targeted manner showed possibility in improving the intake of fruits and vegetables, and reducing intake of added sugar in their diets. The present study also found initial benefits in reducing the levels of depression and anxiety in the women irrespective of randomization. Although some of these initial findings were encouraging, a larger sample size and sufficient follow-up duration are needed to observe health-related benefits.
Several study limitations deserve to be mentioned. The present study does not have sufficient information about women’s pre-pregnancy risk factors and lacks understanding on the influence of low socio-economic status and minority ethnicity on their risk of dysglycemia and other clinical outcomes. The study mobile App was only made available for Android smartphone users, future studies could aim to extend the outreach to include iOS smartphone users. Due to the short duration of the pilot study, the intervention effects on the clinical outcomes cannot be fully examined. Furthermore, women in the Control group who were also at risk of future T2D were given an opportunity to monitor their lifestyle using the Oura Rings which might have narrowed the observed differences between the two groups.
Taken together, the present study supports adopting a holistic approach to understand women’s lifestyle behaviors including sleep and stress beyond the conventional focus on diet and physical activity. Recommendations can be personalized and tailored to promote overall physical health and mental well-being among women with a history of GDM at an individual level. The proposed holistic approach may also be applicable to preventing GDM that shares largely similar risk factors of T2D. Larger studies with sufficient assessment timepoints and longer follow-up duration are warranted to improve the evaluation of intervention effects on the clinical outcomes. It is also crucial to ensure that the minority ethnic groups and women from lower socioeconomic status are well-represented in future studies. An integrated solution could potentially elevate the efficiency of mHealth strategies and benefit stakeholders involved in holistic lifestyle interventions.
5 Conclusions
The holistic approach appeared feasible for developing a holistic understanding of lifestyle behaviors including sleep and stress beyond the conventional focus on diet and PA. Lifestyle recommendations can be personalized and tailored to promote physical and mental well-being among women with a history of GDM. Larger studies with sufficient assessment timepoints, longer follow-up duration and sufficient representation of women from minority ethnic groups and lower socioeconomic status are warranted to improve the evaluation of intervention effects on clinical outcomes.
Data availability statement
The datasets presented in this article are not readily available because Data preparation and analysis involving other component of the study is ongoing. Requests to access the datasets should be directed to amFuaWNlLmxAbnVzLmVkdS5zZw==.
Ethics statement
The studies involving humans were approved by National Healthcare Group (NHG) Domain Specific Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
SL and JE contributed to conception, design of the study and development of the study protocol. YC assessed and evaluated dietary information. MT determined parameters related to women’s metabolic health. SL performed data processing and statistical analysis. SL and CS provided the interpretation of Oura Ring data. SL wrote the first draft of the manuscript and JE provided supervision and reviewed the manuscript. JE obtained the research funding for this study. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by: Human Health and Potential - Prenatal/Early Childhood Grant (Grant number: H22P0M0004) from the Agency for Science, Technology and Research (A*STAR) Singapore, and Human Potential Translational Research Programme, Yong Loo Lin School of Medicine, National University of Singapore, Singapore.
Acknowledgments
We thank the Singapore Institute for Clinical Sciences (SICS) for valuable contributions: data and safety monitoring, conduct of baseline and endpoint assessments at HDRC, delivery of lifestyle recommendations to the Intervention group according to the study protocol using the purpose-built study mobile App and providing support in administrative and logistics matter during this study. We thank the Connectify.AI Pte Ltd for developing the study mobile App important for health coaches to collect dietary information and deliver lifestyle recommendations to the women in the Intervention group.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Bellamy L, Casas JP, Hingorani AD, Williams D. Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet (2009) 373(9677):1773–9. doi: 10.1016/S0140-6736(09)60731-5
2. Xu Y, Shen S, Sun L, Yang H, Jin B, Cao X. Metabolic syndrome risk after gestational diabetes: a systematic review and meta-analysis. PloS One (2014) 9(1):e87863. doi: 10.1371/journal.pone.0087863
3. Zhu Y, Zhang C. Prevalence of gestational diabetes and risk of progression to type 2 diabetes: a global perspective. Curr Diabetes Rep (2016) 16:1–1. doi: 10.1007/s11892-015-0699-x
4. Di Cianni G, Lacaria E, Lencioni C, Resi V. Preventing type 2 diabetes and cardiovascular disease in women with gestational diabetes–the evidence and potential strategies. Diabetes Res Clin Practice (2018) 145:184–92. doi: 10.1016/j.diabres.2018.04.021
5. Kramer CK, Campbell S, Retnakaran R. Gestational diabetes and the risk of cardiovascular disease in women: a systematic review and meta-analysis. Diabetologia (2019) 62:905–14. doi: 10.1007/s00125-019-4840-2
6. Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the international diabetes federation diabetes atlas. Diabetes Res Clin Practice (2019) 157:107843. doi: 10.1016/j.diabres.2019.107843
7. Yuen L, Saeedi P, Riaz M, Karuranga S, Divakar H, Levitt N, et al. Projections of the prevalence of hyperglycaemia in pregnancy in 2019 and beyond: Results from the international diabetes federation diabetes atlas. Diabetes Res Clin Practice (2019) 157:107841. doi: 10.1016/j.diabres.2019.107841
8. Vounzoulaki E, Khunti K, Abner SC, Tan BK, Davies MJ, Gillies CL. Progression to type 2 diabetes in women with a known history of gestational diabetes: systematic review and meta-analysis. BMJ (2020) 369. doi: 10.1136/bmj.m1361
9. Rayanagoudar G, Hashi AA, Zamora J, Khan KS, Hitman GA, Thangaratinam S. Quantification of the type 2 diabetes risk in women with gestational diabetes: a systematic review and meta-analysis of 95,750 women. Diabetologia (2016) 59:1403–11. doi: 10.1007/s00125-016-3927-2
10. Ratner RE, Christophi CA, Metzger BE, Dabelea D, Bennett PH, Pi-Sunyer X, et al. Prevention of diabetes in women with a history of gestational diabetes: effects of metformin and lifestyle interventions. J Clin Endocrinol Metab (2008) 93(12):4774–9. doi: 10.1210/jc.2008-0772
11. Goveia P, Cañon-Montañez W, Santos DD, Lopes GW, Ma RC, Duncan BB, et al. Lifestyle intervention for the prevention of diabetes in women with previous gestational diabetes mellitus: a systematic review and meta-analysis. Front Endocrinology (2018) 9:583. doi: 10.3389/fendo.2018.00583
12. Li N, Yang Y, Cui D, Li C, Ma RC, Li J, et al. Effects of lifestyle intervention on long-term risk of diabetes in women with prior gestational diabetes: A systematic review and meta-analysis of randomized controlled trials. Obes Rev (2021) 22(1):e13122. doi: 10.1111/obr.13122
13. Fiordelli M, Diviani N, Schulz PJ. Mapping mHealth research: a decade of evolution. J Med Internet Res (2013) 15(5):e95. doi: 10.2196/jmir.2430
14. Singapore Health Promotion Board. Health Promotion Board Introduces My Healthy Plate to Inculcate Healthy Eating Habits amongst Singaporeans. Available at: https://www.hpb.gov.sg/newsroom/article/health-promotion-board-introduces-my-healthy-plate-to-inculcate-healthy-eating-habits-amongst-Singaporeans (Accessed on 28th August 2023).
15. Singapore HealthHub. How to eat right to feel right. Available at: https://www.healthhub.sg/live-healthy/15/dietary_guidelines_adults#:~:text=Total%20fat%20should%20be%20limited,with%20palm%2Dbased%20vegetable%20oil (Accessed on 28th August 2023).
16. Beck AT, Steer RA, Brown G. Beck depression inventory–II (BDI-II). psychological assessment. APA PsycTests (1996) 1. doi: 10.1037/t00742-000
17. Spielberger CD, Gonzalez-Reigosa F, Martinez-Urrutia A, Natalicio LF, Natalicio DS. The state-trait anxiety inventory. Rev Interamericana Psicologia/Interamerican J Psychol (1971) 5(3 & 4). doi: 10.30849/rip/ijp.v5i3&4.620
18. Tan KCB. Appropriate body-mass index for asian populations and its implications for policy and intervention strategies. Lancet (2004) 363(9403):157–63. doi: 10.1016/S0140-6736(03)15268-3
19. de Zambotti M, Rosas L, Colrain IM, Baker FC. The sleep of the ring: comparison of the ŌURA sleep tracker against polysomnography. Behav Sleep Med (2019) 17(2):124–36. doi: 10.1080/15402002.2017.1300587
20. Chee NIYN, Ghorbani S, Golkashani HA, Leong RL, Ong JL, Chee MW. Multi-night validation of a sleep tracking ring in adolescents compared with a research actigraph and polysomnography. Nat Sci Sleep (2021) 15. 13:177–90. doi: 10.2147/NSS.S286070
21. Kristiansson E, Fridolfsson J, Arvidsson D, Holmäng A, Börjesson M, Andersson-Hall U. Validation of oura ring energy expenditure and steps in laboratory and free-living. BMC Med Res Methodology (2023) 23(1):1–1. doi: 10.1186/s12874-023-01868-x
22. Ware JE. SF-36 health survey. manual and interpretation guide Vol. 6. . New England Medical Center: The health institute (1993) p. 1–6: 22.
23. Lyubomirsky S, Lepper HS. A measure of subjective happiness: Preliminary reliability and construct validation. Soc Indic Res (1999) 46:137–55. doi: 10.1023/A:1006824100041
24. Lee JWR, Brancati FL, Yeh HC. Trends in the prevalence of type 2 diabetes in asians versus whites: results from the united states national health interview survey, 1997–2008. Diabetes Care (2011) 34(2):353–7. doi: 10.2337/dc10-0746
25. Chen L, Shi L, Zhang D, Chao SM. Peer reviewed: Influence of acculturation on risk for gestational diabetes among asian women. Preventing Chronic Disease (2019) 16. doi: 10.5888/pcd16.190212
26. Rollo ME, Baldwin JN, Hutchesson M, Aguiar EJ, Wynne K, Young A, et al. The feasibility and preliminary efficacy of an eHealth lifestyle program in women with recent gestational diabetes mellitus: a pilot study. Int J Environ Eesearch Public Health (2020) 17(19):7115. doi: 10.3390/ijerph17197115
27. Seely EW, Weitzman PF, Cortes D, Vicente SR, Levkoff SE. Development and feasibility of an app to decrease risk factors for type 2 diabetes in hispanic women with recent gestational diabetes (Hola bebe, adios diabetes): pilot pre-post study. JMIR Formative Res (2020) 4(12):e19677. doi: 10.2196/19677
28. Halligan J, Whelan ME, Roberts N, Farmer AJ. Reducing weight and BMI following gestational diabetes: a systematic review and meta-analysis of digital and telemedicine interventions. BMJ Open Diabetes Res Care (2021) 9(1):e002077. doi: 10.1136/bmjdrc-2020-002077
29. Tandon N, Gupta Y, Kapoor D, Lakshmi JK, Praveen D, Bhattacharya A, et al. Effects of a lifestyle intervention to prevent deterioration in glycemic status among south asian women with recent gestational diabetes: a randomized clinical trial. JAMA Network Open (2022) 5(3): – :e220773. doi: 10.1001/jamanetworkopen.2022.0773
30. Mohammad Rahimi GR, Aminzadeh R, Azimkhani A, Saatchian V. The effect of exercise interventions to improve psychosocial aspects and glycemic control in type 2 diabetic patients: a systematic review and meta-analysis of randomized controlled trials. Biol Res Nursing (2022) 24(1):10–23. doi: 10.1177/10998004211022849
31. Mesarwi O, Polak J, Jun J, Polotsky VY. Sleep disorders and the development of insulin resistance and obesity. Endocrinol Metab Clinics (2013) 42(3):617–34. doi: 10.1016/j.ecl.2013.05.001
32. Hurrle S, Hsu WH. The etiology of oxidative stress in insulin resistance. Biomed J (2017) 40(5):257–62. doi: 10.1016/j.bj.2017.06.007
33. Koren D, Taveras EM. Association of sleep disturbances with obesity, insulin resistance and the metabolic syndrome. Metabolism (2018) 84:67–75. doi: 10.1016/j.metabol.2018.04.001
34. Dennison RA, Chen ES, Green ME, Legard C, Kotecha D, Farmer G, et al. The absolute and relative risk of type 2 diabetes after gestational diabetes: a systematic review and meta-analysis of 129 studies. Diabetes Res Clin Practice (2021) 171:108625. doi: 10.1016/j.diabres.2020.108625
35. Li LJ, Huang L, Tobias DK, Zhang C. Gestational diabetes mellitus among asians–a systematic review from a population health perspective. Front Endocrinology (2022) 13:870. doi: 10.1177/10998004211022849
36. Li Z, Cheng Y, Wang D, Chen H, Chen H, Ming WK, et al. Incidence rate of type 2 diabetes mellitus after gestational diabetes mellitus: a systematic review and meta-analysis of 170,139 women. J Diabetes Res (2020) 2020. doi: 10.1155/2020/3076463
37. Kong AP, Xu G, Brown N, So WY, Ma RC, Chan JC. Diabetes and its comorbidities–where east meets west. Nat Rev Endocrinology (2013) 9(9):537–47. doi: 10.1038/nrendo.2013.102
38. Chen LW, Soh SE, Tint MT, Loy SL, Yap F, Tan KH, et al. Combined analysis of gestational diabetes and maternal weight status from pre-pregnancy through post-delivery in future development of type 2 diabetes. Sci Rep (2021) 11(1):5021. doi: 10.1038/s41598-021-82789-x
39. Hu G, Tian H, Zhang F, Liu H, Zhang C, Zhang S, et al. Tianjin gestational diabetes mellitus prevention program: study design, methods, and 1-year interim report on the feasibility of lifestyle intervention program. Diabetes Res Clin Practice (2012) 98(3):508–17. doi: 10.1016/j.diabres.2012.09.015
40. Shek NW, Ngai CS, Lee CP, Chan JY, Lao TT. Lifestyle modifications in the development of diabetes mellitus and metabolic syndrome in chinese women who had gestational diabetes mellitus: a randomized interventional trial. Arch Gynecology Obstetrics (2014) 289:319–27. doi: 10.1007/s00404-013-2971-0
Keywords: diabetes, gestational diabetes mellitus, feasibility, pilot, randomized controlled trial, holistic, Asian, women
Citation: Liew SJ, Soon CS, Chooi YC, Tint MT and Eriksson JG (2023) A holistic approach to preventing type 2 diabetes in Asian women with a history of gestational diabetes mellitus: a feasibility study and pilot randomized controlled trial. Front. Clin. Diabetes Healthc. 4:1251411. doi: 10.3389/fcdhc.2023.1251411
Received: 01 July 2023; Accepted: 29 August 2023;
Published: 28 September 2023.
Edited by:
Chittaranjan Yajnik, KEM Hospital Research Centre, IndiaReviewed by:
Amelia Caretto, San Raffaele Hospital (IRCCS), ItalyJaakko Tuomilehto, National Institute for Health and Welfare, Finland
Copyright © 2023 Liew, Soon, Chooi, Tint and Eriksson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Johan Gunnar Eriksson, b2JnamdlQG51cy5lZHUuc2c=
 Seaw Jia Liew
Seaw Jia Liew Chun Siong Soon
Chun Siong Soon Yu Chung Chooi
Yu Chung Chooi Mya Thway Tint1,3
Mya Thway Tint1,3