
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Clin. Diabetes Healthc. , 27 January 2023
Sec. Diabetes Health Services and Health Economics
Volume 4 - 2023 | https://doi.org/10.3389/fcdhc.2023.1087303
This article is part of the Research Topic Exercise and Type 2 Diabetes: Reducing Vascular Comorbidities Across Populations View all 4 articles
Introduction: Periodic health checkups (PHCs) represent a unique system in Japan that is useful for the early detection of lifestyle-related diseases and cardiovascular diseases (CVDs). This study aims to investigate the association of PHCs with the hospitalization risk of patients with type 2 diabetes mellitus (T2DM).
Methods: A retrospective cohort study was conducted from April 2013 to December 2015 and included participant information such as CVD history, lifestyle, and whether PHC was conducted in addition to regular medical examinations. Difference in clinical data between patients with and without PHC was examined. Furthermore, Cox regression analysis was performed to investigate the independent association of PHCs with hospitalization.
Results: Herein, 1,256 patients were selected and followed up for 2.35 ± 0.73 years. In the PHC group, body mass index, waist circumference, proportion of patients with a history of CVD, and number of hospitalizations were lower than those in the non-PHC group. Furthermore, the PHC group exhibited a significant association with lower hospitalization risk (hazard ratio = 0.825; 95% confidence interval, 0.684 to 0.997; p = 0.046) in the Cox model.
Conclusion: This study revealed that PHCs minimized the risk of hospitalization in patients with T2DM. Furthermore, we discussed the effectiveness of PHCs in enhancing health outcomes and reducing health care costs in such patients.
Periodic health checkups (PHCs) that are usually conducted annually represent a unique system in Japan created for the early detection of lifestyle-associated diseases and cancer (1). The goal of PHCs is to extend the healthy life span of individuals via early detection and treatment of serious ailments, such as cancer and cardiovascular diseases (CVDs), which is the presumed advantage of conducting PHCs. The rate of cancer detection, including that of suspected cancer cases and confirmed cancer diagnoses in examinees, has been estimated as follows: lung cancer, 0.41% and 6.65%; gastric cancer, 0.7% and 11.36%; and breast cancer, 1.34% and 16.23%; respectively (1). However, overdiagnosis or under diagnosis of the target disease constitute a disadvantage of PHCs (1). However, the effectiveness of PHCs from the perspective of public health and health economics remains unclear. Hackl et al. (2) reported that a general health screening program substantially increased both inpatient and outpatient health care costs in the short-term, reduced outpatient health care cost in the medium-term, and demonstrated no effect on both health care cost and health status in examinees in the long-term. A meta-analysis of 17 randomized trials also showed that health checkups exhibited no effect on all-cause mortality, CVD death rate, and the risk of reducing ischemic heart disease and stroke (3). Thus, the overall effectiveness of PHCs is controversial. However, the efficacy of this system also depends on the method and frequency of application and the appropriate selection of individuals (4).
Cost escalation of health care is a serious problem worldwide. The global economic burden of T2DM will increase to >$2 trillion by 2030 (5). The treatment costs of each patient with T2DM and CVDs increase by $3418–$9705 annually compared with patients with T2DM without CVDs (6). The total cost of cancer treatment has inflated faster than cancer incidence among Europeans (7). Hence, it is important to detect such serious diseases at an early stage to prevent disease progression and reduce health care costs.
Patients with T2DM exhibit physically weakness (8), susceptibility to infections (9), high prevalence of CVDs (10), and increased risk of cancer incidence (11); thus, PHCs may contribute to the reduction of health care costs by the early detection and treatment of such serious diseases requiring hospitalization. However, to the best of our knowledge, no studies have investigated the association of PHCs with the hospitalization risk of patients with T2DM. Therefore, this study aims to analyze the association of PHC with the hospitalization risk of T2DM at a regional core hospital in Japan.
This retrospective cohort study was conducted at National Center for Global Health and Medicine (NCGHM), Kohnodai Hospital, a public, secondary care hospital in Japan. Between April 2013 and December 2015, patients who came to the outpatient department and were diagnosed with T2DM were enquired regarding their medical history. Furthermore, data regarding diabetes and lifestyle-related behaviors after obtaining informed consent from the patients were collected from the Biobank for Metabolic Disorders in the NCGHM Kohnodai Hospital (12) and retrospectively analyzed. As a standard guideline, patient information, such as CVD history, smoking habit, drinking habit, exercise regularity, and whether PHCs were conducted in addition to regular medical examinations, was collected. Regular medical examinations included parameters such as physical measurements of the body, blood pressure (BP) measurement, vision and hearing assessment, routine blood and urine examination, chest X-ray, and electrocardiogram, which were performed at first visit. Patients were excluded if their age was <20 years. Participants were recommended to consume a strict low-calorie diet of 25–30 kcal/kg of ideal body weight at the very first visit by a certified nutritionist. The dietary adherence of the patients was confirmed at every consultation, and the patients followed the diet throughout the research duration. All the participants were assessed and followed up till the end of follow-up up (May 2016) or death. At the end of the follow-up, information regarding hospitalization was collected from the medical record review. The number of hospitalizations was calculated for all the participants. PHCs, which were the primary outcome analyzed, were associated with minimized the hospitalization risk of patients with T2DM. The impact of PHCs on the occurrence of CVDs and all-cause mortality was also examined.
The research design was certified by the Medical Ethics Committee of the NCGHM (Reference No. NCGM-G-002052), this research was conducted as per the Declaration of Helsinki.
PHCs are performed voluntarily and separately from regular medical examinations for patients with T2DM as well as healthy individuals. In Japan, company employees and students have the provision of availing PHCs annually. In addition, Japanese individuals aged between 40 and 74 years are encouraged to undergo annual health checkups that include physical body measurements and examination, BP measurement, blood examination (serum triglycerides, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, aspartate aminotransferase, alanine aminotransferase, γ-glutamyl transpeptidase, and plasma glucose or hemoglobin A1c [HbA1c]) and urine examination (protein and glucose) to prevent the incidence and progression of lifestyle-associated diseases, such as diabetes mellitus, hypertension, and dyslipidemia (13). Although the Japanese health insurance system does not cover these PHCs, companies and schools cover the costs of the PHCs of their employees and students, respectively. In addition, individuals can avail free PHC services provided by some health insurances schemes (e.g., National Health Insurance). The components of the examinations vary depending on the type of health checkup. For example, a complete comprehensive health checkup known as “Ningen Dock” is conducted in Japan. It includes detailed radiological investigations, such as ultrasonography, computed tomography, magnetic resonance imaging, and endoscopic investigations, in addition to routine blood and urine examinations (1).
A rigid stadiometer (TTM stadiometer; Tsutsumi Co., Ltd., Tokyo, Japan) was employed to document the height of the participants and a standard calibrated scale (AD-6107NW; A&D Medical Co., Ltd., Tokyo, Japan) was used to determine the body weight (BW). Body mass index (BMI) was calculated via the standard formula: BW (kg) divided by the square of individual height measured (m). Waist circumference (WC) was measured in centimeter using an inch tape at the umbilical level at the end of expiration from a standing position. A standard automatic sphygmomanometer (HBP-9020; Omron Co., Ltd, Tokyo, Japan) was used to measure the BP in a seated position and sedentary state.
A trained professional from the Clinical Research Center of the NCGHM at Kohnodai Hospital recorded the CVD history of the patients, comprising information such as stroke, nonfatal coronary artery or peripheral artery disease, and foul habits, including smoking and alcoholism, during the baseline evaluation. To quantify the smoking habits of the participants, their Brinkman index was calculated as the number of cigarettes smoked per day multiplied by the number of years of smoking (14). Alcohol consumption (AC) was estimated by the type of liquor and amount consumed daily. Furthermore, we enquired regarding the exercise regularity and type, such as jogging, cycling, and calisthenics, of the participants. Using the available information, we calculated the daily exercise duration. Additionally, patients were asked regarding their daily walk-time, except volitional exercise.
We measured the blood glucose and HbA1c of the participants at the time of enrollment. The glomerular filtration rate (eGFR) of the participants was documented using the revised equation exclusively adjusted for the Japanese patients (15).
As sample size estimation is very vital for such studies, we employed post-hoc sample size estimation using a command comparing survival curves between two independent groups in EZR (16). During this study period, assuming that the hospitalization rates of patients who did and did not undergo PHCs were 38.2% and 48.2%, respectively, the groups were of equal size (1:1 ratio), and the two-tailed level was 0.05. The final sample size was 730 observations needed for a power of 80%. This indicates that the selected sample size had the required power to detect the association between PHCs and hospitalization risk.
Data analyses were conducted using SPSS version 25 (IBM Co., Ltd., Chicago, IL). Continuous variables were presented as the mean ± standard deviation (SD). Student’s t test or the Mann–Whitney test, depending on whether the variables followed normal or non-normal distribution, was preferred to find differences between patients who did and did not undergo PHCs, respectively. Categorical variables were expressed as numbers and compared using χ2 test. The Cox proportional hazard equation was used to examine the independent associations of hospitalization, CVD occurrence, and death with PHCs. We included age, gender, BMI, CVD history, AC, Brinkman index for smoking habit, exercise time, systolic BP (SBP), diastolic BP (DBP), blood glucose, HbA1c, and eGFR in the Cox model. The significance level for the study was fixed at <0.05.
The study recruited 1,256 patients with T2DM, of which 695 were men, 561 were women, and 557 (44.3%) had undergone a PHC. The mean age and BMI were 63.7 ± 13.9 years and 25.5 ± 5.5 kg/m2, respectively. Patient characteristics are presented in Table 1.
BMI, WC, number of patients with CVD history, and number of hospitalizations during the study period were lower in the PHC group than in the non-PHC group. Furthermore, AC, exercise time, and walking time were higher in the PHC group than in the non-PHC group. On an average, patients without PHC were admitted once to our hospital during the study period (Table 2).
During a mean follow-up of 857 ± 267 days, 20 patients (1.6%) died, 14 (1.1%) sustained cardiovascular events, and 550 (43.8%) were admitted to our hospital. The number of patients who were hospitalized at least once was 213 (38.2%) in the PHC group and 337 (48.2%) in the non-PHC group. The total number of hospitalizations was 1092, of which 382 belonged to the PHC group and 710 to the non-PHC group. Of these, 378 (34.6%) belonged to the diabetes, endocrinology, and metabolism ward, 165 (15.1%) to the surgery ward, 135 (12.4%) to the internal medicine ward, 85 (7.8%) to the ophthalmology ward, 79 (7.2%) to the gastroenterology ward, 65 (6.0%) to the hepatology ward, 36 (7.5%) to the cardiology ward, 27 (2.5%) to the respiratory medicine ward, and 122 (11.1%) to other wards, such as neurology, rheumatology, and psychiatry.
Furthermore, Cox proportional hazard analyses with adjustment for age, gender, BMI, CVD history, drinking habit, smoking habit, exercise time, SBP, DBP, blood glucose, HbA1c, and eGFR showed that PHCs exhibited a significant impact on patient hospitalization risk (hazard ratio [HR] = 0.825; 95% confidence interval [CI], 0.684–0.997; p = 0.046); however, there was no significant association of PHCs with CVDs and all-cause mortality (Table 3).
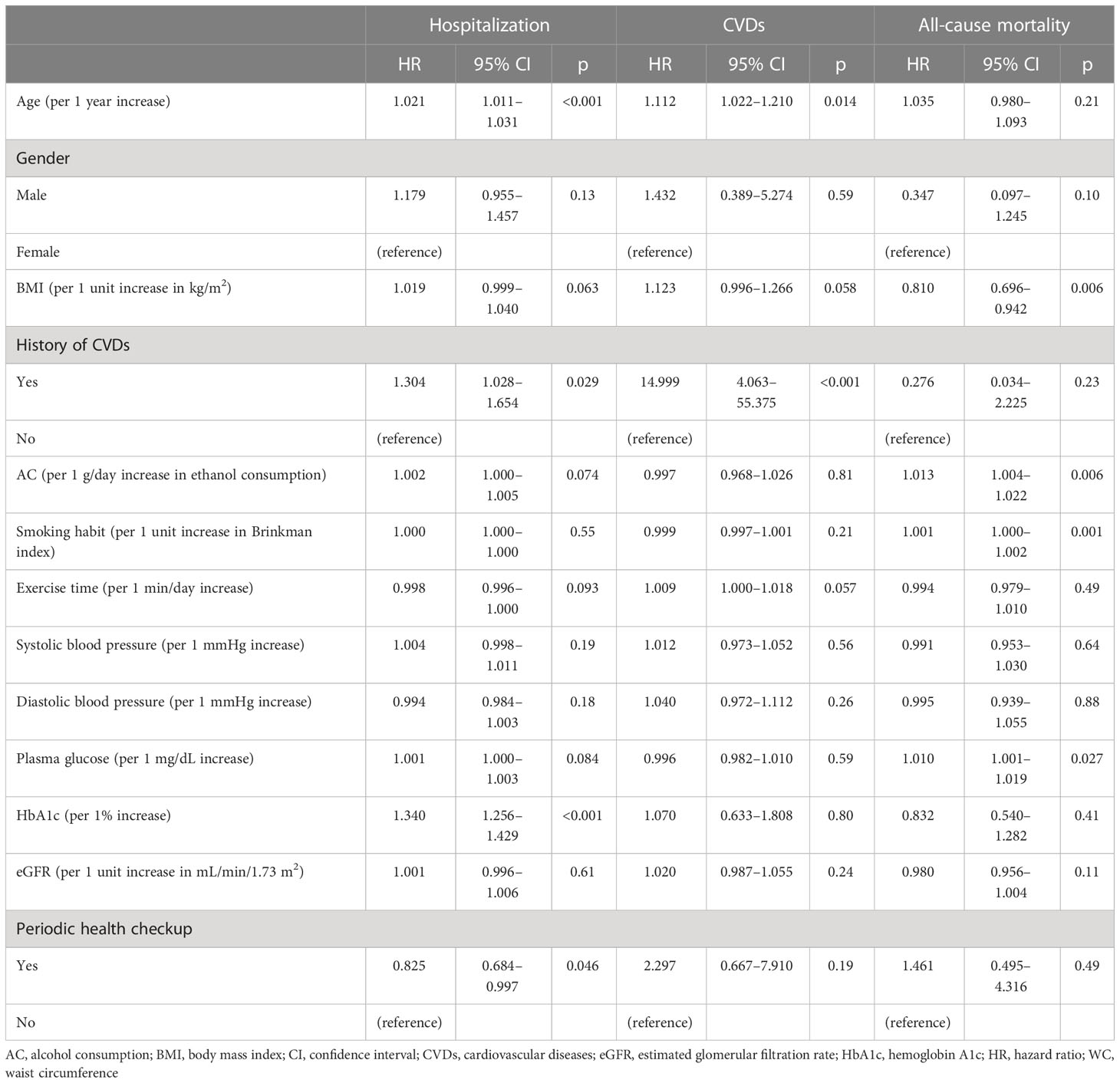
Table 3 Cox proportional hazard analysis for evaluating the association of periodic health checkups with hospitalization, CVDs, and all-cause mortality in patients with type 2 diabetes.
We demonstrated that PHCs can remarkably lower the hospitalization risk of patients with T2DM. Although PHCs were not correlated with CVDs and all-cause mortality, the primary result of the study suggests that PHCs improved health outcomes in patients with T2DM. To the best of our knowledge, this is the first study to demonstrate that all-cause hospitalization could be prevented in patients with T2DM who have undergone a PHC in addition to regular medical examinations.
A previous systematic review and meta-analysis concluded that general PHCs were not beneficial for reducing all-cause mortality and cardiovascular events; however, the studies included were from Western countries (United States, United Kingdom, Denmark, Sweden, Belgium, Poland, Italy, and Montenegro) (3). Ethnic differences should be considered while evaluating the effectiveness of PHCs on health outcomes in patients with T2DM. The average BMI of Japanese individuals with T2DM was 24.8 kg/m² in 2021 (17). The prevalence of a BMI of ≥30 kg/m² varies by country and ranges from 3.7% in Japan to 38.2% in the United States (18). Obese individuals are susceptible to stress-induced eating habits, with a greater preference for high-sugar and high-fat foods (19), which deteriorate metabolic health and results in the development of diseases that require hospitalization. Hence, evidence regarding the effectiveness of PHCs for health in Western countries is not always applicable to Eastern countries such as Japan. In this regard, the findings of the present study are important.
Generally, patients who regularly visit hospitals for chronic diseases undergo PHCs voluntarily in Japan; thus, health consciousness and literacy could also influence their behavior. A systematic review reported that health literacy was a significant determinant of obesity (20). Moreover, adequate health literacy was inversely related to physical inactivity (odds ratio [OR] = 0.48; 95% CI, 0.39–0.59) in individuals with CVDs (21), and patients with diabetes who did not adequately understand health information were sedentary (OR = 3.43; 95% CI, 2.14–5.51) (22). Herein, patients in the PHC group were less obese and more active than patients in the non-PHC group. Furthermore, rate of history of CVD was lesser in the PHC group than in the non-PHC group. These results suggest that patients who underwent PHC exhibited high health literacy and consciously attempted to prevent obesity through increasing daily physical activity, thereby resulting in primary prevention activities against CVDs. Health literacy also constitutes an important factor for the self-management of diabetes in patients with T2DM (23); however, there was no significant difference in HbA1c levels between the groups in this study. The reason behind why chronic glycemic control did not vary between the groups cannot be explained based on the findings of the present study. However, glucose fluctuation, which cannot be assessed by HbA1c levels, appears to encourage the development of cardiovascular events in patients with diabetes than chronic hyperglycemia (24). Furthermore, high plasma glucose levels have been independently associated with inadequate health literacy in patients with T2DM (25). Hence, patients in the non-PHC group could have possibly experienced hypoglycemia and hyperglycemia more often compared with patients in the PHC group. Further studies are warranted to characterize the relationship between PHCs and the rate of health literacy and glycemic control.
A higher AC in the PHC group than in the non-PHC group is inconsistent with the finding that the patients who underwent PHCs were less obese and more active than the patients who did not undergo PHC. However, previous studies have indicated that AC impacted the levels of physical activity in a positive manner (26). Additionally, AC was 19.3 and 17.6 g/day in the PHC and non-PHC groups, respectively, which is not harmful for cancer, CVDs, and mortality in Japanese people (27). Furthermore, even after adjusting AC in the Cox model, PHC was significantly associated with hospitalization risk in this study. Therefore, we propose that PHCs are not directly related to increase in AC.
Treatment costs vary depending on the cause of hospitalization, type and severity of disease, patient condition, and type of health care organization. For example, hospitalization due to uncontrolled diabetes costs ~¥40,000 ($296 at the current exchange rate) per day in our organization (28). Considering that the average length of a hospital stay due to diabetes is 13–14 days in our organization (28), the hospitalization cost is >¥50,0000 ($3,703 at the current exchange rate). Conversely, the cost of PHCs also varies significantly depending on the components of examination. For example, a nationwide annual health checkup to prevent the incidence and progression of lifestyle-associated diseases costs ~¥7,000 ($55 at the current exchange rate) per examination (29), whereas a comprehensive health checkup in our organization, which includes chest X-ray, abdominal ultrasonography, gastroscopy, and some cancer screening tests, in addition to routine blood and urine examinations costs ¥57,000 ($422 at the current exchange rate) for men and ¥64,000 for women ($474 at the current exchange rate) (30). Herein, PHC was equated with a 17.5% reduction in the risk of all-cause hospitalization in patients with T2DM, which is comparable with >¥87,500 ($648 at the current exchange rate) when converted to hospitalization costs due to diabetes. This study is not a randomized controlled trial; however, if the number of patients who would need intervention is calculated as follows: 1/(0.482 − 0.382) = 10, we need to provide PHCs to 10 patients to prevent one additional hospitalization in this study cohort. Thus, comprehensive health checkup may not be cost effective; however, providing a general PHC annually might be cost effective for the managing patients with T2DM who are at a higher risk of hospitalization. Furthermore, the cost of hospitalization due to ischemic heart disease with percutaneous coronary intervention (¥1,100,000; $8,148 at the current exchange rate), acute cerebral infarction (¥1,190,000; $8,814 at the current exchange rate), and cancers, such as lung cancer with chemotherapy (¥610,000; $4,519 at the current exchange rate), are higher than that of hospitalization due to diabetes (28). The recurrence risk of CVDs was significantly high (HR = 14.999; 95% CI, 4.063–55.375; p < 0.001) in this study (Table 3). Patients with T2DM exhibit a high prevalence of CVDs (6), and an increased risk of liver, pancreatic, and endometrial cancers (11); therefore, PHCs that focuses on cardiovascular risks and early detection of such cancers may be beneficial for cost-reduction as well as for improving health and life expectancy in such patients.
However, PHC is not necessary for every healthy individual. Current evidence suggests that regular nationwide health checkups are neither beneficial nor cost effective to improve health outcomes (31). Compared with other developed countries, such as the United Kingdom, Canada, and Sweden, PHCs in Japan cover an unusually wide range and high volume of the population, and it is unclear whether all examinations contribute to the overall health of the population and provide financial benefits (31). The target population for PHCs should be narrowed down to ensure that health care providers can effectively and cost-efficiently apply the results of PHCs in primary and secondary prevention activities for CVDs and cancers. In addition, we need to establish nationwide standardized screening programs that include what, when, to whom, and how PHCs should be administered by considering national and international evidence and best practices to efficiently use limited medical resources (31). In this regard, the findings of this study are highly suggestive. At least, we might as well consider the adoption of PHCs as a secondary prevention strategy in the management of patients with T2DM.
Reducing inequities in health and raising health awareness across all social strata are critical for improving health in patients with T2DM. In Japan, company employees and students can avail PHCs every year at the expense of the company or school, respectively. However, the unemployment rate has been positively associated with reduced PHCs (32). Furthermore, women with lower socioeconomic statuses are less likely to avail cancer screening examinations, which cost ¥500−¥1,000 with municipal subsidies (33). Individuals with low socioeconomic statuses generally exhibit a higher risk of smoking, drinking, physical inactivity, poor nutrition, and not undergoing PHCs (32, 34, 35). Therefore, it is also vital that health promotion policies for PHCs target patients with T2DM with low socioeconomic statuses.
There are several limitations of this study that need to be addressed. First, we did not investigate the components of PHCs. Whether or not the participants have undergone a PHC was gathered from their response to the question “Do you have a PHC except regular medical examinations for diabetes?” Hence, information regarding the type of PHC; for example, general health checkup, cancer screening test, or comprehensive PHC, was lacking. Second, we did not assess the detailed causes of the hospitalizations; for example, the name and severity of the disease. We can speculate that a certain number of hospitalizations were related to diabetes because one third of the total hospitalizations were in the diabetes, endocrinology, and metabolism ward; however, how PHCs were related with the heightened risk of hospitalizations due to a specific disease remains unknown. Third, we assessed the adherence of the participants to the diet therapy by asking the question “Do you stick to the diet therapy?” at the regular medical examinations approximately once a month; however, the adherence rate of the diet therapy should be measured via a specific tool (e.g., diet diary). Fourth, the socioeconomic status and educational level of the participants were not investigated. Individuals with high risk factors, such as smoking, physical inactivity, and low education and socioeconomic statuses, are less likely to attend PHCs than others (28, 29). Such demographic data should be incorporated in future studies.
PHCs exhibit a significant role in minimizing the hospitalization risk of patients with T2DM. PHCs may be useful in improving health outcomes of patients and reduce health care costs when targeting individuals with high risk factors, such as T2DM. Health policy makers need to improve PHC programs by including what, when, to whom, and how PHCs should be administered. Furthermore, a discussion should be conducted to reach a consensus regarding how the results of PHCs can be effectively applied to effectively patient management.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by The Medical Ethics Committee of the National Center for Global Health and Medicine (Reference No. NCGM-G-002052). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
HH conducted the study, performed the data analyses, drafted the manuscript, and revised the manuscript. HY critically reviewed the manuscript and the scientific interpretations of study results. All authors contributed to the article and approved the submitted version.
The authors appreciate the support of Tomoko Kaga and Izumi Omigawa who helped collect the data.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Lu J. Ningen dock: Japan’s unique comprehensive health checkup system for early detection of disease. Glob. Health Med. (2022) 4(1):9–13. doi: 10.35772/ghm.2021.01109
2. Hackl F, Halla M, Hummer M, Pruckner GJ. The effectiveness of health screening. Health Econ (2015) 24(8):913–35. doi: 10.1002/hec.3072
3. Krogsbøll LT, Jørgensen KJ, Gøtzsche PC. General health checks in adults for reducing morbidity and mortality from disease. Cochrane Database Syst. Rev. (2019) 1(1):CD009009. doi: 10.1002/14651858.CD009009.pub3
4. Collen MF. The cost-effectiveness of health checkups–an illustrative study. West J. Med. (1984) 141(6):786–92.
5. Bommer C, Sagalova V, Heesemann E, Manne-Goehler J, Atun R, Bärnighausen T, et al. Global economic burden of diabetes in adults: Projections from 2015 to 2030. Diabetes Care (2018) 41(5):963–70. doi: 10.2337/dc17-1962
6. Einarson TR, Acs A, Ludwig C, Panton UH. Economic burden of cardiovascular disease in type 2 diabetes: A systematic review. Value Health (2018) 21(7):881–90. doi: 10.1016/j.jval.2017.12.019
7. Hofmarcher T, Lindgren P, Wilking N, Jönsson B. The cost of cancer in Europe 2018. Eur. J. Cancer (2020) 129:41–9. doi: 10.1016/j.ejca.2020.01.011
8. Hamasaki H. Daily physical activity and type 2 diabetes: a review. World J. Diabetes (2016) 7(12):243–51. doi: 10.4239/wjd.v7.i12.243
9. Berbudi A, Rahmadika N, Tjahjadi AI, Ruslami R. Type 2 diabetes and its impact on the immune system. Curr. Diabetes Rev. (2020) 16(5):442–9. doi: 10.2174/1573399815666191024085838
10. Einarson TR, Acs A, Ludwig C, Panton UH. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007-2017. Cardiovasc. Diabetol. (2018) 17(1):83. doi: 10.1186/s12933-018-0728-6
11. Ling S, Brown K, Miksza JK, Howells L, Morrison A, Issa E, et al. Association of type 2 diabetes with cancer: A meta-analysis with bias analysis for unmeasured confounding in 151 cohorts comprising 32 million people. Diabetes Care (2020) 43(9):2313–22. doi: 10.2337/dc20-0204
12. Yanai H, Takano Y, Adachi H, Kawaguchi A, Hakoshima M, Waragai Y, et al. Data collection and the questionnaires for the effective use of biobank for metabolic disorders. J. Endocrinol. Metab. (2017) 7(1):1–4. doi: 10.14740/jem400w
13. Ministry of Health, Labour and Welfare. Concept of health checkups and guidance. Available at: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/kenkou_iryou/kenkou/seikatsu/index.html (Accessed 8 April 2022).
14. Brinkman GL, Coates EO Jr. The effect of bronchitis, smoking, and occupation on ventilation. Am. Rev. Respir. Dis. (1963) 87:684–93. doi: 10.1164/arrd.1963.87.5.684
15. Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Collaborators developing the Japanese equation for estimated GFR. revised equations for estimated GFR from serum creatinine in Japan. Am. J. Kidney Dis. (2009) 53(6):982–92. doi: 10.1053/j.ajkd.2008.12.034
16. Kanda Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant. (2013) 48(3):452–8. doi: 10.1038/bmt.2012.244
17. Japan Diabetes Clinical Data Management Study Group. Basic statistics in 2021. mean BMI. Available at: http://jddm.jp/public-information/index-2021/ (Accessed 25 November 2022).
18. Blüher M. Obesity: global epidemiology and pathogenesis. Nat. Rev. Endocrinol. (2019) 15(5):288–98. doi: 10.1038/s41574-019-0176-8
19. Torres SJ, Nowson CA. Relationship between stress, eating behavior, and obesity. Nutrition (2007) 23(11-12):887–94. doi: 10.1016/j.nut.2007.08.008
20. Chrissini MK, Panagiotakos DB. Health literacy as a determinant of childhood and adult obesity: A systematic review. Int. J. Adolesc. Med. Health (2021) 33(3):9–39. doi: 10.1515/ijamh-2020-0275
21. Aaby A, Friis K, Christensen B, Rowlands G, Maindal HT. Health literacy is associated with health behaviour and self-reported health: A large population-based study in individuals with cardiovascular disease. Eur. J. Prev. Cardiol. (2017) 24(17):1880–8. doi: 10.1177/2047487317729538
22. Friis K, Vind BD, Simmons RK, Maindal HT. The relationship between health literacy and health behaviour in people with diabetes: a Danish population-based study. J. Diabetes Res. (2016) 2016:7823130. doi: 10.1155/2016/7823130
23. Nam S, Chesla C, Stotts NA, Kroon L, Janson SL. Barriers to diabetes management: patient and provider factors. Diabetes Res. Clin. Pract. (2011) 93(1):1–9. doi: 10.1016/j.diabres.2011.02.002
24. Nusca A, Tuccinardi D, Albano M, Cavallaro C, Ricottini E, Manfrini S, et al. Glycemic variability in the development of cardiovascular complications in diabetes. Diabetes Metab. Res. Rev. (2018) 34(8):e3047. doi: 10.1002/dmrr.3047
25. Sarkar U, Karter AJ, Liu JY, Moffet HH, Adler NE, Schillinger D. Hypoglycemia is more common among type 2 diabetes patients with limited health literacy: The diabetes study of northern California (DISTANCE). J. Gen. Intern. Med. (2010) 25(9):962–8. doi: 10.1007/s11606-010-1389-7
26. Dodge T, Clarke P, Dwan R. The relationship between physical activity and alcohol use among adults in the united states. Am. J. Health Promot (2017) 31(2):97–108. doi: 10.1177/0890117116664710
27. Lin Y, Kikuchi S, Tamakoshi A, Wakai K, Kawamura T, Iso H, et al. Alcohol consumption and mortality among middle-aged and elderly Japanese men and women. Ann. Epidemiol. (2005) 15(8):590–7. doi: 10.1016/j.annepidem.2004.10.010
28. National Canter for Global Health and Medicine. Table of average cost of inpatient cases. Available at: http://www.hosp.ncgm.go.jp/en/inpatient/070/index.html (Accessed 20 April 2022).
29. Japan Health Insurance Association. Medical examination, health instruction. rate. Available at: https://www.kyoukaikenpo.or.jp.e.ame.hp.transer.com/g4/cat410/sb4030/r91/ (Accessed 8 April 2022).
30. National Canter for Global Health and Medicine. Medical examination center. examination items and prices. Available at: http://www.hosp.ncgm.go.jp/en/mec/menu.html (Accessed 20 April 2022).
31. Organization for Economic Co-operation and Development. OECD reviews of public health: Japan: A healthier tomorrow. Paris: OECD Publishing (2019). doi: 10.1787/9789264311602-en
32. Fukuda Y, Nakamura K, Takano T. Accumulation of health risk behaviours is associated with lower socioeconomic status and women's urban residence: A multilevel analysis in Japan. BMC Public Health (2005) 5:53. doi: 10.1186/1471-2458-5-53
33. Fukuda Y, Nakamura K, Takano T. Reduced likelihood of cancer screening among women in urban areas and with low socio-economic status: A multilevel analysis in Japan. Public Health (2005) 119(10):875–84. doi: 10.1016/j.puhe.2005.03.013
34. Hoebel J, Starker A, Jordan S, Richter M, Lampert T. Determinants of health check attendance in adults: findings from the cross-sectional German health update (GEDA) study. BMC Public Health (2014) 14:913. doi: 10.1186/1471-2458-14-913
Keywords: periodic health checkup, type 2 diabetes, hospitalization, cardiovascular disease, cost-effectiveness
Citation: Hamasaki H and Yanai H (2023) Periodic health checkups reduce the risk of hospitalization in patients with type 2 diabetes. Front. Clin. Diabetes Healthc. 4:1087303. doi: 10.3389/fcdhc.2023.1087303
Received: 02 November 2022; Accepted: 05 January 2023;
Published: 27 January 2023.
Edited by:
Ali A. Rizvi, University of Central Florida, United StatesReviewed by:
Claudia Huber, University of Applied Sciences and Arts Western Switzerland (Fribourg(Fribourg), SwitzerlandCopyright © 2023 Hamasaki and Yanai. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hidetaka Hamasaki, aC1oYW1hc2FraUB1bWluLmFjLmpw
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.