- 1HES-SO University of Applied Sciences and Arts Western Switzerland, School of Health Science Fribourg, Fribourg, Switzerland
- 2Florence Nightingale Faculty of Nursing, Midwifery & Palliative Care, King’s College London, James Clerk Maxwell Building, London, United Kingdom
- 3Institute of Higher Education and Research in Healthcare, University of Lausanne, Lausanne, Switzerland
The integration of self-management education and support into the routine diabetes care is essential in preventing complications. Currently, however, there is no consensus on how to conceptualise integration in relation to self-management education and support. Therefore, this synthesis presents a framework conceptualising integration and self-management.
Methods: Seven electronic databases (Medline, HMIC, PsycINFO, CINAHL, ERIC, Scopus and Web of Science) were searched. Twenty-one articles met the inclusion criteria. Data were synthesised using principles of critical interpretive synthesis to build the conceptual framework. The framework was presented to 49 diabetes specialist nurses working at different levels of care during a multilingual workshop.
Results: A conceptual framework is proposed in which integration is influenced by five interacting components: the programme ethos of the diabetes self-management education and support intervention (content and delivery), care system organisation (the framework in which such interventions are delivered), adapting to context (the aspects of the people receiving and delivering the interventions), interpersonal relationship (the interactions between the deliverer and receiver of the intervention), and shared learning (what deliverer and receiver gain from the interactions). The critical inputs from the workshop participants related to the different priorities given to the components according to their sociolinguistic and educational experiences, Overall, they agreed with the conceptualisation of the components and their content specific to diabetes self-management education and support.
Discussion: Integration was conceptualised in terms of the relational, ethical, learning, contextual adapting, and systemic organisational aspects of the intervention. It remains uncertain which prioritised interactions of components and to what extent these may moderate the integration of self-management education and support into routine care; in turn, the level of integration observed in each of the components may moderate the impact of these interventions, which may also apply to the impact of the professional training.
Conclusion: This synthesis provides a theoretical framework that conceptualises integration in the context of diabetes self-management education and support in routine care. More research is required to evaluate how the components identified in the framework can be addressed in clinical practice to assess whether improvements in self-management education and support can be effectively realised in this population.
Introduction
A large number of people living with type 2 diabetes mellitus – a debilitating long-term metabolic condition – develop chronic complications related to micro- and macrovascular damage (1). These severe long-term health deficits are hallmarks of the length and gravity of metabolic dysfunctions in type 2 diabetes (2). In 2015, the Global Burden of Disease Study identified diabetes as the 6th leading cause of disability, with an increasing incidence among people of working age (3). This global rise of diabetes disability is mostly due to type 2 diabetes, which accounts for 90% of the estimated 422 million people living with diabetes worldwide (4). This means that more and more people are living more years with functional health impairments – which has far-reaching implications for the wellbeing of individuals and their families, and also for the delivery of health care services and the financing of health systems.
It is well known that lowering blood glucose levels has beneficial effects on micro- and macrovascular complications and that people benefit from early detection and the intensive patient-centred management of type 2 diabetes (5–8). However, as a recent study conducted in a large integrated health care system showed, in more than half of their study population the initiation of antihyperglycemic therapy was delayed by at least 6 months; and this despite evidence that delayed therapy initiation is generally associated with poorer glycaemic control and a higher risk of complications (9).
Besides prescription medicines, there is strong evidence that diabetes self-management education and support (DSMES) is effective in improving glycaemic control and patient-related outcome measures, especially when combined with psychosocial interventions, as well as being cost-effective (10–13). However, despite the demonstrated benefits, participation in DSMES remains low (14–16). This strongly suggests that DSMES is not yet fully integrated into routine health care although it is recommended in most national and international guidelines (17). Higher attendance rates in DSMES were observed in systems with structured health care provision. For example, disease management programmes with structured DSME for type 1 and type 2 diabetes were introduced in Germany in 2003. There are similarities between DSMES in type 1 and in type 2 diabetes, however approaches used vary considerably between the different types of diabetes and the target populations (18). The focus of type-2-diabetes DSMES is often on lifestyle changes (exercise and weight loss), which is distinct from the focus in type 1 diabetes. As the 2020 evaluation of the type 2 diabetes cohort in Germany showed, DSMES participation rates in the age group up to 30 years increased to almost 60% in the first year of enrolment in a disease management programme, with a high drop over the following years (19). This indicates that more integrated structures and continuous support may be important features to improve the uptake and outcome of DSMES in both type 1 and type 2 diabetes. The DSMES interventions have multiple facets influenced by the characteristics, activities and interactions of the people living with diabetes, the healthcare professionals involved in delivery, and the health care systems themselves – all of which may hinder or facilitate the integration of a person-centred approach to DSMES into routine care (20). There is a wide agreement that such an approach respects and responds to needs, values and preferences of people with diabetes and that their values should guide the clinical decision process (21). However, there is less understanding on how to implement this approach in routine care. For example, whilst person-centredness is a core element of care, in daily practice healthcare professionals may be ambivalent about encouraging people with diabetes to express their emotional and psychosocial concerns in the limited time they have available during consultations (22, 23). This relative disregard highlights the importance of creating conditions that include person-centredness in care delivery. Such conditions are generally advocated in integrated care systems which are considered essential in improving care for people with chronic conditions who require ongoing care and support (24–26).
Integrated care is largely expected to achieve better outcomes, experiences and use of resources through shared responsibilities of healthcare professionals coordinated across care facilities and support systems (27, 28). In many health care systems, evaluations of integrated care interventions have shown equivocal results due to the broad range of activities and concepts associated with integrated care, which is a complex concept with no agreed definition (29, 30). The concept has been related to integrated care processes that build a whole-system approach of coordinated care delivery, as well as conceptual components that share an integrated whole-care philosophy of healthcare professionals’ collaboration (28, 29, 31–33). For the purpose of this study, this widely used definition of integration in health care delivery is used: “a coherent set of methods and models on the funding, administrative, organisational, service delivery and clinical levels designed to create connectivity, alignment and collaboration within and between the cure and care sectors” (32). These multiple interactions may be affected by the different underlying approaches of healthcare professionals providing elements of DSMES within a fragmented delivery of health services that may further impede person-centred support (34–37). To address these shortcomings, it is important to understand these multiple interactions and identify the essential components of integration in the context of DSMES in routine care.
This study uses the theory of complex adaptive systems (CAS) to explore the different components of integrating DSMES in the often complex and multifaceted situations in routine care. The CAS’s main features are emergent behaviours, self-organisation, co-evolution using simple rules and non-linear processes that represent interacting systems in health care (38–40). These perspectives are used in contexts that face disordered and uncertain conditions to understand the behaviour of systems and identify components that explain their interactions and relationships (41–49). Several aspects of the CAS perspective have been used, for example, to explore the transformative processes in the experiential participatory learning processes of DSMES and identity the mutual influences of healthcare professionals and people with diabetes towards a new context-specific relationship (50–53). These relationships continue to develop during interactions, shaping the kind of consensus-building required in the processes of shared decision-making and promoting the exchange of skills and competencies (54, 55). Considering these features helps understand the multiple dynamic interactions influencing DSMES and the level of integration along the different axes of integrated care which are also considered in the Chronic Care Model (32, 56).
This study aims are to conceptualise integration in relation to DSMES from a CAS perspective and to propose a theoretical model that can serve as starting point for developing a shared understanding of integration within the healthcare professional community.
Methods
The guidance for Undertaking Reviews in Health Care was used to inform the development of the search strategy, identify inclusion and exclusion criteria, select studies and extract the data (57). Principles from critical interpretive synthesis were used for data synthesis (58). This transformation-based approach incorporates elements of conventional systematic reviews with an interpretative and critical approach to data synthesis and is well suited to developing new theoretical models (59). Within this configurative qualitative evidence synthesis, concepts from included qualitative and quantitative articles were extracted and examined across studies in terms of similarities and differences to develop a theoretical proposal (60). This approach of synthesising concepts allowed the researchers to build a line of argumentation, define the synthesising “integration” argument and develop a model of integrated self-management education and support in routine care.
Review Question and Searching the Literature
Several preliminary searches identified that the term “integration” was mainly related to integrated care with tendencies towards linking similar levels of care (multi-professional teams) and different levels of care delivery (primary, secondary and tertiary care) to collaborate in and coordinate the processes of integrated care for improved continuity, access, quality, user satisfaction and efficiency. However, some studies reported conditions and features of DSMES to extrapolate data for developing the components of integration in this context. After team discussion, the review was guided by the following review question: What are the essential components of integration in relation to DSMES and how do they manifest themselves (considering structures of DSMES, context and participant experience)?
The search strategy was developed in collaboration with a librarian according to the principles of critical interpretive synthesis and used to specifically identify articles relevant to the conceptualisation in the following databases from 2004 to 2014 with a search update in January 2022: 1) Medical Literature Analysis and Retrieval System Online (Medline), Current Index to Nursing and Allied Health Literature (CINAHL), Psychological Information Database (PsycINFO), Health Management Information Consortium (HMIC), Education Resources Information Centre (ERIC), Scopus, Web of Science; 2) hand-searching of the bibliographies of retrieved articles and grey literature and 3) identifying articles through colleagues with experience in this field (58, 61). The databases were searched for relevant literature, using both the Medical Subject Headings (MeSH) and free-text keywords that referred to self-management, education and support, type 2 diabetes, integration, and interdisciplinary teams. Validated methodological filters for capturing quantitative and qualitative articles were identified by consulting the librarian and various guidelines (62, 63). The syntax of the search terms was adapted for each database. The citations were exported to Endnote (version x7), and all duplicates were removed.
Inclusion and Exclusion Criteria
The inclusion and exclusion criteria were developed to capture empirical studies (qualitative and interventional study designs) representing components of integration in relation to DSMES into routine care. The main inclusion criteria were a description of the integration of DSMES into routine care and/or research evidence to extrapolate such an integration. The articles were limited to those that a) described at least two instances of integration (considering structures, context and participant experiences); b) included a clear description or definition of DSMES based on research evidence; c) defined linkages to an interprofessional team (including peers); d) demonstrated continuous DSMES in different settings of care delivery with evident linkages to a community, to primary/secondary/tertiary care or to a virtual network for ongoing support; and e) addressed DSMES to adult participants (≥ 18 years of age) with diagnosed type 2 diabetes and defined the healthcare professionals who delivered DSMES to these participants. Articles with access to the full text were included. Articles published before 2004 or in languages other than English, French and German, or without an English abstract, were excluded.
Sampling
All titles and abstracts were initially assessed by one reviewer for their relevance to contributing to the conceptualisation of the integration of DSMES into routine care. At this stage, articles were rated as “irrelevant”, “of uncertain relevance” or “probably relevant” using the inclusion/exclusion criteria. A random selection of 5% was checked for relevance by a second reviewer. The articles rated as “of uncertain relevance” and “probably relevant” were further assessed. A formal test of interrater agreement was not conducted, but the results from each reviewer were discussed in two meetings and all articles were compared in detail in terms of their theoretical contribution to the conceptualisation until a high level of mutual agreement had been reached. According to the principles of a critical interpretive synthesis, articles were included based on their conceptual quality, which means that the identified articles provided content relevant to the review questions (58).
Determination of Quality
The articles were assessed using the five quality criteria associated with the likely relevance of an article as described for critical interpretative synthesis (58): 1) clearly stated aim and objectives of the research; 2) clearly specified research design, appropriate for the aims and objectives of the research; 3) researchers provided a clear account of the process by which their findings were produced; 4) enough data displayed to support their interpretations and conclusions; and 5) appropriate method of analysis and adequate explication (64). Consistent with this approach, articles with lower relevance or methodological limitations were discussed by the reviewers.
Data Extraction
The following data were extracted from the selected articles: author, year, country, study design, purpose/aim, sample setting, participants (i.e. receivers of the intervention) and healthcare professionals (i.e. deliverers of the intervention); in addition, the following information was extracted from the quantitative articles: intervention, including theoretical framework, follow-up, control, primary outcome and, if available, patient-reported outcomes; and from the qualitative studies: participant eligibility criteria, recruitment context, data collection methods, data analysis, and identified themes and sub-themes.
Data Analysis and Synthesis
The data from the full-text articles were coded for pertinent information by one researcher and 5% of the data coding was reviewed by a second researcher. After the coding of each article, a critique reflecting the comments of each article was recorded to capture the different ways in which the literature had conceptualised the integration of DSMES into routine care. To facilitate the processes of discovering the themes and patterns emerging from the articles, the data were imported into NVivo 11 software for sorting, classifying, and arranging the information. The synthesis in this review was organised around the core construct of integration related to DSMES in routine care.
The synthesis used four overlapping steps as transforming techniques for qualitative and quantitative articles (58, 65). First, the coding was analysed to identify themes that capture the content of integration from the relevant information of the articles. Second, the themes were compared with the data of each article and the initial concepts examined in terms of similarities and differences across articles. Third, the patterns were expressed as a transformed conceptualisation, that in critical interpretive synthesis is known as a synthetic construct. This developed as a critique of the literature, expressing contradictions and flaws in the evidence. Fourth, the identified concepts and critique were integrated into a theoretical framework in order to produce the synthesising argument which links the constructs to the themes. The synthesis integrates the evidence with the components of integration and interprets their interactions in the context of DSMES in routine care. The synthesis was done by one researcher and regularly discussed with a second researcher and team members to interpret the emerging findings. The saturation of themes and their repetition across data sets were discussed among researchers who used reflexivity at each stage of the data analysis and synthesis (66).
Establishing Face Validity of the Theoretical Model
With the conceptual model having been developed through the literature and input from experts, the model was then presented and discussed in the nurse community to assess its face validity and acceptability (67). The conceptual model was presented and discussed in a workshop with diabetes specialist nurses working in primary, secondary and tertiary care in Switzerland. The workshop was simultaneously translated between German and French. The workshop participants were asked for verbal informed consent before the workshop started, explaining to them that their participation entailed the discussion of the conceptual model by answering two open-ended questions. The rounds of discussion were analysed directly during the workshop using a concept mapping approach (68. With this approach, concept mapping and note-taking were shared with the participants for immediate feedback at the end of the workshop.
Before the workshop, the model of integrated self-management education and support was briefly explained to the participants (10 minutes), then the workshop was opened by asking two open-ended questions:
1. How and why (or why not) do the components represent integration in relation to DSMES from your viewpoint?
2. How would you rate the importance of each of the components and which additional components, that promote self-management, are missing in the model from your viewpoint?
The participants first discussed each question in small groups of a maximum of 5 people (sitting at the same table) and then one person from each group summarised the most important points and presented them to the whole group while two facilitators wrote down the keywords (2 x 15 minutes). Afterwards, the components were discussed in the whole group, synthesised and validated with regard to the linguistic subtleties and the different interpretations for an additional 15 minutes. The facilitators gave the participants feedback of their understanding with simultaneous translation between German and French. The participants added commentaries until consensus was reached within and between the two linguistic groups.
Results
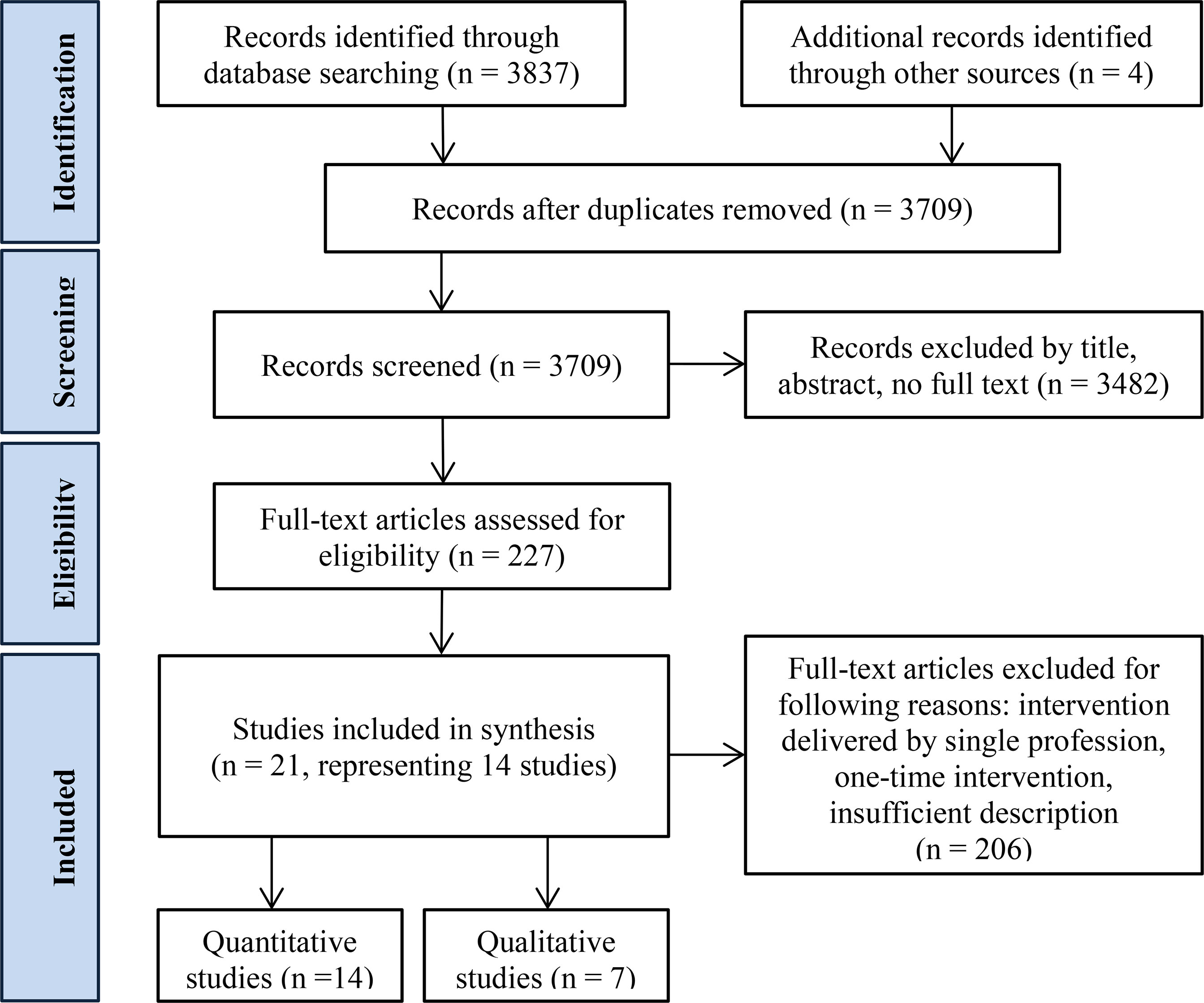
The electronic bibliographic database search yielded 3709 articles for screening after excluding 132 duplicates and adding four records identified through other sources. Full texts were obtained for 227 articles, of which 206 articles were excluded for the following reasons: intervention delivered by one profession without a connecting network, one-time intervention, insufficient description.
Altogether, 21 articles were found to be relevant for conceptualisation, of which 14 had interventional study designs, and seven were qualitative. These 21 articles represented 14 studies covering DSMES in the following settings: community care, primary care, secondary care, tertiary care, and pharmacies. The flow chart in Figure 1 illustrates the study selection process (69).
Characteristics of Relevant Studies
The articles all originated from industrialised countries: Australia (70, 71), Belgium (72, 73), France (74, 75), Italy (76), the Netherlands (77), Norway (78, 79), South Korea (80), Sweden (81–83), the UK (84–86) and the USA (87–90). The characteristics of the study designs, contexts and participants, together with the key concepts and themes related to integration, are presented in tables as Supplementary Material. The qualitative articles had clear research aims and an adequately described methodology. The quality score of the quantitative studies varied from medium to low. Because in critical interpretive synthesis conceptual relevance is more important than methodological rigour (58), all selected articles were included in the review. The contributions of each article to the conceptualisation of the components of integration are represented in Table 1.
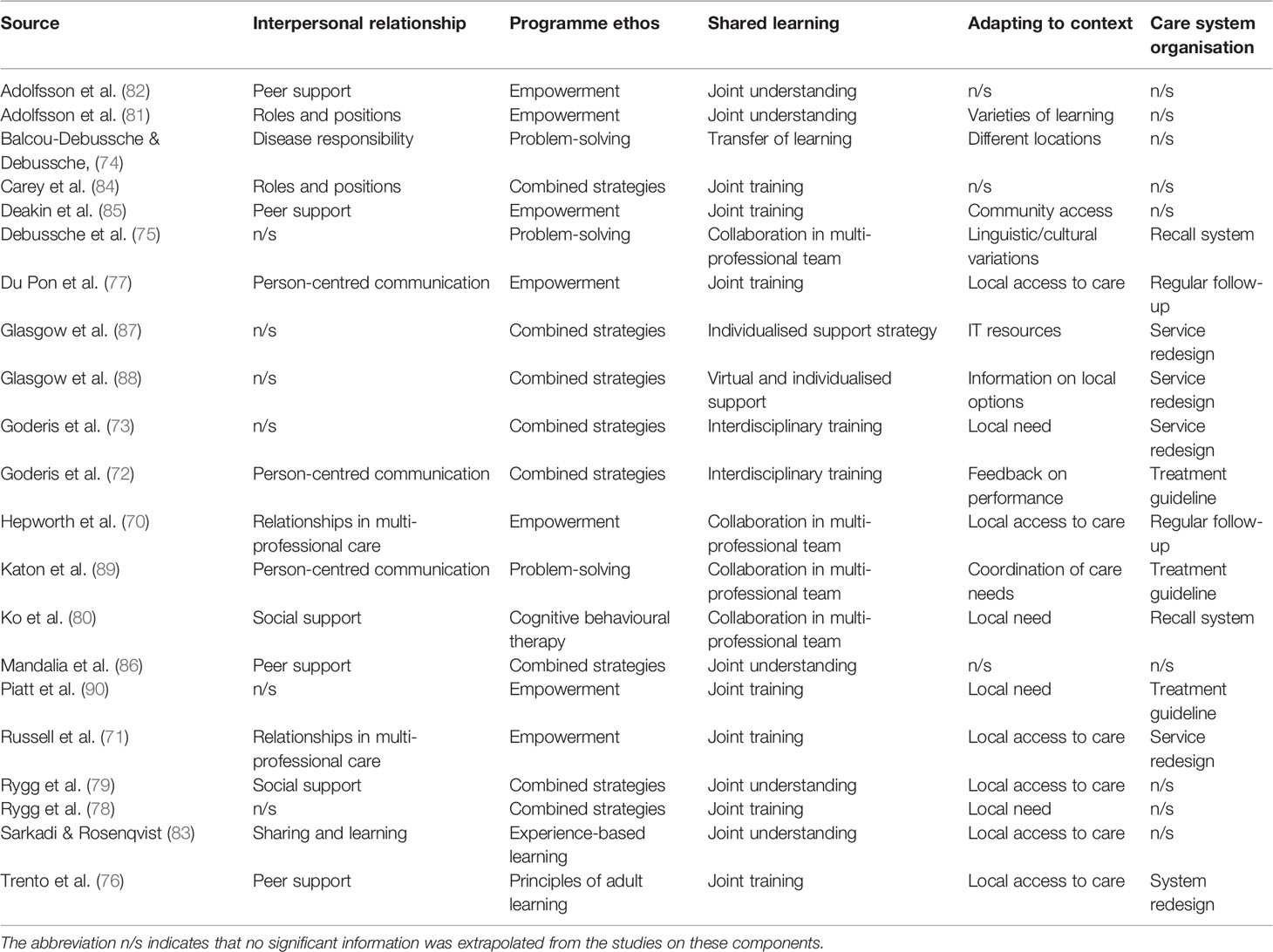
Table 1 Contributions of the studies to the conceptualising of the components of the integration of DSMES into routine care.
The five components of integration in the context of DSMES are presented to explain how the theoretical framework links to the key concepts identified in the articles.
Integration Is Constructed Through Interpersonal Relationship
The literature emphasised the importance of interpersonal relationships in DSMES as a key feature to mediate the extent to which people with diabetes participate in self-management behaviours (70, 71, 74, 76, 77, 79, 81–86). It was evident that the different roles and positions as well as the manner in which healthcare professionals developed relationships with people with diabetes influenced these interactions. Intent to support people with diabetes in their self-management behaviour was prevalent in the interactions described in the studies. In one study however, primarily the number of medical appointments was increasing, while participation in programmes of self-management education remained low (71). In that context, the general practitioner-led intervention encouraging people with diabetes to participate in self-management, the participants of the intervention group were three times more likely to achieve their treatment goals within a 12-month period; however, their use of health care services was three times higher than in the control group, while overall participation in DSMES programmes remained low and their self-efficacy did not improve in either the intervention or control groups (71). This contradiction may be due to the way in which some healthcare professionals tend to communicate their support: imparting knowledge as they learned it during their own training, tending to give information and being more verbally active than the chronically ill person with the support needs (74). Furthermore, DSMES programmes with short durations may not be sufficient to increase confidence and self-efficacy in people with diabetes to participate in consultations with healthcare professionals (77).
The extent to which a person-centred approach is put into place by healthcare professionals may relate to their understanding and appreciation of patient participation and thus influence their roles and positioning during their interactions. The involvement of a peer person may bring in new aspects and help the healthcare professionals to understand the patient perspective and train their listening skills (76, 84–86). The different insights of healthcare professionals and peers are complementary and, therefore, might be an ideal training ground for improved DSMES. Furthermore, adding peer support to group consultations helped to maintain favourable clinical and psychological outcomes over a longer time (76). Another option identified in the literature was using reflective strategies in simulations and discussions to encourage healthcare professionals to think about patient disease experiences (72, 81–83, 89). There was some evidence from the literature that experiential participatory learning raised some healthcare professionals’ awareness of their own training needs, although this was not explicitly stated. Observational data obtained from videotaped training sessions, for example, indicated that some healthcare professionals rarely asked open-ended questions to encourage patients’ own problem-solving processes and insufficiently used listening skills which elicited some concern about the implementation of DSMES (82).
All in all, interpersonal relationship is critical in the interactions between healthcare professionals and people with diabetes and influences the roles and positions in the DSMES learning experience. This construct is decisive for effectively integrating DSMES into routine care. These relationships may be shaped by whether healthcare professionals have been trained in person-centred care delivery, which may help them support people with diabetes according to their individual needs.
Integration Is Shaped by the Underpinning Ethos of Programme
An essential factor in shaping how integration was implemented in care delivery related to the prevailing educational ethos and the underpinning psycho-educational theories of DSMES programmes. A myriad of psychological approaches and educational models existed and they were often combined in different ways (70–90). Widely used approaches within these articles included empowerment-based models with problem-solving strategies. Another commonly used theoretical approach combined social-cognitive theory with an emphasis on self-regulation and self-determination. Psychological approaches, for example, the transtheoretical model of behaviour change, some cognitive behavioural therapy techniques and motivational interviewing were combined with adult-based learning techniques, such as experience-based learning and persuasion techniques. It was found that the solid theoretical background of DSMES benefited the person with diabetes because the interactions during consultations were more comprehensible and focused on their needs. At the same time, the interventions of DSMES were clearly structured and thus replicable in population groups with similar needs identified elsewhere by different healthcare professionals.
An important feature was the training of the healthcare professionals who delivered DSMES, although it might have been challenging for some to choose the most suitable strategy from the variety of available strategies; all the more so since the most promising DSMES often involved a combination of different strategies. Furthermore, the literature implied that these forms of person-centred provision may not be sustained over time, especially when provided for a short period and disconnected from the ongoing care experiences of people with diabetes (74, 77). In situations where people with diabetes experience encouragement only in the context of DSMES, they, but also healthcare professionals, may become disengaged because the ethos of self-management support does not infuse into routine care. Rather than pointing at the inadequacy of DSMES, this may indicate a failure to adequately integrate the experience of DSMES with the ongoing patient care.
Altogether, programme ethos, which provides the philosophical underpinnings of how education and support are delivered in DSMES, influences how people with diabetes experience the delivery of DSMES and how they integrate self-management behaviour into their daily lives. The ethos of a programme plays an important role in facilitating the translation of programme content into practiced health behaviours. While many DSMES interventions tend to impart knowledge of disease and treatment, learning how to live with the disease may encourage people with diabetes to transfer this experience into their life context because the understanding becomes relevant for them. The extent to which the relevance of DSMES persists beyond the initial initiative may relate to the mechanisms within DSMES that enable people with diabetes to connect with their daily lives, the personal goals they have developed, and with their ongoing interactions with healthcare professionals.
Integration Is Created Through Shared Learning
Shared learning experiences promoted collaboration between multiple healthcare professionals and helped them to develop a common understanding of DSMES across different settings of care delivery (70, 75, 78, 80, 89). DSMES was provided in a wide variety of settings, including community venues (85), pharmacies (83), primary care (70–73, 77, 81, 82, 84, 86–90), and hospital inpatient and outpatient clinics (74–76, 78–80). From the literature, it appeared that the different settings created specific situations and social relations that consciously or subconsciously resonated when the term DSMES was used and, therefore, influenced how people with diabetes experienced DSMES (74). Some might have perceived hospital settings to represent illness and treatment, while associating community settings with neighbourhood support (74). It is important that healthcare professionals from the various settings exchange information regularly, whether through joint case discussions or coaching (71, 72). Establishing channels of good communication between the healthcare professionals and the different sectors of care is crucial, particularly as the primary care sector is increasingly accountable for diabetes management.
Building up collaborative care requires investments in time and effort. Joining processes and structures for service delivery, open communication and a mutual understanding of DSMES nurtured the collaboration of the different disciplines involved in patient care, which in turn may have improved the patient experience (70–73, 75–78, 80, 82–84, 86, 89, 90). However, multi-professional training for healthcare professionals as a format for conveying an understanding of a person-centred approach to DSMES has not yet been widely used. This is all the more important because DSMES, especially in people with diabetes who have developed late complications, necessitates continuous encouragement so that they learn how to cope with impairments in everyday life.
Overall, the component of shared learning refers to the conditions that foster collaborative care and may be promoted in multi-professional trainings of healthcare professionals. This conceptualisation may be extended to include people with diabetes as they relate their experiences to the care setting. Shared learning thus promotes collaboration and an integrated care experience that may be facilitated through coordinated DSMES and delivery support.
Integration Is Developed Through Adapting to Context
An important feature of DSMES in the literature was how the content and delivery were adapted to local conditions and individual needs (70–74, 76–80, 83, 85, 90). In some situations, linguistic and cultural needs were taken into account to adapt DSMES to the socio-cultural backgrounds of the people with diabetes (75, 85, 88). To this end, professional interpreters or bilingual healthcare professionals adapted the content of DSMES and the information conveyed about disease conditions to the context of specific population groups. In addition, more advice on how to access medical services and community resources related to diabetes was provided to address specific needs.
Considering the values and beliefs of people with diabetes was crucial to help them understand their disease (74). Furthermore, different strategies and modes of delivery addressed the individual preferences of people with diabetes. For example, individualised follow-up was integrated with web-based DSMES because this approach was flexible and could fit the time availability of people with diabetes regardless of where they were located (87, 88). Structured DSMES was also delivered individually or in group settings (76, 80, 83, 90). In some situations, delivery was adapted to the needs of primary care by offering specialist support to improve local access to DSMES (71, 72, 89).
Altogether, adapting to context considers the values, beliefs and preferences of people with diabetes and healthcare professionals to enhance their acceptance of DSMES. Reflecting on these conditions is important for the integration of DSMES into the routine care of local health care systems.
Integration Is Mediated by the Organisation of the Care System
The literature exposed the extent to which DSMES was embedded in the broader health care system (70–73, 75, 76, 80, 87–90). The level of integration was associated with normative mechanisms, such as structured treatment plans with common protocols, shared guidelines and care pathways, and with contextual mediators that represent how DSMES was integrated into the processes and structures of routine patient care (70–73, 75–77, 80, 89, 90).
It was evident that using information technology (IT) to transfer information improved communication between healthcare professionals and people with diabetes (87, 88). Nevertheless, concern was raised about computer access and the necessary e-health literacy that could further disadvantage some people with diabetes. The literature indicated that the integration of technology-enabled tools into routine care required access to and acceptance of the technology, as well as the skills needed to use it, and the necessary precautions to protect data.
Including regular follow-up and recall systems within treatment protocols and guidelines were beneficial for the integration of DSMES into the care delivery processes (70–73, 75, 76, 80, 89, 90). However, in some situations the necessary organisational changes were not implemented, so DSMES was not integrated into routine care and therefore could not contribute their potential to improve patient outcomes even though the healthcare professionals received financial incentives for the provision of DSMES (73).
Overall, DSMES is conveyed by the care system organisation and their strategies for integrating DSMES into routine care. Structured treatment plans with defined guidelines, common protocols and care pathways govern the processes of DSMES delivery, and the necessary information transfer may be eased through the use of technology.
Interactions and Relationships Between the Components of Integration
The five components of integration were conceived as a cascade-like interaction (20), assuming a systemic non-linear interdependence (see Figure 2).

Figure 2 Theoretical model of interacting components influencing the integration of DSMES to affect person-centred care and self-management behaviour in routine care.
Interactions between the components may influence the delivery of person-centred DSMES and the uptake of self-management behaviour according to the importance and priority given to each individual component. The interpersonal relationship component expresses the interactions between the healthcare professionals and the person with diabetes during DSMES and is likely driven by the underlying positions people take in their exchanges, as evidenced by how they participate and contribute. These interactions may interrelate with the other components, for example, by influencing how opportunities for shared learning between healthcare professionals and people with diabetes are encouraged in DSMES. The shared learning component, in response, may affect the delivery and implementation of DSMES and be influenced by how the programme ethos, underpinning DSMES, supports self-management behaviour in practice. The approach in the programme ethos component, in turn, may guide and influence healthcare professionals’ positions in conducting DSMES. The adapting to context component considers the specific situations of the person with diabetes and healthcare professionals and may influence the content and delivery mode of DSMES. This contextualisation addresses the different needs and preferences of a diverse population in DSMES. The model considers the collaborative interactions that are observable in DSMES and delivered by multiple healthcare professionals. These collaborative interactions are reflected in the ways different health care services are linked to each other. The care system organisation component in the model illustrates that structures and processes, such as protocols, care pathways, guidelines and IT systems, build the context for the delivery of DSMES and its transfer into routine care. The components of integration are expressed in a systemic approach, with dynamic interactions that may extend or diminish the sense of integration experienced by both the people with diabetes and the healthcare professionals. The importance and prioritisation of individual components influence the context and thereby the conditions that enable healthcare professionals to provide person-centred care and support people with diabetes to develop their self-management behaviours.
This conceptual model of integration was presented and discussed with diabetes specialist nurses (DSNs) in a workshop at the annual conference of the Swiss Diabetes Specialist Nursing Organisation in March 2016 in Berne, Switzerland. Forty-nine DSNs participated in the workshop, which was simultaneously translated between French and German: 19 DSNs spoke French (including 2 DSNs from the Italian-speaking part of Switzerland), and 30 DSNs spoke German (including 1 DSN from the Romansch-speaking part of Switzerland). The workshop was simultaneously translated in order to capture different linguistic interpretations and to directly discuss any differences. The workshop participants agreed on the most important features of each component and identified an opportunity for improvement in the components that were currently receiving low priority in the Swiss context. The priorities given and the consensus reached for components are shown in Table 2. It was interesting to note that French-speaking DSNs focused rather on the component of interpersonal relationship while some German-speaking DSNs prioritised the component of the programme ethos underpinning DSMES and suggested arranging the other components around the ethos of DSMES. Overall, the participants agreed that the conceptualisation of the components and their content was fit for purpose and specific for DSMES (67).
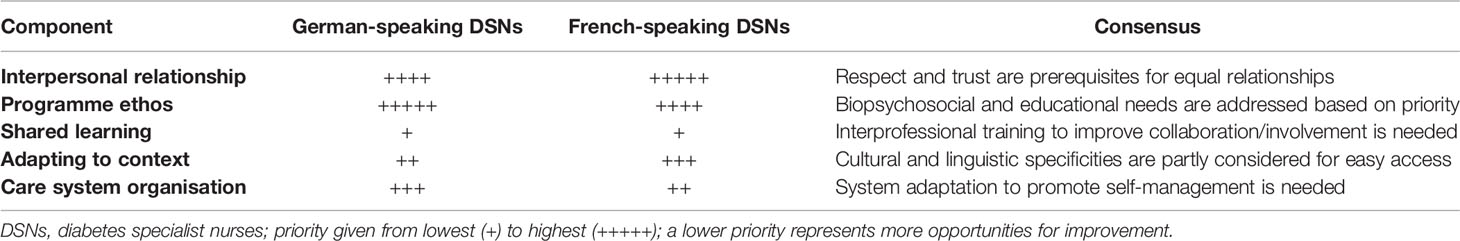
Table 2 Level of importance given by the participants to components, consensus reached between DSNs from different linguistic areas, and identified opportunities for improvement.
Discussion
A critical interpretative synthesis was conducted to conceptualise the integration of DSMES into routine care. Five interacting components of integration were identified and described. This conceptualisation contributes to the understanding of integration – which is needed because of the many different interpretations – in the context of DSMES. Prior to the conduct of this review, a definition of the meaning of “integration of DSMES” was missing in the literature. The components broadly cluster around relational, ethical, learning, contextual adapting, and systemic organisational aspects of DSMES. In addition to developing the model, several new findings emerged from the review.
Interpersonal relationships between healthcare professionals and people with diabetes are crucial for their experience of DSMES, this is already widely acknowledged (17, 21, 91–95). However, it might be that healthcare professionals are less aware of how different agendas and expectations shape their interactions with people with diabetes, and in what ways this may create discrepancies in their experiences. Specific training for healthcare professionals could help them to build relationship and provide support that will be beneficial for the person with diabetes. Although person-centred DSMES has already expanded into many care delivery settings, a more patronising approach to patient care, where healthcare professionals adopt a rather authoritarian attitude, is still present and may impede the implementation of person-centred initiatives (96, 97). Integrating the training element of person-centred care delivery for healthcare professionals into any DSMES would therefore improve the conditions for relationship-building, and thus, the participant experience in DSMES.
Structured DSMES use diverse disease models and different approaches related to psycho-educational, learning and behaviour change theories. These aspects are well known in the literature and showed better results the more frequently and intensively they were used and the more the healthcare professionals were trained in implementing DSMES (12, 18). In spite of that, it remains still unclear to what extent the healthcare professionals’ training, especially in therapeutic patient education, is effectively implemented in routine care in terms of building a person-centred relationship. Therapeutic patient education has been evolving in Europe for over 25 years, albeit in different ways, leading in some places to lasting changes in the treatment, education and support of people with diabetes as well as in the training of healthcare professionals and their perceptions of their roles (98–101). For example, in Switzerland, therapeutic patient education has developed strongly in French-speaking Switzerland around the Division of Therapeutic Education for Chronic Diseases of the Geneva University Hospitals (HUG), where specialised postgraduate training courses in therapeutic patient education have been offered to healthcare professionals from different disciplines since 1998 (102). Training healthcare professionals in therapeutic patient education has shown promising results in terms of how DSMES is implemented in clinical practice (103, 104). The helpful implementation of the underlying ethos of DSMES and the associated experiences of care also play an important role in integrating DSMES into the daily lives of people with diabetes. The extent to which self-management behaviours persist beyond one-off patient support is mediated by the interacting components, potentially triggered by mechanisms within DSMES, that enable people with diabetes to reconcile the personal goals they have developed with the demands of their daily lives and the ongoing interactions with healthcare professionals.
The vast diversity of people participating in DSMES creates its own context with specific situations during their exchanges. The features of these exchanges are shaped by the healthcare professionals with their professional experience, knowledge of the disease and priorities in the patient treatments, and by the people with diabetes with their life experience, understanding of the disease and priorities in life. Such interactions may produce disconnects and uncertainties that require negotiation to reach an agreement because they often originate in different priorities (105). Multiple healthcare professionals provide DSMES. Therefore, the context of DSMES also refers to the conditions that encourage collaborative care, promoted in multi-professional trainings of healthcare professionals, where dynamic interactions form the behaviour of a healthcare professional team (106, 107). In addition to the multi-professional training, the inclusion of the person with diabetes in the delivery of DSMES helps the healthcare professionals to better understand what it means to live with diabetes. Interactions with people with diabetes are also an important source of learning for healthcare professionals because interactions based on a narrow biomedical understanding of patient needs may lead to a transfer of knowledge that is not relevant for the person with diabetes, and thus, creating a disconnect for them (108). The conditions for DSMES integration could be further promoted through regular interprofessional training, more opportunities for shared learning also involving people with diabetes, and the provision of support for the interprofessional DSMES delivery, which are not yet sufficiently implemented in many health care services.
The extent to which DSMES adapts the content and delivery mode to the cultural, ethnic, geographic, cognitive and literacy aspects of a population is an important factor for the uptake of DSMES, which is widely acknowledged in the literature (18, 109). Tailoring to a specific population’s needs is even more important when addressing difficult-to-reach populations and those with a low level of health literacy, as they often have complex health needs and are more affected by diabetes complications; integration in such a context may imply, for example, that some people with diabetes need to learn how to navigate the health care system in order to access care (110–112). The way in which healthcare professionals deliver care may also be influenced by their values, beliefs and preferences; thus, their likelihood that they adopt the person-centred approach to DSMES and adapt their care delivery. Such contextual adaptation takes into account the specific situations and experiences of both people with diabetes and healthcare professionals in order to choose the most suitable ways to deliver DSMES. Reflecting on these conditions in the development and improvement processes of DSMES is worthwhile when considering the integration of DSMES into the routine care structures of the local health care system.
The integration of DSMES also depends on the structures and processes of the care system organisation that are available to implement DSMES. In many instances of DSMES implementation, ongoing support and quality assurance are scarce and could benefit from being embedded in structured disease management programmes. It is also important to monitor participation rates to identify groups that may be less likely to attend DSMES, so that adaptations can be made such as directing programmes towards these groups and, where appropriate, changing how they are delivered. There is an ongoing policy shift towards more person-centred DSMES, and it is expected that the strategies used will be most beneficial when integrated into the interdisciplinary structures and coordinated processes of routine care, as advocated, for example, in the chronic care model (113–115). Furthermore, integrated care systems are thought to improve patients’ experiences, their health outcomes, and the use of resources; but so far, the evidence has shown equivocal results, especially with regard to person-centred care delivery (30, 116, 117). The reasons for these inconclusive results are multifactorial and may relate to the imprecise definition of integrated care with its wide range of activities and concepts, but also to the insufficient impact of the collective activities of healthcare professionals in changing the patient health status in their context, as shown, for example, by the inconsistency in patient experiences and outcomes (30).
Integrated care is an organisational form for health care delivery and contains a set of care initiatives aimed at implementing person-centred care to help people manage their chronic conditions (118). DSMES is a care initiative whose integration into routine care is influenced by the identified interacting components and shaped by the priorities of people with diabetes, the healthcare professionals involved and the prevalent conditions within health care systems. The defined components contribute to the development of strategies to improve the patient experiences and outcomes of DSMES. Another important strategy for greater integration of DSMES into routine care is adequate reimbursement structures, especially in care systems without universal healthcare coverage (119).
An organisational context and structures that take into account the patient experiences and outcomes of DSMES also provide improvement opportunities for healthcare professionals. Such approaches enable healthcare professionals to realistically adapt to specific situations and thereby also improve their experience of DSMES. These conditions may take into account the dynamically emerging relationships between the healthcare professionals and people with diabetes during DSMES; and thus, may sustain the person-centred approach promoted by the ethos of DSMES programmes more strongly and for a longer time in routine care. It is expected that contexts, integrating these five components of DSMES into their care provision, will encourage the delivery of person-centred care and the adoption of self-management behaviour, which may lead to improved uptake and impact of DSMES.
Strengths and Limitations
Using a critical interpretive synthesis approach, we conceptualised and defined five interacting components of integration related to DSMES in routine care. This approach offered the prospect to reframe and reinterpret existing literature through the argument of integration that generated new insights. As in many interpretive syntheses, some of the articles only indirectly addressed the review questions; the synthesis extrapolated data on the integration of DSMES from those articles.
Inherent to critical interpretive syntheses, articles were included based on their conceptual quality, which means that the identified articles provided content relevant to the review questions. We searched multiple databases and used inclusive search terms. The study designs and how the studies contributed to the conceptualisation were included in the review. All articles were discussed and compared in detail in terms of their theoretical contribution to the conceptualisation. The review team supported reflexivity throughout the review process, documented the decision processes and guarded against framing the analysis according to a single perspective. Given the wide range of topics covered by this critical interpretive synthesis, we may have missed relevant studies. Because our aim was conceptual saturation, we consider this interpretive approach acceptable. Furthermore, the components and the model were discussed for their face validity during an interactive workshop at an annual professional meeting with diabetes specialist nurses familiar with DSMES. Though, for further evaluation, study designs with higher validity levels and multi-professional teams will be used. A further limitation of the study inheres to the translation processes in the workshop discussions and their interpretation for this study. While it is a strength of the study that the components and the model were discussed with diabetes specialist nurses from different linguistic and cultural backgrounds as well as from different work settings with the help of professional translators, the workshop’s findings were translated into English. And therefore, the interpretation of the components might be different in a predominantly English-speaking context. The translation processes may alter the interpretation and though not reflect the true understanding.
Conclusion
Based on this critical interpretative synthesis, the integration of DSMES into routine care is defined as five interacting components related to relational, ethical, learning, contextual adapting, and systemic organisational aspects that interact within and among themselves and manifest in non-linear interactions in the context in which they are presented. However, it remains unclear which mechanisms trigger these interactions; this is the subject of a follow-up study that will be reported elsewhere. Furthermore, more research is needed to evaluate how the professional training of healthcare professionals in person-centred therapeutic patient education affects the components of integration.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Author Contribution
CH and AF conceived the study and drafted the key areas for review. CH searched the literature; the results were discussed with CM and AF. CH led the development of the theoretical model in conjunction with CM and AF with expansion from DC. All named authors participated in the preparation of the manuscript, providing written comments on drafts and approving the final version.
Funding
This study presents independent research funded by an unconditional grant from the Nursing Science Foundation Switzerland.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors would like to thank Aline Lasserre Moutet, pedagogue, center manager, Unit of Therapeutic Patient Education (WHO collaborating center), Montserrat Castellsague, clinical diabetes nurse specialist, and Luz Perrenoud, clinical diabetes nurse specialist, Department of Endocrinology, Diabetology, Nutrition and Therapeutic Patient Education, University Hospital of Geneva, Geneva, Switzerland, for their advice in preparing and co-facilitating the interactive bilingual German-French workshop. The authors would also like to thank all the nurses for their constructive criticism during the workshop and thus for their contribution to the conceptualisation. The authors would like to acknowledge the Nursing Science Foundation Switzerland who sponsored the PhD fellowship of the first author. The manuscript presents adapted and extended content from the doctoral thesis of the first author (20).
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcdhc.2022.845547/full#supplementary-material
References
1. Chatterjee S, Khunti K, Davies MJ. Type 2 Diabetes. Lancet (2017) 389(10085):2239–51. doi: 10.1016/S0140-6736(17)30058-2
2. Fowler MJ. Microvascular and Macrovascular Complications of Diabetes. Clin Diabetes (2011) 29(3):116–22. doi: 10.2337/diaclin.29.3.116
3. Kassebaum NJ, Arora M, Barber RM, Bhutta ZA, Brown J, Carter A, et al. Global, Regional, and National Disability-Adjusted Life-Years (DALYs) for 315 Diseases and Injuries and Healthy Life Expectancy (HALE), 1990–2015: A Systematic Analysis for the Global Burden of Disease Study 2015. Lancet (2016) 388(10053):1603–58. doi: 10.1016/S0140-6736(16)31460-X
4. Beagley J, Guariguata L, Weil C, Motala AA. Global Estimates of Undiagnosed Diabetes in Adults. Diabetes Res Clin Pract (2014) 103(2):150–60. doi: 10.1016/j.diabres.2013.11.001
5. Prattichizzo F, de Candia P, De Nigris V, Nicolucci A, Ceriello A. Legacy Effect of Intensive Glucose Control on Major Adverse Cardiovascular Outcome: Systematic Review and Meta-Analyses of Trials According to Different Scenarios. Metabolism (2020) 110:154308. doi: 10.1016/j.metabol.2020.154308
6. Roussel R, Steg PG, Mohammedi K, Marre M, Potier L. Prevention of Cardiovascular Disease Through Reduction of Glycaemic Exposure in Type 2 Diabetes: A Perspective on Glucose-Lowering Interventions. Diabetes Obes Metab (2018) 20(2):238–44. doi: 10.1111/dom.13033
7. UK Prospective Diabetes Study Group. Effect of Intensive Blood-Glucose Control With Metformin on Complications in Overweight Patients With Type 2 Diabetes (UKPDS 34). UK Prospective Diabetes Study (UKPDS) Group. Lancet (1998) 352(9131):854–65.
8. Zoungas S, Arima H, Gerstein HC, Holman RR, Woodward M, Reaven P, et al. Effects of Intensive Glucose Control on Microvascular Outcomes in Patients With Type 2 Diabetes: A Meta-Analysis of Individual Participant Data From Randomised Controlled Trials. Lancet Diabetes Endocrinol (2017) 5(6):431–7. doi: 10.1016/S2213-8587(17)30104-3
9. An J, Nichols GA, Qian L, Munis MA, Harrison TN, Li Z, et al. Prevalence and Incidence of Microvascular and Macrovascular Complications Over 15 Years Among Patients With Incident Type 2 Diabetes. BMJ Open Diabetes Res Care (2021) 9(1):e001847. doi: 10.1136/bmjdrc-2020-001847
10. Gillett M, Dallosso HM, Dixon S, Brennan A, Carey ME, Campbell MJ, et al. Delivering the Diabetes Education and Self Management for Ongoing and Newly Diagnosed (DESMOND) Programme for People With Newly Diagnosed Type 2 Diabetes: Cost Effectiveness Analysis. BMJ (2010) 341:c4093. doi: 10.1136/bmj.c4093
11. Lorig K, Ritter PL, Turner RM, English K, Laurent DD, Greenberg J. A Diabetes Self-Management Program: 12-Month Outcome Sustainability From a Nonreinforced Pragmatic Trial. J Med Internet Res (2016) 18(12):e322. doi: 10.2196/jmir.6484
12. Pillay J, Armstrong MJ, Butalia S, Donovan LE, Sigal RJ, Vandermeer B, et al. Behavioral Programs for Type 2 Diabetes Mellitus: A Systematic Review and Network Meta-Analysis. Ann Intern Med (2015) 163(11):848–60. doi: 10.7326/M15-1400
13. Upsher R, Onabajo D, Stahl D, Ismail K, Winkley K. The Effectiveness of Behavior Change Techniques Underpinning Psychological Interventions to Improve Glycemic Levels for Adults With Type 2 Diabetes: A Meta-Analysis. Front Clin Diabetes Healthcare (2021) 2(5). doi: 10.3389/fcdhc.2021.699038
14. Holt RI, Nicolucci A, Kovacs Burns K, Escalante M, Forbes A, Hermanns N, et al. Diabetes Attitudes, Wishes and Needs Second Study (DAWN2): Cross-National Comparisons on Barriers and Resources for Optimal Care - Healthcare Professional Perspective. Diabetes Med (2013) 30(7):789–98. doi: 10.1111/dme.12242
15. Winkley K, Stahl D, Chamley M, Stopford R, Boughdady M, Thomas S, et al. Low Attendance at Structured Education for People With Newly Diagnosed Type 2 Diabetes: General Practice Characteristics and Individual Patient Factors Predict Uptake. Patient Educ Couns (2016) 99(1):101–7. doi: 10.1016/j.pec.2015.08.015
16. Zuercher E, Casillas A, Hagon-Traub I, Bordet J, Burnand B, Peytremann-Bridevaux I. Baseline Data of a Population-Based Cohort of Patients With Diabetes in Switzerland (CoDiab-Vd). Swiss Med Wkly (2014) 144:w13951. doi: 10.4414/smw.2014.13951
17. Davies MJ, D’Alessio DA, Fradkin J, Kernan WN, Mathieu C, Mingrone G, et al. Management of Hyperglycaemia in Type 2 diabetes, 2018. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia (2018) 61(12):2461–98. doi: 10.1007/s00125-018-4729-5
18. Chatterjee S, Davies MJ, Heller S, Speight J, Snoek FJ, Khunti K. Diabetes Structured Self-Management Education Programmes: A Narrative Review and Current Innovations. Lancet Diabetes Endocrinol (2018) 6(2):130–42. doi: 10.1016/S2213-8587(17)30239-5
19. Huppmann M, Leinert J, Reiche R, Südhof S. Bericht der Strukturierten Behandlungsprogramme der Gesetzlichen Krankenkassen – Indikation Diabetes Mellitus Typ 2. Bonn: Infas Institut Fuer Angewandte Sozialwissenschaft GmbH (2020) Available from: https://www.g-693ba.de/downloads/17-98-5072/2019-12-31_DMP-Evaluationsbericht_DM2.pdf
20. Huber C. Exploring the Integration of Self-Management Education in Routine Care of People With Type 2 Diabetes Mellitus: A Qualitative Study. London: King’s College London (2019).
21. Powers MA, Bardsley J, Cypress M, Duker P, Funnell MM, Fischl AH, et al. Diabetes Self-Management Education and Support in Type 2 Diabetes: A Joint Position Statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. Diabetes Educator (2017) 43(1):40–53. doi: 10.1177/0145721716689694
22. Greenfield G. GPs Should be Rewarded for Patient Experience to Encourage a Person Centred NHS. BMJ (2014) 349:g6422. doi: 10.1136/bmj.g6422
23. Ignatowicz A, Greenfield G, Pappas Y, Car J, Majeed A, Harris M. Achieving Provider Engagement: Providers' Perceptions of Implementing and Delivering Integrated Care. Qual Health Res (2014) 24(12):1711–20. doi: 10.1177/1049732314549024
24. Cloninger CR, Salvador-Carulla L, Kirmayer LJ, Schwartz MA, Appleyard J, Goodwin N, et al. A Time for Action on Health Inequities: Foundations of the 2014 Geneva Declaration on Person- and People-Centered Integrated Healthcare for All. Int J Pers Cent Med (2014) 4(2):69–89.
25. Ham C, Walsh N. Making Integrated Care Happen at Scale and Pace. London: The King's Fund (2013).
26. WHO. Everybody's Business: Strengthening Health Systems to Improve Health Outcomes: WHO's Framework for Action. Geneva: World Health Organisation (2007).
27. Cash-Gibson L, Rosenmoller M. Project INTEGRATE: A Common Methodological Approach to Understand Integrated Health Care in Europe. Int J Integr Care (2014) 14(4):e035. doi: 10.5334/ijic.1980
28. Singer SJ, Burgers J, Friedberg M, Rosenthal MB, Leape L, Schneider E. Defining and Measuring Integrated Patient Care: Promoting the Next Frontier in Health Care Delivery. Med Care Res Rev (2011) 68(1):112–27. doi: 10.1177/1077558710371485
29. Armitage GD, Suter E, Oelke ND, Adair CE. Health Systems Integration: State of the Evidence. Int J Integr Care (2009) 9(2). doi: 10.5334/ijic.316
30. Hughes G, Shaw SE, Greenhalgh T. Why Doesn't Integrated Care Work? Using Strong Structuration Theory to Explain the Limitations of an English Case. Sociol Health Illn (2022) 44:113–29. doi: 10.1111/1467-9566.13398
31. Goodwin N. Thinking Differently About Integration: People-Centred Care and the Role of Local Communities. Int J Integr Care (2014) 14:e026. doi: 10.5334/ijic.1736
32. Kodner DL, Spreeuwenberg C. Integrated Care: Meaning, Logic, Applications, and Implications – A Discussion Paper. Int J Integrated Care (2002) 2(4):1–6. doi: 10.5334/ijic.67
33. Kodner DL. All Together Now: A Conceptual Exploration of Integrated Care. Healthc Q (2009) 13(Spec No):6–15. doi: 10.12927/hcq.2009.21091
34. Braithwaite J, Churruca K, Long JC, Ellis LA, Herkes J. When Complexity Science Meets Implementation Science: A Theoretical and Empirical Analysis of Systems Change. BMC Med (2018) 16(1):63–77. doi: 10.1186/s12916-018-1057-z
35. Curry N, Ham C. Clinical and Service Integration: The Route to Improve Outcomes. London: The Kings Fund (2010).
36. Shaw S, Rosen R, Rumbold B. What is Integrated Care? An Overview of Integrated Care in the NHS. London: Nuffield Trust (2011).
37. Sturmberg JP, Martin CM, Katerndahl DA. Systems and Complexity Thinking in the General Practice Literature: An Integrative, Historical Narrative Review. Ann Fam Med (2014) 12(1):66–74. doi: 10.1370/afm.1593
38. Benham-Hutchins M, Clancy TR. Social Networks as Embedded Complex Adaptive Systems. JONA (2010) 40(9):352–6. doi: 10.1097/NNA.0b013e3181ee42bc
39. Ellis B, Herbert SI. Complex Adaptive Systems (CAS): An Overview of Key Elements, Characteristics and Application to Management Theory. Inform Prim Care (2011) 19(1):33–7. doi: 10.14236/jhi.v19i1.791
40. Tsasis P, Evans JM, Owen S. Reframing the Challenges to Integrated Care: A Complex-Adaptive Systems Perspective. Int J Integr Care (2012) 12:e190. doi: 10.5334/ijic.843
41. Begun JW, Kaissi AA. Uncertainty in Health Care Environments: Myth or Reality? Health Care Management Rev (2004) 29(1):31–9. doi: 10.1097/00004010-200401000-00005.
43. Fraser SW, Greenhalgh T. Coping With Complexity: Educating for Capability. BMJ (2001) 323(7316):799–803. doi: 10.1136/bmj.323.7316.799
44. Lansing JS. Studying Complex Adaptive Systems. J Syst Sci Complex (2003) 32(1):183–204. doi: 10.1146/annurev.anthro.32.061002.093440
45. Kannampallil TG, Schauer GF, Cohen T, Patel VL. Considering Complexity in Healthcare Systems. J BioMed Inform (2011) 44(6):943–7. doi: 10.1016/j.jbi.2011.06.006
46. Khan S, Vandermorris A, Shepherd J, Begun JW, Lanham HJ, Uhl-Bien M, et al. Embracing Uncertainty, Managing Complexity: Applying Complexity Thinking Principles to Transformation Efforts in Healthcare Systems. BMC Health Serv Res (2018) 18(1):192. doi: 10.1186/s12913-018-2994-0
47. Paina L, Peters DH. Understanding Pathways for Scaling Up Health Services Through the Lens of Complex Adaptive Systems. Health Policy Plan (2012) 27(5):365–73. doi: 10.1093/heapol/czr054
48. Plsek PE, Greenhalgh T. Complexity Science: The Challenge of Complexity in Health Care. BMJ (2001) 323(7313):625–8. doi: 10.1136/bmj.323.7313.625
49. Plsek PE, Wilson T. Complexity Science: Complexity, Leadership, and Management in Healthcare Organisations. BMJ (2001) 323(7315):746–9. doi: 10.1136/bmj.323.7315.746
50. Cooper HC, Geyer R. Riding the Diabetes Rollercoaster: A New Approach for Health Professionals, Patients and Carers. Oxford: Radcliffe Publishing (2007).
51. Cooper HC, Geyer R. What can Complexity do for Diabetes Management? Linking Theory to Practice. J Eval Clin Pract (2009) 15(4):761–5. doi: 10.1111/j.1365-2753.2009.01229.x
52. Griffiths F, Borkan J, Byrne D, Crabtree BF, Dowrick C, Gunn J, et al. Developing Evidence for How to Tailor Medical Interventions for the Individual Patient. Qual Health Res (2010) 20(12):1629–41. doi: 10.1177/1049732310377453
53. Lacroix A, Assal JP. L'éducation Thérapeutique Des Patients - Accompagner Les Patients Avec Une Maladie Chronique: Nouvelle Approaches. 3rd ed. Maloine, editor. Paris: Maloine (2013).
54. Innes AD, Campion PD, Griffiths FE. Complex Consultations and the "Edge of Chaos". Br J Gen Pract (2005) 55(510):47–52.
55. Innes JE, Booher DE. Consensus Building and Complex Adaptive Systems. J Am Plann Assoc (1999) 65(4):412–23. doi: 10.1080/01944369908976071
56. Wagner EH. Chronic Disease Management: What Will It Take to Improve Care for Chronic Illness? Effective Clinical Practice (1998) 1(1):2–4.
57. Centre for Reviews and Dissemination’s Guidance for Undertaking Reviews in Health Care. University of York (2009). 1900640473. https://www.york.ac.uk/crd/SysRev/!SSL!/WebHelp/SysRev3.htm
58. Dixon-Woods M, Cavers D, Agarwal S, Annandale E, Arthur A, Harvey J, et al. Conducting a Critical Interpretive Synthesis of the Literature on Access to Healthcare by Vulnerable Groups. BMC Med Res Methodol (2006) 6:35. doi: 10.1186/1471-2288-6-35
59. Sinnott C, Georgiadis A, Park J, Dixon-Woods M. Impacts of Operational Failures on Primary Care Physicians' Work: A Critical Interpretive Synthesis of the Literature. Ann Fam Med (2020) 18(2):159–68. doi: 10.1370/afm.2485
60. Pluye P, Hong QN. Combining the Power of Stories and the Power of Numbers: Mixed Methods Research and Mixed Studies Reviews. Annu Rev Public Health (2014) 35(1):29–45. doi: 10.1146/annurev-publhealth-032013-182440
61. Greenhalgh T, Peacock R. Effectiveness and Efficiency of Search Methods in Systematic Reviews of Complex Evidence: Audit of Primary Sources. BMJ (2005) 331(7524):1064–5. doi: 10.1136/bmj.38636.593461.68
62. Flemming K, Briggs M. Electronic Searching to Locate Qualitative Research: Evaluation of Three Strategies. J Adv Nurs (2007) 57(1):95–100. doi: 10.1111/j.1365-2648.2006.04083.x
63. McKibbon KA, Wilczynski NL, Haynes RB, Hedges T. Retrieving Randomized Controlled Trials From Medline: A Comparison of 38 Published Search Filters. Health Info Libr J (2009) 26(3):187–202. doi: 10.1111/j.1471-1842.2008.00827.x
64. Annandale E, Harvey J, Cavers D, Dixon-Woods M. Gender and Access to Healthcare in the UK: A Critical Interpretive Synthesis of the Literature. Evidence Policy: A J Res Debate Pract (2007) 3(4):463–86. doi: 10.1332/174426407782516538
65. Boyko JA, Lavis JN, Abelson J, Dobbins M, Carter N. Deliberative Dialogues as a Mechanism for Knowledge Translation and Exchange in Health Systems Decision-Making. Soc Sci Med (2012) 75(11):1938–45. doi: 10.1016/j.socscimed.2012.06.016
66. Finlay L. “Outing” the Researcher: The Provenance, Process, and Practice of Reflexivity. Qual Health Res (2002) 12(4):531–45. doi: 10.1177/104973202129120052
67. Belone L, Lucero JE, Duran B, Tafoya G, Baker EA, Chan D, et al. Community-Based Participatory Research Conceptual Model: Community Partner Consultation and Face Validity. Qual Health Res (2016) 26(1):117–35. doi: 10.1177/1049732314557084
68. Trochim WM, McLinden D. Introduction to a Special Issue on Concept Mapping. Eval Program Planning (2017) 60:166–75. doi: 10.1016/j.evalprogplan.2016.10.006
69. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Ann Intern Med (2009) 151(4):264–9. doi: 10.7326/0003-4819-151-4-200908180-00135
70. Hepworth J, Askew D, Jackson C, Russell A. "Working With the Team": An Exploratory Study of Improved Type 2 Diabetes Management in a New Model of Integrated Primary/Secondary Care. Aust J Prim Health (2013) 19(3):207–12. doi: 10.1071/PY12087
71. Russell AW, Baxter KA, Askew DA, Tsai J, Ware RS, Jackson CL. Model of Care for the Management of Complex Type 2 Diabetes Managed in the Community by Primary Care Physicians With Specialist Support: An Open Controlled Trial. Diabetes Med (2013) 30(9):1112–21. doi: 10.1111/dme.12251
72. Goderis G, Borgermans L, Grol R, Van Den Broeke C, Boland B, Verbeke G, et al. Start Improving the Quality of Care for People With Type 2 Diabetes Through a General Practice Support Program: A Cluster Randomized Trial. Diabetes Res Clin Pract (2010) 88(1):56–64. doi: 10.1016/j.diabres.2009.12.012
73. Goderis G, Borgermans L, Mathieu C, Van Den Broeke C, Hannes K, Heyrman J, et al. Barriers and Facilitators to Evidence Based Care of Type 2 Diabetes Patients: Experiences of General Practitioners Participating to a Quality Improvement Program. Implement Sci (2009) 4:41. doi: 10.1186/1748-5908-4-41
74. Balcou-Debussche M, Debussche X. Hospitalization for Type 2 Diabetes: The Effects of the Suspension of Reality on Patients' Subsequent Management of Their Condition. Qual Health Res (2009) 19(8):1100–15. doi: 10.1177/1049732309341642
75. Debussche X, Rollot O, Le Pommelet C, Fianu A, Le Moullec N, Regnier C, et al. Quarterly Individual Outpatients Lifestyle Counseling After Initial Inpatients Education on Type 2 Diabetes: The REDIA Prev-2 Randomized Controlled Trial in Reunion Island. Diabetes Metab (2012) 38(1):46–53. doi: 10.1016/j.diabet.2011.07.002
76. Trento M, Gamba S, Gentile L, Grassi G, Miselli V, Morone G, et al. Rethink Organization to Improve Education and Outcomes (ROMEO): A Multicenter Randomized Trial of Lifestyle Intervention by Group Care to Manage Type 2 Diabetes. Diabetes Care (2010) 33(4):745–7. doi: 10.2337/dc09-2024
77. du Pon E, van Dooren A, Kleefstra N, van Dulmen S. Effects of a Proactive Interdisciplinary Self-Management Program on Patient Self-Efficacy and Participation During Practice Nurse Consultations: A Randomized Controlled Trial in Type 2 Diabetes. J Clin Med Res (2020) 12(2):79–89. doi: 10.14740/jocmr3965
78. Rygg LO, Rise MB, Gronning K, Steinsbekk A. Efficacy of Ongoing Group Based Diabetes Self-Management Education for Patients With Type 2 Diabetes Mellitus. A Randomised Controlled Trial. Patient Educ Couns (2012) 86(1):98–105. doi: 10.1016/j.pec.2011.04.008
79. Rygg LO, Rise MB, Lomundal B, Solberg HS, Steinsbekk A. Reasons for Participation in Group-Based Type 2 Diabetes Self-Management Education. A Qualitative Study. Scand J Public Health (2010) 38(8):788–93. doi: 10.1177/1403494810382475
80. Ko SH, Song KH, Kim SR, Lee JM, Kim JS, Shin JH, et al. Long-Term Effects of a Structured Intensive Diabetes Education Programme (SIDEP) in Patients With Type 2 Diabetes Mellitus: A 4-Year Follow-Up Study. Diabetes Med (2007) 24(1):55–62. doi: 10.1111/j.1464-5491.2007.02013.x
81. Adolfsson ET, Starrin B, Smide B, Wikblad K. Type 2 Diabetic Patients' Experiences of Two Different Educational Approaches: A Qualitative Study. Int J Nurs Stud (2008) 45(7):986–94. doi: 10.1016/j.ijnurstu.2007.07.007
82. Adolfsson ET, Walker-Engstrom ML, Smide B, Wikblad K. Patient Education in Type 2 Diabetes: A Randomized Controlled 1-Year Follow-Up Study. Diabetes Res Clin Pract (2007) 76(3):341–50. doi: 10.1016/j.diabres.2006.09.018
83. Sarkadi A, Rosenqvist U. Experience-Based Group Education in Type 2 Diabetes: A Randomised Controlled Trial. Patient Educ Couns (2004) 53(3):291–8. doi: 10.1016/j.pec.2003.10.009
84. Carey ME, Mandalia PK, Daly H, Gray LJ, Hale R, Martin Stacey L, et al. Increasing Capacity to Deliver Diabetes Self-Management Education: Results of the DESMOND Lay Educator non-Randomized Controlled Equivalence Trial. Diabetes Med (2014) 31(11):1431–8. doi: 10.1111/dme.12483
85. Deakin TA, Cade JE, Williams R, Greenwood DC. Structured Patient Education: The Diabetes X-PERT Programme Makes a Difference. Diabetes Med (2006) 23(9):944–54. doi: 10.1111/j.1464-5491.2006.01906.x
86. Mandalia PK, Stone MA, Davies MJ, Khunti K, Carey ME. Diabetes Self-Management Education: Acceptability of Using Trained Lay Educators. Postgrad Med J (2014) 90(1069):638–42. doi: 10.1136/postgradmedj-2014-132865
87. Glasgow RE, Kurz D, Dickman JM, Osuna D, Strycker L, King DK. Linking Internet-Based Diabetes Self-Management to Primary Care: Lessons Learned and Implications for Research Translation and Practice Implementation. Transl Behav Med (2012) 2(3):313–21. doi: 10.1007/s13142-012-0109-8
88. Glasgow RE, Kurz D, King D, Dickman JM, Faber AJ, Halterman E, et al. Twelve-Month Outcomes of an Internet-Based Diabetes Self-Management Support Program. Patient Educ Couns (2012) 87(1):81–92. doi: 10.1016/j.pec.2011.07.024
89. Katon WJ, Lin EH, Von Korff M, Ciechanowski P, Ludman EJ, Young B, et al. Collaborative Care for Patients With Depression and Chronic Illnesses. N Engl J Med (2010) 363(27):2611–20. doi: 10.1056/NEJMoa1003955
90. Piatt GA, Orchard TJ, Emerson S, Simmons D, Songer TJ, Brooks MM, et al. Translating the Chronic Care Model Into the Community: Results From a Randomized Controlled Trial of a Multifaceted Diabetes Care Intervention. Diabetes Care (2006) 29(4):811–7. doi: 10.2337/diacare.29.04.06.dc05-1785
91. Beach MC, Inui T. Relationship-Centered Care Research Network. Relationship-Centered Care. A Constructive Reframing. J Gen Intern Med (2006) 21(1):3–8. doi: 10.1111/j.1525-1497.2006.00302.x.
92. Entwistle VA, Watt IS. Treating Patients as Persons: A Capabilities Approach to Support Delivery of Person-Centered Care. AJOB (2013) 13(8):29–39. doi: 10.1080/15265161.2013.802060
93. McCormack B, Karlsson B, Dewing J, Lerdal A. Exploring Person-Centredness: A Qualitative Meta-Synthesis of Four Studies. Scand J Caring Sci (2010) 24(3):620–34. doi: 10.1111/j.1471-6712.2010.00814.x
94. Rodriguez-Gutierrez R, Gionfriddo MR, Ospina NS, Maraka S, Tamhane S, Montori VM, et al. Shared Decision Making in Endocrinology: Present and Future Directions. Lancet Diabetes Endocrinol (2016) 4(8):706–16. doi: 10.1016/S2213-8587(15)00468-4
95. Snoek FJ. Self Management Education and Good Professional Consultation Skills for Patients With Diabetes. BMJ (2012) 344:e2673. doi: 10.1136/bmj.e2673
96. Fix GM, VanDeusen Lukas C, Bolton RE, Hill JN, Mueller N, LaVela SL, et al. Patient-Centred Care is a Way of Doing Things: How Healthcare Employees Conceptualise Patient-Centred Care. Health Expect (2018) 21(1):300–7. doi: 10.1111/hex.12615
97. Snow R, Humphrey C, Sandall J. What Happens When Patients Know More Than Their Doctors? Experiences of Health Interactions After Diabetes Patient Education: A Qualitative Patient-Led Study. BMJ Open (2013) 3(11):e003583. doi: 10.1136/bmjopen-2013-003583
98. Assal JP. Revisiting the Approach to Treatment of Long-Term Illness: From the Acute to the Chronic State. A Need for Educational and Managerial Skills for Long-Term Follow-Up. Patient Educ. Couns (1999) 37(2):99–111. doi: 10.1016/S0738-3991(98)00109-8
99. Assal JP, Jacquemet S, Morel Y. The Added Value of Therapy in Diabetes: The Education of Patients for Self-Management of Their Disease. Metabolism (1997) 46(12 Suppl 1):61–4. doi: 10.1016/S0026-0495(97)90320-6
100. Deccache A, Aujoulat I. A European Perspective: Common Developments, Differences and Challenges in Patient Education. Patient Educ Counseling (2001) 44(1):7–14. doi: 10.1016/S0738-3991(01)00096-9
101. Visser A, Deccache A, Bensing J. Patient Education in Europe: United Differences. Patient Educ Counseling (2001) 44(1):1–5. doi: 10.1016/S0738-3991(01)00111-2
102. Assal JP, Golay A. Patient Education in Switzerland: From Diabetes to Chronic Diseases. Patient Educ Couns (2001) 44(1):65–9. doi: 10.1016/S0738-3991(01)00105-7
103. Golay A, Lagger G, Chambouleyron M, Carrard I, Lasserre-Moutet A. Therapeutic Education of Diabetic Patients. Diabetes Metab Res Rev (2008) 24(3):192–6. doi: 10.1002/dmrr.798
104. Sofra D, Delgado H, Masmont-Berwart S, Ruiz J. The Therapeutic Education: An Awareness Program for Health Professionals. Rev Med Suisse (2014) 10(433):1249–50, 52-3.
105. Loskutova NY, Tsai AG, Callen E, Ajayi K, Carroll JK, Harrington M, et al. Differences in Perspectives Regarding Diabetes Management Between Health Care Providers and Patients. Transl Behav Med (2018) 8(3):328–40. doi: 10.1093/tbm/iby024
106. MacInnes J, Williams L. A Review of Integrated Heart Failure Care. Prim Health Care Res Dev (2018) 20:e57. doi: 10.1017/S1463423618000312
107. Pype P, Mertens F, Helewaut F, Krystallidou D. Healthcare Teams as Complex Adaptive Systems: Understanding Team Behaviour Through Team Members' Perception of Interpersonal Interaction. BMC Health Serv Res (2018) 18(1):570. doi: 10.1186/s12913-018-3392-3
108. de Camargo Catapan S, Nair U, Gray L, Cristina Marino Calvo M, Bird D, Janda M, et al. Same Goals, Different Challenges: A Systematic Review of Perspectives of People With Diabetes and Healthcare Professionals on Type 2 Diabetes Care. Diabetes Med (2021) 38(9):e14625. doi: 10.1111/dme.14625
109. Caballero AE. The "A to Z" of Managing Type 2 Diabetes in Culturally Diverse Populations. Front Endocrinol (Lausanne) (2018) 9479. doi: 10.3389/fendo.2018.00479
110. Franzen J, Mantwill S, Rapold R, Schulz PJ. The Relationship Between Functional Health Literacy and the Use of the Health System by Diabetics in Switzerland. Eur J Public Health (2013) 24(6):997–1003. doi: 10.1093/eurpub/ckt202
111. Loignon C, Dupere S, Fortin M, Ramsden VR, Truchon K. Health Literacy - Engaging the Community in the Co-Creation of Meaningful Health Navigation Services: A Study Protocol. BMC Health Serv Res (2018) 18(1):505. doi: 10.1186/s12913-018-3315-3
112. Young CF, Yun K, Kang E, Shubrook JH, Dugan JA. Correlations Between A1C and Diabetes Knowledge, Diabetes Numeracy, and Food Security in a Vulnerable Type 2 Diabetes Population. Diabetes Spectr (2018) 31(2):177–83. doi: 10.2337/ds17-0036
113. Kousoulis AA, Patelarou E, Shea S, Foss C, Ruud Knutsen IA, Todorova E, et al. Diabetes Self-Management Arrangements in Europe: A Realist Review to Facilitate a Project Implemented in Six Countries. BMC Health Serv Res (2014) 14:453. doi: 10.1186/1472-6963-14-453
114. Lim LL, Lau ESH, Kong APS, Davies MJ, Levitt NS, Eliasson B, et al. Aspects of Multicomponent Integrated Care Promote Sustained Improvement in Surrogate Clinical Outcomes: A Systematic Review and Meta-Analysis. Diabetes Care (2018) 41(6):1312–20. doi: 10.2337/dc17-2010
115. Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving Chronic Illness Care: Translating Evidence Into Action. Health Affairs (Millwood) (2001) 20(6):64–78. doi: 10.1377/hlthaff.20.6.64
116. Busetto L, Luijkx K, Huizing A, Vrijhoef B. Implementation of Integrated Care for Diabetes Mellitus Type 2 by Two Dutch Care Groups: A Case Study. BMC Fam Pract (2015) 16:105. doi: 10.1186/s12875-015-0320-z
117. Schusselé Filliettaz S, Berchtold P, Kohler D, Peytremann-Bridevaux I. Integrated Care in Switzerland: Results From the First Nationwide Survey. Health Policy (2018) 122(6):568–76. doi: 10.1016/j.healthpol.2018.03.006
118. Damarell RA, Lewis S, Trenerry C, Tieman JJ. Integrated Care Search: Development and Validation of a PubMed Search Filter for Retrieving the Integrated Care Research Evidence. BMC Med Res Methodol (2020) 20(1):12. doi: 10.1186/s12874-020-0901-y
Keywords: integration, self-management education and support, critical interpretive synthesis, theory development, complex adaptive systems, type 2 diabetes
Citation: Huber C, Montreuil C, Christie D and Forbes A (2022) Integrating Self-Management Education and Support in Routine Care of People With Type 2 Diabetes Mellitus: A Conceptional Model Based on Critical Interpretive Synthesis and A Consensus-Building Participatory Consultation. Front. Clin. Diabetes Healthc. 3:845547. doi: 10.3389/fcdhc.2022.845547
Received: 29 December 2021; Accepted: 23 March 2022;
Published: 03 June 2022.
Edited by:
Frank Jan Snoek, Academic Medical Center, NetherlandsReviewed by:
Dominic Ehrmann, Research Institute of the Diabetes Academy Mergentheim (FIDAM), GermanyNebojsa Lalic, University of Belgrade, Serbia
Copyright © 2022 Huber, Montreuil, Christie and Forbes. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Claudia Huber, Y2xhdWRpYS5odWJlckBoZWZyLmNo
†These authors share last authorship
 Claudia Huber
Claudia Huber Chantal Montreuil
Chantal Montreuil Derek Christie1†
Derek Christie1† Angus Forbes
Angus Forbes