- 1School of Medicine, University of Alabama at Birmingham (UAB), Birmingham, AL, United States
- 2Division of Preventive Medicine, University of Alabama at Birmingham (UAB), Birmingham, AL, United States
- 3Department of Epidemiology, School of Public Health, University of Alabama at Birmingham (UAB), Birmingham, AL, United States
- 4Department of Nutrition Sciences, University of Alabama at Birmingham (UAB) Diabetes Research Center, Birmingham, AL, United States
Temporary closures of outpatient health facilities and transitions to virtual care during the COVID-19 pandemic interrupted the care of millions of patients with diabetes contributing to worsening psychosocial factors and enhanced difficulty in managing type 2 diabetes mellitus. We explored associations between COVID time period and self-reported diabetes distress on self-reported health among a sample of Alabama Medicaid-covered adults with diabetes pre-COVID (2017-2019) and during-COVID (2020-2021).
Method: In this cross-sectional study, we surveyed a population-based sample of adults with type 2 diabetes covered by the Alabama Medicaid Agency. Participants were dichotomized into pre-COVID (March 2017 to October 2019) vs during-COVID (October 2020 to May 2021) groups. Participants with missing data were removed from analyses. We assessed diabetes related stress by the Diabetes Distress Scale. We measured self-reported health using a single item with a 5-point Likert scale. We ran logistic regressions modeling COVID time period on self-reported poor health controlling for demographics, severity of diabetes, and diabetes distress.
Results: In this sample of 1822 individuals, median age was 54, 74.5% were female and 59.4% were Black. Compared to pre-COVID participants, participants surveyed during COVID were younger, more likely to be Black (64.1% VS 58.2%, p=0.01) and female (81.8% VS 72.5%, p<0.001). This group also had fewer individuals from rural areas (29.2% VS 38.4%, p<0.001), and shorter diabetes duration (7 years VS 9 years, p<0.001). During COVID individuals reported modestly lower levels of diabetes distress (1.2 VS 1.4, p<0.001) when compared to the pre-COVID group. After adjusting for demographic differences, diabetes severity, and diabetes distress, participants responding during COVID had increased odds of reporting poor health (Odds ratio [OR] 1.41, 95% Confidence Interval [CI] 1.11-1.80).
Discussion: We found respondents were more likely to report poorer health during COVID compared to pre-COVID. These results suggest that increased outreach may be needed to address diabetes management for vulnerable groups, many of whom were already at high risk for poor outcomes prior to the pandemic.
Introduction
The coronavirus disease of 2019 (COVID-19) pandemic had extensive impact in the United States causing over 700,000 deaths and sparked new fears of economic turmoil and social isolation (1). The US underwent several protective measures including temporary closure of public facilities, suspending external travel, and nightly curfews to prevent the spread of coronavirus (2).
These changes posed new barriers to care for patients with chronic disease including closing of outpatient clinics, decreased inpatient capacity, staff shortage, and medicine shortage. During COVID, many patients were unable to afford medicines or access transportation resulting in delay in seeking care (3, 4), For patients with Diabetes Mellitus (DM), these experiences could contribute to worse disease management and elevated diabetes distress, defined as an emotional state where people experience feelings such as stress, guilt, or denial that arise from living with diabetes and the burden of self-management (5, 6). Increased diabetes distress is closely linked to poor glycemic control in adults with DM (7).
The “Diabetes Belt,” a term coined by the Centers for Disease Control (CDC), refers to the southeastern region of the United States where prevalence of DM is disproportionately high (> 11%) as are rates of diabetes-related complications and mortality (8). Notably, this region has a greater percentage of African Americans (23.8% compared to 8.6%) and higher rates of poverty compared to the rest of the country (9). Centrally located within the Diabetes Belt, Alabama is the 6th poorest state in the US with over 37% of the population living at or below 200% federal poverty level (7). Limited studies have reviewed the effects of the COVID pandemic on this population. The compounding high burden of disease with limited financial resources may further complicate diabetes management and may worsen diabetes distress.
Evidence also suggests that COVID protective measures may have had significant impact on individuals physical and mental health, with some populations experiencing higher rates of anxiety, depression, and perceived stress during the pandemic (10). Moreover, individuals who were directly impacted by COVID reported declines in self-rated health (11). Lower self-rated health and higher levels of mental distress are associated with poor health management, increased hospitalizations, and increased mortality in patients managing chronic disease (12).
In this study, we examined the relationship between diabetes distress, depressive symptoms, diabetes management self-efficacy, and perceived stress with self-reported health in Alabama Medicaid-covered adults with diabetes between COVID time periods (prior to vs during).
Methods
Study Design and Population
We conducted a cross-sectional survey within the Alabama Care Plan study. Briefly, the Alabama Care Plan (ACP) was an observational study of the quality of care of adults with diabetes covered by Alabama Medicaid. The Alabama Care Plan study enrolled a population-based sample of adults with type 1 or 2 diabetes who were covered by Alabama Medicaid between March 2017 and May 2021. Medicaid eligibility for adults in Alabama includes parents of minor children with incomes at or below 18% of Federal Poverty Level (FPL) and adults with disability eligible for the Supplemental Security Income (SSI) program (13). As part of the ACP study, a survey was conducted among a sample of Medicaid-covered adults with diabetes to assess patient-reported outcomes and satisfaction with care.
The current study examines survey responses before and during the COVID pandemic. Adults were eligible if they met the following criteria: age 19 to 64 years old, covered by Medicaid for the prior 12 months, and were diagnosed with diabetes, defined by the presence of at least one inpatient or two outpatient International Classification of Diseases (ICD-9 or ICD-10) diagnosis codes used by the CMS Chronic Conditions Warehouse project (14), in the preceding two years (15). Potential participants were excluded if they were non-English speaking, were mentally or physically incapable of completing the survey per caregiver report. All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Review Board and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. All study data were HIPAA-compliant and secured with additional password protection.
Data Collection
Survey methods have been described previously (7). Briefly, using Alabama Medicaid enrollment and claims data files, the survey unit generated a list of potential participants who met the age, Medicaid enrollment and diabetes diagnosis inclusion criteria. We contacted potential participants by letter, which provided information about the study and an option to decline participation by contacting a toll-free number or by mail. Subsequently, study interviewers contacted potential participants who did not decline by phone to invite them to participate and schedule a time to complete the survey. Study interviewers called participants multiple times at different times and days, including evenings and weekends, with a maximum of 15 call attempts. For eligible participants who agreed to participate, informed consent was obtained by phone. Study interviewers used a computer-assisted telephone interview system to complete a 125-item survey which included measures detailed below. The study was reviewed and approved by the UAB Institutional Review Board.
Measures
Measures (described below) included those that assessed self-reported health, depressive symptoms, perceived stress, diabetes management, and stress relating to diabetes with additional questions on socio-demographics. Participants during COVID completed additional questions relating to COVID experiences and access to care.
Self-Reported Health Survey
The self-reported health survey is a single-item ordinal measure with 5 levels varying from excellent, very good, good, fair, or poor. This survey is a widely used indicator of general health status in epidemiologic and population health research and is often categorized into excellent, very good, or good versus fair or poor (16).
Patient Health Questionnaire-8 (PHQ-8)
The PHQ-8 is an 8-item survey used for assessing depression that incorporates DSM-IV depression criteria with other leading major depressive symptoms into a numerical score graded as mild (5-9), moderate (10-14), moderately severe (15-19), and severe depression (>20) (17).
Perceived Stress Scale (PSS-4)
The PSS-4 is a 4-item survey used to measure perceived psychological stress relating to general stress in the previous month. Scores range from 0 to 16 with higher scores indicating greater perceived stress (18, 19).
Perceived Diabetes Self-Management Scale (PDSMS)
The PDSMS is an 8-item survey measuring diabetes self-efficacy, adapted from the Perceived Medical-Condition Self-Management Scale. Scores range from 8 to 40, with higher scores indicating more confidence in self-managing one’s diabetes. Higher scores are associated with higher reported self-care activities and better glycemic control (20).
Diabetes Distress Scale
The DDS is a 17-item scale that evaluates distress relating to the emotional burden, physician-related distress, regimen-related distress, and interpersonal distress of managing type 2 diabetes over the past month. The mean score is graded on a possible score range of 1–6 with a score of less than 2 indicating low diabetes distress, 2 to greater than 3 moderate diabetes distress and ≥3 severe diabetes distress (7).
Questions on the Impact of COVID
To assess the impact of COVID in the past 6-months, questions (n=20) were pulled from two sources and modified based on feedback from a community advisory board and/or to simplify administration over the phone (21, 22). Participants reported if they experienced any cancelled or rescheduled medical appointments, completed any telemedicine appointments, or faced any delay in diabetes medications or supplies. Participants were also asked if they experienced any income change via loss of employment or employment loss of spouse related to COVID.
Analysis
For analysis, participants were dichotomized into pre-COVID (March 2017 to October 2019) vs during-COVID (October 2020 to May 2021) groups (see Figure 1). These dates were defined based on availability of data. Survey implementation was paused after October of 2019 due to a Medicaid policy change whereby primary care providers were no longer designated as gatekeepers for care. Surveys were scheduled to resume in early Spring however this was delayed due to the impact of COVID on University operations; as such, survey implementation resumed in October 2020. All respondents were unique: no individuals were surveyed twice (pre and during COVID). First, we examined the distribution of continuous variables and the number of observations per cell. Descriptive statistics were used to characterize the study population overall and by COVID time period. Wilcoxon’s tests, t-tests, and chi-square tests were used to determine differences between demographics, depressive symptoms, perceived stress, diabetes distress and self-reported health between groups. Wilcoxon’s and t-test results were similar; results from Wilcoxon’s tests are presented here. Logistic regression was used to model the effect of COVID time period on self-rated health controlling for demographics, severity of diabetes, and diabetes distress. The self-reported health survey scores were dichotomized into to poor health (poor, fair) and better health (good, very good, excellent) for analysis. Covariates selected were either: 1. Specified a priori based on established or potential relationship of the covariate with our outcome variable; or 2. Found to differ between the pre- vs. during-COVID groups. Model 1 adjusted for demographics, model 2 added disease severity factors to model 1 and model 3 added diabetes distress to model 2. We present results for model 3. We then compared experiences of individuals reporting poor and better health during COVID.
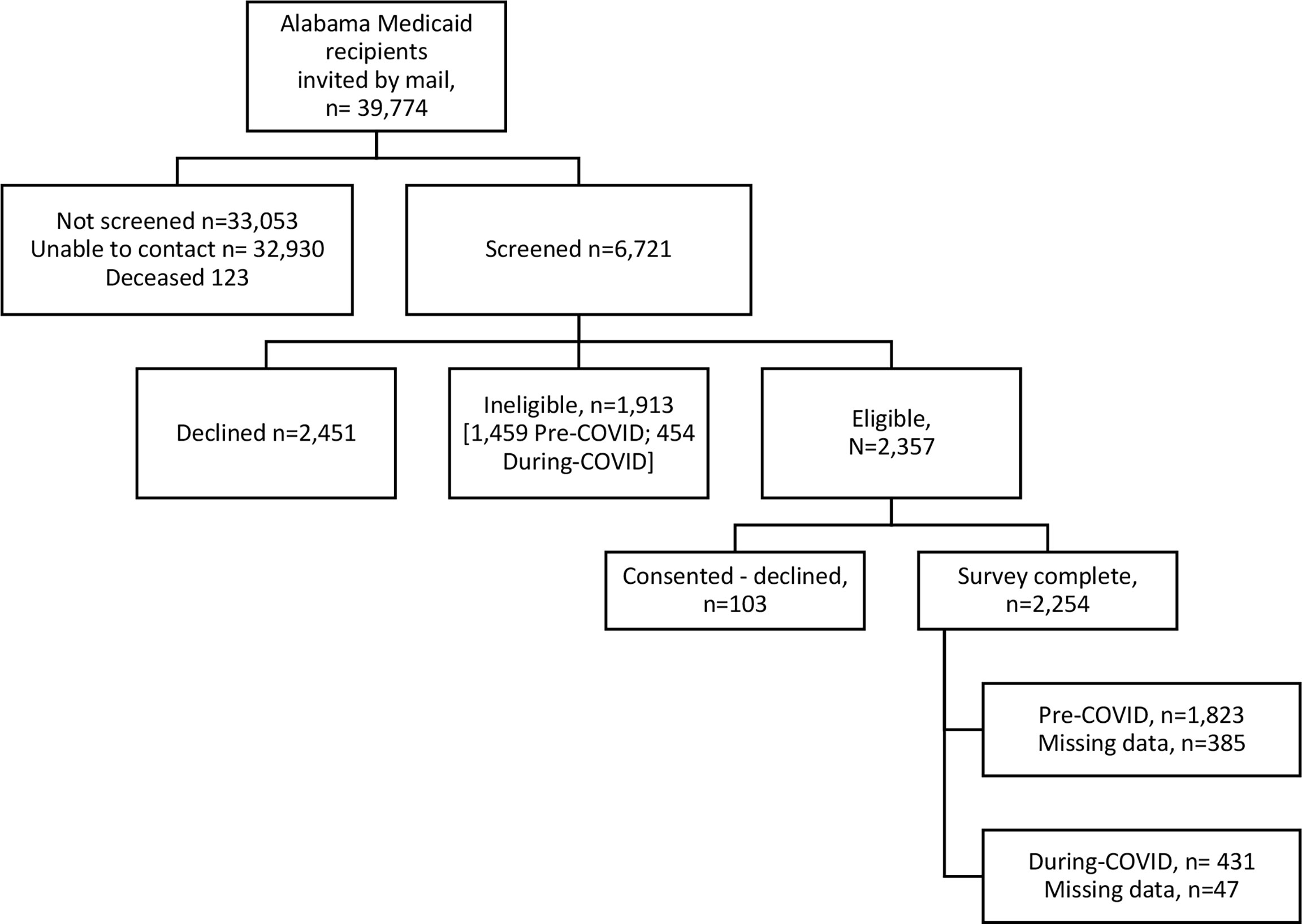
Figure 1 Survey population flow diagram of Alabama Medicaid-covered adults with type 2 diabetes mellitus (March 2017 to May 2021).
Results
Population
In this sample of 1,822 individuals (Table 1), median age was 54, 74.5% were female and 59.4% were Black. Most participants had a high school level education and were unable to work. Median time with DM was 9 years and 44.2% were on insulin. Only 43.3% of participants reported having received diabetes education. Of the sample, 1,438 participants were dichotomized into pre-COVID (March 2017 to October 2019) group and 384 during-COVID (October 2020 to May 2021) group.
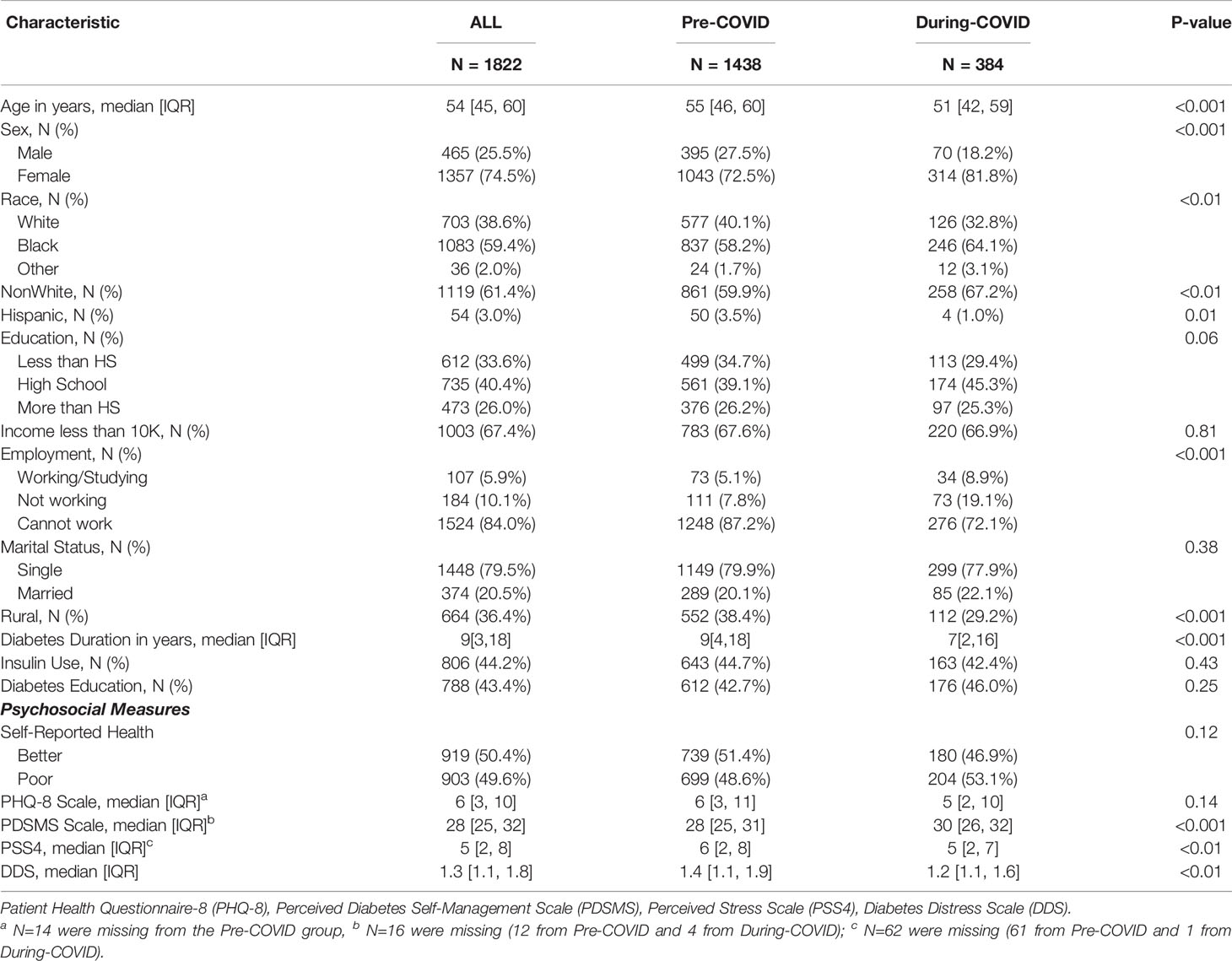
Table 1 Characteristics of survey participants with type 2 diabetes covered by Alabama Medicaid prior to the COVID-19 pandemic and during the COVID-19 pandemic.
Bivariate Associations by COVID Time Group
Participants during COVID were younger with higher proportion of Black individuals (64.1% VS 58.2%, p=0.01) and more females (81.8% VS 72.5%, p<0.001). The during COVID group had fewer individuals reporting inability to work (72.1% VS 87.2%, p<0.001); fewer individuals from rural areas (29.2% VS 38.4%, p<0.001); and a shorter diabetes duration (10.6 years VS 12.5 years, p<0.001). The during COVID group reported slightly higher perceived self-management (PDSMS Score 30 VS 28, p<0.001); moderately better stress ratings (PSS-4 Score 5 VS 6, p<0.01); and modestly lower levels of diabetes distress (1.4 VS 1.2, p<0.01) when compared to the pre-COVID group.
Multivariable Analysis
After adjusting for demographic differences, diabetes severity, and diabetes distress, participants responding during COVID had increased odds of reporting poor or fair health (Odds ratio [OR] 1.41, 95% Confidence Interval [CI] 1.11-1.80) as seen in Table 2.
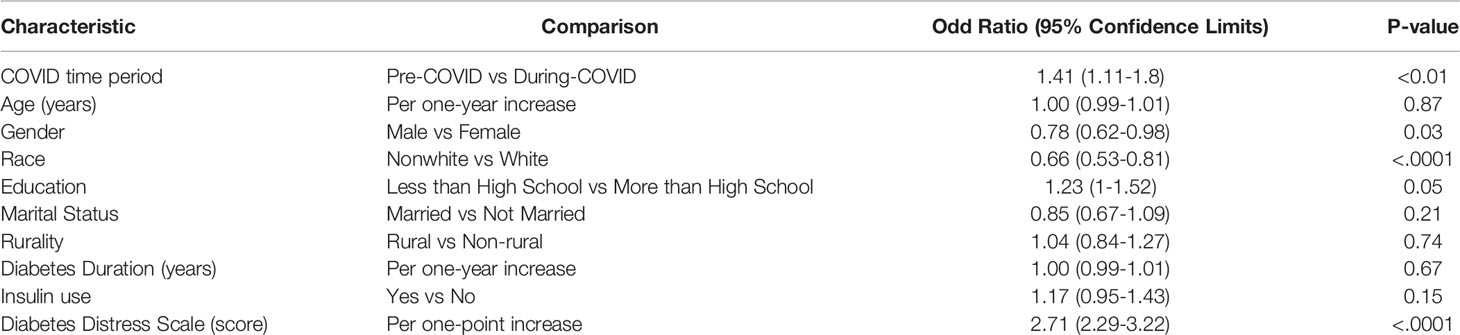
Table 2 Association of COVID time period on self-reported poor health among survey participants with type 2 diabetes covered by Alabama Medicaid (N = 1,822).
Bivariate Differences Between Poor Health vs Better Health During COVID
Participants during COVID who reported poor health were less likely to be working (5.9% VS 12.3%, p=0.0352) compared to those with better health. This group was also less likely to be married (81.9% VS 73.3%, p=0.0445). This group had higher PHQ-8 scores (8 VS 3, p<0.001), lower PDSMS scores (28 VS 30, p<0.001), higher PSS-4 scores (5 VS 4, p<0.001), and higher DSS scores (1.2 VS 1.4, p<0.001) as seen in Table 3.
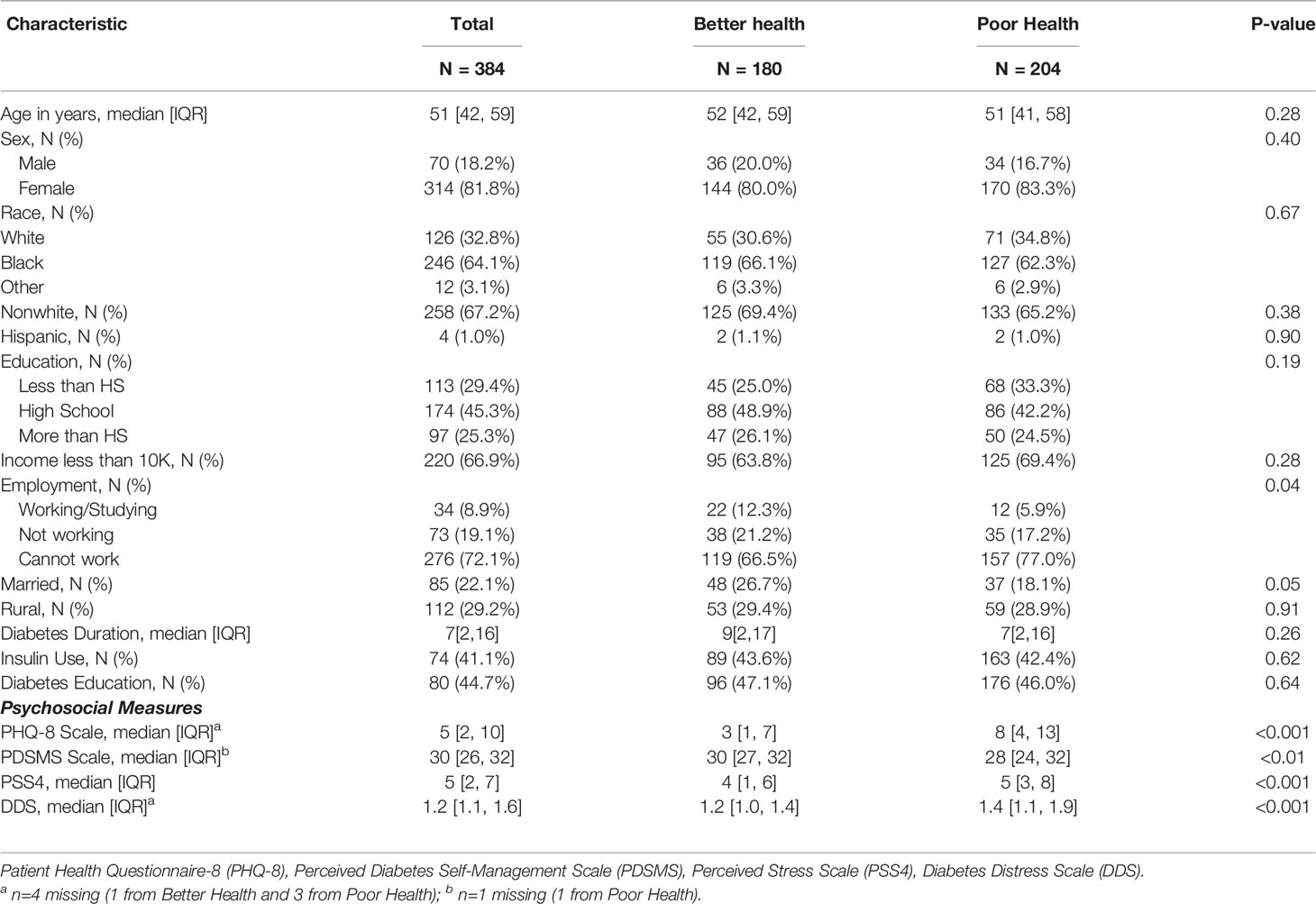
Table 3 Comparison of during-COVID survey participants with type 2 diabetes mellitus by self-reported health status.
Impact of COVID Between Poor Health vs Better Health During COVID
Among participants surveyed during COVID, 34.8% of participants experienced an appointment cancellation or rescheduled appointment with majority due to doctor’s office canceling or moving appointment. Over half of participants were offered a virtual visit via telehealth or phone visit with majority of this group completing a telephone visit. Within this group, 19.8% of participants reported a video visit. Participants who reported poor health were significantly more likely to believe they have had COVID-19 regardless of testing.
Discussion
We found significant differences between the pre-COVID and during-COVID groups participants (Table 1). Notably, the during-COVID group is a younger and more urban group with less diabetes severity. This likely contributes to the higher levels of diabetes self-management (PMDS), reduced perceived stress (PSS-4), and lower levels of diabetes distress (DDS) observed in this analysis. However, there was a modest decrease in self-reported health in the during-COVID group. Multivariate analysis allowed a deeper look into the association of the COVID time period and poor self-reported health (Table 2). After controlling for demographics, severity of diabetes, and diabetes distress, the participants surveyed during COVID were significantly more likely to report poor self-reported health compared to those pre-COVID. Within the during-COVID group, individuals reporting poor health were more likely to report worse depressive symptoms, worse perceived stress, less competency in managing their diabetes, and higher levels of diabetes distress compared to those with better health as seen in Table 3. These factors likely contribute to an overall decreased sense of health and could contribute to worse health outcomes in this group.
Our survey questions related to healthcare experiences during COVID (Table 4) shed additional light on possible barriers experienced by participants. Over a third of respondents experienced cancellation or rescheduled appointment and more than half experienced a virtual health appointment. However, few participants reported delays of care or experienced changes to household income during COVID. Moreover, there was no significant difference in experience between individuals reporting better health or poor health. We predicted that this transition may have been challenging to populations with significant financial barriers and limited access to or unfamiliarity with technology (10, 11, 23). However, this population tolerated this transition well and seems to have minimal changes to their care and household income. This could be related to a limited baseline utilization of healthcare resources within this population prior to COVID and the increased use of virtual medicine during COVID. Recent studies describing the many benefits of virtual care suggest that virtual care is effective in managing patients with diabetes, especially in low socioeconomic groups. With proper access, virtual care can motivate patients, facilitate better medical competency, and provide better decision support for patients. These studies also support the effectiveness of virtual care shown by A1C management similar to or superior to usual care (24).
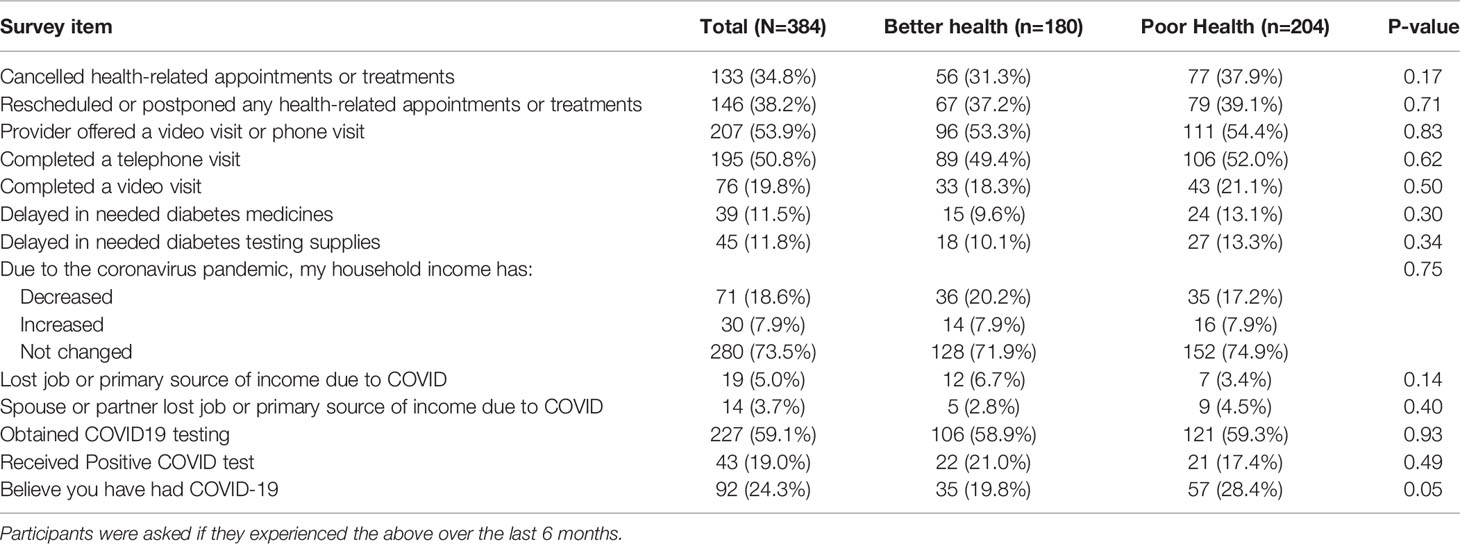
Table 4 Responses to COVID specific questions by self-reported health status among survey participants who participated during COVID (October 2020 to May 2021).
Interestingly, participants who reported poor health were significantly more likely to believe they have had COVID regardless of testing. Additional studies may be needed to identify other contributors to poor self-reported health during COVID within this Alabama Medicaid population.
Limitations
This is a cross-sectional study; thus, we are unable to infer causation between COVID and poor self-reported health. A longitudinal survey with the same respondents at both time periods would help mitigate this limitation. Further, we cannot be sure that differences were not due to policy changes occurring within Medicaid itself or other seasonal changes that may have co-occurred temporally. Our study sample includes adults with type 2 diabetes covered by Alabama Medicaid, which limits the generalizability of our findings to other populations. We used single item measures to review self-reported health which does not fully reflect the multidimensionality or complexity of a participant’s health. Assessments of health were based on self-report, we were unable to include objective measures of diabetes control such as HbA1c. Additional limitations include the limited number of respondents in the during-COVID group and significant demographic differences between respondent groups.
Conclusions
In this sample of Medicaid-covered adults with type 2 DM living in Alabama, individuals surveyed during-COVID reported poorer health compared to those surveyed pre-COVID. Within the during-COVID group, those reporting poor health were more likely to report worse psychosocial symptoms than those who reported better health. Further findings also suggest that while individuals reporting poor health and better health faced similar delays in care, those reporting poor health during-COVID were more likely to believe they have had COVID regardless of testing. Taken together, these findings suggest that physical and mental health may have worsened among some low-income individuals with type 2 DM. Outreach efforts should include specific screening for stress and depression in order to identify and support those in need.
Data Availability Statement
The datasets presented in this article are not readily available because of institutional restriction, the generated dataset is not publicly available. Requests to access the datasets should be directed to Andrea Cherrington, MD, MPH,YWNoZXJyaW5ndG9uQHVhYm1jLmVkdQ==.
Ethics Statement
The studies involving human participants were reviewed and approved by University of Alabama at Birmingham, Office of the Institutional Review Board. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
ACA contributed to the design of the study, analyzed the data, wrote the manuscript, and revised prior drafts of the manuscript for intellectually important content. CH contributed to the design of the study, wrote the manuscript, and revised prior drafts of the manuscript for intellectually important content. ACA, CH, and CP assisted LJ with the analysis and revised the manuscript for intellectually important content. EL contributed to the conception and design of the study, provided expertise on the analysis plan, and revised the manuscript for intellectually important content. AAA contributed to the design of the study and provided expertise on survey implementation. LJ takes responsibility for the integrity of the data and the accuracy of the data analysis. CP provided input on the analysis plan and revised prior drafts of the manuscript for intellectually important content. ACA and AC conceived and designed the study, assisted in data analysis and interpretation, wrote parts of the introduction and discussion section, and revised prior drafts of the manuscript for intellectually important content. The survey data from reported here were collected from Alabama Medicaid Agency recipients with diabetes mellitus. All authors contributed to the article and approved the submitted version.
Funding
The project described was supported by the National Institute of Diabetes and Digestive and Kidney Diseases (R18DK109501, Cherrington). Support was also provided by UAB Diabetes Research Center (P30 DK079626, Cherrington).
Author Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institutes of Health, or the Alabama Medicaid Agency. Representatives for the Alabama Medicaid Agency were provided an opportunity to review and provide comments on the manuscript prior to submission. This manuscript was not prepared in collaboration with the Alabama Medicaid Agency and does not necessarily reflect the opinions or represent the official views of the Alabama Medicaid Agency.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Statistics CNCfH. COVID-19 Mortality Overview: Provisional Death Counts for Coronavirus Disease 2019 (COVID-19) (2021). Available at: https://www.cdc.gov/nchs/covid19/mortality-overview.htm.
2. Basu S. Non-Communicable Disease Management in Vulnerable Patients During Covid-19. Indian J Med Ethics (2020) V(2):103–5. doi: 10.20529/IJME.2020.041
3. Czeisler ME, Barrett CE, Siegel KR, Weaver MD, Czeisler CA, Rajaratnam SMW, et al. Health Care Access and Use Among Adults With Diabetes During the COVID-19 Pandemic - United States, February-March 2021. MMWR Morb Mortal Wkly Rep (2021) 70(46):1597–602. doi: 10.15585/mmwr.mm7046a2
4. Mohseni M, Ahmadi S, Azami-Aghdash S, Mousavi Isfahani H, Moosavi A, Fardid M, et al. Challenges of Routine Diabetes Care During COVID-19 Era: A Systematic Search and Narrative Review. Primary Care Diabetes (2021) 15(6):918–22. doi: 10.1016/j.pcd.2021.07.017
5. Kreider KE. Diabetes Distress or Major Depressive Disorder? A Practical Approach to Diagnosing and Treating Psychological Comorbidities of Diabetes. Diabetes Ther (2017) 8(1):1–7. doi: 10.1007/s13300-017-0231-1
6. Holloway EE, Hendrieckx C, Company G, Skinner TC, Speight J. Diabetes Distress During COVID-19: Three Brief ‘Snapshot’ Surveys of Adults With Diabetes Calling the Australian National Diabetes Services Scheme Helpline. Front Clin Diabetes Healthc (2021) 2. doi: 10.3389/fcdhc.2021.769528
7. Presley CA, Mondesir FL, Juarez LD, Agne AA, Riggs KR, Li Y, et al. Social Support and Diabetes Distress Among Adults With Type 2 Diabetes Covered by Alabama Medicaid. Diabetic Med: J Br Diabetic Assoc. (2021) 38(4):e14503. doi: 10.1111/dme.14503
8. Prevention C-CfDCa. Appalachian Diabetes Control and Translation Project (2021). Available at: https://www.cdc.gov/diabetes/programs/appalachian.html.
9. Barker LE, Kirtland KA, Gregg EW, Geiss LS, Thompson TJ. Geographic Distribution of Diagnosed Diabetes in the U.S.: A Diabetes Belt. Am Prev Med (2011) 40(4):434–9. doi: 10.1016/j.amepre.2010.12.019
10. Xiong J, Lipsitz O, Nasri F, Lui LMW, Gill H, Phan L, et al. Impact of COVID-19 Pandemic on Mental Health in the General Population: A Systematic Review. J Affect Disord (2020) 277:55–64. doi: 10.1016/j.jad.2020.08.001
11. Peters A, Rospleszcz S, Greiser KH, Dallavalle M, Berger K. Complete List of Authors Available Under C. The Impact of the COVID-19 Pandemic on Self-Reported Health. Dtsch Arztebl Int (2020) 117(50):861–7. doi: 10.3238/arztebl.2020.0861
12. Gold M, Franks P, Erickson P. Assessing the Health of the Nation. The Predictive Validity of a Preference-Based Measure and Self-Rated Health. Med Care (1996) 34(2):163–77. doi: 10.1097/00005650-199602000-00008
13. Foundation KF. Medicaid in Alabama 2019 (2019). Available at: http://files.kff.org/attachment/fact-sheet-medicaid-state-AL.
14. Chronic Conditions Data Warehouse: Centers for Medicare & Medicaid Services (CMS). Available at: https://www2.ccwdata.org/web/guest/condition-categories.
15. Bronstein JM, Huang L, Shelley JP, Levitan EB, Presley CA, Agne AA, et al. Primary Care Visits and Ambulatory Care Sensitive Diabetes Hospitalizations Among Adult Alabama Medicaid Beneficiaries. Primary Care Diabetes (2022) 16(1):116–21. doi: 10.1016/j.pcd.2021.10.005
16. Zajacova A, Dowd JB. Reliability of Self-Rated Health in US Adults. Am Epidemiol (2011) 174(8):977–83. doi: 10.1093/aje/kwr204
17. Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a Measure of Current Depression in the General Population. J Affect Disord (2009) 114(1-3):163–73. doi: 10.1016/j.jad.2008.06.026
18. Vallejo MA, Vallejo-Slocker L, Fernandez-Abascal EG, Mananes G. Determining Factors for Stress Perception Assessed With the Perceived Stress Scale (PSS-4) in Spanish and Other European Samples. Front Psychol (2018) 9:37. doi: 10.3389/fpsyg.2018.00037
19. Warttig SL, Forshaw MJ, South J, White AK. New, Normative, English-Sample Data for the Short Form Perceived Stress Scale (PSS-4). J Health Psychol. (2013) 18(12):1617–28. doi: 10.1177/1359105313508346
20. Wallston KA, Rothman RL, Cherrington A. Psychometric Properties of the Perceived Diabetes Self-Management Scale (PDSMS). J Behav Med (2007) 30(5):395–401. doi: 10.1007/s10865-007-9110-y
21. CAHPS Adult Survey 5.0. Available at: https://www.ahrq.gov/cahps/surveys-guidance/hp/index.html.
22. Services CfMM. 2020 Summer Supplemental Covid-19 Questionnaires (2020). Available at: https://www.cms.gov/research-statistics-data-and-systemsresearchmcbsquestionnaires/2020-summer-supplemental-covid-19-questionnaires.
23. Hossain MM, Tasnim S, Sultana A, Faizah F, Mazumder H, Zou L, et al. Epidemiology of Mental Health Problems in COVID-19: A Review. F1000Res (2020) 9:636. doi: 10.12688/f1000research.24457.1
Keywords: diabetes, self-reported health, medicaid, COVID, survey
Citation: Amerson AC, Juarez LD, Howell CR, Levitan EB, Agne AA, Presley CA and Cherrington AL (2022) Diabetes Distress and Self-Reported Health in a Sample of Alabama Medicaid-Covered Adults Before and During the COVID-19 Pandemic. Front. Clin. Diabetes Healthc. 3:835706. doi: 10.3389/fcdhc.2022.835706
Received: 14 December 2021; Accepted: 14 March 2022;
Published: 10 May 2022.
Edited by:
Rossella Messina, University of Bologna, ItalyReviewed by:
Maria Helena M. Lima, State University of Campinas, BrazilMarica Iommi, University of Bologna, Italy
Copyright © 2022 Amerson, Juarez, Howell, Levitan, Agne, Presley and Cherrington. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Andrea L. Cherrington, YWNoZXJyaW5ndG9uQHVhYm1jLmVkdQ==
 Alesha C. Amerson
Alesha C. Amerson Lucia D. Juarez2
Lucia D. Juarez2