
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Clin. Diabetes Healthc. , 15 March 2022
Sec. Diabetes Self-Management
Volume 3 - 2022 | https://doi.org/10.3389/fcdhc.2022.830353
This article is part of the Research Topic Psychosocial Repercussions of the Covid-19 Pandemic for People Living with or Supporting Others with Diabetes View all 10 articles
Background: The effect of the COVID-19 pandemic on diabetes self-management behaviors is unclear.
Objectives: This paper is a scoping review of studies examining health behaviors among people with type 2 diabetes during the COVID-19 pandemic.
Eligibility Criteria: We searched articles available in English using the Search terms “COVID” and “diabetes”, and, separately, each of the following terms: “lifestyle”, “health behavior”, “self-care”, “self-management”, “adherence”, “compliance”, “eating”, “diet”, “physical activity”, “exercise”, “sleep”, “self-monitoring of blood glucose”, or “continuous glucose monitoring”.
Sources of Evidence: We searched PubMed, PsychInfo, and Google Scholar databases from December 2019 through August 2021.
Charting Methods: Data were extracted by 4 calibrated reviewers and study elements were charted.
Results: The search identified 1,710 articles. After screening for relevance and eligibility, 24 articles were included in this review. Findings show the strongest evidence for reduced physical activity and stable glucose monitoring and substance use. There was equivocal evidence for deleterious changes in sleep, diet, and medication intake. With one minor exception, there was no evidence for favorable changes in health behaviors. Limitations of the literature include small samples, predominantly cross-sectional study designs, reliance on retrospective self-reports, sampling through social media, and few standardized measures.
Conclusions: Early studies of health behaviors among people with type 2 diabetes during the COVID-19 pandemic suggest a need for novel interventions to support diabetes self-management, especially targeting physical activity. Future studies should go beyond documenting changes in health behaviors and examine predictors of change over time.
Over 460 million individuals, which equates to over six percent of the global population, have type 2 diabetes mellitus (T2DM) (1). Prevalence rates continue to rapidly incline across age groups and all regions of the world (1). The diabetes epidemic is alarming, as a diagnosis of T2DM is associated with a greater risk of mortality (2) and chronic (e.g., heart disease; renal disease) (3) and terminal (e.g., cancer) illnesses (4). To effectively manage T2DM, patients are prescribed a comprehensive self-management plan (5). Diabetes self-management plans typically encourage regular engagement in various health behaviors, including but not limited to self-monitoring blood glucose levels (SMBG), medication intake, conducting foot examinations, eating a balanced diet, and engaging in physical activity (5). However, due to various factors (e.g., financial constraints, difficulties with planning, low self-efficacy), patients with T2DM often struggle with regularly completing their diabetes self-management behaviors (6).
In response to increased stressors and social distancing requirements, the Coronavirus Disease of 2019 (COVID-19) pandemic has affected individuals’ engagement in daily health behaviors (7–9). It can be hypothesized that health behavior engagement in the T2DM community has been impacted as well. For example, in a pre-pandemic study, adults with T2DM reported financial strain as a reason for below-target medication intake (6). The pandemic has affected the financial security of many individuals globally, causing downstream effects on financial stress and psychopathology (10), such that it can be anticipated that patients with T2DM have encountered additional barriers that further reduced their medication intake in the context of the COVID-19 pandemic. Accordingly, researchers have examined changes in metabolic outcomes in patients with T2DM during the COVID-19 pandemic (11–15). Data are equivocal and suggest metabolic control has either decreased or remained stable in patients with T2DM during the pandemic (11–15). Yet, less attention has been paid to examining changes in the diabetes self-management behaviors that are important in contextualizing metabolic outcomes in this population. The pandemic is expected to persist (16) and pandemics will continue to present in the future (17). It is imperative to explore diabetes self-management behavior engagement during the COVID-19 pandemic to identify ways to support patients with T2DM, both during the pandemic and beyond.
The purpose of the current review was two-fold: 1) to characterize diabetes self-management behavior engagement in individuals with T2DM during the COVID-19 pandemic, and 2) where available, to characterize changes in diabetes self-management behavior engagement in individuals with T2DM from the pre-pandemic period to the pandemic period. Given the dearth of studies in the area, we conducted a scoping review. Scoping reviews are uniquely indicated to identify and map types of available evidence, to examine how research has been conducted, and to identify knowledge gaps. Based on the extant literature reviewed, we provide recommendations for future research and preliminary suggestions for practice with individuals with T2DM during and after the pandemic.
We followed methodological guidance (18) for Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) (19). We systematically searched PubMed, PsychInfo, and Google Scholar databases from December 2019 through August 2021. We restricted the search to articles available in English and used the Search terms “COVID” and “diabetes”, and, in separate searches, each of the following terms: “lifestyle”, “health behavior”, “self-care”, “self-management”, “adherence”, “compliance”, “eating”, “diet”, “physical activity”, “exercise”, “sleep”, “self-monitoring of blood glucose”, “SMBG”, “continuous glucose monitoring”, or “CGM”.
One author (JW) drafted a data extraction chart based on PRISMA scoping guidelines which was beta tested by all four authors and modified to include directional arrows for results. Data were charted for author, publication year, country and time period of data collection, sample size and characteristics, sampling method, health behavior(s) studied, specific measures, results, and unique or ancillary findings.
One author (KS) conducted the electronic database searches and screened all titles and abstracts to remove irrelevant papers. Two screeners (KS and JW) reviewed remaining abstracts to remove ineligible papers. All four authors (CC, RT, KS, JW) read the remaining full articles, and further removed ineligible papers. To address consistency across the reviewers and to decrease bias, five articles were reviewed independently by all four reviewers and extracted data were compared. Differences in responses were noted and discussed until consensus was reached. An additional five articles were reviewed independently by two reviewers (CC and RT) using the same process until the first author (CC) judged that data extraction was sufficiently consistent. The first author reviewed the final tables for accuracy and consistency.
We followed guidelines for conducting (18) and reporting (19) a scoping review. A scoping review is a particular type of review that is indicated for topics in which the body of literature is nascent. A scoping review should be differentiated from, for example, a systematic review or a meta-analysis, which are indicated when a body of literature is well developed and are designed to produce statements to guide clinical decision making (20). Scoping reviews do not report indicators of assessments of bias. Also, scoping reviews are, by definition, not designed to produce clear practice guidelines, but instead to update readers regarding needed future research. To describe the role of COVID-19 on health behaviors, attempts were made to characterize results in terms of increase, decrease, or no change in the health behavior compared to pre-COVID-19 levels.
See Figure 1 for PRISMA-ScR flow diagram. Search results identified 1,710 articles. Of them, 1,428 articles were removed because they were not relevant. Many of the articles that were removed at this stage reported, for example, incidence and prevalence of COVID-19 among people with diabetes, hyperglycemia as a risk factor for COVID-19 morbidity and mortality, or experimental treatments for COVID-19 in people with diabetes.
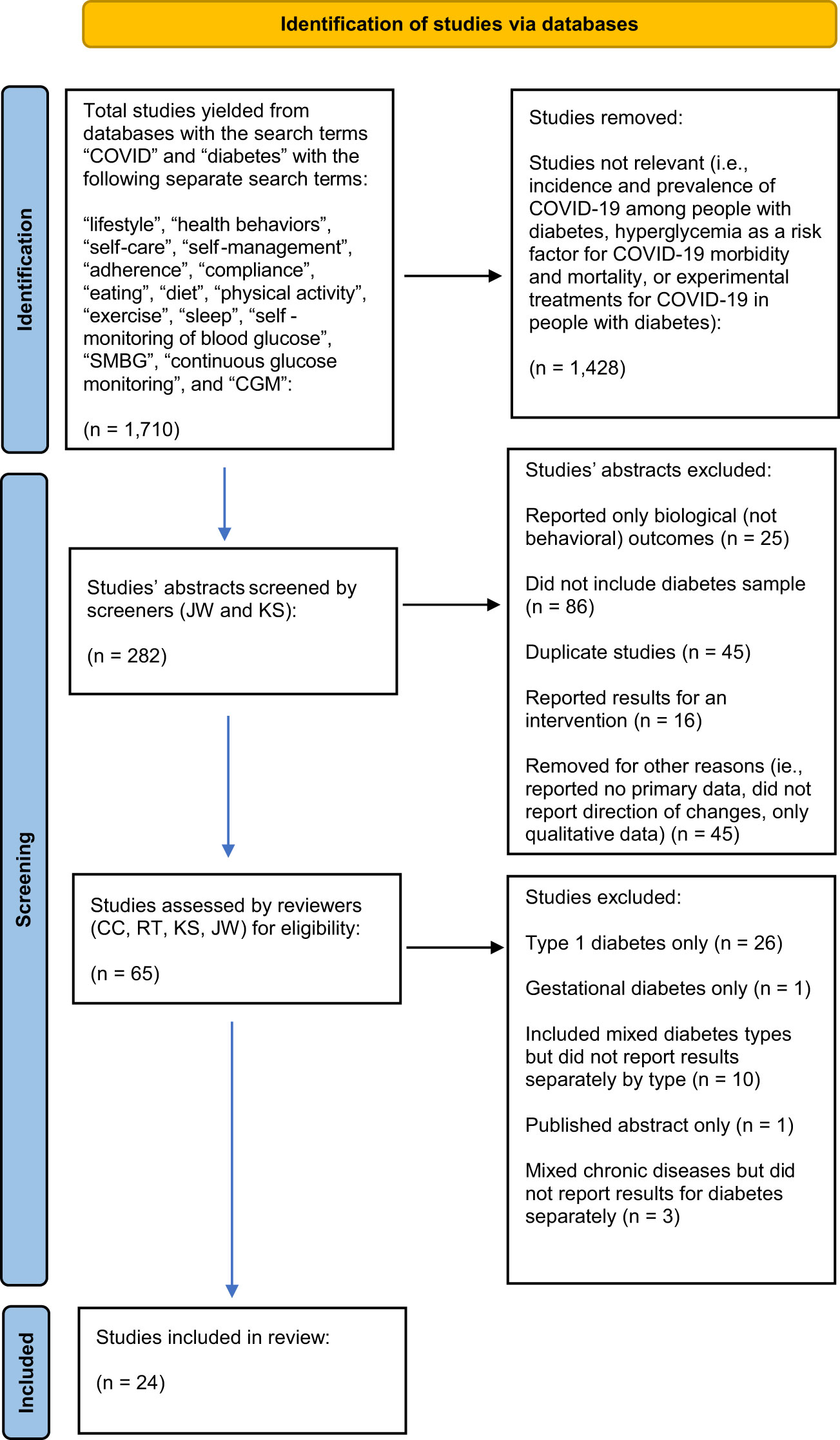
Figure 1 PubMed, PsychInfo, and Google Scholar databases from December 2019 through August 2021.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. doi: 10.1136/bmj.n71.
The remaining 282 abstracts were reviewed and of them, n=25 were removed because they reported only biological (not behavioral) outcomes (to be included, articles were not required to report health behaviors as the primary outcome but were required to report health behaviors). Additional articles were removed because they were case studies or did not include a diabetes sample (n=86), reported results of an intervention (n=16), were reviews that did not report any primary data (n=42), included qualitative data (n=1), or reported that there had been changes in health behaviors but did not report the direction of the changes (n=2). Of the remaining articles, an additional n=45 were removed because they were duplicates across searches. The remaining full articles were read and an additional n=41 articles were removed because they reported data only for type 1 diabetes mellitus (n=26) or gestational diabetes (n=1), or they included mixed diabetes types but did not report results separately by type of diabetes (n=10). One article was a published abstract only and three reported mixed chronic diseases and did not report results for diabetes separately.
Articles were divided into two categories based on study design. One category of studies asked participants about their current level of health behaviors; those articles only reported frequencies or means of health behaviors during COVID-19 (n=5). The other category attempted to characterize changes in self-management from pre-COVID-19 levels to COVID-19 levels (n=19). See Figure 2 for a map of health behaviors measured by number of studies.
In the first category, articles reported data from Brazil, China, Ethiopia, and Turkey. Sample sizes ranged from n=101 in Turkey (21) to n=1,253 in China (22). All participants were recruited from clinics. Shimels et al. (23) studied people with diabetes and comorbid hypertension. For the articles that reported a time period of data collection, dates ranged from March 2020 to August 2020. See Table 1. Note that where articles reported only frequencies—even if there was considerable variability—for parsimony we present only the modal response.
Three studies assessed physical activity. Onmez et al. (21) found that the modal response was that physical activity rarely or never occurred. Kaplan Serin and Bulbuloglu (27) found that physical activity was irregular. Tao et al. (22) found moderate levels of physical activity.
Four studies assessed diet. Onmez et al. (21) found that the modal response was that following dietary recommendations rarely occurred. Alessi et al. (24) found that 74% screened positive for an eating disorder. However, Kaplan Serin and Bulguloglu (27) found high dietary compliance and Tao et al. (22) found regular meal intake.
One study (24) assessed sleep and found that 78% screened positive for a sleep disorder.
Two studies assessed medication intake. Shimels et al. (23) found low levels of medication intake and Tao et al. (22) found high levels of medication intake.
Two studies assessed SMBG. Onmez et al. (21) found that the modal response was that SMBG rarely occurred. Tao et al. (22) found that the modal response was ≥ 2 times per week for SMBG.
No studies in this category assessed substance use.
In the second category (i.e., papers that described change in health behaviors from pre-COVID-19 to COVID-19), articles reported data from Australia, Brazil, France, India, Japan, Malaysia, Mexico, the Netherlands, Poland, Saudi Arabia, Spain, Turkey, United Kingdom, and USA. Notably, one study examined bariatric surgery patients (32) and another studied children and adolescents (33). Only n=3 implemented longitudinal methodology, i.e., followed the same cohort over time; they were based in India (34), the United Kingdom (35), and Australia (36). For the articles that reported a time period of data collection, dates ranged from March 2020 to April 2021, though Rowlands et al. (35) had baseline data dating back to 2017. One study in Brazil compared data from a sample of people with diabetes during COVID-19 to data from an age-matched sample of people with diabetes in 2016 (37). The remainder (n=15) of studies asked participants to report their current health behaviors and also to recall their pre-COVID-19 health behaviors. Sample sizes ranged from n=56 in Japan (38) to n=1,633 in Brazil (39). N=4 were recruited using social media, n=3 reported data from people with diabetes in registries or who were already enrolled in research studies, and the remainder (n=12) recruited clinic samples. See Table 2.
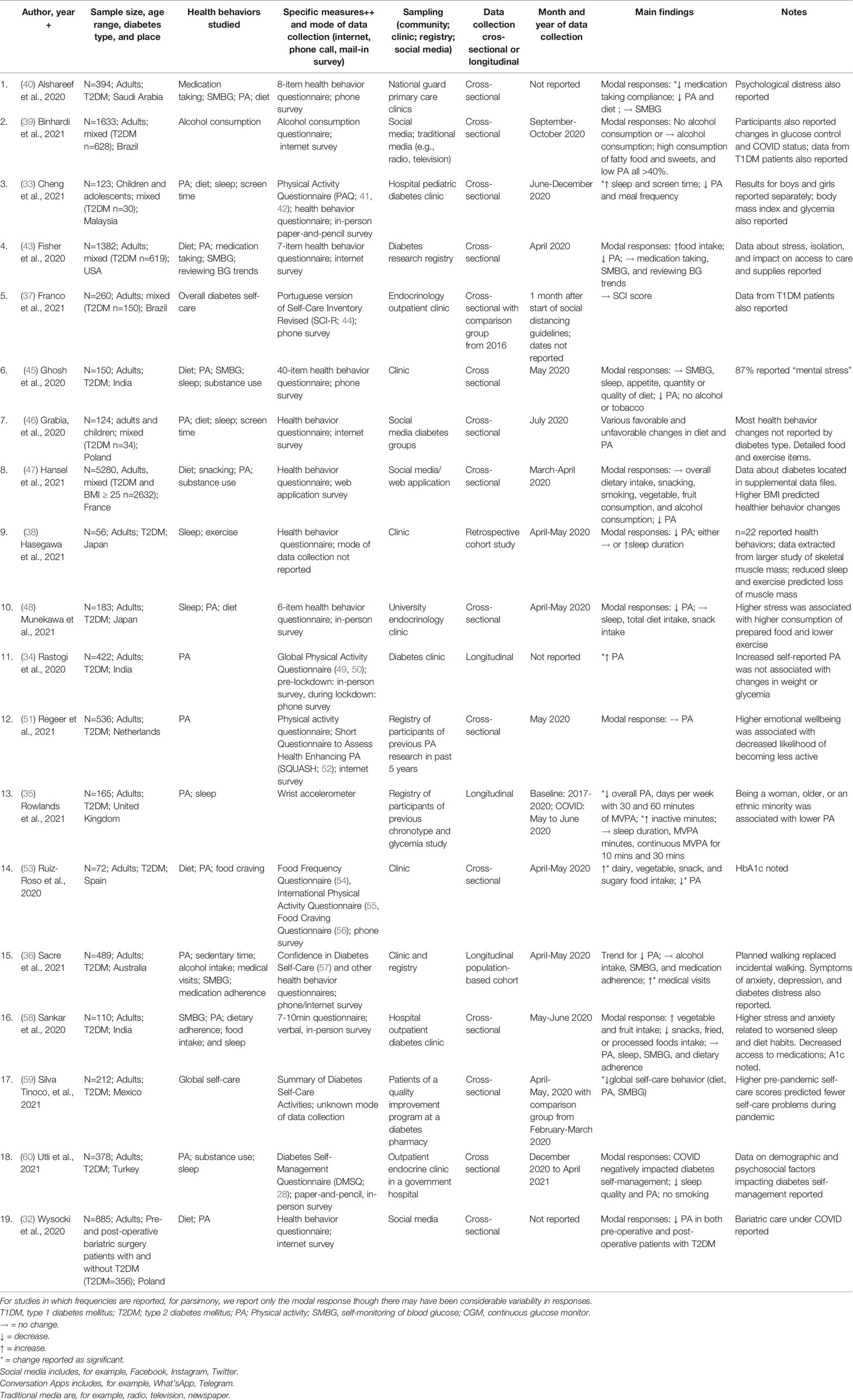
Table 2 Change in health behaviors from pre-COVID period to COVID among people with type 2 diabetes.
Sixteen of the 19 articles assessed physical activity. The majority (n=15) of studies reported decreased physical activity (32, 33, 35, 38, 40, 43, 45–48, 53, 60) or low physical activity (39). Three studies reported no change (36, 51, 58) and one reported increased physical activity (34). Regeer et al. (51) found that changes in physical activity were related to stress and emotional wellbeing; participants with higher emotional wellbeing were more likely to report no change than to report decreased physical activity. Rowlands et al. (35) found that being a woman or having a higher body mass index predicted lower physical activity and higher inactive time. Being older or an ethnic minority predicted higher inactive time.
Eleven studies assessed diet. Several studies reported an increase in unfavorable dietary habits, including decreased dietary adherence (40), high consumption of fatty foods and sweets (39), and increased food intake (43, 53). One study reported favorable changes in diet, i.e., increased fruit and vegetables and decreased snacks, fried, or processed foods (58). Four studies reported no change in dietary habits, including no change in appetite, quantity or quality of diet, or consumption of fruits (45), no change in overall dietary intake, snacking, fruit and vegetable consumption (47), and no change in total dietary intake or snack intake (48). One study reported various detailed favorable and unfavorable changes in diet (46).
Eight studies reported on sleep. Cheng et al. (33) reported increased sleep and Hasegawa et al. (38) reported increased sleep duration. One study reported decreased sleep quality (60). Four studies reported that the modal response was no changes in sleep (35, 45, 48, 58).
Four studies reported medication intake. Two studies reported decreased medication intake (40), and two studies reported no change (36, 43).
All five studies that assessed SMBG reported no change (36, 40, 43, 45, 58).
Six studies reported substance use. For alcohol, Binhardi et al. (39) and Ghosh et al. (45) reported that modal responses were no alcohol consumption or no change in alcohol consumption, respectively. Hansel et al. (47) and Sacre et al. (36) reported no change in alcohol consumption. For smoking, Utli et al. (60) and Ghosh et al. (45) reported no smoking as the modal response.
Three studies examined global diabetes self-care scores. One study reported no change (37) and two studies (59, 60) reported decreased total diabetes self-care scores. Silva-Tinoco et al. (59) found that higher pre-pandemic self-care was related to fewer problems with self-care during the pandemic. Utli et al. (60) found that being a man, smoker, and older in age, and having more anxiety and stress and decreased support from healthcare providers, predicted lower global self-care.
This scoping review examined the extant literature regarding health behavior engagement among individuals with T2DM during the COVID-19 pandemic. Across studies, the strongest evidence was for a reduction in physical activity and there was small but consistent evidence for no change in SMBG and substance use. Global diabetes self-care decreased in two of three studies. Overall, dietary habits appear to have remained stable or worsened and in one study a high percentage of participants screened positive for a possible eating disorder. There were equivocal findings regarding medication intake and sleep. Older age, lower pre-pandemic self-care, and decreased emotional wellbeing and support from healthcare providers predicted greater deterioration in diabetes self-care behaviors. Unfortunately, many studies included the administration of unstandardized measures and descriptive statistics as an analytic plan; thus, a comparison of findings across studies and evaluation of effect sizes could not be conducted. This review points to multiple recommendations for future research and clinical practice with the T2DM population.
Most studies demonstrated a reduction in physical activity during the pandemic, highlighting the need for novel interventions to support individuals with T2DM in engaging in this essential diabetes management behavior. A few studies (35) pointed out that when activity occurred, planned fitness activities (e.g., a workout session) may have replaced incidental physical activity (e.g., walking to the store). It has been hypothesized that reductions in physical activity by the general public in the context of the pandemic might be a function of stress and fear associated with potential contraction of COVID-19 (7), which may in turn motivate individuals to reduce or avoid physical activity in groups and in public areas. This may be especially true for the T2DM population, who have received public health messaging that they are at a higher risk of contracting COVID-19 and experiencing severe symptoms due to their altered immune and metabolic system functioning (61). Given the key role of physical activity in supporting optimal glycemic control in this population (62), it is imperative to further investigate patterns of physical activity during the pandemic and as societies shift towards “normalcy” and a post-pandemic period.
A lack of change in SMBG levels was observed in the studies that reviewed glucose monitoring, which suggests that, despite an increase in stress and disruption in individuals’ daily routine (63), SMBG remained relatively stable in this population. Given that SMBG is strongly correlated with glycemic control (64), and some studies show an increase in blood glucose levels and glycated hemoglobin during the pandemic (11), this finding is surprising and suggests that other key diabetes management behaviors might be impacted during the pandemic that are causing downstream unfavorable effects on individuals’ glycemic control. Moreover, the lack of change in SMBG should be of concern when considering that those individuals who demonstrated low SMBG pre-pandemic were also likely to demonstrate continued difficulties with SMBG (65); thus, there remains a subpopulation of individuals with T2DM (i.e., those who demonstrate low SMBG and, in turn, above-target glycemic control) who are highly susceptible to experiencing adverse reactions when acquiring COVID-19. Continued study of SMBG and its relation to glycemic control, and possibly COVID-19 infection severity, across the pandemic is warranted.
Most individuals with T2DM reported little to no substance use during the pandemic and no change from the pre-pandemic period. This is inconsistent with data highlighting the widespread increase in substance use by the general population during the pandemic (66). It is possible that participants may have underreported substance use due to demand characteristics and social desirability, especially when questionnaires were administered by healthcare providers (e.g., studies with samples of patients that were being seen in clinic at the time of questionnaire completion). Nonetheless, findings suggest that substance use may be a relatively lower priority for researchers and clinicians to address in their work with people with diabetes, compared to other health behaviors that were more clearly impacted by the pandemic, such as physical activity.
Studies examining changes in and frequency of engagement in the remaining health behaviors yielded equivocal results. Specifically, there was a near-even split of studies that reported a lack of change or decrease in medication intake, sleep, and diet. Only two studies suggested a favorable increase in any of these health behaviors, finding an increase in participants’ consumption of dairy, vegetables, and/or fruits (53, 58), but this was an exception. For the T2DM population as a whole, the reviewed studies suggest that there are no consistent or compelling data to suggest that diabetes self-management behaviors improved during the pandemic.
There are several possible explanations for differing results across studies, including the time frame of data collection, region in which the study was conducted, measure/questionnaire employed, and sampling strategy. First, it is possible that contradictory findings may be a result of differences in COVID-19 guidelines and lockdown regulations across time and regions. For example, medication intake and SMBG may have been influenced by an individual’s inability to pick up prescriptions in regions that had more restrictive lockdowns, or when medical supply chains were disrupted. Second, inconsistent findings may have emerged due to use of varying measures. Most studies reviewed designed their own questionnaires which varied by content, item stem, and response options. Most were retrospective self-reports that required participants to recall temporally distal health behaviors from 6-months to 1-year ago or more. Self-report measures are subject to numerous sources of bias and retrospective measures are subject to poor recall. Depending on the research question at hand, objective measures may be preferable when feasible. Objective sleep and physical activity characteristics may be best captured by actigraphy data, which was only used in one study that indicated decreased overall physical activity and stable sleep duration from the pre-pandemic period to the pandemic period (35). Diet is extremely challenging to measure without intensive methods, such as photographic food records (67), which were not used in any studies. Measuring the frequency of glucose monitoring is made easier with uploadable meters and continuous glucose monitors, but these data were not reported in most studies. Also, substance use is best measured via daily reports (68) or, in some cases, biospecimen testing. Finally, sampling strategies may have yielded differing results. Several studies recruited participants through social media. Data from those studies may have limited generalizability, as reviews have shown that participants recruited through social media differ from those recruited through traditional methods (69).
Perhaps the greatest missed opportunity in the literature to date is that, with a few exceptions (35, 51, 59, 60), the majority of studies simply reported change in behavior as frequencies of ‘increase’, ‘decrease’, or ‘no change,’ but did not examine predictors of direction or degree of change. In order to efficiently direct resources to the patients most in need of self-management support, it is helpful to know the individual characteristics that predict diabetes self-management during the pandemic. For example, perhaps individuals who experienced financial downturn, who live alone, or whose pre-pandemic glycemic control was suboptimal are in the greatest need of self-management support during the pandemic. On the other hand, perhaps those who were allowed to work from home, with greater access to outdoor space for physical activity, or with home prescription delivery were able to maintain or even improve their diabetes self-management. Elucidating the factors related to behavioral vulnerability and resilience can help tailor intervention development and delivery.
It should be acknowledged that researchers had to move quickly to document changes in diabetes self-management during the COVID-19 pandemic. Planning the study, procuring funding, obtaining ethics approval, and collecting data are all time intensive. Moreover, this research was being conducted in the midst of social distancing measures that made best-practices for behavioral diabetes research difficult or impossible. Efforts to conduct research under these conditions are to be lauded. Notwithstanding these commendations, as researchers continue to collect data on pandemic-specific health behavior engagement in this population, it will be important going forward to use standardized, objective measures where possible, as well as recruit participants who are well characterized, follow them over time across different phases of the pandemic, and examine predictors of behavior change.
Our conclusions are qualified by several limitations of this review. First, database review concluded in August of 2021, and it is likely that additional articles have been published since then but were not included in the current review. Second, studies reviewed were limited to data from individuals with T2DM. Findings may not be representative of changes in health behavior in individuals with type 1 diabetes, gestational diabetes, or pre-diabetes. This is an area for future research. Third, most studies were conducted with adult samples, thus findings may not generalize to health behavior of children and adolescents with diabetes. Fourth, due to the extreme heterogeneity in samples, sampling, and measures across studies, a meta-analysis could not be conducted, thus the interpretability of findings is limited. Fifth, in those studies that reported frequencies only, we reported modal responses. Across every study, there were subsamples of participants who reported favorable changes, unfavorable changes, and stable health behaviors. Therefore, it should not be concluded that all individuals with T2DM demonstrated self-management decrements in response to the pandemic. Finally, scoping reviews do not report indicators of assessment of bias and do not produce clear practice guidelines.
Findings from this brief review indicate that individuals with T2DM demonstrated reduced engagement in physical activity during the pandemic and no change in SMBG or substance use. The frequency of and potential change in medication intake, sleep, and diet during the pandemic was less clear, but there is virtually no evidence that the population as a whole improved their diabetes self-management during the COVID-19 pandemic.
Moving forward, researchers should aim to use standardized health behavior measures to allow for a comparison of findings across samples. In addition, where available, researchers should attempt to access pre-existing data, such as data located within patients’ medical records, to allow for more precision in their comparisons of health behavior prior to and during the pandemic. These data are especially important in identifying ways to support this population in returning to “normalcy” and re-establishing their diabetes self-management routines as the pandemic progresses and eventually ends. Even if the pandemic does eventually conclude, there may be other pandemics, natural disasters, climate disruptions, warfare, or civil unrest that have the potential to drastically impact the self-management of people with diabetes. In addition, researchers should prioritize conducting research with children and adolescents with T2DM. Moreover, future data should help identify those individuals with T2DM who demonstrated limited engagement in diabetes self-management behaviors pre-pandemic and continued to struggle, or deteriorate, throughout the pandemic. This subpopulation is important to study and may require more assistance in developing an individualized, specific diabetes self-management plan. Upon publication of further reports, a systematic review and meta-analysis should be conducted to further characterize the frequency of and changes in diabetes self-management health behaviors during the COVID-19 pandemic.
Clinically, providers are encouraged to closely monitor diabetes self-management in their patients, especially their older patients, as the pandemic continues to unfold globally with additional waves and new variants. Specifically, we recommend patient-provider problem-solving of specific steps to increase physical activity within the confines of COVID-19 guidelines and restrictions, such as scheduling daily 30-minute virtual physical activity exercises with friends or family. Patients should be encouraged to explore outdoor venues, such as parks, trails, and other open space, if available, in their neighborhood. Next, with the current increases in access to digital health technologies, healthcare providers should consider “prescribing” patients to download and complete digital health programs. This could include informal tracking of diet and physical activity with applications that allow users to share these data with friends and/or family, thereby providing external motivation and social support to improve the corresponding diabetes self-management behaviors. More structured digital health programs exist and should be considered. For example, see Fu et al. (70) for a review of existing diabetes/lifestyle applications. Last, and importantly, for those individuals with T2DM who demonstrate disruptions in diabetes self-management as a result of impaired psychological functioning in the context of the pandemic, providers should connect patients to psychological care where it is accessible. This might include “prescribing” patients mindfulness/meditation, relaxation, or other evidence-based digital mental health applications. In addition, provision of either in-person or telemedicine mental health services is recommended for patients experiencing significant mental health concerns and may elicit downstream improvements in diabetes self-management.
The data that support the findings of this study are available from the corresponding author, JW, upon reasonable request.
JW conceived of the study and wrote methods and results. KS screened articles. CC, JW, KS, and RT reviewed articles and populated tables. CC and JW wrote the manuscript. RT formatted tables. CC and KS designed figures. KS and RT edited the manuscript. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Khan MAB, Hashim MJ, King JK, Govender RD, Mustafa H, Al Kaabi J. Epidemiology of Type 2 Diabetes–Global Burden of Disease and Forecasted Trends. J Epidemiol Global Health (2020) 10(1):107. doi: 10.2991/jegh.k.191028.001
2. Carrillo-Larco RM, Barengo NC, Albitres-Flores L, Bernabe-Ortiz A. The Risk of Mortality Among People With Type 2 Diabetes in Latin America: A Systematic Review and Meta-Analysis of Population-Based Cohort Studies. Diabetes/Metabolism Res Rev (2019) 35(4). doi: 10.1002/dmrr.3139
3. Visaria J, Iyer NN, Raval A, Kong S, Hobbs T, Bouchard J, et al. Incidence and Prevalence of Microvascular and Macrovascular Diseases and All-Cause Mortality in Type 2 Diabetes Mellitus: A 10-Year Study in a US Commercially Insured and Medicare Advantage Population. Clin Ther (2019) 41(8):1522–36. doi: 10.1016/j.clinthera.2019.05.012
4. Onitilo AA, Engel JM, Glurich I, Stankowski RV, Williams GM, Doi SA. Diabetes and Cancer I: Risk, Survival, and Implications for Screening. Cancer Causes Control (2012) 23(6):967–81. doi: 10.1007/s10552-012-9972-3
5. Beck J, Greenwood DA, Blanton L, Bollinger ST, Butcher MK, Condon JE, et al. 2017 National Standards for Diabetes Self-Management Education and Support. Diabetes Educator (2018) 44(1):35–50. doi: 10.2337/dc14-S144
6. Adu MD, Malabu UH, Malau-Aduli AE, Malau-Aduli BS. Enablers and Barriers to Effective Diabetes Self-Management: A Multi-National Investigation. PloS One (2019) 14(6). doi: 10.1371/journal.pone.0217771
7. Cummings C, Humiston T, Cohen LB, Lansing AH. The Role of COVID-19 Fears and Related Behaviors in Understanding Daily Adolescent Health Behaviors During the Pandemic. J Health Psychol (2021). doi: 10.1177/13591053211044533
8. Rebić N, Park J, Garg R, Ellis U, Kelly A, Davidson E, et al. A Rapid Review of Medication Taking (A’dherence’) Among Patients With Rheumatic Diseases During the COVID-19 Pandemic. Arthritis Care Res (2021). doi: 10.1002/acr.24744
9. Stanton R, To QG, Khalesi S, Williams SL, Alley SJ, Thwaite TL, et al. Depression, Anxiety and Stress During COVID-19: Associations With Changes in Physical Activity, Sleep, Tobacco and Alcohol Use in Australian Adults. Int J Environ Res Public Health (2020) 17. doi: 10.3390/ijerph17114065
10. Hertz-Palmor N, Moore TM, Gothelf D, DiDomenico GE, Dekel I, Greenberg DM, et al. Association Among Income Loss, Financial Strain and Depressive Symptoms During COVID-19: Evidence From Two Longitudinal Studies. J Affect Disord (2021) 291. doi: 10.1016/j.jad.2021.04.054
11. Biamonte E, Pegoraro F, Carrone F, Facchi I, Favacchio G, Lania AG, et al. Weight Change and Glycemic Control in Type 2 Diabetes Patients During COVID-19 Pandemic: The Lockdown Effect. Endocrine (2021) 72(3):604–10. doi: 10.1007/s12020-021-02739-5
12. D’Onofrio L, Pieralice S, Maddaloni E, Mignogna C, Sterpetti S, Coraggio L, et al. Effects of the COVID-19 Lockdown on Glycaemic Control in Subjects With Type 2 Diabetes: The Glycalock Study. Diabetes Obes Metab (2021). doi: 10.1111/dom.14380
13. Eberle C, Stichling S. Impact of COVID-19 Lockdown on Glycemic Control in Patients With Type 1 and Type 2 Diabetes Mellitus: A Systematic Review. Diabetol Metab Syndrome (2021) 13(1). doi: 10.1186/s13098-021-00705-9
14. Noh J. Impact of Social Distancing Due to Coronavirus Disease 2019 on the Changes in Glycosylated Hemoglobin Level in People With Type 2 Diabetes Mellitus. Diabetes Metab J (2021) 45(2):275–6. doi: 10.4093/dmj.2020.0226
15. Park SD, Kim SW, Moon JS, Lee YY, Cho NH, Lee JH, et al. Impact of Social Distancing Due to Coronavirus Disease 2019 on the Changes in Glycosylated Hemoglobin Level in People With Type 2 Diabetes Mellitus. Diabetes Metab J (2021) 45(1):109–14. doi: 10.4093/dmj.2020.0226
16. Fontanet A, Cauchemez S. COVID-19 Herd Immunity: Where Are We? Nat Rev Immunol (2020) 20:583–4. doi: 10.1038/s41577-020-00451-5
17. Marani M, Katul GG, Pan WK, Parolari AJ. Intensity and Frequency of Extreme Novel Epidemics. Proc Natl Acad Sci (2021) 118(35). doi: 10.1073/pnas.2105482118
18. Peters MD, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, et al. Updated Methodological Guidance for the Conduct of Scoping Reviews. JBI Evidence Synthesis (2020) 18(10):2119–26. doi: 10.11124/JBIES-20-00167
19. Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-Scr): Checklist and Explanation. Ann Intern Med (2018) 169(7):467–73. doi: 10.7326/M18-0850
20. Munn Z, Peters MD, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic Review or Scoping Review? Guidance for Authors When Choosing Between a Systematic or Scoping Review Approach. BMC Med Res Method (2018) 18(1):1–7. doi: 10.1186/s12874-018-0611-x
21. Önmez A, Gamsızkan Z, Özdemir Ş, Kesikbaş E, Gökosmanoğlu F, Torun S, et al. The Effect of COVID-19 Lockdown on Glycemic Control in Patients With Type 2 Diabetes Mellitus in Turkey. Diabetes Metab Syndr: Clin Res Rev (2020) 14(6):1963–6. doi: 10.1016/j.dsx.2020.10.007
22. Tao J, Gao L, Liu Q, Dong K, Huang J, Peng X, et al. Factors Contributing to Glycemic Control in Diabetes Mellitus Patients Complying With Home Quarantine During the Coronavirus Disease 2019 (COVID-19) Epidemic. Diabetes Res Clin Pract (2020) 170. doi: 10.1016/j.diabres.2020.108514
23. Shimels T, Asrat Kassu R, Bogale G, Bekele M, Getnet M, Getachew A, et al. Magnitude and Associated Factors of Poor Medication Adherence Among Diabetic and Hypertensive Patients Visiting Public Health Facilities in Ethiopia During the COVID-19 Pandemic. PloS One (2021) 16(4). doi: 10.1371/journal.pone.0249222
24. Alessi J, De Oliveira GB, Franco DW, Do Amaral BB, Becker AS, Knijnik CP, et al. Mental Health in the Era of COVID-19: Prevalence of Psychiatric Disorders in a Cohort of Patients With Type 1 and Type 2 Diabetes During the Social Distancing. Diabetol Metab Syndr (2020) 12(1):1–10. doi: 10.1186/s13098-020-00584-6
25. Garner DM, Garfinkel PE. The Eating Attitudes Test: An Index of the Symptoms of Anorexia Nervosa. Psychol Med (1979) 9(2):273–9. doi: 10.1017/S0033291700030762
26. Zomer J, Peled R, Rubin A, Lavie P. Mini-Sleep Questionnaire (MSQ) for Screening Large Populations for EDS Complaints. In: Koella WP, Rüther E, Schulz H, editors. Proceedings of the Seventh European Congress on Sleep - Research, vol. 84. Basel, Switzerland: Karger Publishers (1985). p. 467–70. Sleep.
27. Kaplan Serin E, Bülbüloğlu S. The Effect of Attitude to Death on Self-Management in Patients With Type 2 Diabetes Mellitus During the COVID-19 Pandemic. OMEGA-J Death Dying (2021). doi: 10.1177/00302228211020602
28. Schmitt A, Gahr A, Hermanns N, Kulzer B, Huber J, Haak T. The Diabetes Self-Management Questionnaire (DSMQ): Development and Evaluation of an Instrument to Assess Diabetes Self-Care Activities Associated With Glycaemic Control. Health Qual Life Outcomes (2013) 11(1):1–14. doi: 10.1186/1477-7525-11-138
29. Ware J.R JE, Sherbourne CD. The MOS 36-Item Short-Form Health Survey (SF-36): I. Conceptual Framework and Item Selection. Med Care (1992) 30:473–83.
30. Koçyiğit H, Aydemir Ö, Fişek G, Ölmez N, Memiş AK. Form-36 (KF-36) ’nın Türkçe Versiyonunun Güvenilirliği Ve Geçerliliği. Ilaç ve tedavi dergisi (1999) 12(2):102–6.
31. Morisky DE, Ang A, Krousel‐Wood M, Ward HJ. Predictive Validity of a Medication Adherence Measure in an Outpatient Setting. J Clin Hypertension (2008) 10(5):348–54. doi: 10.1111/j.1751-7176.2008.07572.x
32. Wysocki M, Walędziak M, Proczko-Stepaniak M, Pędziwiatr M, Szeliga J, Major P. Lifestyle Changes in Patients With Morbid Obesity and Type 2 Diabetes Mellitus During the COVID-19 Pandemic. Diabetes Metab J (2020) 73. doi: 10.1016/j.diabet.2020.06.002
33. Cheng HP, Wong JSL, Selveindran NM, Hong JYH. Impact of COVID-19 Lockdown on Glycaemic Gontrol and Lifestyle Changes in Children and Adolescents With Type 1 and Type 2 Diabetes Mellitus. Endocrine (2020). doi: 10.1007/s12020-021-02810-1
34. Rastogi A, Hiteshi P, Bhansali A. Improved Glycemic Control Amongst People With Long-Standing Diabetes During COVID-19 Lockdown: A Prospective, Observational, Nested Cohort Study. Int J Diabetes Develop Cntr (2020) 40(4):476–81. doi: 10.1007/s13410-020-00880-x
35. Rowlands AV, Henson JJ, Coull NA, Edwardson CL, Brady E, Hall A, et al. The Impact of COVID-19 Restrictions on Accelerometer-Assessed Physical Activity and Sleep in Individuals With Type 2 Diabetes. Diabetic Med (2021). doi: 10.1111/dme.14549
36. Sacre JW, Holmes-Truscott E, Salim A, Anstey KJ, Drummond GR, Huxley RR, et al. Impact of the COVID-19 Pandemic and Lockdown Restrictions on Psychosocial and Behavioural Outcomes Among Australian Adults With Type 2 Diabetes: Findings From the PREDICT Cohort Study. Diabetic Med (2021). doi: 10.1111/dme.14611
37. Franco DW, Alessi J, Becker AS, Amaral BBD, Oliveira GBD, Schaan BD, et al. Medical Adherence in the Time of Social Distancing: A Brief Report on the Impact of the COVID-19 Pandemic on Adherence to Treatment in Patients With Diabetes. Arch Endocrinol Metab (2021) 65. doi: 10.20945/2359-3997000000362
38. Hasegawa Y, Takahashi F, Hashimoto Y, Munekawa C, Hosomi Y, Okamura T, et al. Effect of COVID-19 Pandemic on the Change in Skeletal Muscle Mass in Older Patients With Type 2 Diabetes: A Retrospective Cohort Study. Int J Environ Res Public Health (2021) 18(8). doi: 10.3390/ijerph18084188
39. Binhardi BA, de Souza Teixeira CR, de Almeida-Pititto B, Barbosa-Junior F, Franco LJ, de Melo KFS. Diabetes Self-Care Practices and Resilience in the Brazilian COVID-19 Pandemic: Results of a Web Survey: Diabetesvid. Diabetol Metab Syndr (2021) 13(1):1–11. doi: 10.1186/s13098-021-00706-8
40. Alshareef R, Al Zahrani A, Alzahrani A, Ghandoura L. Impact of the COVID-19 Lockdown on Diabetes Patients in Jeddah, Saudi Arabia. Diabetes Metab Syndr: Clin Res Rev (2020) 14(5):1583–7. doi: 10.1016/j.dsx.2020.07.051
41. Crocker PR, Bailey DA, Faulkner RA, Kowalski KC, McGrath R. Measuring General Levels of Physical Activity: Preliminary Evidence for the Physical Activity Questionnaire for Older Children. Med Sci Sports Exercise (1997) 29(10):1344–9. doi: 10.1097/00005768-199710000-00011
42. Kowalski KC, Crocker PR, Donen RM. The Physical Activity Questionnaire for Older Children (PAQ-C) and Adolescents (PAQ-a) Manual. Coll Kinesiol Univ Saskatchewan (2004) 87(1):1–38.
43. Fisher L, Polonsky W, Asuni A, Jolly Y, Hessler D. The Early Impact of the COVID-19 Pandemic on Adults With Type 1 or Type 2 Diabetes: A National Cohort Study. J Diabetes Complications (2020) 34(12). doi: 10.1016/j.jdiacomp.2020.107748
44. Teló GH, de Souza MS, Schaan BDA. Cross-Cultural Adaptation and Validation to Brazilian Portuguese of Two Measuring Adherence Instruments for Patients With Type 1 Diabetes. Diabetol Metab Syndr (2014) 6(1):1–6. doi: 10.1186/1758-5996-6-141
45. Ghosh A, Arora B, Gupta R, Anoop S, Misra A. Effects of Nationwide Lockdown During COVID-19 Epidemic on Lifestyle and Other Medical Issues of Patients With Type 2 Diabetes in North India. Diabetes Metab Syndr: Clin Res Rev (2020) 14(5):917–20. doi: 10.1016/j.dsx.2020.05.044
46. Grabia M, Markiewicz-Żukowska R, Puścion-Jakubik A, Bielecka J, Nowakowski P, Gromkowska-Kępka K, et al. The Nutritional and Health Effects of the COVID-19 Pandemic on Patients With Diabetes Mellitus. Nutrients (2020) 12(10). doi: 10.3390/nu12103013
47. Hansel B, Potier L, Chalopin S, Larger E, Gautier JF, Delestre F, et al. The COVID-19 Lockdown as an Opportunity to Change Lifestyle and Body Weight in People With Overweight/Obesity and Diabetes: Results From the National French COVIDIAB Cohort. Nutrition Metab Cardiovasc Dis (2021) 31. doi: 10.1016/j.numecd.2021.05.031
48. Munekawa C, Hosomi Y, Hashimoto Y, Okamura T, Takahashi F, Kawano R, et al. Effect of Coronavirus Disease 2019 Pandemic on the Lifestyle and Glycemic Control in Patients With Type 2 Diabetes: A Cross-Section and Retrospective Cohort Study. Endocrine J (2020) 68. doi: 10.1507/endocrj.EJ20-0426
49. Anjana RM, Pradeepa R, Das AK, Deepa M, Bhansali A, Joshi SR, et al. Physical Activity and Inactivity Patterns in India: Results From the ICMR-INDIAB Study (Phase-1) [ICMR-INDIAB-5]. Int J Behav Nutr Phys Activity (2014) 11(1):1–11. doi: 10.1186/1479-5868-11-26
50. Cleland CL, Hunter RF, Kee F, Cupples ME, Sallis JF, Tully MA. Validity of the Global Physical Activity Questionnaire (GPAQ) in Assessing Levels and Change in Moderate-Vigorous Physical Activity and Sedentary Behaviour. BMC Public Health (2014) 14(1):1–11. doi: 10.1186/1471-2458-14-1255
51. Regeer H, Nieuwenhuijse EA, Vos RC, Kiefte-de Jong JC, van Empelen P, de Koning EJ, et al. Psychological Factors Associated With Changes in Physical Activity in Dutch People With Type 2 Diabetes Under Societal Lockdown: A Cross-Sectional Study. Endocrinol Diabetes Metab (2021). doi: 10.1002/edm2.249
52. Wendel-Vos GW, Schuit AJ, Saris WH, Kromhout D. Reproducibility and Relative Validity of the Short Questionnaire to Assess Health-Enhancing Physical Activity. J Clin Epidemiol (2003) 56(12):1163–9. doi: 10.1016/S0895-4356(03)00220-8
53. Ruiz-Roso MB, Knott-Torcal C, Matilla-Escalante DC, Garcimartín A, Sampedro-Nuñez MA, Dávalos A, et al. COVID-19 Lockdown and Changes of the Dietary Pattern and Physical Activity Habits in a Cohort of Patients With Type 2 Diabetes Mellitus. Nutrients (2020) 12(8). doi: 10.3390/nu12082327
54. Martin-Moreno JM, Boyle P, Gorgojo L, Maisonneuve P, Fernandez-Rodriguez JC, Salvini S, et al. Development and Validation of a Food Frequency Questionnaire in Spain. Int J Epidemiol (1993) 22(3):512–9. doi: 10.1093/ije/22.3.512
55. Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International Physical Activity Questionnaire: 12-Country\Reliability and Validity. Med Sci Sports Exercise (2003) 35(8):1381–95. doi: 10.1249/01.MSS.0000078924.61453.FB
56. Moreno S, Rodríguez S, Fernandez MC, Tamez J, Cepeda-Benito A. Clinical Validation of the Trait and State Versions of the Food Craving Questionnaire. Assessment (2008) 15(3):375–87. doi: 10.1177/1073191107312651
57. Van Der Ven NC, Weinger K, Yi J, Pouwer F, Adèr H, Van Der Ploeg HM, et al. The Confidence in Diabetes Self-Care Scale: Psychometric Properties of a New Measure of Diabetes-Specific Self-Efficacy in Dutch and US Patients With Type 1 Diabetes. Diabetes Care (2003) 26(3):713–8. doi: 10.2337/diacare.26.3.713
58. Sankar P, Ahmed WN, Koshy VM, Jacob R, Sasidharan S. Effects of COVID-19 Lockdown on Type 2 Diabetes, Lifestyle and Psychosocial Health: A Hospital-Based Cross-Sectional Survey From South India. Diabetes Metab Syndr: Clin Res Rev (2020) 14(6):1815–9. doi: 10.1016/j.dsx.2020.09.005
59. Silva-Tinoco R, GonzÁLez-Cant ÚA, de la Torre-Salda ÑAV, GuzmÁN-Olvera E, Cuatecontzi-Xochitiotzi T, Castillo-Martínez L, et al. Effect in Self-Care Behavior and Difficulties in Coping With Diabetes During the COVID-19 Pandemic. Rev Mexicana Endocrinol Metabol y Nutr (2020) 8. doi: 10.24875/RME.20000063
60. Utli H, Vural Doğru B. The Effect of the COVID-19 Pandemic on Self-Management in Type 2 Diabetics. Primary Care Diabetes (2021) 58. doi: 10.1016/j.pcd.2021.07.009
61. Erener S. Diabetes, Infection Risk and COVID-19. Mol Metab (2020) 39. doi: 10.1016/j.molmet.2020.101044
62. Boniol M, Dragomir M, Autier P, Boyle P. Physical Activity and Change in Fasting Glucose and Hba1c: A Quantitative Meta-Analysis of Randomized Trials. Acta Diabetologica (2017) 54(11):983–91. doi: 10.1007/s00592-017-1037-3
63. Jurblum M, Ng CH, Castle DJ. Psychological Consequences of Social Isolation and Quarantine: Issues Related to COVID-19 Restrictions. Aust J Gen Pract (2020) 49(12):778–83. doi: 10.31128/AJGP-06-20-5481
64. Toschi E, Bailey RJ, Miller KM, Calhoun PM. Improvement in A1c Levels in Early Adulthood in the T1D Exchange: Impact of Racial, Socioeconomic, and Clinical Factors. J Clin Endocrinol Metab (2021) 106(5):1294–302. doi: 10.1210/clinem/dgab077
65. Merzon E, Green I, Shpigelman M, Vinker S, Raz I, Golan-Cohen A, et al. Haemoglobin A1c is a Predictor of COVID-19 Severity in Patients With Diabetes. Diabetes/Metabol Res Rev (2021) 37(5). doi: 10.1002/dmrr.3398
66. Czeisler MÉ, Lane RI, Petrosky E, Wiley JF, Christensen A, Njai R, et al. Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic—United States, June 24–30, 2020. Morbid Mortal Wkly Rep. (2020) 69(32):1049–57. doi: 10.15585/mmwr.mm6932a1
67. Fontana JM, Pan Z, Sazonov ES, McCrory MA, Thomas JG, McGrane KS, et al. Reproducibility of Dietary Intake Measurement From Diet Diaries, Photographic Food Records, and a Novel Sensor Method. Front Nutr (2020) 7:99. doi: 10.3389/fnut.2020.00099
68. Merrill JE, Fan P, Wray TB, Miranda Jr R. Assessment of Alcohol Use and Consequences: Comparison of Data Collected via Timeline Followback Interview and Daily Reports. J Stud Alcohol Drugs (2020) 81(2):212–9. doi: 10.15288/jsad.2020.81.212
69. Topolovec-Vranic J, Natarajan K. The Use of Social Media in Recruitment for Medical Research Studies: A Scoping Review. J Med Internet Res (2016) 18(11). doi: 10.2196/jmir.5698
Keywords: type 2 diabetes, COVID-19, self-management, physical activity, diet, adherence
Citation: Cummings C, Seng K, Tweet R and Wagner J (2022) Lifestyles Under Lockdown: A Scoping Review of International Studies on Type 2 Diabetes Self-Management Behaviors During COVID-19. Front. Clin. Diabetes Healthc. 3:830353. doi: 10.3389/fcdhc.2022.830353
Received: 07 December 2021; Accepted: 27 January 2022;
Published: 15 March 2022.
Edited by:
Emma Berry, Queen’s University Belfast, United KingdomReviewed by:
Sriram Gubbi, National Institute of Diabetes and Digestive and Kidney Diseases (NIH), United StatesCopyright © 2022 Cummings, Seng, Tweet and Wagner. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Julie Wagner, anV3YWduZXJAdWNoYy5lZHU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.