
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Clin. Diabetes Healthc. , 16 March 2022
Sec. Diabetes Clinical Epidemiology
Volume 3 - 2022 | https://doi.org/10.3389/fcdhc.2022.756022
This article is part of the Research Topic Patient-Related Outcomes in Diabetes and Population-Based Registries View all 7 articles
 Ilka Anker1,2
Ilka Anker1,2 Erika Nyman3,4
Erika Nyman3,4 Malin Zimmerman1,2
Malin Zimmerman1,2 Ann-Marie Svensson5,6
Ann-Marie Svensson5,6 Gert S. Andersson7
Gert S. Andersson7 Lars B. Dahlin1,2,3*
Lars B. Dahlin1,2,3*The impact of preoperative electrophysiology on outcome of surgical treatment in ulnar nerve entrapment at the elbow (UNE) is not clarified. Our aim was to evaluate influence of preoperative electrophysiologic grading on outcome and analyse how age, sex, and in particular diabetes affect such grading. Electrophysiologic protocols for 406 UNE cases, surgically treated at two hand surgery units reporting to the Swedish National Quality Register for Hand Surgery (HAKIR; 2010-2016), were retrospectively assessed, and graded as normal, reduced conduction velocity, conduction block or axonal degeneration. Outcome of surgery after primary and revision surgery was evaluated using QuickDASH and a doctor reported outcome measure (DROM) grading. No differences in QuickDASH or DROM were found between the four groups with different electrophysiologic grading preoperatively, or at three and 12 months or at follow up, respectively. When dichotomizing the electrophysiologic grading into normal and pathologic electrophysiology, cases with normal electrophysiology had worse QuickDASH than cases with pathologic electrophysiology preoperatively (p=0.046). Presence of a conduction block or axonal degeneration indicated a worse outcome by DROM grading (p=0.011). Primary surgeries had electrophysiologic more pronounced nerve pathology compared to revision surgeries (p=0.017). Cases of older age, men, and those with diabetes had more severe electrophysiologic nerve affection (p<0.0001). In the linear regression analysis, increasing age (unstandardized B=0.03, 95% CI 0.02-0.04; p<0.0001) and presence of diabetes (unstandardized B=0.60, 95% CI 0.25-0.95; p=0.001) were associated with a higher risk of a worse electrophysiologic classification. Female sex was associated with a better electrophysiologic grading (unstandardized B=-0.51, 95% CI -0.75- -0.27; p<0.0001). We conclude that older age, male sex, and concomitant diabetes are associated with more severe preoperative electrophysiologic nerve affection. Preoperative electrophysiologic grade of ulnar nerve affection may influence surgical outcome.
Ulnar nerve entrapment at the elbow (UNE) is mainly considered to be idiopathic. However, risk factors, such as age, sex, concomitant carpal tunnel syndrome (CTS), heavy manual work and multiple occasions of minor pressure at the retrocondylar groove, may predispose to the condition indicating surgery (1–4), but the factors also risks for UNE relapse requiring surgical revision (5–7). Furthermore, diabetes is a known risk factor for compression neuropathies, including UNE (3, 8–10).
The diagnosis of UNE is often based on patient history, symptoms, and clinical signs, supported by electrophysiologic findings (sensitivity 73-96%) to localize the site and estimating the severity of nerve compression (11–13). In addition, electrophysiologic examination may predict surgical outcome according to some studies (14, 15). However, outcome of primary simple decompression does not seem to differ between cases with solely clinical diagnosis compared to cases with a diagnosis supported by electrophysiology, indicating that clinical symptoms weigh heavily for diagnosis and treatment (14). There is no clear consensus on optimal management of UNE, and the benefit of preoperative electrophysiology for diagnosis, and prognosis of surgery. There is also a debate about the impact of comorbidity, such as diabetes (16).
Outcome of surgical treatment for UNE seems to be similar (17–19) irrespective of surgical method, with respect to improvements in both clinical and electrophysiologic variables, and even regarding severity of UNE (16). Diabetes does not affect patient reported outcome after simple decompression in primary UNE, but men with diabetes have a risk for more residual postoperative symptoms (20). In addition, the relation between preoperative electrophysiologic grading and outcome in UNE patients with diabetes is not known.
There is a need for a clinically applicable preoperative electrophysiologic grading in UNE in order to predict outcome as related to patient characteristics as well as to comorbidities. Our aim was to evaluate the impact of the preoperative electrophysiologic grade of ulnar nerve pathology on outcome of surgery for UNE at the elbow with respect to age, sex, and diabetes.
All surgically treated UNE cases between 2010-2016 [identified by ICD-10 diagnosis code G562 and surgical codes ACC53 (simple decompression), ACC43 (transposition) or NCK19 (medial epicondylectomy)], from two hand surgery departments (Malmö and Linköping) included in the Swedish National Quality Register for Hand Surgery (HAKIR; www.hakir.se) (21), were identified and cases with available preoperative electrophysiologic data were included in the study. Electrophysiologic protocols and medical charts were retrospectively assessed. The Swedish National Diabetes Registry (NDR; www.ndr.nu) for adults was merged with data from HAKIR to obtain data for patients with diabetes. The NDR contains data on type of diabetes treatment, complications, and associated risk factors (20, 22). Each case was defined as a treated nerve. The expression UNE was consistently used in the present study, independently exactly where the ulnar nerve was affected; thus, possibly at the level of the medial epicondyle or by the ligament of Osborne in accordance with previous publications (20, 23). The study was approved by the Regional Ethical Review Boards in Lund, Sweden (No 2016/931 and 2018/57) and Regional Ethics Review Board, Linköping, Sweden (register number 2016/88-31).
Data from HAKIR consisted of age, sex, type of ulnar nerve surgery, other concomitant hand surgical procedures, operated side and date of surgery. Pre- and postoperative disability were in the register assessed using the Swedish version of the patient reported outcome measure (PROM) QuickDASH (shortened version of the DASH; Disability of Arm, Shoulder and Hand questionnaire; total calculated score 0-100, higher score indicating more disability). Outcome was scored at three and 12 months postoperatively, as earlier described (20, 23–25).
Additional clinical data, not registered in HAKIR, was retrospectively sampled from patient charts as previously described (23). Doctor reported outcome measure (DROM) was based on the last out-patient visit (graded by IA; not treating surgeon in any case) and was graded into four groups; cured, improved, unchanged and worsened, and later dichotomized into two groups for statistical analyses (cured/improved and unchanged/worsened).
Electrophysiologic examinations were performed on the ulnar nerves, in most cases bilaterally. The nerves were stimulated at the wrist, below and above elbow and a response was recorded from the abductor digiti minimi muscle. The patients in Lund, Sweden, were also examined with a short segment (2 cm) stimulation across the elbow segment. F-waves and orthodromic sensory response of the ulnar nerve to stimulation of the little finger were also recorded. The results were revised, assessed and graded by one of the authors (GS.A; specialist in neurophysiology; blinded to treatment and outcome) into four groups based on reference values at the Departments of Clinical Neurophysiology in Lund and Linköping, Sweden, respectively, with defined diagnostic criteria for the abnormal groups: i.e. (1) normal findings, (2) reduced conduction velocity across the elbow segment [if upper normal limits are exceeded for a single 2 cm segment (0.9 msec for men and 0.8 msec for women), two segments (1.3 msec men, 1.2 msec women) or all seven segments (3.3 msec men, 3.0 msec women)], (3) nerve conduction block (a 20% amplitude drop over the elbow segment when stimulating above elbow compared with stimulating below elbow), or (4) axonal degeneration [sensory and/or motor amplitudes below normal limit (dependent on age, sex and body height) as earlier described (14, 26). If a nerve showed both reduced conduction velocity and axonal degeneration, it was graded according to its most pathological parameter.
Data are presented as median [interquartile range; IQR; Q25-Q75]. Nominal data are presented as numbers (%). For nominal data, a Chi-squared test (Pearson or Fisher´s exact test) was used to compare differences between groups. Non-parametric Kruskal-Wallis test was used to compare differences between groups for continuous data, with subsequent post-hoc analyses (Mann-Whitney U test). Correlations were assessed by Point-Biserial correlation coefficient for dichotomous variables (r, with p-value). An r-value of ≥0.30 (positive or negative value) was interpreted as a correlation (0.30 – 0.7 = moderate correlation; >0.70 = strong correlation). Linear regression analyses were performed to analyse effects of nominal factors on QuickDASH score (unstandardized B [95% CI]; p-value). A linear regression analysis was performed to investigate the effect of another hand surgical procedure or surgery for another nerve entrapment performed at the same time as UNE surgery on QuickDASH results. All regressions were adjusted for age, sex and diabetes. A p-value <0.05 was considered statistically significant. IBM® SPSS® Statistics, version 26, 2019 (IBM Inc., Chicago, IL) was used for all calculations. Each treated arm was analysed as a separate case and statistical entity.
A larger proportion of the patient cohort has been described earlier (23). Characteristics of the cases grouped by surgical procedure are presented in Table 1. Out of the original population, consisting of 548 UNE surgeries, solely 406/548 (74%) surgeries, on which preoperative electrophysiologic data was available, were included in the present study (Figure 1). Out of the included 406 UNE surgeries, 356/406 (88%) were primary surgeries (81% simple decompression) and 50/406 (12%) were reoperations (86% transpositions). There were no cases surgically treated with a medial epicondylectomy or endoscopic decompression (Table 1).
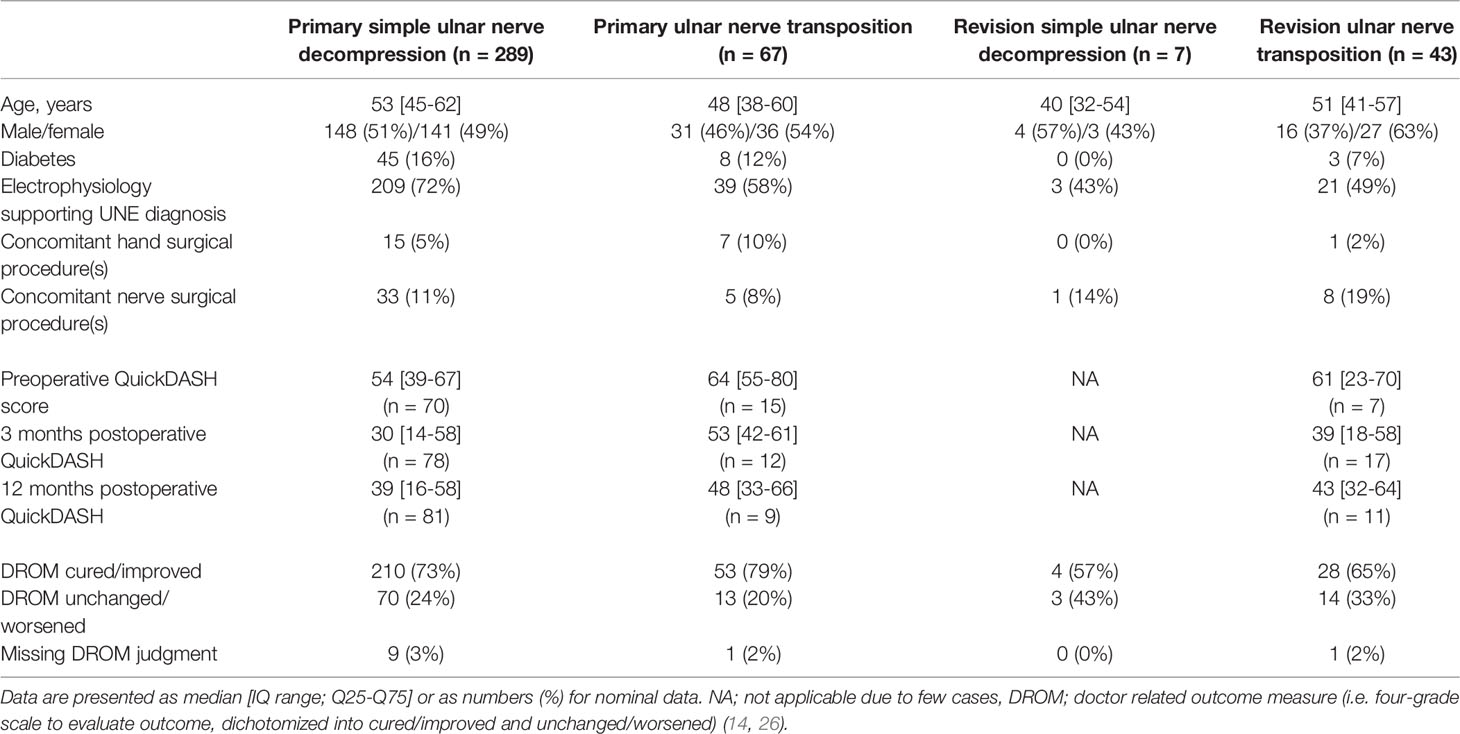
Table 1 Characteristics of 406 surgically treated cases with ulnar nerve entrapment (UNE) grouped by surgical procedure performed at two hand surgery units.
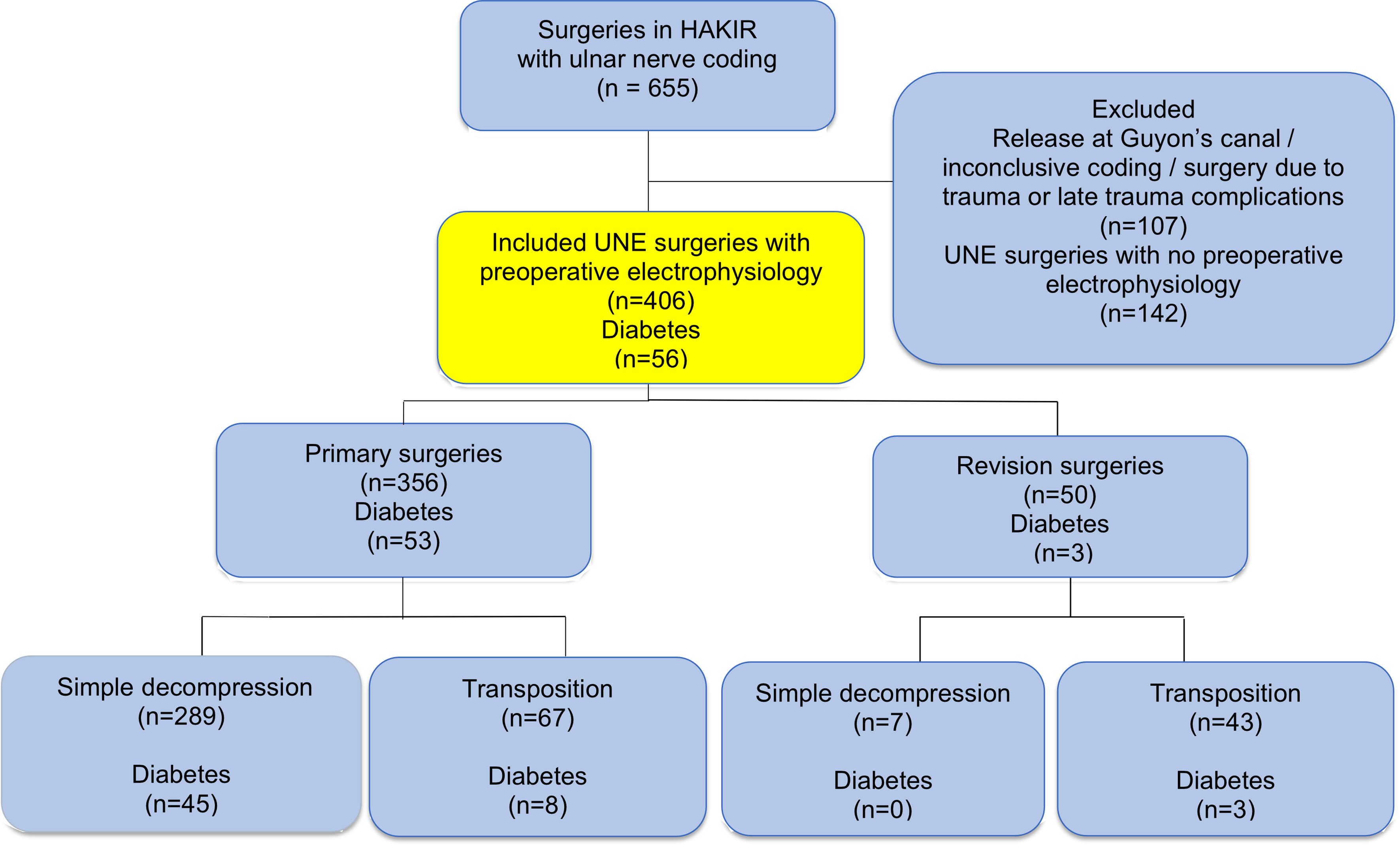
Figure 1 Flow chart describing the inclusion process of surgeries due to ulnar nerve compression from national quality register HAKIR (top blue), where preoperative electrophysiology examination was available of cases with ulnar nerve compression at the elbow (UNE) (yellow). Included cases are indicated and also specified concerning the number of cases with diabetes. For details see text.
Out of all surgically treated cases, 207/406 (51%) were females, with a median age of 50 [interquartile range; IQR 41-59] years for women and 53 [44-62] for men (Table 1). In total, 56/406 (14%) had concomitant diabetes [16/56 (29%) with type 1 and 35/56 (62%) with type 2 diabetes, data missing or unclassified in 5 cases; 9%]. Another hand surgical procedure was performed at the same time as the surgery for UNE in 6% of cases; i.e. surgery for trigger finger, thumb basal osteoarthritis, ganglion, de Quervain’s tenosynovitis or idiopathic synovitis. Another nerve entrapment surgery was performed at the same time as the surgery for UNE in 12%; i.e. carpal tunnel release, decompression of the ulnar nerve at wrist level (Guyon´s canal), decompression of the radial nerve or surgery on multiple nerves. These concomitant hand surgical and nerve related entrapment procedures (adjusted for age, sex, and diabetes) did not affect QuickDASH results at 3 or at 12 months (regression analysis; data not shown).
Among primary surgeries, there were relatively more cases with reduced nerve conduction velocity and axonal degeneration, based on the electrophysiologic grading, than among revision surgeries (p=0.017; Table 2). Electrophysiologic grading preoperatively did not differ when comparing primary simple decompressions with primary ulnar nerve transpositions (p=0.07; results not shown). There were too few cases among revision simple decompression surgeries with electrophysiologic pathology [3/50 (6%)] for adequate statistical analyses to be made on revision surgeries (data not shown).
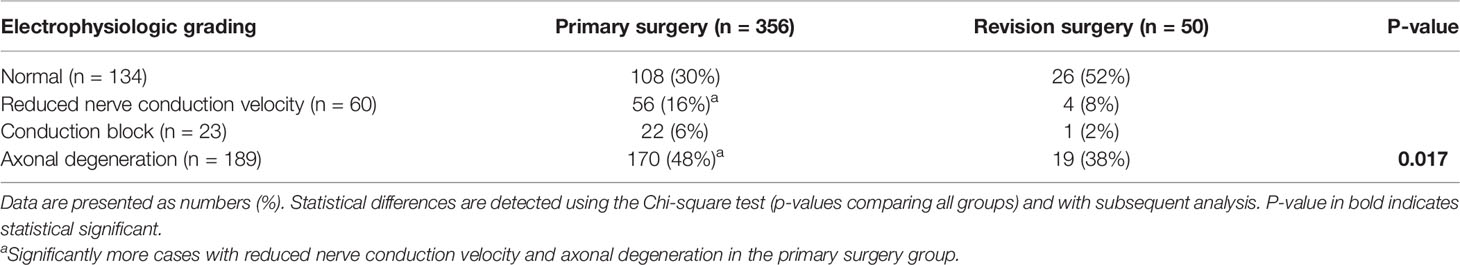
Table 2 Relation between electrophysiologic grading and type of surgery in 406 surgically treated cases with ulnar nerve entrapment.
QuickDASH response rates were 92/406 (23%) preoperatively, 107/406 (27%) at three months postoperatively and 101/406 (25%) at 12 months postoperatively. DROM grading (median follow up time 3.0 months [IQR 1.5-6.0]), was possible to evaluate in 395/406 (97%; missing in 11 cases; 3%) of cases. In the remaining cases, no postoperative outcome was noted in the patient charts.
When analysing all surgically treated UNE cases, no difference in QuickDASH was found neither preoperatively, nor at three or 12 months postoperatively, between the four electrophysiology groups (Table 3). Similar results were found when analysing solely primary UNE surgeries, i.e. no significant differences in QuickDASH score in relation to electrophysiologic grading preoperatively or at three or 12 months postoperatively (p=0.14 preoperatively; p=0.79 at 3 months; p=0.07 at 12 months postoperatively; data not shown). QuickDASH response rates were too low among revision surgeries for statistical analyses to be made.
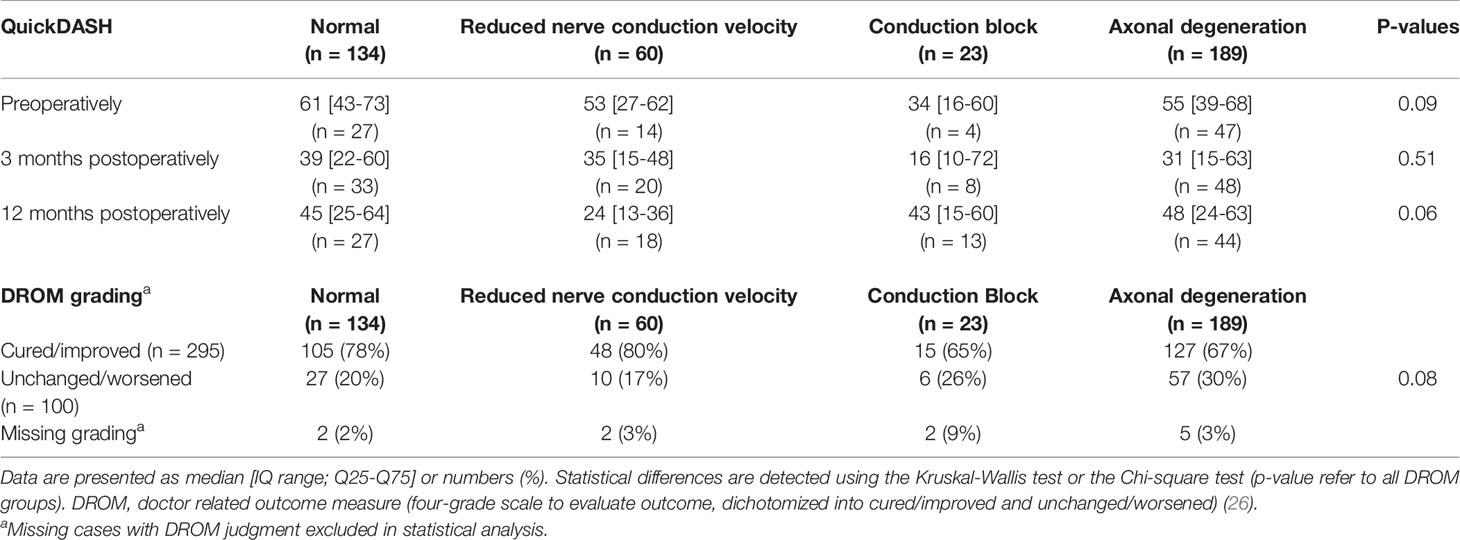
Table 3 Relation between electrophysiologic grading and postoperative outcome using QuickDASH or DROM grading score in 406 and 395, respectively, surgically treated cases with ulnar nerve entrapment, irrespective of surgical method.
When analysing DROM grading in all surgically treated cases (p=0.08; Table 3) and solely primary UNE cases (p=0.07; data not shown), no differences were found in postoperative outcome in relation to the four electrophysiologic grades of nerve affection.
Furthermore, when dichotomizing the electrophysiologic grading into normal [n=132; cured/improved=105 (80%) and unchanged/worsened=27 (20%)] and pathologic [n=263; cured/improved=190 (72%) and unchanged/worsened=73 (28%)] electrophysiology, no difference was observed in the DROM grading (p=0.14; Fisher’s exact test). Using the same dichotomizing procedure, the QuickDASH scores differed preoperatively (normal 61 [43-73], n=27; pathologic 55 [34-64], n=65; p=0.046), but not at three (39 [22-60], n=33; 30 [14-57], n=76; respectively, p=0.16) and 12 months (45 [25-64], n=27; 41 [15-59], n=75, respectively; p=0.31).
When the electrophysiologic grading was divided into two other groups in accordance with a previous method (14), normal and reduced velocity [n=190; cured/improved=153 (81%) and unchanged/worsened=37 (19%)] versus conduction block and axonal degeneration [n=205; cured/improved=142 (69%) and unchanged/worsened=63 (31%)], a significant difference was observed in grading with DROM (p=0.011; Fisher’s exact test). Using the same procedure, the QuickDASH scores did not differ preoperatively (normal/reduced velocity 59 [40-71], n=41; conduction block/axonal degeneration 55 [39-68], n=51; p=0.38), at three (39 [19-58], n=53; 30 [14-63], n=56; respectively, p=0.50) or 12 months (34 [18-55], n=45; 45 [21-62], n=57, respectively; p=0.25).
No moderate or strong correlations were found between neither electrophysiologic grading and pre- or postoperative QuickDASH scores, nor DROM grading.
Cases at older age (regardless of sex and both in all and solely primary UNE) had more severe electrophysiologic findings than cases at younger age (p<0.0001; Table 4). A moderate positive correlation (r=0.38, p<0.0001) was found between age and electrophysiologic grade of nerve affection.
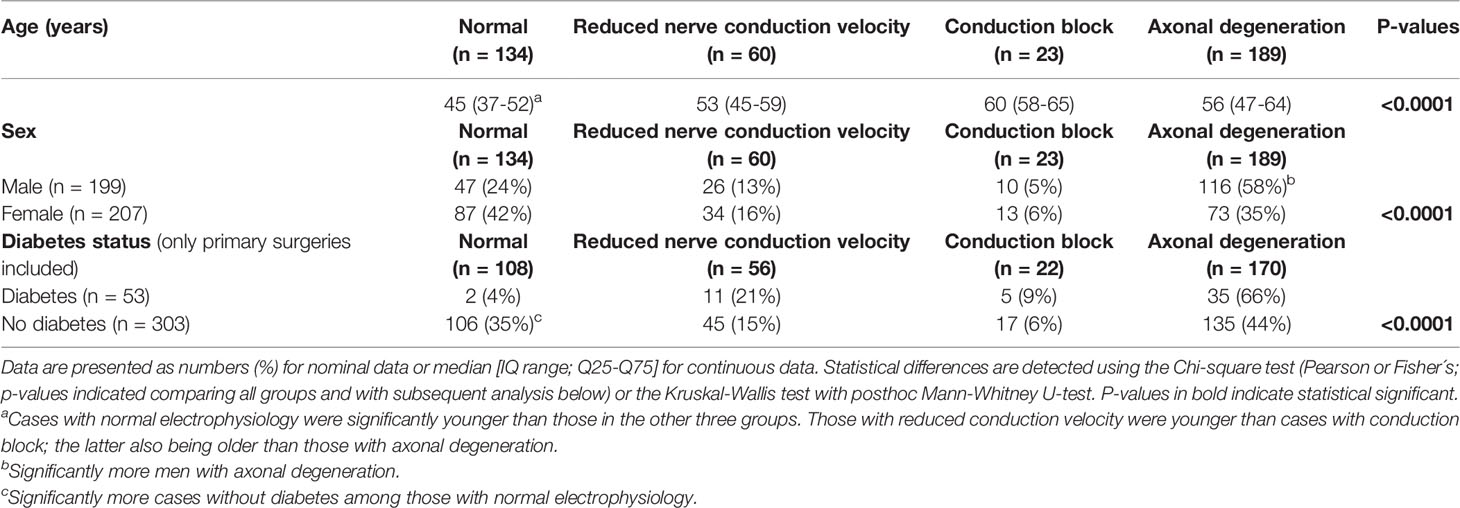
Table 4 Relation between electrophysiologic grading and age of the patients, sex and diabetes (latter only primary cases) in 406 (all) and 356 (primary), respectively, surgically treated cases with ulnar nerve entrapment, irrespective of surgical method.
Men more often had axonal degeneration at the electrophysiologic examination than women (p<0.0001; Table 4). No correlation (moderate or strong) was found between electrophysiologic grading and sex.
Cases with diabetes who had undergone primary surgeries were older (58 [IQR 53-64] years; n=53) compared to cases without diabetes (51 [IQR 42-61]) (p<0.0001; n=303; Mann-Whitney U-test), but with no differences in sex distribution (p=0.13; Fisher´s exact test). In addition, there was no significant difference in sex distribution among all the cases concerning presence of diabetes (males with diabetes 32/199 (16%) and females with diabetes 24/207 (12%); p=0.12; Fisher´s exact test). Most cases with diabetes were found among primary surgeries (53/56; 95%). Among revision surgeries only three cases had concomitant diabetes [3/56 (5%); among revision with ulnar nerve transpositions only; Table 1] and due to the low frequency, further analyses on and including revision surgeries were not performed.
Primary UNE cases with diabetes (only primary cases analysed due to few revision cases among patients with diabetes) had significantly more severe electrophysiologic pathology, in the form of reduced nerve conduction velocity, nerve conduction block and axonal degeneration compared to cases without diabetes (p<0.0001; Table 4), which was also found to be similar for men with diabetes (p=0.012) and women with diabetes (p=0.011; Table 5). No moderate or strong correlations were found between concomitant diabetes and electrophysiologic grade of nerve pathology.
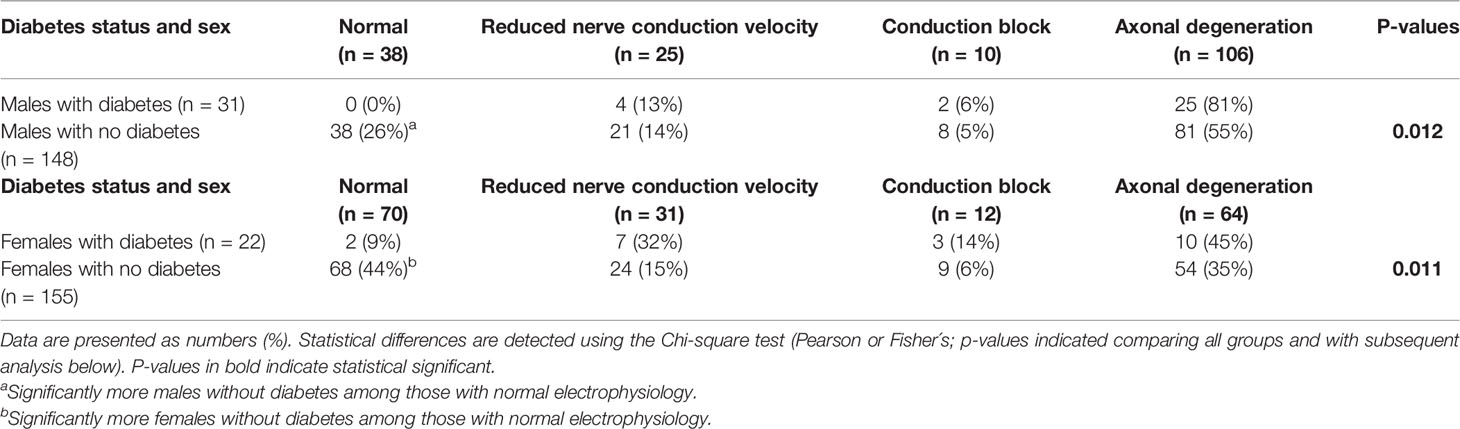
Table 5 Relation between electrophysiologic grading and diabetes among men and women in 356 surgically treated cases with primary ulnar nerve entrapment.
Increasing age (unstandardized B=0.03, 95% CI 0.02-0.04; p<0.0001) and concomitant diabetes (unstandardized B=0.60, 95% CI 0.25-0.95; p=0.001) were associated with a higher risk of a worse electrophysiology classification, while female sex was associated with better grading in the electrophysiology classification (unstandardized B=-0.51, 95% CI -0.75- -0.27; p<0.0001).
In the present study, we found no significant differences in outcome, evaluated with QuickDASH or DROM, in all surgically treated cases or in solely primary cases, neither at three nor at 12 months postoperatively or at follow-up, respectively, when four different grades of electrophysiologic pathology were compared. This is in line with a previous systematic review reporting effectiveness and safety of treatment for UNE referencing few studies with a follow-up longer than 12 months (16). However, in accordance with our previous retrospective study (14), dichotomizing patients with a preoperative nerve conduction block or axonal degeneration against normal findings and reduced conduction velocity, a higher risk of worse postoperative outcome after primary simple decompression was found when outcome was analysed with DROM (14), but not with QuickDASH, even though DROM and QuickDASH has been found to be related (27). No statistical correlation analysis between individual nerve conduction velocities (in m/s) and QuickDASH scores was performed due to the limited number of cases. Electrophysiologic grading is not always considered in larger systematic reviews and meta-analysis when evaluating safety and outcome of surgical procedures for UNE (28). However, it is still a debate if and how the preoperative electrophysiologic grading influence outcome of surgery, which may depend on the methods of evaluation (29, 30).
One cannot exclude that a relation exists between the different severities of electrophysiologic grading and outcome as evaluated by QuickDASH, although significance was not achieved among the four groups, which may be related to statistical power. An explanation of our findings, regarding outcome when QuickDASH was used, may be due to a limited number of cases in each group and being an effect of under-power. When a dichotomizing procedure was performed, dividing electrophysiologic grade into normal and pathologic findings, the former had a slightly higher Quick DASH score preoperatively (around 6 points), but with no differences at three or 12 months, indicating more disability preoperatively for cases with normal electrophysiologic grading. This is clinically a minor difference in disability, meaning that those findings should be interpreted with caution. Nevertheless, the DROM grading indicated that if the patients present with the two worst electrophysiology grades, there is a risk of worse outcome, irrespective of being a nerve conduction block or presence of axonal degeneration. However, a larger population is required to distinguish the outcome of surgery based on the electrophysiology grades nerve conduction block and axonal degeneration. Furthermore, we cannot explain the present observation that there was an initial improvement in QuickDASH at three months and a subsequent worsening at 12 months among the patients with preoperative electrophysiology findings of axonal degeneration. One may speculate that such an affected nerve, due to the lower number of functioning nerve fibres, may be more susceptible to further trauma, such as development of scar tissue around the nerve over time.
In the current study, we found more cases with electrophysiologic more severe nerve pathology among primary surgeries compared to revision surgeries. In primary UNE cases, simple decompression is usually the surgical gold standard treatment, regardless of electrophysiologic severity of nerve affection (16). If an ulnar nerve dislocation is found pre- or perioperatively, an ulnar nerve transposition is commonly performed instead as the primary procedure. Even after a simple decompression a greater mobility of the ulnar nerve can be expected with a risk for dislocation of the ulnar nerve; a statement that is supported by a recent study (23). A significantly higher presence of ulnar nerve dislocation was found among revision surgeries compared to primary surgeries, and at the same time significantly higher presence of ulnar nerve dislocation among primary transposition surgeries was observed compared to primary simple decompressions (23). Hence, we interpret that our current findings might be reflecting a presence of ulnar nerve dislocation among revision surgeries and primary ulnar nerve transpositions, being the reason for these cases presenting an electrophysiological normal or less severe nerve pathology, i.e. due to these unstable ulnar nerves having normal electrophysiologic findings.
Further, we found that men and cases at older age had more severe electrophysiologic impact on nerve function compared to women and cases at younger age. For the latter, we also found a moderate positive correlation, altogether indicating that increasing age may affect electrophysiologic findings negatively and increase severity of nerve pathology. Some earlier studies point out that older age and male sex, among others, are risk factors to develop UNE (1–4). Men in the present study showed a higher proportion of axonal degeneration based on the electrophysiology examination, which also may indicate an increased susceptibility to compression. It has been shown that men have lower intraepidermal nerve fibre density in biopsies from skin at wrist level compared to women (31). This can be interpreted as men having a more sensitive peripheral nervous system, with less reserve nerve fibre capacity, being more prone to be affected by compression, compared to women and might support our findings of men, and particularly those with diabetes, having electrophysiologic more severe impact on nerve function. Data from national registers also support the notion that men with diabetes may not have the same benefit as women with diabetes to improve by a simple decompression (20).
When analysing comorbidity in form of concomitant diabetes, we found that cases with diabetes were significantly older, but there were no differences in sex distribution. Cases with diabetes had more severe electrophysiologic nerve pathology. Diabetes may affect the peripheral nervous system and is a known risk factor for distal sensory polyneuropathy (32) and compression neuropathies, such as carpal tunnel syndrome (33). Several studies have found diabetes to be a risk factor for primary UNE as well (3, 8–10), although it has not consistently been found to increase risk of UNE relapse (5–7). Diabetes affects peripheral nerves by inducing intraneural structural changes (34). We interpret our findings, of cases with diabetes having more severe electrophysiologic nerve affection, as a reflection of this known peripheral nerve affection due to the mentioned structural changes in the nerves.
The interpretation of our combined results, with male sex and diabetes as comorbidity being related to electrophysiological more severe nerve affection, might be explained by men having a more sensitive peripheral nervous system with less reserve capacity when it comes to nerve fibre quantity (31) and the fact that men, as reported, seem to be affected by diabetic neuropathy to a greater extent and earlier compared to women (35, 36).
The low response rate in QuickDASH scores is a limitation even if similar rates have been reported in earlier studies. The HAKIR register was at the time of data collection (2010-2016) also a rather new register with initial problems to include patients. Due to the coding system in HAKIR, we did not have data on which type of transposition that was performed and data on whether surgery was primary or revision was not appropriately specified in HAKIR. Hence, the latter data was added after the thorough retrospective evaluation made on each unique patient chart. A further weakness is that we could not in detail, based on the information from the patient charts, define the exact level of ulnar nerve affection; thus, being at or just proximal to the medial epicondyle or distally, exactly at the ligament of Osborne (37), although the latter location was probably the most common site. However, we defined the presently used expression UNE as a single entity, including both locations, in accordance with previous publications (20, 23). A strength is the use of data from the two national quality registers (HAKIR and NDR), combined with data from each unique patient chart together with a validated outcome measure (QuickDASH), which enables analyses of outcome concerning a nationwide population.
We conclude that older age, male sex, and diabetes are associated with more severe preoperative electrophysiologic nerve affection, which may be interpreted as more susceptible peripheral nerves in men and in diabetes that should be taken into account when surgically treating UNE patients. Preoperative electrophysiologic assessment and severe grade of ulnar nerve affection may influence surgical outcome.
The datasets generated and/or analysed during the current study are not publicly available. Public access to data is restricted by the Swedish Authorities (Public Access to Information and Secrecy Act; https://www.government.se/information-material/2009/09/public-access-to-information-and-secrecy-act/), but data can be available for researchers after a special review that includes approval of the research project by both an Ethics Committee at the national level (etikprövningsmyndigheten.se) and the authorities’ data safety committees (such as “KVB-decision”).
The study was approved by the Regional Ethical Review Boards in Lund, Sweden (No 2016/931 and 2018/57) and Regional Ethics Review Board, Linköping, Sweden (register number 2016/88-31). The patients/participants provided their written informed consent to participate in HAKIR and NDR.
IA, EN, MZ, and LD generated the hypothesis and outline of the project. All authors interpreted the data and critically reviewed the report. IA and EN collected the data from electrophysiologic examinations and patients’ charts. GA analysed and interpreted the electrophysiologic data. A-MS was responsible for collecting the data from the diabetes register. IA performed the initial analyses and drafted the first manuscript. LD performed the final statistical analyses. A-MS and GA contributed to hypothesis generation and to writing the manuscript. All authors fulfilled the criteria for authorship. All authors contributed to the article and approved the submitted version.
This study was supported by grants from the Lund University, ALF [grant number 2018-Project 0104], Region Skåne (Funds from Skåne University Hospital Malmö-Lund), the Swedish Diabetes Foundation [grant number DIA2016-117 and DIA2020-492], the Swedish Research Council [grant number 2021-01942], Sydvästra Skånes Diabetesförening, Sweden, and ALF Grants [grant number LIO-823361], Region Östergötland, Sweden.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The authors thank the national quality registries HAKIR and NDR as well as the contributing nurses, physicians, and patients. We regret that one of the authors, A-MS, passed away just after the project was finalized – we will miss her in our future research.
1. Osei DA, Groves AP, Bommarito K, Ray WZ. Cubital Tunnel Syndrome: Incidence and Demographics in a National Administrative Database. Neurosurgery (2017) 80:417–20. doi: 10.1093/neuros/nyw061
2. Omejec G, Podnar S. What Causes Ulnar Neuropathy at the Elbow? Clin Neurophysiol (2016) 127:919–24. doi: 10.1016/j.clinph.2015.05.027
3. Bartels RH, Verbeek AL. Risk Factors for Ulnar Nerve Compression at the Elbow: A Case Control Study. Acta Neurochir (Wien) (2007) 149:669–74; discussion 74. doi: 10.1007/s00701-007-1166-5
4. Descatha A, Leclerc A, Chastang JF, Roquelaure Y, Study Group on Repetitive W. Incidence of Ulnar Nerve Entrapment at the Elbow in Repetitive Work. Scand J Work Environ Health (2004) 30:234–40. doi: 10.5271/sjweh.784
5. Camp CL, Ryan CB, Degen RM, Dines JS, Altchek DW, Werner BC. Risk Factors for Revision Surgery Following Isolated Ulnar Nerve Release at the Cubital Tunnel: A Study of 25,977 Cases. J Shoulder Elbow Surg (2017) 26:710–5. doi: 10.1016/j.jse.2016.10.028
6. Krogue JD, Aleem AW, Osei DA, Goldfarb CA, Calfee RP. Predictors of Surgical Revision After in Situ Decompression of the Ulnar Nerve. J Shoulder Elbow Surg (2015) 24:634–9. doi: 10.1016/j.jse.2014.12.015
7. Gaspar MP, Kane PM, Putthiwara D, Jacoby SM, Osterman AL. Predicting Revision Following In Situ Ulnar Nerve Decompression for Patients With Idiopathic Cubital Tunnel Syndrome. J Handb Surg Am (2016) 41:427–35. doi: 10.1016/j.jhsa.2015.12.012
8. Mondelli M, Aretini A, Rossi S. Ulnar Neuropathy at the Elbow in Diabetes. Am J Phys Med Rehabil (2009) 88:278–85. doi: 10.1097/PHM.0b013e318190b89d
9. Rota E, Zavaroni D, Parietti L, Iafelice I, De Mitri P, Terlizzi E, et al. Ulnar Entrapment Neuropathy in Patients With Type 2 Diabetes Mellitus: An Electrodiagnostic Study. Diabetes Res Clin Pract (2014) 104:73–8. doi: 10.1016/j.diabres.2014.01.024
10. Rydberg M, Zimmerman M, Gottsater A, Nilsson PM, Melander O, Dahlin LB. Diabetes Mellitus as a Risk Factor for Compression Neuropathy: A Longitudinal Cohort Study From Southern Sweden. BMJ Open Diabetes Res Care (2020) 8:e001298. doi: 10.1136/bmjdrc-2020-001298
11. Visser LH, Beekman R, Franssen H. Short-Segment Nerve Conduction Studies in Ulnar Neuropathy at the Elbow. Muscle Nerve (2005) 31:331–8. doi: 10.1002/mus.20248
12. Todnem K, Michler RP, Wader TE, Engstrom M, Sand T. The Impact of Extended Electrodiagnostic Studies in Ulnar Neuropathy at the Elbow. BMC Neurol (2009) 9:52. doi: 10.1186/1471-2377-9-52
13. Pelosi L, Mulroy E. Diagnostic Sensitivity of Electrophysiology and Ultrasonography in Ulnar Neuropathies of Different Severity. Clin Neurophysiol (2019) 130:297–302. doi: 10.1016/j.clinph.2018.11.018
14. Anker I, Zimmerman M, Andersson GS, Jacobsson H, Dahlin LB. Outcome and Predictors in Simple Decompression of Ulnar Nerve Entrapment at the Elbow. Hand Microsurg (2018) 7:24–32. doi: 10.5455/handmicrosurg.266188
15. Osterman AL, Davis CA. Subcutaneous Transposition of the Ulnar Nerve for Treatment of Cubital Tunnel Syndrome. Handb Clin (1996) 12:421–33.
16. Caliandro P, La Torre G, Padua R, Giannini F, Padua L. Treatment for Ulnar Neuropathy at the Elbow. Cochrane Database Syst Rev (2016) 11:CD006839. doi: 10.1002/14651858.CD006839
17. Liu CH, Wu SQ, Ke XB, Wang HL, Chen CX, Lai ZL, et al. Subcutaneous Versus Submuscular Anterior Transposition of the Ulnar Nerve for Cubital Tunnel Syndrome: A Systematic Review and Meta-Analysis of Randomized Controlled Trials and Observational Studies. Med (Baltimore) (2015) 94:e1207. doi: 10.1097/MD.0000000000001207
18. Biggs M, Curtis JA. Randomized, Prospective Study Comparing Ulnar Neurolysis in Situ With Submuscular Transposition. Neurosurgery (2006) 58:296–304; discussion 296-304. doi: 10.1227/01.NEU.0000194847.04143.A1
19. Gervasio O, Gambardella G, Zaccone C, Branca D. Simple Decompression Versus Anterior Submuscular Transposition of the Ulnar Nerve in Severe Cubital Tunnel Syndrome: A Prospective Randomized Study. Neurosurgery (2005) 56:108–17; discussion 17. doi: 10.1227/01.NEU.0000145854.38234.81
20. Zimmerman M, Anker I, Karlsson A, Arner M, Svensson AM, Eeg-Olofsson K, et al. Ulnar Nerve Entrapment in Diabetes: Patient-Reported Outcome After Surgery in National Quality Registries. Plast Reconstr Surg Glob Open (2020) 8:e2740. doi: 10.1097/GOX.0000000000002740
21. Arner M. Developing a National Quality Registry for Hand Surgery: Challenges and Opportunities. EFORT Open Rev (2016) 1:100–6. doi: 10.1302/2058-5241.1.000045
22. Lind M, Bounias I, Olsson M, Gudbjornsdottir S, Svensson AM, Rosengren A. Glycaemic Control and Incidence of Heart Failure in 20,985 Patients With Type 1 Diabetes: An Observational Study. Lancet (2011) 378:140–6. doi: 10.1016/S0140-6736(11)60471-6
23. Anker I, Zimmerman M, Nyman E, Dahlin LB. Ulnar Nerve Dislocation in Ulnar Nerve Entrapment at the Elbow. Influence on Surgical Outcome. Hand Surg Rehabil (2022) 41(1):96–102 doi: 10.1016/j.hansur.2021.09.003
24. The Swedish Translated Version of QuickDASH. Available at: http://www.dash.iwo.on.ca/assets/images/pdfs/OuickDASH_Swedish.pdf.
25. Zimmerman M, Eeg-Olofsson KMDP, Svensson Am Rn P, Astrom M, Arner M, Dahlin L. Open Carpal Tunnel Release and Diabetes: A Retrospective Study Using PROMs and National Quality Registries. BMJ Open (2019) 9:e030179. doi: 10.1136/bmjopen-2019-030179
26. Anker I, Andersson G, Zimmerman M, Jacobsson H, Dahlin LB. Subcutaneous and Submuscular Transposition Due to Ulnar Nerve Entrapment at the Elbow – Analyses of 43 Primary and 44 Revision Cases. Hand Microsurg (2019) 8:9–18. doi: 10.5455/handmicrosurg.299222
27. Dahlin E, Dahlin E, Andersson GS, Thomsen NO, Bjorkman A, Dahlin LB. Outcome of Simple Decompression of the Compressed Ulnar Nerve at the Elbow - Influence of Smoking, Gender, and Electrophysiological Findings. J Plast Surg Handb Surg (2017) 51:149–55. doi: 10.1080/2000656X.2016.1210520
28. Wade RG, Griffiths TT, Flather R, Burr NE, Teo M, Bourke G. Safety and Outcomes of Different Surgical Techniques for Cubital Tunnel Decompression: A Systematic Review and Network Meta-Analysis. JAMA Netw Open (2020) 3:e2024352. doi: 10.1001/jamanetworkopen.2020.24352
29. Beekman R, Wokke JH, Schoemaker MC, Lee ML, Visser LH. Ulnar Neuropathy at the Elbow: Follow-Up and Prognostic Factors Determining Outcome. Neurology (2004) 63:1675–80. doi: 10.1212/01.WNL.0000142535.24626.90
30. Shi Q, MacDermid J, Grewal R, King GJ, Faber K, Miller TA. Predictors of Functional Outcome Change 18 Months After Anterior Ulnar Nerve Transposition. Arch Phys Med Rehabil (2012) 93:307–12. doi: 10.1016/j.apmr.2011.08.040
31. Thomsen NO, Englund E, Thrainsdottir S, Rosen I, Dahlin LB. Intraepidermal Nerve Fibre Density at Wrist Level in Diabetic and Non-Diabetic Patients. Diabetes Med (2009) 26:1120–6. doi: 10.1111/j.1464-5491.2009.02823.x
32. Barrell K, Smith AG. Peripheral Neuropathy. Med Clin North Am (2019) 103:383–97. doi: 10.1016/j.mcna.2018.10.006
33. Tseng CH, Liao CC, Kuo CM, Sung FC, Hsieh DP, Tsai CH. Medical and Non-Medical Correlates of Carpal Tunnel Syndrome in a Taiwan Cohort of One Million. Eur J Neurol (2012) 19:91–7. doi: 10.1111/j.1468-1331.2011.03440.x
34. Dahlin LB, Rix KR, Dahl VA, Dahl AB, Jensen JN, Cloetens P, et al. Three-Dimensional Architecture of Human Diabetic Peripheral Nerves Revealed by X-Ray Phase Contrast Holographic Nanotomography. Sci Rep (2020) 10:7592. doi: 10.1038/s41598-020-64430-5
35. Aaberg ML, Burch DM, Hud ZR, Zacharias MP. Gender Differences in the Onset of Diabetic Neuropathy. J Diabetes Complications (2008) 22:83–7. doi: 10.1016/j.jdiacomp.2007.06.009
36. Ennis SL, Galea MP, O’Neal DN, Dodson MJ. Peripheral Neuropathy in the Hands of People With Diabetes Mellitus. Diabetes Res Clin Pract (2016) 119:23–31. doi: 10.1016/j.diabres.2016.06.010
Keywords: diabetes, ulnar nerve, neuropathy, surgery outcome, axonal degeneration, QuickDASH
Citation: Anker I, Nyman E, Zimmerman M, Svensson A-M, Andersson GS and Dahlin LB (2022) Preoperative Electrophysiology in Patients With Ulnar Nerve Entrapment at the Elbow-Prediction of Surgical Outcome and Influence of Age, Sex and Diabetes. Front. Clin. Diabetes Healthc. 3:756022. doi: 10.3389/fcdhc.2022.756022
Received: 09 August 2021; Accepted: 04 February 2022;
Published: 16 March 2022.
Edited by:
Tamara Poljicanin, Croatian Institute of Public Health, CroatiaReviewed by:
Simon Podnar, University Medical Centre Ljubljana, SloveniaCopyright © 2022 Anker, Nyman, Zimmerman, Svensson, Andersson and Dahlin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lars B. Dahlin, bGFycy5kYWhsaW5AbWVkLmx1LnNl
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.