- 1Department of Health Outcomes Research and Policy, Harrison College of Pharmacy, Auburn University, Auburn, AL, United States
- 2Department of Medical Research, China Medical University Hospital, Taichung, Taiwan
Introduction: Evidence is needed for 30-day readmission risk factors (clinical factors and social needs) among patients with diabetes in the Deep South. To address this need, our objectives were to identify risk factors associated with 30-day readmissions among this population and determine the added predictive value of considering social needs.
Methods: This retrospective cohort study utilized electronic health records from an urban health system in the Southeastern U.S. The unit of analysis was index hospitalization with a 30-day washout period. The index hospitalizations were preceded by a 6-month pre-index period to capture risk factors (including social needs), and hospitalizations were followed 30 days post-discharge to evaluate all-cause readmissions (1=readmission; 0=no readmission). We performed unadjusted (chi-square and student’s t-test, where applicable) and adjusted analyses (multiple logistic regression) to predict 30-day readmissions.
Results: A total of 26,332 adults were retained in the study population. Eligible patients contributed a total of 42,126 index hospitalizations, and the readmission rate was 15.21%. Risk factors associated with 30-day readmissions included demographics (e.g., age, race/ethnicity, insurance), characteristics of hospitalizations (e.g., admission type, discharge status, length of stay), labs and vitals (e.g., highest and lowest blood glucose measurements, systolic and diastolic blood pressure), co-existing chronic conditions, and preadmission antihyperglycemic medication use. In univariate analyses of social needs, activities of daily living (p<0.001), alcohol use (p<0.001), substance use (p=0.002), smoking/tobacco use (p<0.001), employment status (p<0.001), housing stability (p<0.001), and social support (p=0.043) were significantly associated with readmission status. In the sensitivity analysis, former alcohol use was significantly associated with higher odds of readmission compared to no alcohol use [aOR (95% CI): 1.121 (1.008-1.247)].
Conclusions: Clinical assessment of readmission risk in the Deep South should consider patients’ demographics, characteristics of hospitalizations, labs, vitals, co-existing chronic conditions, preadmission antihyperglycemic medication use, and social need (i.e., former alcohol use). Factors associated with readmission risk can help pharmacists and other healthcare providers identify high-risk patient groups for all-cause 30-day readmissions during transitions of care. Further research is needed about the influence of social needs on readmissions among populations with diabetes to understand the potential clinical utility of incorporating social needs into clinical services.
Introduction
According to the International Diabetes Federation as of 2021, diabetes affects 536.6 million people across the world (1). Diabetes is most prevalent in high-income countries (HIC) at 11.1% compared to middle-income (10.8%) and low-income (5.5%) countries (1). Problematic increases in the prevalence of diabetes are expected across the world in the coming decades, and predictions reveal that low- and middle-income countries (LMIC) will account for 94% of the increased prevalence by 2045 (1). The World Health Organization’s Global Report on Diabetes highlights the burden of diabetes due to complications, such as vision impairment, kidney problems, cardiovascular disease, and lower extremity amputations (2). Additional burdens resulting from complications of diabetes or other co-existing chronic conditions might include hospitalizations and subsequent readmissions, which are the focus of this report.
Populations with diabetes are at risk of experiencing burdensome hospitalizations. Diabetes and related complications have been estimated to be the fifth leading reason for hospital admissions in the U. S. (3). The process of patients receiving hospital care, being discharged from hospital care, and returning to home care is known as a ‘transition of care’ (4). Transitions of care have been referred to as “vulnerable exchange points that contribute to unnecessarily high rates of health services use and health care spending” that “expose chronically ill people to lapses in quality and safety” (4). This point is particularly true for populations with diabetes, who are highly susceptible to readmissions within the next 30 days after hospital discharge (5, 6). This 30-day period is a commonly used target indicator for risk standardization by the Centers for Medicare and Medicaid Services (CMS) (7). Patients with diabetes face significantly higher all-cause 30-day readmission rates than those without diabetes (24.3% versus 17.7%, respectively) (8) and longer hospital stays (9). These frequent and longer duration hospitalizations constitute a sizeable economic burden globally for patients with diabetes (2). Reducing 30-day readmission rates is essential to decreasing medical expenditures (10). Overall, readmissions among populations with diabetes are an important public health issue in diabetes care.
In efforts to inform evidence for reducing readmissions, prior research studied risk factors associated with readmissions for patients with diabetes, but evidence gaps remain. In 2020, a systematic review and meta-analysis pooled findings across 18 studies to estimate the influence of risk factors for 30-day readmissions among populations with diabetes (11). The risk was higher based on male gender, older age, non-White race, Medicare and Medicaid insurance coverage, the presence of comorbidities, longer length of stay, and use of insulin (11). In accordance with findings from this systematic review, literature on risk factors has focused mainly on patient demographics and clinical data elements from electronic health records (EHRs) to predict readmissions for populations with diabetes (9, 11–16). Also, the EHRs used in these investigations mostly covered populations in the Northeast region of the U.S., so the generalizability to people living in the Deep South is questionable. Additionally, looking outside the scope of demographics and healthcare alone is needed given the recognized impact of non-healthcare factors, like social determinants of health and behaviors, on diabetes care, management, and outcomes (17).
Social and behavioral factors are now widely recognized to influence health outcomes. It is essential to consider these factors (which we will refer to as ‘social needs’) during the investigation of readmissions when these patient-reported measures are captured through data integration in EHRs (18). CMS defines social needs as “individual-level, adverse social conditions that can negatively impact a person’s health or health care” (19). Social needs, such as homelessness, substance use, and challenges affording basic needs (e.g., food, clothing, utilities) or healthcare, have been linked with preventable 30-day readmissions (20). Further, a recent national investigation revealed an increased risk of readmission with a higher number of unmet social needs; the readmission rate more than doubled between having no social needs (11.5%) versus one social need (27.0%) (21). These prior investigations of social needs were among the general adult population (19–21), so the impact of social needs on readmission for people with diabetes remains unclear.
Patients with diabetes living in the Deep South have not been a population of focus for the literature studying readmission risk or transitions of care, despite the disproportionately higher diabetes prevalence in this area (22). Thus, our study seeks to expand and generalize prior research on readmission risk factors for patients with diabetes to the Deep South. The novelty of our approach includes expanding the risk factors considered to include social needs, along with differentiation of readmission status by diabetes type (type 1 versus type 2 diabetes). Our objectives were to identify risk factors associated with all-cause 30-day readmissions among patients with diabetes in the Deep South and determine whether social needs added value in predicting all-cause 30-day readmissions. Findings of risk factors associated with readmissions will apply to the unique needs of patients with diabetes in the Deep South. Our definition of the Deep South includes states such as Alabama, Georgia, Louisiana, Mississippi, South Carolina, and Tennessee (23, 24), and findings will be represented by a population of patients with diabetes in Alabama.
Materials and methods
Study design and data source
This retrospective cohort study used EHRs from an urban health system in the Southeastern U.S. from January 1, 2016 through October 1, 2020. Data from the EHRs were generated through routine clinical practice, and the data were not collected for research purposes. The EHRs were de-identified and extracted to be used for secondary research in this study. Because the pre-existing, de-identified EHRs were used, this research did not involve any interaction with patients. The study protocol was reviewed and approved by the Auburn University Institutional Review Board for the Protection of Human Subjects in Research (IRB) under the exempt review application process.
Study population
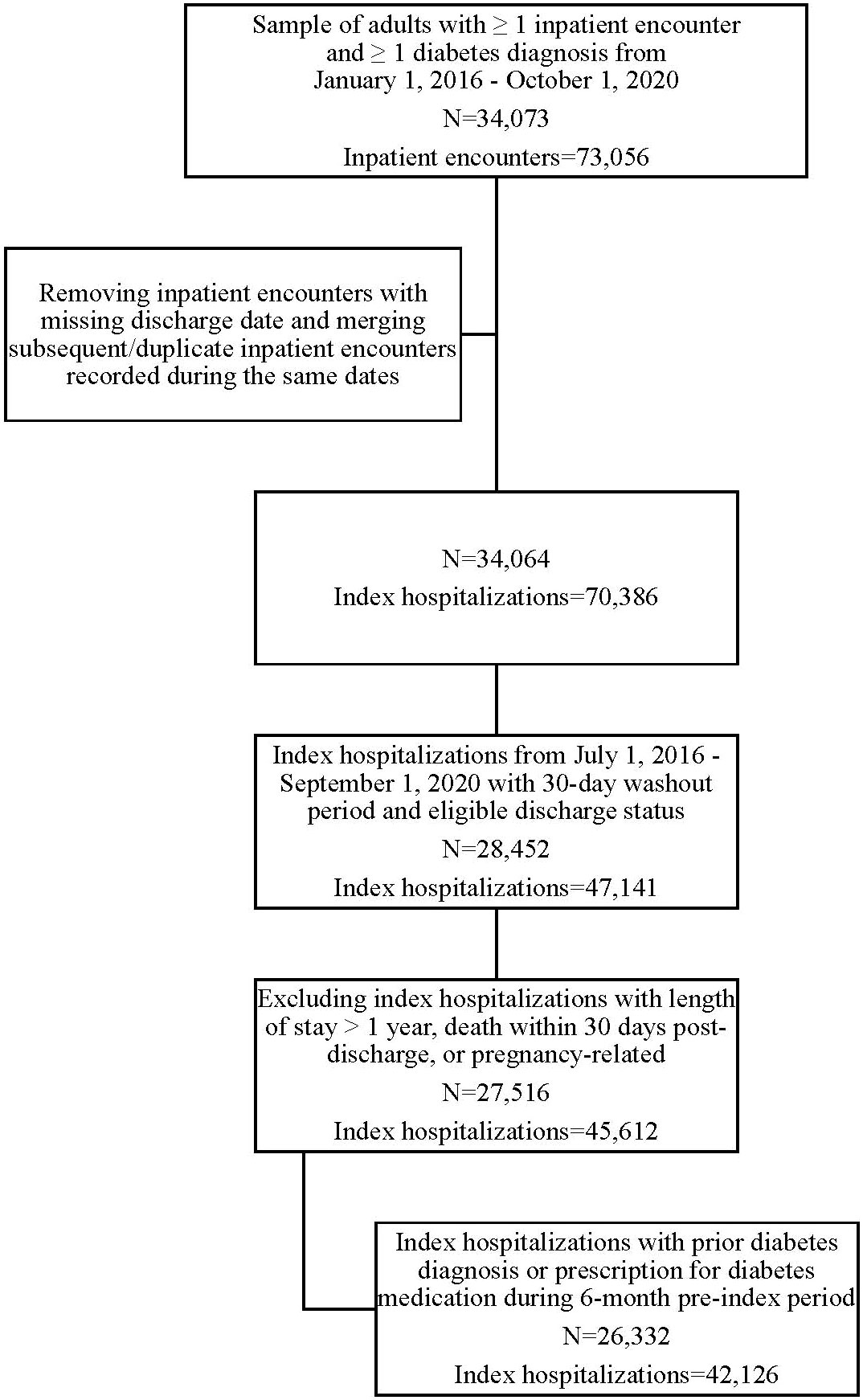
Patients eligible for inclusion were adults (≥18 years old at the time of hospital admission) diagnosed with diabetes (type 1 or type 2) before an inpatient hospitalization. Diagnosis of diabetes was identified through at least one diabetes diagnosis code before the index hospitalization (ICD-9-CM or ICD-10-CM from the Chronic Conditions Warehouse (25) or SNOMED code). People without a diabetes diagnosis were included and assumed to have diabetes if a prescription for diabetes medication was ordered during the 6-month period before hospitalization (13, 15). Patients with diagnosis codes for gestational diabetes were excluded. The cohort flow diagram (Figure 1) depicts how the original sample of adults with diabetes and ≥ one inpatient encounter was selected from the EHRs. From this original sample, we made further restrictions to identify eligible index hospitalizations following the eligibility criteria outlined in Outcomes section below. When identifying the eligible study population, we did not consider patients’ socioeconomic status within the sampling strategy because data for socioeconomics were not available in the EHRs.
Outcomes
The primary outcome was all-cause 30-day readmission, which was operationalized dichotomously as 1=readmission versus 0=no readmission. We focused on all-cause 30-day readmissions, as opposed to diabetes-related readmissions, to reflect the overall healthcare experiences during readmissions for patients with diabetes. We used index hospitalization as the unit of analysis so that each person could have multiple index hospitalizations. We followed each index hospitalization for 30 days after discharge to evaluate readmission status. Subsequent hospitalizations that were recorded during the same or overlapping time periods (e.g., the same discharge date) were counted as the same hospitalization to avoid duplicate counting of hospitalizations (13, 26).
We required that index hospitalizations be preceded by a 6-month pre-index period to capture baseline risk factors (12). We also required that index hospitalizations have a 30-day washout period (with no documented inpatient hospitalization) before the admission date to ensure the hospitalization was an initial admission and not a readmission itself (12). We excluded index hospitalizations that were pregnancy-related [following prior literature of pregnancy-related diagnosis codes (27)] or had a length of stay longer than one year (26). We also excluded hospitalizations with missing discharge dates or hospitalizations discharged to hospital transfer or unknown/missing discharge status (13, 15). Hospitalizations discharged to hospice were also excluded to remove patients receiving ‘end-of-life care’ due to the variability of readmissions after discharge to hospice (28). Lastly, we excluded hospitalizations with documented death during hospitalization (13, 15) or death within 30 days post-discharge (when readmission did not precede the death date).
Risk factors
The selection and inclusion of specific risk factors were driven by prior literature that identified associations with 30-day readmissions among patients with diabetes. The research conducted previously indicates that various factors may impact readmission risk in diabetes, such as demographics, labs, medication use, healthcare utilization, other chronic conditions, etc. (9, 11–15, 26). We incorporated findings of readmission risk factors from the foundational works of Rubin et al. through validation of the Diabetes Early Readmission Risk Indicator (DERRI™) (14, 15) and Karunakaran et al. through expansion of the DERRI™ to include additional pre- and post-discharge risk factors (13). However, we were limited to including risk factors available through data elements in the EHRs. Details about the measurement of all risk factors can be found in the Supplemental Table (see Supplementary Material).
Prior literature guided our operationalization of risk factors (9, 11–15, 26). We differentiated between type 1 and type 2 diabetes based on diagnosis codes any time before the index hospitalization. Diabetes type was coded as unknown when no diagnosis code was present, but a prescription for a diabetes medication was filled during the 6-month pre-index period. Preadmission prescriptions for diabetes medications were classified into the following medication classes: insulin, metformin, sulfonylureas, thiazolidinediones (TZD), dipeptidyl peptidase 4 (DPP-4) inhibitors, sodium-glucose cotransporter-2 (SGLT2) inhibitors, glucagon-like peptide-1 (GLP-1) receptor agonists, and others (meglitinides, α-glucosidase inhibitors, amylin analog, cycloset, bile acid sequestrants). Prior research found extreme blood glucose measures [i.e., high (>180 mg/dL) and low (<70 mg/dL)] to be associated with readmissions (13), so we retained the highest and lowest blood glucose value during the index hospitalization to represent proxy variables for hyperglycemia and hypoglycemia, respectively. For labs (HbA1c, albumin, creatinine, hematocrit, white blood cell count, potassium, sodium), body mass index (BMI), and blood pressure, we retained the record nearest to the index hospitalization admission date (15). HbA1c was capped at 3.5% and 18.5% in the EHRs. Implausible values for other labs and blood pressure were excluded following cut-offs recommended by Estiri et al. (29), except for creatinine [<0.1 mg/dL or >15 mg/dL was used (30)] and hematocrit (observations outside of six standard deviations were removed as an alternative approach used by Estiri). We also excluded implausible values for BMI [<10 kg/m2 or >100 kg/m2 (30)]. Vitals, including BMI, systolic blood pressure, and diastolic blood pressure, were converted to categorical variables based on clinical cut-points from the National Heart, Lung, and Blood Institute (31) and the American College of Cardiology/American Heart Association (32). We captured comorbidities using the Charlson Comorbidity Index (CCI) (33).
Risk factors for the index hospitalization were included, such as length of stay, admission type (i.e., emergency, elective, urgent, trauma), and discharge status (i.e., home, home health, skilled nursing facility, against medical advice, other). Discharge statuses of ‘other’ included discharges to court/law enforcement, custodial care or support, federal facilities, psychiatric facilities, short-term facilities, and other facilities. We captured macrovascular and microvascular complications using ICD-9-CM codes from Karunakaran et al. (13), and we translated these to ICD-10-CM codes using the following resources: icd9data.com, icd10data.com, and Glasheen et al. (33). Social needs were available through structured data obtained from patients’ self-reported measures in the EHRs; the social needs were descriptive measures, not validated questionnaires. We followed the definition and conceptualization from CMS to include the following 20 social needs (19): activities of daily living, feeling unsafe at home, alcohol use, substance use, smoking/tobacco use, e-cigs/vaping device use, household characteristics (i.e., abuse, alcohol abuse, substance abuse, smoking), employment, work activity level, education, financial security, housing stability, living situation, social support, feeling stressed, stressors, and physical activity. We retained the social needs response from the record nearest to the index hospitalization admission date. Some social needs were not included in the analyses due to high rates of missingness in the data source. For instance, food security was not included because responses were missing for >99% of index hospitalization records.
Statistical analysis
We stratified index hospitalizations by all-cause 30-day readmission status. For univariate analyses, chi-square and t-tests (where applicable) compared risk factors for index hospitalizations with versus without 30-day readmission. Risk factors associated with 30-day readmission status at the p<0.10 level were included in the adjusted analyses (13). For adjusted analyses, we used logistic regression with generalized estimating equations (GEE) to account for the correlation within individuals because one individual could have multiple index hospitalizations (13–15). We employed a multivariable logistic regression model with GEE for the adjusted analysis and reported adjusted odds ratios (aOR) and 95% confidence intervals (95% CIs) for risk factors to demonstrate their relationship with 30-day readmission status. We did not include macrovascular complications in the adjusted regression model because this information was already captured in the CCI calculation, while microvascular complications were retained in the model.
We used chi-square tests to compare social needs for index hospitalizations with versus without 30-day readmission. We evaluated whether social needs added value in predicting all-cause 30-day readmissions by comparing a multivariable logistic regression model without social needs to the model with social needs. After controlling for all covariates in the baseline regression model, a significant association between the newly added variables (i.e., social needs) was considered to add predictive value (34). We used SAS, version 9.4 (SAS Institute, Cary, NC) for data analyses.
Handling of missing data
We treated missing EHRs data to be missing at random based on the possibility that the documentation of clinical records or reporting of social needs could be related to patients’ healthcare utilization. We imputed missing data using multiple imputations by chained equations (MICE), also known as fully conditional specification, which has been recommended as a valid method to handle missing EHR data (35). During the imputation of missing data, we followed recommendations from Wells et al. to perform imputation while considering variables representing healthcare use (prior hospitalization, follow-up appointment post-discharge), diabetes severity (HbA1c), comorbidities (CCI score), socio-economic status (insurance type), and the outcome (30-day readmission) (35). The levels of missingness were highest for social needs variables (reported in Table 2), so we performed a sensitivity analysis to remove social needs with high levels of missingness (≥70%) from the regression model.
Results
Among the original sample of 34,073 adults with diabetes and one or more inpatient hospitalization, 26,332 adults were retained after applying eligibility criteria (Figure 1). Of the 42,126 index hospitalizations, 6407 (15.21%) were followed by all-cause 30-day readmissions. Among those readmitted, the average time to readmission was approximately 13 days (Mean (SD)=13.34 (8.41), Median=12.00, Min=1, Max=30).
Characteristics of study population
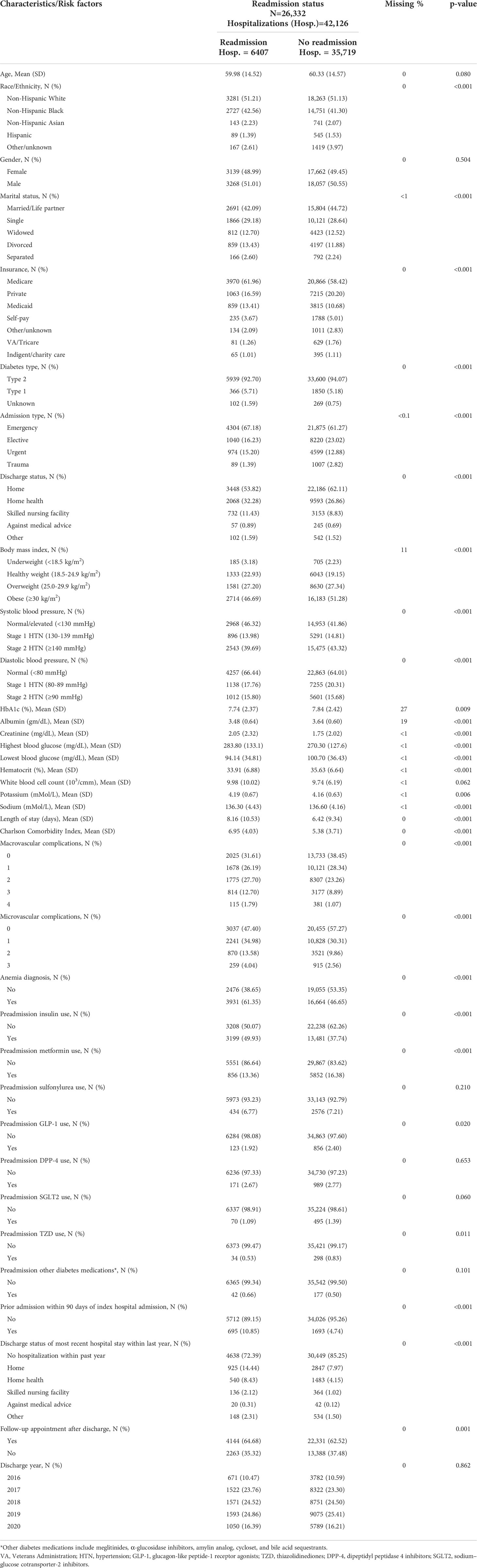
Personal characteristics, including race/ethnicity, marital status, and insurance coverage, were associated with readmission status (p<0.001), while age and gender were not significantly associated with readmission status. The year of discharge was not significant in univariate analysis (p=0.862). The distribution of other risk factors with readmission status can be found in Table 1.
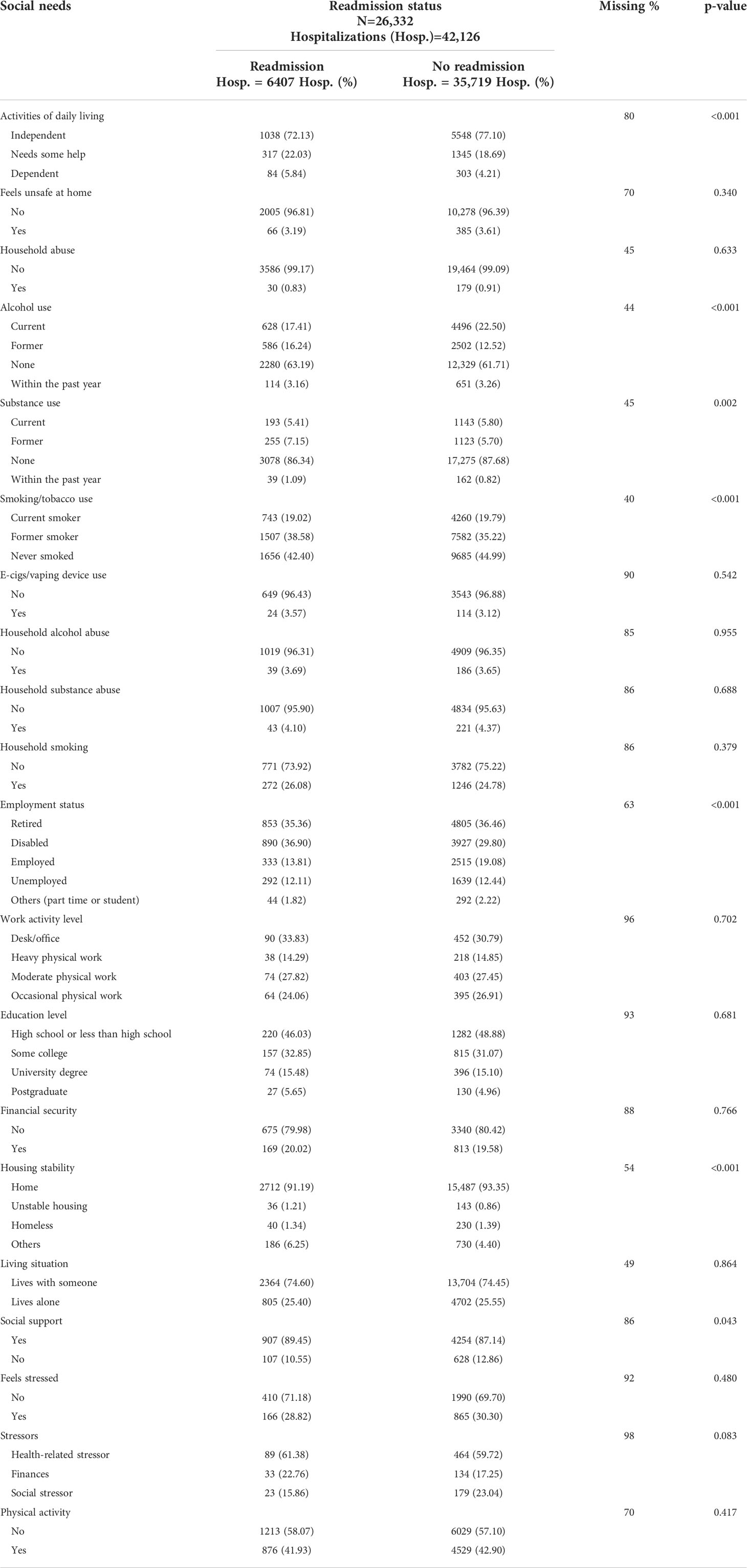
Distribution of social needs by readmission status
The distributions of social needs by readmission status are presented in Table 2. For activities of daily living, readmission was associated with higher distributions of needing some help or being dependent on others compared to no readmission (p<0.001; see Table 2 for frequencies). Readmission was associated with higher distributions of former alcohol use (p<0.001), former substance use (p=0.002), and former smoking/tobacco use (p<0.001) compared to no readmission. Readmission was associated with higher distributions of disabled employment status and lower distributions of employed status compared to no readmission (p<0.001). Unstable housing was more frequent among the readmission group than the no-readmission group (p<0.001), and social support was significantly associated with readmission status (p=0.043). Social needs demonstrating an insignificant relationship with readmission status included feeling unsafe at home, household characteristics (i.e., abuse, alcohol abuse, substance abuse, smoking), using vaping devices, work activity level, education level, financial security, living situation, feeling stressed, types of stressors, and participating in physical activity (p≥0.05 for all).
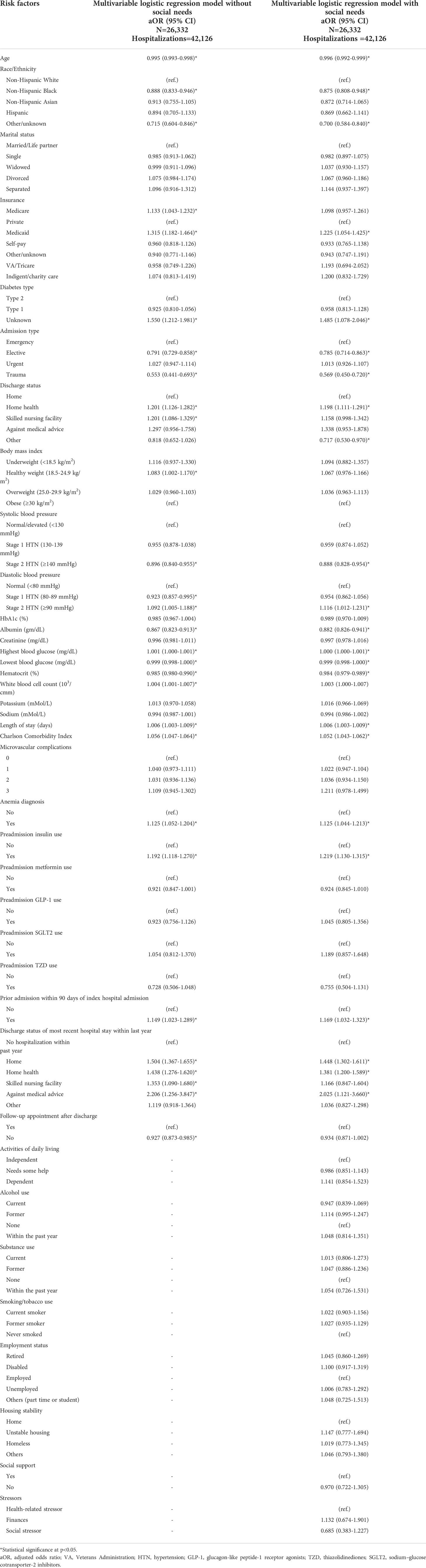
Likelihood of readmission from regression models
The adjusted odds for the multivariable logistic regression models without and with social needs are presented in Table 3. Here, we summarize results from the multivariable logistic regression model without social needs. Increasing age was associated with a lower likelihood of readmission [aOR (95% CI): 0.995 (0.993-0.998)]. Patients of non-Hispanic Black or other/unknown race/ethnicity had lower odds of being readmitted than patients of non-Hispanic White race/ethnicity [aOR (95% CI): 0.888 (0.833-0.946) and 0.715 (0.604-0.846), respectively]. Patients with Medicare or Medicaid were significantly more likely to be readmitted than those covered by private insurance [aOR (95% CI): 1.133 (1.043-1.232) and 1.315 (1.182-1.464), respectively]. While there was no significant difference in readmission between type 1 and type 2 diabetes, patients with unknown diabetes had higher odds of readmission than patients with type 2 diabetes [aOR (95% CI): 1.550 (1.212-1.981)].
Index hospitalizations classified as elective or trauma admissions had lower odds of being readmitted than those with emergency-related admissions [aOR (95% CI): 0.791 (0.729-0.858) and 0.553 (0.441-0.693), respectively]. Index hospitalizations discharged to home health or skilled nursing facilities had higher odds of being readmitted than those discharged to home [aOR (95% CI): 1.201 (1.126-1.282) and 1.201 (1.086-1.329), respectively]. The healthy BMI category was associated with higher odds of readmission compared to obese BMI [aOR (95% CI): 1.083 (1.002-1.170)]. Stage 1 hypertension (diastolic blood pressure 80-90 mmHg) was associated with lower odds of readmission compared to normal diastolic blood pressure [aOR (95% CI): 0.923 (0.857-0.995)], but stage 2 hypertension (diastolic blood pressure ≥90 mmHg) was associated with higher odds of readmission [aOR (95% CI): 1.092 (1.005-1.188)].
HbA1c was not significantly associated with readmission status. For blood glucose measurements during hospitalization, higher values for the highest blood glucose were associated with a higher likelihood of readmission, and increasing values for the lowest blood glucose were associated with a lower likelihood of readmission. Other labs, including albumin [aOR (95% CI): 0.867 (0.823-0.913)], hematocrit [aOR (95% CI): 0.985 (0.980-0.990)], and white blood cell count [aOR (95% CI): 1.004 (1.001-1.007)], were significantly associated with readmission status. The odds of readmission were increased with a longer length of stay [aOR (95% CI): 1.006 (1.003-1.009)] and a higher CCI [aOR (95% CI): 1.056 (1.047-1.064)].
An anemia diagnosis increased the odds of readmission compared to no diagnosis [aOR (95% CI): 1.125 (1.052-1.204)]. Preadmission insulin use increased the odds of readmission [aOR (95% CI): 1.192 (1.118-1.270)], but other diabetes medication classes were not associated with readmission status. A prior hospital stay within the past 90 days increased the odds of readmission [aOR (95% CI): 1.149 (1.023-1.289)]. The discharge status of the most recent hospitalization within the last year was a significant predictor of readmission. Discharges to home [aOR (95% CI): 1.504 (1.367-1.655)], home health [aOR (95% CI): 1.438 (1.276-1.620)], skilled nursing facility [aOR (95% CI): 1.353 (1.090-1.680)], or against medical advice [aOR (95% CI): 2.206 (1.256-3.847)] were associated with increased odds of readmission compared to those with no prior hospitalizations within the last year. Lastly, no follow-up appointment after discharge was associated with lower odds of readmission [aOR (95% CI): 0.927 (0.873-0.985)].
Added predictive value of social needs
We briefly highlight the different results for the regression model with social needs here. The risk factors no longer significantly associated with readmission status were Medicare versus private insurance, discharge status to a skilled nursing facility, healthy BMI category, diastolic blood pressure 80-89 mmHg, white blood cell count, discharge status of most recent hospital stay to a skilled nursing facility, and follow-up appointment after discharge. After controlling for clinical risk factors in the baseline model and social needs, index hospital discharge status to other vs. home was significantly associated with a lower likelihood of readmission [aOR (95% CI): 0.717 (0.530-0.970)]. Here, no social needs were significantly associated with readmission status (p≥0.05; see Table 3 for aORs for social needs). In the sensitivity analysis, we excluded social needs with high levels of missingness (≥70%) from the regression model (i.e., activities of daily living, social support, and types of stressors). Results were similar to the two reported regression models in Table 3, except for the result for former versus no alcohol use. In the sensitivity analysis, former alcohol use was significantly associated with higher odds of readmission compared to no alcohol use [aOR (95% CI): 1.121 (1.008-1.247)].
Discussion
We identified various factors associated with 30-day readmissions among patients with diabetes in the Deep South. These factors included demographics (i.e., age, race/ethnicity, insurance status, unknown diabetes type), characteristics of hospitalizations (i.e., admission type, discharge status, length of stay, prior hospitalizations, discharge status of the most recent hospital stay within the last year), labs and vitals (i.e., albumin, hematocrit, highest and lowest blood glucose measurements, blood pressure), co-existing chronic conditions (i.e., CCI score and anemia diagnosis), preadmission medication use (i.e., insulin use), and social need (i.e., former alcohol use). These risk factors can support the readmission risk assessment for patients with diabetes in the Deep South. Factors associated with readmission risk can help identify high-risk patient groups for all-cause 30-day readmissions during pharmacy clinical services.
Our work in studying readmission risk among patients with diabetes in the Deep South expands upon the foundational work by Rubin et al. and Karunakaran et al. in creating, validating, and extending the DERRI™ (13–15). Our findings apply these prior works to the Deep South population. The majority of risk factors we found to be associated with readmission risk are supported by similar findings from Karunakaran et al., but some key differences were found for risk factors, such as age, gender, employment status, creatinine, having a follow-up appointment after discharge, etc. (13). Looking at pooled results across studies from a systematic review, our findings for readmission risk being associated with insurance type, comorbidities, insulin use, and length of stay align closely with prior literature (11). However, our findings for gender, race, and age contrasted with their results, demonstrating key differences in findings from the Deep South population compared to other U.S. populations (11).
Our study adds value and new information to the transitions of care literature in its comprehensive assessment of factors influencing readmissions among people with diabetes and its expansion to include social needs. Even though social factors have long been recognized to influence health outcomes (18), limited studies investigating readmissions have considered social needs among non-disease-specific populations (20, 21). In contrast, a recent study by Pinheiro et al. recognized the cumulative effect of social needs in increasing patients’ risk for heart failure-related hospitalizations (36). Our study applied a similar approach to Pinheiro et al. (36) by applying their methods to the diabetes context investigating the influence of social needs on readmissions. We identified various social needs associated with readmission risk in unadjusted analyses, and we found former alcohol use to be associated with an increased risk of readmission in the sensitivity analysis. Thus, alcohol use was found to be “an independent predictor” (34) of 30-day readmissions among patients with diabetes in the Deep South. Prior literature among other populations also found alcohol use/abuse to increase readmission risk (37) or to have no significant effect (38). We are limited in interpreting our finding of the potential relationship between alcohol use and readmission because all people reporting alcohol use were grouped together into “current” or “former” alcohol use categories. Thus, we were not able to determine the amount of alcohol consumption or to differentiate between alcohol use versus abuse, which could influence the relationship with readmissions.
The recognized importance and consideration of social needs in health outcomes and clinical care also bring forth expected challenges. Our experience through this study demonstrates the challenges from incomplete data capture of social needs within EHRs. The missingness of data for social needs varied by concept, ranging from a low of 40% for smoking/tobacco use to a high of 98% for type of stressors. Due to the lack of complete data, we imputed missing data using multiple imputation. Imputation of social needs with high missingness likely limited our ability to learn anything about the associations we were interested in testing due to high variance. Thus, the high levels of missingness for social needs may have influenced the nonsignificant findings between social needs and readmission status in the adjusted regression model. Still, our findings of significant relationships between social needs and readmission status in either unadjusted or the sensitivity analysis support a call for further research. Further research with more complete social needs data is needed to understand the influence of social needs on readmissions among populations with diabetes. Recent work in linking EHRs with social factors available through U.S. Census data brings a potential solution to the challenge of capturing social needs in clinical data (39). Further work is also needed to understand the potential clinical utility of incorporating social needs into clinical services. For instance, pharmacy clinical services could serve an integral role in collecting social needs data from patients given pharmacists’ more routine interactions with patients compared to other healthcare settings.
One major strength of this study and its findings is its focus on patients with diabetes in the Deep South. Our focus on the Deep South fills the existing research gap for readmissions among the diabetes population in this area, where the prevalence of diabetes surpasses the national average (22). Prior literature in this realm has studied many other populations with diabetes, such as insured populations (commercial, Medicare, or Medicaid), clinical data from the general U.S. population, or EHRs from health systems in the Northeast (9, 11–15, 40). In the present study, we demonstrated the multitude of risk factors contributing to readmission risk among patients with diabetes in the Deep South. Our findings can support decision-making around factors influencing patients’ readmission risks in the Deep South, including expanding healthcare decision-making to consider individuals’ social needs (41). Our findings can also provide evidence for future intervention studies for populations with diabetes. Different clinical interventions, including pharmacy clinical services (42), have been efficacious in reducing hospital readmission rates among patients with diabetes (5, 43). Community health workers could serve a vital role in coordinating social needs through community-based interventions to further reduce readmissions (44). Further, incorporating social needs into a case management intervention has proven beneficial in reducing inpatient admissions (45).
Another key strength of this study was investigating readmission risk by diabetes type. We found no significant difference in readmission risk for patients diagnosed with type 1 versus type 2 diabetes. Through a recent systematic review, Soh et al. identified a gap in the literature studying readmission risk by diabetes type because most studies lump patients with type 1 and type 2 diabetes together (11). To address this gap, we included diabetes type as a risk factor in studying readmission risk. Our findings demonstrate that diabetes type may not significantly affect readmission risk among patients in the Deep South. However, patients with unknown diabetes type had significantly higher odds of 30-day readmission than patients with type 2 diabetes. Patients were classified as having an unknown diabetes type because they were prescribed a diabetes medication before the hospitalization but did not have any diabetes diagnosis codes. The higher readmission risk for patients with unknown diabetes in the Deep South is an interesting finding that calls for further investigation. Our finding is supported by prior research showing a higher likelihood of readmission when diabetes is not coded in the medical record, further highlighting the importance of diabetes even when patients may be hospitalized for other reasons (40).
In conclusion, we identified the factors that impacted the risk of 30-day readmissions among patients with diabetes in the Deep South. Clinical assessment of readmission risk in the Deep South should consider patients’ demographics, characteristics of hospitalizations, labs, vitals, co-existing chronic conditions, preadmission antihyperglycemic medication use, and social needs. Factors associated with readmission risk can help pharmacists and other healthcare providers identify high-risk patient groups for all-cause 30-day readmissions during transitions of care. Further research is needed about the influence of social needs on readmissions among populations with diabetes to understand the potential clinical utility of incorporating social needs into clinical services.
Limitations
We cautiously report that factors are associated with increased readmission risk due to the secondary data analysis of EHRs. Because our data source was EHRs, we were limited to capturing readmissions within our health system, and we may have missed readmissions occurring in another health system. Although we made efforts to control for confounding variables in the adjusted analysis, there is still potential for residual confounding. We were also limited in analyzing factors available in the EHRs. Other factors that might be expected to influence readmissions and diabetes care, such as detailed information from physician notes about discharge planning, self-care behaviors, psychosocial factors (e.g., diabetes distress) (46), or other social needs (38), were not available in the limited dataset. The missingness of social needs data is a major limitation of this study, and the population of patients reporting social needs could represent a biased sample. Clinically important variables, such as cholesterol and procedures, were not available in the data source. We also did not have access to 9-digit zip codes, which prevented us from calculating the patients’ living distance from the hospital that has been continually documented as an important predictor for readmission in patients with diabetes (13–15). We acknowledge that this data was collected for clinical practice purposes rather than research purposes, so the reliability of data elements, such as outpatient prescription records, could be a limitation. However, previous research among patients with diabetes has shown that prescription orders documented in EHRs can be used to represent prescriptions filled and dispensed (47). Lastly, there is a potential for misclassification bias in identifying patients with diabetes. Patients taking antihyperglycemic medications for other conditions (e.g., metformin for prediabetes or polycystic ovary syndrome) could have been incorrectly classified as having diabetes. However, this was not expected to have major effects on findings because less than 0.9% of patients took antihyperglycemic medications but did not have a diabetes diagnosis code.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: The dataset used in this study is confidential and cannot be shared.
Ethics statement
The studies involving human participants were reviewed and approved by Auburn University Institutional Review Board for the Protection of Human Subjects in Research (IRB). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
CM and CC contributed to conceptualization, methodology, data acquisition, investigation, project administration, funding acquisition, and reviewing/editing the manuscript. CM performed software programming, data curation, formal analysis, and writing the original manuscript draft. CC supervised the research. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under award number TL1TR003106. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. McDaniel was supported by the American Foundation for Pharmaceutical Education (AFPE), and she is currently supported by the PhRMA Foundation under the Pre-Doctoral Fellowship in Health Outcomes Research. Chou is currently supported by the PhRMA Collaborative Actions to Reach Equity (CAREs) grant program.
Acknowledgments
Preliminary results from this work were presented in abstract form at the Association for Clinical and Translational Science Annual Meeting in April 2021 and the American Association of Colleges of Pharmacy Annual Meeting in July 2022.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcdhc.2022.1050579/full#supplementary-material
References
2. World Health Organization (WHO). Global report on diabetes. Geneva, Switzerland: WHO Press (2016).
3. Agency for Healthcare Research and Quality (AHRQ), Healthcare Cost and Utilization Project (HCUP), National Inpatient Sample (NIS). Clinical Classifications Software Refined (CCSR) for ICD-10-CM default categorization scheme for the principal diagnosis. (2018). Available at: https://www.hcup-us.ahrq.gov/faststats/national/inpatientcommondiagnoses.jsp (Accessed March 9, 2022).
4. Naylor MD, Aiken LH, Kurtzman ET, Olds DM, Hirschman KB. The care span: The importance of transitional care in achieving health reform. Health Aff (Millwood) (2011) 30:746–54. doi: 10.1377/hlthaff.2011.0041
5. Garnica P. Transition of care for patients with diabetes. Curr. Diabetes Rev. (2017) 13:263–79. doi: 10.2174/1573399813666161123104407
6. Powers MA, Bardsley J, Cypress M, Duker P, Funnell MM, Fischl AH, et al. Diabetes self-management education and support in type 2 diabetes. Diabetes Educ. (2017) 43:40–53. doi: 10.1177/0145721716689694
7. Centers for Medicare and Medicaid Services. 2015 measure information about the 30-day all-cause hospital readmission measure, calculated for the value-based payment modifier program . Available at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeedbackProgram/Downloads/2015-ACR-MIF.pdf (Accessed March 9, 2022).
8. Ostling S, Wyckoff J, Ciarkowski SL, Pai CW, Choe HM, Bahl V, et al. The relationship between diabetes mellitus and 30-day readmission rates. Clin. Diabetes Endocrinol. (2017) 3:3. doi: 10.1186/s40842-016-0040-x
9. Enomoto LM, Shrestha DP, Rosenthal MB, Hollenbeak CS, Gabbay RA. Risk factors associated with 30-day readmission and length of stay in patients with type 2 diabetes. J. Diabetes Complications (2017) 31:122–7. doi: 10.1016/j.jdiacomp.2016.10.021
10. Bansal V, Mottalib A, Pawar TK, Abbasakoor N, Chuang E, Chaudhry A, et al. Inpatient diabetes management by specialized diabetes team versus primary service team in non-critical care units: impact on 30-day readmission rate and hospital cost. BMJ Open Diabetes Res. Care (2018) 6:e000460. doi: 10.1136/bmjdrc-2017-000460
11. Soh JGS, Wong WP, Mukhopadhyay A, Quek SC, Tai BC. Predictors of 30-day unplanned hospital readmission among adult patients with diabetes mellitus: a systematic review with meta-analysis. BMJ Open Diabetes Res. Care (2020) 8:e001227. doi: 10.1136/bmjdrc-2020-001227
12. Eby E, Hardwick C, Yu M, Gelwicks S, Deschamps K, Xie J, et al. Predictors of 30 day hospital readmission in patients with type 2 diabetes: a retrospective, case-control, database study. Curr. Med. Res. Opin. (2015) 31:107–14. doi: 10.1185/03007995.2014.981632
13. Karunakaran A, Zhao H, Rubin DJ. Predischarge and postdischarge risk factors for hospital readmission among patients with diabetes. Med. Care (2018) 56:634–42. doi: 10.1097/mlr.0000000000000931
14. Rubin DJ, Handorf EA, Golden SH, Nelson DB, McDonnell ME, Zhao H. Development and validation of a novel tool to predict hospital readmission risk among patients with diabetes. Endocr. Pract. (2016) 22:1204–15. doi: 10.4158/e161391.Or
15. Rubin DJ, Recco D, Turchin A, Zhao H, Golden SH. External validation of the diabetes early re-admission risk indicator (DERRI(™)). Endocr. Pract. (2018) 24:527–41. doi: 10.4158/ep-2018-0035
16. Collins J, Abbass IM, Harvey R, Suehs B, Uribe C, Bouchard J, et al. Predictors of all-cause 30 day readmission among Medicare patients with type 2 diabetes. Curr. Med. Res. Opin. (2017) 33:1517–23. doi: 10.1080/03007995.2017.1330258
17. Hill-Briggs F, Adler NE, Berkowitz SA, Chin MH, Gary-Webb TL, Navas-Acien A, et al. Social determinants of health and diabetes: a scientific review. Diabetes Care (2021) 44:258–79. doi: 10.2337/dci20-0053
18. Committee on the Recommended Social and Behavioral Domains and Measures for Electronic Health Records, Board on Population Health and Public Health Practice, Institute of Medicine. Capturing social and behavioral domains in electronic health records: phase 1 (2014). Washington (DC: National Academies Press (US. Available at: https://www.ncbi.nlm.nih.gov/books/NBK222134/ (Accessed March 9, 2022).
19. Center for Medicare & Medicaid Services (CMS). A guide to using the accountable health communities health-related social needs screening tool: promising practices and key insights (2021). Available at: https://innovation.cms.gov/media/document/ahcm-screeningtool-companion (Accessed November 11, 2021).
20. Carter J, Ward C, Thorndike A, Donelan K, Wexler DJ. Social factors and patient perceptions associated with preventable hospital readmissions. J. Patient Exp. (2020) 7:19–26. doi: 10.1177/2374373518825143
21. Bensken WP, Alberti PM, Koroukian SM. Health-related social needs and increased readmission rates: findings from the nationwide readmissions database. J. Gen. Intern. Med. (2021) 36:1173–80. doi: 10.1007/s11606-021-06646-3
22. Barker LE, Kirtland KA, Gregg EW, Geiss LS, Thompson TJ. Geographic distribution of diagnosed diabetes in the U.S.: a diabetes belt. Am. J. Prev. Med. (2011) 40:434–9. doi: 10.1016/j.amepre.2010.12.019
23. Peirce NR. The deep south states of America: people, politics, and power in the seven deep south states [book review]. J. South. History (1974) 40:639–41.
24. Wills MJ, Whitman MV, English TM. Travel distance to cancer treatment facilities in the deep south. J. Healthc Manag (2017) 62:30–43.
25. Chronic conditions data warehouse: condition categories . Available at: https://www2.ccwdata.org/web/guest/condition-categories (Accessed December 17, 2021).
26. McCoy RG, Lipska KJ, Herrin J, Jeffery MM, Krumholz HM, Shah ND. Hospital readmissions among commercially insured and Medicare advantage beneficiaries with diabetes and the impact of severe hypoglycemic and hyperglycemic events. J. Gen. Intern. Med. (2017) 32:1097–105. doi: 10.1007/s11606-017-4095-x
27. Kuklina EV, Tong X, Bansil P, George MG, Callaghan WM. Trends in pregnancy hospitalizations that included a stroke in the united states from 1994 to 2007: reasons for concern? Stroke (2011) 42:2564–70. doi: 10.1161/strokeaha.110.610592
28. Cao T, Johnson A, Coogle J, Zuzelski A, Fitzgerald S, Kapadia V, et al. Incidence and characteristics associated with hospital readmission after discharge to home hospice. J. Palliat Med. (2020) 23:233–9. doi: 10.1089/jpm.2019.0246
29. Estiri H, Klann JG, Murphy SN. A clustering approach for detecting implausible observation values in electronic health records data. BMC Med. Inform Decis Mak (2019) 19:142. doi: 10.1186/s12911-019-0852-6
30. Dawwas MF, Lewsey JD, Neuberger JM, Gimson AE. The impact of serum sodium concentration on mortality after liver transplantation: a cohort multicenter study. Liver Transpl (2007) 13:1115–24. doi: 10.1002/lt.21154
31. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults–the evidence report. national institutes of health. Obes. Res. (1998) 6 Suppl 2:51s–209s. doi: 10.1002/j.1550-8528.1998.tb00690.x
32. Whelton PK, Carey RM, Aronow WS, Casey DE Jr., Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American college of Cardiology/American heart association task force on clinical practice guidelines. Hypertension (2018) 71:1269–324. doi: 10.1161/hyp.0000000000000066
33. Glasheen WP, Cordier T, Gumpina R, Haugh G, Davis J, Renda A. Charlson comorbidity index: ICD-9 update and ICD-10 translation. Am. Health Drug Benefits (2019) 12:188–97.
34. Vickers AJ, Cronin AM, Begg CB. One statistical test is sufficient for assessing new predictive markers. BMC Med. Res. Methodol (2011) 11:13. doi: 10.1186/1471-2288-11-13
35. Wells BJ, Chagin KM, Nowacki AS, Kattan MW. Strategies for handling missing data in electronic health record derived data. EGEMS (2013) 1:1035. doi: 10.13063/2327-9214.1035
36. Pinheiro LC, Reshetnyak E, Sterling MR, Levitan EB, Safford MM, Goyal P. Multiple vulnerabilities to health disparities and incident heart failure hospitalization in the REGARDS study. Circ. Cardiovasc. Qual Outcomes (2020) 13:e006438. doi: 10.1161/circoutcomes.119.006438
37. Patel N, Singh S, Desai R, Desai A, Nabeel M, Parikh N, et al. Thirty-day unplanned readmission in hospitalised asthma patients in the USA. Postgrad Med. J. (2021). doi: 10.1136/postgradmedj-2021-140735
38. Navathe AS, Zhong F, Lei VJ, Chang FY, Sordo M, Topaz M, et al. Hospital readmission and social risk factors identified from physician notes. Health Serv. Res. (2018) 53:1110–36. doi: 10.1111/1475-6773.12670
39. Udalova V, Carey TS, Chelminski PR, Dalzell L, Knoepp P, Motro J, et al. Linking electronic health records to the American community survey: feasibility and process. Am. J. Public Health (2022) 112:923–30. doi: 10.2105/ajph.2022.306783
40. Robbins JM, Webb DA. Diagnosing diabetes and preventing rehospitalizations: the urban diabetes study. Med. Care (2006) 44:292–6. doi: 10.1097/01.mlr.0000199639.20342.87
41. Kotay A, Huang JL, Jordan WB, Korin E. Exploring family and social context through the electronic health record: physicians' experiences. Fam Syst. Health (2016) 34:92–103. doi: 10.1037/fsh0000190
42. Murphy JA, Schroeder MN, Ridner AT, Gregory ME, Whitner JB, Hackett SG. Impact of a pharmacy-initiated inpatient diabetes patient education program on 30-day readmission rates. J. Pharm. Pract. (2020) 33:754–9. doi: 10.1177/0897190019833217
43. Rubin DJ. Correction to: hospital readmission of patients with diabetes. Curr. Diabetes Rep. (2018) 18:21. doi: 10.1007/s11892-018-0989-1
44. Carter J, Hassan S, Walton A, Yu L, Donelan K, Thorndike AN. Effect of community health workers on 30-day hospital readmissions in an accountable care organization population: a randomized clinical trial. JAMA Netw Open (2021) 4:e2110936. doi: 10.1001/jamanetworkopen.2021.10936
45. Brown DM, Hernandez EA, Levin S, De Vaan M, Kim MO, Lynch C, et al. Effect of social needs case management on hospital use among adult Medicaid beneficiaries: A randomized study. Ann. Intern. Med. (2022) 175:1109–17. doi: 10.7326/m22-0074
46. Gonzalez JS, Tanenbaum ML, Commissariat PV. Psychosocial factors in medication adherence and diabetes self-management: implications for research and practice. Am. Psychol. (2016) 71:539–51. doi: 10.1037/a0040388
Keywords: diabetes, readmission, transitions of care, risk factor, social need, Deep South
Citation: McDaniel CC and Chou C (2022) Clinical risk factors and social needs of 30-day readmission among patients with diabetes: A retrospective study of the Deep South. Front. Clin. Diabetes Healthc. 3:1050579. doi: 10.3389/fcdhc.2022.1050579
Received: 21 September 2022; Accepted: 10 October 2022;
Published: 26 October 2022.
Edited by:
Muhammad Shahzad Aslam, Xiamen University, Malaysia, MalaysiaReviewed by:
Mirrat Gul Butt, Mayo Hospital, PakistanQurratulain Leghari, Hamdard University, Pakistan
Copyright © 2022 McDaniel and Chou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chiahung Chou, Y3pjMDEwOUBhdWJ1cm4uZWR1
 Cassidi C. McDaniel
Cassidi C. McDaniel Chiahung Chou
Chiahung Chou