
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Child Adolesc. Psychiatry, 05 June 2024
Sec. Interventions for Adolescent Mental Health
Volume 3 - 2024 | https://doi.org/10.3389/frcha.2024.1393401
This article is part of the Research TopicImproving Impacts of Mental Health Treatment on Substance Misuse and Vice VersaView all 3 articles
Introduction: Although research on the development and efficacy of adolescent substance use treatment has made recent strides, many models do not translate into practice, especially when working with underserved youth who often face barriers to treatment. Meal incentives, rolling admission, and transportation assistance may be promising approaches to decrease barriers, thereby increasing treatment engagement, retention, and completion. The purpose of this evaluation was two-fold: (1) to examine treatment engagement amongst diverse, underserved youth in an intensive outpatient program for substance misuse in an urban metropolitan area, and (2) to investigate the role of meal incentives, rolling admission, and transportation assistance in youth engagement.
Methods: The intervention was 8 weeks of Acceptance and Commitment Therapy and trauma-focused group intervention, combined with contingency management, meal incentives, and transportation assistance. Treatment engagement, retention, and completion was compared against selected demographic variables (i.e., race and insurance coverage) and at three phases of program implementation: cohort admissions with transportation assistance (phase 1); rolling admissions with transportation assistance (phase 2); and rolling admissions with transportation assistance and meal incentives (phase 3). Data was analyzed using two-way ANOVAs; identified interactions were probed.
Results: Participants were 110 adolescents (ages 13–17) consecutively admitted to an intensive outpatient substance treatment program. Racial identities of participants were 40.0% Latinx, 3.6% Black, 0.9% American Indian or Alaska Native, 6.4% two or more races, and 49.1% White. A total of 67 of 110 (60.9%) youth had state-funded Medicaid or no insurance. Of the youth that engaged in treatment across all implementation phases, 68.7% were provided transportation assistance. Analyses illustrated no difference in outcomes based on selected demographic variables. The percentage of youth completing treatment was 22.7% and the average number of groups attended was 6.32 (SD = 6.49). Results showed a significant improvement in outcomes with the implementation of incentives such that engagement and retention in treatment was significantly higher for those in phase 3 compared to those in phase 1 (p < .001) and phase 2 (p = .021).
Discussion: This evaluation shows that previously documented health disparities in substance treatment engagement and retention are not found when certain barriers are addressed.
According to the (1) report, the number of youths who reported a substance use disorder in the past year increased over 50%, from 4.08% in 2021 (2) to 6.34% in 2022 (1). Further, youths who experienced a major depressive episode in the past year increased from 10.6% in 2021 (2) to 11.5% in 2022 (1), with only 28% of youth with severe depression receiving some consistent treatment (1). Now more than ever, there is a need to reduce the overall burden of disease and risk of premature mortality associated with mental health and substance use disorders among young people. However, the current models of treatment for adolescent substance use disorders, particularly those from lower-socioeconomic status (SES) and ethnic and racial minority backgrounds with less access to care, have significant limitations, particularly in higher-level outpatient settings [i.e., intensive outpatient programs (IOP)] (3, 4).
First, many adolescents drop out of treatment, and Black and Latinx youth are significantly less likely than White youth to complete treatment for substance-related concerns (4). More specifically, previous research has found that about half of Black and Latinx youth drop out of treatment, in comparison to one-third of their White counterparts (4). Moreover, Black adolescents are 38% less likely to access care than White adolescents, and are less likely to engage in treatment, even when care is accessed (3). These findings demonstrate the systemic factors that create disparities in treatment access, engagement, and retention between racially and ethnically minoritized youths and their White peers.
Second, many treatment programs do not address the patient, family, contextual-, social and cultural barriers that prevent accessibility to treatment, particularly amongst racially and ethnically minoritized youth. Some specific barriers to treatment include self-perceived and parent-perceived stigma and fear (5), as well as family education and cultural norms around mental health (6). Further, families with limited resources might not be able to prioritize treatment due to other structural inequalities and urgent competing demands, such as food insecurity, unstable housing, work conflicts, transportation problems, and lack of child-care (6). It is not uncommon for new immigrant families to live in multigenerational households, where older adolescents are expected to either care for younger siblings or elderly grandparents at home (7); therefore, prioritizing treatment becomes a challenge.
Due to these barriers, typical programming for intensive outpatient care becomes particularly inaccessible for youths with low-SES and from racial/ethnic minority groups. Generally, youth attending IOP spend an average of 15 h per week in individual, family, and group treatment settings with a multidisciplinary team of professionals, including psychiatrists, psychologists, counselors, social workers, and others (8). However, given the barriers that youth from low-SES and racial/ethnic minority groups may already face, this programmatic structure then creates a barrier to treatment—not all adolescents, nor their parents, have the privilege of time or resources to spend in (much less travel to and from) treatment four to five days a week.
There are several approaches to reducing these barriers and facilitate access, engagement, retention, and completion in IOP treatment for substance use disorders for underserved adolescents including: (a) reducing the programming's time commitment; (b) providing transportation assistance; (c) decreasing treatment wait times by implementing rolling admission; (d) incentivizing participation by helping adolescents and their families address basic needs that become impacted through treatment. These interventions have potential to reduce disruptions in adolescents' and their family's daily lives by reducing the amount of time needed to engage in treatment.
The current evaluation was designed to report the impact of these interventions on treatment engagement, retention, and completion for diverse youth enrolled in IOP treatment for substance use disorders. The implemented IOP for adolescent substance use treatment was intentionally designed to reduce barriers and facilitate access to treatment in an urban hospital-based outpatient clinic. Utilizing data from two years of program implementation, this non-randomized, quality improvement program evaluation had two main objectives: (1) to examine treatment engagement, retention, and completion amongst diverse and traditionally underserved adolescents participating in a reduced-time 8-week IOP for adolescent substance use disorders and co-occurring mental health conditions; and (2) to investigate the effect of interventions aimed at facilitating access to IOP treatment (e.g., meal incentives, rolling admission, and transportation assistance) on treatment engagement, retention, and completion. Because past research has illustrated notable differences in treatment engagement, retention, and completion based on demographic factors, such as race and socioeconomic status (3, 5, 6), one major goal of our IOP was to reduce barriers to treatment by implementing barrier reduction interventions at all phases of treatment in order to create equitable access to treatment for youth from racially and ethnically marginalized and low-SES backgrounds and essentially level the playing field for youth who have historically had less access to care. Thus, we hypothesized no significant differences in treatment engagement, retention, and completion based on selected youth demographic variables (youth of color vs. White youth; youth with state-funded Medicaid or no insurance vs. youth with private or commercial insurance) in our present sample. In other words, with the consistent implementation of barrier reduction interventions, we predict that youth of color and youth with state-funded Medicaid or no insurance will engage in, retain in, and complete treatment at a similar rate as their White and private or commercially insured peers, respectively. Similarly, we did not anticipate significant interactions between selected youth demographic variables and the implementation of barrier reduction interventions. However, we did predict higher engagement, retention, and completion rates with the implementation of meal incentives, rolling admission, and transportation assistance. In sum, we expected that the implementation of additional barrier reduction interventions (beyond transportation assistance) would improve treatment engagement, retention, and completion for all participating youth.
Outcomes data are regularly collected as part of the program's ongoing quality improvement procedures. These data are also used to inform programmatic and clinical changes to enhance the delivery of services. This evaluation is a non-randomized, retrospective chart review designed to determine whether interventions aimed at reducing barriers to treatment are associated with an increase in engagement, retention, and completion in intensive outpatient programming amongst historically underserved adolescents. This evaluation was reviewed and approved by the Colorado Multiple Institutional Review Board (COMIRB).
Patients are referred to the IOP through direct relationships with the program [e.g., Substance Treatment, Education, and Prevention (STEP) traditional outpatient program, hospitals, care networks, physicians, community partners]. Upon completing an intake to the STEP program, intake therapists completed an assessment to determine whether the patient qualified for ASAM Criteria Level 2.1 or higher. The ASAM Criteria are a unified set of standards for determining patient admission, continued service, and transfer criteria by assessing patient needs on six dimensions (e.g., Acute Intoxication and/or Withdrawal Potential; Biomedical Conditions and Complications; Emotional, Behavioral, or Cognitive Conditions and Complications; Readiness to Change; Relapse, Continued Use, or Continued Problem Potential; and Recovering/Living Environment (9);. ASAM Level 2.1 refers to Intensive Outpatient Programming (IOP). Primary clinical presentations included, but are not limited to, opioid use disorder, alcohol use disorder, cocaine use disorder, cannabis use disorder, and/or methamphetamine use disorder. Co-occurring psychiatric disorders included, but are not limited to, major depressive disorder, social anxiety disorder, generalized anxiety disorder, adjustment disorder, and/or posttraumatic stress disorder. Patients consented to treatment at intake and continued to assent to treatment by continuing to present to and engage in IOP interventions.
After it was determined that patients qualify for ASAM Level 2.1 level of care, patients were then referred to the IOP and scheduled to begin during the closest Tuesday from referral date if there is availability. Standard of care for patients participating in IOP included group therapy twice a week for three hours per day (6 h per week) for 8 consecutive weeks, individual therapy for one hour once per week, parent support/consultation for 30 min to one hour once per week, and medication management or medication for substance use disorders as needed. Group size is capped at eight patients. The amount of time patients spent in group therapy was decreased from typical IOPs (3 h, 2 days per week vs. 3 h, 3–4 days per week) to increase accessibility of treatment to adolescents with limited sources.
The IOP provides in-person substance use and co-occurring mental health treatment to adolescents aged 13–17 with high acuity substance use and mental health diagnoses in an urban United States city. The program specializes in treating complex cases, including youth with severe trauma, neglect, justice system involvement, foster case experience, and youth who have had multiple inpatient or hospital admissions.
The group structure and content were developed using impACT (10), an integrated Motivational Interviewing (MI) and Acceptance and Commitment Therapy (ACT) model for adolescent substance use treatment, DNA-V (11), a model of ACT developed for adolescents, and Structured Psychotherapy for Adolescents Responding to Chronic Stress (12) group therapy curriculums and informed by the theory of emotionality stigma (13). Group content was adapted for the specific substance use treatment needs of the patient population and the structure was adapted to meet ASAM Level 2.1 clinical care guidelines for IOP services for adolescents (9).
Each group session was composed of a 180-min block and was led by two group leaders, a licensed psychologist and a psychology resident. At each clinical appointment, therapists conducted urine drug screens and provided contingency management aimed at rewarding attendance and engagement. The contingency management was modeled after the fishbowl method in which adolescents draw tickets corresponding to $5, $10, $25, or $100 (14). The total amount earned was loaded onto a debit card. The number of tickets drawn was one plus the number of consecutive IOP group appointments attended. Total payouts are not tracked for this project.
Interventions to reduce barriers to care and facilitate access to treatment were implemented in three distinct phases that built upon each other. To reduce barriers to care, transportation services via MetroTaxi, a local cab service, or Intelliride, a Medicaid transportation service, was provided to any patient that expressed a need for transportation assistance (phase 1). During phase 1, patients were admitted on a cohort basis, with new patients being admitted every 4 weeks. To increase access to care and care availability, the group began admitting on a rolling basis, as opposed to cohorts, with new participants allowed to be admitted every Tuesday (phase 2). Later, several incentives were provided to address basic need impacts as barriers to treatment, such as providing patients with dinner and snacks (phase 3).
Baseline demographic variables including patient age, sex, and race were self-reported. We also gathered client's insurance coverage data as a measure of socioeconomic status. The following are the three treatment outcomes for this study:
(1) Treatment engagement. Treatment engagement was used to track which referred and enrolled patients started treatment. This variable was dichotomously coded (0 = patient did not start treatment, 1 = patient did start treatment).
(2) Treatment retention. This outcome was measured by the number of sessions completed (Range = 0–16) within the 8 weeks of treatment. While some youth requested to stay in the program for longer than 8 weeks of treatment, for the purpose of this paper, only retention through the intended 8 weeks of treatment was included.
(3) Treatment completion. This outcome was measured by the number of youth completing and graduating from the IOP. This variable was dichotomously coded (0 = patient did complete treatment, 1 = patient did complete treatment).
To examine our hypotheses, we utilized a series of two-way ANOVAs as well as follow-up tests to probe any identified interactions. First, we investigated the main effects of the selected demographic variable of race and barrier reduction interventions (phase; phase 1: cohort admissions; phase 2: rolling admissions; phase 3: rolling admissions plus meal incentives) as well as their interaction on youth treatment engagement, retention, and completion rates. We then repeated this analysis replacing insurance as the demographic variable. All assumptions of ANOVA were met in our dataset.
Youth (N = 110) who qualified for American Society of Addiction Medicine (ASAM) 2.1 level of care (9) and were referred to the STEP IOP are included in this study. Participants ranged in age from 13 to 17 (M = 15.61, SD = 1.31). Approximately half of youth identified as racially diverse (50.9%; 40.0% Latinx, 3.6% Black, 0.9% American Indian or Alaska Native, and 6.4% two or more races), with the other 49.1% identifying as White. A total of 67 of 110 (60.9%) youth either had state-funded Medicaid or no insurance. Of the youth that engaged in treatment across each phase of implementation, 68.7% were provided with transportation assistance. Participants identified as cisgender males (65.5%), cisgender females (28.2%), transgender (3.6%), and non-binary (2.7%). For all included demographic variables separated by treatment engagement, see Table 1.
Descriptively, of the 110 youth referred for the tested treatment program, most were referred in phase 3 (n = 51), followed by phase 1 (n = 38), and phase 2 (n = 21). No differences emerged in terms of youth racial identity [F (2,107) = 0.47, p = .627, η2 = .009] nor insurance coverage [F (2,107) = 0.41, p = .668, η2 = .008] based on the phase of referral. Separated by phase, 42.1% of youth referred in phase 1 started treatment and 15.8% completed; 47.6% of youth referred in phase 2 started treatment and 14.3% completed; and 80.4% of youth referred in phase 3 started treatment and 31.4% completed. Bivariate correlations between engagement, retention, and completion rates are displayed in Table 2.
In line with our goal of improving access to care for all youth, results illustrated no differences in treatment engagement [F (1,104) = 3.16, p = .079, η2 = .029], retention [F (1,85) = 0.67, p = .417, η2 = .008], nor completion [F (1,59) = 0.04, p = .840, η2 = .001] based on race. In other words, youth of color and White youth were just as likely to start treatment, stay in treatment, and complete treatment. Similarly, no differences in engagement [F (1,104) = 1.56, p = .214, η2 = .015], retention [F (1,85) = 0.80, p = .375, η2 = .009], nor completion [F (1,59) = 0.17, p = .683, η2 = .003] emerged between those with private insurance and those with state funded Medicaid or no insurance.
When investigating the interaction between these selected demographic variables and the implementation of interventions to reduce barriers (phase), we found similar findings. Specifically, results showed no significant interaction effect between phase and race for engagement [F (2,104) = 0.76, p = .470, η2 = .014] nor retention [F (2,85) = 1.90, p = .156, η2 = .043]. Similarly, when looking at insurance, no significant interaction effects emerged for engagement [F (2,104) = 2.23, p = .112, η2 = .041], retention [F (2,85) = 0.01, p = .988, η2 = .000], nor completion [F (2,59) = 0.32, p = .731, η2 = .011]. On the contrary, results illustrated a significant interaction between race and phase on completion rates [F (2,59) = 6.22, p = .004, η2 = .174] such that youth of color who participated in IOP during phase 3 were significantly more likely to graduate [F (2,34) = 6.71, p = .004, η2 = .283] than youth of color who participated during phase 2 specifically (Mdiff = 0.59, SE = 1.77, p = .006, 95% CI = 0.14–1.03), whereas there was no significant difference in graduation between phases for White participants [F (2,25) = 1.41, p = .264, η2 = .101]. See Figure 1 for a visual of these interaction effects.
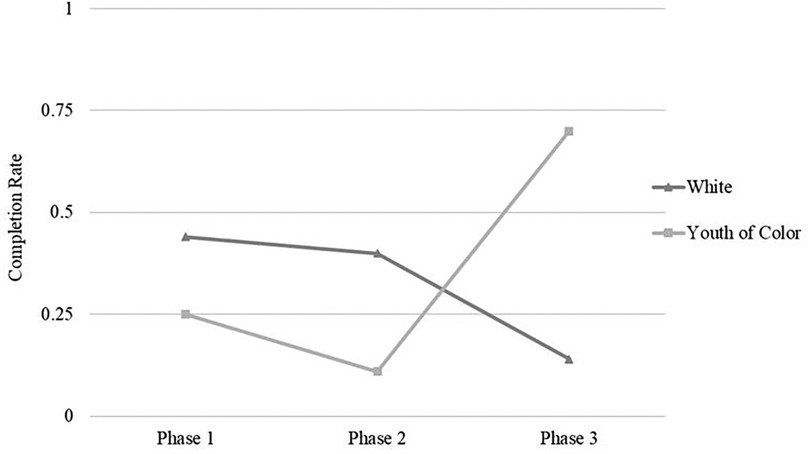
Figure 1. Interaction effect of race and phase on treatment completion. The rates of completion varied from 0 to 1. There is a significant difference between treatment completion rates at phase 2 and phase 3 for youth of color. All other comparisons are non-significant.
While we did not anticipate interaction effects due to our implementation of barrier reduction interventions at all phases of treatment, we proposed that youth would be more likely to start treatment, stay in treatment, and complete treatment as additional interventions to reduce barriers to care were implemented. Accordingly, we found significant differences in engagement [F (2, 104) = 8.18, p < .001, η2 = .136] and retention [F (2,85) = 9.32, p < .001, η2 = .180] based on implemented interventions to reduce barriers (see Figure 2). Specifically, results identified phase 3 of treatment in which participating youth were provided transportation assistance and meal incentives and accepted into treatment on a rolling basis to be related to significantly higher rates of engagement as compared to phase 2 of treatment in which rolling admissions were implemented with transportation assistance (Mdiff = 0.33, SE = 0.12, p = .021, 95% CI = 0.04–0.62) and phase 1 of treatment which followed a cohort model with transportation assistance (Mdiff = 0.37, SE = 0.10, p < .001, 95% CI = 0.13–0.61). Phase 3 of treatment was also related to higher retention rates as compared to phase 1 specifically (Mdiff = 5.90, SE = 1.37, p < .001, 95% CI = 2.55–9.24). No significant differences in treatment completion rates emerged based on phase [F (2,59) = 0.66, p = .52, η2 = .022].
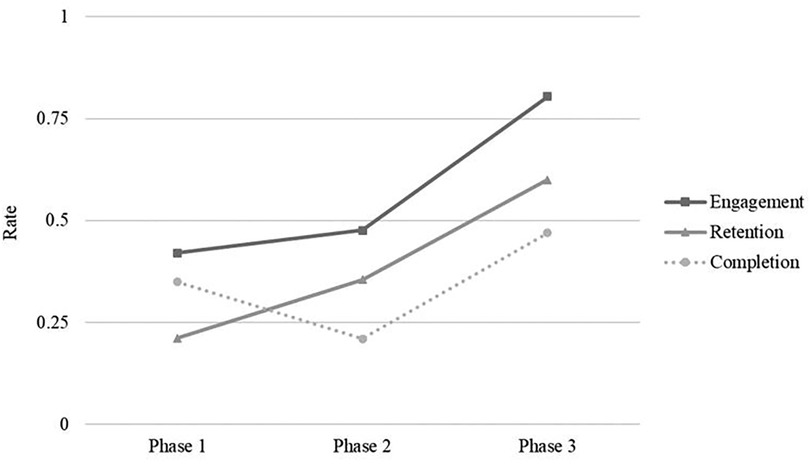
Figure 2. Engagement, retention, and completion rates by phase of enrollment. Treatment retention rates were scaled to match the dichotomous scoring of treatment engagement and treatment completion; all rates displayed range from 0 to 1.
Given the discrepancies in treatment engagement, retention, and completion between racially and ethnically minoritized youth and their White counterparts (3, 4, 15), as well as the documented barriers to treatment (5, 6), we sought to investigate methods for decreasing barriers and increasing access to treatment and their effect on these variables. As hypothesized, this evaluation showed no significant differences in treatment engagement, retention, and completion based on selected youth demographic variables (i.e., race and insurance coverage). We also found no significant interaction effects between phase and race for engagement and retention, as well as between phase and insurance coverage for engagement, retention, and completion. Unexpectedly, a significant interaction effect was found between phase and race on treatment completion such that youth of color who participated with all three barrier reduction interventions implemented (phase 3) were significantly more likely to complete treatment than those who participated during phase 2.
Regarding the role of barrier reduction interventions in increasing engagement, retention, and completion for all youth, we found partial support for our hypothesis when evaluating the sample as a whole. Specifically, phase 3 of treatment was related to significantly higher rates of engagement and retention, in comparison to phase 1 and 2. However, there was no significant difference between treatment engagement, retention, and completion for phase 1 and 2, and no significant differences in completion rates between any of the implemented phases.
Taken together, youth of color and youth with state-funded Medicaid or no insurance started, stayed in, and completed treatment just as much as their White and private or commercially insured peers, respectively. The introduction of new barrier reduction interventions at each phase did not increase treatment engagement or retention for youth of color in comparison to their White counterparts, but it did significantly increase their likelihood of treatment completion. Lastly, White youth and youth of color alike were more likely to start and stay in treatment in phase 3, as compared to phases 1 and 2, when all three barrier reduction interventions (e.g., transportation assistance, rolling admissions, and meal incentives) were present, but they were not more likely to complete treatment.
Results provided support that when interventions aimed at reducing barriers are implemented within an intensive outpatient treatment program, discrepancies in treatment engagement, retention, and completion between youth of color and White youth will diminish. Analyses found that rates of treatment engagement, retention, and completion were comparable across races, suggesting that youth of color were just as likely to start treatment, stay in treatment, and complete treatment as White youth. Similar results were found when comparing socioeconomic variables (e.g., Medicaid and no insurance vs. commercially insured youth). This is important given that previous research has shown that racially and ethnically minoritized youth engage in treatment less and have a higher likelihood of dropping out of treatment than their White counterparts (3, 4, 15). The notable difference between this past research and our research presented here may suggest that treatments that incorporate interventions aimed at reducing barriers have potential to eliminate discrepancies in treatment engagement and retention between minoritized youth and their White counterparts. In other words, the lack of significant differences in engagement, retention, and completion between groups suggest that implementing barrier reduction interventions level the playing field for youth from racially and ethnically marginalized and low-SES backgrounds and promotes equitable access to treatment for these groups of youth who have historically had less access to care. Thus, given our results, coupled with previous research that has shown that youth of color start and stay in treatment at a lower rate than White youth (3, 4, 15), it is imperative to note that it is not that racial and ethnic minority youth do not engage in treatment or are not receptive to treatment, but that systemic variables significantly and negatively impact socially and economically disadvantaged youths' ability to engage and remain in treatment.
Indeed, it is difficult to definitively assert that it is due to these barrier reduction interventions that discrepancies in treatment engagement, retention, and completion diminish because we do not have baseline data for these variables without any barrier reduction intervention. However, because barrier reduction interventions were present across all phases of implementation, which is the most defining characteristic of this IOP that separates it from other treatment programs, it is reasonable to conclude that no significant differences in treatment engagement, retention, and completion between groups is attributable to these barrier reduction interventions. Baseline data for these variables without barrier reduction interventions would be important for future research.
In terms of efforts to reduce barriers, given the lack of differences we found in engagement, retention, and completion based on selected demographic variables that have been repeatedly supported in past research (3, 4, 15), it is possible that the addition of transportation assistance alone increased access and reduced barriers to where all youth were able to access services similarly. This is just a prediction and needs to be further tested in future research as this evaluation did not test phase 1 against a no barrier reduction intervention control hindering our ability to draw conclusions on the unique contribution of transportation assistance in increasing access.
Furthermore, results highlight the combination of transportation assistance, rolling admission, and meal incentives to be related to higher rates of engagement and retention. Overall, our results seem to suggest that the implementation of all three barrier reduction interventions in unison significantly improved engagement and retention as compared to transportation assistance alone (phase 1) or when paired with rolling admission (phase 2). Additionally, for youth of color, specifically, completion rates increased significantly in phase 3 as compared to phase 2 further suggesting a benefit of this combined intervention approach to reduce barriers. However, notably, this evaluation was unable to separately test each barrier reduction intervention due to the nature of being a quality improvement project. Therefore, it could be that meal incentives are a strong intervention alone driving the statistical difference between phase 1, phase 2, and phase 3. Alternatively, it could be that it is these three interventions in combination that is responsible for increased engagement and retention. Further investigation of the unique contribution of these barrier reduction interventions is an important avenue for future research.
Although we found significantly higher rates of engagement and retention in participants referred for phase 3, we did not see a significant difference in completion rates between phases of treatment. If youth are more likely to start treatment and stay in treatment in phase 3, it is logical that youth would be more likely to complete treatment as well. This was partially supported by our finding that youth of color were more likely to complete treatment in phase 3 than in phase 2. Furthermore, descriptively, 31.4% of youth in phase 3 completed treatment as compared to the 15.8% and the 14.3% who completed treatment in phase 1 and phase 2, respectively. Therefore, it may be that based on dropout rates, our sample size for youth completing treatment was too small to properly assess differences between phases. Indeed, with only 25 out of 110 participants completing treatment, these analyses are underpowered which could result in an over-estimation or an underestimation of the significance of effects (16). Therefore, this is another avenue for continued research.
In addition to the detailed limitations of our research including our small sample size and lack of randomized control, our study has many notable strengths. While our sample is small, it is highly diverse with over 50% of youth identifying as multicultural and over 60% of youth either having state-funded Medicaid or no insurance. Given our aim of understanding the role of barrier reduction interventions in increasing engagement, retention, and completion of treatment for diverse and traditionally underserved youth, the racial and socioeconomic representation in our sample is key. Additionally, we were able to compare three unique phases of implementation and investigate youth's ability to access care throughout treatment. By following youth throughout treatment, we were able to see how these individual aspects of treatment are impacted. Specifically, though youth are more likely to start and continue treatment with barrier reduction interventions, they are no more likely to complete treatment. While more research is needed in this area due to power limitations, if future research replicates this finding, it will be important to develop additional strategies to aid in completion of treatment specifically. Furthermore, the pragmatic nature of this evaluation also adds some increased generalizability as compared to some randomized, controlled research designs.
These data have several important implications for policy, practice, and equity. First, these data support the use of specific barrier reduction and treatment access facilitating interventions, such as transportation, meal incentives, and rolling admissions, in increasing engagement and retention in intensive outpatient programming for low-SES and racial and ethnic minority youth. This finding is important because youth of color have historically had less access to treatment and higher rates of treatment dropout compared to White youth (3, 4, 15). Programs intentionally addressing barriers to care is one way of addressing systemic factors that inhibit equitable access to health and mental healthcare. Second, providing interventions aimed at reducing barriers to care may eliminate health disparities in engaging in higher-level care substance treatment. Specifically, addressing barriers and facilitating access to care may help non-White youth engage in and remain in care. Lastly, these data have important research implications. While this study demonstrated that interventions aimed at reducing barriers to care can eliminate disparities in treatment engagement and retention between racially and ethnically minoritized youth and their White peers, this study did not investigate treatment outcomes related to changes in individual functioning. Therefore, an important next step would be to evaluate treatment outcomes and therapeutic intervention effects for adolescents in intensive outpatient programming.
Overall, our results suggest a combination of barrier reduction interventions (transportation assistance, rolling admissions, and meal incentives) as a promising avenue for decreasing barriers and increasing access to higher-level substance use treatment for diverse and traditionally underserved youth. From this research, continued exploration of the unique effects of different barrier reduction interventions are necessary. Furthermore, while these efforts were related to higher rates of engagement and retention, they were not related to differential rates of treatment completion and completion rates overall remained low. Therefore, continued efforts as well as novel strategies to reduce barriers, increase access, and specifically increase likelihood of treatment completion are necessary. Nonetheless, this evaluation presents promising pilot data that justifies the necessity for further investigation on barriers and facilitating access to treatment to better understand how we can best promote health equity for adolescents needing treatment for substance use disorders.
The datasets presented in this article are not readily available because the dataset includes protected health information. Requests to access the datasets should be directed toZWlsZWVuLmNoZW5AZGhoYS5vcmc=.
The studies involving humans were approved by Colorado Multiple Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The Ethics Committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because this was a quality improvement project that involved a retrospective review of electronic health records. Participants were adolescent patients in an outpatient substance use treatment program consenting to their own treatment and data collected were collected as part of routine clinical care.
EC: Conceptualization, Data curation, Investigation, Methodology, Project administration, Resources, Software, Supervision, Visualization, Writing – original draft, Writing – review & editing. HS: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. CT: Funding acquisition, Supervision, Writing – review & editing, Conceptualization.
The authors declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Reinert M, Fritze D, and Nguyen T. (2022). The State of Mental Health in America 2023. Alexandria VA: Mental Health America.
2. Reinert M, Fritze D, and Nguyen T. (2021). The State of Mental Health in America 2022. Alexandria VA: Mental Health America.
3. Lu W, Xu L, Goodwin RD, Muñoz-Laboy M, and Sohler N. (2023). Widening gaps and disparities in the treatment of adolescent alcohol and drug use disorders. Am J Prev Med 64 (5), 704–15. doi: 10.1016/j.amepre.2023.01.036
4. Saloner B, Carson N, and Cook BL. (2014). Explaining racial/ethnic differences in adolescent substance abuse treatment completion in the United States: a decomposition analysis. J Adolesc Health 54 (6), 646–53. doi: 10.1016/j.jadohealth.2014.01.002
5. Lu W, Todhunter-Reid A, Mitsdarffer ML, Munoz-Laboy M, Yoon AS, and Xu L. (2021). Barriers and facilitators for mental health service use among racial/ethnic minority adolescents: a systematic review of literature. Front Public Health 9, 1–16. doi: 10.3389/fpubh.2021.641605
6. Acevedo A, Harvey N, Kamanu M, Tendulkar S, and Fleary S. (2020). Barriers, facilitators, and disparities in retention for adolescents in treatment for substance use disorders: a qualitative study with treatment providers. Subst Abuse Treat Prev Policy 15 (42), 1–13. doi: 10.1186/s13011-020-00284-4
7. Keene JR, and Batson CD. (2010). Under one roof: a review of research on intergenerational coresidence and multigenerational households in the United States. Sociol Compass 4, 642–57. doi: 10.1111/j.1751-9020.2010.00306.x
8. Leffler JM, and D'Angelo EJ. (2020). Implementing evidence-based treatments for youth in acute and intensive treatment settings. J Cogn Psychother 34 (3), 185–99. doi: 10.1891/JCPSY-D-20-00018
9. Mee-Lee D. (2013). The ASAM Criteria: Treatment Criteria for Addictive, Substance-Related, and Co-Occurring Conditions. 3rd ed. Carson City, NV: Change Companies.
10. Thurstone C, Hull M, Timmerman J, and Emrick C. (2017). Development of a motivational interviewing/acceptance and commitment therapy model for adolescent substance us treatment. J Contextual Behav Sci 6 (4), 375–9. doi: 10.1016/j.jcbs.2017.08.005
11. Hayes L, and Ciarrochi J. (2015). The Thriving Adolescent: Using ACT and Positive Psychology to Help Teens Manage Emotions, Achieve Goals, and Build Connection. California: Context Press.
12. DeRosa R, Habib M, Pelcovitz D, Rathus J, Sonnenklar J, Ford J, et al. (2006). Structured Psychotherapy for Adolescents Responding to Chronic Stress (SPARCS): A Trauma-Focused Guide. New York: North Shore University Hospital.
13. Seely HD, and Mickelson KD. (2021). Role of gender and emotionality stigma in perceived parental emotion dysregulation and adult children’s internalizing symptoms. Sex Roles 85, 515–27. doi: 10.1007/s11199-021-01237-2
14. Petry NM, Peirce JM, Stitzer ML, Blaine J, Roll JM, Cohen A, et al. (2005). Effect of prize-based incentives on outcomes in stimulant abusers in outpatient psychosocial treatment programs. Arch Gen Psychiatry 62 (10), 1148–56. doi: 10.1001/archpsyc.62.10.1148
15. Thurstone C, Loh R, O’Leary S, Bruce S, and Ladegard K. (2023). School-based services may eliminate substance treatment disparities: results from a nonrandomized program evaluation. J Sch Health 94 (3), 267–72. doi: 10.1111/josh.13413
Keywords: adolescents, substance use treatment, treatment engagement, barriers to treatment, intensive outpatient, access to care, health equity, social determinants of health
Citation: Chen E, Seely HD and Thurstone C (2024) Reducing barriers to promote engagement and retention in adolescent substance use treatment: results from a quality improvement evaluation. Front. Child Adolesc. Psychiatry 3:1393401. doi: 10.3389/frcha.2024.1393401
Received: 29 February 2024; Accepted: 21 May 2024;
Published: 5 June 2024.
Edited by:
Amy Yule, Boston Medical Center, United StatesReviewed by:
Colin Burke, Massachusetts General Hospital and Harvard Medical School, United States© 2024 Chen, Seely and Thurstone. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Eileen Chen, ZWlsZWVuLmNoZW5AZGhoYS5vcmc=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.