- 1Virginia Tech Autism Clinic & Center for Autism Research, Virginia Tech, Blacksburg, VA, United States
- 2Human Nutrition, Foods, and Exercise, Virginia Tech, Blacksburg, VA, United States
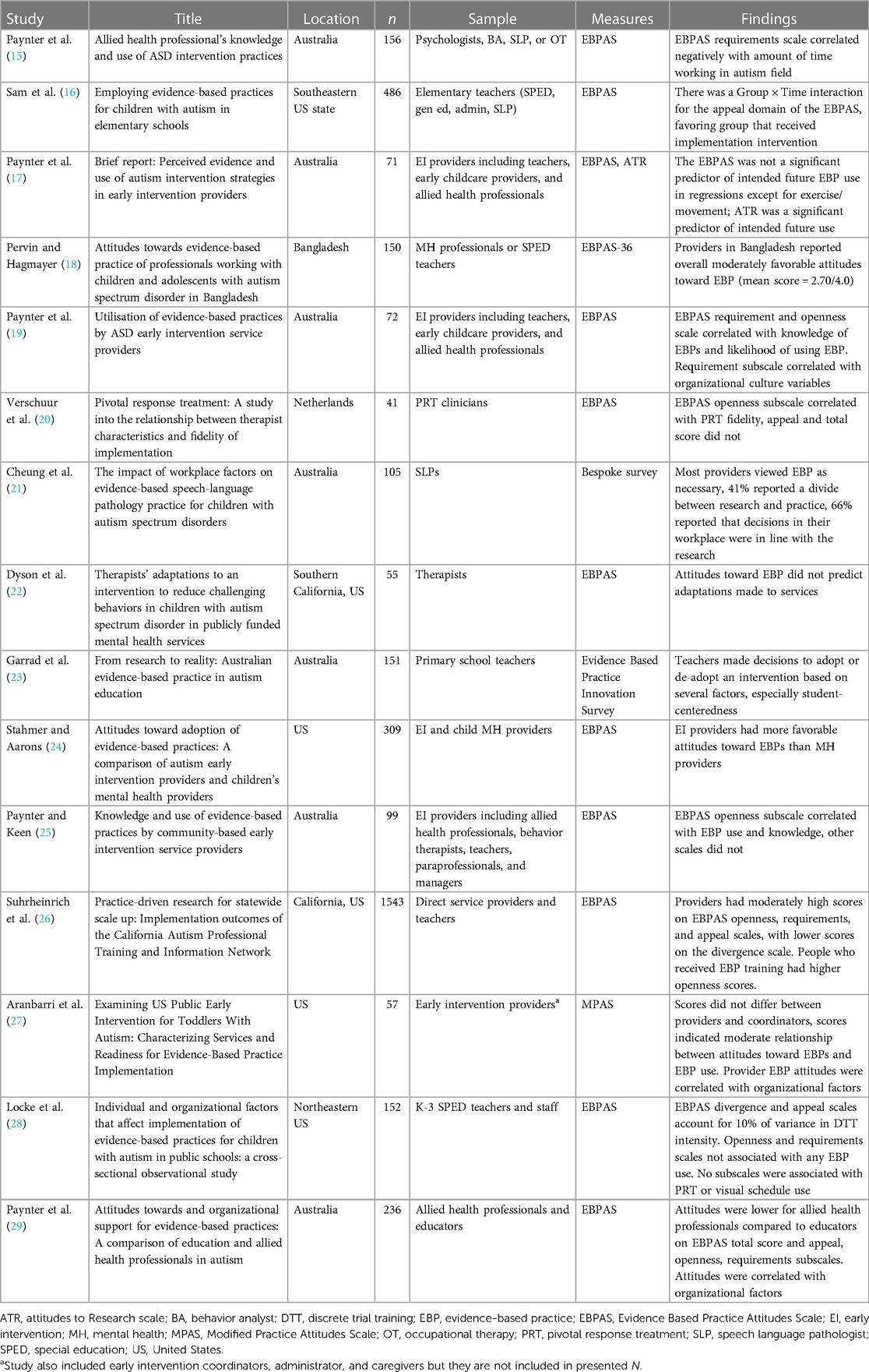
There are many established evidence-based practices (EBPs) for autistic youth which facilitate wellbeing and skill development across a range of domains. However, individuals on the autism spectrum are consistently underserved in mental health settings, limiting their access to these EBPs. Positive provider attitudes toward EBPs may increase their uptake or use. The current mini-review seeks to synthesize the literature regarding attitudes toward EBPs among providers working with autistic youth across a variety of settings (i.e., school, early intervention, and general mental health). Fifteen quantitative studies were included. The majority of studies (n = 13, 87%) utilized the Evidence Based Practice Attitudes Scale (EBPAS) or a variation of this scale. Attitudes toward EBPs were primarily used as a correlate or covariate, although some studies reported descriptive statistics of provider attitudes. When available, the reported results suggest that attitudes toward EBPs are moderately positive at baseline, although they vary between provider types. Two studies (13%) examined change in attitudes toward EBPs and suggested that they may be responsive to intervention. However, findings were mixed as to whether attitudes toward EBPs are predictive of EBP use/uptake. Implications and future directions are discussed.
1 Introduction
A variety of evidence-based practices (EBPs) have been established to improve outcomes for autistic youth across domains such as mental health, communication, interfering behaviors, adaptive behavior, and social skills (1). Despite the existence of such EBPs, youth on the autism spectrum are continuously underserved in behavioral health and educational settings. Autistic youth face significant barriers to evidence-based healthcare at the provider, organizational, and systemic levels (2). As a result, scholars in the field of autism research have made repeated calls to utilize dissemination and implementation science (DIS) to integrate existing EBPs into settings such as behavioral/mental health clinics, early intervention providers, and schools (3, 4).
While DIS often focuses on organizational level factors to increase uptake of EBPs, some literature has identified individual provider characteristics that are likely to be important to EBP implementation in autism, such as previous training and motivation (5), buy-in and beliefs about own capabilities, and beliefs about program outcomes (6). More work is needed to fully understand the role that provider characteristics may play in adoption, implementation, and sustainment processes. However, both theory and empirical evidence from related fields suggest that provider characteristics are likely to play a role in the improved implementation of EBPs for autistic individuals. The theory of planned behavior [TPB (7)] suggests that individual attitudes, subjective norms, and perceived behavioral control all influence individual intention to act, which in turn influences individual behavior. Applied to DIS, the TPB posits that attitudes toward EBPs should influence provider intention to conduct EBPs, which in turn should influence a provider's behavior of implementing an evidence-based approach.
This theoretical frame appears to be supported by the general literature regarding implementation of an innovation as well as the mental health EBP literature. In the business literature, Frambach and Schillewaert (8) identify that individual attitudes play a role in the adoption of new innovative practices, and Candel and Pennings (9) suggest that the affective component of attitudes is predictive of choosing to implement innovations. In the mental health literature, a study of providers found that attitudes toward specific EBPs were correlated with the degree to which providers used that practice (10). Attitudes toward EBPs are also associated with uptake of components of mental health EBPs such as consultation (11) and routine outcome assessment following a training (12). Attitudes toward research, a closely related concept to attitudes toward EBPs, are also predictive of self-reported EBP use among mental health clinicians (13).
2 Research strategy
Despite a robust extant literature on the TPB and attitudes toward EBPs in general, no work has synthesized the literature regarding attitudes toward EBPs in providers working with autistic youth. As such, the current review sought to describe and integrate the literature regarding attitudes toward EBPs among providers, including educators and behavioral or allied health professionals, who work with autistic children and adolescents. The aims of this mini-review are twofold: (1) To characterize and synthesize attitudes toward EBPs among providers who work with autistic youth and (2) to consider key correlates, predictors, and/or outcomes related to EBP attitudes for autism providers.
Studies were included in the current review if they (1) included a measure of provider attitudes toward behavioral health EBPs; (2) included a sample of educators, other school providers, behavioral health providers, or allied health professionals (e.g., occupational therapists), and (3) included a sample of providers working with autistic individuals at least part of the time.
The databases PsycInfo and PubMed were searched in April and May 2023 for terms related to autism, evidence-based practice, attitudes/beliefs, and providers/clinicians/educators. Search terms included: autism, autis*, ASD, autism spectrum disorder, Asperger's, PDD-NOS, attitudes, beliefs, perceptions, opinions, evidence based practice, evidence-based practice, EBP, evidence based treatment, EBT, evidence based, best practice, evidence based intervention, EBI, clinician, teacher, therapist, educator, and provider. Studies meeting the inclusion criteria were retained for synthesis. The Covidence review software was utilized to aid in organization of included studies (14). This search should not be considered exhaustive. Rather, results are intended to provide a broad overview of the scope of the existing literature in order to inform future research on the topic. The search yielded 15 studies, which are included in the current review.
3 Results
Refer to Table 1 for details of the following results (15–29).
3.1 Location and demographics
Seven studies (47%) took place in Australia while six (40%) took place in the United States. One study each took place in Bangladesh (7%) and the Netherlands (7%). Eleven studies reported participant gender; all of these samples were predominately female. Five studies reported participant race; 80% of these included predominately white participants. Mean age ranged from 30.5 (18) to 44.6 (27) among the six studies that reported average age (six additional studies reported age range breakdowns).
3.2 Setting/provider types
3,683 providers were participants in the research. Most of these providers participated in studies which included both school and behavioral health providers. 11% of participants were in studies which only included providers in behavioral health and allied health settings, and 21% of providers were in studies that exclusively investigated school provider attitudes.
3.3 Measurement strategy
Most studies (87%) utilized the Evidence Based Practice Attitudes Scale [EBPAS (30)] either in its original form (73%) or an adaptation (13%; the EBPAS-36 or the Modified Practice Attitudes Scale, MPAS). The EBPAS is a 15-item measure of provider attitudes toward EBPs. It includes four subscales rated on a scale of 0–4: Requirements (i.e., likelihood of using an EBP if it was required by your organization); Appeal (i.e., likelihood of using an EBP if it is intuitively appealing); Openness (i.e., general open-mindedness to using an EBP) and Divergence (i.e., amount that EBPs diverge or are different from your current practices). The EBPAS-36 (31) is a 36-item form of the measure, and the Modified Practice Attitudes Scale [MPAS (32)] is an 8-item version. Paynter et al. (17) utilized the EBPAS as well as the Attitude To Research Scale [ATR (33)]. The two remaining studies used other questionnaire/survey measures, including the Evidence Based Practice Innovation Survey [EBPIAS (23)] which assesses factors involved in EBP decision making among teachers, and a measure of EBP attitudes, knowledge, and training (21, 34).
3.4 Overall attitudes toward EBPs
Most studies did not explicitly report descriptive statistics on EBP attitudes and primarily reported provider attitudes as a covariate or correlate of the likelihood of using EBPs (17, 19, 25), fidelity to EBPs (20) or adaptations to EBPs (22). In studies that did report overall EBP attitudes, attitudes were reported as moderately positive. Average scores ranged from 2.99 to 3.32 out of 4 for all EBPAS subscales except divergence reported in Suhrheinrich et al. (26) Also, EBPAS average score was reported as 2.7 in Pervin and Hagmayer (18).
3.5 Group differences in attitudes
Three studies (20%) compared EBP attitudes among provider types. Two of these studies found significant group differences. Autism early intervention providers had more positive EBP attitudes than mental health clinicians working in the United States (24). Additionally, in a study of 261 Australian educators and allied health providers, allied health professionals demonstrated less positive EBP attitudes than did educators (29). In a comparison of early intervention providers and coordinators, there were no group differences on attitudes toward EBPs (27).
3.6 Attitudes as a predictor of EBP use
Overall, findings were mixed with respect to the utility of EBP attitudes as a predictor/correlate of outcomes. Several studies identified an association between attitudes and EBP use/fidelity. For example, in a study of early intervention providers in Australia, the Requirement and Openness subscales of the EBPAS were correlated with overall likelihood of using EBPs (19). Another study from the same research team found that in a sample of 99 early intervention providers, the Openness subscale was associated with EBP use and knowledge, while other EBPAS scales did not correlate with EBP use (25). Paynter et al. also investigated the EBPAS's predictive value for the use of several specific EBPs among early intervention clinicians; they found that the EBPAS predicted future use of exercise, an EBP for autistic youth, but did not predict the future use of other EBPs (17). A study of 153 K-3 special education teachers and staff in the northeastern United States found that the Divergence and Appeal subscales of the EBPAS accounted for 10% of the variance in use of discrete trial training (28).
On the other hand, several studies also presented null findings with respect to the association between attitudes and EBP use. Dyson et al. (22) found no association between EBP attitudes and the likelihood of making adaptations to an EBP for autistic youth. Although Locke et al. (28) found a positive association between EBP attitudes and discrete trial training, they noted that there was no association between the EBPAS and use of two other autism EBPs (pivotal response treatment and visual schedules). Furthermore, for many of the studies discussed, particular subscales/components of EBP attitudes were most associated with outcomes, rather than an association between outcomes and a provider's overall EBP attitudes.
3.7 Altering attitudes toward EBPs
Two studies investigated whether intervention could change individual provider attitudes toward EBPs. These interventions included approaches such as training, goal setting, and coaching/feedback, and attitudes toward EBPs improved when these DIS interventions were implemented. For example, Sam et al. (16) conducted a study in which schools were assigned to a professional development model called the National Professional Development Center (NPDC) or to services as usual. Schools in the NPDC condition used a four-part process which included focus on overall classroom quality, designation of measurable student goals, matching student goals with appropriate EBPs, and coaching/feedback. The authors found a group by time interaction effect on the appeal domain of the EBPAS, such that attitudes toward intuitively appealing EBPs improved from pre-test to post-test, only for the NPDC condition. Another study investigated EBP attitudes in providers who had vs. had not participated in the California Autism Professional Training and Implementation Network [CAPTAIN (26)]. CAPTAIN is a network designed to develop dissemination plans and provide training on EBPs throughout California. Results indicated that individuals who had attended CAPTAIN training displayed higher levels of Openness on the EBPAS, indicating more willingness to implement EBPs into their practice, relative to the control group.
4 Discussion
The included studies suggest a mixed literature regarding autism provider attitudes toward EBPs. However, they provide some evidence for the importance of attitudes as an implementation factor, consistent with both the TPB and existing DIS frameworks. Overall, the reviewed literature suggests that autism providers have moderately positive attitudes toward EBPs, although there is room for improving attitudes. Interestingly, the vast majority (87%) of included studies used a version of the EBPAS to measure attitudes. Future psychometric research would do well to evaluate the use of this measure specifically with autism providers, to better understand how the measure applies for this population. Additionally, there is some evidence that attitudes toward EBPs are malleable in the two studies that examined interventions, with improved attitudes after DIS strategies including feedback, training, and goal setting (16, 26). This finding is encouraging, as it suggests that there is potential for modifying EBP attitudes through intervention.
Another important question to consider, then, is whether attitudes are a meaningful construct in terms of predicting EBP use/fidelity in providers working with autistic youth. DIS researchers identify intervention acceptability and appropriateness, concepts closely related to attitudes, as key implementation outcomes (35–37), suggesting their importance in implementation success. Within the autism literature specifically, qualitative research has suggested that providers perceive EBP attitudes (at the provider and leadership level) as important in influencing implementation (38). Several studies in the current review supported this idea, finding that EBP attitudes are correlated with EBP use (17, 19, 25, 28), and one study identified an association between EBP attitudes and implementation fidelity (20). Yet, other studies found no association between attitudes and EBP use (17, 22, 28). There was considerable variability in the settings and types of autism providers involved in the studies, which could explain the range of findings. Overall, the present review highlights that while EBP attitudes have promise as a predictor of implementation outcomes, there is an overall lack of consensus in the literature regarding the impact of provider EBP attitudes. While the wider literature has established that leadership and organizational factors are key to implementing EBPs in autism practice (38–40), this review underscores the need for further research to clarify the mixed landscape regarding individual provider attitudes toward EBPs.
It is also important to consider the variety of practices which fall under the EBP umbrella in the autism literature. DIS has firmly established the importance of contextual factors when implementing interventions (41–44), and a wide range of contexts are at play in autism intervention due to the interdisciplinary nature of autism services. In recent years, the COVID-19 pandemic has resulted in a shift to telehealth services for many health professionals, including those who work with autistic individuals (45–47). The impact of this contextual factor on providers' attitudes toward EBPs is not well understood, and future research should investigate this further. Gabellone et al. (46) developed a questionnaire examining provider attitudes toward using telehealth with autistic patients; this measure may provide a useful starting point to consider provider attitudes toward conducting EBPs over telehealth.
Additionally, attitudes toward EBPs as a broad construct may be significantly different than attitudes toward an individual EBP. The clearest example of this possibility is applied behavioral analysis (ABA), an umbrella term which can encompass a range of autism EBPs. ABA has been subject to increasing scrutiny over the last decade, with many autistic individuals arguing that the outcomes ABA seeks to create are akin to “normalization” of autistic people and do not target factors that are most important to autistic individuals themselves (48). This perspective highlights an important consideration within the context of the current review: there is substantial heterogeneity in the outcomes targeted in autism EBPs. Such variability highlights the importance of using participatory designs that consider autistic perspectives when conducting future research on attitudes toward and use of EBPs.
4.1 Implications for implementation science
The present review has implications for implementation science in general and within the autism field. Given the emerging evidence provided here for malleability of attitudes, it is recommended that implementation scientists consider implementation strategies, such as those identified by Powell et al. (49) (e.g., educational outreach, local consensus discussions, providing ongoing consultation) with the explicit goal of altering attitudes toward EBPs in general and toward specific EBPs. This work can subsequently measure downstream effects on adoption decisions, implementation, and sustainment. If effective, using DIS strategies to alter attitudes may serve to decrease translational lag time and ultimately improve access to services.
The process of changing attitudes should be done in collaboration with the community, preferably through participatory research (50, 51). In addition to including autistic individuals in research partnerships, it may also be beneficial to include caregivers for autistic people, given that many EBPs include a family-mediated approach (1). Models such as the integrated research-practice partnership process model (52) may aid in this approach. In addition, applying a health equity lens to existing frameworks, as described by Fort et al. (53) may prove important particularly for historically underserved populations. When considering attitudes, it is critically important for implementation scientists to consider the role and perception of researchers by the community. Partnering with community groups is therefore a necessary step. As such, the implementation strategy of identifying champions (46) may prove useful, particularly if attitudes are to be targeted.
It is further recommended that implementation scientists also consider provider attitudes toward a specific EBP to determine whether modifying attitudes toward a particular approach changes uptake. General mental health literature suggests that EBP attitudes can vary by EBP type (10). In the short term, implementation scientists should consider measuring both attitudes toward EBPs broadly as well as attitudes toward a specific EBP, in order to clarify the role that attitudes toward EBPs broadly and attitudes toward specific practices play in the implementation process [e.g., Kemp et al. (54)].
5 Conclusion
The current review offers a synthesis of existing literature regarding attitudes to EBPs among autism providers and suggests several future research directions. Overall, EBPs are generally viewed favorably, though attitudes may differ by provider type, and the research is mixed on whether EBP attitudes impact uptake by autism providers. Future implementation science, ideally with participatory research designs, should continue to consider autism provider EBP attitudes and the factors that influence their impact on EBP use with autistic youth.
Author contributions
ED: Conceptualization, Writing – original draft, Writing – review & editing. SH: Supervision, Writing – review & editing. AS: Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article.
Open access publication of this article was supported by the Virginia Tech Center for Autism Research and the Virginia Tech Department of Human Nutrition, Foods, and Exercise.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Steinbrenner JR, Hume K, Odom SL, Morin KL, Nowell SW, Tomaszewski B, et al. Evidence-Based Practices for Children, Youth, and Young Adults with Autism. Chapel Hill, NC: FPG Child Development Institute (2020).
2. Vohra R, Madhavan S, Sambamoorthi U, St Peter C. Access to services, quality of care, and family impact for children with autism, other developmental disabilities, and other mental health conditions. Autism. (2014) 18(7):815–26. doi: 10.1177/1362361313512902
3. Boyd BA, Stahmer AC, Odom SL, Wallisch A, Matheis M. It’s time to close the research to practice gap in autism: the need for implementation science. Autism. (2022) 26(3):569–74. doi: 10.1177/13623613211064422
4. Odom SL, Hall LJ, Suhrheinrich J. Implementation science, behavior analysis, and supporting evidence-based practices for individuals with autism. Eur J Behav Anal. (2020) 21(1):55–73. doi: 10.1080/15021149.2019.1641952
5. Brookman-Frazee L, Chlebowski C, Suhrheinrich J, Finn N, Dickson KS, Aarons GA, et al. Characterizing shared and unique implementation influences in two community services systems for autism: applying the EPIS framework to two large-scale autism intervention community effectiveness trials. Adm Policy Ment Health Ment Health Serv Res. (2020) 47:176–87. doi: 10.1007/s10488-019-00931-4
6. Carruthers S, Mleczko N, Page S, Ahuja S, Ellis C, Howlin P, et al. Using implementation science frameworks to explore barriers and facilitators for parents’ use of therapeutic strategies following a parent-mediated autism intervention. Autism. (2023) 27(4):1011–25. doi: 10.1177/13623613221125630
7. Ajzen I. From intentions to actions: a theory of planned behavior. In: Kuhl J, Beckmann J, editors. Action Control: From Cognition to Behavior. Berlin, Heidelberg: Springer (1985). p. 11–39. doi: 10.1007/978-3-642-69746-3_2
8. Frambach RT, Schillewaert N. Organizational innovation adoption: a multi-level framework of determinants and opportunities for future research. J Bus Res. (2002) 55(2):163–76. doi: 10.1016/s0148-2963(00)00152-1
9. Candel MJ, Pennings JM. Attitude-based models for binary choices: a test for choices involving an innovation. J Econ Psychol. (1999) 20(5):547–69. doi: 10.1016/s0167-4870(99)00024-0
10. Reding ME, Chorpita BF, Lau AS, Innes-Gomberg D. Providers’ attitudes toward evidence-based practices: is it just about providers, or do practices matter, too? Adm Policy Ment Health Ment Health Serv Res. (2014) 41:767–76. doi: 10.1007/s10488-013-0525-1
11. Nelson MM, Shanley JR, Funderburk BW, Bard E. Therapists’ attitudes toward evidence-based practices and implementation of parent–child interaction therapy. Child Maltreat. (2012) 17(1):47–55. doi: 10.1177/1077559512436674
12. Pemberton JR, Conners-Burrow NA, Sigel BA, Sievers CM, Stokes LD, Kramer TL. Factors associated with clinician participation in TF-CBT post-workshop training components. Adm Policy Ment Health Ment Health Serv Res. (2017) 44:524–33. doi: 10.1007/s10488-015-0677-2
13. Nelson TD, Steele RG. Predictors of practitioner self-reported use of evidence-based practices: practitioner training, clinical setting, and attitudes toward research. Adm Policy Ment Health Ment Health Serv Res. (2007) 34:319–30. doi: 10.1007/s10488-006-0111-x
14. Covidence systematic review software. Veritas Health Innovation, Melbourne, Australia (2023). Available online at: www.covidence.org
15. Paynter J, Sulek R, Luskin-Saxby S, Trembath D, Keen D. Allied health professionals' knowledge and use of ASD intervention practices. J Autism Dev Disord. (2018) 48:2335–49. doi: 10.1007/s10803-018-3505-1
16. Sam AM, Odom SL, Tomaszewski B, Perkins Y, Cox AW. Employing evidence-based practices for children with autism in elementary schools. J Autism Dev Disord. (2021) 51:2308–23. doi: 10.1007/s10803-020-04706-x
17. Paynter J, Luskin-Saxby S, Keen D, Fordyce K, Frost G, Imms C, et al. Brief report: perceived evidence and use of autism intervention strategies in early intervention providers. J Autism Dev Disord. (2020) 50:1088–94. doi: 10.1007/s10803-019-04332-2
18. Pervin M, Hagmayer Y. Attitudes towards evidence-based practice of professionals working with children and adolescents with autism spectrum disorder in Bangladesh. Adm Policy Ment Health Ment Health Serv Res. (2022) 49(5):861–80. doi: 10.53846/goediss-9684
19. Paynter JM, Ferguson S, Fordyce K, Joosten A, Paku S, Stephens M, et al. Utilisation of evidence-based practices by ASD early intervention service providers. Autism. (2017) 21(2):167–80. doi: 10.1177/1362361316633032
20. Verschuur R, Huskens B, Korzilius H, Bakker L, Snijder M, Didden R. Pivotal response treatment: a study into the relationship between therapist characteristics and fidelity of implementation. Autism. (2020) 24(2):499–514. doi: 10.1177/1362361319876213
21. Cheung G, Trembath D, Arciuli J, Togher L. The impact of workplace factors on evidence-based speech-language pathology practice for children with autism spectrum disorders. Int J Speech Lang Pathol. (2013) 15(4):396–406. doi: 10.3109/17549507.2012.714797
22. Dyson MW, Chlebowski C, Brookman-Frazee L. Therapists’ adaptations to an intervention to reduce challenging behaviors in children with autism spectrum disorder in publicly funded mental health services. J Autism Dev Disord. (2019) 49:924–34. doi: 10.1007/s10803-018-3795-3
23. Garrad TA, Rayner C, Pedersen S, Cuskelly M. From research to reality: australian evidence-based practice in autism education. J Res Spec Educ Needs. (2021) 21(4):381–91. doi: 10.1111/1471-3802.12537
24. Stahmer AC, Aarons GA. Attitudes toward adoption of evidence-based practices: a comparison of autism early intervention providers and children’s mental health providers. Psychol Serv. (2009) 6(3):223. doi: 10.1037/a0010738
25. Paynter JM, Keen D. Knowledge and use of intervention practices by community-based early intervention service providers. J Autism Dev Disord. (2015) 45(6):1614–23. doi: 10.1007/s10803-014-2316-2
26. Suhrheinrich J, Nahmias AS, Yu Y, Melgarejo M, Schetter P, Holt TC, et al. Practice-driven research for statewide scale up: implementation outcomes of the California autism professional training and information network. Autism. (2022) 26(3):727–36. doi: 10.1177/13623613211068224
27. Aranbarri A, Stahmer AC, Talbott MR, Miller ME, Drahota A, Pellecchia M, et al. Examining US public early intervention for toddlers with autism: characterizing services and readiness for evidence-based practice implementation. Front Psychiatry. (2021) 12:786138. doi: 10.3389/fpsyt.2021.786138
28. Locke J, Lawson GM, Beidas RS, Aarons GA, Xie M, Lyon AR, et al. Individual and organizational factors that affect implementation of evidence-based practices for children with autism in public schools: a cross-sectional observational study. Implement Sci. (2019) 14(1):1–9. doi: 10.1186/s13012-019-0877-3
29. Paynter J, Sulek R, Trembath D, Keen D. Attitudes towards and organizational support for evidence-based practices: a comparison of education and allied health professionals in autism. Res Autism Spectr Disord. (2022) 92:101932. doi: 10.1016/j.rasd.2022.101932
30. Aarons GA. Mental health provider attitudes toward adoption of evidence-based practice: the evidence-based practice attitude scale (EBPAS). Ment Health Serv Res. (2004) 6:61–74. doi: 10.1023/b:mhsr.0000024351.12294.65
31. Rye M, Torres EM, Friborg O, Skre I, Aarons GA. The evidence-based practice attitude scale-36 (EBPAS-36): a brief and pragmatic measure of attitudes to evidence-based practice validated in US and Norwegian samples. Implement Sci. (2017) 12(1):1. doi: 10.1186/s13012-017-0573-0
32. Borntrager CF, Chorpita BF, Higa-McMillan C, Weisz JR. Provider attitudes toward evidence-based practices: are the concerns with the evidence or with the manuals? Psychiatr Serv. (2009) 60(5):677–81. doi: 10.1176/appi.ps.60.5.677
33. Dixon GN, McKeever BW, Holton AE, Clarke C, Eosco G. The power of a picture: overcoming scientific misinformation by communicating weight-of-evidence information with visual exemplars. J Commun. (2015) 65(4):639–59. doi: 10.1111/jcom.12159
34. Togher L, Lincoln M, Power E, Munro N, McCabe P, Worrall L. Facilitating the integration of evidence based practice into speech-language pathology curricula: a scoping study to examine the congruence between academic curricula and work based needs (Project Report). Sydney: University of Sydney (2007).
35. Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health Ment Health Serv Res. (2011) 38:65–76. doi: 10.1007/s10488-010-0319-7
36. Weiner BJ, Lewis CC, Stanick C, Powell BJ, Dorsey CN, Clary AS, et al. Psychometric assessment of three newly developed implementation outcome measures. Implement Sci. (2017) 12:1–2. doi: 10.1186/s13012-017-0635-3
37. Wolfenden L, Foy R, Presseau J, Grimshaw JM, Ivers NM, Powell BJ, et al. Designing and undertaking randomised implementation trials: guide for researchers. Br Med J. (2021) 372. doi: 10.1136/bmj.m3721
38. Suhrheinrich J, Melgarejo M, Root B, Aarons GA, Brookman-Frazee L. Implementation of school-based services for students with autism: barriers and facilitators across urban and rural districts and phases of implementation. Autism. (2021) 25(8):2291–304. doi: 10.1177/13623613211016729
39. Barry L, Holloway J, McMahon J. A scoping review of the barriers and facilitators to the implementation of interventions in autism education. Res Autism Spectr Disord. (2020) 78:101617. doi: 10.1016/j.rasd.2020.101617
40. Williams NJ, Frank HE, Frederick L, Beidas RS, Mandell DS, Aarons GA, et al. Organizational culture and climate profiles: relationships with fidelity to three evidence-based practices for autism in elementary schools. Implement Sci. (2019) 14:1–4. doi: 10.1186/s13012-019-0863-9
41. Aarons GA, Hurlburt M, Horwitz SM. Advancing a conceptual model of evidence-based practice implementation in public service sectors. Adm Policy Ment Health Ment Health Serv Res. (2011) 38:4–23. doi: 10.1007/s10488-010-0327-7
42. Feldstein AC, Glasgow RE. A practical, robust implementation and sustainability model (PRISM) for integrating research findings into practice. Jt Comm J Qual Patient Saf. (2008) 34(4):228–43. doi: 10.1016/S1553-7250(08)34030-6
43. McCreight MS, Rabin BA, Glasgow RE, Ayele RA, Leonard CA, Gilmartin HM, et al. Using the practical, robust implementation and sustainability model (PRISM) to qualitatively assess multilevel contextual factors to help plan, implement, evaluate, and disseminate health services programs. Transl Behav Med. (2019) 9(6):1002–11. doi: 10.1093/tbm/ibz085
44. Nilsen P, Bernhardsson S. Context matters in implementation science: a scoping review of determinant frameworks that describe contextual determinants for implementation outcomes. BMC Health Serv Res. (2019) 19(1):1–21. doi: 10.1186/s12913-019-4015-3
45. Kryszak EM, Albright CM, Fell LA, Butter EM, Kuhlthau KA. Clinician perspectives on telehealth assessment of autism Spectrum disorder during the COVID-19 pandemic. J Autism Dev Disord. (2022) 52(12):5083–98. doi: 10.1007/s10803-022-05435-z
46. Gabellone A, Marzulli L, Matera E, Petruzzelli MG, Margari A, Giannico OV, et al. Expectations and concerns about the use of telemedicine for autism spectrum disorder: a cross-sectional survey of parents and healthcare professionals. J Clin Med. (2022) 11(12):3294. doi: 10.3390/jcm11123294
47. Ali D, O'Brien S, Hull L, Kenny L, Mandy W. ‘The key to this is not so much the technology. It’s the individual who is using the technology’: perspectives on telehealth delivery for autistic adults during the COVID-19 pandemic. Autism. (2023) 27(2):552–64. doi: 10.1177/13623613221108010
48. Kirkham P. ‘The line between intervention and abuse’–autism and applied behaviour analysis. Hist Human Sci. (2017) 30(2):107–26. doi: 10.1177/0952695117702571
49. Powell BJ, Waltz TJ, Chinman MJ, Damschroder LJ, Smith JL, Matthieu MM, et al. A refined compilation of implementation strategies: results from the expert recommendations for implementing change (ERIC) project. Implement Sci. (2015) 10(1):1–4. doi: 10.1186/s13012-015-0209-1
50. Aguilar-Gaxiola S, Ahmed SM, Anise A, Azzahir A, Baker KE, Cupito A, et al. Assessing meaningful community engagement: a conceptual model to advance health equity through transformed systems for health: organizing committee for assessing meaningful community engagement in health & health care programs & policies. NAM Perspect. (2022) 2022. doi: 10.31478/202202c
51. Fort MP, Paniagua-Avila A, Beratarrechea A, Cardona S, Figueroa JC, Martinez-Folgar K, et al. Stakeholder engagement in the translation of a hypertension control program to Guatemala’s public primary health care system: lessons learned, challenges, and opportunities. Glob Heart. (2019) 14(2):155–63. doi: 10.1016/j.gheart.2019.05.005
52. Estabrooks PA, Harden SM, Almeida FA, Hill JL, Johnson SB, Porter GC, et al. Using integrated research-practice partnerships to move evidence-based principles into practice. Exerc Sport Sci Rev. (2019) 47(3):176. doi: 10.1249/JES.0000000000000194
53. Fort MP, Manson SM, Glasgow RE. Applying an equity lens to assess context and implementation in public health and health services research and practice using the PRISM framework. Front Health Serv. (2023) 3:1139788. doi: 10.3389/frhs.2023.1139788
Keywords: evidence-based practice, autism spectrum disorder, provider attitudes, implementation science, dissemination and implementation, autism
Citation: DeLucia EA, Harden SM and Scarpa A (2024) Provider attitudes toward evidence-based practice in autism: a mini-review. Front. Child Adolesc. Psychiatry 3:1363532. doi: 10.3389/frcha.2024.1363532
Received: 30 December 2023; Accepted: 27 February 2024;
Published: 2 May 2024.
Edited by:
Marco Turi, University of Salento, ItalyReviewed by:
Alessandra Gabellone, University of Bari Aldo Moro, Italy© 2024 DeLucia, Harden and Scarpa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Elizabeth A. DeLucia bGl6ZGVsdWNpYUB2dC5lZHU=
 Elizabeth A. DeLucia
Elizabeth A. DeLucia Samantha M. Harden
Samantha M. Harden Angela Scarpa
Angela Scarpa