- 1Public Health Emergency Management, Ethiopia Public Health Institute, Addis Ababa, Ethiopia
- 2Department of Epidemiology, School of Public Health, St Paul's Hospital Millennium Medical College, Addis Ababa, Ethiopia
- 3Department of Psychiatry, Hawasa University, Hawasa, Ethiopia
Background: Every year, more than 800,000 people die due to suicide (one person every 40 s), ranking as the second leading cause of death next to traffic accidents in individuals aged 15–29 years. The objective of this study was to assess the prevalence and factors associated with suicidal ideation and attempts among mentally ill patients.
Method: An institutional-based, cross-sectional study was conducted between December 2019 and January 2020. Data were collected using a convenient sampling technique until the required sample size was achieved. The total sample size was 385. The Suicidal Behavior Questionnaire-Revised (SBQ-R), Oslo Social Support Scale, and self-prepared to assess suicide were used. Data collection was carried out by psychiatry professionals through face-to face interviews. Data were analyzed, and bivariate and multivariable logistic regression analyses were conducted using Statistical Package for the Social Sciences (SPSS) version 23.
Result: A total of 385 patients participated in the study. Of these, 216 (56%) were men. The prevalence of suicide ideation was 255 (66.2%). The odds of suicidal ideation and attempt was almost three times higher [adjusted odds ratio (AOR) = 2.79, 95% confidence interval (CI) 1.11–6.98]; among patients who felt hopeless, the OR was around two times higher (AOR = 2.44, 95% CI 1.17–5.08); among patients who had a family history of suicide, the OR was almost three times higher (AOR = 2.56, 95% CI 1.00–6.53); among patients who stopped their medication, the OR was approximately two times higher (AOR = 2.25, 95% CI 1.14–4.46); the OR of suicidal ideation and attempts was almost six and four times higher (AOR = 5.86, 95% CI 1.30–26.41; and AOR = 3.61, 95% CI 1.01–12.88) among patients who were educated to primary and secondary level, respectively.
Conclusion: In this study, carried out in Ethiopia, suicidal ideation and attempts were more common among men than women. The prevalence of suicidal ideation and attempts showed a significant public health issue among hospital-attending and chronic mentally ill adolescents, which requires a large emphasis. We recommend that suicide prevention needs to involve non-governmental and non-profit organizations, universities, and civil society at different levels.
Background
Suicide is a serious, preventable public health problem that results in social, emotional, and economic consequences for family, friends, and colleagues (1). Because suicide remains a sensitive issue, it is very likely that it is underreported due to stigma, criminalization, and weak surveillance systems. It demands our attention and action even though its prevention and control are difficult (2).
Several environmental, psychosocial, and behavioral factors have been found to be associated with suicidal ideation, suicidal attempts, and suicide. Suicidal behaviors often coexist with other health risk behaviors, such as aggressive behavior, smoking, and experiences of sexual intercourse (3, 4). Suicide ideation and attempted suicide were also related to many severe mental health problems, such as anxiety, schizophrenia, bipolar disorder, mood disorder, depression, and others (5).
The method of the suicide attempt influences the morbidity and completion rates, independent of the severity of the intent to die at the time of suicidal behavior. The most common methods of attempting suicide are hanging, poisoning, slashing, and shooting (6, 7).
The burden of suicide constitutes a serious public health issue worldwide, and mental health professionals need to increase their awareness of the warning signs for suicide. Suicide warning signs are associated with acute factors that inform clinicians about observable signs and expressed emotions, and are important for saving lives by early detection and intervention for those at risk (8).
Every year, more than 800,000 people die due to suicide (one person every 40 s), ranking it the second leading cause of death next to traffic accidents in individuals aged 15–29 years. Among nearly 250 causes of death, suicide was the 14th leading cause of global mortality (9). In addition, it is also predicted that, by 2020, the rate of death due to suicide will be increased to one every 20 s (10). Suicide accounts for 50% and 71% of all violent deaths globally in men and women, respectively.
Internationally, suicide rates range from highs of more than 25 per 100,000 individuals in Scandinavia, Switzerland, Germany, Austria, the eastern European countries, and Japan to less than 10 per 100,000 in Spain, Italy, Ireland, Egypt, and the Netherlands (11). Rates of suicide among adolescents and young adults have increased considerably in recent decades (12).
In sub-Saharan Africa, death from suicide is estimated to be 34,000 per year (13). The prevalence of suicide ideation was estimated to be 7% in Tanzania (3), 6.2% in Seychelles (14), 31.3% in Zambia (15), 23.3% in Benin (5), and 21.6% in Uganda. This even occurs even though some mental health problems may arise from infectious diseases (16). However, in Ethiopia, there was no adequate research on the magnitude or burden of suicidal ideation and attempts. The aim of the present study was to determine the prevalence of suicidal ideation and attempts and the factors associated with suicidal ideation and attempts among mentally ill patients.
Method
Study area
Saint Paul's Hospital Millennium Medical College (SPHMMC) was established at the center of the country, in Addis Ababa, through a decree of the Council of Ministers in 2010, although the medical school was opened in 2007. The hospital was established in 1968 by the late Emperor Haile Selassie. It is governed by a board under the Federal Ministry of Health. The SPHMMC has many specialist programs and has many departments, including a psychiatry department. The psychiatry department started approximately 40 years earlier, i.e., in the 1975 Ethiopian calendar.
Study design and period
An institutional-based, cross-sectional study was conducted between December 2019 and January 2020.
Sample size determination
The sample size was determined using a single population proportion formula as follows:
where P = the prevalence 64.8% (0.648) from the study by Mekonnen and Kebede (17), and the absolute precision or tolerable margin of error (d) = 5% (0.05). Zα/2 = Z value at (α = 0.05) = 1.96 corresponding to the 95% confidence interval (CI). After adjusting for a 10% contingency for non-response rates, a total of 385 study populations were involved in the study.
Sampling techniques and procedures
All patients presenting at the SPHMMC Psychiatry Patient Department (outpatient department, OPD) between December 2019 and January 2020 were included in this study using a consecutive sampling technique until the required sample size was achieved. Both new and follow-up patients were included in the study.
Data collection procedures and instruments
Data were collected using an interviewer-administered structured questionnaire. The questionnaire included sociodemographic characteristics, patient clinical characteristics, social support of the patient, environmental risk factors, methods used for suicide attempts, and items related to patients’ suicidal behavior, i.e., ideation and attempt. A pretest was carried out with 5% of the sample size at St. Peter Specialized Hospital among patients with mental illness before the actual study was conducted and the data collection tool was revised based on the findings of the pretest. Data collectors were 10 trained psychiatric nurses; 2 senior mental health experts were assigned as supervisors to the data collectors. The patients were diagnosed by psychiatrists, psychiatry residents, and senior or mental health professionals. Therefore, the diagnosis and some clinical factors were reviewed from each patient's chart.
Items used to assess suicidal ideation and attempt were used, adapted from Suicidal Behavior Questionnaire-Revised (SBQ-R) (18). The items included in the questionnaire were as follows: item 1 taps into lifetime suicidal ideation and attempt; item 2 assesses the frequency of suicidal ideation over the past 12 months; and item 3 taps into the threat of suicidal behavior. The level of social support among patients with mental illness was assessed using the three-item Oslo Social Support Scale (OSSS) and the scores were in the range of 3–14 (19).
Data processing and analysis
Data were checked for completeness and consistency, and then coded and entered into Epi info version 7.2.1.0. They were then exported to Statistical Package for the Social Sciences (SPSS) version 23 for analysis. Descriptive analyses of ratios, proportions, and rates were computed. Bivariate and multivariate logistic regression analyses were also conducted. Variables with a P-value <0.2 in the bivariate analysis were fitted to multivariable logistic regression. Those variables with a P-value <0.05 in the multivariable analysis were considered to be significant.
Results
Sociodemographic characteristics
A total of 385 participants (age range = 18–85 years) were enrolled in the study, with a response rate of 100%. Of the total participants, 216 (56%) were men. Of the participants, 197 (51%) were single, 232 (48.9%) were illiterate, 140 (36.4%) had a level of education from grade 9 to 12, and 77 (18.4%) were private/non-governmental organization (NGO) employees (Table 1).
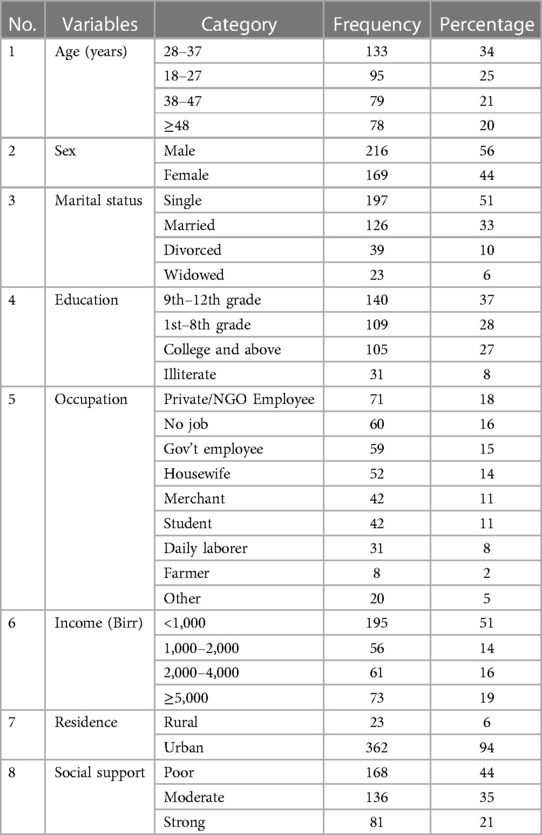
Table 1. Sociodemographic characteristics of study participant patients with mental illness were attending the Psychiatric Department of SPHMMC in Addis Ababa.
Clinical characteristics of participants
In total, 297 (77%) participants were diagnosed as mentally ill before presenting at SPHMMC. As to the duration of being psychiatric patients, among the study participants, 195 (51%) reported that they experienced mental illnesses for more than 5 years before coming to SPHMMC (Table 2).
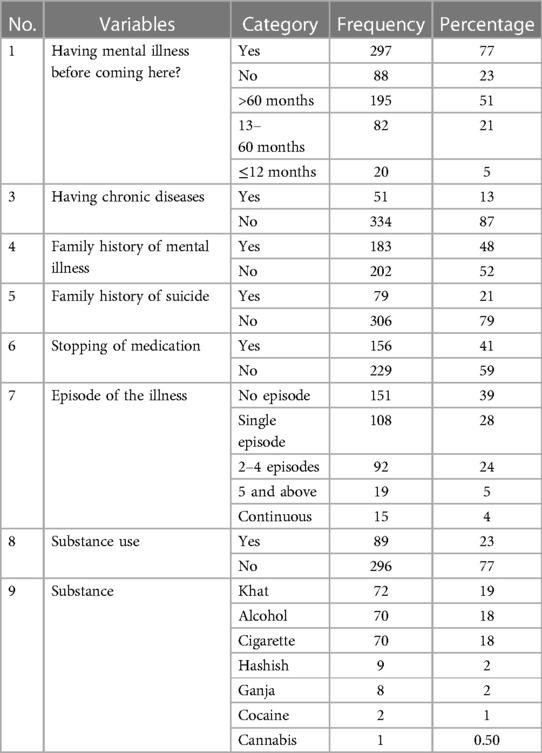
Table 2. Clinical characteristics of participants visiting psychiatric OPD of SPHMMC, Addis Ababa, 2020.
Of the participants with suicidal ideation and attempts, 71 (34.4%) were diagnosed with major depression disorder (MDD) and 53 (25.6%) were diagnosed with schizophrenia (Table 3).

Table 3. Mental illnesses diagnosed among the study participants and those who reported in both suicidal ideation and attempts during the study period, SPHMMC, 2020.
Prevalence of suicide ideation and attempts
Of the 385 respondents, 255 (66.2%) [men = 143 (37%), women = 112 (29%)] had suicidal ideation and 210 (55%) attempted suicide [men = 115 (30%), women = 95 (25%)]. Of the study participants, 207 (54%) had thought of suicide and attempt. Of them, 19 (5%) were told by someone that they were going to commit suicide or they might have to do it in their lifetime (Table 4).
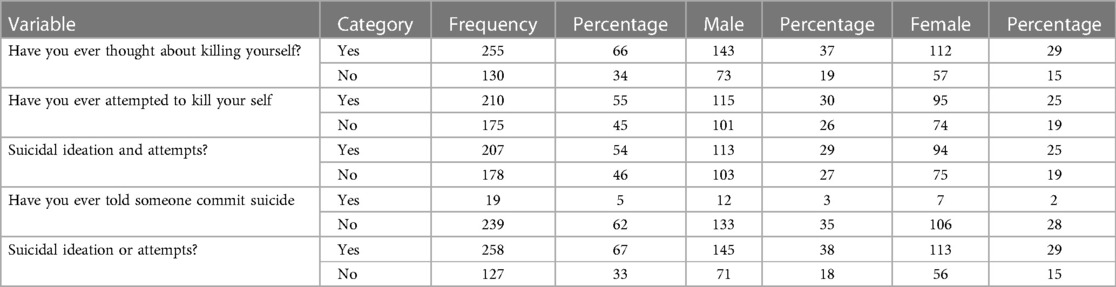
Table 4. Frequency distribution of suicide ideation and attempt among mental Ill patients in SPHMMC, Addis Ababa, Ethiopia, 2020 (n = 385).
Among all participants, the age range of 28–37 years was the most affected age group (see Figure 1).
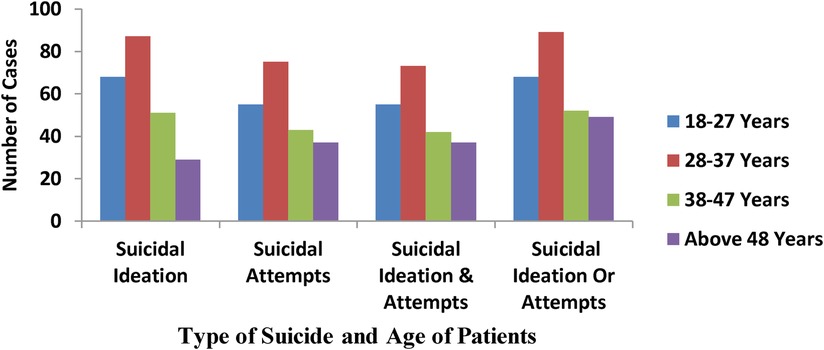
Figure 1. Distribution of suicide ideation and attempt by age among mental Ill patients of psychiatry OPD of SPHMMC, Addis Ababa, Ethiopia, 2020 (N = 385).
Of the participants, 142 (55%) rarely had suicidal ideation and attempts (one time only) and 7 (3%) had five or more suicidal thoughts and attempts (Figure 2).
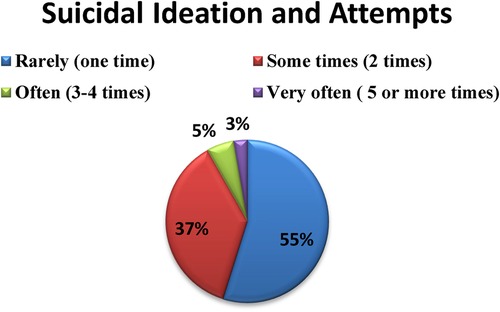
Figure 2. Percentage distribution of frequency of suicide ideation and attempt among mental Ill patients in SPHMMC, Addis Ababa, Ethiopia, 2020 (n = 385).
Methods of suicidal ideation and attempts
Of the participants, 98 (47%) thought of attempting suicide using drug overdose/poisoning and 92 (44%) of them thought of attempting suicide by hanging themselves. The smallest proportion of participants (n = 5, 2%) thought of attempting suicide using a gun.
From all methods listed in the questionnaire and the participants applied to them and thought to kill themselves based on sex drug dose/poisoning were the highest one female (51) and male (47) (Figure 3).

Figure 3. Frequency distribution of methods of suicidal ideation and attempts at sex among mentally Ill patients in SPHMMC, Addis Ababa, Ethiopia, 2020.
Factors associated with suicidal ideation and attempt
In the bivariate analysis, the following information was collected: age, marital status, occupation, education, religion, monthly income, residence of the participant, duration of mental illness, family history of mental illness, family history of suicide, stopped mental illness medication, Oslo Social Support Scale, recurrence/relapse of mental illness, current psychiatric diagnosis, feelings of hopelessness, having mental health issues, and death in family (Table 5).
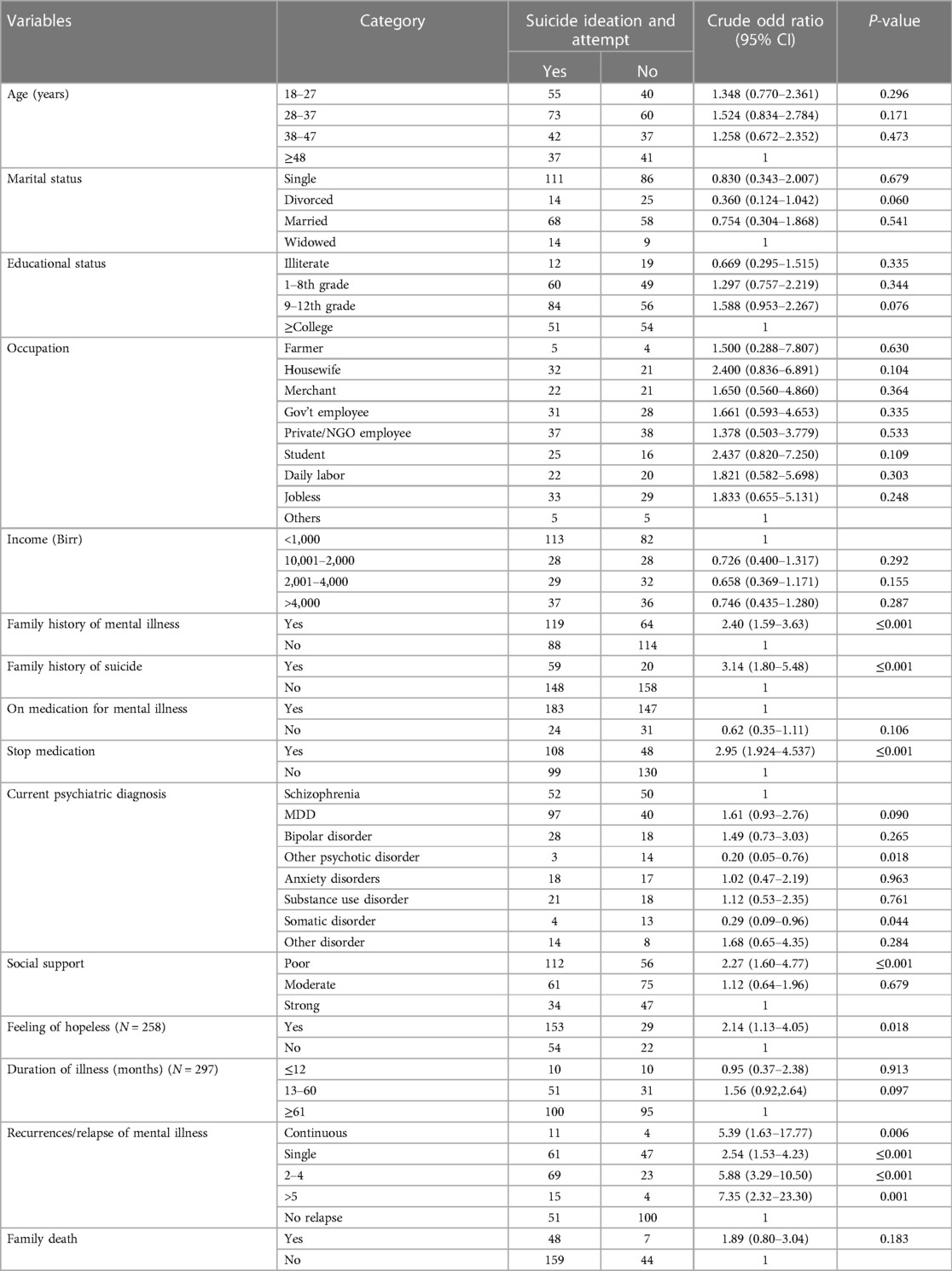
Table 5. Bivariate logistic regression results of suicide ideation and attempt among mental Ill patients in SPHMMC, Addis Ababa, Ethiopia, 2020 (n = 385).
The odds of suicidal ideation and attempt were lower among divorced people [adjusted odds ratio (AOR) = 0.31, 95% CI 0.11–0.85, p-value = 0.022] compared to single people; individuals with a primary and secondary education had a more likely risk of suicide ideation and attempts than those educated to college level and above (AOR = 5.86, 95% CI 1.30–26.41; and AOR = 3.61, 95% CI 1.01–12.88), respectively (Table 6). Individuals who stopped their mental illness medication had a higher risk of suicide ideation and attempt than those continuing with their medication (AOR = 2.56, 95% CI 1.00–6.53), and individuals with a family history of suicide had a more likely risk of suicide ideation and attempts than those who do not have a family history of suicide or higher (AOR = 2.44, 95% CI 1.17–5.08) (Table 1).
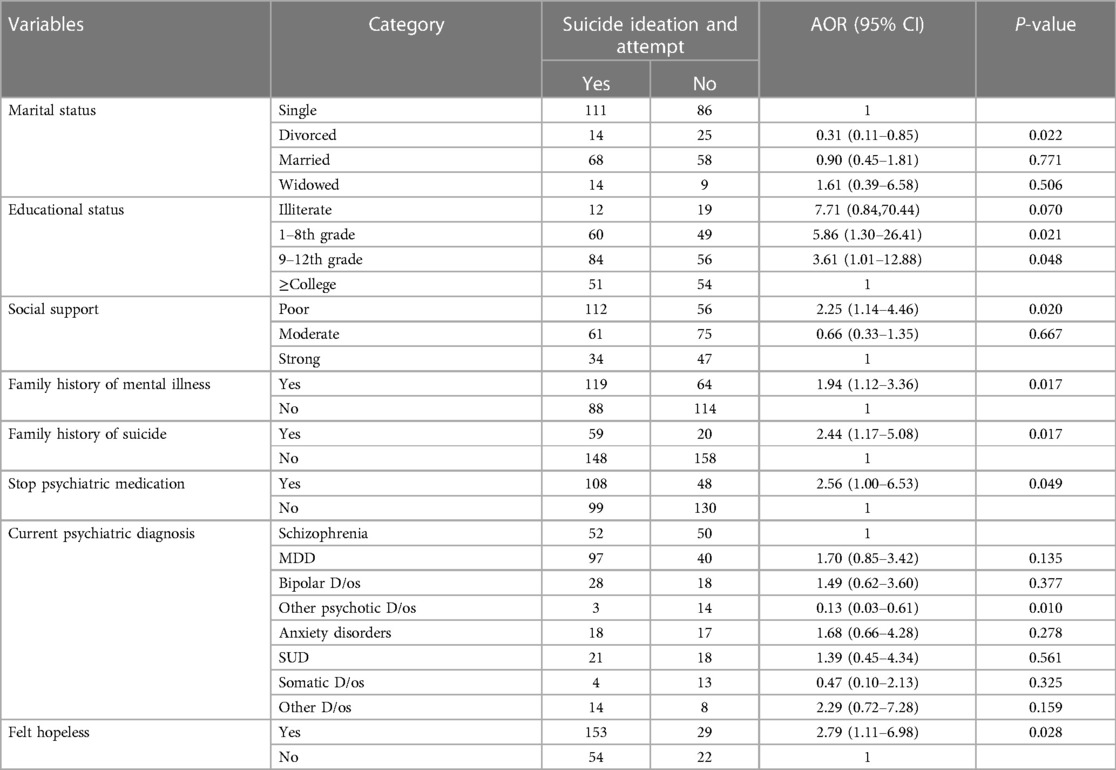
Table 6. Multivariate logistic regression on prevalence and associated factors of suicidal ideation and attempts among mentally Ill patients in psychiatry OPD at SPHMMC, in Addis Ababa, Ethiopia, 2020 (n = 385).
Discussion
In this study, the sociodemographic of the participants’ sex was different from other studies: our study consisted of 56% men and 44% women. The percentage of women was higher in the study carried out in Dangla (men = 48.3%, women = 51.7%) (8). This might be due to a high level of participation in social activities or the suppression of women in that study area. In the study carried out in Gondar Hospital, 54% of participants were men and 46% were women (20); in a study carried out in Istanbul, Turkey, 30.8% were women and 69.2% were men (21). However, many studies show that men had more suicidal ideation and attempts than women.
In our study, the primary and secondary education level had 5.86 times and 3.61 times more likely risk of association of suicidal ideation and attempts (AOR = 5.86, 95% CI 1.30–26.41; and AOR = 3.61, 95% CI 1.01–12.88, respectively). The level of education in the present study was higher than that in the study carried out in Amanuel Hospital (AOR = 1.63, 95% CI 0.68–3.89; and AOR = 2.51, 95% CI 1.11–5.68, respectively) (22). This might be due to academic failure or low satisfaction in the future of their job due to their education.
In addition, hopelessness was a more likely risk of association with suicidal ideation and attempts. The present study had a 2.79 times more likely risk of association of suicidal ideation and attempts (AOR = 2.79, 95% CI 1.11–6.98). This was slightly higher than that in a study carried out in Amanuel Hospital (AOR = 2.510, 95% CI 1.459–4.320) (22). This might be due to those psychotic patients who do not see futurity, have no plans to live, do not think positively, and are not anxious to take any opportunities that might put them in a better position.
In our study, we determined that suicidal behavior was significantly less common in patients with mental illness who were divorced compared with those who were single or never married. This study was also lower than that in a study carried out in the USA (AOR = 2.1, 95 CI 1.83–2.33) (23). Thus, studies further suggested that the highest risk increase was in never-married individuals and those who were separated or divorced (24). Similarly, being single was associated with an increased risk of suicide in women aged 20–34 years (20). Furthermore, individuals who had poor social support were 2.25 times more likely to have suicidal ideation and attempts than patients who had strong social support. This was similar to the results from recent studies (25, 26).
In this study, patients with a family history of mental disorders significantly increased the rate of suicidal ideation and attempt, which is 1.94 times more likely risk of suicidal ideation and attempts (AOR = 1.94, 95% CI 1.12–3.36), which is slightly lower than or comparable to a study carried out on psychiatry patients at Jimma University Hospital (AOR = 2.25, 95% CI 1.11–4.57) (2). In addition, suicidal behavior was more likely to occur in patients with a family history of suicidal behavior when compared with patients without a family history of suicidal behavior. Our findings seemed to be similar to those in studies showing that a history of suicide in the family could increase the risk of suicidal behavior in patients with mental illness (21, 27). In their study, Trémeau et al. indicated that a family history of suicide significantly increased the risk of suicide attempts, with higher lethality and frequency of suicide attempts (28).
As a limitation, institutional-based studies could not address those adolescents outside the institution, which assessed the lifetime prevalence of suicidal ideation and attempts at the point of current prevalence during the stated period. In addition, this study assessed their status of suicidal ideation and attempt based on their stated response; in this case, individuals may not disclose their actual thoughts or attempts about suicide.
Conclusion
In our study on the sociodemographic of sex, men were more affected by suicidal ideation and attempts than women. The prevalence of suicide ideation and attempts was high, showing a significant public health issue among hospital-attending and chronic mentally ill patients that requires a great emphasis. These risk factors were primary and secondary grade/school education, feelings of hopelessness, stopping mental illness medication, family history of mental illness, family history of suicide, being divorced, social support of the patient, and current psychotic diagnosis of other diagnosis of illness had positively or more likely risk of association with suicidal ideation and attempts.
Therefore, suicide prevention needs to involve different actors and disciplines working at suicide non-governmental and non-profit organizations, universities, and civil society at different levels. Early detection and intervention are the single most important prevention strategy of suicide in patients with mental illness. Thus, clinicians are strongly recommended to identify those patients with the abovementioned high-risk factors. The prediction of suicide in patients with mental illness is complex and difficult, and efforts at prevention should also focus on optimizing social support and adherence to psychiatric medication for people with mental illness. Furthermore, St. Paul’s Hospital should have a different psychiatry treatment center and rehabilitation center that separates them from other services.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: The data will be available based on reasonable request to the author. Requests to access these datasets should be directed to Awol Dawud,YXdvbC5tb2RAZ21haWwuY29t.
Ethics statement
The studies involving humans were approved by St. Paul Hospital Millennium Medical College Ethical review committee. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
AM: Data curation, Funding acquisition, Methodology, Resources, Supervision, Visualization, Writing – original draft, Writing – review & editing, Project administration. TM: Methodology, Supervision, Validation, Writing – review & editing. MoA: Methodology, Supervision, Writing – review & editing. TT: Supervision, Writing – review & editing. MiA: Methodology, Supervision, Writing – review & editing. NT: Supervision, Writing – review & editing.
Funding
The authors declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Amare T, Meseret Woldeyhannes S, Haile K, Yeneabat T. Prevalence and associated factors of suicide ideation and attempt among adolescent high school students in Dangila Town, Northwest Ethiopia. Psychiatry J. (2018) 2018:1–9. doi: 10.1155/2018/7631453
2. Lieberman R, Cowan KC. Bullying and youth suicide: breaking the connection. Princ Leadersh. (2011) 12:12–7.
3. Dunlavy AC, Aquah EO, Wilson ML. Suicidal ideation among school-attending adolescents in Dar es Salaam Tanzania. Tanzan J Health Res. (2015) 17(1).
4. Ghrayeb FAW, Mohamed Rusli A, Mohd Ismail I, Al Rifai A. Prevalence of suicide ideation and attempt among Palestinian adolescents: a cross-sectional study. World J Med Sci. (2014) 10(3):261–6. doi: 10.5829/idosi.wjms.2014.10.3.82386
5. Randall JR, Doku D, Wilson ML, Peltzer K. Suicidal behaviour and related risk factors among school-aged youth in the republic of Benin. PLoS One. (2014) 9(2). doi: 10.1371/journal.pone.0088233
6. Sadock BJ, Sadock VA, Ruiz P. Synopsis of Psychiatry: Behavioral Sciences Clinical Psychiatry. 11th ed. New York: Wolters Kluwer (2015).
7. Alem A, Kebede D, Jacobsson L, Kullgren G. Suicide attempts among adults in Butajira, Ethiopia. Acta Psychiatr Scand Suppl. (1999) 397:70–6. doi: 10.1111/j.1600-0447.1999.tb10697.x
8. Rudd MD. Suicide warning signs in clinical practice, Department of Psychology, Texas Tech University, MS 42051, Lubbock, TX 79409-2051, USA.
9. Johnston AK, Pirkis JE, Burgess PM. Suicidal thoughts and behaviours among Australian adults: findings from the 2007 National Survey of Mental Health and Wellbeing. Aust N Z J Psychiatry. (2009) 43:635–43. doi: 10.1080/00048670902970874
10. Värnik P. Suicide in the world. Int J Environ Res Public Health. (2012) 9(3):760–71. doi: 10.3390/ijerph9030760
11. Palmier JB. Prevalence and correlates of suicidal ideation among students in sub-Saharan Africa (master’s thesis). Georgia State University (2011). p. 1–55. doi: 10.57709/2120397
12. Sijuwade PO. Suicide ideation among the adolescents: an exploratory study research. J Appl Sci. (2011) 6:167–73. doi: 10.3923/rjasci.2011.167.173
13. Mars B, Burrows S, Hjelmeland H, Gunnell D. Suicidal behavior across the African continent: a review of the literature. BMC Public Health. (2014) 14:1–8. doi: 10.1186/1471-2458-14-606
14. Muula AS, Kazembe LN, Rudatsikira E, Siziya S. Suicidal ideation and associated factors among in-school adolescents in Zambia. Tanzan Health Res Bull. (2007) 9(3):202–6.18087900
15. World Health Organization. Preventing suicide, Geneva (2014). Available online at: https://scholar.google.com/scholar?q=Worl+d+Health+Organization,+Preventing+suicide,+Geneva,+2014%3B+(Accessed+on+August+2019)&hl=en&as_sdt=0&as_vis=1&oi=scholart (Accessed August 2019).
16. Rudatsikira E, Muula AS, Siziya S, Twa-Twa J. Suicidal ideation and associated factors among school-going adolescents in rural Uganda. BMC Psychiatry. (2007) 7:1–6. doi: 10.1186/1471-244X-7-67
17. Mekonnen D, Kebede Y. The prevalence of suicidal ideation and attempts among individuals attending an adult psychiatry out-patient clinic in Gondar, Ethiopia. College of Medicine and Health Sciences, University of Gondar, Ethiopia (2006).
18. Osman A, Bagge CL, Guitierrez PM, Konic LC, Kooper BA, Barrios FX. The Suicidal Behaviors Questionnaire-Revised (SBQ-R): validation with clinical and nonclinical samples. Assessment. (2001) 8:443–54. doi: 10.1177/107319110100800409
19. Abiola T, Udofia O, Zakari M. Psychometric properties of the 3-item Oslo Social Support Scale among clinical students of Bayero University Kano, Nigeria. Malaysian J Psychiatry. (2013) 22:32–41.
20. Corcoran P, Nagar A. Suicide and marital status in Northern Ireland. Soc Psychiatry Epidemiol. (2009) 45:795–800. doi: 10.1007/s00127-009-0120-7
21. Rossau CD, Mortensen PB. Risk factors for suicide in patients with schizophrenia: nested case-control study. Br J Psychiatry. (1997) 171:355–9. doi: 10.1192/bjp.171.4.355
22. Schreiber J, Culpepper L, Roy-Byrne PP, Solomon D. Suicidal ideation and behavior in adults (2020). Topic 1708, Version 56.0.
23. Hana B, Crosbyb AE, Ortegac LAG, Parksb SE, Comptond WM, Gfroerera J. Suicidal ideation, suicide attempt, and occupations among employed adults aged 18–64 years in the United States. Compr Psychiatry. (2016) 66:176–86. doi: 10.1016/j.comppsych.2016.02.001
24. Agerbo E. Midlife suicide risk, partner’s psychiatric illness, spouse and child bereavement by suicide or other modes of death: a gender specific study. J Epidemiol Community Health. (2005) 59:407–12. doi: 10.1136/jech.2004.024950
25. Peltzer K, Pengpid S. Suicidal ideation and associated factors among school-going adolescents in Thailand. Int J Environ Res Public Health. (2012) 9(2):462–73. doi: 10.3390/ijerph9020462
26. Abdu Z, Hajure M, Desalegn D. Suicidal behavior and associated factors among students in Mettu University, South West Ethiopia: an institutional based cross-sectional study. Psychol Res Behav Manag. (2020) 13:233–43. doi: 10.2147/PRBM.S240827
27. McGirr A, Tousignant M, Routhier D, Pouliot L, Chawky N, Margolese HC, et al. Risk factors for completed suicide in schizophrenia and other chronic psychotic disorders: a case–control study. Schizophr Res. (2006) 84:132–43. doi: 10.1016/j.schres.2006.02.025
Keywords: suicidal ideation, prevalence, mentally ill, suicidal attempts, risk factor
Citation: Mohammed AD, Menna T, Ayalew M, Teshome T, Alayu M and Tesfay N (2024) Prevalence and factors associated with suicidal ideation and attempts among mentally ill patients in the psychiatry OPD at St. Paul's Hospital Millennium Medical College, Addis Ababa, Ethiopia. Front. Child Adolesc. Psychiatry 3:1342257. doi: 10.3389/frcha.2024.1342257
Received: 23 November 2023; Accepted: 26 March 2024;
Published: 10 April 2024.
Edited by:
Massy Mutumba, University of Michigan, United StatesReviewed by:
Sigita Lesinskiene, Vilnius University, LithuaniaKaren Schmeelk-Cone, University of Rochester Medical Center, United States
© 2024 Mohammed, Menna, Ayalew, Teshome, Alayu and Tesfay. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Awol Dawud Mohammed YXdvbC5tb2RAZ21haWwuY29t
Abbreviations CI, confidence interval; MDD, major depression disorder; OR, odds ratio; OPD, outpatient department; OSSS, Oslo Social Support Scale; SPHMMC, St. Paul Hospital Millennium Medical College; SBQ-R, Suicidal Behavior Questionnaire-Revised; SPSS, Statistical Package for the Social Sciences.
 Awol Dawud Mohammed
Awol Dawud Mohammed Takele Menna
Takele Menna Mohammed Ayalew
Mohammed Ayalew Tesfalem Teshome2
Tesfalem Teshome2 Neamin Tesfay
Neamin Tesfay