- 1Department of Psychiatry and Behavioral Sciences, University of California, San Francisco, San Francisco, CA, United States
- 2School of Medicine, University of Texas Health San Antonio, San Antonio, TX, United States
- 3Bexar County Juvenile Probation Department, San Antonio, TX, United States
- 4Department of Psychiatry and Behavioral Sciences, University of Texas Health San Antonio, San Antonio, TX, United States
Background: Incarcerated youth commonly present with emotion dysregulation, aggression, and comorbid psychiatric disorders, yet often do not receive necessary mental health treatment while confined. It is therefore crucial to expand the evidence base regarding empirically supported mental health interventions which are feasible to implement in secure settings to address incarcerated youth's mental health needs. Through a community-academic partnership, the current pilot study evaluated a comprehensive dialectical behavior therapy program implemented in a juvenile correctional treatment center.
Methods: Youth participants (N = 113) were on average 15.37 years old (SD = 1.10, range = 13–17), 68.1% boys, and identified as 69.0% Latinx, 22.1% Black, 8.0% White, and 0.9% Native American. Youth received comprehensive dialectical behavior therapy for adolescents (DBT-A), including individual therapy, skills training groups, family therapy, multi-family skills training groups, and skills coaching in the milieu by direct care staff who participated in extensive training and ongoing consultation team meetings. As part of a facility-designed program evaluation, youth completed a battery of empirically validated assessments of mental health and emotion regulation prior to and following completion of the program.
Results: Results show that comprehensive DBT-A is feasible to implement in a juvenile correctional treatment center and overall, youth improved from pre- to post-treatment in mental health symptoms and emotion regulation, with small to medium effect sizes.
Conclusion: These findings build upon a growing literature showing dialectical behavior therapy is a promising intervention for treating emotion dysregulation and mental health conditions and can be successfully implemented in juvenile forensic settings.
1. Introduction
On any given day, approximately 43,580 youth are confined in the U.S. due to involvement with the juvenile or criminal legal systems; these 2017 estimates represent an approximately 60% reduction from a high of 108,802 in 2000 (1). Numerous studies have identified high rates of mental health needs among incarcerated youth, with estimates up to 80% having at least one psychiatric disorder (2–8). Epidemiologic data from incarcerated youth indicate half of boys and almost half of girls meet criteria for a substance use disorder, more than 40% of boys and girls for disruptive behavior disorders, and almost 20% of boys and more than 25% of girls for affective disorders (6, 9). Comorbid psychiatric disorders (e.g., affective, anxiety, behavioral, substance use) are also common; 56.5% of girls and 45.9% of boys meet criteria for two or more disorders (10). Incarcerated youth commonly present with extensive trauma histories (11), aggression and emotional dysregulation (12, 13), and are likely to experience re-incarceration as adults, substance abuse, financial difficulty, adverse health outcomes, and early mortality (14–17).
Incarcerated youth face multiple layers of stress and marginalization, requiring thoughtful implementation of evidence-based practices. Racism, poverty and community violence are some commonly experienced social determinants of health that may precipitate mental health needs, limit access to timely and quality mental healthcare and expedite entry into the legal system (18–24). Implementation of evidence-based interventions must strive to reduce the trauma and violence frequently encountered inside facilities, impacting both youth (e.g., peer-to-peer violence, seclusion as punishment) and staff (e.g., assaults on staff) (25, 26). Facility-wide efforts to reduce trauma exposure, address mental health needs, and prevent future legal involvement are desperately needed.
Dialectical behavior therapy (DBT), which was originally developed to treat adults exhibiting suicidal behavior (27), utilizes acceptance, behavioral change, and cognitive intervention strategies collaboratively with clients to achieve behavioral targets, prioritized by order of severity. Priority treatment targets include behaviors harmful to self and/or others, followed by therapy- and quality of life-interfering behaviors, other symptom relief, achieving individual goals and greater self-respect, in service of building a “life worth living.” DBT teaches adaptive core skills of mindfulness, distress tolerance, interpersonal effectiveness, and emotion regulation. Due to its effectiveness in promoting the development of emotional and behavioral management skills, DBT has been adapted to treat conditions associated with emotional dysregulation [e.g., oppositional defiant disorder, eating disorders; (28–30)] and to build positive emotions, resilience, and social-emotional learning (31, 32).
DBT's adaptation for adolescents (DBT-A) incorporates families into treatment and a middle path skills training module, which seeks to synthesize two seemingly opposite positions common to parent-child relationships [e.g., over-pathologizing normal behavior vs. normalizing pathological behavior; (33)]. To attain optimal results, comprehensive DBT-A includes: (1) individual therapy, (2) group skills training to teach skills and enhance capabilities, (3) coaching to ensure generalization of acquired skills, (4) family DBT “as needed” to teach caregivers skills and for structuring the environment in support of treatment, and (5) consultation teams to provide support, enhance skills, and increase motivation among providers (34).
DBT has also been adapted for incarcerated populations (DBT Corrections-Modified; DBT-CM) (35), with modifications to the manual language and content of “real life” scenarios to make them more understandable and relevant (e.g., vocabulary and pictures for the lower educational level common to incarcerated populations). Skills training also includes plans for after release (36). DBT-CM has been implemented in juvenile correctional settings and found to reduce aggressive behavior, suicidal ideation, and recidivism (36–38).
Comprehensive DBT has better outcomes than without all DBT elements (39). It involves training for youth and staff, which is crucial given evidence that implementation of trauma-informed practices addresses correctional violence only if a certain threshold of both youth and staff are trained (40). A recent scoping review revealed eight published studies evaluating the effectiveness of DBT in secure youth forensic settings (41). Existing literature on DBT within these settings is limited and relies on predominantly small sample sizes of youth (i.e., half had 90 or fewer participants) in single facilities and using within-subjects designs without comparison conditions. No studies reviewed evaluated comprehensive DBT; one intended to, however environmental demands prevented them from doing so (42). This review also documented how implementation of DBT in these settings can be challenging due to lack of resources, lack of staff or staff turnover, or uncertainty about best practices for program implementation (43, 44).
The current pilot study was an academic-community partnership examining a comprehensive DBT-A program implemented in a long-term, post-adjudication juvenile correctional treatment center. The aim was to gather preliminary evidence regarding the impact of participating in comprehensive DBT-A on youth mental health and emotion regulation. It was hypothesized youth would exhibit improvements in emotion regulation and mental health. This pilot study also aims to document one facility's approach to implementing comprehensive DBT-A, in the hopes that lessons learned could guide other facilities interested in developing such programs.
2. Method
2.1. Facility
Participants resided in a county-operated 96-bed juvenile correctional treatment center serving adolescent boys and girls. Youth are court ordered to this secure facility, typically after multiple adjudications and efforts to provide community-based supervision and treatment. All youth in the facility receive comprehensive DBT-A from a multidisciplinary treatment team; youth can also receive psychiatric care and substance use treatment, as needed. The facility was selected because of the: (1) established multidisciplinary treatment structure which facilitated effective coordination of DBT-A; (2) average length of stay for youth in the facility, which allowed the opportunity to complete all skills training modules (approximately 6 months); and (3) population of English-speaking youth who had been difficult to engage in lesser intensive settings and with other treatment modalities but had not yet been convicted of an aggravated crime which typically would lead to the commitment to the state juvenile system.
2.2. Program
In 2017, the county obtained grant support to acquire intensive training and consultation in the implementation of comprehensive DBT-A. DBT-A was selected due to its developmental appropriateness (e.g., skills training to help adolescents resolve age specific challenges, incorporates family); the curriculum was adapted to include elements of DBT-CM and DBT for substance use disorders to meet the specific needs of incarcerated youth.1
2.2.1. Staff training
All participating administrators, medical, educational, mental health and direct care staff participated in a yearlong intensive training schedule including: (1) introduction of the DBT-A model to executive leadership during one 8-hour session; (2) four 8-hour sessions with clinicians on utilizing DBT-A within individual, group, and family sessions; (3) five 8-hour sessions with clinicians, correctional supervisors, and direct care staff on implementing skills training modules within the milieu; (4) five different consultation teams discussing implementation issues with the expert trainer for 2 h per month over 6 months; and (5) another 8-hour session with executive management to review progress and formulate future plans. Ongoing consultation with the DBT trainer and annual booster training for the entire facility has continued since. Regarding turnover, the introductory DBT-A training is offered with each new officer orientation. Two DBT coaches (mid-level correctional staff) also provide shoulder-to-shoulder training and coaching as staff utilize DBT-A in their daily interactions with teens.
2.2.2. DBT-A components
Participating youth received the following services from trained master's level licensed clinicians: (1) weekly individual therapy; (2) weekly skills training groups; (3) bi-weekly family therapy; and (4) multi-family skills training groups. Youth also had access to skills coaching in the milieu by direct care staff, designated DBT coaches, and clinicians. Diary Cards were completed weekly and reviewed in individual therapy. Behavior Chain Analyses were completed regularly for effective and ineffective behaviors. Families were invited to attend biweekly family therapy with their teen, weekly visitation hours, and multifamily DBT focused sessions. Parental attendance was documented for family therapy and multifamily sessions and included in reports to probation and the court with annual participation rates ranging from 80%-92%.
Once youth completed all 18 skills groups and the accompanying homework, they took a DBT Competency Exam and participated in a coaching role play to determine whether they fundamentally grasped DBT-A concepts; in the history of the program, except for two youth, all have passed this exam on their first attempt. Youth then participated in a three-week Crime Review group (adapted from DBT-CM) led by a DBT-A clinician, completing a behavior chain analysis on their referring offense and learning skills that could have been used to interrupt the chain of events. Youth also participated in a Graduation Review presentation in which they acknowledged their accomplishments in placement, shared their therapeutic gains, and discussed their future plans.
Multidisciplinary treatment teams met weekly to address youth's treatment needs, progress, and award incentives. These teams ensured youth made progress toward treatment targets and directed adaptations as needed to meet any individual needs. Treatment targets on diary cards were evaluated to ensure they were realistic and attainable, and specialized interventions were developed for additional support in achieving these targets (e.g., individual coaching in the milieu to understand instructions and manage transitions and feelings in the moment). Clinicians and direct care staff utilized DBT-A strategies such as validation, “foot in the door” and “pros and cons” to encourage willingness to engage in treatment. With full recognition of the external pressures experienced by youth as the result of incarceration and court-mandated requirements for release, it was especially important to avoid coercive demands for compliance in favor of an emphasis on acceptance and validation.
Consultation Teams provide emotional support and validation for direct care staff and mental health providers, help ensure treatment fidelity, improve provider capabilities and reduce burn-out (45, 46). Mental health providers had regular consultation team meetings and the Staff Education and Support Meeting functioned as the Consultation Team for direct care staff; correctional supervisory staff regularly attended and direct care staff rotated attendance due to shift schedules (47). Clinicians facilitated these meetings to validate experiences working with youth and promote learning and practicing DBT-A skills which they, in turn, can offer as they coach youth within the milieu.
The facility's behavioral intervention plan was improved to align more generally with DBT-A principles and emphasize supportive and trauma informed approaches. The reward system focused on encouraging skillful behavior through increasing privileges and autonomy and discouraging unskillful behavior through consequences designed to expand learning opportunities. Youth exhibiting harmful or severely program disruptive behavior requiring separation from the general population were expected to follow the Egregious Behavior Protocol; they completed a behavior chain analysis of the incident and reviewed it with staff to identify unique vulnerabilities and triggers leading to the incident and to determine specific skills or behavior necessary to prevent future incidents. Youth remained on protocol until completion of the repair consisting of correction/overcorrection. Youth corrected damage caused by their behavior (e.g., fixing or paying for property they destroyed, working to repair damage to relationships) and overcorrected by identifying, learning, and practicing a new behavior or skill designed to break the old behavioral pattern.
2.3. Participants
Youth included in the current analysis (N = 212) participated in the comprehensive DBT-A program from its 2017 inception through October 2021. Youth who completed pre- and post-tests (n = 113) were the primary analytic sample. Youth who were missing post-test information were not included in primary analyses (n = 99); these youth did not significantly differ from those included on any demographic factors or primary variables of interest at pre-test. Type of discharge differed between those included (92.0% successful, 3.5% unsuccessful, 0.9% alternate placement, 3.5% probation expired) and excluded (65.7% successful, 26.3% unsuccessful, 1.0% alternate placement, 4.0% probation expired, 3% unknown). Excluded youth were significantly more likely to have an unsuccessful discharge and included youth were significantly more likely to have a successful discharge (X2 = 23.86, p < .001); alternate placement and probation expired were not included in the comparison given the small cell sizes.
2.4. Measures
Eight master's level clinicians (full-time facility employees delivering DBT-A) administered the following self-report measures within 30 days of admission (pre-test) and 30 days before discharge (post-test). Clinicians also recorded youth demographic information.
2.4.1. Difficulties in emotion regulation scale short form (DERS-Sf)
The DERS-SF (48) is an 18-item assessment of an individual's ability to manage feelings. Responses are rated from 1 (almost never) to 5 (almost always) and averaged to create six, three-item subscales: strategies (α: pre = .49, post = .72), non-acceptance (α: pre = .72, post = .76), impulse (α: pre = .88, post = .90), goals (α: pre = .86, post = .86), awareness (α: pre = .74, post = .82), and clarity (α: pre = .66, post = .65); item level data to calculate alphas was only available for a subset of youth (n = 80–96 depending on subscale and timepoint) and the remainder had subscale scores only. Higher scores reflect greater emotion dysregulation.
2.4.2. Beck youth inventories, 2nd edition (BYI-2)
The BYI-2 (49) is a 100-item assessment of emotional and social impairments. Responses are rated from 0 (never) to 3 (always) and summed to create raw totals for five, 20-item subscales: self-concept, anxiety, depression, anger, and disruptive behavior. Raw scores are converted to t-scores using age- and gender-based norms. T-scores are interpreted as: 55 or less = average, 55–59 = mildly elevated, 60–69 = moderately elevated, and 70+=extremely elevated; for self-concept, t-scores in the elevated ranges reflect more positive self-concept compared to peers. BYI-2 data was only available for a subset of the sample (approximately 40%) primarily due to measure supply shortages. Item-level data used to calculate alphas was available for only a subset of those youth (n = 29–34 depending on subscale and timepoint). Alphas at pre- and post-test, respectively are: self-concept (.88,.88), anxiety (.92,.88), depression (.92,.93), anger (.94,.92), and disruptive behavior (.88,.88).
2.4.3. Adolescent anger rating scale (AARS)
The AARS (50) is a 41-item assessment of anger responses. Responses are rated from 1 (hardly ever) to 4 (very often) and summed to created three subscales: Instrumental Anger (20 items), Reactive Anger (8 items), and Anger Control (13 items); the raw total for the subscale anger control is subtracted from the sum of the instrumental and reactive anger subscales to obtain a total anger subscale. Although the assessment has grade- and gender-based norms, the current study compared the raw total scores because: (1) youth in the facility are on average 2 grades behind their same-age peers, often due to frequent moves and truancy (based on facility data), and (2) the grade level of most youth was not recorded at the time the measures were administered. AARS data was only available for a subset of the sample (approximately 61%) also because of measure supply shortages. Alphas at pre- and post-test, respectively are: instrumental anger (.84, .85), reactive anger (.85, .82), and anger control (.75, .82).
2.4.4. Trauma symptom checklist for children (TSCC)
The TSCC (51) is a 54-item measure of youth posttraumatic symptomatology. Items are rated from 0 (never) to 3 (almost all the time), summed to create raw scores, and converted to t-scores using age- and gender-based norms. Clinical scales include: Anxiety (9 items; α: pre = .80, post = .70), Depression (9 items; α: pre = .84, post = .76), Anger (9 items; α: pre = .89, post = .82), Posttraumatic Stress (10 items; α: pre = .89, post = .82), Dissociation (10 items; α: pre = .85, post = .81), and Sexual Concerns (10 items; α: pre = .73, post = .74). Twenty-two items are included in multiple subscales. The TSCC also includes validity scales assessing under- and hyper-reporting.
2.4.5. Juvenile victimization questionnaire, 2nd revision, reduced item (JVQ-R2)
The JVQ-R2 (52) is a 12-item shortened version of the original Juvenile Victimization Questionnaire (53). Youth respond yes or no to each item asking if they have experienced the following types of victimization: emotional maltreatment (2 items), witnessing (3 items), physical maltreatment (4 items), property assault (1 item), and sexual victimization (2 items). The cutoff for polyvictimization is 5 or more endorsed items.
2.5. Plan of analysis
All analyses were conducted using SPSS v.28 statistical software. Preliminary analyses included descriptive statistics of all study variables. Dependent samples t-tests were used to assess pre/post changes in emotion regulation and mental health symptoms. Cohen's d was calculated as a measure of effect size and is interpreted following Cohen's (1988) established guidelines (0.20 = small, 0.50 = medium, 0.80 = large) (54).
We also examined whether pre-test demographic and mental health characteristics were related to type of discharge from the program (successful vs. unsuccessful). These analyses incorporated the full sample for whom type of discharge was known (n = 198). Chi-square tests were used for categorical variables (e.g., gender, race and ethnicity) and t-tests for continuous variables (e.g., mental health variables, age, length of stay).
3. Results
3.1. Sample characteristics
Youth (n = 113) were on average 15.37 years old (SD = 1.10, range = 13–17), 68.1% boys, and identified as 69.0% Latinx, 22.1% Black, 8.0% White, and 0.9% Native American. At pre-test, 95% of youth reported lifetime trauma exposure. Additional characteristics are presented in Table 1.
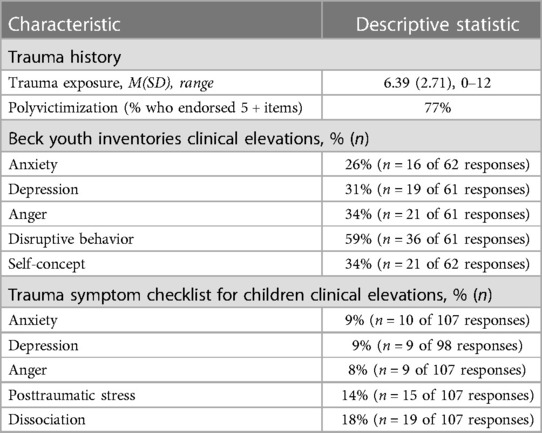
Table 1. mental health and trauma exposure characteristics of juvenile correctional center youth participants (2017-2021).
3.2. Changes in emotion regulation and mental health symptoms
Results are displayed in Table 2. Improvements in emotion regulation were observed on the DERS-SF, in all subscales except non-acceptance, representing small to medium effects (d's = 0.20–0.37). Improvement in anger control on the AARS was also observed, with medium effect sizes for total, instrumental, and reactive anger (d = 0.50–0.68) and a small effect (d = .21) for anger control.
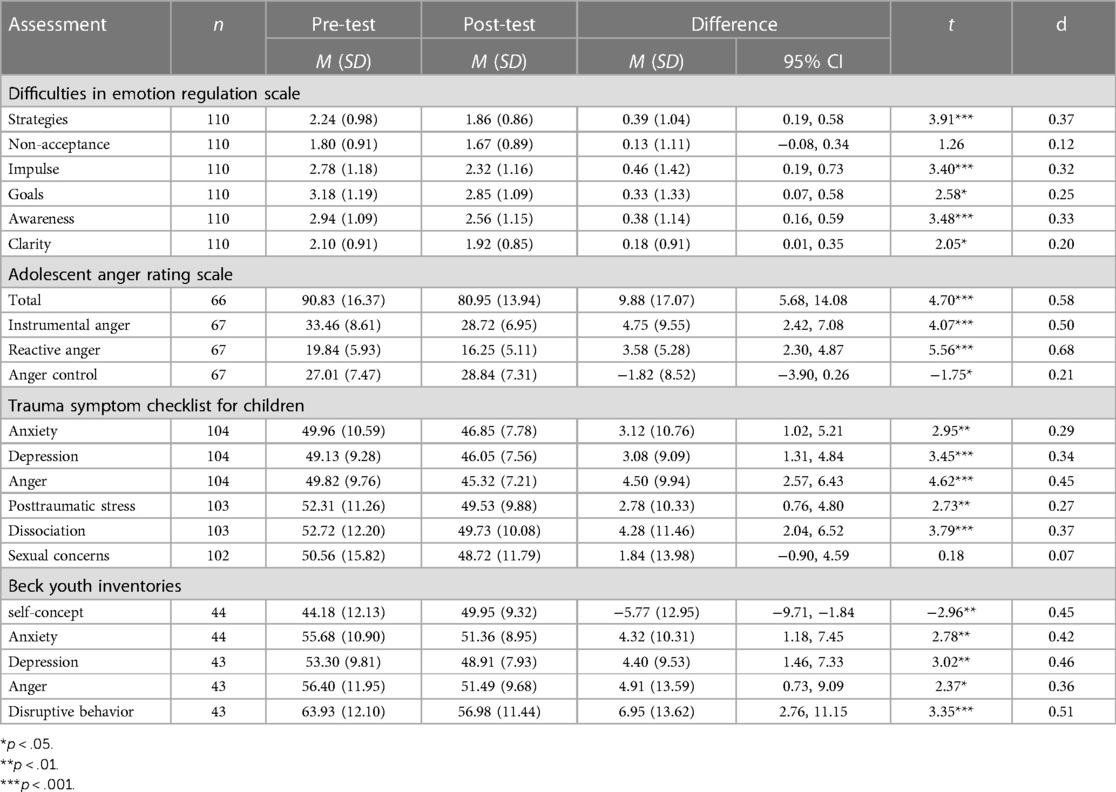
Table 2. Changes in emotion regulation and mental health symptoms following participation in a comprehensive DBT program.
Improvements in mental health were observed on all TSCC domains except sexual concerns, representing small to medium effect sizes (d's = 0.20–0.45). Most youth (72.6%, n = 77) produced valid TSCC responses, with no significant elevations on the under or overreporting subscales at pre- or post-test. At pre-test, 15.0% of respondents were elevated on the underreporting subscale and 3.7% on the overreporting subscale. At post-test, 17.3% of respondents were elevated on underreporting and 0.9% on overreporting. Analyses of TSCC data were conducted excluding respondents with elevations on validity scales; findings were consistent with analyses of the full sample, with the exception sexual concerns. Anxiety [t(76) = 1.90, p = .030, d = 0.22], depression [t(76) = 2.84], p = .003, d = 0.32), anger, t(76) = 4.05, p < .001, d = 0.46), posttraumatic stress [t(76) = 2.35, p = .011, d = 0.27], and dissociation [t(76) = 3.62], p < .001, d = 0.41) all improved; no changes were observed in sexual concerns [t(75) = 0.18, p = .276, d = 0.07].
Improvements in mental health on all domains of the BYI were also observed, reflecting small to medium effects (d’s = .36-0.51).
3.3. Characteristics related to type of discharge
Boys were significantly more likely to be unsuccessfully discharged and girls more likely to be successfully discharged than expected (X2 = 4.05, p = .044). There were no significant differences in type of discharge based on age, race, ethnicity, length of stay in the facility, or any mental health characteristic at pre-test.
4. Discussion
The current pilot study evaluated a comprehensive DBT-A program in a juvenile correctional treatment center. Consistent with prior studies of DBT in juvenile incarceration settings, improvements in mental health symptoms and emotion regulation were observed from pre- to post-treatment (36, 55, 56). This is promising given the documented high rates of mental health symptoms and disorders among incarcerated youth, as well as their elevated risk for suicide (57). Furthermore, evidence indicates improving emotion regulation during incarceration reduces the likelihood of youth recidivism (58). These findings build upon a growing literature showing DBT is a promising intervention for treating emotion dysregulation and can be successfully implemented in juvenile forensic settings (28–30).
Implementation required significant resources and commitment from the county and facility. Prior studies show comprehensive DBT can be difficult to implement in juvenile correctional settings due to lack of resources, insufficient staffing, and uncertainty about how best to implement the program (43, 44). Implementation was costly due to the scarcity of expert training available, need for intensive initial training followed by ongoing training and consultation to minimize learning loss and consultation to ensure fidelity, and the importance of acquiring essential therapeutic resources (e.g., trauma-informed care intervention tools, incentives); for many facilities this approach is cost prohibitive.
The institution's multidisciplinary organizational structure was crucial to facilitating implementation, however this may not be standard in other facilities. Comprehensive DBT can be challenging to implement due to limited communication and coordination of interventions by mental health and correctional staff (59). Put simply, mental health staff often incorporate acceptance-based interventions (e.g., increasing self-awareness, validating emotions) whereas correctional staff interventions are generally change-based (e.g., environmental structure using a plan of contingencies to modify behavior). Comprehensive DBT is unique in seeking to enhance mutual understanding between these two seemingly opposite approaches, as illustrated by one of its fundamental assumptions: People may not have caused all their problems (acceptance), yet they must solve them anyway (change).
Successful comprehensive DBT-A implementation required a commitment to truly collaborative work to create fully functioning multidisciplinary teams sharing the goal of accepting the youths’ experiences, perspectives, feelings and thoughts as valid while simultaneously helping them navigate systems of accountability. The legal system has not demonstrated effectiveness in reducing recidivism or improving youth wellbeing, so clinicians and correctional staff can use DBT to balance acceptance of limitations and work toward necessary change of the systems they uphold. Building effective communication to overcome distrust and improve collaboration between treatment and corrections professionals is addressed specifically in consultation team meetings. Effective DBT multidisciplinary teams work to find solutions so youth obtain the intended benefit of the treatment tool while at the same time, minimize potential risks of harm to self and others within the facility.
4.1. Strengths, limitations, and future directions
This study adds to the literature as it is the first evaluation, to our knowledge, of comprehensive DBT-A in a secure youth forensic setting. Strengths include use of empirically validated assessments, inclusion of girls and boys and an ethnoracially diverse sample, and a larger sample than most prior studies evaluating DBT in secure youth incarceration settings (41). This pilot study also reflects real-world challenges to both the empirical analysis of treatment effects as well as the implementation of a comprehensive DBT-A treatment model in a juvenile correctional setting. First, the study relied on archival self-report data collected as part of a program evaluation involving a pre-post design and no comparison condition. This may limit confidence in the findings as change in outcomes could be due to maturation or timing effects or to other interventions received (e.g., psychiatric or substance use services). Federal protections for research with incarcerated youth necessarily limit the use of control groups, however future research should consider alternate designs (e.g., interrupted time series) to examine effectiveness (60). Although rigorous and valuable, randomized control trials are not always possible and alternate designs can provide useful evidence regarding the effectiveness of interventions (61). Future research should also incorporate behavioral (e.g., frequency of self-harm behavior) and collateral data (e.g., incident reports, frequency of restraint use) to understand the full impact of participation in DBT-A in a correctional setting.
Second, it is possible the sample was biased toward documenting improvements, as youth with available post-treatment data were more likely to be successfully discharged than those with only pre-treatment data. Discharge decisions are complex and treatment length therefore is individualized. Future studies should maximize post-treatment data collection from youth with unsuccessful discharges, including by providing opportunities to complete assessments post-release or in new placement settings.
Third, the current sample was from a single facility and impacted by the available resources. Running out of paid assessment measures and human-error (e.g., missing the backside of double-sided forms, youth refusal to complete full assessment batteries) resulted in missing data. Data gathering, management and analysis could be strengthened by establishing early partnerships with academic centers. Fidelity was supported through consultation team meetings and DBT coaches assisting staff, but not monitored systematically, a consideration for future studies.
Fourth, although our sample was racially diverse, analyses were not sufficiently powered to examine differential effectiveness of the intervention on youth from different ethnoracial backgrounds. Detailed data on youth ethnicity, beyond whether they identified as Latinx, was also unavailable. Future research should explore whether youth from certain ethnoracial groups and other identities (e.g., gender) benefit differentially from DBT-A.
Fifth, additional research is needed to examine the long-term effects of comprehensive DBT-A on youth and society more broadly. Our study was limited to examining changes in mental health and emotion regulation during incarceration; future research should examine impacts on post-incarceration outcomes such as recidivism, family cohesion and linkage to ongoing mental health treatment, as well as on staff burnout, turnover, and secondary traumatic stress. Finally, future research should consider the social and monetary cost of implementing comprehensive DBT-A in correctional settings as opposed to in the community.
5. Conclusion
Findings from the current study build upon a growing literature showing DBT-A is a promising intervention well-suited for treating emotion dysregulation and mental health conditions. With careful attention to the context of youth incarceration (e.g., punitive and mandated nature of incarceration, need for collaboration with legal system direct care staff), comprehensive DBT-A can be successfully implemented in secure juvenile forensic settings.
Data availability statement
Due to the sensitive nature of the data collected from incarcerated youth, data is not publicly available. Requests to access the datasets should be directed to Johanna Folk,am9oYW5uYS5mb2xrQHVjc2YuZWR1.
Ethics statement
The studies involving humans were approved by The University Of Texas Health Science Center At San Antonio Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin because this project was approved as "non-human subjects research"; only de-identified chart review data was used.
Author contributions
The first, second, third, and last authors conceptualized and drafted the first version of the manuscript. The first author conducted data analysis. The third author conceptualized the program implementation and data collection plan. The third and fourth authors assisted with data collection and management. All authors participated in the interpretation of findings and the writing and editing process. All authors contributed to the article and approved the submitted version.
Funding
Initial funding for this work was provided by the Texas Office of the Governor, Criminal Justice Division with further support provided, in part, by the County Grants Department operated by the Texas Juvenile Justice Department. Johanna Folk receives salary support from the National Institute on Drug Abuse (K23DA050798).
Acknowledgments
This research would not have been possible without the adolescents who participated, the staff who gave their time and effort to implement the program and support the evaluation, and the support of the Bexar County Juvenile Probation Department. We also wish to acknowledge Ashley Powell, PhD who contributed to the original conceptualization and planning of this manuscript, and Michele Galietta, PhD for her role in training staff, developing the data collection plan, and critically reviewing this manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author JF declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Footnote
1Additional details regarding the implementation plan, training materials, and adapted intervention materials are available upon request to Anne Thomas (athomas1234@att.net).
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Sawyer W. Youth confinement: The whole pie. Northampton, MA: Prison Policy Initiative (2019). Available at: https://www.prisonpolicy.org/reports/youth2019.html (Accessed April 14, 2023).
2. Colins O, Vermeiren R, Vreugdenhil C, van den Brink W, Doreleijers T, Broekaert E. Psychiatric disorders in detained male adolescents: a systematic literature review. Can J Psychiatry. (2010) 55(4):255–63. doi: 10.1177/070674371005500409
3. Gilbert AL, Grande TL, Hallman J, Underwood LA. Screening incarcerated juveniles using the MAYSI-2. J Correct Health Care. (2015) 21(1):35–44. doi: 10.1177/1078345814557788
4. McCuish EC. Substance use profiles among juvenile offenders: a lifestyles theoretical perspective. J Drug Issues. (2017) 47(3):448–66. doi: 10.1177/0022042617699197
5. Peltonen K, Ellonen N, Pitkänen J, Aaltonen M, Martikainen P. Trauma and violent offending among adolescents: a birth cohort study. J Epidemiol Community Health. (2020) 74(10):845–50. doi: 10.1136/jech-2020-214188
6. Teplin LA, Abram KM, McClelland GM, Dulcan MK, Mericle AA. Psychiatric disorders in youth in juvenile detention. Arch Gen Psychiatry. (2002) 59(12):1133–43. doi: 10.1001/archpsyc.59.12.1133
7. Underwood LA, Washington A. Mental illness and juvenile offenders. Int J Environ Res Public Health. (2016) 13(2):228. doi: 10.3390/ijerph13020228
8. Wasserman GA, McReynolds LS, Schwalbe CS, Keating JM, Jones SA. Psychiatric disorder, comorbidity, and suicidal behavior in juvenile justice youth. Crim Justice Behav. (2010) 37(12):1361–76. doi: 10.1177/0093854810382751
9. Teplin LA, Potthoff LM, Aaby DA, Welty LJ, Dulcan MK, Abram KM. Prevalence, comorbidity, and continuity of psychiatric disorders in a 15-year longitudinal study of youths involved in the juvenile justice system. JAMA Pediatr. (2021) 175(7):e205807. doi: 10.1001/jamapediatrics.2020.5807
10. Abram KM, Teplin LA, McClelland GM, Dulcan MK. Comorbid psychiatric disorders in youth in juvenile detention. Arch Gen Psychiatry. (2003) 60(11):1097–108. doi: 10.1001/archpsyc.60.11.1097
11. Weber S, Lynch S. Understanding the relations among adverse childhood experiences (ACE), substance use, and reoffending among detained youth. Child Abuse Negl. (2021) 120:105211. doi: 10.1016/j.chiabu.2021.105211
12. Atkins DL, Pumariega AJ, Rogers K, Montgomery L, Nybro C, Jeffers G, et al. Mental health and incarcerated youth. I: prevalence and nature of psychopathology. J Child Fam Stud. (1999) 8(2):193–204. doi: 10.1023/A:1022040018365
13. Kelly EL, Novaco RW, Cauffman E. Anger and depression among incarcerated male youth: predictors of violent and non-violent offending during adjustment to incarceration. J Consult Clin Psychol. (2019) 87(8):693–705. doi: 10.1037/ccp0000420
14. Barnert ES, Abrams LS, Tesema L, Dudovitz R, Nelson BB, Coker T, et al. Child incarceration and long-term adult health outcomes: a longitudinal study. Int J Prison Health. (2018) 14(1):26–33. doi: 10.1108/IJPH-09-2016-0052
15. Barnert ES, Dudovitz R, Nelson BB, Coker TR, Biely C, Li N, et al. How does incarcerating young people affect their adult health outcomes? Pediatrics. (2017) 139(2):e20162624. doi: 10.1542/peds.2016-2624
16. Gilman AB, Hill KG, Hawkins JD. When is youths’ debt to society paid off? Examining the long-term consequences of juvenile incarceration for adult functioning. J Dev Life Course Criminol. (2015) 1(1):33–47. doi: 10.1007/s40865-015-0002-5
17. Massoglia M, Pare PP, Schnittker J, Gagnon A. The relationship between incarceration and premature adult mortality: gender specific evidence. Soc Sci Res. (2014) 46:142–54. doi: 10.1016/j.ssresearch.2014.03.002
18. Anoshiravani A. Addressing the unmet health needs of justice system-involved youth. The Lancet Public Health. (2020) 5(2):e83. doi: 10.1016/S2468-2667(19)30251-8
19. Borschmann R, Janca E, Carter A, Willoughby M, Hughes N, Snow K, et al. The health of adolescents in detention: a global scoping review. The Lancet Public Health. (2020) 5(2):e114–26. doi: 10.1016/S2468-2667(19)30217-8
20. Jones MS, Pierce H. Early exposure to adverse childhood experiences and youth delinquent behavior in Fragile families. Youth Soc. (2021) 53(5):841–67. doi: 10.1177/0044118X20908759
21. Turner D, Wolf AJ, Barra S, Müller M, Gregório Hertz P, Huss M, et al. The association between adverse childhood experiences and mental health problems in young offenders. Eur Child Adolesc Psychiatry. (2021) 30(8):1195–207. doi: 10.1007/s00787-020-01608-2
22. Lacey C. Racial disparities and the juvenile justice system: a legacy of trauma (2013). Los Angeles, CA and Durham, NC: National Center for Child Traumatic Stress. Available at: https://www.nctsn.org/sites/default/files/resources//racial_disparities_and_juvenile_justice_system_legacy_of_trauma.pdf (Accessed April 14, 2023).
23. Rovner J. Black disparities in youth incarceration. Washington, DC: The Sentencing Project (2021). Available at: https://www.sentencingproject.org/publications/black-disparities-youth-incarceration/ (Accessed April 14, 2023).
24. Janku A D, Yan J. Exploring patterns of court-ordered mental health services for juvenile offenders: is there evidence of systemic bias? Crim Justice Behav. (2009) 36(4):402–19. doi: 10.1177/0093854808330799
25. Mendel RA. No place for kids: the case for reducing juvenile incarceration. Baltimore, MD: Annie E. Casey Foundation (2011). Available at: https://assets.aecf.org/m/resourcedoc/aecf-NoPlaceForKidsFullReport-2011.pdf (Accessed April 14, 2023).
26. Mendel RA. Maltreatment of youth in U.S. Juvenile corrections facilities: an update. Baltimore, MD: Annie E. Casey Foundation (2015). Available at: https://assets.aecf.org/m/resourcedoc/aecf-maltreatmentyouthuscorrections-2015.pdf (Accessed April 14, 2023).
27. Linehan MM, Armstrong HE, Suarez A, Allmon D, Heard HL. Cognitive-behavioral treatment of chronically parasuicidal borderline patients. Arch Gen Psychiatry. (1991) 48(12):1060–4. doi: 10.1001/archpsyc.1991.01810360024003
28. Kenny TE, Carter JC, Safer DL. Dialectical behavior therapy guided self-help for binge-eating disorder. Eat Disord. (2020) 28(2):202–11. doi: 10.1080/10640266.2019.1678982
29. Linehan MM, Wilks CR. The course and evolution of dialectical behavior therapy. Am J Psychother. (2015) 69(2):97–110. doi: 10.1176/appi.psychotherapy.2015.69.2.97
30. Nelson-Gray RO, Keane SP, Hurst RM, Mitchell JT, Warburton JB, Chok JT, et al. A modified DBT skills training program for oppositional defiant adolescents: promising preliminary findings. Behav Res Ther. (2006) 44(12):1811–20. doi: 10.1016/j.brat.2006.01.004
31. Lee S, Mason M. Effectiveness of brief DBT-informed group therapy on psychological resilience: a preliminary naturalistic study. J College Stud Psychother. (2019) 33(1):25–37. doi: 10.1080/87568225.2018.1425646
32. Mazza JJ, Dexter-Mazza ET. DBT Skills in schools: implementation of the DBT steps—a social emotional curriculum. In: Swales MA, editor. The Oxford handbook of dialectical behaviour therapy. New York, NY, US: Oxford University Press; (2019). p. 719–33.
34. Miller AL, Rathus JH, Linehan MM. Dialectical behavior therapy with suicidal adolescents. New York: Guilford Press (2007).
35. Berzins LG, Trestman RL. The development and implementation of dialectical behavior therapy in forensic settings. Int J Forensic Ment Health. (2004) 3(1):93–103. doi: 10.1080/14999013.2004.10471199
36. Shelton D, Kesten K, Zhang W, Trestman R. Impact of a dialectic behavior therapy - corrections modified (DBT-CM) upon behaviorally challenged incarcerated male adolescents. J Child Adolesc Psychiatr Nurs. (2011) 24(2):105–13. doi: 10.1111/j.1744-6171.2011.00275.x
37. Fox AM, Miksicek D, Veele S, Rogers B. An evaluation of dialectical behavior therapy for juveniles in secure residential facilities. J Offender Rehabil. (2020) 59(8):478–502. doi: 10.1080/10509674.2020.1808557
38. Per M, Spinelli C, Sadowski I, Schmelefske E, Anand L, Khoury B. Evaluating the effectiveness of mindfulness-based interventions in incarcerated populations: a meta-analysis. Crim Justice Behav. (2020) 47(3):310–30. doi: 10.1177/0093854819891457
39. Tomlinson MF. A theoretical and empirical review of dialectical behavior therapy within forensic psychiatric and correctional settings worldwide. Int J Forensic Ment Health. (2018) 17(1):72–95. doi: 10.1080/14999013.2017.1416003
40. Baetz CL, Surko M, Moaveni M, McNair F, Bart A, Workman S, et al. Impact of a trauma-informed intervention for youth and staff on rates of violence in juvenile detention settings. J Interpers Violence. (2021) 36(17–18):NP9463–82. doi: 10.1177/0886260519857163
41. Yang P, Folk JB, Lugosi SI, Bemat Z, Thomas A, Robles-Ramamurthy B. Dialectical behavior therapy in juvenile correctional and detention facilities: a scoping review. Journal of Correctional Healthcare. (2023) 29(5):355–69. doi: 10.1089/jchc.22.05.0041
42. Wakeman EE. Modified core mindfulness skills training in an adolescent female correctional sample [Thesis Tuscaloosa (AL)): University of Alabama (2010).
43. Fox KC, Whitt AL. Telemedicine can improve the health of youths in detention. J Telemed Telecare. (2008) 14(6):275–6. doi: 10.1258/jtt.2008.008002
44. Restum ZG. Public health implications of substandard correctional health care. Am J Public Health. (2005) 95(10):1689–91. doi: 10.2105/AJPH.2004.055053
45. Carmel A, Fruzzetti AE, Rose ML. Dialectical behavior therapy training to reduce clinical burnout in a public behavioral health system. Community Ment Health J. (2014) 50(1):25–30. doi: 10.1007/s10597-013-9679-2
46. Haynos AF, Fruzzetti AE, Anderson C, Briggs D, Walenta J. Effects of dialectical behavior therapy skills training on outcomes for mental health staff in a child and adolescent residential setting. J Hosp Adm. (2016) 5(2):55–61. doi: 10.5430/jha.v5n2p55
47. Galietta M. “Dialectical behavior therapy in correctional settings”. In: Jeglic E, Calkins C, editors. New frontiers in offender treatment – the translation of evidence-based practices to correctional settings. New York: Springer (2018). p. 147–69.
48. Kaufman EA, Xia M, Fosco G, Yaptangco M, Skidmore CR, Crowell SE. The difficulties in emotion regulation scale short form (DERS-SF): validation and replication in adolescent and adult samples. J Psychopathol Behav Assess. (2016) 38(3):443–55. doi: 10.1007/s10862-015-9529-3
49. Beck JS, Beck AT, Jolly JB. BECK Youth inventories of emotional and social impairment. New York: Psychological Corporation (2001).
50. Burney DM, Kromrey J. Initial development and score validation of the adolescent anger rating scale. Educ Psychol Meas. (2001) 61(3):446–60. doi: 10.1177/00131640121971310
51. Briere J. Trauma symptom checklist for children: professional manual. Florida: Psychological Assessment Resources Inc (1996).
52. Finkelhor D, Hamby SL, Turner H, Ormrod R. The juvenile victimization questionnaire: 2nd revision (JVQ-R2). New Hampshire: Crimes Against Children Research Center. (2011).
53. Finkelhor D, Hamby SL, Ormrod R, Turner H. The juvenile victimization questionnaire: reliability, validity, and national norms. Child Abuse Negl. (2005) 29(4):383–412. doi: 10.1016/j.chiabu.2004.11.001
54. Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed New York: Routledge (1988).
55. Shelton D. Patterns of treatment services and costs for young offenders with mental disorders. J Child Adolesc Psychiatr Nurs. (2005) 18(3):103–12. doi: 10.1111/j.1744-6171.2005.00013.x
56. Trupin EW, Stewart DG, Beach B, Boesky L. Effectiveness of a dialectical behaviour therapy program for incarcerated female juvenile offenders. Child Adolesc Ment Health. (2002) 7(3):121–7. doi: 10.1111/1475-3588.00022
57. Golzari M, Hunt SJ, Anoshiravani A. The health status of youth in juvenile detention facilities. J Adolesc Health. (2006) 38(6):776–82. doi: 10.1016/j.jadohealth.2005.06.008
58. Docherty M, Lieman A, Gordon BL. Improvement in emotion regulation while detained predicts lower juvenile recidivism. Youth Violence Juv Justice. (2022) 20(2):164–83. doi: 10.1177/15412040211053786
59. Stone DT, Thomas AC. A multidisciplinary treatment team model for youth offenders. In: Kleinberg JL, editors. Group psychotherapy. New Jersey: Wiley (2012). p. 645–64.
60. Office for Human Research Protections. Prisoner involvement in research. Washington, DC: U.S. Department of Health & Human Services (2003). Available at: https://www.hhs.gov/ohrp/regulations-and-policy/guidance/prisoner-research-ohrp-guidance-2003/index.html (Accessed April 14, 2023).
Keywords: dialectical behavior therapy for adolescents, forensic psychology, adolescent, mental health, juvenile justice
Citation: Folk JB, Yang P, Thomas A, Lyon J, Patel J, Yoon C and Robles-Ramamurthy B (2023) Comprehensive dialectical behavior therapy for adolescents in a juvenile correctional treatment center: a pilot evaluation. Front. Child Adolesc. Psychiatry 2:1207575. doi: 10.3389/frcha.2023.1207575
Received: 17 April 2023; Accepted: 19 October 2023;
Published: 3 November 2023.
Edited by:
Yael Dvir, University of Massachusetts Medical School, United StatesReviewed by:
Boris Lorberg, University of Massachusetts Medical School, United StatesMatt Dobbertin, Boys Town National Research Hospital, United States
© 2023 Folk, Yang, Thomas, Lyon, Patel, Yoon and Robles-Ramamurthy. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Johanna B. Folk am9oYW5uYS5mb2xrQHVjc2YuZWR1
 Johanna B. Folk
Johanna B. Folk Phillip Yang2
Phillip Yang2 Anne Thomas
Anne Thomas Jayme Lyon
Jayme Lyon