
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
PERSPECTIVE article
Front. Child Adolesc. Psychiatry, 15 May 2023
Sec. Interventions for Adolescent Mental Health
Volume 2 - 2023 | https://doi.org/10.3389/frcha.2023.1186722
 Kamyar Keramatian*
Kamyar Keramatian* Emma Morton
Emma Morton
Bipolar disorder (BD) in youth often goes unrecognized and therefore untreated. However, little is known about pathways to treatment of youth with BD and factors that influence the time taken for each stage of these pathways. In this article, we use the conceptual framework by Scott and colleagues called the Model of Pathways to Treatment as a foundation to explore the components of delay in the diagnosis and treatment of youth with BD. The total time from the onset of symptoms until treatment initiation was divided into four sequential intervals; i.e., the Appraisal, the Help-seeking, the Diagnostic and the Pre-treatment intervals and potential disease, patient, and healthcare system/provider factors that influence each interval were identified. This multidimensional conceptual framework can offer a systematic approach to understanding and exploring barriers to early identification and interventions in BD, which is a crucial step in the development of strategies to facilitate prompt diagnosis and treatment. We hope this work contributes to the discussion on delayed diagnosis and treatment of youth with BD and provides a roadmap to inform future research studies and policy decisions.
Bipolar disorder (BD) is a potentially debilitating psychiatric condition characterized by recurrent episodes of depression and (hypo)mania. Statistics Canada data indicates that the lifetime prevalence of BD in Canada is 2.6%, meaning that almost 1 million Canadians are affected (1). BD typically emerges during adolescence and early adulthood and is associated with significant cognitive impairment (2), brain tissue loss (3) and functional disability (4) even in the early stages of the illness. Data from the World Health Organization Global Burden of Disease study ranked BD as the 4th leading cause of disability worldwide among the 10–24 year age group (5). Despite the high prevalence and large disability burden, many studies have shown that BD often goes unrecognized for several years (6, 7). A recently published Canadian multicentre naturalistic study showed that the median delay between the first mood episode and the accurate diagnosis of BD in Canada is 8 years (7). Even more concerning was the median delay of 15 years for pediatric-onset BD. Such prolonged diagnostic delays can result in a subsequent delay in appropriate treatment initiation, which in turn is linked to serious consequences including poor social adjustment (8), disruption of crucial age-specific developmental tasks (9), employment difficulties (10), suboptimal response to mood stabilizing treatment (11), greater severity and frequency of mood episodes (12), higher number of hospitalizations (13), greater risk of developing substance use disorders (14), and elevated risk of suicide (7). In addition, delay in the diagnosis of BD is associated with significantly higher healthcare costs (15) as well as higher indirect costs due to work loss (15, 16). Therefore, accurate identification and appropriate treatment initiation in the earlier stages of BD may lead to improved clinical and functional outcomes and reduction in morbidity in youth with BD as well as cost savings for the healthcare systems.
Previous studies have investigated demographic and clinical factors associated with delays in the diagnosis and treatment of BD. Those would include bipolar disorder subtype (bipolar II disorder), age of onset (younger), polarity of onset (depression), and history of attempted suicide, according to a recently published systematic review (17). However, little is known about pathways to treatment of youth with BD and factors that influence the time taken for each stage of these pathways (i.e., components of delay). A better understanding of these components as well as various factors that can contribute to each component would be a crucial step in the development of strategies to facilitate prompt diagnosis and treatment in youths with BD. To our knowledge, no attempt has been made to analyse components of delay in the diagnosis and treatment of youth with BD. In this article, we use the conceptual framework by Scott and colleagues called the Model of Pathways to Treatment (18) as a foundation to explore the components of delay in the diagnosis and treatment of youth with BD and identify potential factors influencing each component. According to this framework, the total time from the onset of symptoms until treatment initiation is divided into four sequential intervals. The Appraisal interval is defined as the time from the onset of mood symptoms to perceiving a reason to discuss such symptoms with a healthcare professional (HCP). The Help-seeking interval describes the time from perceiving a reason to discuss symptoms with a HCP to the first consultation regarding those symptoms. The Diagnostic interval represents the time between the first appointment with a HCP and receiving the formal diagnosis. The Pre-treatment interval describes the time between receiving the formal diagnosis and initiation of treatment (18). Subsequently, various factors contributing to each interval are grouped into three categories: patient factors (that would also include social, cultural and family factors), healthcare provider and system factors and disease factors (Figure 1). In the following sections, we use this categorization to map out potential factors that influence the time taken for each component of delay in the diagnosis and treatment of youth with BD (see summary in Table 1).
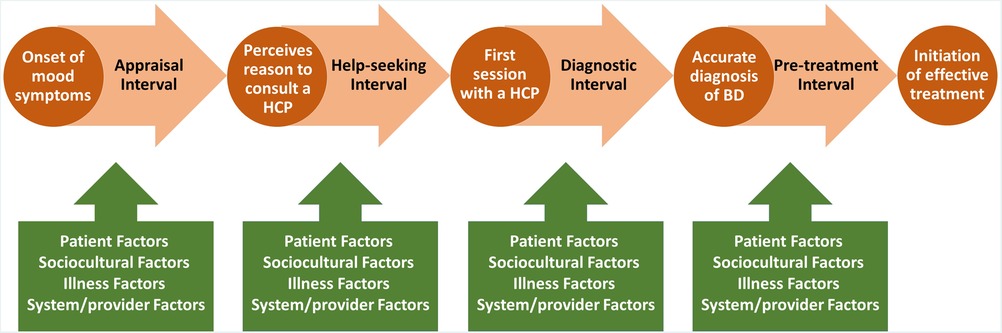
Figure 1. A multidimensional conceptual framework, based on the model of pathways to treatment by Scott et al. (18), to explore potential factors involved in delayed diagnosis and treatment of bipolar disorders in youth. Circles represent key events and arrows represent components of delay.
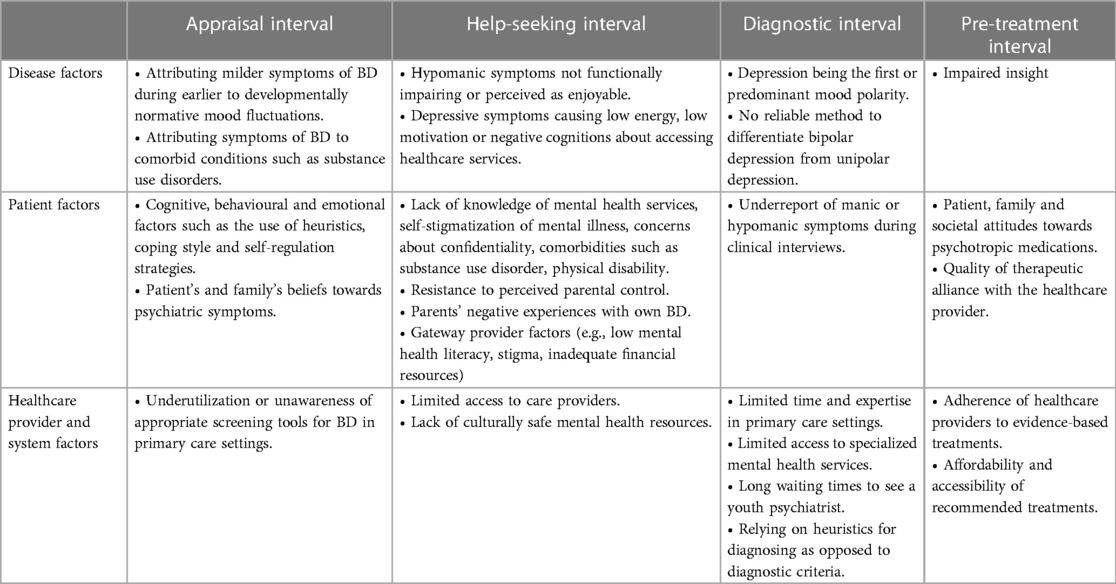
Table 1. Summary of contributing factors to each component of delay in the diagnosis and treatment of youth with bipolar disorder.
The time from detection of first mood symptoms to perceiving a reason to discuss symptoms a HCP can be influenced by disease factors, patient factors (including social, cultural and family context), and healthcare/system factors.
According to the “clinical staging model”, BD can evolve through successive stages from an asymptomatic at-risk period to subclinical mood symptoms in youth, followed by full syndromal mood episodes (19, 20). It is reasonable to assume that milder symptoms of BD during earlier stages of the illness can be mistaken for the developmentally normative mood fluctuations seen in adolescents (21).
Another factor contributing to the Appraisal interval is possible misattribution of mood symptoms to other common conditions in this age group such as substance use, which in fact tends to start after the onset of the index mood episode (22, 23) and may represent a self-management strategy to cope with the very symptoms caused by BD (24).
Cognitive, behavioural and emotional factors can influence individuals' response to the newly detected symptoms and how those symptoms are interpreted (25). Those would include patients' attitude towards mood symptoms, and perceived meaning and significance of these symptoms. Patients also use variety of heuristics, colloquially known as “rules of thumb” or “mental shortcuts”, to make sense of their symptoms and form an interpretation (18). Examples of relevant heuristics would include stress-illness heuristics (symptoms that emerge during times of stress are attributed to stress rather than an illness) and severity rule (only symptoms that are persistent or severe and impact day to day functioning requires psychiatric care) (18). Patients' coping style and self-regulation strategies and evaluation of the effectiveness of these strategies to mitigate mood symptoms may impact their decision to seek professional help for their symptoms.
Youth with BD and their families may hold a wide range of beliefs regarding the origins of psychiatric symptoms in general. These beliefs, which include “normalizing attributions” (26) (attributing the symptoms to non-pathological causes such as environmental stressors, or volitional behaviours), supernatural (27), psychosocial and biological attributions (28), can influence the perception of the need to seek professional care.
A recent systematic review and meta-analysis estimated that about 17% of patents who are diagnosed as having a unipolar depression have unrecognized BD (29). This can be at least partly due to the underutilization or unawareness of appropriate screening tools for BD. In fact, it has been shown that screening for BD primary care settings can improve early identification and appropriate treatment of BD (30).
Several factors can affect the decision to seek professional help for symptoms of BD and therefore contribute to the overall treatment delay.
Depressive episodes have shown to be the predominant and most debilitating mood state among youth with BD (31) whereas periods of mood elevation (especially in the case of hypomania) tend to be shorter, not as functionally debilitating, and even perceived at times as enjoyable (32). This can cause affected youth not to be motivated to seek help during hypomanic episodes. On the other hand, youth may lack energy and motivation to access healthcare services, or may have negative cognitions such as not being deserving of care or being hopeless about getting better during depressive episodes.
Lack of knowledge of available mental health services, self-stigmatization of mental illness, comorbid conditions such as substance use disorder (24), physical disability and concerns about confidentiality may prevent youth from seeking appropriate help. Other patient factors that can influence this interval include individuals' perceived ability to seek help (i.e., self-efficacy) as well as perceived consequences of such help seeking (i.e., outcome expectations) (18, 33). In addition, developmental tasks during adolescence such as the need for independence and individuation from parents can result in resistance to perceived parental control, which can serve a barrier to help-seeking (34). Finally, since about one-third of youth with BD have a biological parent with the condition (35), parents' own experiences with BD may influence help-seeking in youth. More specifically, although having been exposed to symptoms of BD may help with early detection in the appraisal stage, it can also prolong the help-seeking interval especially if it leads to self-stigma or anxiety about the consequences of diagnosis.
The majority of youth help-seeking for emotional distress occur within the informal social network (36), and when it comes to professional help-seeking, youth usually do not seek mental health services on their own (37). Therefore, the role that caregivers, educators and other adults, collectively known as “gateway providers” (37) play in help-seeking in this age group should be recognized. For instance, perceived stigma associated with mental health issues as well as insufficient mental health literacy may prevent some parents and caregivers to seek help for youth who are going through early stages of BD (38). Other potential gateway provider factors include low mental health literacy among educators (39) and caregivers, inadequate financial resources and other psychosocial barriers that may affect caregivers' ability to seek help for the youth.
Potential factors related to healthcare system include limited accessibility to care providers, especially in rural and geographically remote areas, and lack of culturally safe mental health resources for youths and their families.
The time between the first appointment with a HCP and receiving the diagnosis of BD can be influenced by the following factors.
The official diagnosis of BD requires a history of manic or hypomanic episodes; however, the first (hypo)manic episode is frequently preceded by depressive episodes for several years (23, 40, 41). This can lead to an inevitable delay in the diagnosis of BD and inadequate, ineffective or even harmful interventions. Approximately, a quarter of youth with the initial diagnosis of MDD will transition to BD (42). Cross-sectional studies comparing clinical features of unipolar and bipolar depression in youth have identified features such as high rates of psychiatric co-morbidities, family history of psychiatric illness, higher severity of depression and higher level of functional impairment to be associated with bipolar depression (43). Additionally, prospective studies of adolescents and adults with major depressive disorder have shown that family history of BD, earlier age of onset of depression, presence of psychotic symptoms as well as subthreshold manic symptoms can predict future transitioning to BD (44). However, since no pathognomonic clinical features exist to differentiate bipolar depression from unipolar depression (45), the diagnosis of BD is typically delayed at least until the emergence of first threshold manic or hypomanic episode.
It has been shown that youths with BD tend to underreport their manic or hypomanic symptoms during clinical interviews (46) and therefore, in the absence of reliable collateral information or observable sign of mania during the clinical assessment, they may be diagnosed as having a unipolar depression.
Primary care providers are the first point of clinical contact for many individuals with BD (47) and therefore play a major role in early identification. However, they may not have the time and expertise required to assess youth with BD. In addition, limited access to specialized mental health services for youth with mood disorders and long waiting times to see a youth psychiatrist can contribute to a prolonged diagnostic interval. A recently published systematic review showed that access to early intervention services, except for a minority of individuals with BD, remains limited (17).
The HCP clinical decision-making process can be subject to heuristic biases resulting in diagnostic errors (48). For example, availability bias (tendency to rely on information that comes to mind more readily) can result in consideration of the most plausible diagnosis (18) and outcome bias can cause the healthcare professional to opt for diagnostic decisions that lead to more favorable outcomes or an inadvertent dismissal of BD symptoms. In fact, one study showed that 45% of psychiatrists fail to diagnose bipolar disorder when presented with case vignettes describing an individual in a manic state due to heuristic biases (49).
The time between receiving the diagnosis of BD and initiation of effective treatment. During this time, the HCP discusses treatment plans with the youth and their caregivers.
The pre-treatment interval can be impacted by impaired insight (impaired awareness of one's own psychiatric condition, and acceptance of the need for pharmacological or psychological intervention), which is a multidimensional construct and is associated with cognitive and emotional processing and illness characteristics (50). Impaired insight is a common feature of BD; one study showed that the prevalence of impaired insight in symptomatic and remitted adults with BD was 47% and 94% respectively (51). Similarly, another study showed 60% of adults with remitted BD had impaired insight (52).
Patient, family and societal attitudes towards psychotropic medications in general and mood stabilizing medications in particular can influence the pre-treatment interval. For instance, results from the National Stigma Study-Children suggested that approximately half of the responders agreed somewhat or strongly that receiving mental health treatment would “make a child an outsider at school” and “suffer as an adult” (53). Other perceptions that can potentially influence youth attitudes towards mood-stabilizing medications include not wanting to feel different to their friends, feeling pressured by others to stop the medication and not wanting to be reliant on medications (54). Additionally, quality of therapeutic alliance with the HCP (which can also be considered as a provider factor) can influence this interval.
One contributing factor affecting the Pre-treatment interval can include level of adherence of healthcare providers to evidence-based treatments. A recent Canadian study showed that only 59.6 percent of patients with BD received evidence-based treatment recommended by practice guidelines (55). Even the term “pediatric bipolar disorder” and associated interventions remains somewhat controversial among clinicians and academics (56, 57). Other potentially impactful factors include affordability and accessibility of recommended treatments for youths with BD.
The diagnosis and treatment of BD among youth is frequently delayed. Such delay poses a complex public health challenge as it involves different components that can be influenced by a multitude of interconnected disease, patient, and healthcare system factors. The extent to which each of these of factors contribute to the overall duration of undiagnosed and untreated BD in youth remains unknown and therefore warrants further studies. A multidimensional conceptual framework can offer a systematic approach to understanding and exploring barriers to early identification and interventions in BD, which in turn can spur the development of novel interventions and inform policy decisions. In this article, we used the Model of Pathways to Treatment as a foundation to explore potential factors involved in delayed diagnosis and treatment of BD in youth. We must add the caveat that some of the proposed contributing factors were extrapolated from studies of adults with BD or from the broader literature on youth with psychiatric disorders in general.
Fortunately, most of the contributing factors outlined in this article can be potentially amenable to various biomedical, psychosocial or public health policy interventions. As such, a more comprehensive understanding of these interrelated factors can provide countless opportunities for research towards developing innovative early identification strategies across various delay intervals. For instance, the Appraisal interval may be reduced by mental health literacy interventions (58) (patient factor) or through identifying potential biomarkers that would predict future manic or hypomanic episodes in youth who present with—seemingly unipolar—depression (disease factor). Similarly, anti-stigma campaigns (59) may help address patient-related barriers in the Help-seeking interval, which can also be minimized through innovative use of technology to improve access to specialists for youth, families and primary care providers (health-care provider and system factor).
Families, youth, and practitioners who are concerned about the possibility of pediatric BD can consult their local youth mental health services and refer to online resources such as Centre for Youth Bipolar Disorder (https://www.camh.ca/en/science-and-research/institutes-and-centres/centre-for-youth-bipolar-disorder), or Bipolar Disorder in Children and Teens available on the National Institute of Mental Health website (https://www.nimh.nih.gov/health/publications/bipolar-disorder-in-children-and-teens).
We hope this work contributes to the discussion on delayed diagnosis and treatment of youth with BD and provides a roadmap to inform future research studies and policy decisions.
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Ethical review and approval was not required for this study in accordance with the local legislation and institutional requirements.
KK conceived the original idea and drafted the manuscript. EM contributed to the conceptual framework and revised the manuscript. All authors contributed to the article and approved the submitted version.
KK has been on advisory board for AbbVie.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Canadian Community Health Survey (CCHS)- (2012). Available from: https://www23.statcan.gc.ca/imdb-bmdi/instrument/3226_Q1_V9-eng.htm (Accessed January 8, 2023).
2. Keramatian K, Torres IJ, Yatham LN. Neurocognitive functioning in bipolar disorder: what we know and what we don’t. Dialogues Clin Neurosci. (2022) 23(1):29–38. doi: 10.1080/19585969.2022.2042164
3. Keramatian K, Chakrabarty T, Saraf G, Pinto JV, Yatham LN. Grey matter abnormalities in first-episode mania: a systematic review and meta-analysis of voxel-based morphometry studies. Bipolar Disord. (2021) 23(3):228–40. doi: 10.1111/bdi.12995
4. Kauer-Sant’Anna M, Bond DJ, Lam RW, Yatham LN. Functional outcomes in first-episode patients with bipolar disorder: a prospective study from the systematic treatment optimization program for early mania project. Compr Psychiatry. (2009) 50(1):1–8. doi: 10.1016/j.comppsych.2008.05.013
5. Gore FM, Bloem PJN, Patton GC, Ferguson J, Joseph V, Coffey C, et al. Global burden of disease in young people aged 10-24 years: a systematic analysis. Lancet. (2011) 377(9783):2093–102. doi: 10.1016/S0140-6736(11)60512-6
6. Fritz K, Russell AMT, Allwang C, Kuiper S, Lampe L, Malhi GS. Is a delay in the diagnosis of bipolar disorder inevitable? Bipolar Disord. (2017) 19(5):396–400. doi: 10.1111/bdi.12499
7. Keramatian K, Pinto JV, Schaffer A, Sharma V, Beaulieu S, Parikh SV, et al. Clinical and demographic factors associated with delayed diagnosis of bipolar disorder: data from health outcomes and patient evaluations in bipolar disorder (HOPE-BD) study. J Affect Disord. (2022) 296:506–13. doi: 10.1016/j.jad.2021.09.094
8. Matza LS, Rajagopalan KS, Thompson CL, de Lissovoy G. Misdiagnosed patients with bipolar disorder: comorbidities, treatment patterns, and direct treatment costs. J Clin Psychiatry. (2005) 66(11):1432–40. doi: 10.4088/JCP.v66n1114
9. Berk M, Hallam K, Malhi GS, Henry L, Hasty M, MacNeil C, et al. Evidence and implications for early intervention in bipolar disorder. J Ment Health. (2010) 19(2):113–26. doi: 10.3109/09638230903469111
10. McCraw S, Parker G, Graham R, Synnott H, Mitchell PB. The duration of undiagnosed bipolar disorder: effect on outcomes and treatment response. J Affect Disord. (2014) 168:422–9. doi: 10.1016/j.jad.2014.07.025
11. Kessing LV, Vradi E, Andersen PK. Starting lithium prophylaxis early v. late in bipolar disorder. Br J Psychiatry. (2014) 205(3):214–20. doi: 10.1192/bjp.bp.113.142802
12. Post RM, Leverich GS, Kupka RW, Keck PE, McElroy SL, Altshuler LL, et al. Early-onset bipolar disorder and treatment delay are risk factors for poor outcome in adulthood. J Clin Psychiatry. (2010) 71(7):864–72. doi: 10.4088/JCP.08m04994yel
13. Altamura AC, Buoli M, Caldiroli A, Caron L, Cumerlato Melter C, Dobrea C, et al. Misdiagnosis, duration of untreated illness (DUI) and outcome in bipolar patients with psychotic symptoms: a naturalistic study. J Affect Disord. (2015) 182:70–5. doi: 10.1016/j.jad.2015.04.024
14. Lagerberg TV, Larsson S, Sundet K, Hansen CB, Hellvin T, Andreassen OA, et al. Treatment delay and excessive substance use in bipolar disorder. J Nerv Ment Dis. (2010) 198(9):628–33. doi: 10.1097/NMD.0b013e3181ef3ef4
15. Shi L, Thiebaud P, McCombs JS. The impact of unrecognized bipolar disorders for patients treated for depression with antidepressants in the fee-for-services California medicaid (medi-cal) program. J Affect Disord. (2004) 82(3):373–83. doi: 10.1016/j.jad.2004.03.009
16. Birnbaum HG, Shi L, Dial E, Oster EF, Greenberg PE, Mallett DA. Economic consequences of not recognizing bipolar disorder patients: a cross-sectional descriptive analysis. J Clin Psychiatry. (2003) 64(10):1201–9. doi: 10.4088/JCP.v64n1010
17. Scott J, Graham A, Yung A, Morgan C, Bellivier F, Etain B. A systematic review and meta-analysis of delayed help-seeking, delayed diagnosis and duration of untreated illness in bipolar disorders. Acta Psychiatr Scand. (2022) 146(5):389–405. doi: 10.1111/acps.13490
18. Scott SE, Walter FM, Webster A, Sutton S, Emery J. The model of pathways to treatment: conceptualization and integration with existing theory. Br J Health Psychol. (2013) 18(1):45–65. doi: 10.1111/j.2044-8287.2012.02077.x
19. Berk M, Conus P, Lucas N, Hallam K, Malhi GS, Dodd S, et al. Setting the stage: from prodrome to treatment resistance in bipolar disorder. Bipolar Disord. (2007) 9(7):671–8. doi: 10.1111/j.1399-5618.2007.00484.x
20. Vieta E, Reinares M, Rosa AR. Staging bipolar disorder. Neurotox Res. (2011) 19(2):279–85. doi: 10.1007/s12640-010-9197-8
21. Maciejewski DF, van Lier PAC, Branje SJT, Meeus WHJ, Koot HM. A 5-year longitudinal study on mood variability across adolescence using daily diaries. Child Dev. (2015) 86(6):1908–21. doi: 10.1111/cdev.12420
22. Swann AC. The strong relationship between bipolar and substance-use disorder. Ann N Y Acad Sci. (2010) 1187:276–93. doi: 10.1111/j.1749-6632.2009.05146.x
23. Duffy A, Alda M, Hajek T, Sherry SB, Grof P. Early stages in the development of bipolar disorder. J Affect Disord. (2010) 121(1–2):127–35. doi: 10.1016/j.jad.2009.05.022
24. Gould MS, Velting D, Kleinman M, Lucas C, Thomas JG, Chung M. Teenagers’ attitudes about coping strategies and help-seeking behavior for suicidality. J Am Acad Child Adolesc Psychiatry. (2004) 43(9):1124–33. doi: 10.1097/01.chi.0000132811.06547.31
25. Leventhal H, Phillips LA, Burns E. The common-sense model of self-regulation (CSM): a dynamic framework for understanding illness self-management. J Behav Med. (2016) 39(6):935–46. doi: 10.1007/s10865-016-9782-2
26. Bignall WJR, Jacquez F, Vaughn LM. Attributions of mental illness: an ethnically diverse community perspective. Community Ment Health J. (2015) 51(5):540–5. doi: 10.1007/s10597-014-9820-x
27. Kishore J, Gupta A, Jiloha RC, Bantman P. Myths, beliefs and perceptions about mental disorders and health-seeking behavior in Delhi, India. Indian J Psychiatry. (2011) 53(4):324–9. doi: 10.4103/0019-5545.91906
28. Nolan A, O’Connor C. The effect of causal attributions for depression on help-seeking and treatment preferences. J Affect Disord. (2019) 257:477–85. doi: 10.1016/j.jad.2019.07.017
29. Daveney J, Panagioti M, Waheed W, Esmail A. Unrecognized bipolar disorder in patients with depression managed in primary care: a systematic review and meta-analysis. Gen Hosp Psychiatry. (2019) 58:71–6. doi: 10.1016/j.genhosppsych.2019.03.006
30. Hirschfeld RMA, Cass AR, Holt DCL, Carlson CA. Screening for bipolar disorder in patients treated for depression in a family medicine clinic. J Am Board Fam Pract. (2005) 18(4):233–9. doi: 10.3122/jabfm.18.4.233
31. Birmaher B, Axelson D, Goldstein B, Strober M, Gill MK, Hunt J, et al. Four-year longitudinal course of children and adolescents with bipolar spectrum disorders: the course and outcome of bipolar youth (COBY) study. Am J Psychiatry. (2009) 166(7):795–804. doi: 10.1176/appi.ajp.2009.08101569
32. Vieta E. Bipolar II disorder: frequent, valid, and reliable. Can J Psychiatry. (2019) 64(8):541. doi: 10.1177/0706743719855040
34. Macneil CA, Hasty MK, Berk M, Henry L, Evans M, Redlich C, et al. Psychological needs of adolescents in the early phase of bipolar disorder: implications for early intervention. Early Interv Psychiatry. (2011) 5(2):100–7. doi: 10.1111/j.1751-7893.2011.00273.x
35. Brotman MA, Kassem L, Reising MM, Guyer AE, Dickstein DP, Rich BA, et al. Parental diagnoses in youth with narrow phenotype bipolar disorder or severe mood dysregulation. Am J Psychiatry. (2007) 164(8):1238–41. doi: 10.1176/appi.ajp.2007.06101619
36. Rickwood DJ, Braithwaite VA. Social-psychological factors affecting help-seeking for emotional problems. Soc Sci Med. (1994) 39(4):563–72. doi: 10.1016/0277-9536(94)90099-X
37. Stiffman AR, Pescosolido B, Cabassa LJ. Building a model to understand youth service access: the gateway provider model. Ment Health Serv Res. (2004) 6(4):189–98. doi: 10.1023/B:MHSR.0000044745.09952.33
38. Reardon T, Harvey K, Baranowska M, O’Brien D, Smith L, Creswell C. What do parents perceive are the barriers and facilitators to accessing psychological treatment for mental health problems in children and adolescents? A systematic review of qualitative and quantitative studies. Eur Child Adolesc Psychiatry. (2017) 26(6):623–47. doi: 10.1007/s00787-016-0930-6
39. Whitley J, Smith JD, Vaillancourt T. Promoting mental health literacy among educators. Can J Sch Psychol. (2013) 28(1):56–70. 101177/0829573512468852
40. O’Donovan C, Alda M. Depression preceding diagnosis of bipolar disorder. Front Psychiatry. (2020) 11:500. doi: 10.3389/fpsyt.2020.00500
41. Duffy A, Goodday S, Keown-Stoneman C, Grof P. The emergent course of bipolar disorder: observations over two decades from the Canadian high-risk offspring cohort. Am J Psychiatry. (2019) 176(9):720–9. doi: 10.1176/appi.ajp.2018.18040461
42. Yatham LN, Kennedy SH, Parikh S, Schaffer A, Bond DJ, Frey BN, et al. Canadian Network for mood and anxiety treatments (CANMAT) and international society for bipolar disorders (ISBD) 2018 guidelines for the management of patients with bipolar disorder. Bipolar Disord. (2018) 20(2):97. doi: 10.1111/bdi.12609
43. Uchida M, Serra G, Zayas L, Kenworthy T, Faraone S, Biederman J. Can unipolar and bipolar pediatric major depression be differentiated from each other? A systematic review of cross-sectional studies examining differences in unipolar and bipolar depression. J Affect Disord. (2015) 176:1–7. doi: 10.1016/j.jad.2015.01.037
44. Ratheesh A, Davey C, Hetrick S, Alvarez-Jimenez M, Voutier C, Bechdolf A, et al. A systematic review and meta-analysis of prospective transition from major depression to bipolar disorder. Acta Psychiatr Scand. (2017) 135(4):273–84. doi: 10.1111/acps.12686
45. Mitchell PB, Goodwin GM, Johnson GF, Hirschfeld RMA. Diagnostic guidelines for bipolar depression: a probabilistic approach. Bipolar Disord. (2008) 10(1 Pt 2):144–52. doi: 10.1111/j.1399-5618.2007.00559.x
46. Youngstrom EA, Findling RL, Calabrese JR. Effects of adolescent manic symptoms on agreement between youth, parent, and teacher ratings of behavior problems. J Affect Disord. (2004) 82(Suppl 1):S5–16. doi: 10.1016/j.jad.2004.05.016
47. Culpepper L. The diagnosis and treatment of bipolar disorder: decision-making in primary care. Prim Care Companion CNS Disord. (2014) 16(3). doi: 10.4088/PCC.13r01609
48. O’sullivan ED, Schofield SJ. Cognitive bias in clinical medicine. J R Coll Physicians Edinb. (2018) 48(3):225–32. doi: 10.4997/jrcpe.2018.306
49. Meyer F, Meyer TD. The misdiagnosis of bipolar disorder as a psychotic disorder: some of its causes and their influence on therapy. J Affect Disord. (2009) 112(1–3):174–83. doi: 10.1016/j.jad.2008.04.022
50. van der Werf-Eldering MJ, van der Meer L, Burger H, Holthausen EAE, Nolen WA, Aleman A. Insight in bipolar disorder: associations with cognitive and emotional processing and illness characteristics. Bipolar Disord. (2011) 13(4):343–54. doi: 10.1111/j.1399-5618.2011.00934.x
51. Varga M, Magnusson A, Flekkøy K, Rønneberg U, Opjordsmoen S. Insight, symptoms and neurocognition in bipolar I patients. J Affect Disord. (2006) 91(1):1–9. doi: 10.1016/j.jad.2005.09.002
52. Dias VV, Brissos S, Carita AI. Clinical and neurocognitive correlates of insight in patients with bipolar I disorder in remission. Acta Psychiatr Scand. (2008) 117(1):28–34. doi: 10.1111/j.1600-0447.2007.01110.x
53. Pescosolido BA, Perry BL, Martin JK, McLeod JD, Jensen PS. Stigmatizing attitudes and beliefs about treatment and psychiatric medications for children with mental illness. Psychiatr Serv. (2007) 58(5):613–8. doi: 10.1176/ps.2007.58.5.613
54. Tacchi MJ, Scott J. Improving adherence in schizophrenia and bipolar disorders. West Sussex, UK: John Wiley & Sons Ltd (2005).
55. Kozicky JM, Schaffer A, Beaulieu S, McIntosh D, Yatham LN. Use of a point-of-care web-based application to enhance adherence to the CANMAT and ISBD 2018 guidelines for the management of bipolar disorder. Bipolar Disord. (2022) 24(4):392–9. doi: 10.1111/bdi.13136
56. Parens E, Johnston J. Controversies concerning the diagnosis and treatment of bipolar disorder in children. Child Adolesc Psychiatry Ment Health. (2010) 4. doi: 10.1186/1753-2000-4-9
57. James A, Hoang U, Seagroatt V, Clacey J, Goldacre M, Leibenluft E. A comparison of American and English hospital discharge rates for pediatric bipolar disorder, 2000 to 2010. J Am Acad Child Adolesc Psychiatry. (2014) 53(6):614. doi: 10.1016/j.jaac.2014.02.008
58. Kelly CM, Jorm AF, Wright A. Improving mental health literacy as a strategy to facilitate early intervention for mental disorders. Med J Aust. (2007) 187(S7):S26–30. doi: 10.5694/j.1326-5377.2007.tb01332.x
Keywords: bipolar disorder, youth, early intervention, delayed diagnosis, conceptual framework
Citation: Keramatian K and Morton E (2023) Barriers to timely identification of bipolar disorder in youth: a multidimensional perspective. Front. Child Adolesc. Psychiatry 2:1186722. doi: 10.3389/frcha.2023.1186722
Received: 15 March 2023; Accepted: 27 April 2023;
Published: 15 May 2023.
Edited by:
Ty Ridenour, RTI International, United StatesReviewed by:
Lucia Marzulli, University of Bari Aldo Moro, Italy© 2023 Keramatian and Morton. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kamyar Keramatian a2FteWFyLmtlcmFtYXRpYW5AdmNoLmNh
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.