- 1Gillberg Neuropsychiatry Centre, Institute of Neuroscience and Physiology, University of Gothenburg, Gothenburg, Sweden
- 2Child and Adolescent Specialist Centre, Angered Hospital, SV Hospital Group, Gothenburg, Sweden
- 3Research department, Angered hospital, SV Hospital Group, Gothenburg, Sweden
Background: Identifying signs of autism is essential for enabling timely diagnosis and intervention. Children from multiethnic and socioeconomic disadvantaged settings are typically diagnosed with autism later than their general peers. This feasibility study explored the psychometric properties of a new instrument, Joint Attention Observation Schedule Preschool (JA-OBS Preschool), in children with suspected autism.
Methods: Data were collected from a prospective longitudinal study of 46 children aged 2–4 years who lived in a multiethnic, low resource area. The children had been referred from the Child Health Centre to a multiprofessional team for a neuropsychiatric assessment. In the diagnostic process, the instrument JA-OBS Preschool for observation of a child's capability of engaging in joint attention was included. Descriptive statistics and Cronbach's alfa were used to analyze the psychometric properties, including internal consistency reliability and inter-rater consistency.
Results: All 46 children with suspected autism screened positive on the JA-OBS Preschool. The internal consistency reliability of the instrument was calculated at 0.8 (Cronbach's alfa). Percent agreement between two examiners in JA-OBS Preschool ranged from 77% to 100%.
Conclusion: JA-OBS Preschool was found to be a promising instrument for identifying signs of autism in children in this setting. However, further research is needed to determine the psychometric properties of the JA-OBS Preschool in a general child population as well as in a younger age group.
1. Introduction
Autism Spectrum Disorder is a lifelong neurodevelopmental disorder that emerges in early childhood and characterized by impairments in social interaction and communication, as well as in repetitive pattern of behaviours and interests and/or unusual sensory reactions. Autism is associated with significant impairment in everyday functioning (1) and is highly correlated with co-existing conditions, such as language disorders and intellectual developmental disorder (2, 3). Approximately 1%–2% of preschool children in a general population receive an autism diagnosis (4, 5). Studies have indicated a higher prevalence of autism among children of immigrants (6–9). The etiology of autism is complex involving genetic, epigenetic and environmental factors (10, 11). Genetics play a key role in the etiology (12–15), but different factors influence each other (10). Still, the exact etiology remains unknown for the majority of cases. However, early detection of autism is critical to facilitate early intervention to improve developmental outcomes and prevent secondary behavioural problems (16–21). Early autism intervention can also enhance how families adapt and reduce parental stress (22) and societal costs (23).
Early symptoms of autism may emerge during the first years of life, and are manifested as abnormalities in social communication and repetitive behaviours. Impairments in social communication include reduced social engagement, deficits in developing relationship, reduced orienting to name, delayed language development without compensatory pointing or gesturing, and reduced joint attention behaviour (19, 24–27). Joint attention behaviours refer to the ability to coordinate visual attention between two persons and an external object in order to share attention (28, 29). In typically developing children, joint attention emerges in early infancy and continues to develop into more coordinated and complex behaviour between 8 and 18 months of age (24, 28). Children with autism have particular difficulty engaging in joint attention activities, including both initiating joint attention and responding to joint attention attempts of others (25, 28). Children not demonstrating these abilities after 15 months of age should be assessed for autism (30), and even earlier in infants at high familial risk for autism (31, 32).
Several studies have demonstrated that a reliable autism diagnosis can be made from 14 months of age (18, 30, 33–35). In clinical recommendations, screening for autism is recommended at 18- and 24- or 30-month well-child visits (19, 30, 36). A review of early detection procedures for autism in primary care and other community settings have found that routine screening increased overall referral rates (37). Furthermore, screening measures have been shown to be more effective in identifying children with autism than clinical judgment or caregiver concerns alone (38), and together with diagnostic tools for autism, screening has allowed diagnoses at younger ages (39).
Several screening instruments are available for the detection of autism among young children. The most widely used and studied screening tool is the Modified Checklist for Autism in Toddlers (M-CHAT/M-CHAT-R/F) (40, 41). The M-CHAT-R/F is a parent-rated scale, and a positive finding leads to a follow-up interview of health care professionals. The M-CHAT-R/F was found to be an effective tool for screening toddlers, decreasing the age of diagnosis by two years compared to the U.S. national median age of diagnosis (42, 43). Some screening methods use a combination of the parental report and clinical judgement, e.g., the original Checklist for Autism in Toddlers (CHAT) (44–46). Some later developed observation-based screening instruments, all focusing on the early social communication, are the Screening Tool for Autism in Two-Year-Olds (STAT) (47, 48), the Autism Detection in Early Childhood (ADEC) (49), and the Social Attention and Communication Surveillance (SACS) (50). The 5-item instrument Joint Attention Observation Schedule (JA-OBS) for clinical judgement in Child Health Care (CHC) was developed in our group for use in combination with the parent-rated M-CHAT-R (45). In a study by Nygren et al. (45), the positive predictive value for the combination of screening tools was high (89.6%).
Several studies have highlighted that preschool staff can effectively detect early symptoms of autism and other atypical features in early development (51–55), also in low-income and multiethnic settings (56, 57). Day-care workers often have education in child development, as well as experience in working with children with diverse disabilities. In a Swedish study, Nilsson Jobs et al. (58) showed that compared to parents, preschool professionals were able to identify children with autism, and their ratings were more in accordance with clinician-rated symptoms. Considering that developmental disabilities affect at least 8 to 10% of young children (59, 60), preschool may be an essential setting for early detection of autism and other developmental disabilities. In addition, in many countries, many children spend much of their time in a community childcare setting. In Sweden, 90.6% of children aged two years attend preschool (61).
Even though autism can be detected in the first two years of life, the recommendations for screening, and access to effective methods for early identification have not yet become the norm in many countries (19, 62–65). Delayed diagnosis of autism may be even more prevalent in areas with a high prevalence of people with low-income and/or multiethnic backgrounds (8, 44, 66–70).
Therefore, it is important to develop new methods for early detection of autism, which can complement the screening methods already used in health care, this need is emphasized in areas with a high prevalence of families with multiethnic background. The present study is a feasibility study of a new instrument for detection of autism signs in a preschool setting. The aim was to explore the psychometric properties of this new instrument, named Joint Attention Observation Schedule Preschool (JA-OBS Preschool) in children with suspected autism.
2. Materials and methods
2.1. The study setting
The study area consists of one district of Gothenburg, Sweden, with ∼13,200 inhabitants of whom ∼1,350 were children aged 0–5 years. The district is one of the most multiethnic and socioeconomically disadvantaged areas in Gothenburg, where around 90% of the population has a foreign background. The area has a high prevalence of ill health, unemployment, and low income (71). In an earlier study from this area, we have reported a high prevalence of autism, 3.66%, in preschool children (7). For more details regarding the study area, see Linnsand et al. (7).
2.2. The healthcare setting
In Sweden, healthcare is mainly tax-funded and is primarily regulated by the Health and Medical Service Act (SFS 2017:30) (72). Health care is free for all children, CHC has a developmental surveillance program for children between 0 and 6 years and reach about 99% of all children (73).
2.3. The preschool setting
In Sweden, preschool is not compulsory, but approximately 522,000 children (85.4%) aged 1–5 years old attend preschool. Of children aged 1–3 years, approximately 286,000 (78.6%) attend preschool. Of the children aged 1–3 years old with foreign backgrounds, 75.5% attend preschool (61). Preschool education represents the first step in the Swedish educational system and is included in the Swedish Education Act (74). The preschool curriculum contains the fundamental values and tasks of the preschool and goals and guidelines (75). In Sweden, nearly all children with special educational needs are enrolled in regular preschools. Professionals in Swedish preschool mainly include preschool teachers (university degree in Preschool Education) and preschool care workers (upper secondary education).
2.4. Participants
This study is based on 46 children (9 girls, 37 boys) born between 2010 and 2016 and diagnosed with DSM-5 autism (American Psychiatric Association 2013). The average age for the autism diagnosis was 38 months (range = 22–59 months, standard deviation = 9). All children, but one, lived in the same socioeconomic disadvantaged area in Gothenburg. Most of their parents had a non-Swedish background (93.5%).
2.5. Procedure
Data were collected from an ongoing prospective longitudinal study of young children diagnosed with autism. Medical records from the CHC and the comprehensive neuropsychiatric assessment were reviewed by two of the authors (PL and GN) independently. Extracted data included results from the autism screening at CHC, demographics, and the diagnostic assessment results. For more details regarding data collection, see Linnsand et al. (7).
2.5.1. The screening procedure at the child health centre
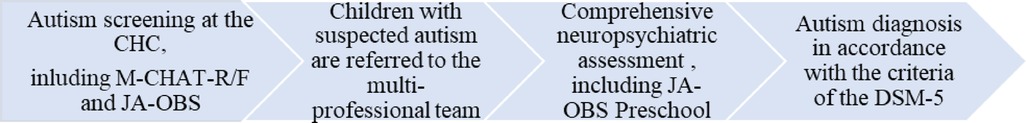
In the city of Gothenburg, all 30-month-old children are invited to autism screening at the CHC (Figure 1). The screening includes a combination of instruments: the parental questionnaire M-CHAT-R/F and the clinical observation of the child, the JA-OBS (Table 1, item 1–5) (45). The methods are also used if there is suspicion of autism before the routine screening. Children with suspected autism or other neurodevelopmental disorders at the CHC are referred to a multiprofessional team for further assessment.
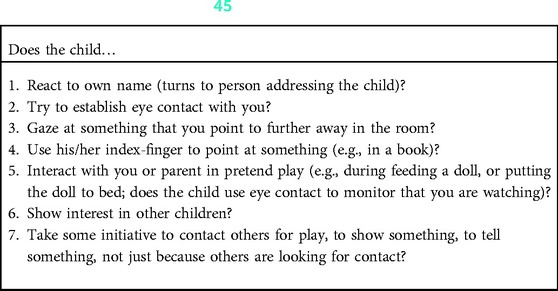
Table 1. JA-OBS (item 1–5) (45) and JA-OBS preschool (item 1–7).
2.5.2. The performance of the Ja-OBS preschool
The neuropsychiatric assessment included an observation of the child in the preschool environment (Figure 1). A special education teacher or a psychologist from the assessment team observed the child in free play and group activities. Also, an interview with the preschool teachers concerning the child's abilities and behaviour in different everyday activities was performed. During the observation, the examiner performed the JA-OBS Preschool (Table 1, item 1–7). The examiner interacted with the child and presented the tasks to him/her, for example, introducing the play, e.g., feeding a doll. Three children in the study group had no placement in any preschool. In these cases, the psychologist observed the child in the home environment, including the JA-OBS (Table 1, item 1–5).
For 13 children, one of two special education teachers from the preschool also performed the JA-OBS Preschool. The preschool special education teachers had received special training in how to perform the observation. The education focused on the typical development of communication and interaction, including joint attention behaviours, and early signs of autism, as well as the practical use of the instrument. The training also included case descriptions, where the different items were discussed.
The preschool special education teachers (the preschool setting) and the psychologist from the assessment team (the health care setting) did not observe the child simultaneously but during the same two-week period. The examiners were not aware of the other's ratings.
2.5.3. The diagnostic procedure at the multiprofessional team
A comprehensive neuropsychiatric assessment was performed for the 46 children, which included a physical developmental examination, a parental interview regarding the child's developmental and medical history, current clinical symptoms and social situation, and assessment of the child's intellectual level [The Wechsler Preschool and Primary Scale of Intelligence, Fourth Edition (WPPSI-IV) (76) for the children over 2:6 years, and for younger children Merrill-Palmer—Revised Scales of Development (MP-R) (77)]. The Autism Diagnostic Observation Schedule (ADOS) (78) or the Autism Diagnostic Observation Schedule Second Edition (ADOS-2) (79) were included. The Vineland Adaptive Behavior Scales Second Edition (VABS-II) (80) was performed with the parents. In addition, an observation of the child in the preschool environment, including JA-OBS Preschool, was also included in the assessment. The autism diagnosis was based on all obtained information from the assessments and in accordance with the criteria of the DSM-5 (299.00, Autism Spectrum Disorder) (1). The multiprofessional team and the assessment are further described in Linnsand et al. (7).
2.6. Measures
2.6.1. Joint attention observation schedule
The JA-OBS is a five-item observation of a child's capability of engaging in joint attention activities (initiation of joint attention and response to joint attention). The observation also includes other social communicative behaviours, i.e., the child's response to own name and the ability to interact in pretend play (Table 1, item 1–5). Nygren et al. (45) developed the JA-OBS based on results received in studies of early autism symptoms related to reduced joint attention behaviours. The screen positivity for autism on the JA-OBS occurred when the examiners did not observe the target behaviours on two or more of the items.
2.6.2. Joint attention observation schedule preschool
The JA-OBS Preschool is a further development of the JA-OBS for use in preschool (developed by the author GN). The JA-OBS Preschool contains the first five-item from the JA-OBS (Table 1, item 1–5) plus two additional items (Table 1, item 6–7). The additional items focus on aspects of social communication that can be observed in a preschool setting. Based on previous research of JA-OBS and the clinical experience of the JA-OBS Preschool, a positive screening result for autism was defined as failure on two or more of the seven items (45).
2.7. Statistical analysis
Internal consistency reliability was calculated using Cronbach's alfa. Inter-rater consistency was calculated as percent agreement. The calculations were performed using SPSS version 27 (81).
3. Results
3.1. Sample characteristics
The study group consisted of 46 children (9 girls, 37 boys) diagnosed with autism in accordance with DSM-5 (1). Regarding autism severity level, 25 children (54.3%) had autism level 1, and 21 children (45.7%) had autism level 2. Six children (13%) had average intellectual functioning (Intelligence Quotient (IQ)/Developmental Quotient (DQ) ≥85), 12 children (26.1%) had borderline intellectual functioning (IQ/DQ 70–84), and 28 children (60.9%) intellectual disability (IQ/DQ <70).
3.2. Results of Ja-OBS and Ja-OBS preschool
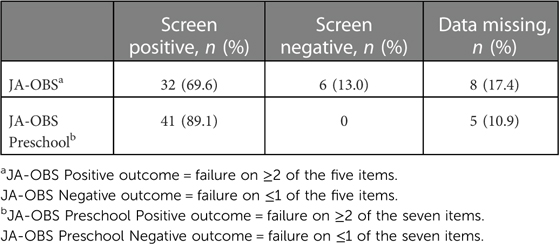
Of the 46 children, 38 had JA-OBS completed from CHC, and 41 children had JA-OBS Preschool completed for them. On the JA-OBS, 32 children screened positive for autism (failure on ≥2 of the five items), whereas all 41 children screened positive on JA-OBS Preschool (failure on ≥2 of the seven items) (Table 2). Of the children, 88.2% screened positive on both JA-OBS and JA-OBS Preschool.
3.3. JA-OBS preschool
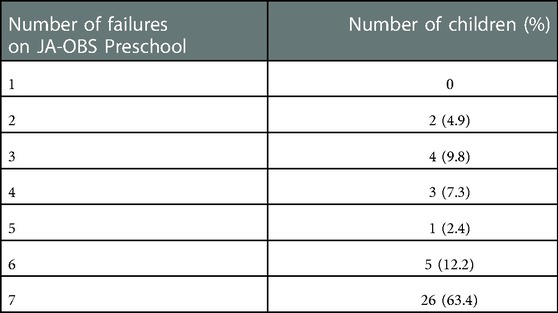
All 41 children screened positive on JA-OBS Preschool, i.e., failed on ≥2 of the seven items, and 75.6% failed on ≥6 of the seven items (Table 3).
The failure on the respective item on JA-OBS Preschool ranged from 70.7% to 97.6% (Figure 2).
3.3.1. Internal consistency reliability
The internal consistency reliability was studied in 41 observations. Internal reliability was analyzed for all items of the JA-OBS Preschool and calculated at 0.80 (Cronbach's alfa).
3.3.2. Inter-rater consistency
Percent agreement of the JA-OBS Preschool was studied for 13 children, where the results from two examiners who completed the JA-OBS Preschool independently of each other where compared. With both examiners, all 13 children screened positive for autism (failure on ≥2 of the seven items). Percent agreement for individual items ranged from 76.9% to 100% (Table 4).
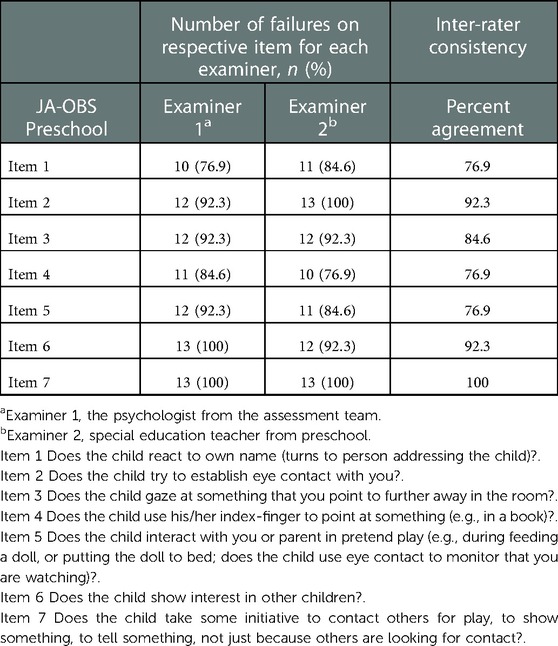
Table 4. Number of failures on respective item for each examiner and percent agreement between two examiners in JA-OBS preschool (n = 13).
4. Discussion
Although the importance of identifying autism at an early age has been highlighted in many studies, early identification and diagnosis has not yet become the norm (17, 19, 62, 63, 82, 83). Moreover, children from multiethnic and socioeconomically disadvantaged settings are typically diagnosed with autism later than their general peers (8, 44, 66, 68), leading to missed opportunities to provide treatment during possibly critical and sensitive developmental periods (18, 20, 66). Several studies have highlighted the value of preschool staff as partners in identification and referral for children with suspected autism (37, 52, 58, 84–86).
However, introducing detection of signs of autism in preschool requires certain basic prerequisites, such as valid instruments and routines for detection. In the present study, we explored the psychometric properties of the JA-OBS Preschool in children with suspected autism. The JA-OBS Preschool seems to be a promising instrument to detect autism symptoms in this setting. All included children with suspected autism screened positive on the JA-OBS Preschool, and 88% of them had a positive outcome on both JA-OBS and JA-OBS Preschool. The high number of positive screened children on the JA-OBS Preschool indicates high sensitivity. Also, the internal consistency reliability of JA-OBS Preschool was good. In addition, the instrument JA-OBS for use in health care has in an earlier study been found to have good psychometric properties (sensitivity 86% and positive predictive value 92.5%) (Nygren et al., 2012). In the present study, we cannot examine the specificity of the instruments, then all children had suspected autism. Therefore, further studies are needed to determine the psychometric properties of the JA-OBS Preschool in a general child population.
The percent agreement in the rating of JA-OBS Preschool was high and ranged from 77% to 100%, which could indicate an actual agreement between the two examiners. This would also be in line with the results of the JA-OBS inter-rater reliability study (45). Nygren et al. found that an agreement for total scores was obtained in 93% of the observations. Other studies have presented similar results, for example, Nilsson Jobs et al. (58) found that, compared to parents, preschool staff rated autism symptoms more in accordance with the health care staff. In line with a study by Zhang et al. (51), we believe that the special education teachers' special knowledge and experience were crucial for detection of signs of autism and level of agreement between the two examiners. In the present study, the preschool special education teachers were able to recognize developmental impairment in respect of joint attention behaviours. They also had knowledge and experience of working with children with autism and other developmental disorders.
In the JA-OBS Preschool, items 6 and 7 highlight the child's interest in other children and the child's ability to initiate contact and play with other children. Most of the children screened positive on these items (93% respectively 98%), and the percent agreement between the two examiners was high (ranged from 92% to 100%). Items 6 and 7 can be observed in a preschool setting and might complement the observation made in health care. Thus, the structured observation, the JA-OBS Preschool, can also provide valuable information in the continued diagnostic process.
In addition to valid instruments, routines for the detection of autism signs in children are important. At the CHC, the autism screening is general. However, in preschool, we propose using the JA-OBS Preschool when there is any concern about the child's social communication and play development. The observation provides support for the preschool teachers in the judgement and interpretation of autism signs. Routines for detecting autism are essential as they also induce the preschool teachers to pay attention to early signs of autism that otherwise may be unnoticed. The use of the JA-OBS and the JA-OBS Preschool in parallel in different settings can provide additional benefits. It may contribute to the health care and preschool staff receiving a common language to talk about the child's deviant development. Good conditions for the detection of autism signs can be created if a close collaboration occurs between CHC and the preschool.
Opportunities for continuing education and supervision for preschool staff are essential. The education needs to focus on the typical development of communication and interaction, including joint attention behaviours, and early signs of autism, as well as the practical use of the instrument JA-OBS Preschool. Approaching parents about potential concerns regarding the child's development might be challenging for several reasons. Some parents may not be ready to take in that their child might have developmental problems. Also, cultural factors (e.g., differences in the norms of typical child development as well as deviant development, stigma and discrimination, and inadequate understanding of the health care system) might be barriers to detecting early signs of autism (8). It is crucial to provide preschool teachers with support and knowledge to find a sensible way to approach the parents about the child's difficulties. Thus, the instrument needs to be used in a context where there are opportunities for assessment and interventions. The preschool teachers need knowledge about the health care system, so they can guide parents to contact healthcare services for further assessments. We find this to be particularly important for parents with a migrant background because they often have difficulty navigating through the health care system (87).
The first autism signs are often noticeable during the second year of life. In the present study, the average age for the diagnosis of autism was pretty high (38 months). It is desirable to identify symptoms of autism earlier. Therefore, in future study, there is a need to validate the JA-OBS Preschool in a younger age group, children aged 18–24 months.
In Linnsand et al. (7), we proposed a new model to increase accessibility to care, with a local multiprofessional team for both assessment and interventions for young children with autism and their families. Together with autism screening at CHC, we suggest that identification of autism symptoms at preschool may be an essential part of this concept. Information from multiple settings, as well as several informants, may facilitate early identification. Even other studies have indicated that implementation of methods for detection of autism in preschool may be effective and might help improve access to early diagnosis and reduce possible healthcare disparities (56, 57). Thus, further studies should also focus on the use of JA-OBS Preschool and its impact on early diagnosis.
4.1. Limitations and strengths
The same multiprofessional team assessed all children in this study, and consistent diagnostic criteria and diagnostic instruments were used.
For a retrospective study like this, the quality of the medical records is essential. In the present study, two pediatricians have met al.l children, and both have very long clinical experience assessing children with different neurodevelopmental and medical disorders, thereby increasing the validity of the data used in this study. In the clinical assessment, to ensure that different areas of development were covered, a medical journal template has been used. Thus, certain data were not available, including missing JA-OBS Preschool for some children.
One limitation of the present study was that the sample consisted of children who had already undergone a previous screening resulting in suspicion of autism. This is likely to have affected the high degree of agreement across examiners. Also, the very high percent of agreement made the use of standard agreement statistics, such as Cohen's Kappa, less appropriate. Instead, we report percentage agreement and highlight that caution should be made in generalizing to other groups on the basis of our results. Further research is needed to determine the psychometric properties of the JA-OBS Preschool in a general child population.The fact that all children had suspected autism and all screened cases were positive, further studies are needed to determine if the observation has the same capacity to confirm the absence of autism signs, i.e., specificity.
Another limitation of the study was the educational level of the preschool special education teacher; the educational level was higher compared to regular preschool teachers. We propose that the high educational level contributes to the high agreement between the special education teacher and the psychologist from the assessment team. Therefore, good knowledge of both the typical development and early signs of autism will be essential in the reliable use of the JA-OBS Preschool.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by The Regional Ethics Committee in Gothenburg, Sweden (ref. nos 653-14, 549-17, 554-18). Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author contributions
GN and PL were part of the study design development, data collection, data analysis, interpretation of the data, and writing. JH was part of the study design development, statistical analysis, interpretation of the data, and writing. CG was part of the study design development, interpretation of the data and writing. All authors provided a critical review of the manuscript and approved the final draft. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by grants from the Research department at Angered hospital, SV Hospital group, Gothenburg, Sweden, and the Anna Ahrenberg foundation, Sweden.
Acknowledgments
The authors gratefully acknowledge the families who participated in the study and the CHC-nurses, clinicians and medical staff.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington: VA: American Psychiatric Publishing (2013).
2. Lundstrom S, Reichenberg A, Melke J, Rastam M, Kerekes N, Lichtenstein P, et al. Autism spectrum disorders and coexisting disorders in a nationwide Swedish twin study. J Child Psychol Psychiatry. (2015) 56:702–10. doi: 10.1111/jcpp.12329
3. Gillberg C. The ESSENCE in child psychiatry: early symptomatic syndromes eliciting neurodevelopmental clinical examinations. Res Dev Disabil. (2010) 31:1543–51. doi: 10.1016/j.ridd.2010.06.002
4. Elsabbagh M, Divan G, Koh YJ, Kim YS, Kauchali S, Marcin C, et al. Global prevalence of autism and other pervasive developmental disorders. Autism Res. (2012) 5:160–79. doi: 10.1002/aur.239
5. Lyall K, Croen L, Daniels J, Fallin MD, Ladd-Acosta C, Lee BK, et al. The changing epidemiology of autism Spectrum disorders. Annu Rev Public Health. (2017) 38:81–102. doi: 10.1146/annurev-publhealth-031816-044318
6. Crafa D, Warfa N. Maternal migration and autism risk: systematic analysis. Int Rev Psychiatry. (2015) 27:64–71. doi: 10.3109/09540261.2014.995601
7. Linnsand P, Gillberg C, Nilses Å, Hagberg B, Nygren G. A high prevalence of autism Spectrum disorder in preschool children in an immigrant, multiethnic population in Sweden: challenges for health care. J Autism Dev Disord. (2020) 51:538–49. doi: 10.1007/s10803-020-04563-8
8. Schmengler H, Cohen D, Tordjman S, Melchior M. Autism Spectrum and other neurodevelopmental disorders in children of immigrants: a brief review of current evidence and implications for clinical practice. Front Psychiatry. (2021) 12:566368. doi: 10.3389/fpsyt.2021.566368
9. Gillberg C, Steffenburg S, Borjesson B, Andersson L. Infantile autism in children of immigrant parents. A population-based study from Goteborg, Sweden. Br J Psychiatry. (1987) 150:856–8. doi: 10.1192/bjp.150.6.856
10. Masini E, Loi E, Vega-Benedetti AF, Carta M, Doneddu G, Fadda R, et al. An overview of the main genetic, epigenetic and environmental factors involved in autism Spectrum disorder focusing on synaptic activity. Int J Mol Sci. (2020) 21(21):8290. doi: 10.3390/ijms21218290
11. Bölte S, Girdler S, Marschik PB. The contribution of environmental exposure to the etiology of autism spectrum disorder. Cell Mol Life Sci. (2019) 76:1275–97. doi: 10.1007/s00018-018-2988-4
12. Taylor MJ, Rosenqvist MA, Larsson H, Gillberg C, D'Onofrio BM, Lichtenstein P, et al. Etiology of autism Spectrum disorders and autistic traits over time. JAMA Psychiatry. (2020) 77:936–43. doi: 10.1001/jamapsychiatry.2020.0680
13. Steffenburg S, Gillberg C, Hellgren L, Andersson L, Gillberg IC, Jakobsson G, et al. A twin study of autism in Denmark, Finland, Iceland, Norway and Sweden. J Child Psychol Psychiatry. (1989) 30:405–16. doi: 10.1111/j.1469-7610.1989.tb00254.x
14. Lai MC, Lombardo MV, Baron-Cohen S. Autism. Lancet. (2014) 383:896–910. doi: 10.1016/s0140-6736(13)61539-1
15. Sandin S, Lichtenstein P, Kuja-Halkola R, Larsson H, Hultman CM, Reichenberg A. The familial risk of autism. JAMA. (2014) 311:1770–7. doi: 10.1001/jama.2014.4144
16. Dawson G. Early behavioral intervention, brain plasticity, and the prevention of autism spectrum disorder. Dev Psychopathol. (2008) 20:775–803. doi: 10.1017/s0954579408000370
17. Devescovi R, Monasta L, Mancini A, Bin M, Vellante V, Carrozzi M, et al. Early diagnosis and early start denver model intervention in autism spectrum disorders delivered in an Italian public health system service. Neuropsychiatr Dis Treat. (2016) 12:1379–84. doi: 10.2147/ndt.S106850
18. Zwaigenbaum L, Bauman ML, Choueiri R, Kasari C, Carter A, Granpeesheh D, et al. Early intervention for children with autism Spectrum disorder under 3 years of age: recommendations for practice and research. Pediatrics. (2015) 136(Suppl 1):S60–81. doi: 10.1542/peds.2014-3667E
19. Zwaigenbaum L, Bauman ML, Fein D, Pierce K, Buie T, Davis PA, et al. Early screening of autism Spectrum disorder: recommendations for practice and research. Pediatrics. (2015) 136(Suppl 1):S41–59. doi: 10.1542/peds.2014-3667D
20. Ismail FY, Fatemi A, Johnston MV. Cerebral plasticity: windows of opportunity in the developing brain. Eur J Paediatr Neurol. (2017) 21:23–48. doi: 10.1016/j.ejpn.2016.07.007
21. Øien RA, Vivanti G, Robins DL. Editorial S.I: early identification in autism Spectrum disorders: the present and future, and advances in early identification. J Autism Dev Disord. (2021) 51:763–8. doi: 10.1007/s10803-020-04860-2
22. Estes A, Swain DM, MacDuffie KE. The effects of early autism intervention on parents and family adaptive functioning. Pediatr Med. (2019) 2:21. doi: 10.21037/pm.2019.05.05
23. Peters-Scheffer N, Didden R, Korzilius H, Matson J. Cost comparison of early intensive behavioral intervention and treatment as usual for children with autism spectrum disorder in The Netherlands. Res Dev Disabil. (2012) 33:1763–72. doi: 10.1016/j.ridd.2012.04.006
24. Jones EJ, Gliga T, Bedford R, Charman T, Johnson MH. Developmental pathways to autism: a review of prospective studies of infants at risk. Neurosci Biobehav Rev. (2014) 39:1–33. doi: 10.1016/j.neubiorev.2013.12.001
25. Franchini M, Armstrong VL, Schaer M, Smith IM. Initiation of joint attention and related visual attention processes in infants with autism spectrum disorder: literature review. Child Neuropsychol. (2019) 25:287–317. doi: 10.1080/09297049.2018.1490706
26. Sacrey LA, Bennett JA, Zwaigenbaum L. Early infant development and intervention for autism Spectrum disorder. J Child Neurol. (2015) 30:1921–9. doi: 10.1177/0883073815601500
27. Tanner A, Dounavi K. The emergence of autism symptoms prior to 18 months of age: a systematic literature review. J Autism Dev Disord. (2021) 51:973–93. doi: 10.1007/s10803-020-04618-w
28. Mundy P. A review of joint attention and social-cognitive brain systems in typical development and autism spectrum disorder. Eur J Neurosci. (2018) 47:497–514. doi: 10.1111/ejn.13720
29. Mundy P, Sullivan L, Mastergeorge AM. A parallel and distributed-processing model of joint attention, social cognition and autism. Autism Res. (2009) 2:2–21. doi: 10.1002/aur.61
30. Sanchack KE, Thomas CA. Autism Spectrum disorder: primary care principles. Am Fam Physician. (2016) 94:972–9. PMID: 28075089
31. McDonald NM, Senturk D, Scheffler A, Brian JA, Carver LJ, Charman T, et al. Developmental trajectories of infants with Multiplex family risk for autism: a baby siblings research consortium study. JAMA Neurol. (2020) 77:73–81. doi: 10.1001/jamaneurol.2019.3341
32. Ozonoff S, Iosif AM, Baguio F, Cook IC, Hill MM, Hutman T, et al. A prospective study of the emergence of early behavioral signs of autism. J Am Acad Child Adolesc Psychiatry. (2010) 49:256–66.e1-2. PMID: 20410715; PMCID: 2923050
33. Ozonoff S, Young GS, Landa RJ, Brian J, Bryson S, Charman T, et al. Diagnostic stability in young children at risk for autism spectrum disorder: a baby siblings research consortium study. J Child Psychol Psychiatry. (2015) 56:988–98. doi: 10.1111/jcpp.12421
34. Pierce K, Gazestani VH, Bacon E, Barnes CC, Cha D, Nalabolu S, et al. Evaluation of the diagnostic stability of the early autism Spectrum disorder phenotype in the general population starting at 12 months. JAMA Pediatr. (2019) 173:578–87. doi: 10.1001/jamapediatrics.2019.0624
35. Dahlgren SO, Gillberg C. Symptoms in the first two years of life. A preliminary population study of infantile autism. Eur Arch Psychiatry Neurol Sci. (1989) 238:169–74. doi: 10.1007/bf00451006
36. Siu AL, Bibbins-Domingo K, Grossman DC, Baumann LC, Davidson KW, Ebell M, et al. Screening for autism Spectrum disorder in young children: uS preventive services task force recommendation statement. JAMA. (2016) 315:691–6. doi: 10.1001/jama.2016.0018
37. Daniels AM, Halladay AK, Shih A, Elder LM, Dawson G. Approaches to enhancing the early detection of autism spectrum disorders: a systematic review of the literature. J Am Acad Child Adolesc Psychiatry. (2014) 53:141–52. doi: 10.1016/j.jaac.2013.11.002
38. Miller JS, Gabrielsen T, Villalobos M, Alleman R, Wahmhoff N, Carbone PS, et al. The each child study: systematic screening for autism spectrum disorders in a pediatric setting. Pediatrics. (2011) 127:866–71. doi: 10.1542/peds.2010-0136
39. Dawson G, Bernier R. A quarter century of progress on the early detection and treatment of autism spectrum disorder. Dev Psychopathol. (2013) 25:1455–72. doi: 10.1017/s0954579413000710
40. Robins DL, Fein D, Barton ML, Green JA. The modified checklist for autism in toddlers: an initial study investigating the early detection of autism and pervasive developmental disorders. J Autism Dev Disord. (2001) 31:131–44. doi: 10.1023/a:1010738829569
41. Robins DL, Dumont-Mathieu TM. Early screening for autism spectrum disorders: update on the modified checklist for autism in toddlers and other measures. J Dev Behav Pediatr. (2006) 27:S111–9. doi: 10.1097/00004703-200604002-00009
42. Robins DL, Casagrande K, Barton M, Chen CM, Dumont-Mathieu T, Fein D. Validation of the modified checklist for autism in toddlers, revised with follow-up (M-CHAT-R/F). Pediatrics. (2014) 133:37–45. doi: 10.1542/peds.2013-1813
43. Sánchez-García AB, Galindo-Villardón P, Nieto-Librero AB, Martín-Rodero H, Robins DL. Toddler screening for autism Spectrum disorder: a meta-analysis of diagnostic accuracy. J Autism Dev Disord. (2019) 49:1837–52. doi: 10.1007/s10803-018-03865-2
44. Barbaro J, Halder S. Early identification of autism Spectrum disorder: current challenges and future global directions. Curr Dev Disord Rep. (2016) 3:67–74. doi: 10.1007/s40474-016-0078-6
45. Nygren G, Sandberg E, Gillstedt F, Ekeroth G, Arvidsson T, Gillberg C. A new screening programme for autism in a general population of Swedish toddlers. Res Dev Disabil. (2012) 33:1200–10. doi: 10.1016/j.ridd.2012.02.018
46. Baron-Cohen S, Allen J, Gillberg C. Can autism be detected at 18 months? The needle, the haystack, and the CHAT. Br J Psychiatry. (1992) 161:839–43. doi: 10.1192/bjp.161.6.839
47. Stone WL, Coonrod EE, Ousley OY. Brief report: screening tool for autism in two-year-olds (STAT): development and preliminary data. J Autism Dev Disord. (2000) 30:607–12. doi: 10.1023/a:1005647629002
48. Stone WL, Coonrod EE, Turner LM, Pozdol SL. Psychometric properties of the STAT for early autism screening. J Autism Dev Disord. (2004) 34:691–701. doi: 10.1007/s10803-004-5289-8
49. Young RL. Autism detection in early childhood: ADEC. Camberwell, VIC: Australian Council of Educational Research (2007).
50. Barbaro J, Dissanayake C. Early markers of autism spectrum disorders in infants and toddlers prospectively identified in the social attention and communication study. Autism. (2013) 17:64–86. doi: 10.1177/1362361312442597
51. Zhang D, Krieber-Tomantschger I, Poustka L, Roeyers H, Sigafoos J, Bölte S, et al. Identifying atypical development: a role of day-care workers? J Autism Dev Disord. (2019) 49:3685–94. doi: 10.1007/s10803-019-04056-3
52. Larsen K, Aasland A, Diseth TH. Brief report: agreement between parents and day-care professionals on early symptoms associated with autism Spectrum disorders. J Autism Dev Disord. (2018) 48:1063–8. doi: 10.1007/s10803-017-3355-2
53. Dereu M, Raymaekers R, Warreyn P, Schietecatte I, Meirsschaut M, Roeyers H. Can child care workers contribute to the early detection of autism spectrum disorders? A comparison between screening instruments with child care workers versus parents as informants. J Autism Dev Disord. (2012) 42:781–96. doi: 10.1007/s10803-011-1307-9
54. Janus M, Mauti E, Horner M, Duku E, Siddiqua A, Davies S. Behavior profiles of children with autism spectrum disorder in kindergarten: comparison with other developmental disabilities and typically developing children. Autism Res. (2018) 11:410–20. doi: 10.1002/aur.1904
55. Nordahl-Hansen A, Hart L, Oien RA. The scientific study of parents and caregivers of children with ASD: a flourishing field but still work to be done. J Autism Dev Disord. (2018) 48:976–9. doi: 10.1007/s10803-018-3526-9
56. Janvier YM, Harris JF, Coffield CN, Louis B, Xie M, Cidav Z, et al. Screening for autism spectrum disorder in underserved communities: early childcare providers as reporters. Autism. (2016) 20:364–73. doi: 10.1177/1362361315585055
57. Gulsrud A, Carr T, Williams J, Panganiban J, Jones F, Kimbrough J, et al. Developmental screening and early intervention in a childcare setting for young children at risk for autism and other developmental delays: a feasibility trial. Autism Res. (2019) 12:1423–33. doi: 10.1002/aur.2160
58. Jobs EN, Bölte S, Falck-Ytter T. Spotting signs of autism in 3-year-olds: comparing information from parents and preschool staff. J Autism Dev Disord. (2019) 49:1232–41. doi: 10.1007/s10803-018-3821-5
59. Zablotsky B, Black LI, Maenner MJ, Schieve LA, Danielson ML, Bitsko RH, et al. Prevalence and trends of developmental disabilities among children in the United States: 2009-2017. Pediatrics. (2019) 144(4):1–11. doi: 10.1542/peds.2019-0811
60. Olusanya BO, Davis AC, Wertlieb D, Boo N-Y, Nair MKC, Halpern R, et al. Developmental disabilities among children younger than 5 years in 195 countries and territories, 1990-2016: a systematic analysis for the global burden of disease study 2016. Lancet Glob Health. (2018) 6:e1100-e21. doi: 10.1016/s2214-109x(18)30309-7
61. Swedish National Agency for Education. Statistics on children and staff in preschool (2019) Available at: https://www.skolverket.se/skolutveckling/statistik/sok-statistik-om-forskola-skola-och-vuxenutbildning?sok=SokC&verkform=F%C3%B6rskola&omrade=Barn%20och%20grupper&lasar=2019&run=12020
62. Bölte S, Bartl-Pokorny KD, Jonsson U, Berggren S, Zhang D, Kostrzewa E, et al. How can clinicians detect and treat autism early? Methodological trends of technology use in research. Acta Paediatr. (2016) 105:137–44. doi: 10.1111/apa.13243
63. García-Primo P, Hellendoorn A, Charman T, Roeyers H, Dereu M, Roge B, et al. Screening for autism spectrum disorders: state of the art in Europe. Eur Child Adolesc Psychiatry. (2014) 23:1005–21. doi: 10.1007/s00787-014-0555-6
64. Hyman SL, Levy SE, Myers SM. Identification, evaluation, and management of children with autism Spectrum disorder. Pediatrics. (2020) 145(1):145. doi: 10.1542/peds.2019-3447
65. Wallis KE, Guthrie W, Bennett AE, Gerdes M, Levy SE, Mandell DS, et al. Adherence to screening and referral guidelines for autism spectrum disorder in toddlers in pediatric primary care. PLoS One. (2020) 15:e0232335. doi: 10.1371/journal.pone.0232335
66. Daniels AM, Mandell DS. Explaining differences in age at autism spectrum disorder diagnosis: a critical review. Autism. (2014) 18:583–97. doi: 10.1177/1362361313480277
67. Mandell DS, Ittenbach RF, Levy SE, Pinto-Martin JA. Disparities in diagnoses received prior to a diagnosis of autism spectrum disorder. J Autism Dev Disord. (2007) 37:1795–802. doi: 10.1007/s10803-006-0314-8
68. Hewitt A, Hall-Lande J, Hamre K, Esler AN, Punyko J, Reichle J, et al. Autism Spectrum disorder (ASD) prevalence in Somali and non-Somali children. J Autism Dev Disord. (2016) 46:2599–608. doi: 10.1007/s10803-016-2793-6
69. de Leeuw A, Happé F, Hoekstra RA. A conceptual framework for understanding the cultural and contextual factors on autism across the globe. Autism Res. (2020) 13:1029–50. doi: 10.1002/aur.2276
70. Constantino JN, Abbacchi AM, Saulnier C, Klaiman C, Mandell DS, Zhang Y, et al. Timing of the diagnosis of autism in African American children. Pediatrics. (2020) 146:1–9. doi: 10.1542/peds.2019-3629
71. SCB/Gothenburg City Council. Göteborgsbladet. (2021). Available at: https://goteborg.se/wps/portal/enhetssida/statistik-och-analys/goteborgsbladet/hamta-statistik/faktablad/goteborgsbladet/
72. Swedish Constitutional Assembly. Health and Medical Service Act (2017). Available at: https://www.riksdagen.se/sv/dokument-lagar/dokument/svensk-forfattningssamling/halso–och-sjukvardslag-201730_sfs-2017-30.
73. Central Health Care in Region Västra Götaland. Child Health Care in Region Västra Götaland Annual. (2018). Available at: https://mellanarkiv-offentlig.vgregion.se/alfresco/s/archive/stream/public/v1/source/available/sofia/rhs3450-1856953649-9/surrogate/VGR_BVC_arsrapport_2018.pdf
74. Swedish Constitutional Assembly. Education Act. (2010). Available at: https://www.riksdagen.se/sv/dokument-lagar/dokument/svensk-forfattningssamling/skollag-2010800_sfs-2010-800
75. Swedish National Agency for Education. Curriculum for the preschool. (2018). Available at: https://www.skolverket.se/undervisning/forskolan/laroplan-for-forskolan/laroplan-lpfo-18-for-forskolan
76. Wechsler D. Wechsler preschool and primary scale of intelligence™—fourth edition (WPPSI™—iV) (Swedish version). San antonio: Pearson Education (2012).
77. Roid GH, Sampers JL. Merrill-Palmer–revised scales of development manual (Swedish version). Wood Dale, IL: Stoelting (2004).
78. Lord C, Rutter M, DiLavore P, Risi S. Autism diagnostic observation schedule (ADOS). Los Angeles: Western Psychological Publishing (1999).
79. Lord C, Rutter M, DiLavore P, Risi S, Gotham K, Bishop S. Autism diagnostic observation schedule, second edition (ADOS-2) manual (part I) (Swedish version). Torrance: Western Psychological Services (2012).
80. Sparrow SS, Cicchetti D, Balla DA. Vineland adaptive behavior scales-2nd edition manual (Swedish version). Minneapolis: NCS Pearson Inc. (2005).
83. Miller LE, Dai YG, Fein DA, Robins DL. Characteristics of toddlers with early versus later diagnosis of autism spectrum disorder. Autism. (2021) 25:416–28. doi: 10.1177/1362361320959507
84. Dereu M, Warreyn P, Raymaekers R, Meirsschaut M, Pattyn G, Schietecatte I, et al. Screening for autism spectrum disorders in flemish day-care centres with the checklist for early signs of developmental disorders. J Autism Dev Disord. (2010) 40:1247–58. doi: 10.1007/s10803-010-0984-0
85. Westman Andersson G, Miniscalco C, Johansson U, Gillberg C. Autism in toddlers: can observation in preschool yield the same information as autism assessment in a specialised clinic? Sci World J. (2013) 2013:384745. doi: 10.1155/2013/384745
86. Branson D, Vigil DC, Bingham A. Community childcare Providers’ role in the early detection of autism Spectrum disorders. Early Child Educ J. (2008) 35(6):523–30. doi: 10.1007/s10643-008-0243-6
Keywords: autism, early detection, preschool, psychometric properties, multiethnic low resource setting
Citation: Linnsand P, Hermansson J, Gillberg C and Nygren G (2023) A feasibility study of a new instrument for detection of autism signs in preschool settings. Psychometric properties of the joint attention observation schedule preschool (JA-OBS preschool). Front. Child Adolesc. Psychiatry 1:1061451. doi: 10.3389/frcha.2022.1061451
Received: 4 October 2022; Accepted: 28 December 2022;
Published: 18 January 2023.
Edited by:
Marco Turi, Fondazione Stella Maris Mediterraneo Onlus, ItalyReviewed by:
Manabu Saito, Hirosaki University, JapanLilia Albores, Hospital Psiquiatrico Infantil Juan N. Navarro, Mexico
© 2023 Linnsand, Hermansson, Gillberg and Nygren. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Petra Linnsand cGV0cmEubGlubnNhbmRAdmdyZWdpb24uc2U=
Specialty Section: This article was submitted to Autism and Other Neurodevelopmental Disorders, a section of the journal Frontiers in Child and Adolescent Psychiatry
 Petra Linnsand
Petra Linnsand Jonas Hermansson
Jonas Hermansson Christopher Gillberg
Christopher Gillberg Gudrun Nygren
Gudrun Nygren