- 1Shaanxi Key Laboratory of Brain Disorders & Institute of Basic Medical Sciences & Institute of Basic and Translational Medicine, Xi’an Medical University, Xi’an, China
- 2State Key Laboratory of Military Stomatology, Department of Anesthesiology, School of Stomatology, The Fourth Military Medical University, Xi’an, China
Whether persons with schizophrenia have a higher or lower incidence of cancer has been discussed for a long time. Due to the complex mechanisms and characteristics of different types of cancer, it is difficult to evaluate the exact relationship between cancers and schizophrenia without considering the type of tumor. Schizophrenia, a disabling mental illness that is now recognized as a neurodevelopmental disorder, is more correlated with brain tumors, such as glioma, than other types of tumors. Thus, we mainly focused on the relationship between schizophrenia and glioma morbidity. Glioma tumorigenesis and schizophrenia may share similar mechanisms; gene/pathway disruption would affect neurodevelopment and reduce the risk of glioma. The molecular defects of disrupted-in-schizophrenia-1 (DISC1), P53, brain-derived neurotrophic factor (BDNF) and C-X-C chemokine receptors type 4 (CXCR4) involved in schizophrenia pathogenesis might play opposite roles in glioma development. Many microRNAs (miRNAs) such as miR-183, miR-9, miR-137 and miR-126 expression change may be involved in the cross talk between glioma prevalence and schizophrenia. Finally, antipsychotic drugs may have antitumor effects. All these factors show that persons with schizophrenia have a decreased incidence of glioma; therefore, epidemiological investigation and studies comparing genetic and epigenetic aberrations involved in both of these complex diseases should be performed. These studies can provide more insightful knowledge about glioma and schizophrenia pathophysiology and help to determine the target/strategies for the prevention and treatment of the two diseases.
Introduction
Early in 1909 (Commissioners in Lunacy for England and Wales, 1909), researchers first proposed a hypothesis that cancer risk decreased in persons with schizophrenia. Since then, numerous cohort studies have been performed to compare cancer incidence rates in persons with schizophrenia with the general population. However, conflicting results have been found; some studies showed a relatively lower risk of cancer in persons with schizophrenia (Lawrence et al., 2000; Cohen et al., 2002; Ji et al., 2013). In particular, Li et al. (2018) reported that the overall cancer incidence among patients with schizophrenia was slightly decreased (RR = 0.90, 95% confidence interval (CI) 0.81–0.99) in an updated meta-analysis of 16 cohort studies in 2018. However, other studies demonstrated a rather higher cancer risk in persons with schizophrenia (Lichtermann et al., 2001; Hippisley-Cox et al., 2007; McGinty et al., 2012). To date, it is still difficult to determine whether schizophrenia is a tumor-promoting factor or a suppressive factor. Researchers tried to give some reasonable explanations for this “century puzzle”: Preti and Wilson (2011) proposed that smoking, alcohol use, sex and lifestyle difference could affect the diagnosis of cancer among persons with schizophrenia. In addition, the antipsychotic therapy itself may have indirect anticancer effects which contribute to the reduced cancer risk in persons with schizophrenia (Dalton et al., 2006; Preti and Wilson, 2011). Genetic explanations showed that the schizophrenia genes may inhibit tumorigenesis (Park et al., 2004; Shi et al., 2008; Ozbey et al., 2011).
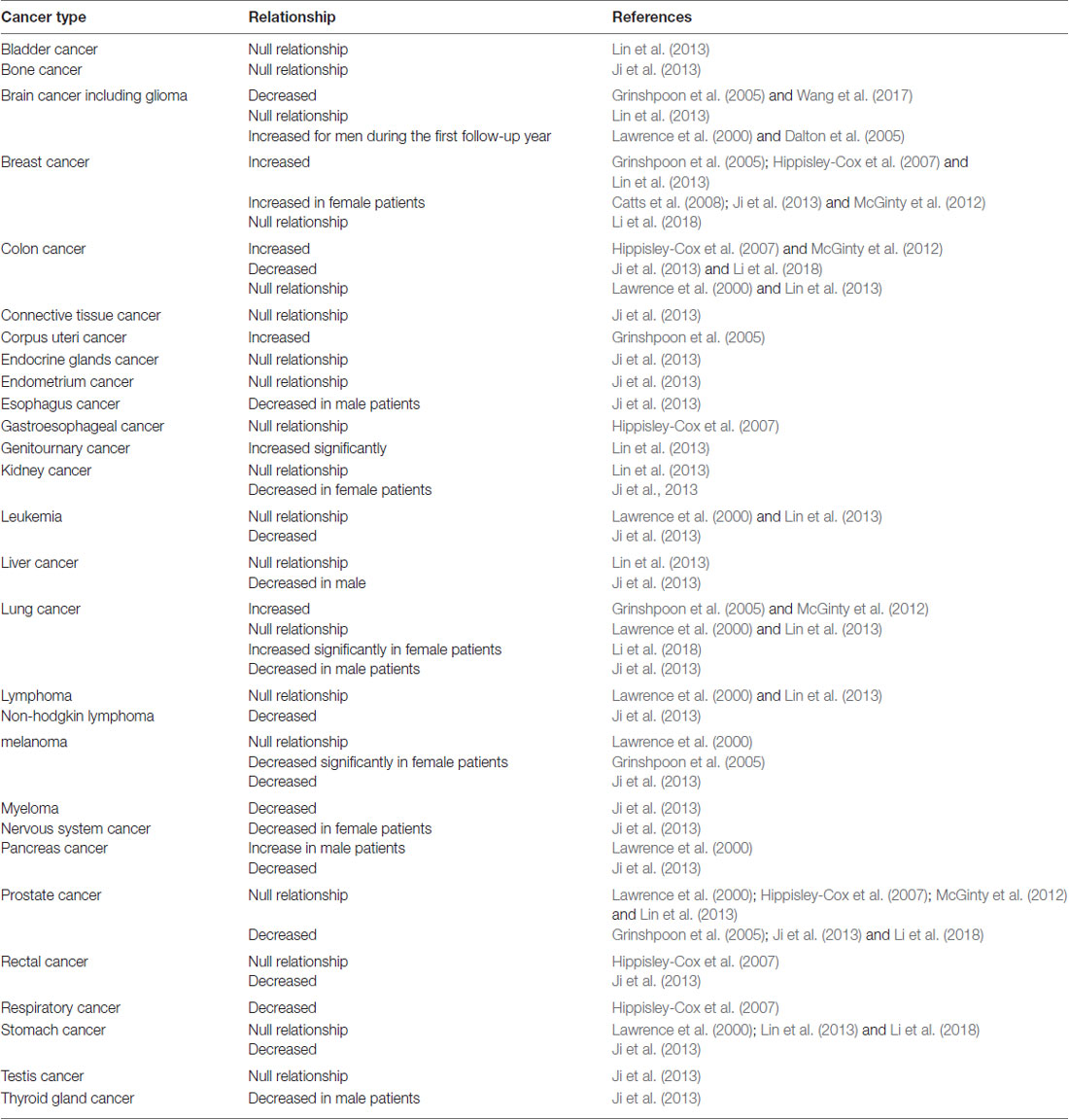
Different types of tumor have different pathogenesis characteristics, and thus, it is hard to generally evaluate the cancer risk in persons with schizophrenia without considering distinct cancer types (Table 1). In fact, numerous epidemiological investigations showed increased risk of breast cancer in people with schizophrenia (Grinshpoon et al., 2005; Hippisley-Cox et al., 2007; Carlsen et al., 2008), but decreased risk of prostate cancer (Grinshpoon et al., 2005; Ji et al., 2013; Li et al., 2018; Table 1). As a disabling mental illness that seems to originate from a disorder of brain development (Owen et al., 2016), schizophrenia is thought to be closely related to brain cancer such as glioma. Hence, we herein mainly focused on the relationship between glioma and schizophrenia. In this review article, we will compare the mechanisms of the glioma tumorigenesis and schizophrenia and try to determine whether the glioma risk in schizophrenia is higher or lower.
Persons With Schizophrenia Have Lower Risk of Gliomas?
Grinshpoon et al. (2005) reported that the standardized incidence ratios (SIRs) were statistically lower for cancer in the brain among men with schizophrenia (0.56, 95% CI 0.32–0.81). Dalton et al. (2005) found an increased brain cancer risk for men during the first follow-up year among persons with schizophrenia, but Lin et al. (2013) did not get similar results. As a result, the relationship between brain cancer risk and schizophrenia is still a puzzle. The brain cancers include the primary, secondary and extraparenchymal tumors (Brandão, 2016). We are interested in glioma, which is the most common and aggressive type of primary brain tumor (Gao et al., 2014, 2015). Previous epidemiological studies showed that persons with schizophrenia may less likely to suffer from gliomas (Grinshpoon et al., 2005; Wang et al., 2017). Although there were few epidemiological investigations about glioma risk and schizophrenia, many studies indicated that mechanisms involved in schizophrenia pathogenesis might play opposite roles in glioma development. These mechanisms are summarized herein. All of these mechanisms suggest that persons with schizophrenia would have lower risk of gliomas than persons without schizophrenia.
The Similar Mechanisms Involved in Glioma Tumorigenesis and Schizophrenia
Dysregulation of Schizophrenia-Related Genes in Glioma
DISC1
Disrupted-in-schizophrenia-1 (DISC1), a predisposing gene first found with its disruption by a balanced t(1;11) (q42;q14) in a large Scottish family, is identified to be closely related to major mental illnesses such as schizophrenia and bipolar disorder (St. Clair et al., 1990; Blackwood et al., 2001). Later, in a smaller American family with schizophrenia, the DISC1 gene was found to have a 4-bp frameshift mutation (Sachs et al., 2005). Studies further verified the potential association of the DISC1 gene with mental illnesses, especially schizophrenia, because many variants and polymorphisms of DISC1 were found in persons with schizophrenia (Thomson et al., 2013). Moreover, functional studies showed that DISC1 contributes to the etiopathology of mental illness, including regulating neural progenitor proliferation, neurite outgrowth, neuronal migration, synapse formation, neurogenesis and cAMP signaling (Lipina et al., 2012; Wen et al., 2014; Meng et al., 2016). These results demonstrated that DISC1 is strongly linked to the pathogenesis of schizophrenia.
Recently, our studies focused on the influence of DISC1 on glioma. A relatively higher expression of DISC1 was observed on glioma cells, and knocking down of DISC1 by shRNA significantly inhibited glioblastoma cell proliferation, migration, invasion and stem cell self-renewal. Further studies demonstrated that inhibition of DISC1 altered the mitochondrial dynamic by regulating Drp1 (Gao et al., 2016). Xie et al. (2015) showed that Drp1 activation is associated with poor prognosis of glioblastoma, suggesting that the mitochondrial dynamics were a regulatory switch for differentiation of glioma stem cells and could be treated as a new therapeutic target. Yin et al. (2016) proved that the Drp1 regulates glioma cell proliferation and invasion by the RHOA/ROCK1 pathway. Therefore, we first proposed a conclusion that DISC1 could play as an oncogene in GBM tumorigenesis.
Taken together, these data support the hypothesis that DISC1 might have the dual effect of regulating glioma tumorigenesis and neurodevelopment. It has been reported that DISC1 could interact with multiple proteins such as NDEL1, LIS1, GSK3β, 14-3-3, MAP1A, Girdin and PDE4 and play a role in either regulating neurodevelopment or promoting glioma progression (Gao et al., 2016).
P53
P53, one of the most important tumor suppressor genes, is usually lowly expressed in normal cells and regulates cellular stress responses (Hong et al., 2014). It has been reported that P53 is found to be mutated or deleted in more than 50% of all human cancers, suggesting that loss of P53 function contributes to cancer development (Peng et al., 2001; Olivier et al., 2002; Zheng et al., 2004; Hsu et al., 2010). Inhibition of P53 function helped to maintain the tumorigenic capacity of brain tumor-initiating cells (BTIC; Fukaya et al., 2016). Moreover, P53 mutant glioma patients exhibited therapeutic resistance and poor outcomes (Chen et al., 2017).
Recently, more and more studies have shown that P53 plays important roles in brain disorders (Agostini et al., 2018). P53 is highly expressed in the young mouse brain and lost in the adult mouse brain (Komarova et al., 1997; Ni et al., 2005). In 2000, Catts and Catts (2000) proposed that P53 might be a candidate susceptibility gene for schizophrenia by regulating apoptosis (Chiu et al., 2001). Moreover, the location of the P53 gene (chromosome 17p13.1) is close to 17p13.3, which is reported to have a significant linkage with schizophrenia incidence (Freedman et al., 2001). Ni et al. (2005) also reported a significant association between P53 and schizophrenia via case-control and family studies. Park et al. (2004) reported that the MspI polymorphisms of the P53 gene were specifically found in Korean schizophrenia and reduced the lung cancer predisposing. A similar result was found in the Turkish population by Ozbey et al. (2011). All these data suggest that P53 would be associated with schizophrenia and exhibit reduced vulnerability to cancer, but the detailed mechanism of the P53 gene in schizophrenia remains to be elucidated.
BDNF
Brain-derived neurotrophic factor (BDNF) plays an important role in neuronal development including neurogenesis, synaptic transmission and consolidation (Soule et al., 2006). Accumulating evidence indicates that the expression level of BDNF is altered in schizophrenia. Many studies showed that BDNF expression was reduced in persons with schizophrenia (Cannon et al., 2008; Pillai, 2008; Pandya et al., 2013), but some studies showed the opposite result (Reis et al., 2008). In addition, it has been reported that the epigenetic regulation of BDNF plays an important role in schizophrenia (Pandya et al., 2013). Kordi-Tamandani et al. (2012) showed that the downregulation of BDNF in persons with schizophrenia was associated with increased DNA methylation level of BDNF by methylation-specific PCR. In 2013, Tempei and colleagues reviewed the correlation between DNA methylation and BDNF promoter and found that the expression of BDNF in neural cells is tightly regulated by DNA methylation, thus suggesting a potential usefulness of the DNA methylation status of BDNF as a biomarker of psychiatric disorders including schizophrenia (Ikegame et al., 2013). Çöpoğlu et al. (2016) reported that there was a correlation between disease duration and DNA methylation, although there was no difference in methylation status of BDNF between persons with schizophrenia and controls. Furthermore, the polymorphisms of BDNF were reported to be associated with schizophrenia. The Val66Met polymorphism (rs6265) is a functional polymorphism affecting the secretion of BDNF. Sun et al. (2013) further found that the BDNF rs6265 may be a predisposing factor in schizophrenia from a Chinese Han population. A case-control meta-analysis showed a significant association between BDNF rs6265 and schizophrenia (Kheirollahi et al., 2016). All these data suggest that the altered BDNF function may be involved in schizophrenia pathophysiology (Angelucci et al., 2005).
In glioma patients, the expression of BDNF was significantly higher compared to control (Yan et al., 2009; Xiong et al., 2013b, 2015). Xiong et al. (2013a) found that the mature BDNF could promote glioma cell growth, inhibit cell apoptosis and increase cell motility and invasion. Furthermore, many studies reported that the Akt and Src are common downstream signaling kinase of BDNF and play an important role in glioma development (Sathornsumetee et al., 2007; Zhang et al., 2013; Saba et al., 2018). Inhibition of the Akt activation could inhibit the glioblastoma and glioblastoma stem-like cells (GSCs) growth, and induce apoptosis of malignant glioma cells (Gallia et al., 2009; Majewska and Szeliga, 2017; Shao et al., 2017). Src-family kinase (SFK) signaling is reported to affect a variety of tumor-related properties, particularly in the case of glioblastoma. Inhibition of Src could reduce growth and migration and change the motility of glioblastoma (Lewis-Tuffin et al., 2015). All these factors suggest that BDNF participates in the progression of glioma by regulating these oncogenic kinases.
CXCR4
C-X-C chemokine receptors type 4 (CXCR4) have been reported to overexpress in most cancers, including glioma (Gatti et al., 2013; Virgintino et al., 2013; Nazari et al., 2017). CXCL12 can bind to and activate CXCR4. Recent studies found that CXCR4 was significantly upregulated in GSCs and mediated the proliferation of GSCs. shRNA-mediated knockdown of CXCR4 in vivo also proved that CXCR4 could increase glioma perivascular invasion and reduce radiation-induced apoptosis (Yadav et al., 2016). PRX177561, a novel CXCR4 antagonist, could reduce GBM cell proliferation and accelerate GSC differentiation in preclinical models (Gravina et al., 2017). All these factors suggest a positive role of CXCR4 in glioma progression.
However, things seem different in schizophrenia. In the neuron development process, CXCR4 could regulate the migration and regional distribution of cortical interneurons (Li et al., 2008; Meechan et al., 2012). It has been reported that CXCR4 expression was downregulated and the promotor region of CXCR4 was hypermethylated in schizophrenia (Xu et al., 2012; Aberg et al., 2014). It has also been reported that 22q11 deletion syndrome (22q11DS) is a significant genetic predisposing factor for psychiatric conditions, including schizophrenia and bipolar disorder (Toritsuka et al., 2013). In a 22q11DS mouse model, the total CXCR4 protein reduced and the interneuron migration was disrupted (Meechan et al., 2012). All these factors suggest that the downregulation of CXCR4 in persons with schizophrenia would be a protective aspect for reducing the incidence of glioma.
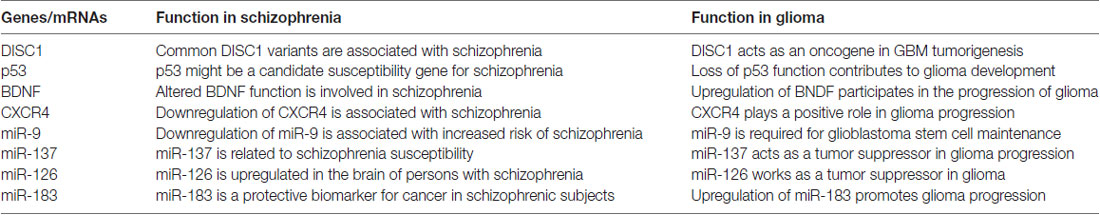
The above examples illustrate that glioma tumorigenesis and schizophrenia may share similar mechanisms, and the molecular defects of DISC1, P53, BDNF and CXCR4 involved in schizophrenia pathogenesis might play opposite roles in glioma development (Table 2).
Dysregulation of miRNA in Schizophrenia and Glioma
MicroRNAs (miRNAs or miRs) are small RNAs containing 20–23 nucleotides which regulate diverse biologic processes by inhibiting gene expression at the post-transcriptional level. Various studies have proved prominent roles of miRNAs in many physiological and pathological processes, and miRNAs could be a diagnostic and prognostic biomarker for various diseases such as cancer and CNS diseases including schizophrenia (Rao et al., 2013). Rizos et al. (2012) found that miR-183 was upregulated in the group of persons with schizophrenia without cancer but was almost undetectable in the group of persons with schizophrenia with a solid tumor. Therefore, they proposed that miR-183 could be a protective biomarker for cancer in schizophrenic subjects (Rizos et al., 2012). However, other studies indicated that highly expressed miR-183 promoted glioma cell proliferation and was significantly correlated with poor prognosis in glioma patients (Wang et al., 2016; Ye et al., 2016; Pavlakis et al., 2017). Therefore, whether miR-183 would be a protective gene for glioma in persons with schizophrenia needs to be further studied. MiR-9, another miRNA, was reported to be significantly downregulated in schizophrenia patient-derived neural progenitor cells, which affected neural migration and was associated with increased risk of schizophrenia (Topol et al., 2017). However, miR-9 was highly abundant in CD133(+) glioblastoma stem cells (Schraivogel et al., 2011). The Schizophrenia Psychiatric Genome-Wide Association Study (GWAS) Consortium (2011) reported that miR-137 was associated with schizophrenia susceptibility and regulated many schizophrenia susceptibility-related target genes (Yin et al., 2014). MiR-137 could also act as a tumor suppressor in glioma progression (Sun et al., 2015; Liang et al., 2016). It was reported that miR-126 was upregulated in the dorsolateral prefrontal cortex (DLPFC) of the brain in persons with schizophrenia (Beveridge et al., 2010). However, miR-126 worked as a tumor suppressor through inhibiting the target gene expression such as VEGF, CXCR4, DNMT1, KRAS in many cancers, especially glioma (Liu et al., 2015; Kong et al., 2016; Li et al., 2017). These studies indicated that many miRNAs play important roles in the development of glioma and schizophrenia (Table 1). The expression change of these miRNAs was associated with schizophrenia susceptibility but lower incidence of glioma.
Antipsychotic Drugs Have Antitumor Effects
Many studies have proved that antipsychotic drugs may have antitumor and radiosensitizing effects (Carney et al., 2006; Fond et al., 2012). A systematic review in 2012 suggested that phenothiazines had antitumor effect by inhibiting various cancer proliferation (Fond et al., 2012). Olanzapine, a second-generation antipsychotic, has been shown to inhibit the human glioblastoma cell lines proliferation, migration, anchorage-independent growth and enhance TMZ anti-tumor activity (Karpel-Massler et al., 2015). Cheng et al. (2015) found that thioridazine, a widely used antipsychotic drug, had potent anti-GBM and anti-GSCs properties. Thioridazine could induce the autophagy and ER stress of the GBM cells and upregulate AMPK activity. More recently, Wang et al. (2017) proved that the atypical antipsychotic quetiapine (QUE) could suppress GSCs-initiated tumor growth, and the anti-tumor activity could be enhanced by combination with TMZ. Furthermore, QUE could induce the differentiation of GSCs towards OL-like cells by inhibiting the Wnt/β-catenin signaling pathway, and suppress GSC and TMZ-resistant gliomas initiation by affecting GSCs proliferation (Wang et al., 2017). ErbB and its ligand epidermal growth factor (EGF) are reported to participate in both glioma development and schizophrenia neuropathology (Berezowska and Schlegel, 2011; Sotoyama et al., 2011; Iwakura and Nawa, 2013; Brocard et al., 2015), so antipsychotic drug targeting the EGF/ErbBs signaling pathway can affect the tumorigenesis of glioma in persons with schizophrenia. Clozapine, an atypical antipsychotic drug that treated schizophrenia by blocking the EGF/ErbBs systems (Paulzen et al., 2014), has been reported to inhibit the U87MG human glioblastoma cells proliferation (Shin et al., 2006; Jeon et al., 2015). Many studies showed that chlorpromazine could inhibit the Akt/mTOR pathway and induce autophagic cell death in glioma cells (Shin et al., 2013), and inhibit the TMZ-resistant glioma cells growth and proliferation in orthotopic mouse brain tumor models (Oliva et al., 2017). Aripiprazole is also an atypical antipsychotic which is widely used to treat schizophrenia. Kim et al. (2018) recently proved that aripiprazole inhibits the glioma cell migration and induces apoptosis by directly inhibiting oncogenic Src kinase. It has been reported that the Src and Akt are common downstream signaling kinases of BDNF (Zhang et al., 2013), so these findings are consistent with the increase of BDNF in glioma patients. All these factors suggest that antipsychotic drugs have antitumor effects; therefore, when taking antipsychotic drugs, persons with schizophrenia also benefit from it inhibiting glioma development.
Conclusions and Perspective
Several pieces of evidence provided here indicate that there might be a negative correlation between glioma and schizophrenia (Eskandari et al., 2015). Levav et al. (2007) found a reduced cancer risk among people with schizophrenia and proposed the presence of a gene with the dual effects of reducing cancer risk and disrupting neurodevelopment. We first discussed the genes which could play dual effects in glioma development and schizophrenia; the molecular defects of DISC1, P53, BDNF and CXCR4 involved in schizophrenia pathogenesis might play opposite roles in glioma development. Then, we indicated that many miRNAs such as miR-183, miR-9, miR-137 and miR-126 play important roles in the development of glioma and schizophrenia, and the expression change of these miRNAs was associated with schizophrenia susceptibility but lower incidence of glioma. Furthermore, many studies have found that antipsychotic drugs may have antitumor effects. All these studies showed that persons with schizophrenia have a decreased incidence of glioma, which can partially solve the “century puzzle” of whether persons with schizophrenia have a decreased incidence of cancer. Certainly, epidemiological investigation about glioma incidence and schizophrenia and further studies about the key genes/pathways involved in the pathogenesis of both glioma and schizophrenia, should be performed. These studies can provide more insightful understanding about glioma and schizophrenia pathophysiology and promote strategies for prevention and treatment applications in schizophrenia as well as cancer.
Author Contributions
All authors listed have made substantial, direct and intellectual contribution to the work, and approved it for publication.
Funding
This work was supported by the National Natural Science Foundation of China (Nos. 81873740, 81601376, 81402063 and 81471265), the Natural Science Basic Research Plan in Shaanxi Province of China (No. 2017JM8086), the China Postdoctoral Science Foundation (Nos. 2016M602993), the Leading Disciplines Development Government Foundation of Shaanxi, China, Xi’an Medical University’s key disciplines of molecular immunology.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Aberg, K. A., McClay, J. L., Nerella, S., Clark, S., Kumar, G., Chen, W., et al. (2014). Methylome-wide association study of schizophrenia: identifying blood biomarker signatures of environmental insults. JAMA Psychiatry 71, 255–264. doi: 10.1001/jamapsychiatry.2013.3730
Agostini, M., Melino, G., and Bernassola, F. (2018). The p53 family in brain disease. Antioxid. Redox Signal. 29, 1–14. doi: 10.1089/ars.2017.7302
Angelucci, F., Brenè, S., and Mathé, A. A. (2005). BDNF in schizophrenia, depression and corresponding animal models. Mol. Psychiatry 10, 345–352. doi: 10.1038/sj.mp.4001637
Berezowska, S., and Schlegel, J. (2011). Targeting ErbB receptors in high-grade glioma. Curr. Pharm. Des. 17, 2468–2487. doi: 10.2174/138161211797249233
Beveridge, N. J., Gardiner, E., Carroll, A. P., Tooney, P. A., and Cairns, M. J. (2010). Schizophrenia is associated with an increase in cortical microRNA biogenesis. Mol. Psychiatry 15, 1176–1189. doi: 10.1038/mp.2009.84
Blackwood, D. H., Fordyce, A., Walker, M. T., St Clair, D. M., Porteous, D. J., and Muir, W. J. (2001). Schizophrenia and affective disorders–cosegregation with a translocation at chromosome 1q42 that directly disrupts brain-expressed genes: clinical and P300 findings in a family. Am. J. Hum. Genet. 69, 428–433. doi: 10.1086/321969
Brandão, L. A. (2016). Adult brain tumors: imaging characterization of primary, secondary and extraparenchymal tumors in the central nervous system, including findings on advanced mr imaging techniques as well as treatment-related abnormalities. Neuroimaging Clin N. Am. 26, xiii–xiv. doi: 10.1016/j.nic.2016.08.008
Brocard, E., Oizel, K., Lalier, L., Pecqueur, C., Paris, F., Vallette, F. M., et al. (2015). Radiation-induced PGE2 sustains human glioma cells growth and survival through EGF signaling. Oncotarget 6, 6840–6849. doi: 10.18632/oncotarget.3160
Cannon, T. D., Yolken, R., Buka, S., Torrey, E. F., and Collaborative Study Group on the Perinatal Origins of Severe Psychiatric Disorders. (2008). Decreased neurotrophic response to birth hypoxia in the etiology of schizophrenia. Biol. Psychiatry 64, 797–802. doi: 10.1016/j.biopsych.2008.04.012
Carlsen, K., Høybye, M. T., Dalton, S. O., and Tjonneland, A. (2008). Social inequality and incidence of and survival from breast cancer in a population-based study in Denmark, 1994–2003. Eur. J. Cancer 44, 1996–2002. doi: 10.1016/j.ejca.2008.06.027
Carney, C. P., Jones, L., and Woolson, R. F. (2006). Medical comorbidity in women and men with schizophrenia: a population-based controlled study. J. Gen. Intern. Med. 21, 1133–1137. doi: 10.1111/j.1525-1497.2006.00563.x
Catts, V. S., and Catts, S. V. (2000). Apoptosis and schizophrenia: is the tumour suppressor gene, p53, a candidate susceptibility gene? Schizophr. Res. 41, 405–415. doi: 10.1016/s0920-9964(99)00077-8
Catts, V. S., Catts, S. V., O’Toole, B. I., and Frost, A. D. J. (2008). Cancer incidence in patients with schizophrenia and their first-degree relatives—a meta-analysis. Acta Psychiatr. Scand. 117, 323–336. doi: 10.1111/j.1600-0447.2008.01163.x
Chen, X. R., Ma, H. H., Wang, Z., Zhang, S. R., Yang, H. R., and Fang, Z. Y. (2017). EZH2 palmitoylation mediated by ZDHHC5 in p53-mutant glioma drives malignant development and progression. Cancer Res. 77, 4998–5010. doi: 10.1158/0008-5472.CAN-17-1139
Cheng, H. W., Liang, Y. H., Kuo, Y. L., Chuu, C. P., Lin, C. Y., Lee, M. H., et al. (2015). Identification of thioridazine, an antipsychotic drug, as an antiglioblastoma and anticancer stem cell agent using public gene expression data. Cell Death Dis. 6:e1753. doi: 10.1038/cddis.2015.77
Chiu, H. J., Wang, Y. C., Chen, J. Y., Hong, C. J., and Tsai, S. J. (2001). Association study of the p53-gene Pro72Arg polymorphism in schizophrenia. Psychiatry Res. 105, 279–283. doi: 10.1016/s0165-1781(01)00328-6
Cohen, M., Dembling, B., and Schorling, J. (2002). The association between schizophrenia and cancer: a population-based mortality study. Schizophr. Res. 57, 139–146. doi: 10.1016/s0920-9964(01)00308-5
Çöpoğlu, Ü. S., Igci, M., Bozgeyik, E., Kokacya, M. H., Igci, Y. Z., Dokuyucu, R., et al. (2016). DNA methylation of BDNF gene in schizophrenia. Med. Sci. Monit. 22, 397–402. doi: 10.12659/msm.895896
Dalton, S. O., Johansen, C., Poulsen, A. H., Nørgaard, M., Sørensen, H. T., McLaughlin, J. K., et al. (2006). Cancer risk among users of neuroleptic medication: a population-based cohort study. Br. J. Cancer 95, 934–939. doi: 10.1038/sj.bjc.6603259
Dalton, S. O., Mellemkjaer, L., Thomassen, L., Mortensen, P. B., and Johansen, C. (2005). Risk for cancer in a cohort of patients hospitalized for schizophrenia in Denmark, 1969–1993. Schizophr. Res. 75, 315–324. doi: 10.1016/j.schres.2004.11.009
Eskandari, M. R., Abdolmaleky, H. M., Zhou, J.-R., and Thiagalingam, S. (2015). “Reduced risk of cancer in schizophrenia, a bridge toward etio-pathology and therapy of both diseases,” in Epigenetics Territory and Cancer, ed. P. Mehdipour (Dordrecht: Springer), 137–166. doi: 10.1007/978-94-017-9639-2_5
Fond, G., Macgregor, A., Attal, J., Larue, A., Brittner, M., Ducasse, D., et al. (2012). Antipsychotic drugs: pro-cancer or anti-cancer? A systematic review. Med. Hypotheses 79, 38–42. doi: 10.1016/j.mehy.2012.03.026
Freedman, R., Leonard, S., Olincy, A., Kaufmann, C. A., Malaspina, D., Cloninger, C. R., et al. (2001). Evidence for the multigenic inheritance of schizophrenia. Am. J. Med. Genet. 105, 794–800. doi: 10.1002/ajmg.10100
Fukaya, R., Ohta, S., Yaguchi, T., Matsuzaki, Y., Sugihara, E., Okano, H., et al. (2016). MIF maintains the tumorigenic capacity of brain tumor-initiating cells by directly inhibiting p53. Cancer Res. 76, 2813–2823. doi: 10.1158/0008-5472.CAN-15-1011
Gallia, G. L., Tyler, B. M., Hann, C. L., Siu, I. M., Giranda, V. L., Vescovi, A. L., et al. (2009). Inhibition of Akt inhibits growth of glioblastoma and glioblastoma stem-like cells. Mol. Cancer Ther. 8, 386–393. doi: 10.1158/1535-7163.MCT-08-0680
Gao, X., Mi, Y., Guo, N., Hu, Z., Hu, F., Liu, D., et al. (2016). Disrupted in schizophrenia 1 (DISC1) inhibits glioblastoma development by regulating mitochondria dynamics. Oncotarget 7, 85963–85974. doi: 10.18632/oncotarget.13290
Gao, X., Mi, Y., Ma, Y., and Jin, W. (2014). LEF1 regulates glioblastoma cell proliferation, migration, invasion and cancer stem-like cell self-renewal. Tumour Biol. 35, 11505–11511. doi: 10.1007/s13277-014-2466-z
Gao, X., Mi, Y., Yan, A., Sha, B., Guo, N., Hu, Z., et al. (2015). The PHLDB1 rs498872 (11q23.3) polymorphism and glioma risk: a meta-analysis. Asia Pac. J. Clin. Oncol. 11, e13–e21. doi: 10.1111/ajco.12211
Gatti, M., Pattarozzi, A., Bajetto, A., Würth, R., Daga, A., Fiaschi, P., et al. (2013). Inhibition of CXCL12/CXCR4 autocrine/paracrine loop reduces viability of human glioblastoma stem-like cells affecting self-renewal activity. Toxicology 314, 209–220. doi: 10.1016/j.tox.2013.10.003
Gravina, G. L., Mancini, A., Colapietro, A., Vitale, F., Vetuschi, A., Pompili, S., et al. (2017). The novel CXCR4 antagonist, PRX177561, reduces tumor cell proliferation and accelerates cancer stem cell differentiation in glioblastoma preclinical models. Tumour Biol. 39:1010428317695528. doi: 10.1177/1010428317695528
Grinshpoon, A., Barchana, M., Ponizovsky, A., Lipshitz, I., Nahon, D., Tal, O., et al. (2005). Cancer in schizophrenia: is the risk higher or lower? Schizophr. Res. 73, 333–341. doi: 10.1016/j.schres.2004.06.016
Hippisley-Cox, J., Vinogradova, Y., Coupland, C., and Parker, C. (2007). Risk of malignancy in patients with schizophrenia or bipolar disorder: nested case-control study. Transl. Psychiatry 64, 1368–1376. doi: 10.1001/archpsyc.64.12.1368
Hong, B., van den Heuvel, A. P., Prabhu, V. V., Zhang, S., and El-Deiry, W. S. (2014). Targeting tumor suppressor p53 for cancer therapy: strategies, challenges and opportunities. Curr. Drug Targets 15, 80–89. doi: 10.2174/1389450114666140106101412
Hsu, F. F., Lin, T. Y., Chen, J. Y., and Shieh, S. Y. (2010). p53-mediated transactivation of LIMK2b links actin dynamics to cell cycle checkpoint control. Oncogene 29, 2864–2876. doi: 10.1038/onc.2010.40
Ikegame, T., Bundo, M., Murata, Y., Kasai, K., Kato, T., and Iwamoto, K. (2013). DNA methylation of the BDNF gene and its relevance to psychiatric disorders. J. Hum. Genet. 58, 434–438. doi: 10.1038/jhg.2013.65
Iwakura, Y., and Nawa, H. (2013). ErbB1-4-dependent EGF/neuregulin signals and their cross talk in the central nervous system: pathological implications in schizophrenia and Parkinson’s disease. Front. Cell. Neurosci. 7:4. doi: 10.3389/fncel.2013.00004
Jeon, S., Kim, Y., Chung, I. W., and Kim, Y. S. (2015). Clozapine induces chloride channel-4 expression through PKA activation and modulates CDK5 expression in SH-SY5Y and U87 cells. Prog. Neuropsychopharmacol. Biol. Psychiatry 56, 168–173. doi: 10.1016/j.pnpbp.2014.09.002
Ji, J. G., Sundquist, K., Ning, Y., Kendler, K. S., Sundquist, J., and Chen, X. N. (2013). Incidence of cancer in patients with schizophrenia and their first-degree relatives: a population-based study in sweden. Schizophr. Bull. 39, 527–536. doi: 10.1093/schbul/sbs065
Karpel-Massler, G., Kast, R. E., Westhoff, M. A., Dwucet, A., Welscher, N., Nonnenmacher, L., et al. (2015). Olanzapine inhibits proliferation, migration and anchorage-independent growth in human glioblastoma cell lines and enhances temozolomide’s antiproliferative effect. J. Neurooncol. 122, 21–33. doi: 10.1007/s11060-014-1688-7
Kheirollahi, M., Kazemi, E., and Ashouri, S. (2016). Brain-derived neurotrophic factor gene Val66Met polymorphism and risk of schizophrenia: a meta-analysis of case-control studies. Cell. Mol. Neurobiol. 36, 1–10. doi: 10.1007/s10571-015-0229-z
Kim, M. S., Yoo, B. C., Yang, W. S., Han, S. Y., Jeong, D., Song, J. M., et al. (2018). Src is the primary target of aripiprazole, an atypical antipsychotic drug, in its anti-tumor action. Oncotarget 9, 5979–5992. doi: 10.18632/oncotarget.23192
Komarova, E. A., Chernov, M. V., Franks, R., Wang, K., Armin, G., Zelnick, C. R., et al. (1997). Transgenic mice with p53-responsive lacZ: p53 activity varies dramatically during normal development and determines radiation and drug sensitivity in vivo. EMBO J. 16, 1391–1400. doi: 10.1093/emboj/16.6.1391
Kong, R. R., Ma, Y. F., Feng, J., Li, S. M., Zhang, W., Jiang, J. T., et al. (2016). The crucial role of miR-126 on suppressing progression of esophageal cancer by targeting VEGF-A. Cell. Mol. Biol. Lett. 21:3. doi: 10.1186/s11658-016-0004-2
Kordi-Tamandani, D. M., Sahranavard, R., and Torkamanzehi, A. (2012). DNA methylation and expression profiles of the brain-derived neurotrophic factor (BDNF) and dopamine transporter (DAT1) genes in patients with schizophrenia. Mol. Biol. Rep. 39, 10889–10893. doi: 10.1007/s11033-012-1986-0
Lawrence, D., Holman, C. D., Jablensky, A. V., Threlfall, T. J., and Fuller, S. A. (2000). Excess cancer mortality in Western Australian psychiatric patients due to higher case fatality rates. Acta Psychiatr. Scand. 101, 382–388. doi: 10.1034/j.1600-0447.2000.101005382.x
Levav, I., Lipshitz, I., Novikov, I., Pugachova, I., Kohn, R., Barchana, M., et al. (2007). Cancer risk among parents and siblings of patients with schizophrenia. Br. J. Psychiatry 190, 156–161. doi: 10.1192/bjp.bp.106.024943
Lewis-Tuffin, L. J., Feathers, R., Hari, P., Durand, N., Li, Z., Rodriguez, F. J., et al. (2015). Src family kinases differentially influence glioma growth and motility. Mol. Oncol. 9, 1783–1798. doi: 10.1016/j.molonc.2015.06.001
Li, G., Adesnik, H., Li, J., Long, J., Nicoll, R. A., Rubenstein, J. L., et al. (2008). Regional distribution of cortical interneurons and development of inhibitory tone are regulated by Cxcl12/Cxcr4 signaling. J. Neurosci. 28, 1085–1098. doi: 10.1523/JNEUROSCI.4602-07.2008
Li, Y., Li, Y. Q. Q., Ge, P. F. F., and Ma, C. Y. (2017). MiR-126 regulates the ERK pathway via targeting KRAS to inhibit the glioma cell proliferation and invasion. Mol. Neurobiol. 54, 137–145. doi: 10.1007/s12035-015-9654-8
Li, H. L., Li, J. S., Yu, X. Y., Zheng, H. W., Sun, X., Lu, Y., et al. (2018). The incidence rate of cancer in patients with schizophrenia: a meta-analysis of cohort studies. Schizophr. Res. 195, 519–528. doi: 10.1016/j.schres.2017.08.065
Liang, M. L., Hsieh, T. H., Ng, K. H., Tsai, Y. N., Tsai, C. F., Chao, M. E., et al. (2016). Downregulation of miR-137 and miR-6500–3p promotes cell proliferation in pediatric high-grade gliomas. Oncotarget 7, 19723–19737. doi: 10.18632/oncotarget.7736
Lichtermann, D., Ekelund, J., Pukkala, E., Tanskanen, A., and Lænnqvist, J. (2001). Incidence of cancer among persons with schizophrenia and their relatives. Arch. Gen. Psychiatry 58, 573–578. doi: 10.1001/archpsyc.58.6.573
Lin, G. M., Chen, Y. J., Kuo, D. J., Jaiteh, L. E., Wu, Y. C., Lo, T. S., et al. (2013). Cancer incidence in patients with schizophrenia or bipolar disorder: a nationwide population-based study in Taiwan, 1997–2009. Schizophr. Bull. 39, 407–416. doi: 10.1093/schbul/sbr162
Lipina, T. V., Wang, M., Liu, F., and Roder, J. C. (2012). Synergistic interactions between PDE4B and GSK-3: DISC1 mutant mice. Neuropharmacology 62, 1252–1262. doi: 10.1016/j.neuropharm.2011.02.020
Liu, R. H., Gu, J., Jiang, P., Zheng, Y. J., Liu, X. M., Jiang, X. C., et al. (2015). DNMT1-microRNA126 epigenetic circuit contributes to esophageal squamous cell carcinoma growth via ADAM9-EGFR-AKT signaling. Clin. Cancer Res. 21, 854–863. doi: 10.1158/1078-0432.CCR-14-1740
Majewska, E., and Szeliga, M. (2017). AKT/GSK3β signaling in glioblastoma. Neurochem. Res. 42, 918–924. doi: 10.1007/s11064-016-2044-4
McGinty, E. E., Zhang, Y., Guallar, E., Ford, D. E., Steinwachs, D., Dixon, L. B., et al. (2012). Cancer incidence in a sample of Maryland residents with serious mental illness. Psychiatr. Serv. 63, 714–717. doi: 10.1176/appi.ps.201100169
Meechan, D. W., Tucker, E. S., Maynard, T. M., and Lamantia, A. S. (2012). Cxcr4 regulation of interneuron migration is disrupted in 22q11.2 deletion syndrome. Proc. Natl. Acad. Sci. U S A 109, 18601–18606. doi: 10.1073/pnas.1211507109
Meng, X., Zhu, S., Shevelkin, A., Ross, C. A., and Pletnikov, M. (2016). DISC1, astrocytes and neuronal maturation: a possible mechanistic link with implications for mental disorders. J. Neurochem. 138, 518–524. doi: 10.1111/jnc.13663
Nazari, A., Khorramdelazad, H., and Hassanshahi, G. (2017). Biological/pathological functions of the CXCL12/CXCR4/CXCR7 axes in the pathogenesis of bladder cancer. Int. J. Clin. Oncol. 22, 991–1000. doi: 10.1007/s10147-017-1187-x
Ni, X., Trakalo, J., Valente, J., Azevedo, M. H., Pato, M. T., Pato, C. N., et al. (2005). Human p53 tumor suppressor gene (TP53) and schizophrenia: case-control and family studies. Neurosci. Lett. 388, 173–178. doi: 10.1016/j.neulet.2005.06.050
Oliva, C. R., Zhang, W., Langford, C., Suto, M. J., and Griguer, C. E. (2017). Repositioning chlorpromazine for treating chemoresistant glioma through the inhibition of cytochrome c oxidase bearing the COX4–1 regulatory subunit. Oncotarget 8, 37568–37583. doi: 10.18632/oncotarget.17247
Olivier, M., Eeles, R., Hollstein, M., Khan, M. A., Harris, C. C., and Hainaut, P. (2002). The IARC TP53 database: new online mutation analysis and recommendations to users. Hum. Mutat. 19, 607–614. doi: 10.1002/humu.10081
Owen, M. J., Sawa, A., and Mortensen, P. B. (2016). Schizophrenia. Lancet 388, 86–97. doi: 10.1016/S0140-6736(15)01121-6
Ozbey, U., Yuce, H., Namli, M., and Elkiran, T. (2011). Investigation of differences in P53 gene polymorphisms between schizophrenia and lung cancer patients in the turkish population. Genet. Res. Int. 2011:483851. doi: 10.4061/2011/483851
Pandya, C. D., Kutiyanawalla, A., and Pillai, A. (2013). BDNF-TrkB signaling and neuroprotection in schizophrenia. Asian J. Psychiatr. 6, 22–28. doi: 10.1016/j.ajp.2012.08.010
Park, J. K., Lee, H. J., Kim, J. W., Park, Y. H., Lee, S. S., Chang, H. I., et al. (2004). Differences in p53 gene polymorphisms between Korean schizophrenia and lung cancer patients. Schizophr. Res. 67, 71–74. doi: 10.1016/s0920-9964(03)00155-5
Paulzen, M., Veselinovic, T., and Gründer, G. (2014). Effects of psychotropic drugs on brain plasticity in humans. Restor. Neurol. Neurosci. 32, 163–181. doi: 10.3233/RNN-139004
Pavlakis, E., Tonchev, A. B., Kaprelyan, A., Enchev, Y., and Stoykova, A. (2017). Interaction between transcription factors PAX6/PAX6–5a and specific members of miR-183–96-182 cluster, may contribute to glioma progression in glioblastoma cell lines. Oncol. Rep. 37, 1579–1592. doi: 10.3892/or.2017.5411
Peng, Y., Chen, L., Li, C., Lu, W., and Chen, J. (2001). Inhibition of MDM2 by hsp90 contributes to mutant p53 stabilization. J. Biol. Chem. 276, 40583–40590. doi: 10.1074/jbc.M102817200
Pillai, A. (2008). Brain-derived neurotropic factor/TrkB signaling in the pathogenesis and novel pharmacotherapy of schizophrenia. Neurosignals 16, 183–193. doi: 10.1159/000111562
Preti, A., and Wilson, D. R. (2011). Schizophrenia, cancer and obstetric complications in an evolutionary perspective-an empirically based hypothesis. Psychiatry Investig. 8, 77–88. doi: 10.4306/pi.2011.8.2.77
Rao, P., Benito, E., and Fischer, A. (2013). MicroRNAs as biomarkers for CNS disease. Front. Mol. Neurosci. 6:39. doi: 10.3389/fnmol.2013.00039
Reis, H. J., Nicolato, R., Barbosa, I. G., Teixeira Do Prado, P. H., Romano-Silva, M. A., and Teixeira, A. L. (2008). Increased serum levels of brain-derived neurotrophic factor in chronic institutionalized patients with schizophrenia. Neurosci. Lett. 439, 157–159. doi: 10.1016/j.neulet.2008.05.022
Rizos, E., Siafakas, N., Koumarianou, A., Katsantoni, E., Filippopoulou, A., Ntounas, P., et al. (2012). miR-183 as a molecular and protective biomarker for cancer in schizophrenic subjects. Oncol. Rep. 28, 2200–2204. doi: 10.3892/or.2012.2052
Saba, J., Turati, J., Ramírez, D., Carniglia, L., Durand, D., Lasaga, M., et al. (2018). Astrocyte truncated-TrkB mediates BDNF antiapoptotic effect leading to neuroprotection. J. Neurochem. doi: 10.1111/jnc.14476 [Epub ahead of print].
Sachs, N. A., Sawa, A., Holmes, S. E., Ross, C. A., DeLisi, L. E., and Margolis, R. L. (2005). A frameshift mutation in disrupted in schizophrenia 1 in an American family with schizophrenia and schizoaffective disorder. Mol. Psychiatry 10, 758–764. doi: 10.1038/sj.mp.4001667
Sathornsumetee, S., Vredenburgh, K. A., Lattimore, K. P., and Rich, J. N. (2007). Malignant glioma drug discovery–targeting protein kinases. Expert Opin. Drug Discov. 2, 1–17. doi: 10.1517/17460441.2.1.1
Schraivogel, D., Weinmann, L., Beier, D., Tabatabai, G., Eichner, A., Zhu, J. Y., et al. (2011). CAMTA1 is a novel tumour suppressor regulated by miR-9/9* in glioblastoma stem cells. EMBO J. 30, 4309–4322. doi: 10.1038/emboj.2011.301
Shao, Y. Y., Zhang, T. L., Wu, L. X., Zou, H. C., Li, S., Huang, J., et al. (2017). AKT axis, miR-21, and RECK play pivotal roles in dihydroartemisinin killing malignant glioma cells. Int. J. Mol. Sci. 18:E350. doi: 10.3390/ijms18020350
Shi, J., Gershon, E. S., and Liu, C. (2008). Genetic associations with schizophrenia: meta-analyses of 12 candidate genes. Schizophr. Res. 104, 96–107. doi: 10.1016/j.schres.2008.06.016
Shin, S. Y., Choi, B. H., Ko, J., Kim, S. H., Kim, Y. S., and Lee, Y. H. (2006). Clozapine, a neuroleptic agent, inhibits Akt by counteracting Ca2+/calmodulin in PTEN-negative U-87MG human glioblastoma cells. Cell. Signal. 18, 1876–1886. doi: 10.1016/j.cellsig.2006.02.004
Shin, S. Y., Lee, K. S., Choi, Y. K., Lim, H. J., Lee, H. G., Lim, Y., et al. (2013). The antipsychotic agent chlorpromazine induces autophagic cell death by inhibiting the Akt/mTOR pathway in human U-87MG glioma cells. Carcinogenesis 34, 2080–2089. doi: 10.1093/carcin/bgt169
Sotoyama, H., Zheng, Y., Iwakura, Y., Mizuno, M., Aizawa, M., Shcherbakova, K., et al. (2011). Pallidal hyperdopaminergic innervation underlying D2 receptor-dependent behavioral deficits in the schizophrenia animal model established by EGF. PLoS One 6:e25831. doi: 10.1371/journal.pone.0025831
Soule, J., Messaoudi, E., and Bramham, C. R. (2006). Brain-derived neurotrophic factor and control of synaptic consolidation in the adult brain. Biochem. Soc. Trans. 34, 600–604. doi: 10.1042/bst0340600
St. Clair, D., Blackwood, D., Muir, W., Carothers, A., Walker, M., Spowart, G., et al. (1990). Association within a family of a balanced autosomal translocation with major mental illness. Lancet 336, 13–16. doi: 10.1016/0140-6736(90)91520-k
Sun, M. M., Yang, L. M., Wang, Y., Feng, X., Cui, K. Y., Liu, L. F., et al. (2013). BDNF Val66Met polymorphism and anxiety/depression symptoms in schizophrenia in a Chinese Han population. Psychiatr. Genet. 23, 124–129. doi: 10.1097/YPG.0b013e328360c866
Sun, J., Zheng, G., Gu, Z., and Guo, Z. (2015). MiR-137 inhibits proliferation and angiogenesis of human glioblastoma cells by targeting EZH2. J. Neurooncol. 122, 481–489. doi: 10.1007/s11060-015-1753-x
The Schizophrenia Psychiatric Genome-Wide Association Study (GWAS) Consortium. (2011). Genome-wide association study identifies five new schizophrenia loci. Nat. Genet. 43, 969–976. doi: 10.1038/ng.940
Thomson, P. A., Malavasi, E. L., Grunewald, E., Soares, D. C., Borkowska, M., and Millar, J. K. (2013). DISC1 genetics, biology and psychiatric illness. Front. Biol. 8, 1–31. doi: 10.1007/s11515-012-1254-7
Topol, A., Zhu, S., Hartley, B. J., English, J., Hauberg, M. E., Tran, N., et al. (2017). Dysregulation of miRNA-9 in a subset of schizophrenia patient-derived neural progenitor cells. Cell Rep. 20:2525. doi: 10.1016/j.celrep.2017.08.073
Toritsuka, M., Kimoto, S., Muraki, K., Landek-Salgado, M. A., Yoshida, A., Yamamoto, N., et al. (2013). Deficits in microRNA-mediated Cxcr4/Cxcl12 signaling in neurodevelopmental deficits in a 22q11 deletion syndrome mouse model. Proc. Natl. Acad. Sci. U S A 110, 17552–17557. doi: 10.1073/pnas.1312661110
Virgintino, D., Errede, M., Rizzi, M., Girolamo, F., Strippoli, M., Walchli, T., et al. (2013). The CXCL12/CXCR4/CXCR7 ligand-receptor system regulates neuro-glio-vascular interactions and vessel growth during human brain development. J. Inherit. Metab. Dis. 36, 455–466. doi: 10.1007/s10545-012-9574-y
Wang, Y., Huang, N., Li, H., Liu, S., Chen, X., Yu, S., et al. (2017). Promoting oligodendroglial-oriented differentiation of glioma stem cell: a repurposing of quetiapine for the treatment of malignant glioma. Oncotarget 8, 37511–37524. doi: 10.18632/oncotarget.16400
Wang, Z. Y., Xiong, J., Zhang, S. S., Wang, J. J., Gong, Z. J., and Dai, M. H. (2016). Up-regulation of microRNA-183 promotes cell proliferation and invasion in glioma by directly targeting NEFL. Cell. Mol. Neurobiol. 36, 1303–1310. doi: 10.1007/s10571-016-0328-5
Wen, Z., Nguyen, H. N., Guo, Z., Lalli, M. A., Wang, X., Su, Y., et al. (2014). Synaptic dysregulation in a human iPS cell model of mental disorders. Nature 515, 414–418. doi: 10.1038/nature13716
Xie, Q., Wu, Q., Horbinski, C. M., Flavahan, W. A., Yang, K., Zhou, W., et al. (2015). Mitochondrial control by DRP1 in brain tumor initiating cells. Nat. Neurosci. 18, 501–510. doi: 10.1038/nn.3960
Xiong, J., Zhou, L., Lim, Y., Yang, M., Zhu, Y. H., Li, Z. W., et al. (2013a). Mature BDNF promotes the growth of glioma cells in vitro. Oncol. Rep. 30, 2719–2724. doi: 10.3892/or.2013.2746
Xiong, J., Zhou, L., Yang, M., Lim, Y., Zhu, Y. H., Fu, D. L., et al. (2013b). ProBDNF and its receptors are upregulated in glioma and inhibit the growth of glioma cells in vitro. Neuro Oncol. 15, 990–1007. doi: 10.1093/neuonc/not039
Xiong, J., Zhou, L. I., Lim, Y., Yang, M., Zhu, Y. H., Li, Z. W., et al. (2015). Mature brain-derived neurotrophic factor and its receptor TrkB are upregulated in human glioma tissues. Oncol. Lett. 10, 223–227. doi: 10.3892/ol.2015.3181
Xu, J., Sun, J., Chen, J., Wang, L., Li, A., Helm, M., et al. (2012). RNA-Seq analysis implicates dysregulation of the immune system in schizophrenia. BMC Genomics 13:S2. doi: 10.1186/1471-2164-13-s8-s2
Yadav, V. N., Zamler, D., Baker, G. J., Kadiyala, P., Erdreich-Epstein, A., Decarvalho, A. C., et al. (2016). CXCR4 increases in vivo glioma perivascular invasion and reduces radiation induced apoptosis: a genetic knockdown study. Oncotarget 7, 83701–83719. doi: 10.18632/oncotarget.13295
Yan, Q., Yu, H. L., and Li, J. T. (2009). Study on the expression of BDNF in human gliomas. Sichuan Da Xue Xue Bao Yi Xue Ban 40, 415–417. Available online at: http://europepmc.org/abstract/MED/19626994
Ye, Z. N., Zhang, Z. H., Wu, L. Y., Liu, C. G., Chen, Q., Liu, J. P., et al. (2016). Upregulation of miR-183 expression and its clinical significance in human brain glioma. Neurol. Sci. 37, 1341–1347. doi: 10.1007/s10072-016-2599-5
Yin, J., Lin, J., Luo, X., Chen, Y., Li, Z., Ma, G., et al. (2014). miR-137: a new player in schizophrenia. Int. J. Mol. Sci. 15, 3262–3271. doi: 10.3390/ijms15023262
Yin, M., Lu, Q., Liu, X., Wang, T., Liu, Y., and Chen, L. (2016). Silencing Drp1 inhibits glioma cells proliferation and invasion by RHOA/ROCK1 pathway. Biochem. Biophys. Res. Commun. 478, 663–668. doi: 10.1016/j.bbrc.2016.08.003
Zhang, Z., Fan, J., Ren, Y., Zhou, W., and Yin, G. (2013). The release of glutamate from cortical neurons regulated by BDNF via the TrkB/Src/PLC-γ1 pathway. J. Cell. Biochem. 114, 144–151. doi: 10.1002/jcb.24311
Keywords: schizophrenia, glioma, protection, DISC1, miRNA
Citation: Gao X, Mi Y, Guo N, Xu H, Jiang P, Zhang R, Xu L and Gou X (2018) Glioma in Schizophrenia: Is the Risk Higher or Lower? Front. Cell. Neurosci. 12:289. doi: 10.3389/fncel.2018.00289
Received: 28 May 2018; Accepted: 13 August 2018;
Published: 03 September 2018.
Edited by:
Federico Giove, Centro Fermi—Museo Storico della Fisica e Centro Studi e Ricerche Enrico Fermi, ItalyReviewed by:
Kayla A. Chase, University of California, San Diego, United StatesYuriko Iwakura, Niigata University, Japan
Copyright © 2018 Gao, Mi, Guo, Xu, Jiang, Zhang, Xu and Gou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lixian Xu, eGx4MTE2QGZtbXUuZWR1LmNu
Xingchun Gou, Z291eGluZ2NodW5AMTg5LmNu
† These authors have contributed equally to this work
 Xingchun Gao
Xingchun Gao Yajing Mi
Yajing Mi Na Guo
Na Guo Hao Xu
Hao Xu Pengtao Jiang1
Pengtao Jiang1 Ruisan Zhang
Ruisan Zhang Xingchun Gou
Xingchun Gou