- 1Emergency Medicine Clinical Research Center, Beijing Chao-Yang Hospital, Capital Medical University, Beijing, China
- 2Beijing Key Laboratory of Cardiopulmonary Cerebral Resuscitation, Beijing Chaoyang Hospital, Capital Medical University, Beijing, China
- 3Clinical Center for Medicine in Acute Infection, Capital Medical University, Beijing, China
Background: Community-acquired pneumonia (CAP) poses a significant health threat to the elderly population, leading to high morbidity and mortality rates. Serum ferritin, a critical indicator of iron metabolism, plays a pivotal role in inflammation and immune regulation. Nevertheless, its specific prognostic relevance in elderly patients with CAP remains unclear. This study aimed to evaluate the predictive capacity of serum ferritin in determining the prognosis of elderly patients with CAP and to investigate its effectiveness when combined with the sequential organ failure assessment (SOFA) or CURB-65 (confusion, uremia, respiratory rate, blood pressure, aged ≥65 years) scores.
Methods: This retrospective cohort study included 451 elderly patients (aged ≥65 years) diagnosed with CAP according to established criteria. Serum ferritin concentrations were measured upon admission and various prognostic indicators such as 28-day mortality, mechanical ventilation requirement, and vasopressor administration were analyzed in conjunction with white blood count (WBC), C-reactive protein (CRP), procalcitonin (PCT), lactate (Lac), SOFA scores, and CURB-65 scores. The independent predictive value of ferritin was assessed through receiver operating characteristic (ROC) curve analysis and multivariate logistic regression.
Results: Among the 451 patients, 99 (22%) died within 28 days. The area under the curve (AUC) of serum ferritin for predicting 28-day mortality was 0.75 (95%CI: 0.695-0.805). Ferritin outperformed WBC, CRP, and PCT in predictive performance, and its performance was comparable to Lac. When combined with SOFA or CURB-65 scores, the AUC of ferritin for predicting 28-day mortality increased to 0.84 and 0.847, respectively (P<0.001). Moreover, the AUC of ferritin for predicting vasopressor administration was 0.707, which increased to 0.864 and 0.822 when combined with SOFA or CURB-65 scores, respectively (P<0.001). Ferritin could predict mechanical ventilation requirement with an AUC of 0.618, but it was not an independent risk factor, and its predictive ability was not significantly different from other indicators.
Conclusion: Admission serum ferritin is an independent predictor for the prognosis of elderly patients with CAP, and it exhibits a strong ability to predict the 28-day mortality and vasopressor administration. The combination of ferritin with SOFA and CURB-65 scores significantly improves the prognostic predictive potency.
Introduction
Community-acquired pneumonia (CAP) is an acute disease characterized by high morbidity and mortality (Cillóniz et al., 2018). The elderly population, due to age-related physiological changes and a greater prevalence of comorbidities, faces an elevated risk of morbidity and mortality associated with CAP (Brown et al., 2018). Rapid progression of the disease in elderly patients often necessitates hospitalization and can lead to poor clinical outcomes in the absence of timely or appropriate treatment. Therefore, identifying reliable prognostic markers is of great significance for predicting disease severity and developing personalized treatment strategies, thus improving the clinical outcomes of patients with CAP (Metlay et al., 2019).
As a protein that can store iron in the cells, ferritin has been extensively explored in different clinical conditions, and it can fulfill various functions, not limited to iron metabolism. Considered an acute-phase reactive protein, it has shown a significant increase in concentration during systemic inflammatory reactions, serving as an indicator of immune system dysregulation severit (Kernan and Carcillo, 2017). The elevated serum ferritin concentration has been validated to be associated with a poor prognosis in inflammatory diseases (such as sepsis and other critical illnesses) (Fang et al., 2022), and this indicator also plays a predictive role in assessing the severity and mortality of diseases. For example, a higher ferritin concentration is associated with the increased mortality of patients with sepsis (Horvat et al., 2022), and it is also correlated with a poor prognosis of some tumors and autoimmune diseases (Wang et al., 2023; Giemza-Stokłosa et al., 2019). Despite the established role of ferritin in various diseases, its predictive value in elderly patients with CAP has not been fully clarified. Therefore, it is necessary to investigate the potential of ferritin as a prognostic tool in elderly patients with CAP, especially in predicting some key outcomes. Given these facts, this study was conducted to assess the predictive ability of ferritin concentrations (the 28-day mortality, mechanical ventilation requirement, and vasopressor administration) in elderly patients with CAP and identify whether ferritin can be used as a reliable biomarker in clinical practice. These efforts are expected to improve the prognostic prediction of CAP and guide clinical decisions for the treatment of this disease.
Materials and methods
Subjects
A retrospective study was conducted on a cohort of 451 elderly patients diagnosed with CAP who were admitted to the emergency department (including the emergency rescue room, emergency observation room, and emergency intensive care unit) of Beijing Chao-yang Hospital, Capital Medical University from 2021 to 2024. The study received approval from the Human Research Ethics Committee of Beijing Chao-yang Hospital, Capital Medical University.
Diagnostic criteria
The diagnosis of CAP was based on the identification of new infiltrative shadows on chest radiographs in conjunction with at least one of the following symptoms: (1) cough; (2) expectoration; (3) dyspnea; (4) body temperature >38.0°C (5) abnormal breath sounds or rales upon auscultation (Niederman et al., 2001).
Inclusion and Exclusion Criteria:
In this study, the inclusion criteria included: (1) patients aged ≥65 years; (2) patients who met the diagnostic criteria of CAP. The exclusion criteria included: (1) patients with advanced disease, including malignant tumors (advanced or metastatic tumors) and end-stage liver disease or kidney disease; (2) patients who were hospitalized within 14 days before the occurrence of symptoms; (3) patients with cystic fibrosis, active pulmonary tuberculosis, and severe immunosuppression; (4) patients who required vasopressors and mechanical ventilation at the time of admission.
Grouping
In this study, the results were evaluated via a 28-day follow-up study. Vasopressor administration, (non-invasive/invasive) mechanical ventilation requirement, and 28-day mortality were selected as endpoint events. A total of 451 elderly patients with CAP (including 268 males and 183 females) were included in this study. Based on the occurrence of endpoint events, 99 patients were classified into the death group, while 352 patients were allocated to the survival group. Furthermore, 110 patients were categorized into the mechanical ventilation group, with 341 patients belonging to the non-mechanical ventilation group. Additionally, 124 patients were segmented into the vasopressor administration group, and 327 patients were included in the non-vasopressor administration group.
Data collection
The demographic characteristics, including age and gender, as well as vital signs and medical history, were systematically documented for all participants. Blood samples, totaling 5-10 mL, were obtained within 6 hours of patient admission and promptly placed in heparin-containing tubes. Subsequent analyses included white blood count (WBC), blood gas assessment, and blood biochemistry tests, all conducted within 24 hours of blood collection. The severity of illness was quantified using the SOFA and CURB-65 scores, derived from clinical indicators and laboratory parameters.
Laboratory tests
The automated hematology detection analyzer (Sysmex XS-500i, Sysmex Corporation Kobe, Japan) was used to perform the WBC analysis. Plasma lactate (Lac) levels were assessed using a blood gas analyzer (GEM Premier 3000, Instrumentation Laboratory, Lexington, MA, USA), with the normal range established as 0.7-2.5 mmol/L. The serum procalcitonin (PCT) concentration was measured using the Mini-VIDAS immunoanalyzer of BioMerieux (Block Scientific, Bohemia), with the limit of detection (LOD) being 0.05ng/L. The serum C-reactive protein (CRP) concentration was determined by immunoturbidimetry (BNII, Siemens Healthcare Diagnostics Inc., Germany), with the normal range being 0-10ng/mL. The serum ferritin concentration was tested by chemiluminescence immunoassay (Beckman Coulter DXI800, USA), with the normal range defined as 11-306.8ng/mL.
Statistical analysis
The statistical analysis was performed with the aid of SPSS 16.0 (SPSS Inc., Chicago, IL, USA). The normally distributed data were expressed as mean ± standard deviation (SD), and the non-normally distributed data were expressed as median (P25, P75). The Mann-Whitney U test was deployed for between-group comparisons, and the Kruskal-Wallis univariate analysis was employed for comparisons involving multiple groups. The WBC, Lac, PCT, CRP, ferritin, SOFA scores, and CURB-65 scores were analyzed in the analysis of vasopressor administration, mechanical ventilation requirement, and 28-day mortality. Additionally, the ROC curve was plotted, and the AUC, sensitivity, and specificity were calculated. Compared with AUC, the Z value was calculated as per Z=(A1-A2)/(SE12+SE22) 1/2 (Z0.05 = 1.96, Z0.01 = 2.58). The binary logistic regression analysis was conducted to identify the independent predictors of vasopressor administration, mechanical ventilation requirement, and 28-day mortality. All statistical analyses were performed based on two-tailed tests. P<0.05 was considered statistically significant.
Results
Baseline data of patients with CAP
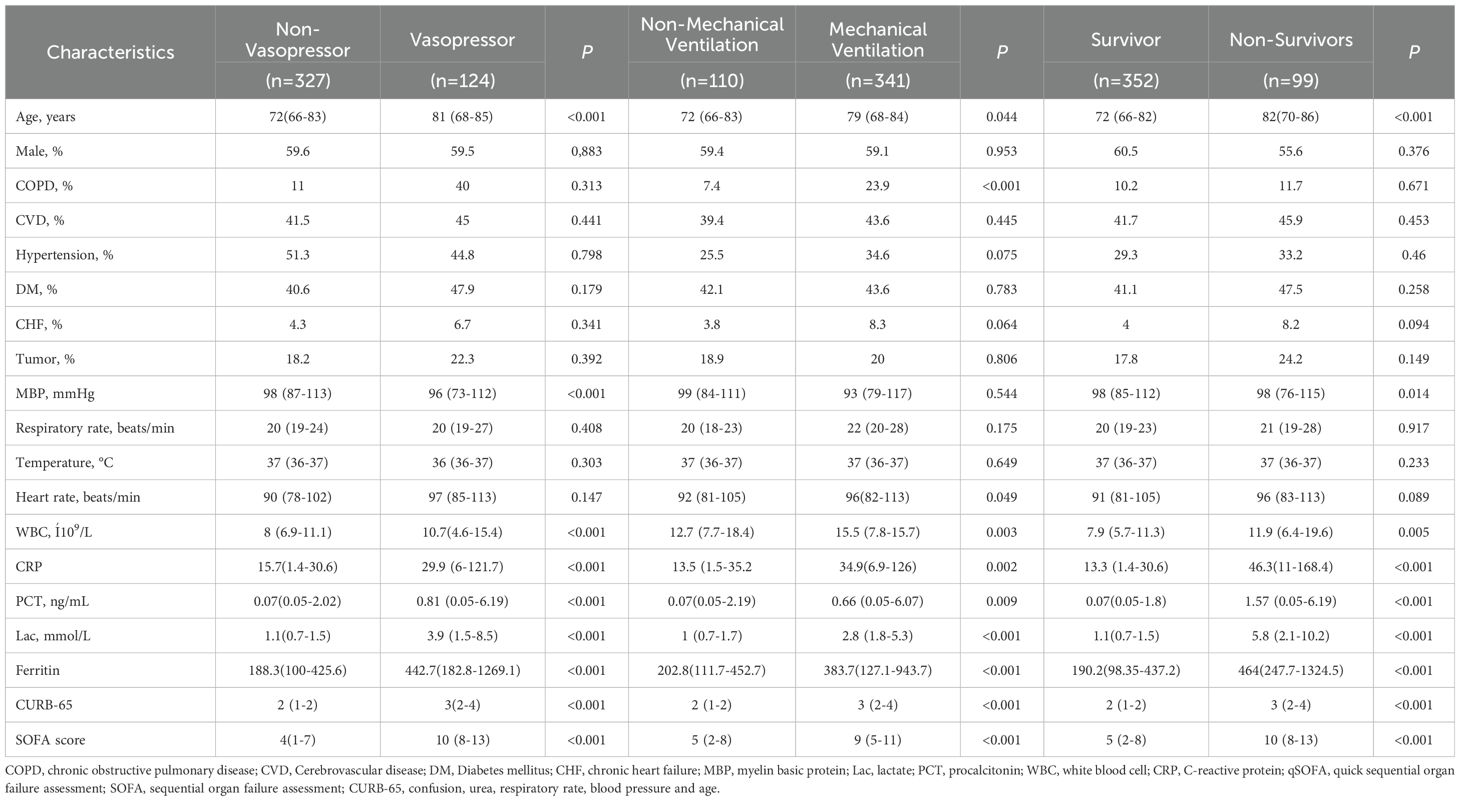
A total of 547 elderly patients with CAP met the inclusion criteria and provided written informed consent upon admission to the emergency department. According to the medical records, 59 patients refused mechanical ventilation, 3 patients refused vasopressor administration (coinciding with mechanical ventilation), and 37 patients were lost to follow-up after being transferred to other hospitals. Eventually, 451 patients completed the 28-day follow-up study. The baseline data of these CAP patients are listed in Table 1.
The 451 elderly patients with CAP were divided into the vasopressor administration group (N=124) and the non-vasopressor administration group (N=327) according to the based on their vasopressor administration in the 28-day follow-up study. The statistical analysis results indicated that there were significant differences in the age (P<0.001), mean arterial pressure (MBP) (P=<0.001), WBC, CRP, PCT, Lac, ferritin (P<0.001), SOFA scores, and CURB65 scores (P<0.001) of patients between the two groups (Table 1). These findings indicate that older age, elevated biomarkers (e.g., ferritin, CRP, and PCT), and higher SOFA and CURB-65 scores are strongly associated with vasopressor requirements, reflecting greater disease severity.
Besides, these patients were divided into the mechanical ventilation group (N=110) and the non-mechanical ventilation group (N=341) according to the application of ventilators in the 28-day follow-up study. The statistical analysis results suggested that there were significant differences in the age (P=0.044), chronic obstructive pulmonary disease (COPD) (P<0.001), heart rate (HR) (P=0.049), WBC (P=0.003), CRP (P=0.002), PCT (P=0.009), Lac, ferritin (P<0.001), SOFA scores, and CURB65 scores (P<0.001) of patients between the two groups (Table 1). This indicates that factors such as pre-existing COPD, systemic inflammation (elevated ferritin, CRP, and PCT levels), and higher SOFA/CURB-65 scores are predictive of mechanical ventilation requirements, emphasizing the importance of these indicators in clinical decision-making.
Moreover, these patients were also divided into the death group (N=352) and the survival group (N=99) according to their survival in the 28-day follow-up study. The statistical analysis results indicated that there were significant differences in the age (P<0.001), WBC (P=0.005), MBP (P=0.014), CRP, PCT, Lac, ferritin (P<0.001), SOFA scores, and CURB65 scores (P<0.001) of patients between the two groups (Table 1). These findings highlight that advanced age, elevated inflammatory markers (e.g., ferritin, CRP, PCT), and higher severity scores (SOFA and CURB-65) are closely linked to poor prognosis, including higher 28-day mortality rates.
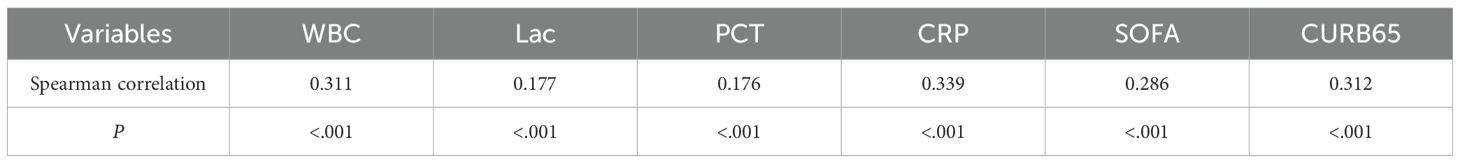
Correlation of serum ferritin and other indicators
To investigate the relationship between serum ferritin levels and various clinical markers including WBC, CRP, PCT, Lac, SOFA scores, and CURB65 scores, the Spearman correlation analysis was performed (Table 2). The analysis revealed significant correlations between serum ferritin and WBC (r=0.311, P<0.001), CRP (r=0.339, P<0.001), PCT (r=0.176, P<0.001), Lac (r=0.177, P<0.001), SOFA scores (r=0.286, P<0.001), and CURB65 scores (r=0.312, P<0.001 (Table 2). These results indicate that ferritin levels are significantly associated with markers of inflammation and disease severity, reinforcing its potential as an integrative marker for assessing the overall health status of elderly CAP patients.
Logistic regression analysis of each variable for the prognosis of patients with CAP
In this study, the independent predictors were analyzed using multivariate logistic regression, as shown in Table 3. The results indicated that serum ferritin (P=0.003, OR=1.001, 95%CI: 1.001-1.002), WBC (P=0.035, OR=1.049, 95%CI: 1.003-1.079), Lac (P<0.019, OR=1.027, 95%CI: 1.004-1.049), SOFA scores (P<0.001, OR=1.23, 95%CI: 1.145-1.321), and CURB65 scores (P<0.001, OR=2.686, 95%CI: 1.905-3.788) were independent risk factors for the 28-day mortality in elderly patients with CAP (Table 3A). Besides, serum ferritin (P=0.034, OR=1.001, 95%CI: 1-1.001), WBC (P=0.043, OR=1.048, 95%CI: 1.001-1.096), PCT (P=0.032, OR=1.062, 95%CI: 1.005-1.122), Lac (P=0.026, OR=1.026, 95%CI: 1.003-1.049), SOFA scores (P<0.001, OR=1.35, 95%CI: 1.25-1.458), and CURB65 scores (P<0.001, OR=2.682, 95%CI: 1.912-3.762) were independent risk factors for the vasopressor administration in elderly patients with CAP (Table 3B). Additionally, SOFA scores (P=0.006, OR=1.081, 95%CI: 1.023-1.143) and CURB65 scores (P<0.001, OR=1.626, 95%CI: 1.241-2.131) were independent risk factors for the mechanical ventilation requirement in elderly patients with CAP (Table 3C).
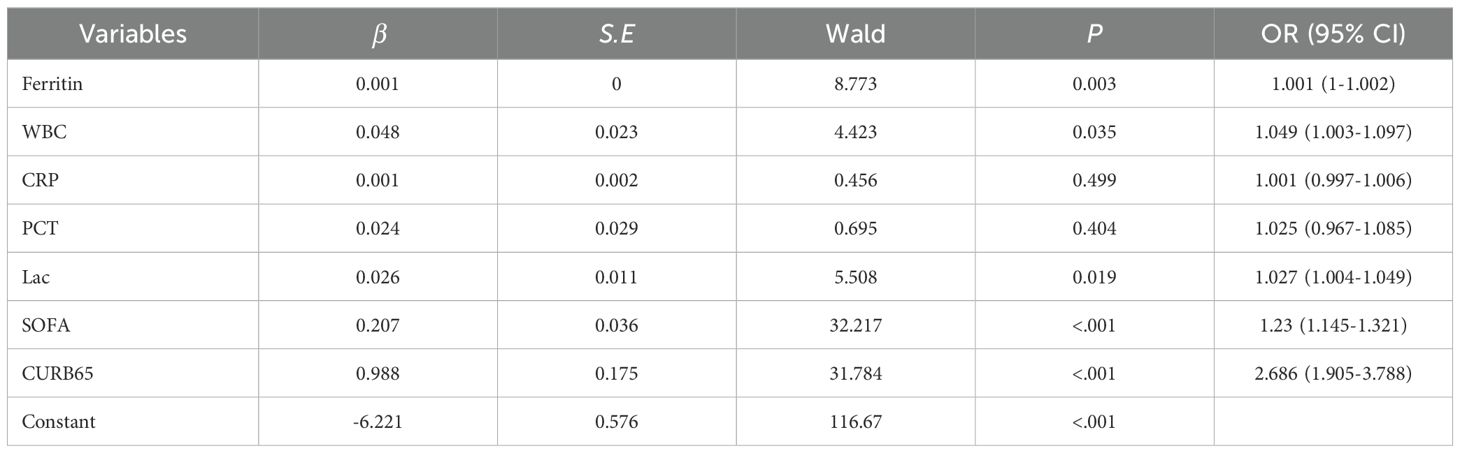
Table 3A. Binary logistic regression analysis of 28-day mortality in elderly patients with community-acquired pneumonia (CAP).
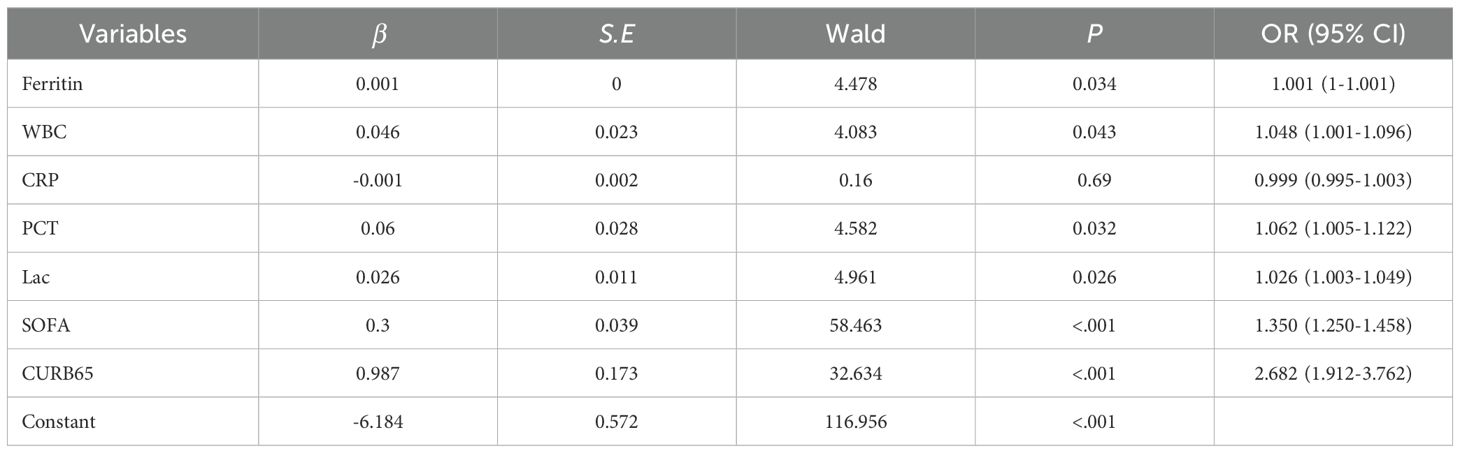
Table 3B. Binary logistic regression analysis of vasopressor use in elderly patients with community-acquired pneumonia (CAP).

Table 3C. Binary logistic regression analysis of mechanical ventilation use in elderly patients with community-acquired pneumonia (CAP).
Prediction of the prognosis of elderly patients with CAP
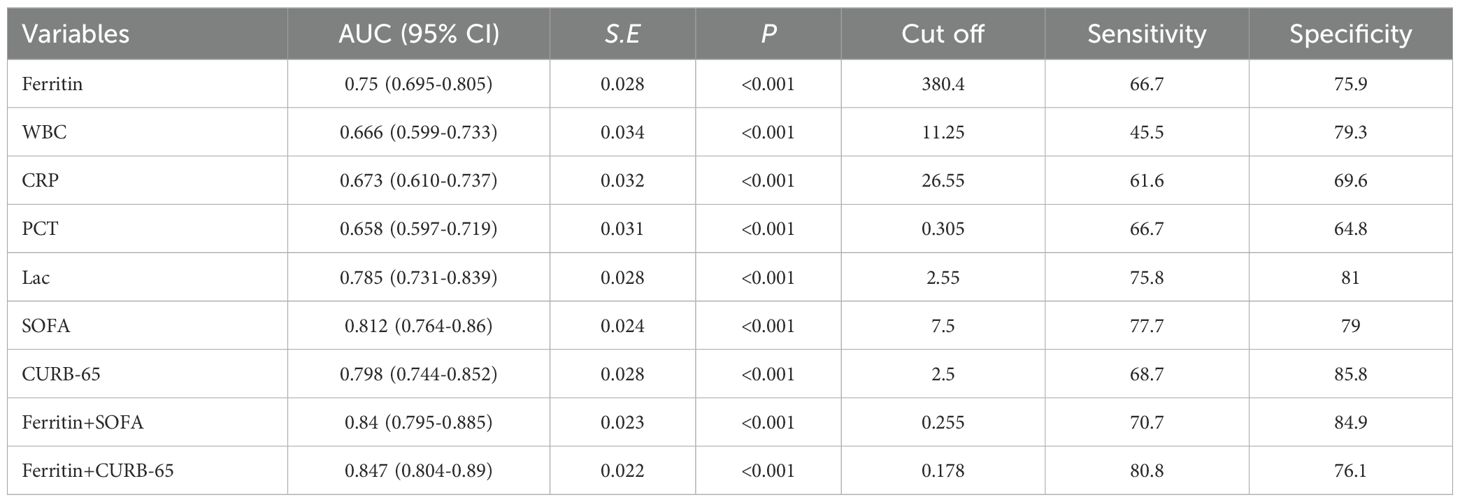
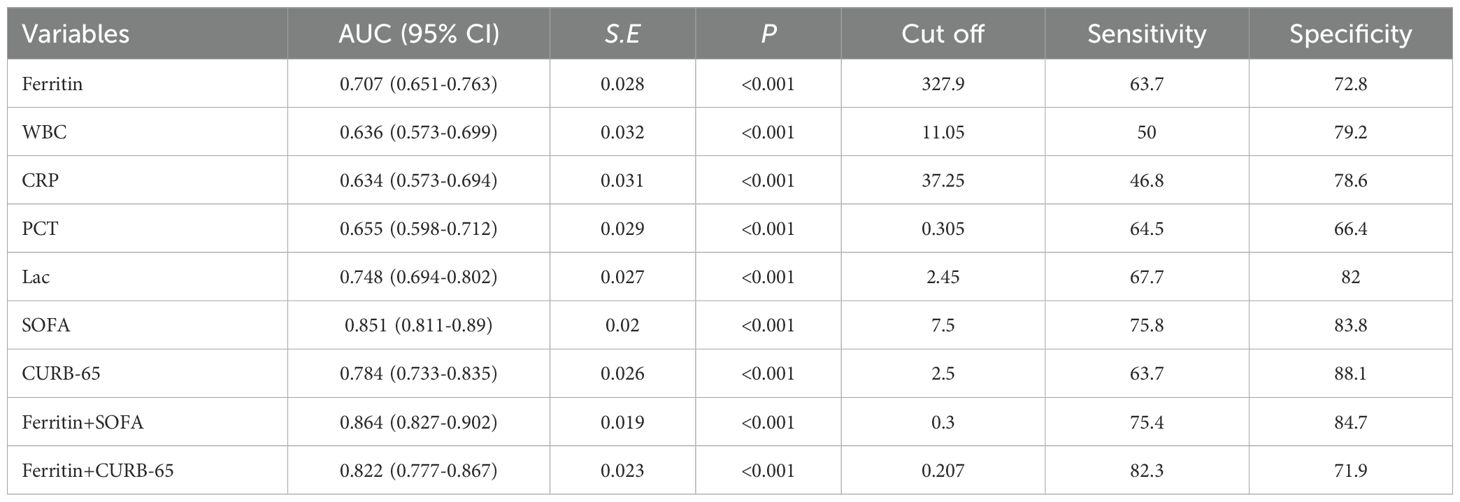
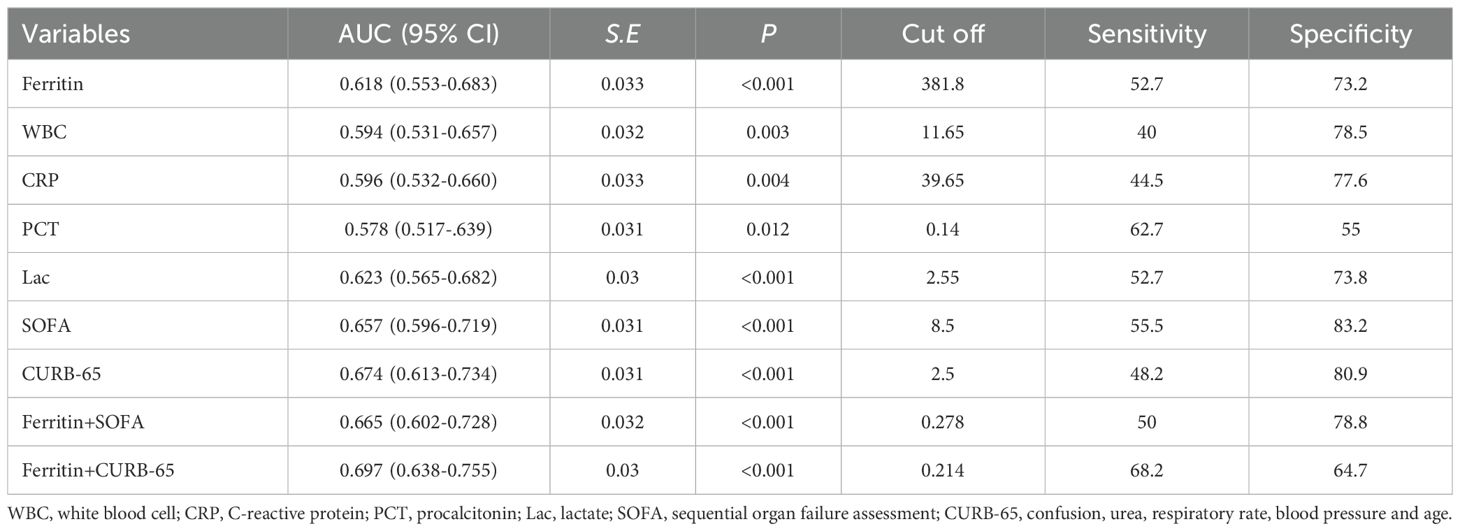
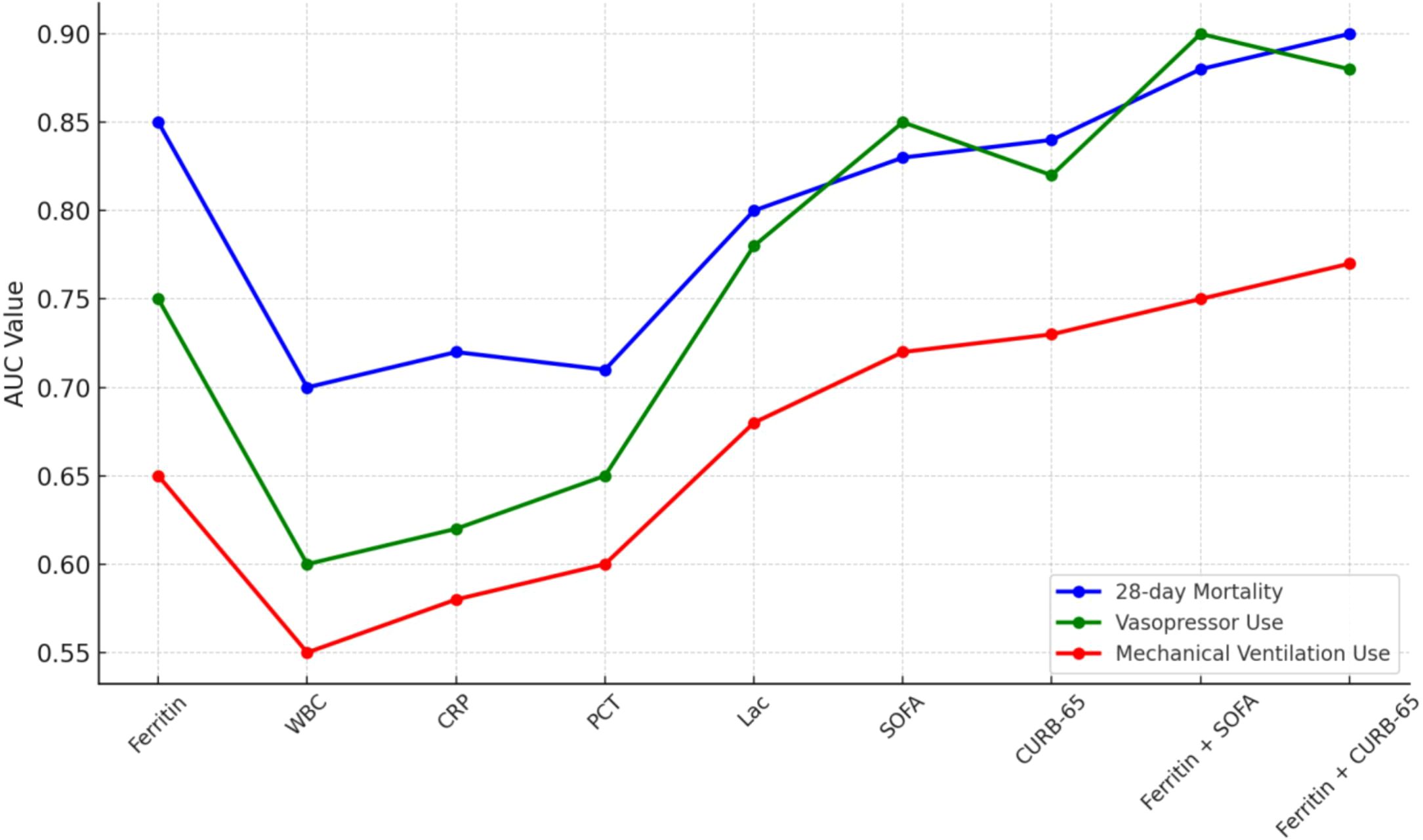
The findings pertaining to the serum ferritin levels and other associated variables, as well as their amalgamations, in the context of forecasting the 28-day mortality, administration of vasopressors, and mechanical ventilation requirement among elderly patients with CAP are presented in Table 4 and illustrated in Figure 1.
The AUC of serum ferritin, WBC, CRP, PCT, Lac, SOFA scores, and CURB-65 scores for predicting the 28-day mortality in elderly patients with CAP was 0.75 (95%CI: 0.695-0.805, P<0.001), 0.666 (95%CI: 0.599-0.733, P<0.001), 0.673 (95%CI: 0.610-0.737, P<0.001), 0.658 (95%CI: 0.597-0.719, P<0.001), 0.785 (95%CI: 0.731-0.839, P<0.001), 0.812 (95%CI: 0.764-0.86, P<0.001), and 0.798 (95%CI: 0.744-0.852, P<0.001),respectively. The AUC of ferritin+SOFA and ferritin+CURB65 for predicting the 28-day mortality in elderly patients with CAP was 0.84 (95%CI: 0.795-0.855, P<0.001) and 0.847 (95%CI: 0.804-0.89, P<0.001), respectively. These results indicate that serum ferritin has predictive power for 28-day mortality, combining ferritin with SOFA and CURB-65 scores significantly enhanced the AUC to 0.84 (95%CI: 0.795-0.855, P<0.001) and 0.847 (95%CI: 0.804-0.89, P<0.001), respectively, suggesting that ferritin can improve the prognostic accuracy of these established scoring systems (Table 4A).
The AUC of serum ferritin, WBC, CRP, PCT, Lac, SOFA scores, and CURB-65 scores for predicting vasopressor administration in elderly patients with CAP was 0.707 (95%CI: 0.651-0.763, P<0.001), 0.636 (95%CI: 0.573-0.669, P<0.001), 0.634 (95%CI: 0.573-0.694, P<0.001), 0.655 (95%CI: 0.598-0.712, P<0.001), 0.748 (95%CI: 0.694-0.802, P<0.001), 0.851 (95%CI: 0.811-0.89, P<0.001), and 0.784 (95%CI: 0.733-0.845, P<0.001), respectively. The AUC of ferritin+SOFA and ferritin+CURB65 for predicting the vasopressor administration in elderly patients with CAP was 0.864 (95%CI: 0.827-0.902, P<0.001) and 0.822 (95%CI: 0.777-0.867, P<0.001), respectively. These findings highlight that serum ferritin provides good predictive accuracy for vasopressor use, comparable to Lac and superior to traditional markers like WBC and CRP. Combining ferritin with SOFA (AUC=0.864, 95%CI: 0.827-0.902, P<0.001) or CURB-65 (AUC=0.822, 95%CI: 0.777-0.867, P<0.001) further improves its predictive performance, underscoring the utility of ferritin in guiding critical care interventions (Table 4B).
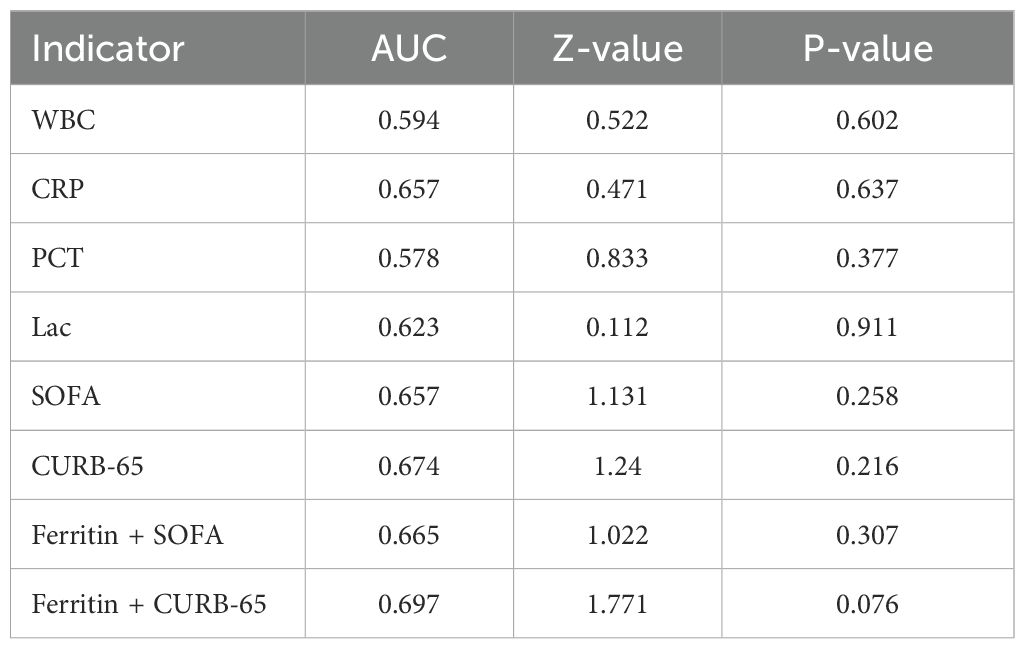
The AUC of serum ferritin, WBC, CRP, PCT, Lac, SOFA scores, and CURB-65 scores for predicting the mechanical ventilation requirement in elderly patients with CAP was 0.618 (95%CI: 0.532-0.66, P<0.001), 0.594 (95%CI: 0.531-0.657, P=0.003), 0.596 (95%CI: 0.573-0.694, P=0.004), 0.578 (95%CI: 0.517-0.639, P=0.012), 0.623 (95%CI: 0.565-0.682, P<0.001), 0.657 (95%CI: 0.596-0.719, P<0.001), and 0.674 (95%CI: 0.617-0.734, P<0.001), respectively. The AUC of ferritin+SOFA and ferritin+CURB65 for predicting the mechanical ventilation requirement in elderly patients with CAP was 0.665 (95%CI: 0.602-0.728, P<0.001) and 0.697 (95%CI: 0.638-0.755, P<0.001), respectively. While ferritin exhibited limited predictive performance for mechanical ventilation (AUC=0.618), Combining ferritin with SOFA (AUC=0.665, 95%CI: 0.602-0.728, P<0.001) or CURB-65 (AUC=0.697, 95%CI: 0.638-0.755, P<0.001) provided modest improvements (Table 4C).
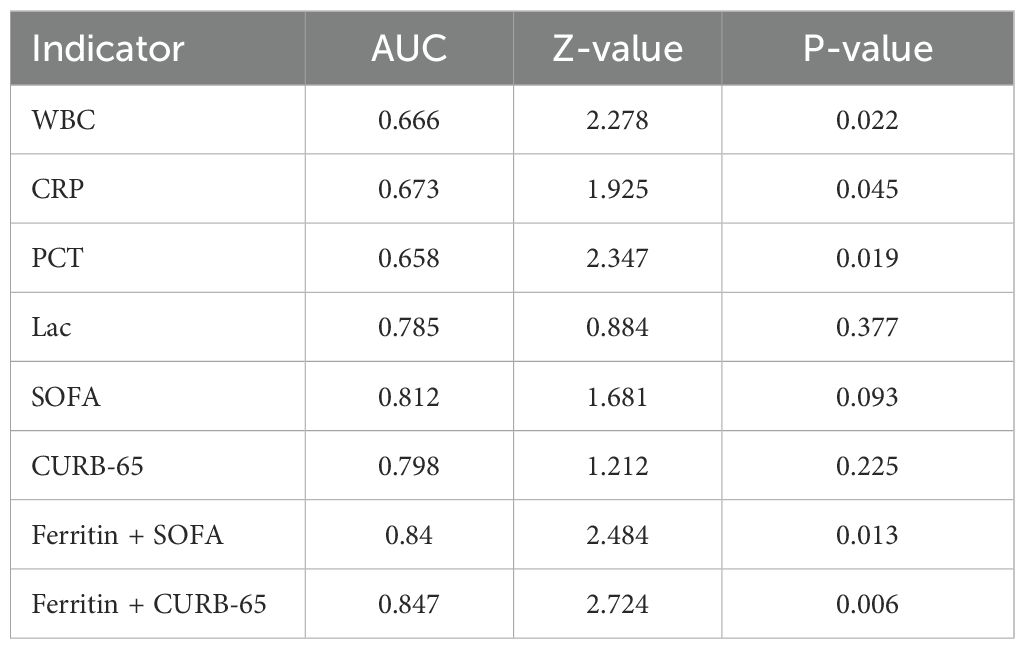
Comparison of serum ferritin and other indicators in predicting the prognosis of elderly patients with CAP
The ability of serum ferritin and other indicators to predict the prognosis of elderly patients with CAP was compared based on their AUC values (Table 5; Figure 2). The results indicated that serum ferritin was superior to WBC (Z=2.278, P=0.022), CRP (Z=1.925, P=0.045), and PCT (Z=2.347, P=0.019) in predicting the 28-day mortality of these elderly patients with CAP. This finding highlights ferritin’s stronger prognostic value compared to traditional inflammatory markers, emphasizing its potential as a primary biomarker for mortality prediction. However, no statistically significant differences were found between serum ferritin and Lactate (Z=0.884, P=0.377), SOFA (Z=1.681, P=0.093), and CURB-65 (Z=1.212, P=0.225), indicating that ferritin performs comparably to these well-established severity scores in predicting 28-day mortality. Furthermore, both ferritin+SOFA and ferritin+CURB-65 exhibited superior predictive power for 28-day mortality compared to serum ferritin alone (Z=2.484, P=0.013; Z=2.724, P=0.006), suggesting that combining ferritin with severity scores significantly enhances prognostic accuracy (Table 5A).
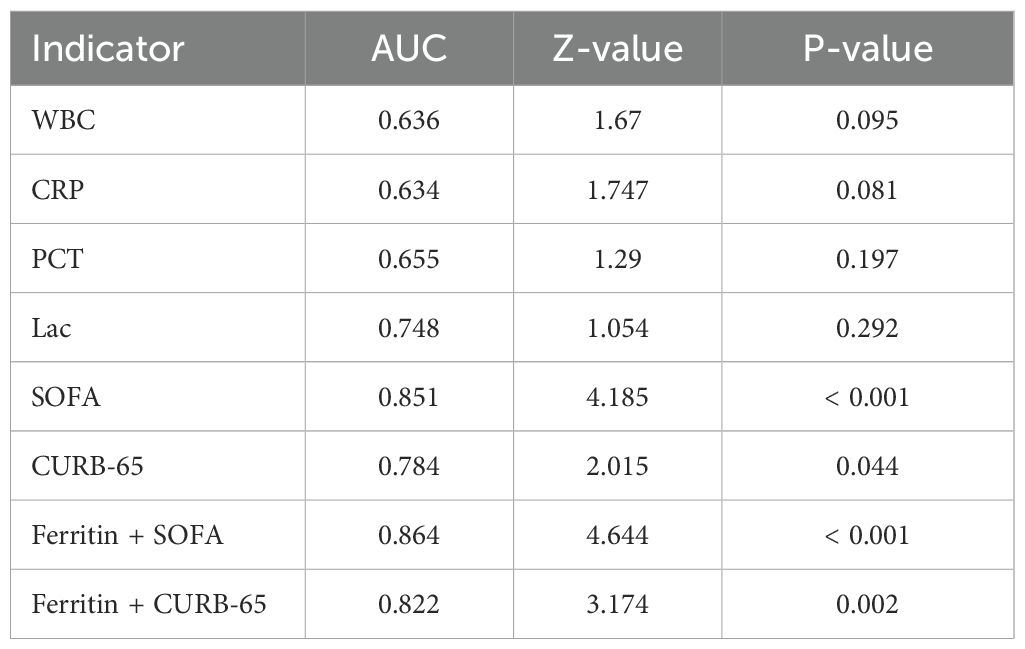
For vasopressor administration, serum ferritin demonstrated comparable predictive performance to WBC (Z=1.67, P=0.095), CRP (Z=1.747, P=0.081), and PCT (Z=1.29, P=0.197), indicating that ferritin performs similarly to traditional markers for this outcome. However, Lac (Z=1.054, P=0.292), SOFA (Z=4.185, P<0.001), CURB-65 (Z=2.015, P=0.044), ferritin+SOFA (Z=4.644, P<0.001), and ferritin+CURB-65 (Z=3.174, P=0.002) exhibited superior predictive accuracy compared to serum ferritin alone. These results suggest that combining ferritin with SOFA or CURB-65 scores enhances its ability to guide clinical decisions regarding vasopressor use (Table 5B).
For predicting mechanical ventilation requirements, serum ferritin did not significantly differ from other biomarkers, including WBC (Z=0.522, P=0.602), CRP (Z=0.471, P=0.637), PCT (Z=0.833, P=0.377), Lac (Z=0.112, P=0.911), SOFA (Z=1.131, P=0.258), CURB-65 (Z=1.24, P=0.216), ferritin+SOFA (Z=1.022, P=0.307), and ferritin+CURB-65 (Z=1.771, P=0.076). This indicates that ferritin has limited predictive value for mechanical ventilation, and its performance is comparable to traditional inflammatory markers (Table 5C).
Discussion
In this study, the prognostic value of serum ferritin in elderly patients with community-acquired pneumonia (CAP) was comprehensively analyzed. The findings demonstrated that serum ferritin is an independent predictor for 28-day mortality, the need for vasopressor administration, and mechanical ventilation in this patient population. Furthermore, combining serum ferritin with established clinical scoring systems, such as CURB-65 and SOFA, significantly enhanced the ability to predict these outcomes, underscoring its utility in guiding risk stratification and optimizing clinical management for elderly CAP patients.
Ferritin has demonstrated superior predictive performance for 28-day mortality in elderly CAP patients compared to other inflammatory markers such as CRP and PCT. Specifically, ferritin exhibited statistically significant differences in AUC values for predicting 28-day mortality compared to CRP (Z=1.925, P=0.045) and PCT (Z=2.347, P=0.019). CRP and PCT are among the most commonly used biomarkers in clinical practice for CAP and are well-recognized prognostic indicators for the disease (Self et al., 2017; Liu et al., 2023). Both markers are independent predictors of CAP outcomes (Khan et al., 2017; Self et al., 2016; Hussain et al., 2022), with elevated levels closely associated with the host’s inflammatory response to infection mm. In bacterial pneumonia, daily monitoring of PCT levels is an effective and safe tool for guiding antibiotic duration and cessation (Branche et al., 2019) (Schuetz et al., 2017). However, as nonspecific acute-phase reactants, CRP and PCT levels may also rise in sterile inflammatory conditions such as pancreatitis, major surgery, or cardiopulmonary resuscitation, limiting their specificity (Carbonell et al., 2023). The superior prognostic capability of ferritin compared to CRP and PCT underscores its value as a more reliable biomarker in predicting CAP outcomes. Notably, ferritin’s predictive performance was comparable to established scoring systems, such as SOFA and CURB-65 scores, in predicting 28-day mortality (P>0.05). This suggests that ferritin, as an independent prognostic marker, has predictive potency comparable to established scoring systems.
The combination of ferritin with CURB-65 or SOFA scores also showed superior performance in predicting the vasopressor administration in these patients. The AUC of ferritin for predicting the vasopressor administration in these patients was 0.707, but in conjunction with CURB-65 or SOFA scores, the AUC rose significantly to 0.822 (P<0.001) and 0.864 (P<0.001), respectively. These results further supported that ferritin was an effective prognostic biomarker. In particular, the application of ferritin in combination with clinical scoring systems can significantly improve the prediction accuracy.
The predictive performance of ferritin for mechanical ventilation was less pronounced, with an AUC of 0.618. However, when combined with CURB-65 scores, the AUC improved to 0.697. This lower predictive efficacy for mechanical ventilation may reflect the complexity of patient decision-making in elderly CAP cases, where personal preferences or family choices often play a role in accepting or declining invasive treatments. Such factors may limit the clinical utility of ferritin in forecasting the need for mechanical ventilation.
Ferritin, as the main iron storage protein in the human body, plays a fundamental role in regulating iron metabolism and immune responses. It consists of 24 subunits and can store up to 4,500 iron ions, ensuring iron homeostasis through storage and release mechanisms (Yanatori et al., 2023). In normal physiological conditions, ferritin levels accurately reflect the body’s iron reserves. However, during pathological states such as infection, ferritin functions as an acute-phase reactant protein, limiting pathogen access to iron—an essential nutrient for microbial growth—through a process termed “nutritional immunity” (Marchetti et al., 2020; Gerner et al., 2020). This iron regulation is complemented by transferrin, which transports free iron in the bloodstream, maintaining systemic iron balance and supporting immune defense
In addition, ferritin helps mitigate oxidative stress by regulating free iron availability. Free ferrous iron (Fe²+) can generate reactive oxygen species (ROS) through the Fenton reaction, leading to cellular damage (Nakamura et al., 2019; Gensluckner et al., 2024). The H subunit of ferritin exhibits ferric oxidase activity, converting Fe²+ to ferric iron (Fe³+), which is safely stored within the protein structure. This mechanism protects host cells from oxidative damage while maintaining antibacterial defenses (Pham et al., 2004). Escalated ferritin levels during infection are indicative of perturbed iron metabolism and an activated inflammatory response, both of which are hallmarks of severe CAP (Fonseca et al., 2023; Moreira et al., 2020).
Research has consistently supported the predictive value of serum ferritin in predicting all-cause mortality, particularly in critically ill patients and those with sepsis (Fang et al., 2022; Nandy et al., 2021; Lungu et al., 2024). Moreover, serum ferritin levels have been found to be closely linked to adverse outcomes in various conditions, including tumors, connective tissue diseases, and COVID-19 (Kirino et al., 2018; Plano et al., 2023; Wang et al., 2023; Perottet et al., 2022; Giemza-Stokłosa et al., 2019). Despite this, there is a scarcity of clinical studies on the predictive capacity of ferritin for CAP in elderly individuals. Mehta P reported that a ferritin concentration exceeding 1380 ng/mL indicated a poor prognosis in adults with acute respiratory distress syndrome (ARDS). Among 847 ARDS patients who received ventilator-assisted ventilation, 204 (24.1%) patients had a ferritin concentration of >1380 ng/mL and a mortality rate of 60%; the remaining patients had a ferritin concentration of <1380 ng/mL and a mortality rate of 35%. In addition, patients with a high ferritin concentration were found to have a significantly lower probability of weaning from mechanical ventilation than those with a low ferritin concentration (Mehta et al., 2024). In a study conducted by Goldhaber G, the association between ferritinemia (the serum ferritin concentration >1000 ug/L) and mortality among elderly inpatients was examined. The findings revealed a median survival time of merely 4.7 months for the 242 patients under scrutiny, with nearly 70% succumbing within a two-year period. Notably, the risk of mortality rose by 1.5% for each 100-unit elevation of serum ferritin concentration (Goldhaber et al., 2020). As reported in some studies, the serum ferritin concentration is significantly related to the survival rate of patients with acute exacerbation of idiopathic pulmonary fibrosis. Patients with a higher ferritin concentration usually have a lower survival rate. In particular, when the ferritin concentration is higher than 500 ng/mL, the risk of death increases significantly (Enomoto et al., 2018). The current study complements these findings by establishing practical thresholds specific to elderly CAP patients: ferritin levels exceeding 380.35 ng/mL for 28-day mortality, 327.85 ng/mL for vasopressor administration, and 381.75 ng/mL for mechanical ventilation. These thresholds provide clinicians with actionable benchmarks for early intervention. Furthermore, ferritin was an independent risk factor for the 28-day mortality and vasopressor administration, and there was no significant difference in the predictive ability for the 28-day mortality between ferritin and Lac in these elderly patients with CAP. Lac is a well-established predictor of both sepsis and CAP (Gattinoni et al., 2019; Huang et al., 2023; Frenzen et al., 2018), serving as an independent prognostic factor. Similarly, both ferritin and lactate have been identified as independent predictors, demonstrating comparable predictive performance for 28-day mortality and vasopressor use. The similar predictive ability of ferritin highlights its potential as a useful adjunct or alternative biomarker, particularly in clinical settings where lactate measurement may be less feasible.
In a neonatal study, it was observed that an increased ferritin concentration exceeding 248.5 ng/mL correlated significantly with a heightened risk of sepsis in newborns (Lungu et al., 2024). Furthermore, multiple studies have demonstrated a noteworthy rise in mortality rates for patients with sepsis and COVID-19 when their ferritin concentrations ranged from 135 ng/mL to 821.5 ng/mL (Fang et al., 2022; Tonial et al., 2021; Cihakova et al., 2021; Liu and Liu, 2023). The variation in the specified cutoff value could likely stem from differences in subjects’ ages and experimental methodologies. This investigation’s findings emphasize the clinical importance of considering ferritin thresholds alongside patient-specific factors to achieve more precise prognostication and targeted care.
The present study highlights the importance of incorporating ferritin into established scoring systems, such as SOFA and CURB-65, to enhance predictive accuracy for CAP outcomes. The integration of ferritin-based thresholds enables clinicians to refine risk stratification models, allowing for more precise prognostic assessments and tailored treatment strategies. In resource-limited settings, ferritin’s affordability and accessibility make it a particularly valuable tool for guiding decisions in emergency and critical care scenarios.
Nevertheless, there are still some limitations in this study. Firstly, the cut-off values proposed in the continuous retrospective single-center study need validation in an independent and multicenter study cohort. Secondly, dynamic monitoring of ferritin was not conducted, and such data could have informed treatment decisions. Thirdly, the retrospective clinical study was unable to sufficiently identify cases where mechanical ventilation was indicated but refused by patients or their families, potentially affecting the accuracy of predicting the need for mechanical ventilation in elderly patients with CAP. Finally, the 2007 IDSA/ATS CAP guidelines recommended by the American Thoracic Society and Infectious Diseases Society of America[3] were not included in the analysis due to missing data. This scoring system has been shown to provide a more accurate assessment of high-risk status in CAP. Future research should address these gaps by employing prospective, multicenter designs and incorporating real-time monitoring of ferritin levels to validate its dynamic role in predicting CAP outcomes
Conclusion
Admission serum ferritin is an independent predictor for the prognosis of elderly patients with CAP, and it exhibits a strong ability to predict the 28-day mortality and vasopressor administration in these patients. The combination of serum ferritin and SOFA or CURB-65 scores can significantly improve the predictive potency. Based on the results of this study, it is recommended that serum ferritin should be used as an important biomarker for risk assessment in elderly patients with CAP, thus better identifying high-risk patients and formulating personalized treatment protocols.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Human Research Ethics Committee of Beijing Chao-yang Hospital, Capital Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The human samples used in this study were acquired from a by- product of routine care or industry. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
XZ: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. NS: Data curation, Writing – original draft. DZ: Data curation, Writing – original draft. JW: Supervision, Writing – review & editing. SG: Funding acquisition, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. Supported by National Key R&D Program of China (grant number: 2023YFC0872400)
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Branche, A., Neeser, O., Mueller, B., Schuetz, P. (2019). Procalcitonin to guide antibiotic decision making. Curr. Opin. Infect. Dis. 32, 130–135. doi: 10.1097/QCO.0000000000000522
Brown, J. D., Harnett, J., Chambers, R., Sato, R. (2018). The relative burden of community-acquired pneumonia hospitalizations in older adults: a retrospective observational study in the United States. BMC Geriatr. 18, 92. doi: 10.1186/s12877-018-0787-2
Carbonell, R., Moreno, G., Martín-Loeches, I., Bodí, M., Rodríguez, A. (2023). The role of biomarkers in influenza and COVID-19 community-acquired pneumonia in adults. Antibiotics (Basel) 12, 161. doi: 10.3390/antibiotics12010161
Cihakova, D., Streiff, M. B., Menez, S. P., Chen, T. K., Gilotra, N. A., Michos, E. D., et al. (2021). High-value laboratory testing for hospitalized COVID-19 patients: a review. Future Virol. 16 (10). doi: 10.2217/fvl-2020-0316
Cillóniz, C., Dominedò, C., Garcia-Vidal, C., Torres, A. (2018). Community-acquired pneumonia as an emergency condition. Curr. Opin. Crit. Care 24, 531–539. doi: 10.1097/MCC.0000000000000550
Enomoto, N., Oyama, Y., Enomoto, Y., Mikamo, M., Karayama, M., Hozumi, H., et al. (2018). Prognostic evaluation of serum ferritin in acute exacerbation of idiopathic pulmonary fibrosis. Clin. Respir. J. 12, 2378–2389. doi: 10.1111/crj.2018.12.issue-8
Fang, Y. P., Zhang, H. J., Guo, Z., Ren, C. H., Zhang, Y. F., Liu, Q., et al. (2022). Effect of serum ferritin on the prognosis of patients with sepsis: data from the MIMIC-IV database. Emerg. Med. Int. 2022, 2104755. doi: 10.1155/2022/2104755
Fonseca, Ó., Ramos, A. S., Gomes, L. T. S., Gomes, M. S., Moreira, A. C. (2023). New perspectives on circulating ferritin: its role in health and disease. Molecules 28, 7707. doi: 10.3390/molecules28237707
Frenzen, F. S., Kutschan, U., Meiswinkel, N., Schulte-Hubbert, B., Ewig, S., Kolditz, M. (2018). Admission lactate predicts poor prognosis independently of the CRB/CURB-65 scores in community-acquired pneumonia. Clin. Microbiol. Infect. 24, 306.e1–306.e6. doi: 10.1016/j.cmi.2017.07.007
Gattinoni, L., Vasques, F., Camporota, L., Meessen, J., Romitti, F., Pasticci, I., et al. (2019). Understanding lactatemia in human sepsis. Potential impact for early management. Am. J. Respir. Crit. Care Med. 200, 582–589. doi: 10.1164/rccm.201812-2342OC
Gensluckner, S., Wernly, B., Datz, C., Aigner, E. (2024). Iron, oxidative stress, and metabolic dysfunction-associated steatotic liver disease. Antioxidants (Basel) 13, 208. doi: 10.3390/antiox13020208
Gerner, R. R., Nuccio, S. P., Raffatellu, M. (2020). Iron at the host-microbe interface. Mol. Aspects Med. 75, 100895. doi: 10.1016/j.mam.2020.100895
Giemza-Stokłosa, J., Islam, M. A., Kotyla, P. J. (2019). Hyperferritinaemia: an iron sword of autoimmunity. Curr. Pharm. Des. 25, 2909–2918. doi: 10.2174/1381612825666190709202804
Goldhaber, G., Segal, G., Dagan, A. (2020). Hyperferritinemia in the elderly can differentiate the bad from the worst: A retrospective cohort analysis. Med. (Baltimore) 99, e21419. doi: 10.1097/MD.0000000000021419
Horvat, C. M., Fabio, A., Nagin, D. S., Banks, R. K., Qin, Y., Park, H. J., et al. (2022). Mortality risk in pediatric sepsis based on C-reactive protein and ferritin levels. Pediatr. Crit. Care Med. 23, 968–979. doi: 10.1097/PCC.0000000000003074
Huang, D., He, D., Yao, R., Wang, W., He, Q., Wu, Z., et al. (2023). Association of admission lactate with mortality in adult patients with severe community-acquired pneumonia. Am. J. Emerg. Med. 65, 87–94. doi: 10.1016/j.ajem.2022.12.036
Hussain, A., Singh, L., Mcalister Iii, J., Jo, Y., Makaryan, T. T., Hussain, S., et al. (2022). Serum procalcitonin as a predictive biomarker in COVID-19: A retrospective cohort analysis. Cureus 14, e27816. doi: 10.7759/cureus.27816
Kernan, K. F., Carcillo, J. A. (2017). Hyperferritinemia and inflammation. Int. Immunol. 29, 401–409. doi: 10.1093/intimm/dxx031
Khan, F., Owens, M. B., Restrepo, M., Povoa, P., Martin-Loeches, I. (2017). Tools for outcome prediction in patients with community acquired pneumonia. Expert Rev. Clin. Pharmacol. 10, 201–211. doi: 10.1080/17512433.2017.1268051
Kirino, Y., Kawaguchi, Y., Tada, Y., Tsukamoto, H., Ota, T., Iwamoto, M., et al. (2018). Beneficial use of serum ferritin and heme oxygenase-1 as biomarkers in adult-onset Still’s disease: A multicenter retrospective study. Mod Rheumatol 28, 858–864. doi: 10.1080/14397595.2017.1422231
Liu, F., Liu, Z. (2023). Association between ferritin to albumin ratio and 28-day mortality in patients with sepsis: a retrospective cohort study. Eur. J. Med. Res. 28, 414. doi: 10.1186/s40001-023-01405-y
Liu, Q., Sun, G., Huang, L. (2023). Association of the NLR, BNP, PCT, CRP, and D-D with the severity of community-acquired pneumonia in older adults. Clin. Lab. 69. doi: 10.7754/Clin.Lab.2023.220330
Lungu, N., Popescu, D. E., Manea, A. M., Jura, A. M. C., Doandes, F. M., Popa, Z. L., et al. (2024). Hemoglobin, ferritin, and lactate dehydrogenase as predictive markers for neonatal sepsis. J. Pers. Med. 14, 476. doi: 10.3390/jpm14050476
Marchetti, M., De Bei, O., Bettati, S., Campanini, B., Kovachka, S., Gianquinto, E., et al. (2020). Iron metabolism at the interface between host and pathogen: from nutritional immunity to antibacterial development. Int. J. Mol. Sci. 21, 2145. doi: 10.3390/ijms21062145
Mehta, P., Samanta, R. J., Wick, K., Coll, R. C., Mawhinney, T., Mcaleavey, P. G., et al. (2024). Elevated ferritin, mediated by IL-18 is associated with systemic inflammation and mortality in acute respiratory distress syndrome (ARDS). Thorax 79, 227–235. doi: 10.1136/thorax-2023-220292
Metlay, J. P., Waterer, G. W., Long, A. C., Anzueto, A., Brozek, J., Crothers, K., et al. (2019). Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the american thoracic society and infectious diseases society of america. Am. J. Respir. Crit. Care Med. 200, e45–e67. doi: 10.1164/rccm.201908-1581ST
Moreira, A. C., Mesquita, G., Gomes, M. S. (2020). Ferritin: an inflammatory player keeping iron at the core of pathogen-host interactions. Microorganisms 8, 589. doi: 10.3390/microorganisms8040589
Nakamura, T., Naguro, I., Ichijo, H. (2019). Iron homeostasis and iron-regulated ROS in cell death, senescence and human diseases. Biochim. Biophys. Acta Gen. Subj 1863, 1398–1409. doi: 10.1016/j.bbagen.2019.06.010
Nandy, A., Mondal, T., Datta, D., Ray, S., Kumar, N., Ivan, M. D., et al. (2021). Serum ferritin as a diagnostic biomarker for severity of childhood sepsis. Indian Pediatr. 58, 1143–1146. doi: 10.1007/s13312-021-2396-y
Niederman, M. S., Mandell, L. A., Anzueto, A., Bass, J. B., Broughton, W. A., Campbell, G. D., et al. (2001). Guidelines for the management of adults with community-acquired pneumonia. Diagnosis, assessment of severity, antimicrobial therapy, and prevention. Am. J. Respir. Crit. Care Med. 163, 1730–1754. doi: 10.1164/ajrccm.163.7.at1010
Perottet, J., Gondolf, C., Grandhomme, F., Creveuil, C., Allouche, S. (2022). Ferritin as a predictive biomarker of severity in Covid-19. Ann. Biol. Clin. (Paris) 80, 363–368. doi: 10.1684/abc.2022.1725
Pham, C. G., Bubici, C., Zazzeroni, F., Papa, S., Jones, J., Alvarez, K., et al. (2004). Ferritin heavy chain upregulation by NF-kappaB inhibits TNFalpha-induced apoptosis by suppressing reactive oxygen species. Cell 119, 529–542. doi: 10.1016/j.cell.2004.10.017
Plano, F., Gigliotta, E., Corsale, A. M., Azgomi, M. S., Santonocito, C., Ingrascì, M., et al. (2023). Ferritin metabolism reflects multiple myeloma microenvironment and predicts patient outcome. Int. J. Mol. Sci. 24, 8852. doi: 10.3390/ijms24108852
Schuetz, P., Wirz, Y., Sager, R., Christ-Crain, M., Stolz, D., Tamm, M., et al. (2017). Procalcitonin to initiate or discontinue antibiotics in acute respiratory tract infections. Cochrane Database Syst. Rev. 10, Cd007498. doi: 10.1002/14651858.CD007498.pub3
Self, W. H., Balk, R. A., Grijalva, C. G., Williams, D. J., Zhu, Y., Anderson, E. J., et al. (2017). Procalcitonin as a marker of etiology in adults hospitalized with community-acquired pneumonia. Clin. Infect. Dis. 65, 183–190. doi: 10.1093/cid/cix317
Self, W. H., Grijalva, C. G., Williams, D. J., Woodworth, A., Balk, R. A., Fakhran, S., et al. (2016). Procalcitonin as an early marker of the need for invasive respiratory or vasopressor support in adults with community-acquired pneumonia. Chest 150, 819–828. doi: 10.1016/j.chest.2016.04.010
Tonial, C. T., Costa, C. A. D., Andrades, G. R. H., Crestani, F., Bruno, F., Piva, J. P., et al. (2021). Performance of prognostic markers in pediatric sepsis. J. Pediatr. (Rio J) 97, 287–294. doi: 10.1016/j.jped.2020.07.008
Wang, F., Deng, G., Liang, N., Hu, P., Liu, K., Liu, T., et al. (2023). Serum ferritin level is an effective prognostic factor for lung cancer immunotherapy. Cancer Biol. Ther. 24, 2285367. doi: 10.1080/15384047.2023.2285367
Keywords: ferritin, community-acquired pneumonia, elderly patients, prognostic prediction, emergency department (ED)
Citation: Zhang X, Shang N, Zhang D, Wu J and Guo S (2025) The independent predictive value of admission serum ferritin concentration for prognosis in elderly patients with community-acquired pneumonia in the emergency department. Front. Cell. Infect. Microbiol. 14:1505207. doi: 10.3389/fcimb.2024.1505207
Received: 02 October 2024; Accepted: 16 December 2024;
Published: 10 January 2025.
Edited by:
Yongqun Oliver He, University of Michigan, United StatesReviewed by:
Marisa Mariel Fernandez, Instituto de Estudios de la Inmunidad Humoral (UBA-CONICET), ArgentinaJie Wei, Renmin Hospital of Wuhan University, China
Copyright © 2025 Zhang, Shang, Zhang, Wu and Guo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Junyuan Wu, d3UwMDc4MzhAc2luYS5jb20=; Shubin Guo, c2h1YmluMDA3QHllYWgubmV0
†These authors have contributed equally to this work
 Xiangqun Zhang
Xiangqun Zhang Na Shang1,2,3
Na Shang1,2,3 Shubin Guo
Shubin Guo