
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cell. Infect. Microbiol. , 01 December 2023
Sec. Virus and Host
Volume 13 - 2023 | https://doi.org/10.3389/fcimb.2023.1298050
This article is part of the Research Topic Bunyaviruses - threats to health and economy View all 6 articles
Objective: The study aimed to comprehensively describe and evaluate the pathogenic and clinical characteristics of severe fever with thrombocytopenia syndrome (SFTS) patients with co-infections.
Methods: We retrospectively collected clinical data and laboratory indicators of the SFTS patients at Tongji Hospital from October 2021 to July 2023.
Results: A total of 157 patients with SFTS virus (SFTSV) infection were involved in the analysis, including 43 co-infection and 114 non-co-infection patients. The pathogens responsible for co-infection were primarily isolated from respiratory specimens. Fungal infections, primarily Aspergillus fumigatus, were observed in 22 cases. Bacterial infections, with Klebsiella pneumoniae and carbapenem-resistant Acinetobacter baumannii as the main pathogens, were identified in 20 cases. SFTS patients with co-infection exhibited higher mortality (P=0.011) compared to non-co-infection patients. Among SFTS patients co-infected with both bacteria and fungi (8 cases) or specific drug-resistant strains (11 cases), the mortality rate was as high as 70% (14/19). In comparison with the non-co-infection group, SFTS patients with co-infection displayed significant alteration in inflammatory markers, coagulation function, and liver function indicators.
Conclusion: The mortality rate of SFTS patients with co-infection is relatively high, underscoring the need for enhanced monitoring and timely, appropriate treatment to minimize the mortality rate.
Severe Fever with Thrombocytopenia Syndrome Virus (SFTSV) is an RNA virus that was first identified in China in 2010 and causes a clinical illness known as severe fever with thrombocytopenia syndrome (SFTS) (Yu et al., 2011; Zhang et al., 2012). Since its discovery, the incidence of SFTS has rapidly increased, posing a significant public health concern. The clinical manifestations of SFTS primarily include fever, diarrhea, and vomiting, and in severe cases, it can progress to multi-organ failure with a high mortality rate, ranging from 6% to 30% (Li et al., 2018; Casel et al., 2021; Li et al., 2021; Miao et al., 2021; Zhang X. et al., 2022).
Currently, the majority of studies have concentrated on predictive laboratory indicators for the occurrence and fatality of SFTS patients (Xu et al., 2018; Zhang et al., 2021; Liu et al., 2022; Zhang et al., 2023), with limited research integrating microbial infections into the assessment of risk factors for patient mortality. It has been reported that the mortality rate in SFTS patients was significantly increased when complicated with invasive pulmonary aspergillosis (IPA) (Chen et al., 2018; Bae et al., 2020; Hu et al., 2021; Xu et al., 2021). However, pathogens involved in co-infections, including Aspergillus, remain elusive (Ge et al., 2022; Zhang Y. et al., 2022), making the diagnosis of co-infections challenging and often leading to delayed treatment. Hence, it is crucial to describe the clinical characteristics of SFTS patients with concurrent infections and evaluate their risk factors, contributing to early diagnosis and timely administration of appropriate antibiotics, thereby reducing patient mortality. Some studies have evaluated laboratory parameters in SFTS patients to determine indicators that can be used for early prediction of IPA occurrence (Cui et al., 2013; Hu et al., 2021; Xu et al., 2021). Nevertheless, there is limited data on SFTS patients concurrently afflicted by bacterial infections. This study aimed to delineate the prevalence of SFTS patients with both bacterial and fungal infections, describe the characteristics of isolated pathogens, and subsequently evaluate the changes in clinical manifestations and laboratory indicators. The goal is to identify the risk factors associated with SFTS patients who are complicated by infections.
This retrospective cohort study was conducted at Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China, from October 2021 and July 2023. Patients were eligible for inclusion if SFTSV infection was confirmed positive by polymerase chain reaction or metagenomic next-generation sequencing (mNGS). Patients with immunosuppression, such as those undergoing transplant procedures or receiving long-term steroid therapy, were specifically excluded. Microorganisms were confirmed positive through cultivation, mNGS, (1, 3)-β-D-glucan (G), and galactomannan (GM) tests. Positive microbiological results were considered co-infections. The strains were identified by matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS) (Autof ms1000, China) and mNGS. Antimicrobial susceptibility tests and results analysis were performed according to the standard of the Clinical and Laboratory Standards Institute (CLSI) (https://clsi.org/) M100 Ed33 guideline and the European Committee on Antimicrobial Susceptibility Testing (EUCAST) (https://www.eucast.org/).
Data was collected for each SFTS patient, including the following variables: (1) demographic (age, sex); (2) underlying diseases (hypertension, coronary disease, diabetes); (3) clinical symptoms (fever, gastrointestinal symptoms (diarrhea, nausea, vomiting, poor appetite, bellyache), disorders of consciousness); (4) laboratory data (laboratory indicators, mNGS results, microbiological culture, and drug sensitivity results); (5) treatment regimens (continuous renal replacement therapy (CRRT), and mechanical ventilation); (6) outcome: The survival time of the patient was defined as the interval between the onset of clinical symptoms (self-reported) and death, with a cut-off point of 28 days. Follow-up by phone call was used to determine outcomes for patients who have not reached the observation time during hospitalization.
Continuous variables were presented as means ± standard deviation (SD) or median (interquartile range, IQR). Categorical variables were presented as numbers (%). Continuous variables were subject to the Wilcoxon rank-sum test or independent sample t test. The categorical variables are compared by Pearson Chi-square and Fisher’s Exact test between two groups. A p-value less than 0.05 was considered statistically significant. All variables with statistical significance in univariate analysis were included in multivariable logistic regression analysis for the model. The performance of various indicators was evaluated by the receiver operating characteristic (ROC) curve. Survival time data were analyzed using the Kaplan-Meier method and the log-rank test. The correlation between laboratory indicators was analyzed and visualized using the R package “corrplot”. Data were analyzed using SPSS version 25.0 (SPSS, Inc., Chicago, IL, USA), and plotted by the R 4.3.0 program (R Core Team).
A total of 157 SFTSV-positive patients including 43 co-infection and 114 non-co-infection patients were enrolled in the analysis. As shown in Table 1, the average age of SFTS patients with co-infection was 63.140 ± 8.587 years old. Among the SFTS patients with co-infection, 28 (65.1%) were female. It was observed that the proportion of SFTS patients with hypertension was higher in the co-infection group compared to the non-co-infection group, and this difference was statistically significant (30/114 (26.3%) vs 20/43 (46.5%), P=0.015). However, there were no significant differences in terms of age, sex, and other underlying diseases between the co-infection and non-co-infection groups.
Our data showed that fever (93.0%) was the most frequent symptom in SFTS patients. Approximately 54.8% of SFTS patients experienced gastrointestinal symptoms, while 35.7% of SFTS patients showed signs of disordered consciousness (Table 1). Statistical analysis results revealed that the probability of disorder of consciousness in the co-infection group was significantly higher than that in the non-co-infection group. A higher proportion of patients in the co-infection group received the CRRT and mechanical ventilation treatment than that of the non-co-infection group. In addition, we found that 23 (53.5%) of the 43 SFTS patients complicated with co-infections died, while 78 (68.4%) of the 114 SFTS patients without co-infections survived, indicating that SFTS patients with co-infections have a significantly higher risk of death (Table 1).
Among 43 SFTS patients with co-infections, 7 patients were positive for GM test in serum, but negative in culture results (Supplementary Table 1). A total of 57 strains were isolated from other 36 SFTS patients with co-infections obtained from various sample sources. The distribution of pathogen types and sample sources of the isolates obtained from SFTS patients are depicted in Figure 1.
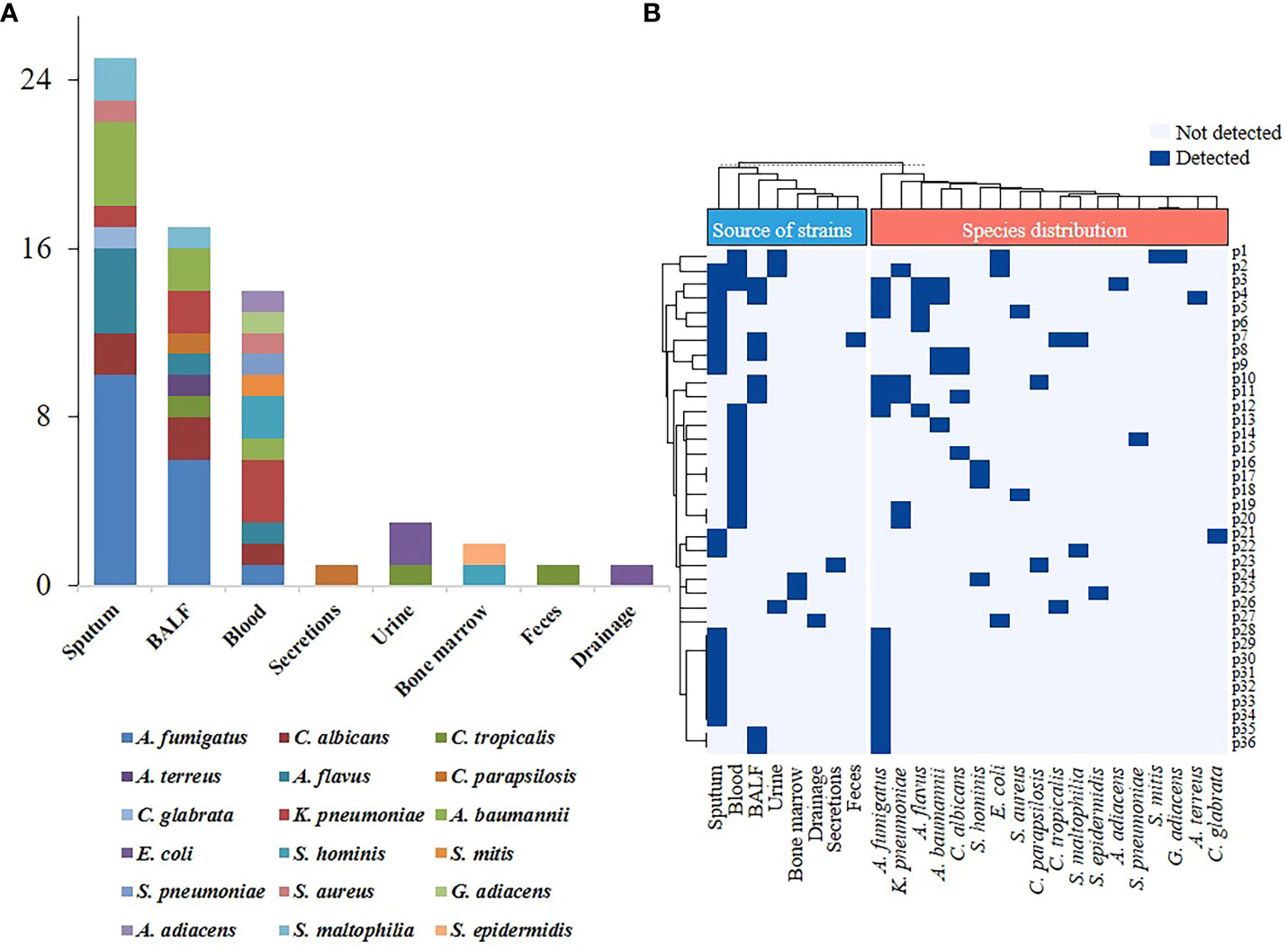
Figure 1 Species distribution and sample sources of pathogens isolated from severe fever with thrombocytopenia syndrome (SFTS) patients. (A) Sample sources of pathogens isolated from SFTS patients. (B) Sample types and pathogens distribution in SFTS patients with co-infection. BALF, bronchoalveolar lavage fluid; A. fumigatus, Aspergillus fumigatus; C. albicans, Candida albicans; C. tropicalis, Candida tropicalis; A. terreus, Aspergillus terreus; A. flavus, Aspergillus flavus; C. parapsilosis; Candida parapsilosis; C. glabrata, Candida glabrata; K. pneumoniae, Klebsiella pneumoniae; A. baumannii, Acinetobacter baumannii; E. coli, Escherichia coli; S. hominis, Staphylococcus hominis; S. aureus, Staphylococcus aureus; S. epidermidis, Staphylococcus epidermidis; S. mitis, Streptococcus mitis; S. pneumoniae, streptococcus pneumoniae; G. adiacens, Granulicatella adiacens; A. adiacens, Abiotrophia adiacens; S. maltophilia, Stenotrophomonas maltophilia.
The pathogens were predominantly isolated from sputum samples (25/57, 43.9%) and bronchoalveolar lavage fluid (BALF) (17/57, 29.8%), followed by blood samples (14/57, 24.6%). Fungi accounted for the majority of isolated pathogens, with the highest isolation rate, observed for Aspergillus fumigatus (A. fumigatus) (15/57, 26.3%), followed by Aspergillus flavus (A. flavus) (5/57, 8.8%), and Candida albicans (C. albicans) (4/57, 7%). Among the cases of bacterial infection, Klebsiella pneumoniae (K. pneumoniae) and Acinetobacter baumannii (A. baumannii) were the most frequently identified pathogens, accounting for 6 out of 57 cases (10.5%) (Supplementary Table 1; Figure 1A).
Our results showed that 11 patients were simultaneously infected with multiple pathogens. Out of these 11 cases, 8 patients had co-infection of bacteria and fungi, with A. fumigatus being the most prevalent co-infecting pathogen. Specifically, one patient (Patient ID: p12) was infected with both A. fumigatus and A. flavus. The remaining two patients exhibited mixed bacterial infections. Patient p1 had Granulicatella adiacens and Streptococcus mitis isolated from blood samples, along with a urine sample that showed an Escherichia coli (E. coli) strain resistant to multiple drugs (Figure 1B; Supplementary Table 1). Patient p2 had simultaneous isolation of K. pneumoniae from both blood and sputum samples. Notably, K. pneumoniae isolated from the blood was susceptible to multiple antibiotics, while the sputum isolate exhibited multidrug resistance (MDR) (Supplementary Table 1). Additionally, this patient also had a multidrug-resistant E. coli isolated from the urine sample. According to the results of the antibiotic susceptibility tests, a total of three strains of the multidrug-resistant organism (MDRO), six strains of carbapenem-resistant A. baumannii (CRAB), two strains of carbapenem-resistant K. pneumoniae (CRKPN) and a strain of methicillin-resistant Staphylococcus hominis (MRSCN) were isolated (Supplementary Table 1). Moreover, two strains of CRAB were isolated from both sputum and BALF samples of the same patient (Patient ID: p4).
The Kaplan-Meier curve indicated a significant difference (P=0.016) in survival rates between the co-infection and non-co-infection groups of SFTS patients (Figure 2). In terms of pathogen type and resistance phenotype, there were no statistically significant differences observed between the two groups of SFTS patients with co-infections who survived and those who did not (Supplementary Table 2). However, the mortality rate of SFTS patients solely infected with bacteria (6/13, 46.2%) or fungi (7/15, 46.7%) was comparable, while SFTS patients infected with both bacteria and fungi experienced a higher mortality rate (6/8, 75.0%) (Supplementary Table 2). Furthermore, the mortality rate among patients infected with specific drug-resistant strains (MDRO, CRAB, CRKPN, MRSCN) reached as high as 72.7% (8/11), which was greater than the mortality rate for SFTS patients infected with drug-sensitive strains (11/25, 44.0%).
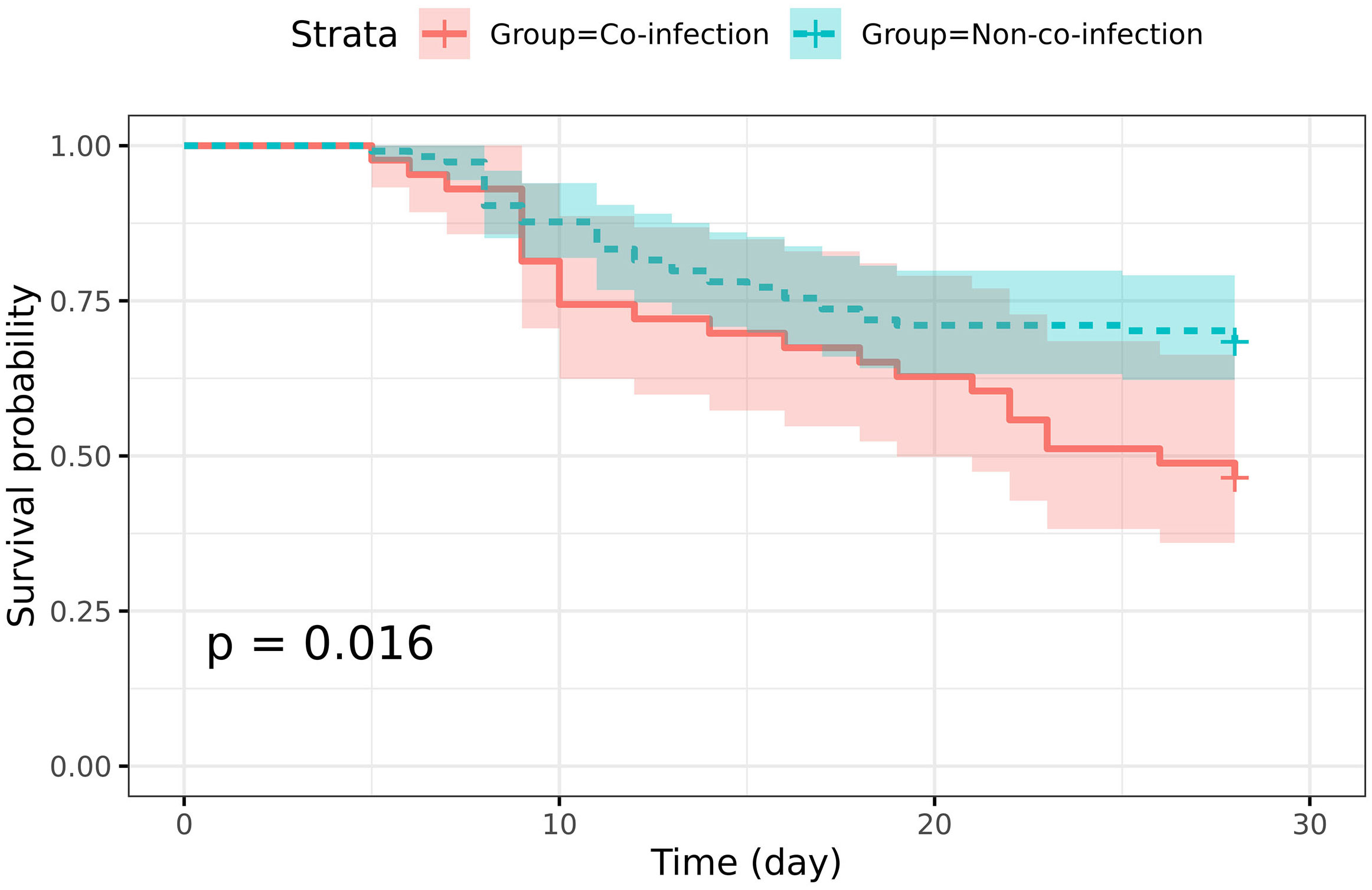
Figure 2 Survival analysis of severe fever with thrombocytopenia syndrome (SFTS) patients with and without co-infection. The Kaplan-Meier survival curve shows the 28-day survival rate of SFTS patients. The 95% confidence interval (CI) areas were displayed in different colors.
It was found that the level of albumin (ALB) was significantly lower in patients with co-infection than in those without co-infection (P=0.001) (Table 2). Additionally, there were statistically significant differences in several laboratory indicators, including aspartate aminotransferase (AST), alkaline phosphatase (ALP), lactate dehydrogenase (LDH), C-reactive protein (CRP), CRP-to-albumin ratio (CAR), procalcitonin (PCT), activated partial thromboplastin time (APTT) and thrombin time (TT), with higher levels in the co-infection group (Table 2). Furthermore, ROC curve analysis of these laboratory indicators showed that the AUC for most indicators ranged from 0.6 to 0.68. Notably, PCT and LDH exhibited higher AUC values, with PCT at 0.716 (95% CI, 0.629-0.802) and LDH at 0.704 (95% CI, 0.611-0.797) (Supplementary Table 3; Figure 3A). Specifically, when a threshold of 0.475 ng/mL was used, PCT showed a sensitivity of 65.1% and a specificity of 72.8% in distinguishing co-infection from non-co-infection patients. Similarly, LDH demonstrated a sensitivity of 60.5% and a specificity of 72.8% with a threshold of 1019.5 U/L (Supplementary Table 3). When the optimal threshold was selected, AST and CRP exhibited higher sensitivity (>70%) but lower specificity (<60%).
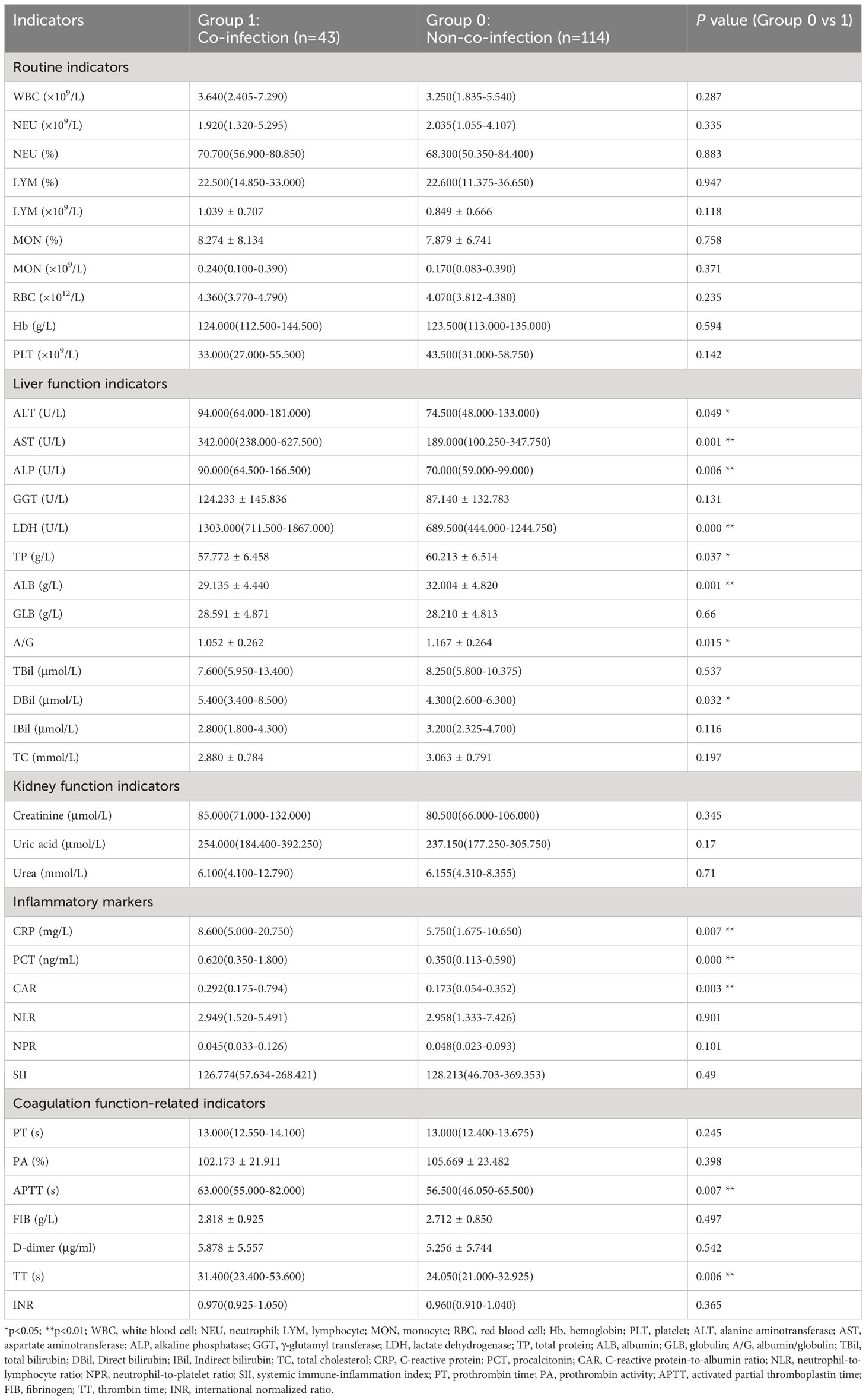
Table 2 Comparison of early laboratory indicators of severe fever with thrombocytopenia syndrome (SFTS) patients with and without co-infection.
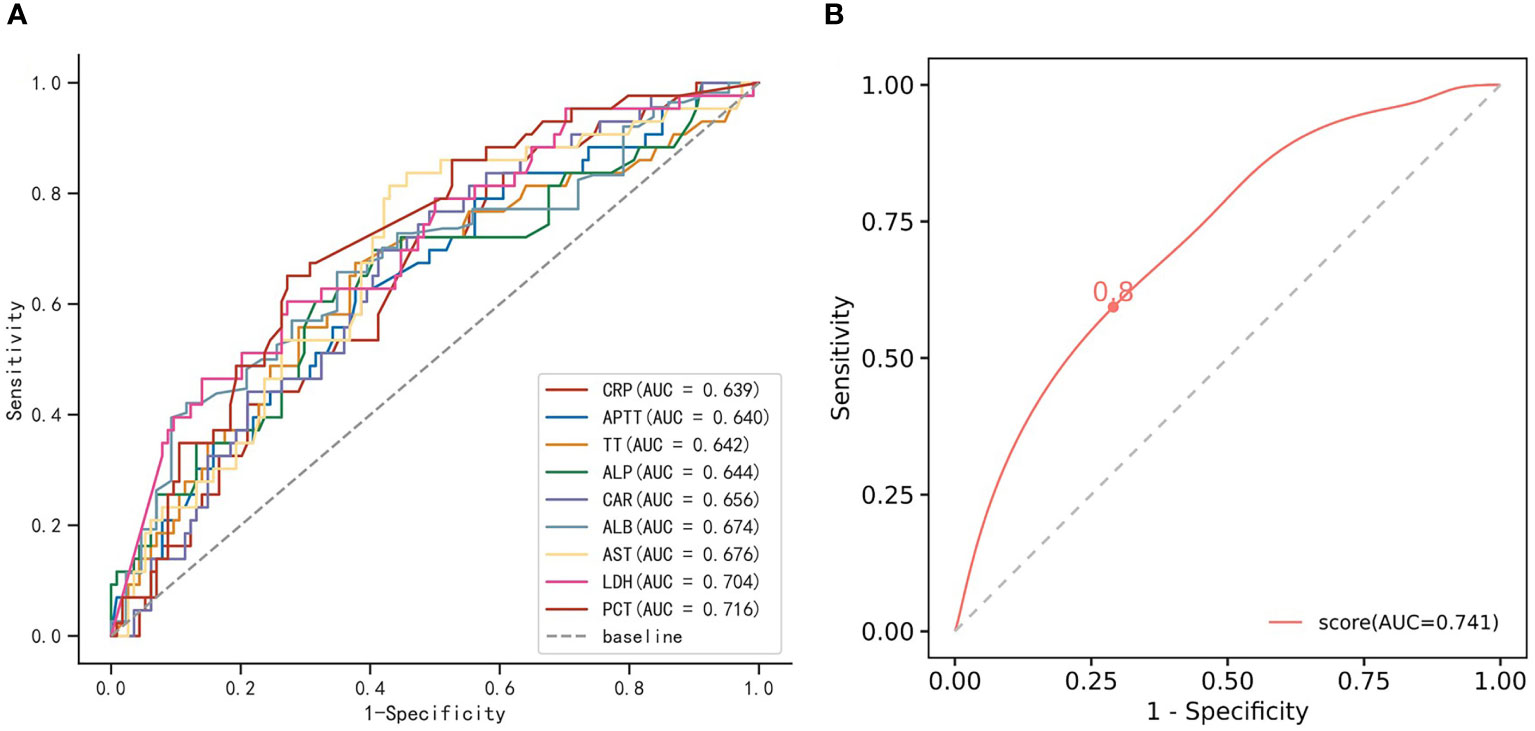
Figure 3 The receiver operating characteristic (ROC) curves. (A) The ROC curves of significant difference indicators in SFTS patients with co-infection and non-co-infection. (B) The ROC curve of the multivariable logistic regression model. The cutoff value is displayed on the graph. SFTS, severe fever with thrombocytopenia syndrome; AUC, area under the curve.
A collinearity analysis of laboratory parameters is presented in Supplementary Figure 1. Considering the correlation between laboratory parameters and the integrity of laboratory data, ALP, ALB, and LDH were ultimately selected for multivariate regression analysis based on both clinical experience and professional knowledge. The results of the multivariate regression analysis indicated LDH as a significant risk factor for co-infection in SFTS patients (P<0.05). Notably, the diagnostic model developed exhibited moderate performance, with an AUC of 0.741. This performance was slightly better than using indicator LDH or PCT as single indicators (Supplementary Table 4; Figure 3B).
SFTS is a life-threatening disease that has garnered global attention. Co-infections can exacerbate the condition, leading to multiple organ dysfunction and higher mortality rates. Therefore, it is crucial to diagnose co-infection in SFTS patients promptly and implement effective treatment strategies. The early identification of risk factors for SFTS co-infection is very important.
Currently, there is limited research that describes the results of microbiological culture in SFTS patients with co-infection. A study by Yin Zhang and colleagues evaluated the incidence and treatment regimes of SFTS patients with microbial infections but did not provide detailed information about the strains or compare laboratory indicators between co-infection and non-co-infection groups (Zhang Y. et al., 2022). In this study, we offered a comprehensive description of the pathogens isolated from SFTS patients with microbial infections, including the types of pathogens, sample sources, and antimicrobial susceptibility results. We found a high incidence of microbial infections in SFTS patients, with respiratory tract fungal infections being more common than bacterial infections. A. fumigatus and A. flavus were the most frequently isolated fungi in SFTS patients, consistent with previous reports (Zhang Y. et al., 2022). Additionally, we observed that the most frequently isolated pathogens in SFTS patients with bacterial infections were CRAB and K. pneumoniae. Notably, CRAB, Aspergillus terreus, and Abiotrophia adiacens were previously unreported in SFTS patients with co-infections.
Previous research indicated that SFTS patients with fungus infections have a higher mortality rate (Li et al., 2018; Xu et al., 2021; Zhang et al., 2021). Similarly, we found that the mortality rate of SFTS patients with microbial infections was significantly higher than that of the non-co-infection group. Our findings revealed an increasing trend in the mortality rate among SFTS patients who were concurrently infected with both bacteria and fungi or infected with specific drug-resistant strains. However, this trend did not reach statistical significance, which may be attributed to the relatively small number of cases available for analysis. Our results suggested that the type of pathogen and the antibiotic susceptibility phenotype of the strain had a certain impact on the prognosis of SFTS patients, emphasizing the importance of microbiological monitoring and identification of drug sensitivity phenotypes.
Neurological symptoms in SFTS patients have been identified as an important predictor of fatal outcomes (Guo et al., 2016). In our study, the SFTS patients with co-infections were more likely to have neurological symptoms and have a higher mortality rate. To determine the predictive indicators of co-infection in SFTS patients, we further compared the differences in laboratory indicators between co-infection and non-co-infection groups. The results showed that the indicators with differences between the two groups were mainly inflammatory markers (CRP, CAR, PCT, IL-6), coagulation function-related indicators (TT, APTT), and liver function-related indicators (ALB, AST, LDH, ALP, etc.). Liver injury is common in SFTS patients and is associated with patient mortality (Lu et al., 2022; Zhao et al., 2022). Previous studies found that ALT and ALP are independent risk factors for mortality in SFTS patients (Li et al., 2018; Xu et al., 2021; Zhang et al., 2021). Based on this, we believe that microbial infections in SFTS patients mainly exacerbate liver damage, thereby increasing mortality. Thus, it is necessary to closely monitor SFTS patient symptoms and evaluate laboratory indicators, especially liver function indices.
This study offered a comprehensive description of the epidemiological and clinical features of microbial infections in SFTS patients, highlighting the complexities of co-infections in SFTS patients. Additionally, potential predictive factors for co-infections in SFTS patients were identified through laboratory indicators analysis, emphasizing the importance of considering these factors in clinical management. However, our study has the following limitations. Firstly, the microbiological testing results were not validated using multiple methods, which could have potentially led to inaccurate infection rates. Secondly, due to the limited number of cases and incomplete laboratory data, certain important clinical indicators were excluded from the prediction model, potentially impacting its accuracy and predictive power.
In conclusion, this study provided valuable Supplementary Data on SFTS patients with co-infections, contributing to the epidemiological investigation of SFTSV infection and offering insights for improved disease management and reduced incidence rate and mortality. Future research should focus on expanding the sample size and incorporating additional laboratory indicators to further investigate the risk factors for co-infection in SFTS patients and optimize diagnostic models.
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
The studies involving humans were approved by the Medical Ethics Committee of Tongji Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because the research has been approved by the Medical Ethics Committee of Tongji Hospital. The committee also approved the abandonment of the informed consent form for participation in this study due to its retrospective design.
HS: Data curation, Formal Analysis, Investigation, Methodology, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. SZ: Methodology, Writing – review & editing. YH: Methodology, Writing – review & editing. YW: Investigation, Writing – review & editing. TW: Investigation, Writing – review & editing. WW: Investigation, Methodology, Writing – review & editing. ZS: Funding acquisition, Investigation, Writing – review & editing. HH: Formal Analysis, Investigation, Methodology, Resources, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by grants from the Special Foundation for National Science and Technology Basic Research Program of China (no. 2019FY101206).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcimb.2023.1298050/full#supplementary-material
Supplementary Figure 1 | The collinearity analysis of significant difference indicators in severe fever with thrombocytopenia syndrome (SFTS) patients. PCT, procalcitonin; LDH, lactate dehydrogenase; AST, aspartate aminotransferase; ALB, albumin; ALP, alkaline phosphatase; TT, thrombin time; APTT, activated partial thromboplastin time; CRP, C-reactive protein; CAR, C-reactive protein-to-albumin ratio.
Bae, S., Hwang, H. J., Kim, M. Y., Kim, M. J., Chong, Y. P., Lee, S., et al. (2020). Invasive pulmonary aspergillosis in patients with severe fever with thrombocytopenia syndrome. Clin. Infect. Dis. 70 (7), 1491–1494. doi: 10.1093/cid/ciz673
Casel, M. A., Park, S. J., Choi, Y. K. (2021). Severe fever with thrombocytopenia syndrome virus: Emerging novel phlebovirus and their control strategy. Exp. Mol. Med. 53 (5), 713–722. doi: 10.1038/s12276-021-00610-1
Chen, X., Yu, Z., Qian, Y., Dong, D., Hao, Y., Liu, N., et al. (2018). Clinical features of fatal severe fever with thrombocytopenia syndrome that is complicated by invasive pulmonary aspergillosis. J. Infect. Chemother. 24, 422–427. doi: 10.1016/j.jiac.2018.01.005
Cui, N., Wang, H., Long, Y., Liu, D. (2013). CD8+ T-cell counts: An early predictor of risk and mortality in critically ill immunocompromised patients with invasive pulmonary aspergillosis. Crit. Care (London England). 17 (4), R157. doi: 10.1186/cc12836
Ge, H., Wang, G., Guo, P., Zhao, J., Zhang, S., Xu, Y., et al. (2022). Coinfections in hospitalized patients with severe fever with thrombocytopenia syndrome: A retrospective study. J. Med. Virol. 94 (12), 5933–5942. doi: 10.1002/jmv.28093
Guo, C., Lu, Q., Ding, S., Hu, C., Hu, J., Wo, Y., et al. (2016). Epidemiological and clinical characteristics of severe fever with thrombocytopenia syndrome (SFTS) in China: An integrated data analysis. Epidemiol. Infect. 144 (6), 1345–1354. doi: 10.1017/S0950268815002678
Hu, L., Kong, Q., Yue, C., Xu, X., Xia, L., Bian, T., et al. (2021). Early-Warning immune predictors for invasive pulmonary aspergillosis in severe patients with severe fever with thrombocytopenia syndrome. Front. Immunol. 12. doi: 10.3389/fimmu.2021.576640
Li, J., Li, S., Yang, L., Cao, P., Lu, J. (2021). Severe fever with thrombocytopenia syndrome virus: A highly lethal bunyavirus. Crit. Rev. Microbiol. 47 (1), 112–125. doi: 10.1080/1040841X.2020.1847037
Li, H., Lu, Q., Xing, B., Zhang, S., Liu, K., Du, J., et al. (2018). Epidemiological and clinical features of laboratory-diagnosed severe fever with thrombocytopenia syndrome in China 2011-17: a prospective observational study. Lancet Infect. diseases. 18 (10), 1127–1137. doi: 10.1016/S1473-3099(18)30293-7
Liu, Z., Zhang, R., Zhou, W., Ma, R., Han, L., Zhao, Z., et al. (2022). High levels of C-reactive protein-to-albumin ratio (CAR) are associated with a poor prognosis in patients with severe fever with thrombocytopenia syndrome in early stage. J. Med. Virol. 94 (11), 5375–5384. doi: 10.1002/jmv.27972
Lu, S., Xu, L., Liang, B., Wang, H., Wang, T., Xiang, T., et al. (2022). Liver function derangement in patients with severe fever and thrombocytopenia syndrome. J. Clin. Trans. hepatology. 10 (5), 825–834. doi: 10.14218/JCTH.2021.00345
Miao, D., Liu, M., Wang, Y., Ren, X., Lu, Q., Zhao, G., et al. (2021). Epidemiology and ecology of severe fever with thrombocytopenia syndrome in China 2010-2018. Clin. Infect. Dis. 73 (11), e3851–e3858. doi: 10.1093/cid/ciaa1561
Xu, Y., Shao, M., Liu, N., Tang, J., Gu, Q., Dong, D. (2021). Invasive pulmonary aspergillosis is a frequent complication in patients with severe fever with thrombocytopenia syndrome: A retrospective study. Int. J. Infect. Dis. 105, 646–652. doi: 10.1016/j.ijid.2021.02.088
Xu, X., Sun, Z., Liu, J., Zhang, J., Liu, T., Mu, X., et al. (2018). Analysis of clinical features and early warning indicators of death from severe fever with thrombocytopenia syndrome. Int. J. Infect. Dis. 73, 43–48. doi: 10.1016/j.ijid.2018.05.013
Yu, X., Liang, M., Zhang, S., Liu, Y., Li, J., Sun, Y., et al. (2011). Fever with thrombocytopenia associated with a novel bunyavirus in China. New Engl. J. Med. 364 (16), 1523–1532. doi: 10.1056/NEJMoa1010095
Zhang, Y., He, Y., Dai, Y., Xiong, Y., Zheng, H., Zhou, D., et al. (2012). Hemorrhagic fever caused by a novel Bunyavirus in China: Pathogenesis and correlates of fatal outcome. Clin. Infect. Dis. 54 (4), 527–533. doi: 10.1093/cid/cir804
Zhang, Y., Huang, Y., Xu, Y. (2022). Associated microbiota and treatment of severe fever with thrombocytopenia syndrome complicated with infections. J. Med. Virol. 94 (12), 5916–5921. doi: 10.1002/jmv.28059
Zhang, Y., Miao, W., Xu, Y., Huang, Y. (2021). Severe fever with thrombocytopenia syndrome in Hefei: Clinical features, risk factors, and ribavirin therapeutic efficacy. J. Med. Virol. 93 (6), 3516–3523. doi: 10.1002/jmv.26544
Zhang, X., Zhao, C., Cheng, C., Zhang, G., Yu, T., Lawrence, K., et al. (2022). Rapid spread of severe fever with thrombocytopenia syndrome virus by parthenogenetic asian longhorned ticks. Emerg. Infect. Dis. 28 (2), 363–372. doi: 10.3201/eid2802.211532
Zhang, Y., Zhong, P., Wang, L., Zhang, Y., Li, N., Li, Y., et al. (2023). Development and validation of a clinical risk score to predict the occurrence of critical illness in hospitalized patients with SFTS. J. infection Public Health 16 (3), 393–398. doi: 10.1016/j.jiph.2023.01.007
Keywords: SFTS, co-infection, mortality, Aspergillus fumigatus, bacterial infection
Citation: Song H, Zou S, Huang Y, Wang Y, Wang T, Wei W, Sun Z and Hou H (2023) The pathogenic and clinical characteristics of severe fever with thrombocytopenia syndrome patients with co-infections. Front. Cell. Infect. Microbiol. 13:1298050. doi: 10.3389/fcimb.2023.1298050
Received: 21 September 2023; Accepted: 30 October 2023;
Published: 01 December 2023.
Edited by:
Feihu Yan, Chinese Academy of Agricultural Sciences (CAAS), ChinaReviewed by:
Liang-jun Chen, Wuhan University, ChinaCopyright © 2023 Song, Zou, Huang, Wang, Wang, Wei, Sun and Hou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hongyan Hou, dGpob3Vob25neWFuQHRqaC50am11LmVkdS5jbg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.