- 1Department of Pulmonary and Critical Care Medicine, Zhongshan Hospital, Fudan University, Shanghai, China
- 2Department of Respiratory Medicine, Tongren Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai, China
- 3Department of Respiratory Medicine, School of Medicine, Ruijin Hospital, Shanghai Jiao Tong University, Shanghai, China
- 4Department of Respiratory Medicine, School of Medicine, Ruijin North Hospital, Shanghai Jiao Tong University, Shanghai, China
- 5Department of Respiratory Medicine, School of Medicine, Renji Hospital, Shanghai Jiao Tong University, Shanghai, China
- 6Department of Respiratory Medicine, Shanghai Putuo District People's Hospital, Shanghai, China
- 7Department of Respiratory Medicine, Shanghai Fifth' Peoples Hospital, Fudan University, Shanghai, China
- 8Department of Respiratory Medicine, Huashan Hospital, Fudan University, Shanghai, China
- 9Department of Respiratory Medicine, Central Hospital of Minhang District, Shanghai, Fudan University, Shanghai, China
- 10Department of Respiratory Medicine, Shanghai General Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai, China
- 11Department of Respiratory Medicine, Shanghai Pulmonary Hospital, Tongji University, Shanghai, China
Objective: To explore impact of Candida on the acute exacerbation of chronic obstructive pulmonary disease (AECOPD) outcome.
Methods: A retrospective, multi-center, case-control study was performed. Patients hospitalized for AECOPD in 25 centers during Jan 2011–Dec 2016 were enrolled. Data were collected, including demographic information, conditions during the stable phase of COPD, clinical characteristics of AECOPD, and follow-up information within 1 year after discharge. Univariate analysis and binary logistic regression were applied, and p < 0.05 was regarded as significant.
Results: Totally 1,103 patients were analyzed, with 644 lower respiratory airway (LTR) Candida positive cases and 459 Candida negative controls. Long-term prognosis was significantly different between Candida positive and negative group, including the recurrent AECOPD within 180 days (75.5 vs. 6.6%, p < 0.001) and mortality within 1 year (6.9 vs. 0.4%, p < 0.001). Univariate logistic analysis showed that LTR Candida isolation was related to higher recurrence rate of AECOPD within 180 days and mortality within 1 year. Binary logistic regression analysis demonstrated that LTR Candida isolation was independently associated with recurrence of AECOPD within 180 days.
Conclusions: LTR Candida isolation was associated with worse long-term prognosis of AECOPD and independently related to higher risks of recurrent AECOPD within 180 days.
Introduction
Chronic obstructive pulmonary disease (COPD) is one of the most common chronic diseases with high morbidity and mortality. According to the 2019 global initiative for COPD (GOLD) report, COPD is the fourth leading cause of death in the world. It is expected to rise to the third place by 2020, and more than 3 million people died of COPD in 2012, accounting for 6% of the total number of deaths in the world (GOLD, 2019). According to the Global Burden of Disease Study data, COPD is the third leading cause of death in China, and the mortality rate is increasing (Wang, 2017). Acute exacerbation of COPD (AECOPD) is the most important acute event in the disease course of COPD, leading to disease progression and poor outcome. It has been reported that every patient with COPD suffered from 1.5 exacerbations a year on average (Wedzicha and Seemungal, 2007). The most common causes of AECOPD were viruses and bacterial infections (Aaron, 2014; Cai et al., 2014). Co-infection of viruses and bacteria has been detected in 25% of exacerbations (Sethi and Murphy, 2008).
Candida is one of the normal floras of human body, and is also the most common conditional fungal pathogen. Invasive Candida infection (ICI) occupies the first place in invasive fungal disease (IFD) (Pfaller and Diekema, 2007). At the same time, Candida is commonly colonized in lower respiratory airway (LTR). It was found that the main risk factors for high Candida isolation rates in LTR were COPD, smoking, tuberculosis, malnutrition, malignant tumors, diabetes, HIV infection, and long-term use of antibiotics. Among them, the LTR isolation rate of Candida in COPD patients was the highest (76.65%) (Jha et al., 2006), particularly in elder patients (≥60) with persistent disease progression, recurrent infection, long-term repeated use of broad-spectrum antibiotics and systemic glucocorticoids application, mechanical ventilation (MV) and invasive procedures, or along with other chronic underlying diseases such as diabetes (Liu and Su-Rong, 2015). Broad-spectrum antibiotics and glucocorticoids are widely used in the treatment of hospitalized AECOPD, which contribute to the high colonization rate of Candida albicans in these patients (Bassetti et al., 2013; De Rosa et al., 2015; Hii et al., 2015). To our knowledge, studies focused on the impact of Candida colonization on respiratory disease were mainly about ventilator-associated pneumonia (VAP) and intensive care unit (ICU)-acquired pneumonia (Williamson et al., 2011; Dong-xing et al., 2016; Terraneo et al., 2016), while impact of Candida colonization on the prognosis of AECOPD was rarely reported. The object of our study was to explore the impact of LTR Candida isolation on the short-term and long-term prognosis of hospitalized AECOPD, which might have important clinical significance for the prevention and treatment of COPD patients.
Materials and Methods
Study Design and Patient Population
A retrospective, multicenter, case-control study was performed to investigate the relationship between Candida isolation in the respiratory tract and the prognosis of hospitalized AECOPD. From January 1st, 2011 to December 31st, 2016, patients hospitalized for AECOPD in 25 hospitals in Shanghai were collected. Only the hospitals where Candida culture of LTR samples were routinely performed and followed during hospitalization for admitted patients with AECOPD were involved into the current study. LTR samples included sputum, endotracheal suction, bronchoscopic flushing and lavage fluid.
The inclusion criteria were as follows: (1). Patients older than 18 years old, hospitalized for AECOPD who met the diagnostic criteria of COPD and acute exacerbation in 2017 GOLD report. Definition of acute exacerbation is the process of acute onset, which is characterized by deterioration of respiratory symptoms, beyond the scope of daily variation, and the need to change drug treatment regimens. (2) Patients with 1 year follow-up data. Those who died <1 year after hospitalization were also involved.
The exclusion criteria were the existence of any of the following: (1). Patients under 18 years old or with mental illness who were not capable of cooperating with access to clinical data; (2). Patients with lung cancer, bronchiectasis, lung abscess, interstitial pulmonary diseases; (3). Positive results of Candida smears or Candida culture in blood, pleural effusion or urine samples.
Data Collection
According to the smears or culture results of respiratory tract specimens, all the participants were divided into Candida positive group and Candida negative group.
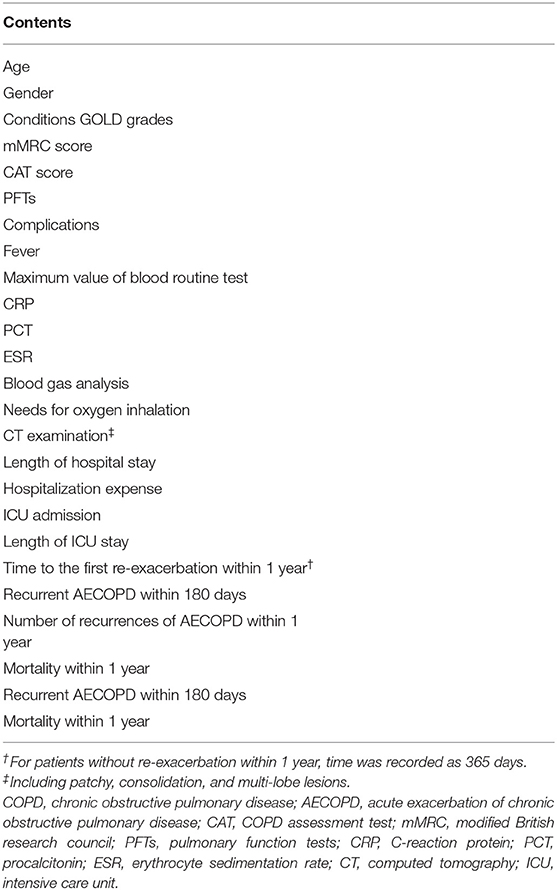
The collected clinical variables are listed in Table 1. The collected data were input into the Epidata system (The EpiData Association, Odense, Denmark) by one investigator, and then checked by another. Any inconsistent data found would be checked and corrected according to the original case report forms.
The first clinical outcome is recurrent AECOPD within 180 days, and the second clinical outcome is mortality within 1 year.
Ethical Approval
The ethics committee of Ruijin Hospital approved the study (Number: 2017-108) according to the principles of the Declaration of Helsinki. Informed consent was waived because the study was retrospective. The study was registered on Chinese Clinical Trial Registry (Registration Number: ChiCTR-RRC-17014078).
Data Analysis
All the data were statistically analyzed by SPSS 22 system (SPSS Inc, Chicago, IL).
Firstly, comparison of conditions during the stable phase of COPD between Candida positive and negative groups was conducted. One-sample Kolmogorov-Smirnoff test was used to evaluate the normality of continuous variables. The continuous variables with normality were expressed as means with standard deviations and assessed for differences by Student t-test. For non-normal variables, medians are presented with interquartile ranges (IQR), and the Mann-Whitney U-test was performed when comparing two groups. The categorical variables were described as rate (%) or percentage (%), and Chi square tests or two-tailed Fisher's exact test were performed for comparisons.
Secondly, patients were separately grouped according to relapse within 180 days or death within 1 year, to identify risk factors associated with the prognosis of AECOPD. Univariate logistic regression was applied in the analysis of risk factors related to prognosis of AECOPD. Variables significant in univariate analysis (P < 0.05) were further evaluated in the binary logistic regression analysis. All reported p-values are 2-tailed, and P < 0.05 was taken as significant.
For missing data, patients without outcomes were withdrawn; and risk factors were deleted when missing data was over 20%.
Results
A total of 1,103 patients were enrolled in this study, including Candida negative controls (n = 459) and Candida positive cases (n = 644). There were 944 male patients and 159 female patients. The flowchart was showed in Figure 1.
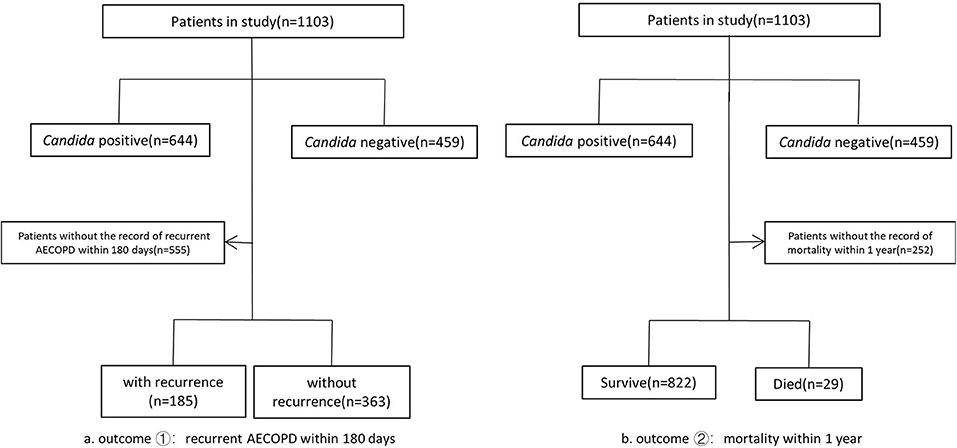
Figure 1. Study population flow chart. The total number of patients enrolled was 1,103. Patients were divided into Candida positive group(n = 644) and Candida negative group(n = 459) according to the smears or culture results of respiratory tract specimens. Death within 1 year and recurrent AECOPD within 180 days were two outcomes analyzed separately in our study. We withdrew patients without the record of death within 1 year (n = 252) and patients without the record of recurrent AECOPD within 180 days(n = 555) separately, and the remained patients were divided into two groups according to the outcomes, respectively.
Patients With Severe Symptoms or Complications Tend to Have Positive LTR Candida
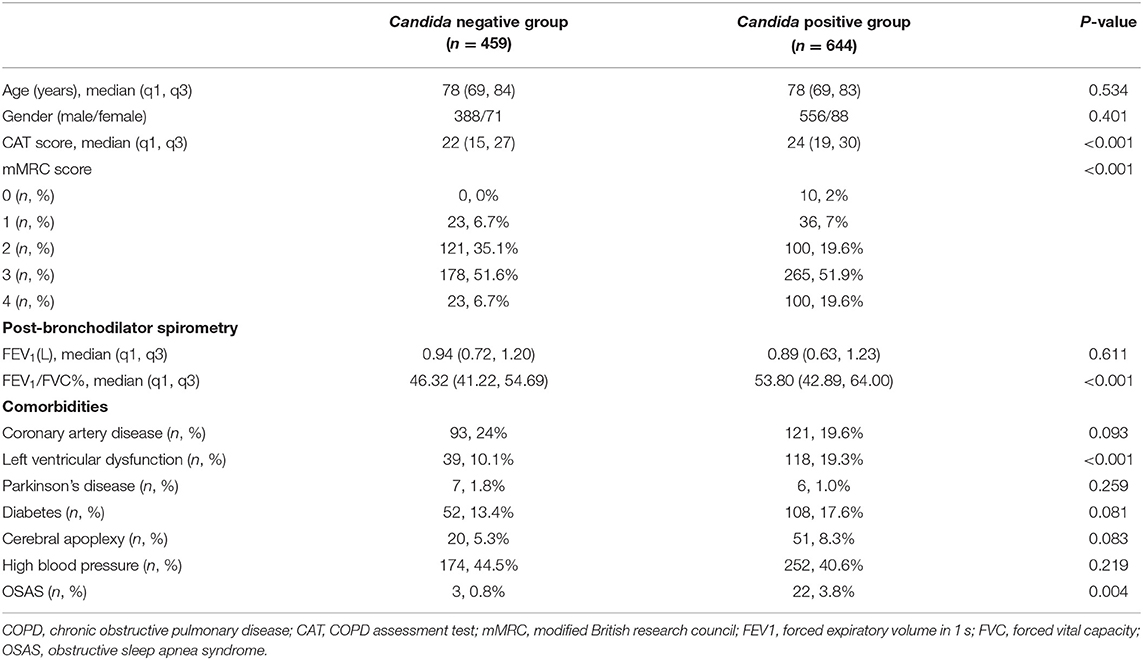
We compared the conditions during the stable phase of AECOPD between Candida positive and Candida negative group. The median age of Candida positive group was 78 (69, 83) years old, including 556 male patients and 88 female patients, and the median age of Candida negative group was 78 (69, 84) years old, including 388 male patients and 71 female patients. No difference in age and sex ratio between the two groups was found.
Data analysis showed that CAT score in Candida positive group was slightly higher than that of Candida negative group (24 (19, 30) vs. 22 (15, 17), P < 0.001). The proportion of patients with mMRC grade 3–4 was also higher in the Candida positive group (71.5 vs. 58.3%, P < 0.001), which indicated that COPD patients with severe symptoms were more likely to be Candida positive.
However, no significant difference was observed in the value of forced expiratory volume in 1 s (FEV1) between the two groups during the stable phase, suggesting that severity of airflow limitation may not related to the LTR Candida. Both the FEV1/FVC% value of Candida positive group and Candida negative group were lower than 70%, which confirmed the diagnosis of COPD.
In terms of complications during the stable phase of COPD, the Candida positive group had a higher proportion of left ventricular dysfunction and obstructive sleep apnea syndrome (OSAS) (19.3 vs. 10.1%, P < 0.001; 3.8 vs. 0.8%, P = 0.004, respectively). Data was shown in Table 2.
Candida Predict Worsening Prognosis of AECOPD
As data shown in Table 3, differences in in-hospital outcome between Candida positive group and Candida negative group were not statistically significant. Length of hospital stay and hospitalization expense were very close between two groups. The proportion of patients admitted in ICU in Candida positive group was higher than that in Candida negative group, but this trend failed to reach statistical significance (7.1 vs. 6.1%, P = 0.531). Nevertheless, patients in Candida positive group were more likely to have a relapse of AECOPD within 180 days (75.5 vs. 6.6%, P < 0.001), and their time to first re-exacerbation was significantly shorter (131.29 ± 143.03 vs. 341.69 ± 87.67 days, P < 0.001). Moreover, Candida positive group was associated with the higher mortality rate within 1 year (6.9 vs. 0.4%, P < 0.001).
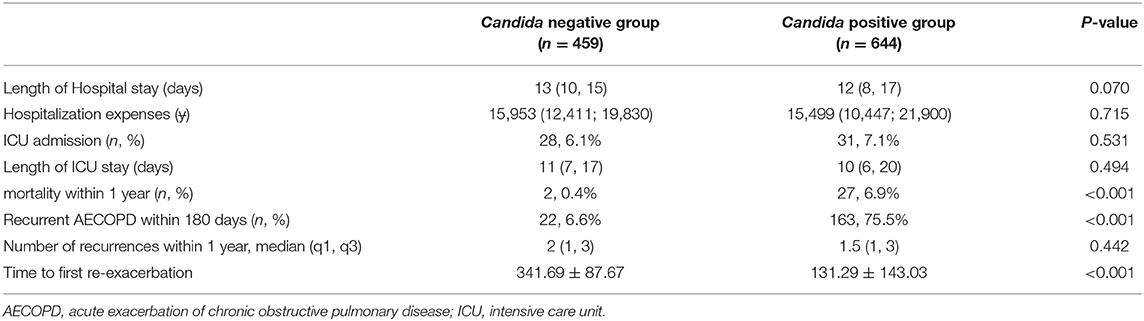
Table 3. Prognosis of hospitalized AECOPD patients with or without Candida isolation from LTR samples.
Other Factors Related to Prognosis of AECOPD
A significant difference in the prognosis was observed between the Candida negative group and the Candida positive group. To validate the role of LTR Candida isolation on the long-term outcome of hospitalized AECOPD, we performed the statistical analysis of related risk factors of “recurrence of AECOPD within 180 days” and “mortality within 1 year.” Data was shown in Supplementary Table 1.
The higher CAT score and mMRC score during the stable phase were two important risk factors affecting the recurrence of AECOPD within 180 days (OR = 1.073, 95% CI (1.039, 1.108), P < 0.001; OR = 1.977, 95% CI (1.475, 2.649), P < 0.001, respectively) and mortality within 1 year (OR = 1.142, 95% CI (1.063, 1.226), P < 0.001; OR = 2.211, 95% CI (1.250, 3.910), P = 0.006, respectively).
Besides, positive Candida colonization showed strong relationship with higher recurrence of AECOPD (OR = 43.336, 95% CI (25.456, 73.775), P < 0.001) and mortality within 1 year (OR = 16.737, 95% CI (3.954, 70.846), P < 0.001). Data showed that high percentage of neutrophils and procalcitonin (PCT) were both risk factors for recurrence of AECOPD within 180 days(OR = 1.017, 95% CI (1.000, 1.033), P = 0.044; OR = 1.036, 95% CI (1.008, 1.064), P = 0.012, respectively) and mortality within 1 year (OR = 1.042, 95% CI (1.003, 1.082), P = 0.032; OR = 1.05, 95% CI (1.028, 1.079), P < 0.001). Patients treated with oxygen inhalation also exhibited higher probability of relapse and mortality (OR = 1.992, 95% CI (1.361, 2.915), P < 0.001; OR = 3.394, 95% CI (1.457, 7.907), P = 0.005, respectively), perhaps due to oxygen inhalation was applied in patients with more serious condition.
LTR Candida Isolation Was Identified as an Independent Risk Factor for AECOPD Relapse Within 180 Days
Considering the results of uni-variate analysis, we recruited variables significant (P < 0.05) into the binary logistic regression analysis of recurrent AECOPD within 180 days. Supplementary Table 2 showed that LTR Candida colonization, RBC, ESR during AECOPD and the mMRC score during the stable phase were independently associated with recurrent AECOPD within 180 days. Among them, Candida colonization status showed the strongest relationship (OR = 1613.620, 95% CI (1.501, 62740.313), P < 0.001)
Besides, the binary logistic regression analysis of mortality within 1 year was also analyzed (Supplementary Table 3). The result showed that PCT during AECOPD was an independent risk factor for mortality within 1 year. However, LTR Candida colonization may also led to higher mortality within 1 year but this trend failed to reach statistical significance.
Discussion
In the current study, we found that patients with higher CAT or mMRC score, or patients with severe complications in stable phase of COPD tends to have positive LTR Candida isolation, and positive LTR Candida significantly worsen the long-term prognosis including recurrence within 180 days and mortality within 1 year. To our knowledge, this is the first study looking into the correlation between LTR Candida and the prognosis of hospitalized AECOPD.
Previous studies have suggested that Candida colonization might be associated with worse clinical outcomes in critically ill patients. Studies conducted by Delisle et al. (2008) showed a correlation between independent colonization of Candida albicans and prolonged hospital stay (59.9 vs. 38.6 days, P = 0.006) in ICU patients who fulfilled criteria for a clinical suspicion of ventilator-associated pneumonia (VAP). Azoulay et al. (2006) also observed that patients with Candida airway colonization had significantly longer ICU residence time (17(9, 32) vs. 9(5, 17), P < 0.001) and hospitalization time (36(19, 74) vs. 22(9, 75), P < 0.001). However, extended hospitalization and ICU residence time of Candida positive group was not observed in our study, and we believed that it was mainly due to different research populations. Previous studies focused on VAP and ICU-acquired pneumonia patients, while our study enrolled patients with AECOPD. Therefore, we suggest that whether there is a correlation between Candida colonization and prolonged hospital stay or ICU residence time could mainly depend on the primary disease.
Mortality is an important indicator of disease prognosis. We observed a significant trend of higher mortality in Candida positive group. It was in accordance with previous studies which found that there was an independent correlation between colonization of airway Candida and a higher hospital mortality (Delisle et al., 2008; Williamson et al., 2011; Hamet et al., 2012). There were also other researches indicated that Candida colonization was not related to an increased in-hospital mortality (Wood et al., 2006; Roux et al., 2009b; Terraneo et al., 2016). However, all these studies were performed in hospitalized or ICU patients with VAP or ICU-acquired pneumonia. Whether there is a correlation between positive LTR Candida and mortality of AECOPD needs to be further studied.
Recurrence of AECOPD was the main objective of our research. To our knowledge, the clinical relevance of LTR Candida isolation and recurrence of AECOPD has not been established. Our research exhibited that patients in positive Candida group were more likely to have a relapse of AECOPD within 180 days. Binary multi-variate regression analysis approved that positive Candida was independently associated with recurrent AECOPD within 180 days. Besides, that patients in Candida group suffered higher death rate.
In theory, LTR Candida may cause detrimental effects in different aspects. Firstly, Candida colonized in the respiratory tract would further adhere to, invade and infect under certain conditions. It was considered that Candida colonization was the precursor risk factor of Candida infection, and may be the risk factor and predictive index of deep Candida infection (Eggimann et al., 2003).
Secondly, Candida could interact with local pathogenic bacteria, affect the occurrence and development of bacterial infection through direct contact or indirect regulation (Ricard and Roux, 2012; Mear et al., 2013), changing the pathogenic process of each other (Shirtliff et al., 2009; De Pascale and Antonelli, 2014). Thus, patients with Candida colonization had a greater chance to acquire pneumonia caused by bacteria infection. A retrospective study in China found that respiratory Candida colonization could increase the risk of bacterial VAP in patients with MV, and the reason may be that Candida colonized in human respiratory tract increased the chance of bacterial infection by interacting with pathogenic bacteria (Dong-xing et al., 2016). A few retrospective studies have shown that airway Candida colonization could promote VAP development, especially when it was caused by Pseudomonas aeruginosa (Azoulay et al., 2006; Roux et al., 2009a). Besides, it has been shown that Staphylococcus aureus could change into resistant phenotype when growing within Candida spp. (Harriott and Noverr, 2009). Candida may also attributed to the formation of biofilm through interactions with other pathogens such as Staphylococcus aureus, resulting in a more effective pattern for pathogens to escape from host immunity (Roux et al., 2009a; Morales and Hogan, 2010; Peters et al., 2010). All these findings suggested that Candida colonization within the respiratory tract could facilitate bacterial growth and defense against antibiotics. For patients with severe COPD, increased bacteria burden would lead to the onset of exacerbation.
Thirdly, it was also proved that Candida could cause allergic bronchopulmonary mycosis (Chowdhary et al., 2014), so the sensitization of colonized Candida could lead to respiratory symptoms.
All these researches may explain the higher rate of recurrence of AECOPD in LTR Candida positive patients.
Antifungal treatment is not routinely recommended in case of positive Candida isolation from LTR samples, because pneumonia is rarely caused by this fungal species (Garnacho-Montero et al., 2013). Studies had also shown that antifungal therapy was not associated with better outcomes of patients with LTR Candida spp. isolation (Wood et al., 2006; Terraneo et al., 2016). Considering the data in the current study, LTR Candida isolation in patients with hospitalized AECOPD should be monitored more carefully and frequently, and evaluation the individualized need for de-colonization therapy is necessary for optimal outcome. More importantly, study on the mechanism how Candida interact with other pathogens as well as human immune system and how this interaction leads to AECOPD are required, with the purpose of finding new interventions.
Our study has several limitations. Firstly, it is a retrospective study, therefore the correlation between the variables could be proven but could not be explained as causal relationship. Secondly, subjective bias cannot be avoided in some ways. We plan to verify the results in prospective studies in the future. Thirdly, we were not able to distinguish whether the patients were colonized with Candida before AECOPD or secondary to the treatment of AECOPD. Fourthly, we could not distinguish if it was Candida infection or Candida colonization, either, which is a common problem in similar researches (Olaechea et al., 2004; Azoulay et al., 2006).
In spite of these limitations, the results can lead to the convincing conclusion that the LTR Candida isolation was associated with worse outcomes of AECOPD patients. There was an independent association between positive LTR Candida with exacerbation relapse within 180 days of hospitalized AECOPD, and it might contribute to an increased 1 year mortality. Besides, it is suggested that the risk of Candida positive in patients with severe symptoms is higher, and the detection should be strengthened. Clinical research with prospective design and adequate sample size are required to validate this relationship and explore specific intervention strategy to improve patients' outcome. Attention should be paid to the impact of Candida on AECOPD patients in clinic practice.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Ethics Statement
The ethics committee of Ruijin Hospital approved the study (Number: 2017-108). This study was registered on Chinese Clinical Trial Registry (Registration Number: ChiCTR-RRC-17014078). Informed consent was waived because the study was retrospective.
Author Contributions
Y-hZ analyzed data and wrote the paper. W-qW was in charge of monitoring the study progress and collecting data. The following authors contributed to data collection: Q-jC, BL, F-yZ, X-yJ, Jq-H, H-yL, Z-yB, Z-jJ, G-fW, X-wG, HS, and J-fX. JZ and J-mQ designed the study. All authors contributed to the article and approved the submitted version.
Funding
This study was funded by the National Key Research and Development Program of China (grant no. 2017YFC1309300) and National Innovative Research Team of High-level Local Universities in Shanghai and the Shanghai Top-Priority Clinical Key Disciplines Construction Project (2017ZZ02013).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The following study centers and investigators participated in the study and contributed in screening and recruitment of patients. Study centers and investigators:
1. Central Hospital of Jiading District, Shanghai; Investigator: Chun-lin Tu
2. Tongji Hospital of Tongji University; Investigator: Qiang Chen
3. Shanghai Eastern Hepatobiliary Surgery Hospital; Investigator: Ji-quan Chen
4. Huadong Hospital, Fudan University; Investigator: Jin Gong
5. Central Hospital of Jingan District, Shanghai; Investigator: Hui-fang Cao
6. 411 Hospital of the people's Liberation Army of China; Investigator: Yi Li
7. Central Hospital of Fengxian District, Shanghai; Investigator: Li-wen Lu
8. Xinhua Hospital, Shanghai Jiao Tong University, School of Medicine; Investigator: Lin Song
9. Shanghai Punan Hospital of Pudong New District; Investigator: Yun-feng Zhao
10. Changhai Hospital, The Second Military Medical University; Investigator: Yi Huang
11. Shanghai Eighth People's Hospital, Jiangsu University; Investigator: De-jie Chu
12. Central Hospital of Putuo District, Shanghai, Shanghai University of Traditional Chinese Medicine; Investigator: Xiong-biao Wang
13. Central Hospital of Xuhui District, Shanghai, Fudan University; Investigator: Rong-huan Yu
14. Shuguang Hospital, Shanghai University of Traditional Chinese Medicine; Investigator: Meng Sun.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcimb.2020.538005/full#supplementary-material
References
Aaron, S. D. (2014). Management and prevention of exacerbations of COPD. BMJ 349:g5237. doi: 10.1136/bmj.g5237
Azoulay, E., Timsit, J. F., Tafflet, M., de Lassence, A., Darmon, M., Zahar, J. R., et al. (2006). Candida colonization of the respiratory tract and subsequent pseudomonas ventilator-associated pneumonia. Chest 129, 110–117. doi: 10.1378/chest.129.1.110
Bassetti, M., Molinari, M. P., Mussap, M., Viscoli, C., and Righi, E. (2013). Candidaemia in internal medicine departments: the burden of a rising problem. Clin. Microbiol. Infect. 19, 281–284. doi: 10.1111/1469-0691.12155
Cai, B. Q., Cai, S. X., Chen, R. C., Cui, L. Y., Feng, Y. L., Gu, Y. T., et al. (2014). Expert consensus on acute exacerbation of chronic obstructive pulmonary disease in the People's Republic of China. Int. J. Chron. Obstruct. Pulmon. Dis. 9, 381–395. doi: 10.2147/COPD.S58454
Chowdhary, A., Agarwal, K., Kathuria, S., Gaur, S. N., Randhawa, H. S., and Meis, J. F. (2014). Allergic bronchopulmonary mycosis due to fungi other than Aspergillus: a global overview. Crit. Rev. Microbiol. 40, 30–48. doi: 10.3109/1040841X.2012.754401
De Pascale, G., and Antonelli, M. (2014). Candida colonization of respiratory tract: to treat or not to treat, will we ever get an answer? Intensive Care Med. 40, 1381–1384. doi: 10.1007/s00134-014-3364-y
De Rosa, F. G., Corcione, S., Filippini, C., Raviolo, S., Fossati, L., Montrucchio, C., et al. (2015). The Effect on mortality of fluconazole or echinocandins treatment in candidemia in internal medicine wards [corrected]. PLoS ONE 10:e0125149. doi: 10.1371/journal.pone.0125149
Delisle, M. S., Williamson, D. R., Perreault, M. M., Albert, M., Jiang, X., and Heyland, D. K. (2008). The clinical significance of Candida colonization of respiratory tract secretions in critically ill patients. J. Crit. Care 23, 11–17. doi: 10.1016/j.jcrc.2008.01.005
Dong-xing, Y., Rui-lan, C., and Xiao-jiang, T. (2016). Study on the relationship between respiratory colonization of Candida spp. and bacterial ventilator? associated Pneumonia. Chin. J. Pract. Int. Med. 36, 493–495.
Eggimann, P., Garbino, J., and Pittet, D. (2003). Epidemiology of Candida species infections in critically ill non-immunosuppressed patients. Lancet Infect. Dis. 3, 685–702. doi: 10.1016/S1473-3099(03)00801-6
Garnacho-Montero, J., Olaechea, P., Alvarez-Lerma, F., Alvarez-Rocha, L., Blanquer, J., Galvan, B., et al. (2013). Epidemiology, diagnosis and treatment of fungal respiratory infections in the critically ill patient. Rev. Esp. Quimioter 26, 173–188.
GOLD (2019). Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. Technical Report, Global Initiative for Chronic Obstructive Lung Disease.
Hamet, M., Pavon, A., Dalle, F., Pechinot, A., Prin, S., Quenot, J. P., et al. (2012). Candida spp. airway colonization could promote antibiotic-resistant bacteria selection in patients with suspected ventilator-associated pneumonia. Intensive Care Med. 38, 1272–1279. doi: 10.1007/s00134-012-2584-2
Harriott, M. M., and Noverr, M. C. (2009). Candida albicans and Staphylococcus aureus form polymicrobial biofilms: effects on antimicrobial resistance. Antimicrob. Agents Chemother. 53, 3914–3922. doi: 10.1128/AAC.00657-09
Hii, I. M., Chang, H. L., Lin, L. C., Lee, Y. L., Liu, Y. M., Liu, C. E., et al. (2015). Changing epidemiology of candidemia in a Medical Center in middle Taiwan. J. Microbiol. Immunol. Infect. 48, 306–315. doi: 10.1016/j.jmii.2013.08.017
Jha, B. J., Dey, S., Tamang, M. D., Joshy, M. E., Shivananda, P. G., and Brahmadatan, K. N. (2006). Characterization of Candida species isolated from cases of lower respiratory tract infection. Kathmandu Univ. Med. J. 4, 290–294.
Liu, H., and Su-Rong, F. U. (2015). Fungal infection types and infection/colonization status in lower respiratory tract of patients at respiratory medicine. Pract. J. Clin. Med. 12, 90–92.
Mear, J. B., Kipnis, E., Faure, E., Dessein, R., Schurtz, G., Faure, K., et al. (2013). Candida albicans and Pseudomonas aeruginosa interactions: more than an opportunistic criminal association? Med. Mal. Infect. 43, 146–151. doi: 10.1016/j.medmal.2013.02.005
Morales, D. K., and Hogan, D. A. (2010). Candida albicans interactions with bacteria in the context of human health and disease. PLoS Pathog 6:e1000886. doi: 10.1371/journal.ppat.1000886
Olaechea, P. M., Palomar, M., Leon-Gil, C., Alvarez-Lerma, F., Jorda, R., Nolla-Salas, J., et al. (2004). Economic impact of Candida colonization and Candida infection in the critically ill patient. Eur. J. Clin. Microbiol. Infect. Dis. 23, 323–330. doi: 10.1007/s10096-004-1104-x
Peters, B. M., Jabra-Rizk, M. A., Scheper, M. A., Leid, J. G., Costerton, J. W., and Shirtliff, M. E. (2010). Microbial interactions and differential protein expression in Staphylococcus aureus-Candida albicans dual-species biofilms. FEMS Immunol. Med. Microbiol. 59, 493–503. doi: 10.1111/j.1574-695X.2010.00710.x
Pfaller, M. A., and Diekema, D. J. (2007). Epidemiology of invasive candidiasis: a persistent public health problem. Clin. Microbiol. Rev. 20, 133–163. doi: 10.1128/CMR.00029-06
Ricard, J. D., and Roux, D. (2012). Candida colonization in ventilated ICU patients: no longer a bystander! Intensive Care Med. 38, 1243–1245. doi: 10.1007/s00134-012-2587-z
Roux, D., Gaudry, S., Dreyfuss, D., El-Benna, J., de Prost, N., Denamur, E., et al. (2009a). Candida albicans impairs macrophage function and facilitates Pseudomonas aeruginosa pneumonia in rat. Crit. Care Med. 37, 1062–1067. doi: 10.1097/CCM.0b013e31819629d2
Roux, D., Gaudry, S., Ear, L. K., Denamur, E., Dreyfuss, D., and Ricard, J. (2009b). Candida albicans airway colonization favors bacterial Pneumonia. Am. J. Resp. Critic. Care Med. 201:A3269. doi: 10.1164/ajrccm-conference.2009.179.1_MeetingAbstracts.A3269
Sethi, S., and Murphy, T. F. (2008). Infection in the pathogenesis and course of chronic obstructive pulmonary disease. N. Engl. J. Med. 359, 2355–2365. doi: 10.1056/NEJMra0800353
Shirtliff, M. E., Peters, B. M., and Jabra-Rizk, M. A. (2009). Cross-kingdom interactions: Candida albicans and bacteria. FEMS Microbiol. Lett. 299, 1–8. doi: 10.1111/j.1574-6968.2009.01668.x
Terraneo, S., Ferrer, M., Martin-Loeches, I., Esperatti, M., Di Pasquale, M., Giunta, V., et al. (2016). Impact of Candida spp. isolation in the respiratory tract in patients with intensive care unit-acquired pneumonia. Clin. Microbiol. Infect. 22, 94:e1-94.e8. doi: 10.1016/j.cmi.2015.09.002
Wang, H. A. A. A. (2017). Global, regional, and national under-5 mortality, adult mortality, age-specific mortality, and life expectancy, 1970-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 390, 1084–1150. doi: 10.1016/S0140-6736(17)31833-0
Wedzicha, J. A., and Seemungal, T. A. (2007). COPD exacerbations: defining their cause and prevention. Lancet 370, 786–796. doi: 10.1016/S0140-6736(07)61382-8
Williamson, D. R., Albert, M., Perreault, M. M., Delisle, M. S., Muscedere, J., Rotstein, C., et al. (2011). The relationship between Candida species cultured from the respiratory tract and systemic inflammation in critically ill patients with ventilator-associated Pneumonia. Can. J. Anaesth. 58, 275–284. doi: 10.1007/s12630-010-9439-5
Keywords: acute exacerbation of chronic obstructive pulmonary disease (AECOPD), prognosis, Candida, recurrence of AECOPD, mortality
Citation: Zuo Y-h, Wang W-q, Chen Q-j, Liu B, Zhang F-y, Jin X-y, Hang J-q, Li H-y, Bao Z-y, Jie Z-j, Wang G-f, Gao X-w, Sun H, Xu J-f, Zhang J and Qu J-m (2020) Candida in Lower Respiratory Tract Increases the Frequency of Acute Exacerbation of Chronic Obstructive Pulmonary Disease: A Retrospective Case-Control Study. Front. Cell. Infect. Microbiol. 10:538005. doi: 10.3389/fcimb.2020.538005
Received: 18 May 2020; Accepted: 02 September 2020;
Published: 30 September 2020.
Edited by:
Anuradha Chowdhary, University of Delhi, IndiaReviewed by:
Aylin Dögen, Mersin University, TurkeyLudmila Baltazar, Federal University of Minas Gerais, Brazil
Copyright © 2020 Zuo, Wang, Chen, Liu, Zhang, Jin, Hang, Li, Bao, Jie, Wang, Gao, Sun, Xu, Zhang and Qu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jing Zhang, aHV4aXpoYW5namluZ0Bmb3htYWlsLmNvbQ==; Jie-ming Qu, am1xdTA5MDZAMTYzLmNvbQ==
†These authors share first authorship
 Yi-hui Zuo
Yi-hui Zuo Wei-qin Wang2,3†
Wei-qin Wang2,3† He Sun
He Sun Jing Zhang
Jing Zhang Jie-ming Qu
Jie-ming Qu