- Department of Neurobiology, Care Sciences and Society, Division of Neurogeriatrics, Center for Alzheimer Research, Karolinska Institutet, Stockholm, Sweden
Alzheimer’s disease (AD) is a neurodegenerative disorder clinically characterized by progressive decline of memory and cognitive functions, and it is the leading cause of dementia accounting for 60%–80% of dementia patients. A pathological hallmark of AD is the accumulation of aberrant protein/peptide aggregates such as extracellular amyloid plaques containing amyloid-beta peptides and intracellular neurofibrillary tangles composed of hyperphosphorylated tau. These aggregates result from the failure of the proteostasis network, which encompasses protein synthesis, folding, and degradation processes. Autophagy is an intracellular self-digesting system responsible for the degradation of protein aggregates and damaged organelles. Impaired autophagy is observed in most neurodegenerative disorders, indicating the link between autophagy dysfunction and these diseases. A massive accumulation of autophagic vacuoles in neurons in Alzheimer’s brains evidences autophagy impairment in AD. Modulating autophagy has been proposed as a therapeutic strategy for AD because of its potential to clear aggregated proteins. However, autophagy modulation therapy for AD is not yet clinically available. This mini-review aims to summarize clinical studies testing potential autophagy modulators for AD and to evaluate their proximity to clinical use. We accessed clinicaltrials.gov provided by the United States National Institutes of Health to identify completed and ongoing clinical trials. Additionally, we discuss the limitations and challenges of these therapies.
1 Introduction
Alzheimer’s disease (AD) is a neurodegenerative disorder clinically characterized by progressive impairment of memory and cognitive functions (Panza et al., 2019; Knopman et al., 2021). AD is the most common cause of dementia accounting for 60%–80% of dementia patients (Alzheimer’s disease facts and figures, 2024). The number of patients with dementia has been increasing over the years, which is estimated to be more than 55 million people worldwide today and 150 million people by 2050 (Collaborators, 2022). AD is pathologically characterized by the accumulation of aberrant protein and peptide aggregation including extracellular amyloid plaques containing amyloid-beta (Aβ) peptides and intracellular neurofibrillary tangles (NFTs) composed of hyperphosphorylated tau. Aβ peptides are secreted to the extracellular space as a consequence of sequential enzymatic cleavages of a type-1 membrane protein, amyloid precursor protein (APP), by β- and γ-secretases (Panza et al., 2019). Tau is a microtubule-associated protein that stabilizes microtubules in the axons of neurons under physiological conditions. In pathological conditions, tau undergoes abnormal posttranslational modifications, such as acetylation and hyperphosphorylation, leading to the formation of aggregated tau (Knopman et al., 2021). These protein aggregates are caused by the failure of the proteostasis network, consisting of protein synthesis, folding, and degradation processes.
Proteasomes and lysosomes are the two major protein-degrading systems in the cells. In general, proteasomes degrade short-lived and soluble misfolded proteins, whereas lysosomes degrade long-lived and insoluble aggregated proteins (Zhao et al., 2022). Autophagy is a part of the lysosomal degrading system and is impaired in most neurodegenerative disorders including AD. Autophagy is categorized into three diverse types: microautophagy, macroautophagy, and chaperone-mediated autophagy (CMA) (Wang et al., 2023). Microautophagy is a process which incorporates cytosolic components into late endosomes or lysosomes by invagination (Kuchitsu and Taguchi, 2024). Macroautophagy starts with the formation of a double membrane vacuole called autophagosome. Cytosolic components including aggregated proteins and damaged organelles are sequestered by the autophagosome and degraded by fusion of the autophagosome and lysosome (Figure 1). In CMA, cytosolic proteins with KFERQ-like motifs (Lys-Phe-Glu-Arg-Gln) bind a chaperone protein, the heat shock cognate protein of 71 kDa (Hsc70). Target proteins are unfolded and taken into the lysosomal lumen through a multimeric complex known as lysosome-associated membrane protein 2A (LAMP2A) (Valdor and Martinez-Vicente, 2024; Kaushik and Cuervo, 2018). Macroautophagy is the most well-studied type of autophagy in the context of AD, hence we will focus on macroautophagy and is hereafter referred to as autophagy. Neurons have a unique autophagic process because of their highly polarized cell shape. Autophagosomes are formed not only in neuronal cell bodies but also in distal axons. Thus, autophagosomes need to be transported on microtubules along axons to the soma by the dynein-dynactin motor machinery (Hill and Colón-Ramos, 2020) (Figure 1). During its retrograde transport, autophagosomes fuse with late endosomes to form amphisomes and with lysosomes to form autolysosomes, leading to the gradual acidification of autophagosomes. Non-dividing cells including neurons are heavily dependent on autophagy for protein homeostasis because these cells cannot dilute toxic aggregates by proliferation as opposed to dividing cells. In addition, synapses are extremely dynamic structures requiring a constant remodelling that involves both protein degradation including autophagy and synthesis of new proteins (Bai et al., 2024).

Figure 1. Overview of the autophagic process in neurons. (1) Several signaling pathways, including mTOR and AMPK, regulate the ULK1 complex, which initiates membrane nucleation and phagophore formation. (2, 3) The phagophore elongates into a closed double-membranous structure called an autophagosome. (4) The autophagosome is transported along microtubules to the neuronal soma. (5) The autophagosome fuses with the lysosome, paving the way for the degradation of the autophagosomal content.
2 Autophagy impairment in Alzheimer's disease
In 1964, several electron microscopy studies firstly described an accumulation of dense bodies around Aβ plaques in AD brain (Bubis and Luse, 1964; Terry et al., 1964; Kidd, 1964). Following this finding, extensive research has revealed a significant impairment of autophagy in AD, indicated by an accumulation of autophagic vacuoles (AVs) in neurons in both postmortem AD brains and AD mouse model brains. (Nixon et al., 2005; Yu et al., 2005; Jiang et al., 2022; Naia et al., 2023). Three different causes of autophagy impairment in AD are proposed so far; 1) altered autophagy initiation, 2) inhibition of AV transport, and 3) impairment of AV degradation caused by lysosomal dysfunction. The impairment of autophagy is most likely caused by a combination of these mechanisms, and the alteration of the autophagy system may differ depending on the stage of the disease.
2.1 Altered autophagy initiation
The expression of Beclin-1, a component of one of the autophagy initiator complexes (Figure 1), is downregulated in moderate to severe AD brains (Pickford et al., 2008). In addition, a reduction of mRNA levels of core autophagy machinery for autophagosome formation including the Beclin-1 gene (BECN1) was reported in the hippocampus of AD brains, suggesting decreased initiation of autophagy as an explanation of autophagy inhibition in AD brains (Lachance et al., 2019). Recently, Tumurbaatar et al., revealed that the protein levels of autophagy-related genes (ATGs) including Beclin-1 are reduced in postmortem hippocampal samples of AD patients, whereas these protein levels are preserved in non-demented individuals with AD neuropathology (Tumurbaatar et al., 2023). On the other hand, others reported that negative and positive regulators of autophagy flux are downregulated and upregulated, respectively, in the entorhinal cortex of AD patients (Lipinski et al., 2010). Concordantly, an increased autophagy initiation in hippocampal neurons of AD brains was also reported (Bordi et al., 2016). Thus, the alteration of autophagy initiation in AD brains is still under discussion.
2.2 Inhibition of AV transport
A disruption of the interaction between amphisomes and dynein complexes was shown in an AD transgenic mouse model (Tammineni et al., 2017). Aβ oligomers interact with amphisomes and inhibit the recruitment of amphisomes by dynein, which leads to its accumulation in axons. Since tau is involved in the stabilization of microtubules and axonal transport under physiological conditions, a destabilization of microtubules caused by dissociation of hyperphosphorylated tau may also lead to the impairment of autophagosome transport in AD (Wang et al., 2015).
2.3 Impairment of AV degradation
Lysosomal dysfunction has been suggested in human AD brains and the brains of AD mouse models. An early upregulation of lysosomal protein cathepsin D levels is observed in AD brains (Cataldo et al., 1995). Presenilin-1 (PS1) is the catalytic subunit of γ-secretase which is the key enzyme in Aβ production from APP. Mutations have been found in more than 100 sites of PS1 in familial AD (FAD), which may increase the Aβ42 to Aβ40 ratio and lead to Aβ plaque depositions. In addition to the role of PS1 in Aβ plaque formation, Lee JH et al., showed its essential function for lysosomal acidification (Lee et al., 2015). Recently, the same group revealed that failed acidification of autolysosomes caused by lowered vATPase activity leads to autolysosome accumulation in AD transgenic mouse models (Lee et al., 2022).
3 Autophagy-targeting therapy for Alzheimer's disease
Since autophagy is severely impaired in AD and plays an important role in aggregated protein clearance, the modulation of autophagic activities has been proposed as therapeutics for AD (Menzies et al., 2017; Liu and Li, 2019; Festa et al., 2021; Zhang et al., 2021). In this review, we will focus on autophagy-targeting AD therapies under evaluation in clinical studies to summarize how close autophagy-targeting therapies are to clinical use. We used ClinicalTrials.gov, a clinical research registry provided by the United States National Institutes of Health, to identify completed and ongoing clinical trials with potential autophagy modulators for AD therapies.
3.1 The mammalian target of rapamycin inhibitors
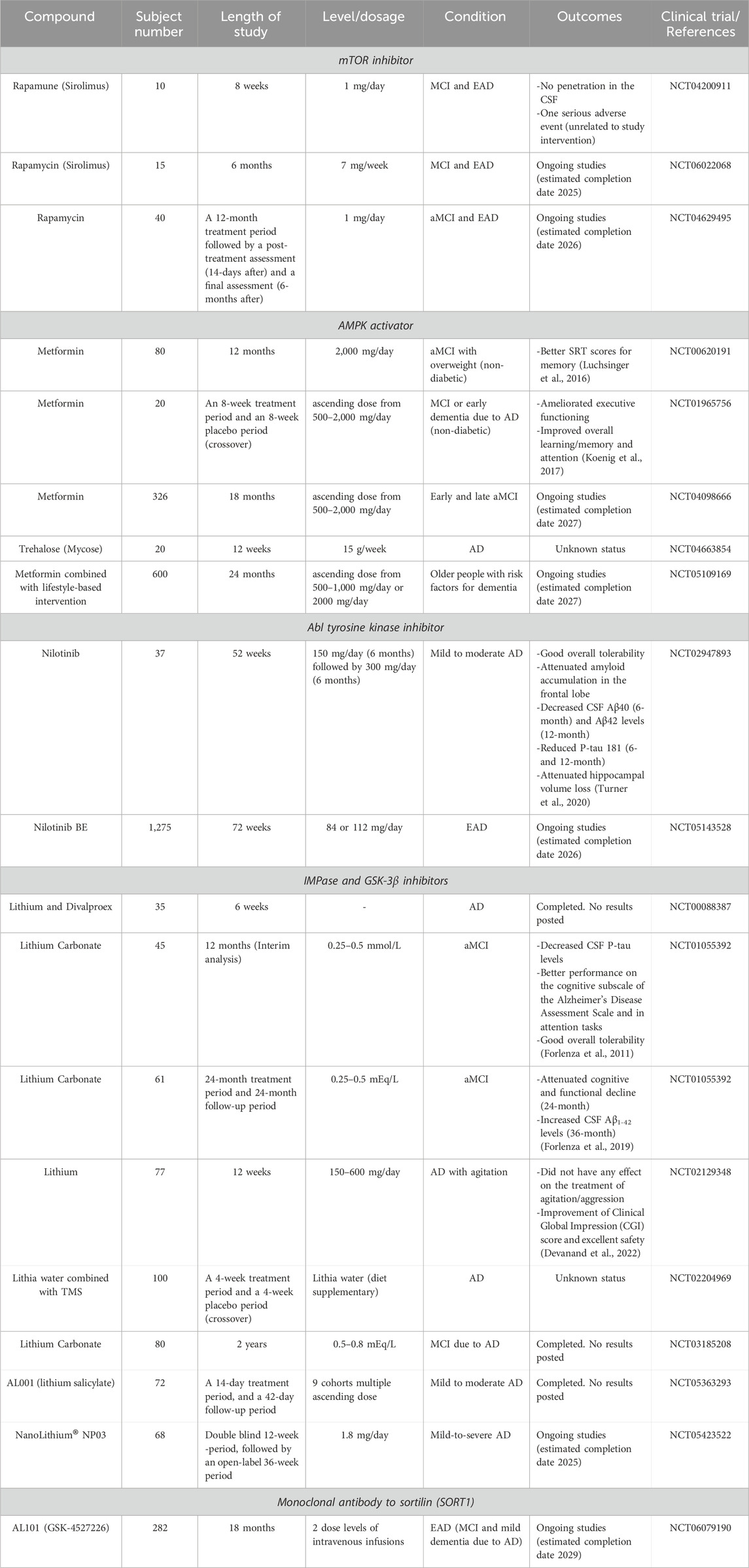
The mammalian target of rapamycin (mTOR) inhibitors including rapamycin, and its analogues are the most intensively investigated autophagy activators. mTOR consists of two different complexes, mTOR complex 1 (mTORC1) and complex 2 (mTORC2). The mTORC1 suppresses autophagy through the inhibition of unc-51-like autophagy activating kinase 1 (ULK1) complex which is a key enzyme complex for autophagy initiation in cells (Figure 1), and therefore inhibition of mTORC1 induces activation of autophagy (Panwar et al., 2023). Rapamycin supplemented in food improved memory function, and reduced Aβ42 and phosphorylated tau levels in AD mouse models at an early stage of pathology development. On the other hand, these effects were no longer observed when rapamycin was administered at a later stage characterized by prominent Aβ plaques and tau tangles (Caccamo et al., 2010; Spilman et al., 2010; Majumder et al., 2011). One early Phase I study was performed to measure rapamycin concentration in the cerebrospinal fluid (CSF) and evaluate the feasibility and safety of rapamycin treatment in a small number of mild cognitive impairment (MCI) or early AD patients (NCT04200911, Table 1). Sixteen adverse events are reported, including one serious adverse event, a possible transient ischemic attack (ITA), which was however unrelated to the study intervention. Two clinical trials of rapamycin treatment for AD are ongoing (NCT04629495, NCT06022068). These are Phase II and Phase I/II studies targeting amnestic MCI (aMCI) and early-stage AD.
3.2 Adenosine monophosphate-activated protein kinase activators
Adenosine monophosphate-activated protein kinase (AMPK) is another autophagy regulator thoroughly investigated. AMPK induces autophagy by direct phosphorylation of ULK1. AMPK also negatively regulates mTOR activity, leading to the activation of autophagy (Figure 1). Metformin and resveratrol are AMPK activators and their potential for AD therapy has been assessed in AD mouse models such as APP/PS1 mice (Chen et al., 2021; Vingtdeux et al., 2010; Zhao et al., 2023). These experiments using AD mouse models showed that AMPK activators reduced Aβ and tau pathologies. Metformin is used as a treatment for type 2 Diabetes Mellitus and is under investigation for AD prevention. Two small Phase II studies of metformin were performed in MCI or mild dementia AD patients (NCT00620191, NCT01965756). In the study conducted at Columbia University, the metformin-treated group showed significantly greater improvement in the score of the Selective Reminding Test for memory compared with the placebo group (Luchsinger et al., 2016). The second clinical study found a significantly better score in the Trails B executive function test by metformin treatment compared to placebo (Koenig et al., 2017). Currently, the placebo-controlled Phase II/III study is ongoing in early or late MCI subjects (NCT04098666). In addition, a Phase II study is recruiting elderly adults at risk for dementia to assess the preventive effects of a combination of metformin and lifestyle intervention on changes in cognition (NCT05109169) (Barbera et al., 2024). Although metformin induces autophagy through the activation of AMPK, it is unclear to what extent autophagy activation contributes to the improvement of memory functions due to additional effects of metformin including modulation of BACE1 expression levels, neuroinflammation, and glucose metabolism (Liao et al., 2022). It is worth noting that a recent study using an AD mouse model showed that metformin treatment increased Aβ plaque formation and phospho-tau levels and caused memory impairment (Cho et al., 2024). Therefore, further assessment of metformin for AD treatment is needed. The disaccharide trehalose potentially activates autophagy through AMPK-dependent and independent mechanisms. Trehalose mimics a starvation condition by blocking the glucose transporter family, leading to the activation of AMPK (Mardones et al., 2016; DeBosch et al., 2016). Trehalose also induces the nuclear translocation of transcription factor EB, which is a central regulator of autophagic-lysosomal protein expression (Rusmini et al., 2019). Inconsistently, some in vitro studies using cell models showed that trehalose inhibits the autophagosome degradation step rather than activating autophagy, raising the question of whether trehalose is an autophagy activator (Yoon et al., 2017; Tien et al., 2016). Although data from different in vitro studies have shown controversial effects of trehalose on autophagy, studies using AD animal models showed that trehalose treatment reduced Aβ levels and tau aggregation and ameliorated cognitive impairment, suggesting neuroprotective effects of trehalose (Perucho et al., 2012; Schaeffer et al., 2012; Du et al., 2013; Portbury et al., 2017). A randomized Phase I study was conducted to evaluate the effectiveness of trehalose in reducing AD symptoms with 20 AD patients (NTC04663854).
3.3 Nilotinib
Nilotinib is a tyrosine kinase inhibitor approved for the treatment of chronic myelogenous leukaemia by the FDA. Nilotinib selectively inhibits the autophosphorylation of Bcr-Abl, which increases parkin-Beclin-1 interaction leading to autophagic vacuole clearance. In addition, nilotinib successfully reduced Aβ plaque load in Tg-SwDI mice (Lonskaya et al., 2013; Lonskaya et al., 2014). A small Phase II study was conducted to assess the safety and tolerability of nilotinib and changes in AD biomarkers in mild to moderate AD patients (NTC02947893). Aβ40 and Aβ42 levels in the CSF were reduced in the nilotinib-treated group compared to the placebo group at 6- and 12-months, respectively. Additionally, phospho-tau 181 levels were reduced in the nilotinib-treated group at 6- and 12-months (Turner et al., 2020). Currently, the efficacy and safety of nilotinib bioequivalent are being evaluated in a Phase III study in early AD patients (NTC05143528).
3.4 Lithium
Lithium is also a potential autophagy-activating medication which has already been approved for the treatment of manic episodes and bipolar disorder by the FDA (Shen et al., 2024). Li+ replaces Mg2+ at the binding site of Mg2+-dependent enzymes, thus Li+ inhibits the activity of multiple enzymes including inositol monophosphatase (IMPase), Akt/b-arrestin-2, and glycogen synthase kinase-3β (GSK-3β) (Puglisi-Allegra et al., 2023). Autophagy is activated through the inhibition of IMPase leading to the reduction of free inositol-1, 4, 5-triphosphate (IP3) levels (Sarkar et al., 2005). Multiple clinical studies of lithium have been conducted to assess its effect on memory and cognitive function as well as on behavioural and psychiatric symptoms of dementia (BPSD) in AD (Table 1). Despite that several clinical studies have shown beneficial effects of lithium on AD and aMCI patients, there is a limitation of lithium usage especially in elderly people because of its narrow therapeutic index, and high risk of side effects and toxicity (Murphy et al., 2023). To overcome this problem, currently, two new types of lithium medication for AD are under evaluation in clinical studies. NanoLithium is composed of lithium citrate and a water-in-oil microemulsion drug delivery system, being transported by lipoproteins into the cytoplasm of cells through lipoprotein receptors. By using this drug delivery system, NanoLithium achieved pharmacological activity at lower doses compared with classical lithium treatments (Guilliot et al., 2024). In animal model studies, NanoLithium rescued memory function in early- and late-stage AD rat models (Guilliot et al., 2024; Wilson et al., 2017). A Phase II proof-of-concept clinical study is being conducted since 2022 (NCT05423522). AL001 is another approach of lithium delivery by using ionic cocrystals of lithium salicylate with organic anions. The safety and maximum tolerated dose of AL001 are under evaluation in a Phase I/IIa study (NCT05363293). The previous study was completed in 2023, but the results have not been posted on ClinicalTrials.gov yet.
3.5 A monoclonal antibody to improve lysosomal function
As previously mentioned, lysosomal dysfunction in AD brains is one of the causes of autophagy impairment. Thus, the improvement of lysosomal function is another approach for autophagy activation. Progranulin (PGRN) is a secreted protein acting as an autocrine and paracrine neurotrophic factor which regulates neuronal survival, axonal growth, and neuroinflammation (Rhinn et al., 2022; Boylan et al., 2023). PGRN also regulates lysosomal function by acting as a chaperone for lysosomal enzymes including cathepsin D. Heterozygous loss-of-function PGRN gene (GRN) mutations cause frontotemporal lobar degeneration (FTLD) with accumulation of transactivation response DNA-binding protein 43 (TDP-43) by reducing more than 50% of PGRN protein levels. In addition, a link between PGRN and AD has been suggested: several mutations in GRN were found in AD patients (Kelley et al., 2010; Cortini et al., 2008; Brouwers et al., 2007). A meta-analysis showed an increased risk of AD associated with the single-nucleotide polymorphism (SNP) rs5848 in the GRN gene, which leads to a reduction in PGRN protein levels in the plasma, CSF, and brain tissue (Nicholson et al., 2014; Rademakers et al., 2008). PGRN is degraded via entering the lysosome via its clearance receptor, sortilin. GSK4527226, a monoclonal antibody against sortilin, blocks the binding between sortilin and PGRN which increases PGRN levels in the brain. A Phase II study evaluating the efficacy and safety of GSK4527226 is ongoing in early AD patients (NCT06079190).
4 Discussion
Since autophagy is involved in both Aβ and tau metabolism and has close bearings to neurodegeneration, it may serve as a potential therapeutic target for AD. Although several potential autophagy modulators are under evaluation in clinical studies for MCI and AD patients, the specificity of these treatments remains unclear. For example, mTOR is a protein kinase contributing to multiple cellular functions including glucose and lipid metabolism, nucleotide biogenesis, and protein biogenesis (Panwar et al., 2023). In addition, targeting such a multifunctional protein with a small compound which can affect the whole body may cause unfavourable effects. This risk could be reduced with drug delivery systems that pass the blood-brain barrier (BBB) and target specific cells including neurons and microglia, hence increasing therapeutic efficacy and leading to lower exposure to other organs (Wu et al., 2023; Guo et al., 2020). Another challenge for the development of autophagy modulators is the lack of autophagy biomarkers evaluating autophagy activity in vivo. Currently available autophagy assays for in vitro and in vivo research are based on direct detection of autophagic proteins in tissues by using antibodies or expression of exogenous autophagy flux reporter genes such as RFP-GFP-LC3 (Mizushima and Murphy, 2020). However, none of them are suitable for detecting autophagy activity in human brains. Without reliable biomarkers to evaluate autophagy activity in the human brain, the development of AD therapeutics targeting autophagy is impossible. A positron emission tomography (PET) tracer detecting a specific autophagy substrate could be an approach for autophagy biomarkers (Mizushima and Murphy, 2020). Another possibility is the detection of autophagic proteins in the CSF. Changes in autophagic protein levels, such as LC3 and p62, have been reported in CSF from patients with neurodegenerative disorders (Youn et al., 2018; Rubino et al., 2022). However, the relationship between these protein levels in the CSF and autophagy activity in the brain remains unclear. Extensive research has revealed a significant impairment of autophagy in AD and highlighted the importance of functional autophagy in clearing aggregated proteins, making autophagy a promising target for AD therapeutics. However, it is still unclear how much autophagy activation contributes to the therapeutic effect in the therapies currently being investigated in clinical trials, because most treatments have multiple mode of actions. Identifying autophagy modulators with higher specificity, i.e., compounds that specifically target the different steps of autophagy; initiation, transport and clearance, and biomarkers assessing autophagy activation in vivo may accelerate the development of autophagy targeting therapeutics for AD.
Author contributions
SF: Writing–original draft, Writing–review and editing. JM: Writing–review and editing. PN: Funding acquisition, Writing–review and editing. MS: Conceptualization, Funding acquisition, Writing–original draft, Writing–review and editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. We are grateful for financial support from: Hållsten Research Foundation, Swedish Research Council, Swedish Brain Foundation, Torsten Söderberg Foundation, Sonja Leikrans donation, The Erling-Persson Family Foundation, the Swedish Alzheimer Foundation, Gun and Bertil Stohnes Foundation, the Strategic Research Program in Neuroscience (StratNeuro), TOYOBO biotechnology foundation, Lindhés Advokatbyrå AB, Åhlén foundation, Stiftelsen För Gamla Tjänarinnor, Demensfonden, Loo and Hans Osterman Foundation, Foundation for Geriatric Diseases, Karolinska Institutet Research Foundation, and by the private initiative Innovative ways to fight Alzheimer´s disease - Leif Lundblad Family and others.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that Generative AI was used in the creation of this manuscript. The authors used Generative AI to verify English grammar.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Alzheimer's disease facts and figures (2024). Alzheimer's disease facts and figures. Alzheimers Dement. 20(5):3708–3821. doi:10.1002/alz.13809
Bai, I., Keyser, C., Zhang, Z., Rosolia, B., Hwang, J.-Y., Zukin, R. S., et al. (2024). Epigenetic regulation of autophagy in neuroinflammation and synaptic plasticity. Front. Immunol. 15, 1322842. doi:10.3389/fimmu.2024.1322842
Barbera, M., Lehtisalo, J., Perera, D., Aspö, M., Cross, M., De Jager Loots, C. A., et al. (2024). A multimodal precision-prevention approach combining lifestyle intervention with metformin repurposing to prevent cognitive impairment and disability: the MET-FINGER randomised controlled trial protocol. Alzheimer's Res. and Ther. 16 (1), 23. doi:10.1186/s13195-023-01355-x
Bordi, M., Berg, M. J., Mohan, P. S., Peterhoff, C. M., Alldred, M. J., Che, S., et al. (2016). Autophagy flux in CA1 neurons of Alzheimer hippocampus: increased induction overburdens failing lysosomes to propel neuritic dystrophy. Autophagy 12 (12), 2467–2483. doi:10.1080/15548627.2016.1239003
Boylan, M. A., Pincetic, A., Romano, G., Tatton, N., Kenkare-Mitra, S., and Rosenthal, A. (2023). Targeting progranulin as an immuno-neurology therapeutic approach. Int. J. Mol. Sci. 24 (21), 15946. doi:10.3390/ijms242115946
Brouwers, N., Nuytemans, K., Jvd, Z., Gijselinck, I., Engelborghs, S., Theuns, J., et al. (2007). Alzheimer and Parkinson diagnoses in progranulin null mutation carriers in an extended founder family. Archives neurology 64 (10), 1436–1446. doi:10.1001/archneur.64.10.1436
Bubis, J. J., and Luse, S. A. (1964). An electron microscopic study of experimental allergic encephalomyelitis in the rat. Am. J. Pathol. 44 (2), 299–317.
Caccamo, A., Majumder, S., Richardson, A., Strong, R., and Oddo, S. (2010). Molecular interplay between mammalian target of rapamycin (mTOR), amyloid-beta, and Tau: effects on cognitive impairments. J. Biol. Chem. 285 (17), 13107–13120. doi:10.1074/jbc.M110.100420
Cataldo, A. M., Barnett, J. L., Berman, S. A., J Li, S. Q., Bursztajn, S., Lippa, C., et al. (1995). Gene expression and cellular content of cathepsin D in Alzheimer's disease brain: evidence for early up-regulation of the endosomal-lysosomal system. Neuron 14 (3), 671–680. doi:10.1016/0896-6273(95)90324-0
Chen, Y., Zhao, S., Fan, Z., Li, Z., Zhu, Y., Shen, T., et al. (2021). Metformin attenuates plaque-associated tau pathology and reduces amyloid-β burden in APP/PS1 mice. Alzheimer's Res. and Ther. 13 (1), 40. doi:10.1186/s13195-020-00761-9
Cho, S. Y., Kim, E. W., Park, S. J., Phillips, B. U., Jeong, J., Kim, H., et al. (2024). Reconsidering repurposing: long-term metformin treatment impairs cognition in Alzheimer’s model mice. Transl. Psychiatry 14 (1), 34. doi:10.1038/s41398-024-02755-9
Collaborators, G. D. F. (2022). Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: an analysis for the Global Burden of Disease Study 2019. Lancet Public Health 7 (2), e105–e125. doi:10.1016/S2468-2667(21)00249-8
Cortini, F., Fenoglio, C., Guidi, I., Venturelli, E., Pomati, S., Marcone, A., et al. (2008). Novel exon 1 progranulin gene variant in Alzheimer’s disease. Eur. J. neurology 15 (10), 1111–1117. doi:10.1111/j.1468-1331.2008.02266.x
DeBosch, B. J., Heitmeier, M. R., Mayer, A. L., Higgins, C. B., Crowley, J. R., Kraft, T. E., et al. (2016). Trehalose inhibits solute carrier 2A (SLC2A) proteins to induce autophagy and prevent hepatic steatosis. Sci. Signal. 9 (416), ra21–ra. doi:10.1126/scisignal.aac5472
Devanand, D. P., Crocco, E., Forester, B. P., Husain, M. M., Lee, S., Vahia, I. V., et al. (2022). Low dose lithium treatment of behavioral complications in Alzheimer's disease: lit-AD randomized clinical trial. Am. J. geriatric psychiatry 30 (1), 32–42. doi:10.1016/j.jagp.2021.04.014
Du, J., Liang, Y., Xu, F., Sun, B., and Wang, Z. (2013). Trehalose rescues Alzheimer's disease phenotypes in APP/PS1 transgenic mice. J. Pharm. Pharmacol. 65 (12), 1753–1756. doi:10.1111/jphp.12108
Festa, B. P., Barbosa, A. D., Rob, M., and Rubinsztein, D. C. (2021). The pleiotropic roles of autophagy in Alzheimer's disease: from pathophysiology to therapy. Curr. Opin. Pharmacol. 60, 149–157. doi:10.1016/j.coph.2021.07.011
Forlenza, O. V., Diniz, B. S., Radanovic, M., Santos, F. S., Talib, L. L., and Gattaz, W. F. (2011). Disease-modifying properties of long-term lithium treatment for amnestic mild cognitive impairment: randomised controlled trial. Br. J. Psychiatry 198 (5), 351–356. doi:10.1192/bjp.bp.110.080044
Forlenza, O. V., Radanovic, M., Talib, L. L., and Gattaz, W. F. (2019). Clinical and biological effects of long-term lithium treatment in older adults with amnestic mild cognitive impairment: randomised clinical trial. Br. J. Psychiatry 215 (5), 668–674. doi:10.1192/bjp.2019.76
Guilliot, S., Wilson, E. N., Touchon, J., and Soto, M. E. (2024). Nanolithium, a new treatment approach to Alzheimer’s disease: a review of existing evidence and clinical perspectives. J. Prev. Alzheimer's Dis. 11 (2), 428–434. doi:10.14283/jpad.2024.26
Guo, Q., Xu, S., Yang, P., Wang, P., Lu, S., Sheng, D., et al. (2020). A dual-ligand fusion peptide improves the brain-neuron targeting of nanocarriers in Alzheimer's disease mice. J. Control. Release 320, 347–362. doi:10.1016/j.jconrel.2020.01.039
Hill, S. E., and Colón-Ramos, D. A. (2020). The journey of the synaptic autophagosome: a cell biological perspective. Neuron 105 (6), 961–973. doi:10.1016/j.neuron.2020.01.018
Jiang, R., Shimozawa, M., Mayer, J., Tambaro, S., Kumar, R., Abelein, A., et al. (2022). Autophagy impairment in app knock-in Alzheimer’s model mice. Front. Aging Neurosci. 14, 878303. doi:10.3389/fnagi.2022.878303
Kaushik, S., and Cuervo, A. M. (2018). The coming of age of chaperone-mediated autophagy. Nat. Rev. Mol. Cell. Biol. 19 (6), 365–381. doi:10.1038/s41580-018-0001-6
Kelley, B. J., Haidar, W., Boeve, B. F., Baker, M., Shiung, M., Knopman, D. S., et al. (2010). Alzheimer disease–like phenotype associated with the c.154delA mutation in progranulin. Archives neurology 67 (2), 171–177. doi:10.1001/archneurol.2010.113
Kidd, M. (1964). Alzheimer’s disease—an electron microscopical study. Brain 87 (2), 307–320. doi:10.1093/brain/87.2.307
Knopman, D. S., Amieva, H., Petersen, R. C., Chételat, G., Holtzman, D. M., Hyman, B. T., et al. (2021). Alzheimer disease. Nat. Rev. Dis. Prim. 7 (1), 33. doi:10.1038/s41572-021-00269-y
Koenig, A. M., Mechanic-Hamilton, D., Xie, S. X., Combs, M. F., Cappola, A. R., Xie, L., et al. (2017). Effects of the insulin sensitizer metformin in alzheimer disease: pilot data from a randomized placebo-controlled crossover study. Alzheimer Dis. Assoc. Disord. 31 (2), 107–113. doi:10.1097/WAD.0000000000000202
Kuchitsu, Y., and Taguchi, T. (2024). Lysosomal microautophagy: an emerging dimension in mammalian autophagy. Trends Cell. Biol. 34 (7), 606–616. doi:10.1016/j.tcb.2023.11.005
Lachance, V., Wang, Q., Sweet, E., Choi, I., Cai, C.-Z., Zhuang, X.-X., et al. (2019). Autophagy protein NRBF2 has reduced expression in Alzheimer’s brains and modulates memory and amyloid-beta homeostasis in mice. Mol. Neurodegener. 14, 43. doi:10.1186/s13024-019-0342-4
Lee, J.-H., McBrayer, M. K., Wolfe, D. M., Mitchell, C. H., Lloyd-Evans, E., Nixon, R. A., et al. (2015). Presenilin 1 maintains lysosomal Ca2+ homeostasis via TRPML1 by regulating vATPase-mediated lysosome acidification. Cell. Rep. 12 (9), 1430–1444. doi:10.1016/j.celrep.2015.07.050
Lee, J.-H., Yang, D.-S., Goulbourne, C. N., Im, E., Stavrides, P., Pensalfini, A., et al. (2022). Faulty autolysosome acidification in Alzheimer's disease mouse models induces autophagic build-up of Aβ in neurons, yielding senile plaques. Nat. Neurosci. 25 (6), 688–701. doi:10.1038/s41593-022-01084-8
Liao, W., Xu, J., Li, B., Ruan, Y., Li, T., and Liu, J. (2022). Deciphering the roles of metformin in Alzheimer’s disease: a snapshot. Front. Pharmacol. 12, 728315. doi:10.3389/fphar.2021.728315
Lipinski, M. M., Zheng, B., Lu, T., Yan, Z., Py, B. F., Ng, A., et al. (2010). Genome-wide analysis reveals mechanisms modulating autophagy in normal brain aging and in Alzheimer's disease. Proc. Natl. Acad. Sci. U. S. A. 107 (32), 14164–14169. doi:10.1073/pnas.1009485107
Liu, J., and Li, L. (2019). Targeting autophagy for the treatment of Alzheimer’s disease: challenges and opportunities. Front. Mol. Neurosci. 12, 203. doi:10.3389/fnmol.2019.00203
Lonskaya, I., Hebron, M. L., Desforges, N. M., Franjie, A., and Moussa, C. E. H. (2013). Tyrosine kinase inhibition increases functional parkin-B eclin-1 interaction and enhances amyloid clearance and cognitive performance. EMBO Mol. Med. 5 (8), 1247–1262. doi:10.1002/emmm.201302771
Lonskaya, I., Hebron, M. L., Desforges, N. M., Schachter, J. B., and Moussa, C. E.-H. (2014). Nilotinib-induced autophagic changes increase endogenous parkin level and ubiquitination, leading to amyloid clearance. J. Mol. Med. 92, 373–386. doi:10.1007/s00109-013-1112-3
Luchsinger, J. A., Perez, T., Chang, H., Mehta, P., Steffener, J., Pradabhan, G., et al. (2016). Metformin in amnestic mild cognitive impairment: results of a pilot randomized placebo controlled clinical trial. J. Alzheimer's Dis. JAD. 51 (2), 501–514. doi:10.3233/JAD-150493
Majumder, S., Richardson, A., Strong, R., and Oddo, S. (2011). Inducing autophagy by rapamycin before, but not after, the formation of plaques and tangles ameliorates cognitive deficits. PloS one 6 (9), e25416. doi:10.1371/journal.pone.0025416
Mardones, P., Rubinsztein, D. C., and Hetz, C. (2016). Mystery solved: trehalose kickstarts autophagy by blocking glucose transport. Sci. Signal 9 (416), fs2. doi:10.1126/scisignal.aaf1937
Menzies, F. M., Fleming, A., Caricasole, A., Bento, C. F., Andrews, S. P., Ashkenazi, A., et al. (2017). Autophagy and neurodegeneration: pathogenic mechanisms and therapeutic opportunities. Neuron 93 (5), 1015–1034. doi:10.1016/j.neuron.2017.01.022
Mizushima, N., and Murphy, L. O. (2020). Autophagy assays for biological discovery and therapeutic development. Trends Biochem. Sci. 45 (12), 1080–1093. doi:10.1016/j.tibs.2020.07.006
Murphy, N., Redahan, L., and Lally, J. (2023). Management of lithium intoxication. BJPsych Adv. 29 (2), 82–91. doi:10.1192/bja.2022.7
Naia, L., Shimozawa, M., Bereczki, E., Li, X., Liu, J., Jiang, R., et al. (2023). Mitochondrial hypermetabolism precedes impaired autophagy and synaptic disorganization in App knock-in Alzheimer mouse models. Mol. psychiatry 28 (9), 3966–3981. doi:10.1038/s41380-023-02289-4
Nicholson, A. M., Finch, N. A., Thomas, C. S., Wojtas, A., Rutherford, N. J., Mielke, M. M., et al. (2014). Progranulin protein levels are differently regulated in plasma and CSF. Neurology 82 (21), 1871–1878. doi:10.1212/WNL.0000000000000445
Nixon, R. A., Wegiel, J., Kumar, A., Yu, W. H., Peterhoff, C., Cataldo, A., et al. (2005). Extensive involvement of autophagy in Alzheimer disease: an immuno-electron microscopy study. J. Neuropathol. Exp. Neurol. 64 (2), 113–122. doi:10.1093/jnen/64.2.113
Panwar, V., Singh, A., Bhatt, M., Tonk, R. K., Azizov, S., Raza, A. S., et al. (2023). Multifaceted role of mTOR (mammalian target of rapamycin) signaling pathway in human health and disease. Signal Transduct. Target. Ther. 8 (1), 375. doi:10.1038/s41392-023-01608-z
Panza, F., Lozupone, M., Logroscino, G., and Imbimbo, B. P. (2019). A critical appraisal of amyloid-β-targeting therapies for Alzheimer disease. Nat. Rev. Neurol. 15 (2), 73–88. doi:10.1038/s41582-018-0116-6
Perucho, J., Casarejos, J., Gomez, A., Solano, M., Garcia de Yebenes, J. A., and Mena, M. (2012). Trehalose protects from aggravation of amyloid pathology induced by isoflurane anesthesia in APPswe mutant mice. Curr. Alzheimer Res. 9 (3), 334–343. doi:10.2174/156720512800107573
Pickford, F., Masliah, E., Britschgi, M., Lucin, K., Narasimhan, R., Jaeger, P. A., et al. (2008). The autophagy-related protein beclin 1 shows reduced expression in early Alzheimer disease and regulates amyloid beta accumulation in mice. J. Clin. Investigation 118 (6), 2190–2199. doi:10.1172/JCI33585
Portbury, S. D., Hare, D. J., Sgambelloni, C., Perronnes, K., Portbury, A. J., Finkelstein, D. I., et al. (2017). Trehalose improves cognition in the transgenic Tg2576 mouse model of Alzheimer’s disease. J. Alzheimer's Dis. 60 (2), 549–560. doi:10.3233/JAD-170322
Puglisi-Allegra, S., Lazzeri, G., Busceti, C. L., Giorgi, F. S., Biagioni, F., and Fornai, F. (2023). Lithium engages autophagy for neuroprotection and neuroplasticity: translational evidence for therapy. Neurosci. and Biobehav. Rev. 148, 105148. doi:10.1016/j.neubiorev.2023.105148
Rademakers, R., Eriksen, J. L., Baker, M., Robinson, T., Ahmed, Z., Lincoln, S. J., et al. (2008). Common variation in the miR-659 binding-site of GRN is a major risk factor for TDP43-positive frontotemporal dementia. Hum. Mol. Genet. 17 (23), 3631–3642. doi:10.1093/hmg/ddn257
Rhinn, H., Tatton, N., McCaughey, S., Kurnellas, M., and Rosenthal, A. (2022). Progranulin as a therapeutic target in neurodegenerative diseases. Trends Pharmacol. Sci. 43 (8), 641–652. doi:10.1016/j.tips.2021.11.015
Rubino, E., Boschi, S., Roveta, F., Marcinnò, A., Cermelli, A., Vigliani, M. C., et al. (2022). Investigating p62 concentrations in cerebrospinal fluid of patients with dementia: a potential autophagy biomarker in vivo? Brain Sci. 12 (10), 1414. doi:10.3390/brainsci12101414
Rusmini, P., Cortese, K., Crippa, V., Cristofani, R., Cicardi, M. E., Ferrari, V., et al. (2019). Trehalose induces autophagy via lysosomal-mediated TFEB activation in models of motoneuron degeneration. Autophagy 15 (4), 631–651. doi:10.1080/15548627.2018.1535292
Sarkar, S., Floto, R. A., Berger, Z., Imarisio, S., Cordenier, A., Pasco, M., et al. (2005). Lithium induces autophagy by inhibiting inositol monophosphatase. J. Cell. Biol. 170 (7), 1101–1111. doi:10.1083/jcb.200504035
Schaeffer, V., Lavenir, I., Ozcelik, S., Tolnay, M., Winkler, D. T., and Goedert, M. (2012). Stimulation of autophagy reduces neurodegeneration in a mouse model of human tauopathy. Brain 135 (7), 2169–2177. doi:10.1093/brain/aws143
Shen, Y., Zhao, M., Zhao, P., Meng, L., Zhang, Y., Zhang, G., et al. (2024). Molecular mechanisms and therapeutic potential of lithium in Alzheimer’s disease: repurposing an old class of drugs. Front. Pharmacol. 15, 1408462. doi:10.3389/fphar.2024.1408462
Spilman, P., Podlutskaya, N., Hart, M. J., Debnath, J., Gorostiza, O., Bredesen, D., et al. (2010). Inhibition of mTOR by rapamycin abolishes cognitive deficits and reduces amyloid-beta levels in a mouse model of Alzheimer's disease. PloS one 5 (4), e9979. doi:10.1371/journal.pone.0009979
Tammineni, P., Ye, X., Feng, T., Aikal, D., and Cai, Q. (2017). Impaired retrograde transport of axonal autophagosomes contributes to autophagic stress in Alzheimer's disease neurons. eLife 6, e21776. doi:10.7554/eLife.21776
Terry, R. D., Gonatas, N. K., and Weiss, M. (1964). Ultrastructural studies in Alzheimer's presenile dementia. Am. J. Pathol. 44 (2), 269–297.
Tien, N. T., Karaca, I., Tamboli, I. Y., and Walter, J. (2016). Trehalose alters subcellular trafficking and the metabolism of the Alzheimer-associated amyloid precursor protein. J. Biol. Chem. 291 (20), 10528–10540. doi:10.1074/jbc.M116.719286
Tumurbaatar, B., Fracassi, A., Scaduto, P., Guptarak, J., Woltjer, R., Jupiter, D., et al. (2023). Preserved autophagy in cognitively intact non-demented individuals with Alzheimer's neuropathology. Alzheimer's and Dementia 19 (12), 5355–5370. doi:10.1002/alz.13074
Turner, R. S., Hebron, M. L., Lawler, A., Mundel, E. E., Yusuf, N., Starr, J. N., et al. (2020). Nilotinib effects on safety, tolerability, and biomarkers in Alzheimer's disease. Ann. neurology 88 (1), 183–194. doi:10.1002/ana.25775
Valdor, R., and Martinez-Vicente, M. (2024). The role of chaperone-mediated autophagy in tissue homeostasis and disease pathogenesis. Biomedicines 12 (2), 257. doi:10.3390/biomedicines12020257
Vingtdeux, V., Giliberto, L., Zhao, H., Chandakkar, P., Wu, Q., Simon, J. E., et al. (2010). AMP-activated protein kinase signaling activation by resveratrol modulates amyloid-beta peptide metabolism. J. Biol. Chem. 285 (12), 9100–9113. doi:10.1074/jbc.M109.060061
Wang, L., Klionsky, D. J., and Shen, H.-M. (2023). The emerging mechanisms and functions of microautophagy. Nat. Rev. Mol. Cell. Biol. 24 (3), 186–203. doi:10.1038/s41580-022-00529-z
Wang, Z.-X., Tan, L., and Yu, J.-T. (2015). Axonal transport defects in Alzheimer’s disease. Mol. Neurobiol. 51, 1309–1321. doi:10.1007/s12035-014-8810-x
Wilson, E. N., Carmo, S. D., Iulita, M. F., Hall, H., Ducatenzeiler, A., Marks, A. R., et al. (2017). BACE1 inhibition by microdose lithium formulation NP03 rescues memory loss and early stage amyloid neuropathology. Transl. psychiatry 7 (8), e1190. doi:10.1038/tp.2017.169
Wu, D., Chen, Q., Chen, X., Han, F., Chen, Z., and Wang, Y. (2023). The blood–brain barrier: structure, regulation and drug delivery. Signal Transduct. Target. Ther. 8 (1), 217. doi:10.1038/s41392-023-01481-w
Yoon, Y.-S., Cho, E.-D., Jung Ahn, W., Won Lee, K., Lee, S.-J., and Lee, H.-J. (2017). Is trehalose an autophagic inducer? Unraveling the roles of non-reducing disaccharides on autophagic flux and alpha-synuclein aggregation. Cell. death and Dis. 8 (10), e3091–e. doi:10.1038/cddis.2017.501
Youn, J., Lee, S.-B., Lee, H. S., Yang, H. O., Park, J., Kim, J. S., et al. (2018). Cerebrospinal fluid levels of autophagy-related proteins represent potentially novel biomarkers of early-stage Parkinson’s disease. Sci. Rep. 8 (1), 16866. doi:10.1038/s41598-018-35376-6
Yu, W. H., Cuervo, A. M., Kumar, A., Peterhoff, C. M., Schmidt, S. D., Lee, J. H., et al. (2005). Macroautophagy--a novel Beta-amyloid peptide-generating pathway activated in Alzheimer's disease. J. Cell. Biol. 171 (1), 87–98. doi:10.1083/jcb.200505082
Zhang, Z., Yang, X., Song, Y.-Q., and Tu, J. (2021). Autophagy in Alzheimer’s disease pathogenesis: therapeutic potential and future perspectives. Ageing Res. Rev. 72, 101464. doi:10.1016/j.arr.2021.101464
Zhao, L., Zhao, J., Zhong, K., Tong, A., and Jia, D. (2022). Targeted protein degradation: mechanisms, strategies and application. Signal Transduct. Target. Ther. 7, 113. doi:10.1038/s41392-022-00966-4
Keywords: Alzheimer’s disease, protein homeostasis, autophagy modulators, clinical studies, autophagy impairment
Citation: Fernandes SM, Mayer J, Nilsson P and Shimozawa M (2025) How close is autophagy-targeting therapy for Alzheimer's disease to clinical use? A summary of autophagy modulators in clinical studies. Front. Cell Dev. Biol. 12:1520949. doi: 10.3389/fcell.2024.1520949
Received: 31 October 2024; Accepted: 16 December 2024;
Published: 08 January 2025.
Edited by:
Fumi Suomi, University of Helsinki, FinlandReviewed by:
Laura Beth McIntire, NewYork-Presbyterian, United StatesCopyright © 2025 Fernandes, Mayer, Nilsson and Shimozawa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Makoto Shimozawa, TWFrb3RvLlNoaW1vemF3YUBraS5zZQ==
 Sofia Miranda Fernandes
Sofia Miranda Fernandes Per Nilsson
Per Nilsson Makoto Shimozawa
Makoto Shimozawa