
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Cell Dev. Biol. , 13 January 2023
Sec. Stem Cell Research
Volume 11 - 2023 | https://doi.org/10.3389/fcell.2023.1007703
This article is part of the Research Topic Advancing Gene and Cell Therapy using Human Mesenchymal Stem Cells View all 9 articles
Stress urinary incontinence (SUI) adversely affects the quality of life of patients, while the currently available surgical and non-surgical therapies are not effective in all patients. Application of mesenchymal stem cells (MSCs) for regaining the ability to control urination has attracted interest. Herein, we reviewed the literature and analyzed recent studies on MSC-based therapies for SUI, summarized recent treatment strategies and their underlying mechanisms of action, while assessing their safety, effectiveness, and prospects. In addition, we traced and sorted the root literature and, from an experimental design perspective, divided the obtained results into four categories namely single MSC type therapy for SUI, MSC-based combination therapy for SUI, treatment of SUI with the MSC secretome, and other factors influencing MSC therapy. Although evidence demonstrates that the treatment strategies are safe and effective, the underlying mechanisms of action remain nebulous, hence more clinical trials are warranted. Therefore, future studies should focus on designing clinical trials of MSC-based therapies to determine the indications for treatment, cell dosage, appropriate surgical strategies, and optimal cell sources, and develop clinically relevant animal models to elucidate the molecular mechanisms underlying stem cell therapies improvement of SUI.
Stress urinary incontinence (SUI) refers to the leakage of urine during sneezing, laughing, coughing, and exercise, due to a sharp increase in intra-abdominal pressure (Hart et al., 2015). Although SUI occurs in both males and females, females are more affected (Abufaraj et al., 2021). This review focuses on female SUI. SUI affects the quality of life of females and increases the financial burden of individuals and health systems. The incidence of SUI in China, South Korea, and Nepal is 18.9% (Zhang et al., 2015), 33.6% (Shim et al., 2021), 24.1% (Chen et al., 2020), respectively. Initial treatment usually includes pelvic floor muscle training and behavioral intervention. Furthermore, bladder training, urethral inserts, and vaginal devices may also alleviate SUI. Injections of urethral bulking agents also alleviate leakage. Adipose tissue, especially MFAT (lipogems and nanofat), is common urethral bulking agents in the treatment of stress urinary incontinence in female patients. Compared with non-surgical treatments, surgical intervention provides better treatment outcome against SUI. Pubovaginal sling and colposuspension are the most effective surgical strategies (Nygaard and Heit, 2004; Silwal Gautam et al., 2014). However, surgical procedures are associated with various adverse effects. The current treatment modalities are suboptimal, as they can only alleviate the symptoms to a certain degree, without curing SUI. In addition, the incidence of urinary incontinence may increase with age, hence other treatment strategies remain warranted. With advancements in regenerative medicine, stem cells have become a focal point in life sciences research owing to their self-renewal and multidirectional differentiation properties. Stem cells are be classified as either embryonic or adult stem cells, according to their developmental stages. Adult stem cells have been previously studied; however, ethical considerations have hampered the extensive study of embryonic stem cells. Based on their differentiative potential, stem cells are divided into totipotent, pluripotent, multipotent and unipotent (Sobhani et al., 2017), of which multipotent stem cells are the current focus of research and are further categorized into hematopoietic and mesenchymal stem cells (MSCs) (Mishra et al., 2020; Figure 1). MSCs, originate from the mesoderm and ectoderm and usually reside in connective tissue and organ stroma (Zheng et al., 2021), exhibit high proliferation, self-renewal, and multidirectional differentiation properties, and display immune-regulatory, paracrine, and other functions (Dominici et al., 2006). MSCs are easily obtained from multiple sources, including the bone marrow, peripheral fat, umbilical cord blood or placenta, 64 amniotic fluid, gingiva, olfactory mucosa, and urine (Shin et al., 2020). MSCs home into injured sites and differentiate into corresponding cells, thereby replacing injured cells, in addition to secreting neurotrophic factors. Additionally, MSCs promote tissue repair by secreting bioactive factors, such as extracellular vesicle (EVs) (Cheng et al., 2020; Zheng et al., 2021), which are lipid-bound secreted by cells into the extracellular space (Zaborowski et al., 2015; Zheng et al., 2021). The three essential EV subtypes are exosomes, micro-vesicle, and apoptotic bodies, classified according to their biogenesis, release pathways, size, content, and function (Borges et al., 2013; Yanez-Mo et al., 2015; Zaborowski et al., 2015). At present, research has primarily focused on the former two. MSC- derived EVs bear varying types of molecules involved in intercellular communication, immune response, homeostasis, coagulation, inflammation, angiogenesis, and antigen presentation (Harrell et al., 2019; Zhao et al., 2020).
Stem cells have been extensively used in medicine; the multilineage differentiation potential and immune modulatory properties of MSCs make them a promising treatment option for various clinical conditions. Previous phase III trials have provided evidence for the effectiveness and safety of MSCs. MSCs have been used in the treatment and prevention of graft-versus-host disease (NCT03106662), mandible fractures (NCT02755922), severe coronavirus disease 2019 (NCT05122234), retinitis pigmentosa (NCT04224207), and inherited retinal dystrophy (NCT04224207). Therapeutic indications of stem cells for SUI are its high prevalence and chronic nature (Shin et al., 2020). Although the number of studies on MSC-based therapy for SUI is limited, such research is critical for addressing urinary control that affects the quality of life of many females globally. Here, we summarize and analyze relevant literature published over the past 10 years, outlining the mechanisms underlying MSC-based therapies in SUI treatment and the latest advances in this field.
The multidirectional differentiation potential of MSCs has been suggested to play a role in SUI treatment. Therefore, previous studies have used single MSCs to treat SUI in animal models to validate this hypothesis; Table 1 lists the features of various single MSC therapies for SUI. For example, Kim et al. (2012) investigated the effect of human amniotic fluid stem cells (hAFSCs) using an animal model with SUI that underwent bilateral pudendal nerve transection. The authors found that hAFSCs can differentiate into muscle progenitor cells when cultured in myogenic induction media, and therefore hypothesized that the grafted hAFSC underwent myogenic differentiation in situ, potentially inducing the regeneration of the host muscle. In addition, the level of neurogenic gene expression in animals with hAFSCs was substantially higher than in those without, suggesting that their injection can exert positive physiological effects on nerve regeneration and the re-formation neuromuscular junctions (Figure 2).
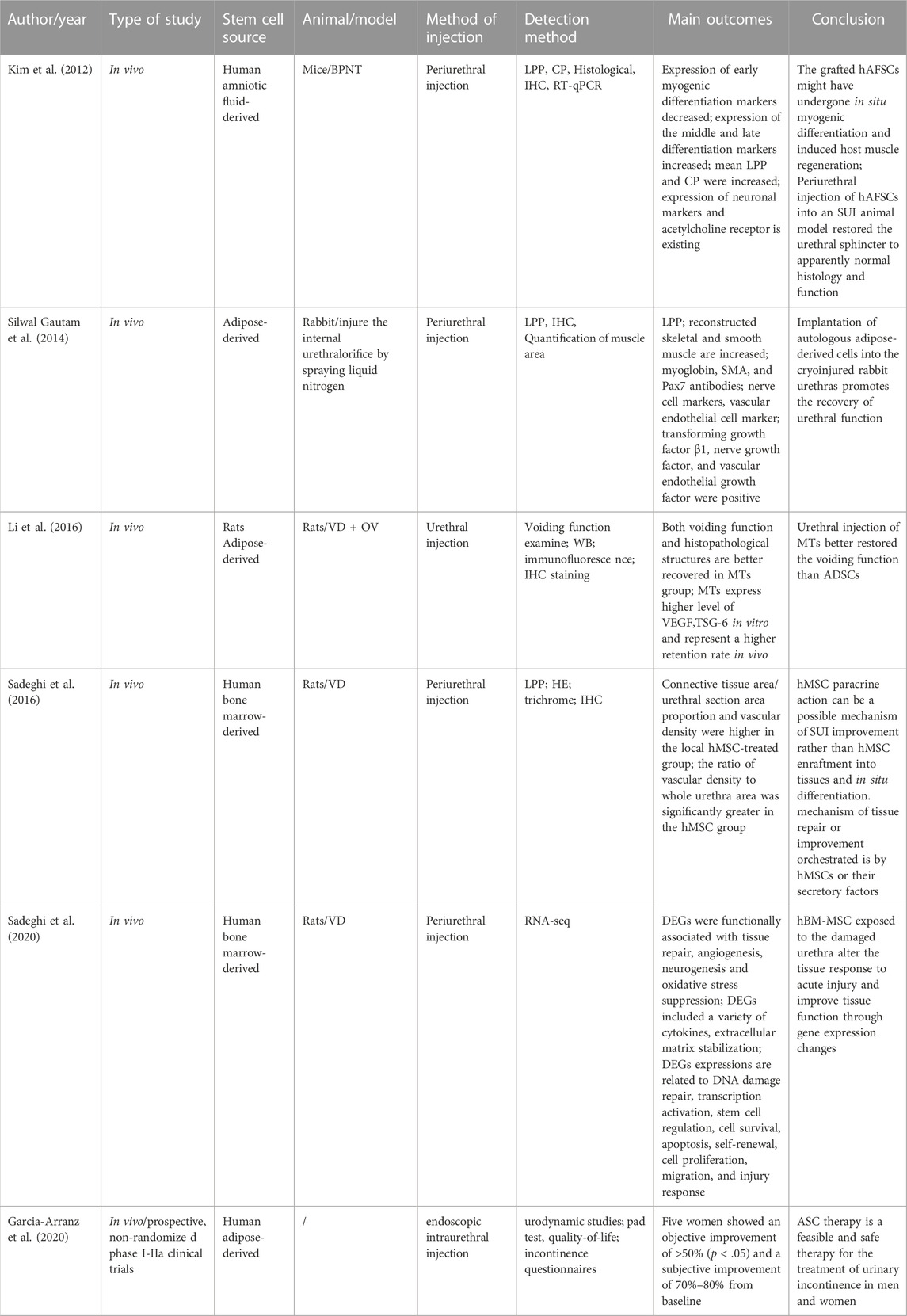
TABLE 1. Study characteristics dealing with Single type of MSC therapy for stress urinary incontinence.
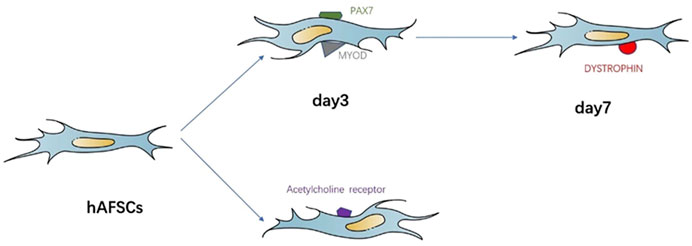
FIGURE 2. Simplified representation of the MSCs in myogenic differentiation and neurogenic differentiation.
In another study, Silwal Gautam et al., 2014 investigated the use of injected autologous adipose-derived stem cells (ADSCs) into cryoinjured rabbit urethras injured by spraying liquid nitrogen for 20 s to simulate SUI. Autologous ADSCs were transplanted 7 days post injury and urinary function was assessed 14 days later. The authors observed that the leak point pressure in the cell-implanted group was substantially higher than that in the cell-free control group. In addition, immunohistochemical examination demonstrated that the reconstructed skeletal and smooth muscle areas were significantly more developed in the cell-implanted regions than control regions. The implanted ADSCs were immunohistochemically positive for skeletal muscle, such as myoglobin, smooth muscle actin, and paired box 7 antibodies, smooth muscle, myoblast progenitor cells, and nerve cell markers (tubulin β3, calcium-binding protein P, vascular endothelial cell markers, and von Willebrand factor). In addition, some implanted cells were positive for the transforming growth factor β1, nerve growth factor, and vascular endothelial growth factor. The authors concluded that the autologous ADSC therapy for the cryoinjured rabbit urethras worked via a comprehensive effect involving myogenic differentiation, neuronal regeneration, neoangiogenesis, and bulking effects (Figure 3).
The adipose tissue is the most practical cell source used to treat female urinary incontinence. Li et al. (2016) sought to improve the efficacy of ADSCs to treat a SUI rat model that underwent vagina dilation followed by bilateral ovariectomy. The authors used the hanging drop method to transform ADSCs into microtissues (MTs), which showed better recovery in terms of voiding function and histopathological structure compared to the ADSC group. In vitro, the authors also found that MTs expressed higher levels of vascular endothelial growth factor and TNFα-stimulated genes/proteins, supporting the higher retention rates observed in vivo and concluded that the therapeutic effect of urethral injection of MTs was superior to that of ADSCs in SUI rats.
Although the feasibility of single MSC therapy for SUI has been recognized, the mechanism of actions has been explained in diverse ways. For example, Sadeghi et al. (2016) found no evidence to support the hypothesis that human MSCs (hMSCs) differentiated into muscle cells after injection in midurethral tissue samples of rats with SUI. Instead, the authors speculated that the paracrine action of hMSCs could be the underlying mechanism of SUI remission. Furthermore, the vascular density of the entire urethral area in the hMSCs-treated group was greater than that in the control group. This suggests that the mechanism of action of the hMSCs, or their secretory factors, involves the induction of vascular preservation or neovascularization in the acutely injured tissue. Interestingly, the study illustrated that the injured urethral tissue did not exhibit prominent inflammatory cell infiltration following hMSC injection, which differed from the findings of Grinnemo et al.’s (2006) of massive macrophage infiltration following hMSC transplantation. Reasons for the different outcomes might be attributed to the cell source, the culture environment in vitro, and the type of receptors. To test the hypothesis that long-term paracrine effects of hMSCs reduce inflammatory responses and modulate a healing microenvironment, Sadeghi et al. (2020) performed the first all-round transcriptomic analysis of hMSC therapy for postpartum SUI. The authors observed various differentially expressed genes in the injured urethra treated with hMSCs related to several signaling pathways involved in tissue regeneration and repair, such as wound healing, vasoprotection, angiogenesis, neurogenesis, and neuroprotection as well as oxidative stress inhibition. Data on the immunomodulatory mechanisms underlying MSC therapy for SUI are limited, hence this new resource provides momentous transcriptomic information on the interaction of hMSCs and injured tissue for identifying potential therapeutic targets for postpartum SUI therapy and prevention.
Two prospective, non-randomized phases I–II a clinical trials have reported that stem cell-based SUI therapy provides acceptable functional results with minimal complications or side effects in female patients (Garcia-Arranz et al., 2020). However, a small number of clinical trials have previously analyzed and compared the results, hence the overall data are not sufficient for assessing the long-term safety of the treatment.
Although the feasibility of MSC therapy for SUI has been demonstrated (Kim et al., 2012; Silwal Gautam et al., 2014; Sadeghi et al., 2016; Garcia-Arranz et al., 2020; Sadeghi et al., 2020), MSCs alone may be insufficient to regenerate whole urethral components. Table 2 lists the features of MSC-based combination therapies for SUI. One limitation of MSC therapy is the low survival rate of MSCs in injured urethral tissue following local engraftment (Kean et al., 2013). Bioactive molecules or biomaterials could enhance the survival and integration of the transplanted cells (Hart et al., 2015). Intravenous injection of MSCs has been reported to lower survival rates since most of were trapped in the lungs and other organs (Acosta et al., 2015). MSCs express diverse unique chemokine receptors that are likely to play a key role in their engraftment (Honczarenko et al., 2006); among them, the chemokine/chemokine receptor axis, C-C motifligand 7 (CCL7)/C-C motif receptor 1 (CCR1), is involved in the recruitment process of MSCs in urethral and vaginal tissues following postpartum injury (Huang et al., 2010). Jiang et al. (2020) injected modified bone marrow-derived MSCs to overexpress CCR1 into SUI rats through the tail vein, along with 2 μg of the active CCL7 peptide around the urethra. The rats showed the highest rate of successfully transplanted MSCs in the injured tissue and level of functional recovery of SUI when compared with the control groups. However, the authors examined the transplantation rate and urethral recovery of MSCs only 1 week after the rats had been injured during childbirth, and therefore did not consider the long-term outcomes.
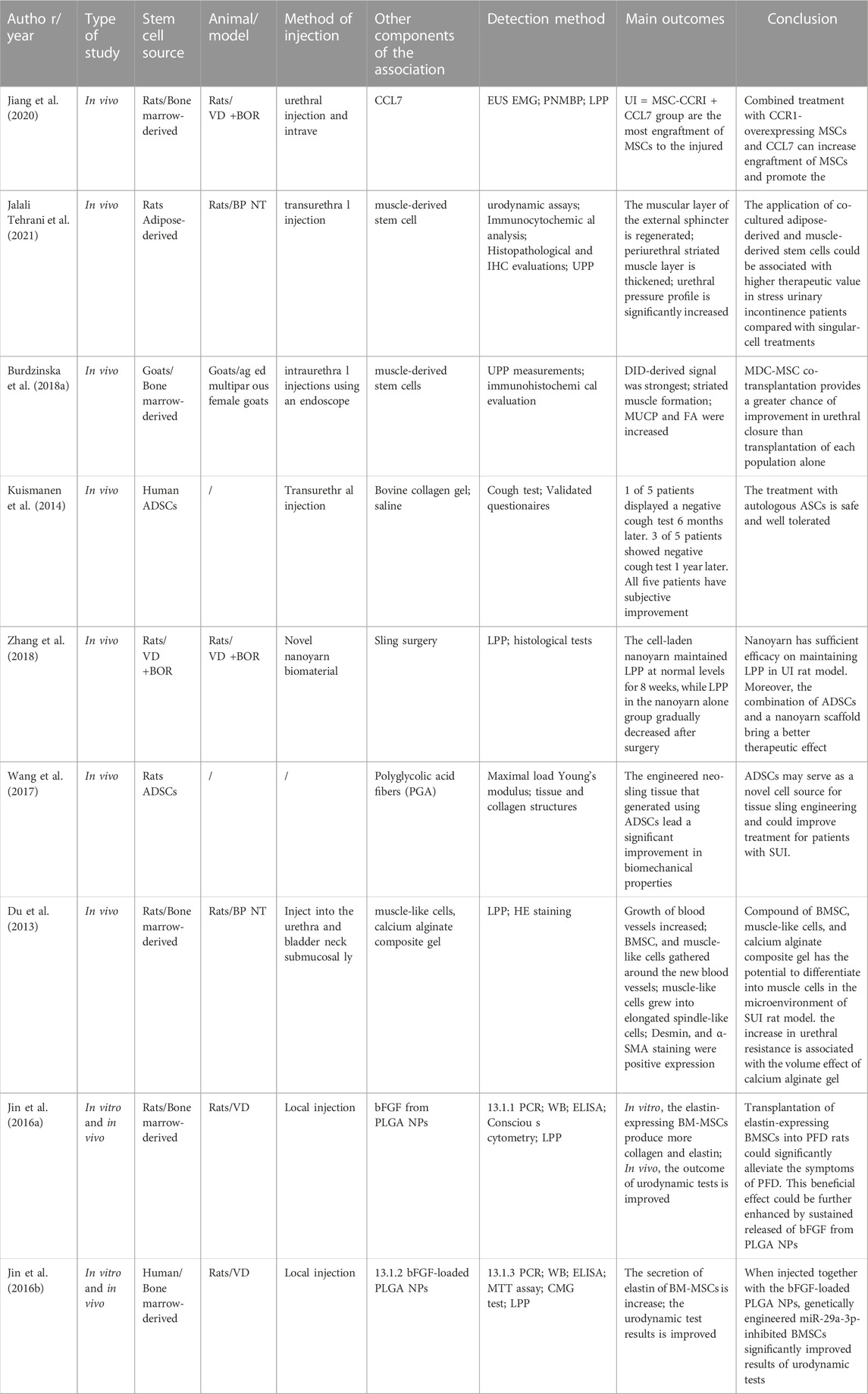
TABLE 2. Study characteristics dealing with MSC based combination therapy for stress urinary incontinence.
Previous studies have attempted to combine MSCs from two different sources to enhance their efficacy of SUI treatment. For instance, Jalali Tehrani et al., 2021 used muscle-derived stem cells (MDSCs), ADSCs, and a combination of the two types of stem cells to treat an animal SUI model that underwent bilateral pudendal nerve transection surgery. The authors found that the urethral pressure curve in the group with the combined two types of stem cells was higher than that of the remaining groups, and showed a thicker periurethral striated muscle layer than those of the groups with only one type of stem cell. The authors suggested that it is beneficial for the recovery of the urethral sphincter function to locally inject stem cells into the urethra and that the therapeutic outcome is amplified when combining two types of stem cells, and finally hypothesized that the application of co-cultured stem cells could enhance therapeutic effects due to the more comprehensive environment of cytokines and paracrine factors.
Similar results have been reported by Burdzinska et al., 2018a, who conducted a study on aged multiparous female goats and found that the co-transplantation of MSCs and MDSCs was more effective than cell therapy alone. However, the underlying mechanism of the increased efficacy of MSC-MDSC co-engraftment remains unclear. The authors concluded that MDSCs enhanced the myogenic activity of MSCs, and that the latter increased the survival rate of the former via paracrine action. The results are consistent with their previous report on soluble factors secreted by MSCs that enhanced the fusion index of myoblasts (Kulesza et al., 2016).
In recent years, significant progress has been made in the field of tissue engineering, particularly in seed cells, scaffold materials, and organization building. Kuismanen et al. (2014) have assessed the effectiveness and safety of autologous adipose stem cells (ASCs) in treating female stress urinary incontinence and, using the cough test, found that following treatment of 5 SUI patients with ASCs combined with bovine collagen gel and saline, one patient tested negative 6 months later, while and three tested negative after 1 year. Besides, the authors also observed some subjective improvement in all five patients. This was the first study to describe the use of autologous ASCs in combination with collagen gel for female SUI treatment and illustrate the safety and well-tolerance of the autologous ASCs-based therapy.
Calcium alginate gel is a mature tissue-engineering scaffolding material. Du et al. (2013) demonstrated that calcium alginate composite gels, bone marrow-derived mesenchymal stem cells (BMSCs), and muscle-like cells could differentiate into muscle cells in an SUI rat model. Hematoxylin-eosin staining showed that desmin, a cytoskeletal intermediate-filament protein and α-skeletal muscle actin were expressed in the tissue, suggesting the regeneration of smooth and striated muscle cells. In the authors assessed urethral function and identified a strong relationship between an increase in urethral resistance and volume effects of calcium alginate gel.
Furthermore, factors such as optimal alginate gel porosity, optimal combination ratio of gel, muscle-like cells, and stem cells are closely associated with cell proliferation and muscle fiber formation (Du et al., 2013). Overall, transplanting seed cells and scaffold material is a promising therapeutic strategy whose safety and efficacy have been demonstrated. Non-etheless, long term studies are lacking, albeit necessary, to obtain evidence to support MSC-based combination therapy.
To limit adverse foreign body reactions induced by non-absorbable materials, previous studies have attempted to use combination of mesenchymal stem cells and biomaterials for SUI to enhance the biocompatibility of materials. Among them, adipose tissue is the most commonly used source of mesenchymal stem cells and its safety and therapeutic effect have also been verified. Zhang et al. (2018) have developed a new nanoyarn biomaterial via a dynamic liquid electrospinning system to apply nanoyarn as a urinary sling. The authors combined nanoyarn with adipose-derived stem cells (ADSCs) and observed that the LPP in the nanoyarn alone group gradually descended, while the cell-laden nanoyarn maintained LPP at normal levels for 8 weeks. The authors suggested that combination of ADSCs and a nanoyarn scaffold is effective to maintain normal LPP in urinary incontinence rat model, which provides a potentially novel strategy to treat female SUI. The implantation of suburethral sling is an effective therapy for SUI. Wang et al. (2017) have attempted to overcome the inherent limitations of suburethral sling implantation by seeding ADSCs used in treating female stress urinary incontinence on polyglycolic acid (PGA) fibers, which generated a neo-scaffold with a shape mimicking a sling complex. The engineered neo-sling tissue displayed a significant improvement in biomechanical properties, which increased the treatment efficacy against SUI.
SUI is a type of pelvic floor dysfunction (PFD), characterized by connective tissue abnormalities and alterations of elastin metabolism. In a rat model, Jin et al., 2016a studied the effects of stem cell-based, elastin gene-modified, and nanoparticle-mediated multidisciplinary therapy against pelvic floor tissues under PFD. Elastin-overexpressing BMSCs were transplanted into damaged tissue induced after vaginal distension. The intervention had beneficial therapeutic effects in PFD rats, where poly lactic-co- glycolic acid nanoparticles were first loaded, followed by loading of basic fibroblast growth factor to enable continuous release of the former, which enhanced the therapeutic effects of BMSCs with modified elastin gene.
Subsequently, to study other latent regulatory factors, such as microRNAs(miRs), Jin et al., 2016b broadened the scope of the therapeutic notion. miRs are a set of non-coding single-stranded RNA molecules encoded by endogenous genes with a length of approximately 22 nucleotides involved in the regulation of post-transcriptional gene expression in animals and plants. miRs can negatively regulate messenger RNAs (mRNAs) by distinguishing specific complementary sequences primarily located in the 3′-UTR of the target mRNAs, thereby either inhibiting its translation or degrading it (Ott et al., 2011). For example, the miR-29 family of miRs downregulates the expression of elastin (Sudo et al., 2015; Zhang et al., 2015). More precisely, miR-29a-3p downregulates the endogenous expression of elastin in BMSCs (Jin et al., 2016a). The inhibition of miR-29a-3p in BMSCs markedly increases the expression and secretion of elastin, consequently enhancing the therapeutic effect of BMSCs following injection into PFD rats.
Finally, although previous studies have indicated that the effects of MSCs combined with bioactivemolecules, other cell types, MSC biomaterials, or MSCs genetically modified for the treatment of SUI are superior to therapies based solely on MSCs, the cost-benefit relationships of such combinatorial therapies requires further assessment.
With recent interest in the exploitation of the paracrine effects of MSCs for SUI treatment, the MSC secretome has been increasingly analyzed, mainly in three aspects: concentrated conditioned media (CCM), exosomes, and EVs, which is also called MSC-based cell-free product. Table 3 outlines the features of SUI treatments based on the MSC secretome previously reported; Dissaranan et al. (2014) hypothesized that MSCs can home into the pelvic organs of animal models following childbirth injury, facilitating the recovery of SUI exerted by paracrine factors. To test this hypothesis, the author first demonstrated the ability of MSCs to home into affected pelvic organs of SUI rat models and validated the effectiveness of MSCs and CCM in SUI treatment by injecting MSCs intravenously, and CCM, into the periurethral tissue. The authors observed an increase in elastin near the external urethral sphincter and the formation of smooth muscles of the urethra, suggesting that MSCs can home into the vagina and urethra, and deduced that the synthesis of elastin was increased via secretion of paracrine factors, which, in turn, promoted SUI recovery (Dissaranan et al., 2014). Similarly, Deng et al. (2015) demonstrated the ability of MSCs to repair damaged tissue in dual injuries of muscles and nerves via secretion of bioactive factors. Other studies have shown that the feasibility of CCM in SUI treatment is similar to that of MSCs (Jiang et al., 2021; Zhuang et al., 2021).
To elucidate the precise mechanism of action of CCM in SUI treatment, previous studies have conducted more in-depth analysis. For instance, Liu et al. (2018) demonstrated that exosomes extracted from ADSC-CCM can regulate the metabolism of type I collagen in fibroblasts and observed that the expression levels of matrix metallopeptidase 1 (MMP1) and MMP2 in fibroblasts decreased, while those of metallopeptidase inhibitors one and three increased, when the fibroblasts were treated with exosomes secreted by ADSCs. The MMP gene family encodes different types of collagenases, enzymes that degrade collagen. Conversely, metallopeptidase inhibitors are specific inhibitors of MMPs that protect collagen against degradation. Therefore, the authors also concluded that exosomes secreted by ADSCs promote the synthesis of collagen while inhibiting its degradation, thereby enhancing the support of the periurethral tissues to the urethra (Liu et al., 2018). Exploring the active ingredients in MSC-CCM provides a theoretical basis for understanding the molecular mechanisms underlying SUI treatment with MSCs (Figure 4).
Exosomes isolated from silent mating type information regulation 2 homolog 1-overexpressing BMSCs improved symptoms in SUI rats (Li et al., 2021), and enhanced the proliferation, differentiation, and activation of stem cells. Wang et al. (2021) demonstrated that EVs from ADSCs protected against SUI through the miR-93/F3 axis. EVs secreted by ADSCs could send miR-93 to fibroblasts and downregulate the expression of coagulation factor III, thereby remolding the extracellular matrix of SUI fibroblasts. A higher expression of miR-93 was also observed in SUI primary satellite cells induced by ADSC-EVs, which directly targeted the expression of coagulation factor III and upregulated the expression of Pax7 and myogenic differentiation (Figure 5). A similar pattern was observed by Zhang et al. (2020) who found that miR-328a-3p from BMSC-derived EVs was transferred to fibroblasts and regulated the extra cellular matrix metabolism via the sirtuin 7/transforming growth factor β1 signaling pathway (Figure 6).
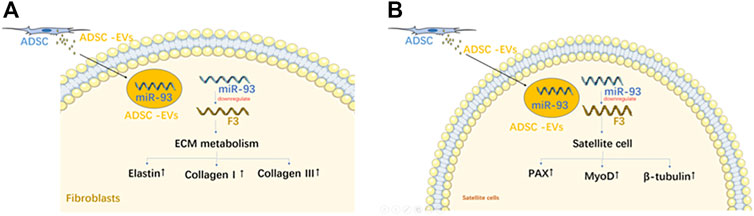
FIGURE 5. The mechanism of EVs from ADSC on fibroblasts (A); The mechanism of EVs from ADSC on satellite cell (B).
Other key factors in the stem cell field include the cell source, injection site, dose, and type of technology used. Table 4 lists aspects associated with MSC-based SUI therapy. Cui et al. (2018) directly injected MDSCs and ADSCs into the bladder and urethra of SUI rats undergone bilateral pudendal nerve transaction. Then, 0-, 15-, 30-, and 60-day post MSC implantation, the urinary voiding function was assessed using a urine dynamics detector, which showed that MDSCs andADSCs improved urination in rats with intrinsic sphincter deficiency, while the effect of MDSC-treatment was more pronounced than in the ADSC-treated groups. Myosin and α-smooth muscleactin contents in the MDSC-treated groups tended to increase. The authors found that the efficacy of MDSCs was higher than that of ADSCs. Burdzinska et al., 2018b studied the limited precision with which cell suspensions are delivered from different injection sites to the target tissues, and performed transurethral and periurethral injections of autologous MSCs in female goats and analyzed differences in their distribution in the urethra. In the periurethral group, cells located in the urethral wall accounted for 68.7% of the total number ofinjected cells, and 67.0% in the transurethral group; in addition, the average proportions of cells in the external urethral sphincter were 18.8% and 17.0%, respectively. In the transurethral injection group, the authors observed leakage of cell suspension and concluded that the precision of delivery of cells into the external sphincter of the urethra was limited regardless of the injection method used. The low efficiency of cell delivery to the external urethral sphincter and the high leakage of cell suspension are key factors that limit the effectiveness of cell therapy (Burdzinska et al., 2018a). Janssen et al. (2019) determined whether increasing the number of MSC could enhance the efficacy of stem cell therapy by injecting MSCs into SUI rat models intravenously on days 1, 7, and 14 post injury. The results showed that all dosages improved urethral integrity by restoring urethral connective tissue and neuromuscular structure. However, two and three doses of MSCs significantly improved the leak point pressure, compared with single dose. This confirms that the efficacy of MSC in the treatment of postpartum urinary incontinence and SUI is enhanced via multiple doses.
Recently, Jager et al., 2020 investigated whether a needle-free waterjet apparatus could deliver living cells under defined settings (including injection pressure, delivery volume, transportation media, and fluid velocity). The authors attempted to accurately penetrate the urothelium and connective tissue adjacent to the sphincter muscle without penetrating the latter. Waterjet injections of MSCs into isotonic cell culture medium resulted in similar or more viable cells compared with those after needle injections. By controlling the injection pressure, waterjet injections of MSCs to the urethra are faster and more accurate than needle injections, without adversely affecting cell viability Jager et al. (2020). Our study enriches existing injection technologies and will facilitate related future research.
The strategies for MSC-based SUI therapies mainly include single MSC type therapy for SUI, MSC- based combination therapy, and MSC secretome-based therapy. Previous studies have explored the optimal sources of MSCs, most suitable injection sites, dosages, and administration methods, and have demonstrated how MSCs treat SUI in terms of muscle repair and regeneration, regulation of extracellular matrix metabolism, nerve regeneration, and blood supply, which provided insights into the molecular mechanisms underlying MSC- mediated SUI treatment. In addition, the limitations of the cited studies could guide future research. Research on the potential mechanisms of action of MSC therapy for SUI in nerve regeneration and immunomodulation is currently limited. Existing studies have included small sample sizes, with animal models majorly based on small rodents, and rarely on large primates, which creates uncertainty in generalizing and applying the derived conclusions to humans. Primate models can better reflect the pathophysiology of human SUI. Only few clinical trials have been conducted, with a small number of participants and short follow-up time, therefore the long-term efficacy of MSC- based therapy for SUI remains to be evaluated. Combining MSCs with other components or approaches in SUI treatment, although promising, presents additional obstacles that deserve further study. Although multidisciplinary approaches are particularly suited for exploiting the therapeutic potential of MSCs, and their treatment strategies are promising, it is also necessary to assess their associated costs. In addition, multicenter clinical trials are warranted to extend the follow-up time and expand the number of participants to improve methodology.
In addition, the emerging MSC-based cell-free therapy has shown great superiority and broad prospects in animal experiments, however, the extraction process of MSC- based cell-free products is complex, while the amount of extraction is the most important challenge for cell-free therapy to overcome. As more MSC-based cell-free therapies are explored, MSC-based cell-free therapies will achieve new breakthroughs and have significant clinical implication.
TL performed and wrote the manuscript. JZ, XLL, WW, and XF collected the references and designed the table. WW and LW drew the figures. JZ and XCL modified the manuscript. XCL designed the manuscript and approved the final manuscript for publication. All authors read and approved the final manuscript.
This work was supported by the National Natural Science Foundation of China (Grant Number 81971365).
We would like to thank Editage (www.editage.cn) for English language editing.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcell.2023.1007703/full#supplementary-material
ADSC, adipose-derived stem cell; BMDSC, bone merrow-derived stem cell; CCM, concentrated conditioned media; EV, extracellular vesicle; hAFSC, human amniotic fluid stem cell; hMSC, human mesenchymal stem cell; MDC, muscle-derived stem cell; miR, microRNA; MMP, matrix metallopeptidase; MSC, mesenchymal stem cell; MV, microvesicle; PFD, pelvic floor dysfunction; SUI, stress urinary incontinence.
Abufaraj, M., Xu, T., Cao, C., Siyam, A., Isleem, U., Massad, A., et al. (2021). Prevalence and trends in urinary 395 incontinence among women in the United States, 2005-2018. American Journal of Obstetrics and Gynecology 225 (2), 166 e1–e12. doi:10.1016/j.ajog.2021.03.016
Acosta, S. A., Tajiri, N., Hoover, J., Kaneko, Y., and Borlongan, C. V. (2015). Intravenous bone marrow stem cell grafts preferentially migrate to spleen and abrogate chronic inflammation in stroke. Stroke 46 (9), 2616–2627. doi:10.1161/STROKEAHA.115.009854
Borges, F. T., Reis, L. A., and Schor, N. (2013). Extracellular vesicles: Structure, function, and potential clinical uses in renal diseases. Brazilian Journal of Medical and Biological Research 46 (10), 824–830. doi:10.1590/1414-431X20132964
Burdzinska, A., Dybowski, B., Zarychta-Wisniewska, W., Kulesza, A., Butrym, M., Zagozdzon, R., et al. (2018a). Intraurethral co-transplantation of bone marrow mesenchymal stem cells and muscle-derived cells improves the urethral closure. Stem Cell Research & Therapy 9 (1), 239. doi:10.1186/s13287-018-0990-2
Burdzinska, A., Dybowski, B., Zarychta-Wisniewska, W., Kulesza, A., Hawryluk, J., Graczyk-Jarzynka, A., et al. (2018b). Limited accuracy of transurethral and periurethral intrasphincteric injections of cellular suspension. Neurourol Urodyn 37 (5), 1612–1622. doi:10.1002/nau.23522
Chen, C. C. G., Avondstondt, A. M., Khatry, S. K., Singh, M., Klasen, E. M., LeClerq, S. C., et al. (2020). Prevalence of symptomatic urinary incontinence and pelvic organ prolapse among women in rural Nepal. International Urogynecology Journal 31 (9), 1851–1858. doi:10.1007/s00192-019-04129-y
Cheng, J., Zhao, Z. W., Wen, J. R., Wang, L., Huang, L. W., Yang, Y. L., et al. (2020). Status, challenges, and future prospects of stem cell therapy in pelvic floor disorders. World Journal of Clinical Cases 8 (8), 1400–1413. doi:10.12998/wjcc.v8.i8.1400
Cui, L., Meng, Q., Wen, J., Gao, Z., Yan, Z., Tian, Y., et al. (2018). A functional comparison of treatment of intrinsic sphincter deficiency with muscle-derived and adipose tissue-derived stem cells. IUBMB Life 70 (10), 976–984. doi:10.1002/iub.1896
Deng, K., Lin, D. L., Hanzlicek, B., Balog, B., Penn, M. S., Kiedrowski, M. J., et al. (2015). Mesenchymal stem cells and their secretome partially restore nerve and urethral function in a dual muscle and nerve injury stress urinary incontinence model. American Journal of Physiology-Renal Physiology 308 (2), F92–F100. doi:10.1152/ajprenal.00510.2014
Dissaranan, C., Cruz, M. A., Kiedrowski, M. J., Balog, B. M., Gill, B. C., Penn, M. S., et al. (2014). Ratmesenchymal stem cell secretome promotes elastogenesis and facilitates recovery from simulated childbirth injury. Cell Transplant 23 (11), 1395–1406. doi:10.3727/096368913X670921
Dominici, M., Le Blanc, K., Mueller, I., Slaper-Cortenbach, I., Marini, F., Krause, D., et al. (2006). Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy 8 (4), 315–317. doi:10.1080/14653240600855905
Du, X. W., Wu, H. L., Zhu, Y. F., Hu, J. B., Jin, F., Lv, R. P., et al. (2013). Experimental study of therapy of bone marrow mesenchymal stem cells or muscle-like cells/calcium alginate composite gel for the treatment of stress urinary incontinence. Neurourol Urodyn 32 (3), 281–286. doi:10.1002/nau.22291
Garcia-Arranz, M., Alonso-Gregorio, S., Fontana-Portella, P., Bravo, E., Diez Sebastian, J., Fernandez- Santos, M. E., et al. (2020). Two phase I/II clinical trials for the treatment of urinary incontinence with autologous mesenchymal stem cells. Stem Cells Translational Medicine 9 (12), 1500–1508. doi:10.1002/sctm.19-0431
Grinnemo, K. H., Mansson-Broberg, A., Leblanc, K., Corbascio, M., Wardell, E., Siddiqui, A. J., et al. (2006). Human mesenchymal stem cells do not differentiate into cardiomyocytes in a cardiac ischemic xenomodel. Annals of Medicine 38 (2), 144–153. doi:10.1080/07853890500422982
Harrell, C. R., Jovicic, N., Djonov, V., Arsenijevic, N., and Volarevic, V. (2019). Mesenchymal stem cell-derived exosomes and other extracellular vesicles as new remedies in the therapy of inflammatory diseases. Cells 8 (12), 1605. doi:10.3390/cells8121605
Hart, M. L., Izeta, A., Herrera-Imbroda, B., Amend, B., and Brinchmann, J. E. (2015). Cell therapy for stress urinary incontinence. Tissue Engineering Part B: Reviews 21 (4), 365–376. doi:10.1089/ten.TEB.2014.0627
Honczarenko, M., Le, Y., Swierkowski, M., Ghiran, I., Glodek, A. M., and Silberstein, L. E. (2006). Human bone marrow stromal cells express a distinct set of biologically functional chemokine receptors. Stem Cells 24 (4), 1030–1041. doi:10.1634/stemcells.2005-0319
Huang, J., Zhang, Z., Guo, J., Ni, A., Deb, A., Zhang, L., et al. (2010). Genetic modification of mesenchymal stem cells overexpressing CCR1 increases cell viability, migration, engraftment, and capillary density in the injured myocardium. Circulation Research 106 (11), 1753–1762. doi:10.1161/circresaha.109.196030
Jager, L., Linzenbold, W., Fech, A., Enderle, M., Abruzzese, T., Stenzl, A., et al. (2020). A novel waterjet technology for transurethral cystoscopic injection of viable cells in the urethral sphincter complex. Neurourol Urodyn 39 (2), 594–602. doi:10.1002/nau.24261
Jalali Tehrani, H., Daryabari, S. S., Fendereski, K., Alijani Zirdehi, M., and KajbafzadehAM, (2021). Application of adipose-derived, muscle-derived, and co-cultured stem cells for the treatment of stress urinary incontinence in rat models. Lower Urinary Tract Symptoms 13 (2), 308–318. doi:10.1111/luts.12360
Janssen, K., Lin, D. L., Hanzlicek, B., Deng, K., Balog, B. M., van der Vaart, C. H., et al. (2019). Multiple doses of stem cells maintain urethral function in a model of neuromuscular injury resulting in stress urinary incontinence. American Journal of Physiology-Renal Physiology 317 (4), F1047–F1057. doi:10.1152/ajprenal.00173.2019
Jiang, H. H., Ji, L. X., Li, H. Y., Song, Q. X., Bano, Y., Chen, L., et al. (2020). Combined treatment with CCR1- overexpressing mesenchymal stem cells and CCL7 enhances engraftment and promotes the recovery of simulated birth injury-induced stress urinary incontinence in rats. Frontiers in Surgery 7, 40. doi:10.3389/fsurg.2020.00040
Jiang, M., Liu, J., Liu, W., Zhu, X., Bano, Y., Liao, H., et al. (2021). Bone marrow stem cells secretome accelerates simulated birth trauma-induced stress urinary incontinence recovery in rats. Aging 13 (7), 10517–10534. doi:10.18632/aging.202812
Jin, M., Chen, Y., Zhou, Y., Mei, Y., Liu, W., Pan, C., et al. (2016a). Transplantation of bone marrow-derived mesenchymal stem cells expressing elastin alleviates pelvic floor dysfunction. Stem Cell Research and Therapy 7 (1), 51. doi:10.1186/s13287-016-0308-1
Jin, M., Wu, Y., Wang, J., Ye, W., Wang, L., Yin, P., et al. (2016b). MicroRNA-29 facilitates transplantation of bone marrow-derived mesenchymal stem cells to alleviate pelvic floor dysfunction by repressing elastin. Stem Cell Research and Therapy 7 (1), 167. doi:10.1186/s13287-016-0428-7
Kean, T. J., Lin, P., Caplan, A. I., and Dennis, J. E. (2013). MSCs: Delivery routes and engraftment, cell-targeting strategies, and immune modulation. Stem Cells Int. 2013, 732742. doi:10.1155/2013/732742
Kim, B. S., Chun, S. Y., Lee, J. K., Lim, H. J., Bae, J. S., Chung, H. Y., et al. (2012). Human amniotic fluid stem cell injection therapy for urethral sphincter regeneration in an animal model. BMC Medicine 10, 94. doi:10.1186/1741-7015-10-94
Kuismanen, K., Sartoneva, R., Haimi, S., Mannerstrom, B., Tomas, E., Miettinen, S., et al. (2014). Autologous adipose stem cells in treatment of female stress urinary incontinence: Results of a pilot study. Stem Cells Translational Medicine 3 (8), 936–941. doi:10.5966/sctm.2013-0197
Kulesza, A., Burdzinska, A., Szczepanska, I., Zarychta-Wisniewska, W., Pajak, B., Bojarczuk, K., et al. (2016). The mutual interactions between mesenchymal stem cells and myoblasts in an autologous Co-culture model. PLoS One 11 (8), e0161693. doi:10.1371/journal.pone.0161693
Li, M., Li, G., Lei, H., Guan, R., Yang, B., Gao, Z., et al. (2016). Therapeutic potential of adipose-derived stem cell-based microtissues in a rat model of stress urinary incontinence. Urology 97 (e1- e7), e1–e277. doi:10.1016/j.urology.2016.08.009
Li, Q., Song, J., Liu, T., Niu, Z., Lu, X., Jia, J., et al. (2021). Exosomes derived by SIRT1-overexpressing bone marrow mesenchymal stem cells improve pubococcygeus muscle injury in rats. International Journal of Stem Cells. doi:10.15283/ijsc21065
Liu, X., Wang, S., Wu, S., Hao, Q., Li, Y., Guo, Z., et al. (2018). Exosomes secreted by adipose-derived mesenchymal stem cells regulate type I collagen metabolism in fibroblasts from women with stress urinary incontinence. Stem Cell Research and Therapy 9 (1), 159. doi:10.1186/s13287-018-0899-9
Mishra, V. K., Shih, H. H., Parveen, F., Lenzen, D., Ito, E., Chan, T. F., et al. (2020). Identifying the therapeutic significance of mesenchymal stem cells. Cells 9 (5), 1145. doi:10.3390/cells9051145
Nygaard, I. E., and Heit, M. (2004). Stress urinary incontinence. Obstet. Gynecol. 104 (3), 607–620. doi:10.1097/01.AOG.0000137874.84862.94
Ott, C. E., Grunhagen, J., Jager, M., Horbelt, D., Schwill, S., Kallenbach, K., et al. (2011). MicroRNAs differentially expressed in postnatal aortic development downregulate elastin via 3' UTR and coding-sequence binding sites. PLoS One 6 (1), e16250. doi:10.1371/journal.pone.0016250
Sadeghi, Z., Isariyawongse, J., Kavran, M., Izgi, K., Marini, G., Molter, J., et al. (2016). Mesenchymal stem cell therapy in a rat model of birth-trauma injury: Functional improvements and biodistribution. International Urogynecology Journal 27 (2), 291–300. doi:10.1007/s00192-015-2831-5
Sadeghi, Z., Kenyon, J. D., Richardson, B., Khalifa, A. O., Cartwright, M., Conroy, B., et al. (2020). TranscriptomicAnalysis of human mesenchymal stem cell therapy in incontinent rat injured urethra. Tissue Engineering Part A 26 (13-14), 792–810. doi:10.1089/ten.tea.2020.0033
Shim, K. H., Choo, S. H., Park, S. G., Yoo, H. J., and Choi, J. B. (2021). Survey on disease insight and prevalence of urinary incontinence in women. Investigative and Clinical Urology 62 (5), 577–583. doi:10.4111/icu.20210019
Shin, J. H., Ryu, C. M., Yu, H. Y., Shin, D. M., and Choo, M. S. (2020). Current and future directions of stem cell therapy for bladder dysfunction. Stem Cell Reviews and Reports 16 (1), 82–93. doi:10.1007/s12015-019-09922-2
Silwal Gautam, S., Imamura, T., Ishizuka, O., Lei, Z., Yamagishi, T., Yokoyama, H., et al. (2014). Implantation of autologous adipose-derived cells reconstructs functional urethral sphincters in rabbit cryoinjured urethra. Tissue Engineering Part A 20 (13-14), 1971–1979. doi:10.1089/ten.TEA.2013.0491
Sobhani, A., Khanlarkhani, N., Baazm, M., Mohammadzadeh, F., Najafi, A., Mehdinejadiani, S., et al. (2017). Multipotent stem cell and current application. Acta Medica Iranica 55 (1), 6–23.
Sudo, R., Sato, F., Azechi, T., and Wachi, H. (2015). MiR-29-mediated elastin down-regulation contributes to inorganic phosphorus-induced osteoblastic differentiation in vascular smooth muscle cells. Genes Cells 20 (12), 1077–1087. doi:10.1111/gtc.12311
Wang, L., Wang, Y., Xiang, Y., Ma, J., Zhang, H., Dai, J., et al. (2021). An in vitro study on extracellular vesicles from adipose-derived mesenchymal stem cells in protecting stress urinary incontinence through MicroRNA-93/F3 Axis. Frontiers in Endocrinology (Lausanne) 12, 693977. doi:10.3389/fendo.2021.693977
Wang, Y., Wang, W., Wang, X., Wang, Y., Wang, J., Fu, Q., et al. (2017). Tissue-engineered sling with adipose-derived stem cells under static mechanical strain. Experimental and Therapeutic Medicine 14 (2), 1337–1342. doi:10.3892/etm.2017.4705
Yanez-Mo, M., Siljander, P. R., Andreu, Z., Zavec, A. B., Borras, F. E., Buzas, E. I., et al. (2015). Biological properties of extracellular vesicles and their physiological functions. Journal of Extracellular Vesicles 4, 27066. doi:10.3402/jev.v4.27066
Zaborowski, M. P., Balaj, L., Breakefield, X. O., and Lai, C. P. (2015). Extracellular vesicles: Composition, biological relevance, and methods of study. Bioscience 65 (8), 783–797. doi:10.1093/biosci/biv084
Zhang, H., Huang, J., Liu, J., Li, Y., and Gao, Y. (2020). BMMSC-sEV-derived miR-328a-3p promotes ECM remodeling of damaged urethral sphincters via the Sirt7/TGFβ signaling pathway. Stem Cell Research and Therapy 11 (1), 286. doi:10.1186/s13287-020-01808-2
Zhang, K., Cao, N., Guo, X., Zou, Q., Zhou, S., Yang, R., et al. (2018). The fabrication of 3D surface scaffold of collagen/poly (L-lactide-co-caprolactone) with dynamic liquid system and its application in urinary incontinence treatment as a tissue engineered sub-urethral sling: In vitro and in vivo study. Neurourol Urodyn 37 (3), 978–985. doi:10.1002/nau.23438
Zhang, L., Zhu, L., Xu, T., Lang, J., Li, Z., Gong, J., et al. (2015). A Population-based survey of the prevalence, potential risk factors, and symptom-specific bother of lower urinary tract symptoms in adult Chinese women. European Urology 68 (1), 97–112. doi:10.1016/j.eururo.2014.12.012
Zhao, Y., Gan, Y., Xu, G., Hua, K., and Liu, D. (2020). Exosomes from MSCs overexpressing microRNA-223- 3p attenuate cerebral ischemia through inhibiting microglial M1 polarization mediated inflammation. Life Science 260, 118403. doi:10.1016/j.lfs.2020.118403
Zheng, Q., Zhang, S., Guo, W. Z., and Li, X. K. (2021). The unique immunomodulatory properties of MSC- derived exosomes in organ transplantation. Frontiers in Immunology 12, 659621. doi:10.3389/fimmu.2021.659621
Zhuang, G., Wen, Y., Briggs, M., Shao, Q., Tran, D., Wang, H., et al. (2021). Secretomes of human pluripotent stem cell-derived smooth muscle cell progenitors upregulate extracellular matrix metabolism in the lower urinary tract and vagina. Stem Cell Research and Therapy 12 (1), 228. doi:10.1186/s13287-021-02292-y
Keywords: mesenchymal stem cells, stress urinary incontinence, stem cell-based therapy, animal model, mechanisms of action
Citation: Liu X, Li T, Zhang J, Lin X, Wang W, Fan X and Wang L (2023) Mesenchymal stem cell-based therapy for female stress urinary incontinence . Front. Cell Dev. Biol. 11:1007703. doi: 10.3389/fcell.2023.1007703
Received: 30 July 2022; Accepted: 04 January 2023;
Published: 13 January 2023.
Edited by:
Wu Yingnan, Yong Loo Lin School of Medicine, National University of Singapore, SingaporeReviewed by:
Nazmul Haque, TotiCell Limited, BangladeshCopyright © 2023 Liu, Li, Zhang, Lin, Wang, Fan and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaochun Liu, dHl4Y2hsaXVAMTYzLmNvbQ==
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.