
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
EDITORIAL article
Front. Cell Dev. Biol. , 08 April 2022
Sec. Molecular and Cellular Pathology
Volume 10 - 2022 | https://doi.org/10.3389/fcell.2022.896194
This article is part of the Research Topic Tumor Microenvironment and Cancer Cell Interactions in Solid Tumor Growth and Therapy Resistance View all 9 articles
Editorial on the Research Topic
Tumor Microenvironment and Cancer Cell Interactions in Solid Tumor Growth and Therapy Resistance
Solid tumour tissues contain a tumour microenvironment (TME) which influences tumour progression and therapy resistance (Romano et al., 2021). TME is a network including non-cancer stromal cells, extracellular matrix (ECM), growth factors, nutrients, blood and lymphatic vessels (Avagliano et al., 2020b), and its structure and components, depending on the type and location of the tumour, make each solid tumour unique (Granato et al., 2017; Avagliano et al., 2020a). Moreover, the TME plasticity leads to its evolution with disease and adaptation to cancer cell and environmental alterations. The components of TME by interacting with each other and with tumour cells generate a cancer niche that sustains immunosuppressive processes, drug resistance, cancer recurrence and dissemination that represent the main causes of cancer related deaths.
This research topic includes eight articles, four reviews and four original articles (Figure 1). Some articles describe the role of extracellular matrix in tumour progression, metastasis formation and resistance to cancer therapy. Other articles describe both the effects of specific proteins in modulating growth, survival and invasion capability of cancer cells as well as the cross-talk between immune, stromal and tumour cells, mediated by cytokines, chemokines or metabolites, capable of creating immunosuppressive or immunostimulatory environments, in different tumour contexts.
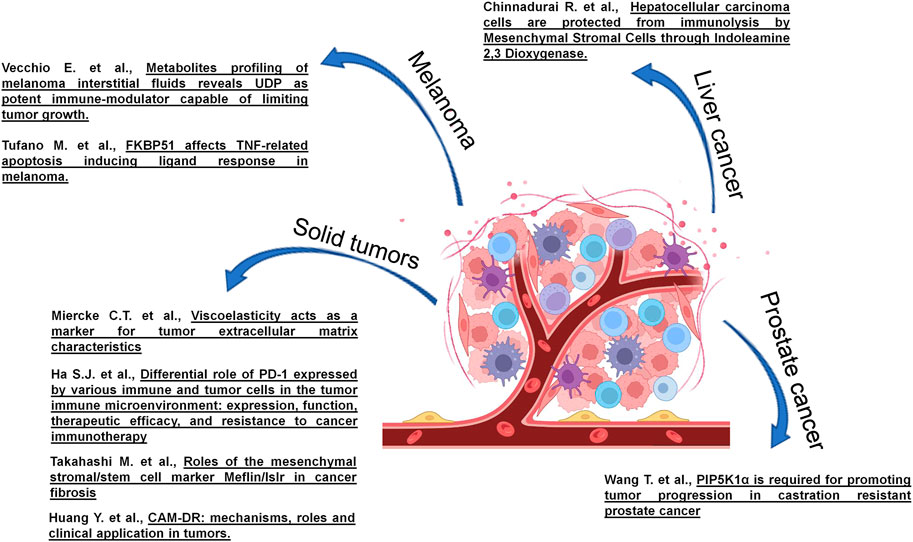
FIGURE 1. Studies on TME of different cancers published in the research topic entitled “Tumor Microenvironment and Cancer Cell Interactions in Solid Tumor Growth and Therapy Resistance.
More specifically, Huang et al. exhaustively described in their review the interactions between tumour cells and extracellular matrix components, including both filamentous proteins (laminin, fibronectin, and collagen) and paracrine factors (cytokines, chemokines, growth factors, exosomes), involved together in the process of cell adhesion-mediated resistance (CAM-DR), essential in different tumours including multiple myeloma, non-Hodgkin’s lymphoma, leukaemia and solid tumours. Finally, they focused on the therapeutic drugs and strategies that could reverse or inhibit CAM-DR process.
Takahashi et al., in their review, after an introduction on the impact of fibroblasts in extracellular matrix remodelling, described the role of Meflin/Islr, a GPI-anchored cell surface protein, a novel marker of Mesenchymal Stromal/Stem Cells (MSC) and cancer associated fibroblasts (CAFs) in different tumours, including pancreatic and colorectal cancers, and in fibrosis of some tissues.
Claudia Tanja Mierke provided us an interesting point of view on the particular importance of a chemical-physical property of extracellular matrix, named viscoelasticity that is referred to a material that exhibits characteristics of both an elastic solid and a fluid, in cancers. Therefore, an accurate measurement of the mechanical features of the tumour extracellular matrix through several techniques could represent a novel marker for prognosis and diagnosis of cancers and provide a further level of comprehension of biological processes in cancer pathogenesis.
Ha et al. exhaustively reviewed different role of PD-1, based on its expression in distinct tumour-infiltrating immune subsets. In particular, they focused on how cell-type-specific ablation or blockade of PD-1 influences tumor growth in a murine tumor model. Further, the authors also describe the effects of PD-1 blockade on TI immune cells in human cancer patients.
Tufano et al., in their article, described a novel pro-oncogenic function of FKBP51 protein in melanoma, which supports NF-κB-mediated resistance and cancer stemness/invasion epigenetic programs. It is worth mentioning that an aberrant expression or activity of NF-κB family member proteins is a common hallmark of various cancers. The NF-κB proteins are a family of transcription factors that regulate the expression of a huge amount of genes and modulate a wide range of cellular processes affecting carcinogenesis, including protein synthesis (Fiume et al., 2013; Pisano et al., 2015), viral expression (Puca et al., 2007; Vitagliano et al., 2011), immune cell development (Fiume et al., 2013; Albano et al., 2019), inflammation (Taniguchi and Karin, 2018), apoptosis (Albensi) and cell survival (Luo et al., 2005), autophagy (Trocoli and Djavaheri-Mergny, 2011), cell motility (Chang et al., 2021). In particular, they found that FKBP51 depletion caused an increased expression of TNF-related apoptosis-inducing ligand (TRAIL)-R2 (DR5), inducing a sensitization of melanoma cells to TRAIL-dependent apoptosis. Their results suggest a novel therapeutic strategy for melanoma treatment.
Chinnadurai et al. described an interesting cross-talk between cells in a tripartite tumour model consisting of PBMCs, MSCs and hepatocellular carcinoma cell line (HepG2). They showed that in co-culture of HepG2 cells and activated PBMCs, HepG2 cells undergo PBMC mediated cytolysis while MSCs protect HepG2 cells from PBMC mediated lysis, through an IDO (indoleamine 2,3 dioxygenase)-dependent mechanism. Finally, they observed that the blockade of IDO activity completely abolishes the ability of MSCs to protect HepG2 cells from cytolysis induced by PBMCs, providing a novel immunotherapeutic strategy for hepatocellular carcinoma treatment.
Vecchio et al. developed a metabolomic technique to analyse the metabolite composition of melanoma interstitial fluid and compare it to plasma of mice engrafted or not with melanoma cells. Among the most enriched metabolites within tumour interstitial fluid, they found guanosine diphosphate (GDP) and uridine diphosphate (UDP). These metabolites acted as stimulator of immune response, increasing the percentage of CD4+CD25+FoxP3–, inducing the phosphorylation of ERK, STAT1, and STAT3 and stimulating the activity of NF-κB subunits p65, p50, RelB, and p52. Further, they observed an increased expression of Th1/Th17 markers and a reduced expression of IL13, a Th2 marker. Finally, they observed that intra-tumoral administration of UDP in mice reduced tumour growth and necrotic areas associated to a higher presence of MHCIIhi tumour-associated macrophage (TAM) and of CD3+CD8+ and CD3+CD4+ tumour-infiltrating T-lymphocytes (TILs). Therefore, they found a novel mediator of immune response, which could potentially represent an adjuvant in cancer immunotherapy.
Wang T. et al. show that the depletion or blockade of PIP5K1α protein suppress growth and invasion of castration-resistant prostate cancer cells (CRPC). The same results were obtained deleting the N-terminal domain of PIP5K1α, required for regulation of mRNA expression and protein stability, in CRPC cells. From a mechanistic standpoint, PIP5K1α acts as an upstream regulator of the androgen receptor (AR) and modulates the expression of AR target genes CDK1 and MMP9. Therefore, their studies identify a novel protein that represents an intriguing target for cancer treatment.
Taken together, these studies on processes modulating the interactions within cancer niche of solid tumours represent one of the most important areas of oncological research that could lead to significant therapeutic advances in medical oncology.
However, we believe that studies focusing on the reversibility of phenotype of TME components that affect cancer development, dissemination, therapeutic resistance and immune escape are missing in this Research Topic and are under-represented in the literature on TME. Understanding whether all TME components are irreversibly differentiated into a pro-tumorigenic phenotype or whether some components of TME can go back to physiological phenotype, acting as anti-tumour components, should be of great relevance.
The identification of molecules and signalling pathways regulating the plasticity of both normal and tumour microenvironment could allow the development of new cancer therapies capable of reducing side effects, improving significantly disease outcome and reduce therapy resistance.
MR, AL and GF edited Manuscripts submitted; AA and GF wrote the editorial; MR, AL and MS edited the editorial. All authors have read and agreed to the published version of the Editorial.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Albano, F., Vecchio, E., Renna, M., Iaccino, E., Mimmi, S., Caiazza, C., et al. (2019). Insights into Thymus Development and Viral Thymic Infections. Viruses 11, 836. doi:10.3390/v11090836
Avagliano, A., Fiume, G., Ruocco, M. R., Martucci, N., Vecchio, E., Insabato, L., et al. (2020b). Influence of Fibroblasts on Mammary Gland Development, Breast Cancer Microenvironment Remodeling, and Cancer Cell Dissemination. Cancers (Basel) 12. doi:10.3390/cancers12061697
Avagliano, A., Fiume, G., Pelagalli, A., Sanità, G., Ruocco, M. R., Montagnani, S., et al. (2020a). Metabolic Plasticity of Melanoma Cells and Their Crosstalk with Tumor Microenvironment. Front. Oncol. 10, 722. doi:10.3389/fonc.2020.00722
Chang, T. Y., Wu, C. T., Sheu, M. L., Yang, R. S., and Liu, S. H. (2021). CARMA3 Promotes Colorectal Cancer Cell Motility and Cancer Stemness via YAP-Mediated NF-Κb Activation. Cancers (Basel) 13. doi:10.3390/cancers13235946
Fiume, G., Rossi, A., De Laurentiis, A., Falcone, C., Pisano, A., Vecchio, E., et al. (2013). Eukaryotic Initiation Factor 4H Is under Transcriptional Control of p65/NF-Κb. PLoS One 8, e66087. doi:10.1371/journal.pone.0066087
Granato, G., Ruocco, M. R., Iaccarino, A., Masone, S., Calì, G., Avagliano, A., et al. (2017). Generation and Analysis of Spheroids from Human Primary Skin Myofibroblasts: an Experimental System to Study Myofibroblasts Deactivation. Cell Death Discov. 3, 17038. doi:10.1038/cddiscovery.2017.38
Luo, J.-L., Kamata, H., and Karin, M. (2005). IKK/NF- B Signaling: Balancing Life and Death - a New Approach to Cancer Therapy. J. Clin. Invest. 115, 2625–2632. doi:10.1172/jci26322
Pisano, A., Ceglia, S., Palmieri, C., Vecchio, E., Fiume, G., De Laurentiis, A., et al. (2015). CRL3IBTK Regulates the Tumor Suppressor Pdcd4 through Ubiquitylation Coupled to Proteasomal Degradation. J. Biol. Chem. 290, 13958–13971. doi:10.1074/jbc.m114.634535
Puca, A., Fiume, G., Palmieri, C., Trimboli, F., Olimpico, F., Scala, G., et al. (2007). IκB-α Represses the Transcriptional Activity of the HIV-1 Tat Transactivator by Promoting its Nuclear Export. J. Biol. Chem. 282, 37146–37157. doi:10.1074/jbc.m705815200
Romano, V., Belviso, I., Venuta, A., Ruocco, M. R., Masone, S., Aliotta, F., et al. (2021). Influence of Tumor Microenvironment and Fibroblast Population Plasticity on Melanoma Growth, Therapy Resistance and Immunoescape. Int. J. Mol. Sci. 22. doi:10.3390/ijms22105283
Taniguchi, K., and Karin, M. (2018). NF-κB, Inflammation, Immunity and Cancer: Coming of Age. Nat. Rev. Immunol. 18, 309–324. doi:10.1038/nri.2017.142
Trocoli, A., and Djavaheri-Mergny, M. (2011). The Complex Interplay between Autophagy and NF-Κb Signaling Pathways in Cancer Cells. Am. J. Cancer Res. 1, 629–649.
Keywords: tumor microenviroment, cutaneous melanoma, tumour extracellular matrix, therapy resistance, cancer immune response
Citation: Ruocco MR, Lamberti A, Serrano MJ, Fiume G and Arcucci A (2022) Editorial: Tumor Microenvironment and Cancer Cell Interactions in Solid Tumor Growth and Therapy Resistance. Front. Cell Dev. Biol. 10:896194. doi: 10.3389/fcell.2022.896194
Received: 14 March 2022; Accepted: 23 March 2022;
Published: 08 April 2022.
Edited and reviewed by:
Ramani Ramchandran, Medical College of Wisconsin, United StatesCopyright © 2022 Ruocco, Lamberti, Serrano, Fiume and Arcucci. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alessandro Arcucci, YWxlc3NhbmRyby5hcmN1Y2NpMkB1bmluYS5pdA==; Giuseppe Fiume, Zml1bWVAdW5pY3ouaXQ=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.