- 1Department of Reproductive Medicine, Department of Prenatal Diagnosis, The First Hospital of Jilin University, Changchun, China
- 2The Laboratory of Cancer Precision Medicine, The First Hospital of Jilin University, Changchun, China
- 3Department of Clinical Laboratory, The First Hospital of Jilin University, Changchun, China
- 4Department of Breast Surgery, The First Hospital of Jilin University, Changchun, China
- 5Hand Surgery Department, The First Hospital of Jilin University, Changchun, China
Premature ovarian failure (POF) has become one of the main causes of infertility in women of childbearing age and the incidence of POF is increasing year by year, seriously affecting the physical and mental health of patients and increasing the economic burden on families and society as a whole. The etiology and pathogenesis of POF are complex and not very clear at present. Currently, hormone replacement therapy is mainly used to improve the symptoms of low estrogen, but cannot fundamentally solve the fertility problem. In recent years, stem cell (SC) transplantation has become one of the research hotspots in the treatment of POF. The results from animal experiments bring hope for the recovery of ovarian function and fertility in patients with POF. In this article, we searched the published literature between 2000 and 2020 from the PubMed database (https://pubmed.ncbi.nlm.nih.gov), and summarized the preclinical research data and possible therapeutic mechanism of mesenchymal stem cells (MSCs) in the treatment of POF. Our aim is to provide useful information for understanding POF and reference for follow-up research and treatment of POF.
Introduction
POF is a kind of ovarian dysfunction characterized by menstrual disorder, ovarian atrophy, decreased sexual life and decreased fertility in women between puberty and 40 years old, which seriously affects female reproductive health and endocrine balance and is one of the main causes of female infertility (Sheikhansari et al., 2018). Approximately 1% of women under the age of 40 suffer from premature ovarian failure (Huhtaniemi et al., 2018). Under the influence of high pressure and a fast paced life, the incidence of POF is increasing and manifesting at younger ages, and it has affected more than 10% of women in recent years (Thakur et al., 2018).
POF treatment is extremely difficult. Although assisted reproductive technology has become an effective treatment, it is not ideal, and fertility loss and low estrogen status have become a great threat to female reproductive health (Laven, 2016). POF has become one of the most severe problems threatening the reproductive health of women of normal childbearing age. Its occurrence may be related to an insufficient reserve of primordial follicular cistern, accelerated follicular atresia, changes of dominant follicular recruitment, follicular maturation disorders and so on (Xiang et al., 2019). In view of the limitations of conventional treatment, clinical and scientific research work has focused on improving ovarian function and restoring fertility in patients with POF. In recent years, MSC transplantation has opened up a new direction for the treatment of POF, but this is still in the stage of preclinical research (Lai et al., 2015; Sun et al., 2017; Zhang et al., 2018; Liu S. et al., 2019; Zheng et al., 2019), and there are few clinical studies so far. The mechanism by which MSCs improve ovarian function has also not been completely elucidated. At present, there is no clear and effective treatment to restore the reproductive function of ovaries. In this paper, we reviewed the preclinical research data of the treatment of POF using MSCs and the possible therapeutic mechanisms to provide a reference for follow-up research and treatment of POF.
The Current Situation of POF Treatment
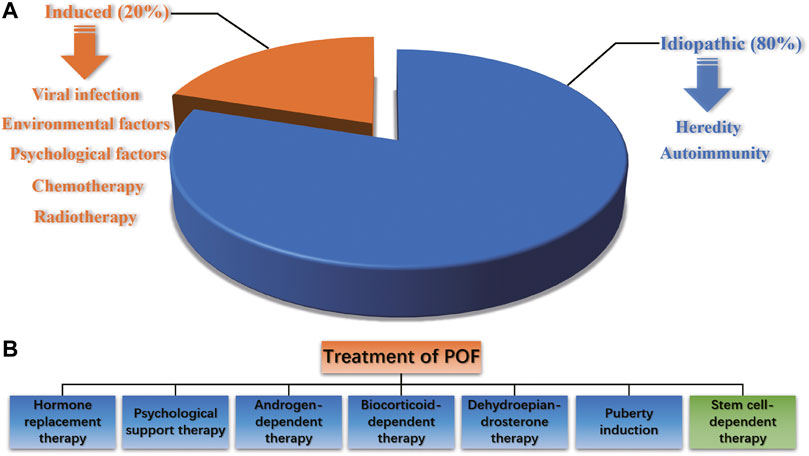
POF is a reproductive endocrine disease that occurs before the age of 40 and is characterized by increased gonadotropin levels and decreased estrogen levels, accompanied by primary or secondary amenorrhea. It is also one of the common diseases leading to female infertility. POF is a highly heterogeneous condition. Abnormal follicular development in all stages can lead to POF, and such damage to ovarian function is irreversible. The pathogenic factors of POF include heredity, autoimmunity, viral infection, iatrogenic factors, and environmental and psychological factors, and approximately eighty percent of POF cases are idiopathic (Webber et al., 2016) (Figure 1A). It has been reported that radiotherapy, chemotherapy and bone marrow transplantation of cancer can result in POF (Dolmans and Donnez, 2021; Imai et al., 2008). The traditional treatment of POF includes hormone replacement therapy (HRT), psychological support therapy, androgen-dependent therapy, biocorticoid-dependent therapy, dehydroepiandrosterone therapy and puberty induction (Figure 1B). However, HRT can only relieve low estrogen symptoms such as vaginal dryness, hot flashes and genitourinary tract atrophy, but has no essential effect on improving ovarian reproductive function. Long-term use of HRT is controversial because it increases the risk of endometrial and ovarian cancer (Ali, 2013; Lee et al., 2020). Since the etiology of POF infertility is complex, the current treatment efficacy is unsatisfactory, and the pregnancy rate and carrying to term rates are still quite low after treatments. Therefore, for women with fertility requirements, it is necessary to strengthen early prevention, early detection and early treatment to delay the development of POF and improve the live birth rate.
The results from animal experiments of MSC transplantation has brought hope to the recovery of ovarian function and fertility in patients with POF. In the following, we will introduce advances in the treatment of POF with MSCs.
MSCs and Fertility Protection
MSCs were the first type of adult stem cell discovered in bone marrow. They originate from mesoderm and are distributed in almost all connective tissue and organ stroma of the entire body. They have the potential for multidirectional differentiation of stem cells and also have a strong migration ability to damaged tissues. Since MSCs have low immunogenicity and fewer disputes in bioethics than fetal-derived stem cells, they are widely applied in clinical research and medical bioengineering (Pers et al., 2016; Badawy et al., 2017; Mu et al., 2018). Currently, MSCs have been used to treat diseases related to the blood, nervous, motor, cardiovascular and skin systems, showing good curative effects (Zaher et al., 2014).
The reproductive capacity of most female mammals is mainly affected by the primordial follicular pool. Under normal circumstances, to avoid depletion of the follicular pool, most primordial follicles in the ovary are maintained in a resting phase. Primordial follicles undergo follicular activation and a series of developmental processes and finally develop into mature follicles. Various molecules are involved in regulating follicular activation, growth and atresia. Ovarian function recovery is based on oocyte production and follicular quantity/quality recovery (Woods and Tilly, 2012; Truman et al., 2017). Several studies have shown that MSCs can directly differentiate into oocyte-like cells, and transplantation of MSCs is conducive to restoring ovarian function and reproductive capacity (Bahrehbar et al., 2020; Yoon et al., 2020; Taheri et al., 2021). Therefore, MSCs are considered a new choice for the treatment of POF.
The effectiveness of MSCs in the treatment of reproductive system diseases has been confirmed by preclinical and clinical research, which has brought great hope to POF infertility and improved female reproductive health (Herraiz et al., 2019; Fu et al., 2021; Li et al., 2021). MSCs used for the treatment of POF include BMSCs, UCMSCs, PMSCs, AMSCs, AFMSCs, MenSCs and ADMSCs. MSCs originating from different sources have some common characteristics, which make them an ideal treatment choice for POF. A number of animal experiments and clinical trials have confirmed that ovarian function can be improved by MSC homing, inhibiting the apoptosis of OGC and promoting ovarian angiogenesis (Esfandyari et al., 2020). For example, Yan et al. transplanted MSCs to 61 patients with POF and found that the number of follicles in each developmental stage, including antral follicles, dominant follicles and mature follicles, increased significantly (Yan et al., 2020). Other researchers have found that autologous MSC transplantation can trigger menstruation to resume, relieve menopausal symptoms, improve ovarian function and help patients become pregnant (Bukovsky and Caudle, 2012; Igboeli et al., 2020; Mashayekhi et al., 2021; Ulin et al., 2021). Ling et al. treated POF mice with MSCs and found that MSC transplantation could significantly restore their hormone secretion ability, improve follicular growth and GC survival, and recover the ovarian function that was destroyed by chemotherapy used to create the POF mice (Ling et al., 2019). A meta-analysis of POF indicated that MSCs could decrease the level of FSH, increase the level of E2 and promote the proliferation of follicles, thus improving the quality of ovaries in POF animals and humans (Chen et al., 2018). Interestingly, Bahrehbar et al. proved that MSC-transplanted POF mice can produce offspring (Bahrehbar et al., 2020).
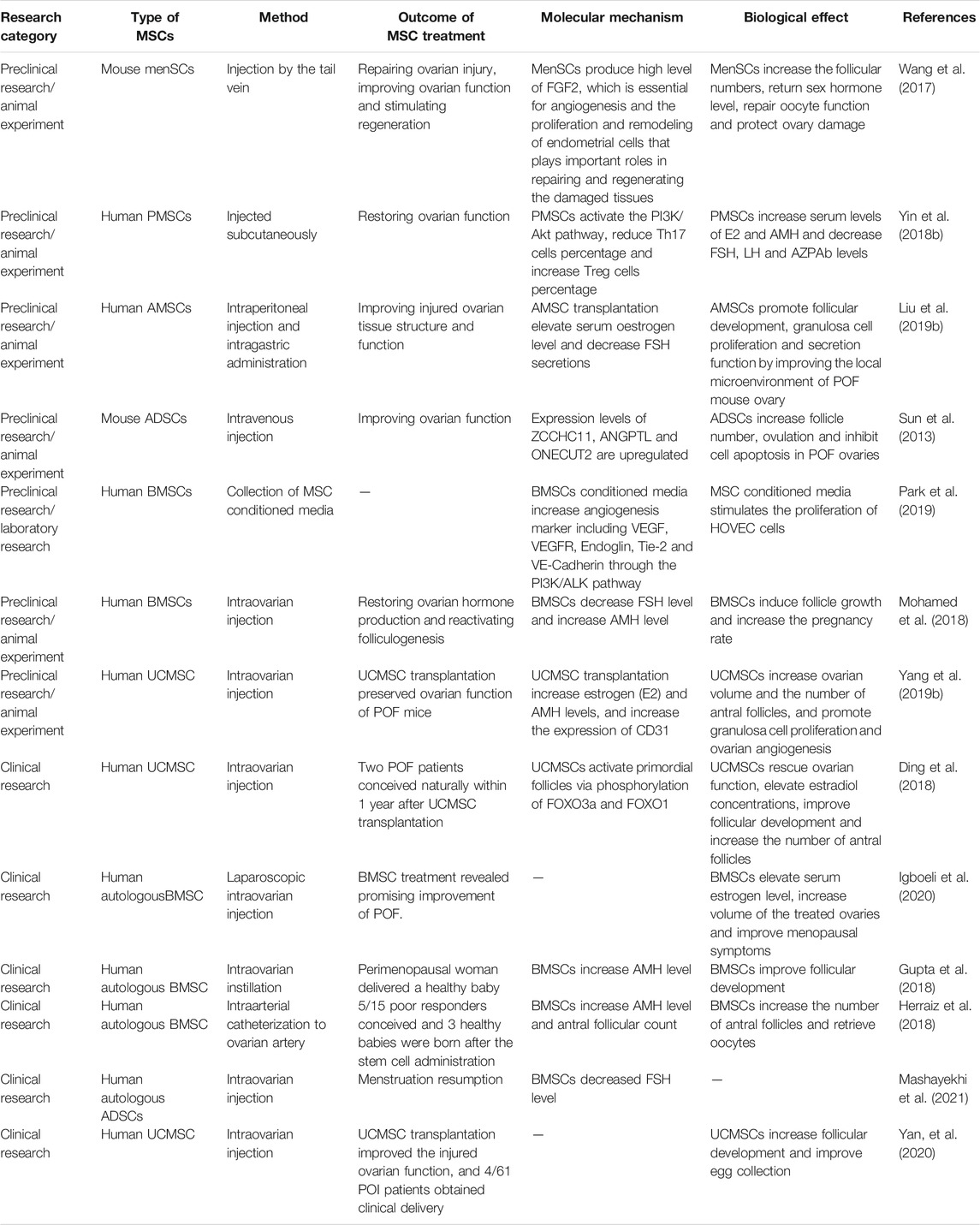
Table 1 summarizes the preclinical and clinical trials that indicate the validity of treating POF with MSCs. However, the underlying molecular and cellular mechanisms are still controversial and need to be further clarified. Additionally, current clinical research is still insufficient, and there is still a long way to go before the large-scale clinical application of MSCs.
The Mechanism of Treating POF With MSCs
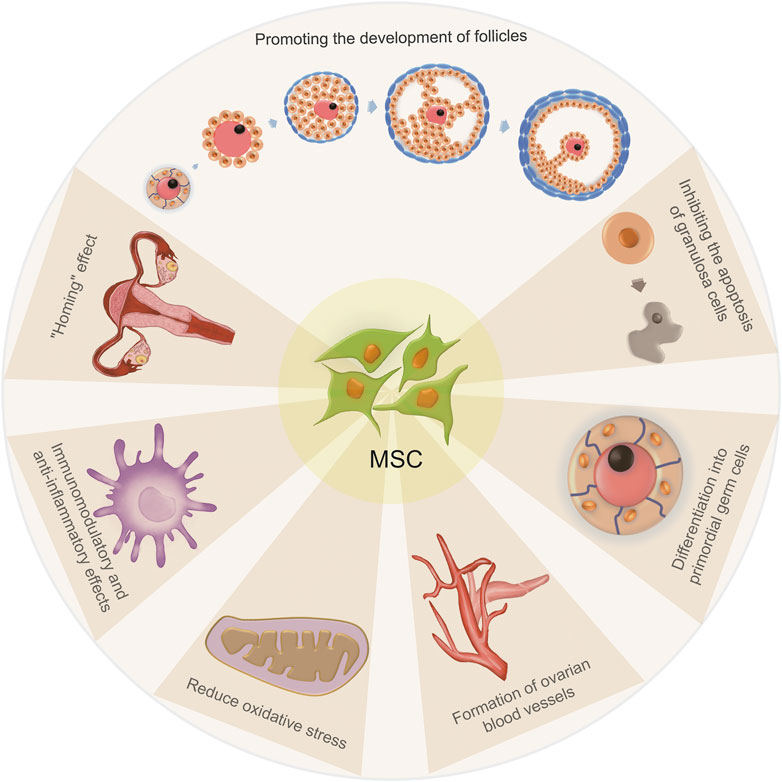
The mechanism of treating POF with MSCs can be summarized as follows (Figure 2): 1) MSCs have a “homing” effect; 2) MSCs can promote the growth and development of follicles at all developmental stages; 3) MSCs may induce and differentiate into primordial germ cells (uncertain); 4) MSCs can directly differentiate into GCs or inhibit the apoptosis of GCs; 5) MSCs can promote the formation of ovarian blood vessels; 6) MSCs have immunomodulatory and anti-inflammatory effects and 7) MSCs can reduce oxidative stress.
Homing Effect of MSCs
The homing capacity of MSCs is an important determinant of effective MSC-based therapy (Li et al., 2017; Lin et al., 2017). Homing refers to the process by which MSCs migrate to damaged tissues and promote their recovery. Therefore, enhancing the homing efficiency of MSCs is essential for optimizing the therapeutic outcome of POF. Noory et al. reported the application of MenSC transplantation as a treatment modality in a rat model of POF and observed that MSCs can survive in ovarian stroma at 2 months after MSC transplantation and directly differentiated into GCs (Noory et al., 2019). Experiments from Liu et al., Jalalie, et al., Lai et al., Song et al. and Park et al. also demonstrated that after transplantation, MSCs home to damaged tissue and reach the site of injured ovaries (Liu et al., 2014; Lai et al., 2015; Jalalie et al., 2019; Park et al., 2021). However, studies have also shown that although MSCs have a homing effect, they cannot directly differentiate into oocytes but do localize in the ovarian matrix, secrete various cytokines and improve ovarian reserve function through the paracrine pathway (Takehara et al., 2013; Gabr et al., 2016; Li et al., 2017). A study by Taheri et al. demonstrated that MSC isolated from follicular fluid cultured in human recombinant BMP15 medium may differentiate into oocyte-like cells in vitro, but they did not investigate whether such MSCs can differentiate into oocytes in vivo (Taheri et al., 2021). Therefore, whether MSCs can directly differentiate into oocytes remains unclear, and more in-depth laboratory experiments are still necessary to solve this scientific problem.
Effects of MSCs on Follicular Development
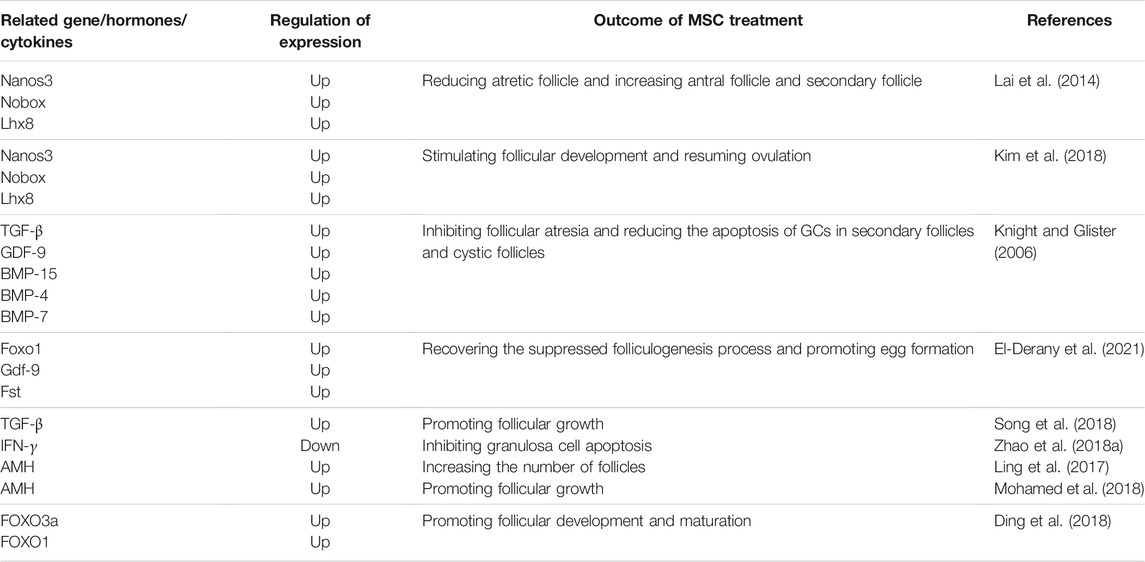
Folliculogenesis is an important part of ovarian function, as it provides oocytes for reproduction (Hua et al., 2015). A large number of genes/proteins have been identified to be associated with follicular development, growth, ovulation and atresia processes. It has been reported that PMSC transplantation can increase the secretion of growth factors, angiogenic factors, pleiotropic cytokines, chemotactic cytokines and extracellular matrix proteins, which are all essential for folliculogenesis (Kupcova Skalnikova, 2013). In POF treatment, the widely discussed follicular development related genes are Nanos3, Nobox and Lhx8. Lai et al. proved that SMSC transplantation could reactivate injured mouse ovaries, with increased expression of the folliculogenesis marker genes Nobox, Nanos3, and Lhx8 in the ovaries of SMSC-treated mice (Lai et al., 2014). Kim et al. showed that three-dimensional cultured PDMSC spheres could upregulate the expression level of Nanos3, Nobox and Lhx8, and resume ovulation through regulation of the follicular microenvironment and stimulation of follicular development (Kim et al., 2018). Peng et al. also showed that the mRNA levels of these three genes in POF mice treated with BMSCs were significantly higher than those in the untreated group (Peng et al., 2018). Other follicular development-related genes include Foxo3a and Foxo1. Ding et al. found that UCMSCs on a collagen scaffold can activate primordial follicles in vitro via phosphorylation of FOXO3a and FOXO1, and transplantation of collagen/UCMSCs to the ovaries of POF patients can elevate estradiol concentrations, improve follicular development and increase the number of antral follicles (Ding et al., 2018).
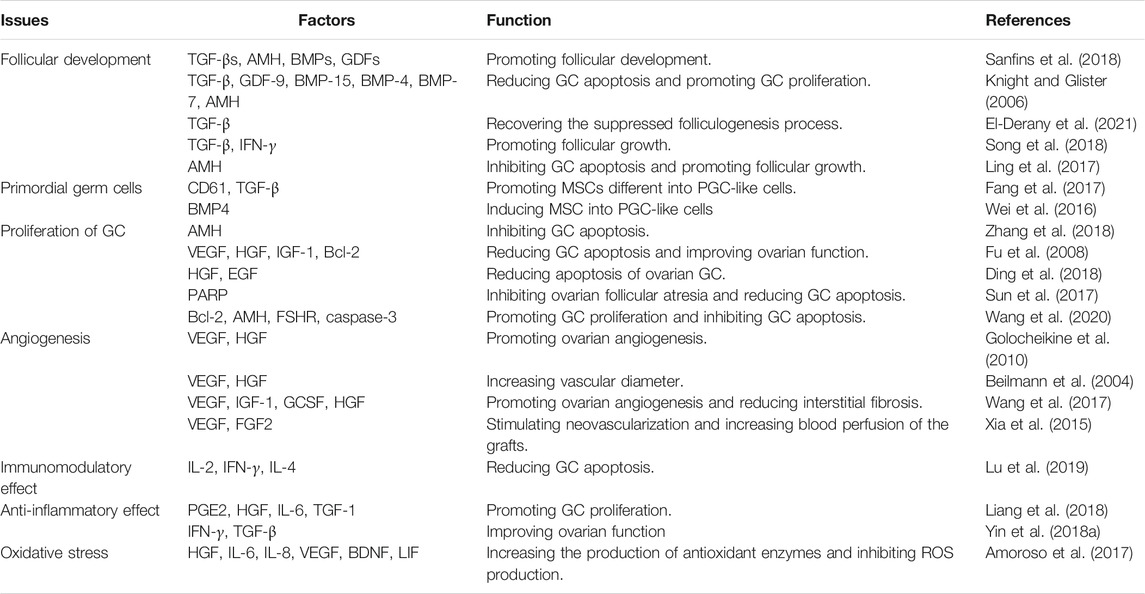
Cytokines are critical regulators of folliculogenesis and ovulation. They contribute to creating an environment supporting follicle selection and growth, regulating cellular proliferation/differentiation, follicular survival/atresia and oocyte maturation (Field et al., 2014). The most important cytokines in POF treatments are TGF-β and IFN-γ. TGF-β superfamily members, including TGF-βs, AMH, activins, inhibins, BMPs and GDFs, impact several stages of follicular development (Trombly et al., 2009; Sanfins et al., 2018). According to Knight et al., the positive TGF-β regulators of preantral follicle growth, include GDF-9 and BMP-15 of oocyte origin, activins of granulosal origin, BMP-4 and BMP-7 of thecal origin and TGF-β from theca and GCs; in contrast, AMH plays a negative role in preantral follicle development (Knight and Glister, 2006). However, the existing research conclusions are not consistent with each other. El-Derany et al. transplanted BMSCs to a γ-ray induced POF rats model and reported that BMSCs recovered the folliculogenesis process, upregulating Foxo1, Gdf-9 and Fst gene expression accompanied by downregulating TGF-β (El-Derany et al., 2021), whereas Song et al. and Yin et al. found that MSC transplantation could increase the level of TGF-β and decrease the level of IFN-γ in POF models (Yin et al., 2018a; Song et al., 2018). Additionally, Ling et al. reported that amnion-derived mesenchymal stem cell transplantation can inhibit granulosa cell apoptosis and that the expression levels of AMH were significantly increased in the treatment group compared to the POF group (Ling et al., 2017). Zhang et al. and Mohamed et al. also found that after MSC transplantation, AMH expression in ovarian tissue was significantly higher than that in the POF group (Mohamed et al., 2018; Zhang et al., 2018).
Although the mechanism of MSCs on follicular development is not completely clear, most research agrees that MSC transplantation can promote the development and formation of primordial follicles, eggs and reduce the apoptosis of GCs. All of the involved genes and their correlated mechanisms are listed in Table 2.
MSCs and PGCs
Multiple studies have shown that MSCs can be induced and differentiate into PGCs. Fang et al. and Li et al. proved that CD61 could promote the differentiation of ADMSC into PGC-like cells through activation of the TGF-β pathway (Li et al., 2016; Fang et al., 2017). Wei et al. found that AMSC can be induced into PGC-like cells by BMP4 (Wei et al., 2016). Ge et al. found that when hfSDSCs were cultured in porcine follicle fluid, they may differentiate into both male and female germ cell-like cells (Ge et al., 2015). Park et al. proved that female mouse skin-derived stem cells could differentiate into ovarian-cell-like cells that are consistent with female germ, and ovarian follicle somatic cells. When ovarian cell-like cells are transplanted into ovariectomized mice, they restore the estrus cycle and serum estradiol levels (Park et al., 2014). Unfortunately, no in vivo research has reported whether MSC-differentiated germ cells can be fertilized and form embryos, and studies in this area are still lacking.
MSCs Can Promote the Proliferation of GCs
OGCs are the most important stromal cells in the ovary, providing necessary nutrition for oocyte development and follicle maturation, participating in the regulation of gonadotropins that modulate oocyte development and maintaining the microenvironment of oocyte maturation through autocrine and paracrine mechanisms. GCs play an important role in all developmental stages of follicles. GCs abnormalities can lead to abnormal hormone secretion, follicular development disorders and even follicular atresia (Lai et al., 2014). Chemotherapy induces GC apoptosis by damaging DNA and activating apoptosis pathways, thus leading POF. Therefore, enhancing GC function and inhibiting GC apoptosis may effectively prevent POF (Bedoschi et al., 2016). Studies have shown that GCs and MSCs express some similar surface markers (Dzafic et al., 2014; Maleki et al., 2014). Transplanted MSCs are mainly located in the GC layer around follicles, suggesting that MSCs have a significant effect on follicle formation and ovulation (Manshadi et al., 2019).
MSCs can inhibit GC apoptosis and promote GC proliferation by releasing cytokines and hormones, upregulating proliferation-related genes and inhibiting apoptosis-related genes (He et al., 2018; Wang et al., 2020). Zhang et al. showed that PMSC transplantation could upregulate the expression of AMH and FSHR in GCs of POF mice, inhibit GC apoptosis and follicular atresia, and thus restore ovarian function (Zhang et al., 2018). Fu et al. also found that BMSC transplantation may reduce GC apoptosis and improve ovarian function by releasing VEGF, HGF, and IGF-1 and upregulating Bcl-2 expression (Fu et al., 2008). Ding et al. showed that coculturing of AMSCs and GCs might inhibit the apoptosis of GCs, and transplantation of AMSCs may improve ovarian function during natural aging by secreting HGF and EGF (Ding et al., 2018).
The underlying mechanism of MSC treatment of POF may be related to exosome-mediated microRNA modulation. Multiple studies have highlighted the potential therapeutic advantages of using exosomal miRNAs from MSCs for the treatment of various diseases and injuries, including POF. Yang et al. demonstrated that BMSC-derived exosomes prevent ovarian follicular atresia in POF rats via the delivery of miR-144-5p, which can decrease GC apoptosis by targeting the PTEN pathway (Yang et al., 2020). Xiao et al. found that miR-146a and miR-10a are rich in exosomes secreted by AFSCs. miR-146a can restore ovarian function by downregulating IRAK1 and TRAF632 expression and miR-10a can inhibit GC apoptosis and prevent follicular atresia by suppressing Bim and caspase-9 expression (Xiao et al., 2016). Sun et al. found that exosomes derived from UCMSCs may prevent and treat chemotherapy-induced OGC apoptosis in vitro by upregulating the expression level of Bcl-2 and downregulating the expression levels of caspase-3, Bax, cleaved caspase-3 and cleaved PARP (Sun et al., 2017). miR-21 is related to apoptosis. Studies have shown that MSC treatment suppresses the expression of PTEN and PDCD4 through upregulation of miR-21 and inhibiting the apoptosis of GCs (Fu et al., 2017). Sun et al. reported that miR-644-5p carried by MSC exosomes could regulate p53 signaling and inhibit GC apoptosis (Sun et al., 2019).
MSCs Promote Angiogenesis
The establishment and remodeling of the ovarian vascular system is the basis of ovarian development and functional recovery. The follicles and corpus luteum can obtain nutritional support through ovarian blood vessels and transport hormones to target organs. Some researchers observed the distribution of BMSCs in ovaries by labeling specific markers of BMSCs and found that BMSCs were mainly distributed in the blood vessels of damaged ovaries (Liu et al., 2014), implying that BMSCs may play a role in ovarian blood vessels construction. Angiogenesis-related factors secreted by MSCs, such as VEGF, HGF, IGF and FGF, are increased in MSC-transplanted POF ovaries. VEGF and HGF have a synergistic effect and synergistically promote angiogenesis (Golocheikine et al., 2010). The combination of VEGF and HGF leads to an increased vascular diameter (Beilmann et al., 2004); VEGF promotes the length, area and branch point number of the induced vessels, while HGF contributes to vascular area growth (He et al., 2018). Wang et al. showed that MSCs could promote ovarian angiogenesis and reduce interstitial fibrosis by secreting VEGF, IGF-1, GCSF and HGF (Wang et al., 2017). Xia et al. demonstrated that MSC transplantation could enhance the expression levels of VEGF, FGF2 and angiogenin, significantly stimulate neovascularization and increase blood perfusion of the grafts in ovarian tissue (Xia et al., 2015). Zhang et al., Cho et al. and Park et al., also proved that MSC transplantation could repair damaged POF ovaries and promote ovarian development and function through angiogenesis (Zhang et al., 2017; Park et al., 2019; Cho et al., 2021).
Microvesicles are cell-derived membrane and cytoplasmic components. There are three subtypes of EVs: exosomes, microvesicles and apoptotic bodies. Exosomes and microvesicles can transfer mRNA, protein and lipids to target cells through surface-expressed ligands and surface receptors, thus affecting the phenotype and function of the target cells (Bidarimath et al., 2017). EVs have a therapeutic effect on female reproductive disorders, such as repairing injured endometrium, suppressing fibrosis of the endometrium, regulating immunity and anti-inflammation, and repressing the apoptosis of GCs in ovaries (Liao et al., 2021). Several studies have shown that MSC-derived microvesicles contain multiple pro-angiogenic proteins, such as VEGF and HGF (Merino-Gonzalez et al., 2016; Pakravan et al., 2017; Han et al., 2019; Shi et al., 2019). Yang et al. showed that UCMSC microvesicles transplantation in POI mice could induce angiogenesis by activating the PI3K/Akt signaling pathway and improve ovarian function (Yang Z. et al., 2019). Sun et al. found that miR-644-5p carried by BMSC-derived exosomes inhibited the apoptosis of ovarian GCs by targeting the p53 pathway (Sun et al., 2019); Zhang et al. also found that UCMSC-derived microvesicles can inhibit the apoptosis of GSs by downregulating the expression level of caspase-3 and upregulating the ratio of Bcl-2/Bax (Zhang J. et al., 2020).
Anti-inflammatory and Immunomodulatory Effect of MSCs
POF is an autoimmune disease. Autoimmune dysfunction is one of the most important pathogeneses of POF, causing inflammatory reactions of the ovary, destroying the ultrastructure of follicular cells (such as zona pellucida damage, gap link rupture and mitochondrial swelling), causing apoptosis of ovarian cells, affecting the maturation and atresia of follicles and inducing a decline in ovarian function (Nelson, 2001; Luo et al., 2017). It has been reported that certain types of immune cells will expand in ovaries with POF and infiltrate into the ovarian tissue, indicating that they are involved in the inflammation associated with POF (van Kasteren et al., 2000; Chernyshov et al., 2001; La Marca et al., 2010; Wang et al., 2018).
The anti-inflammatory effect is a critical mechanism by which MSCs restore ovarian function. MSCs may inhibit the activation and proliferation of lymphocytes, inhibit the secretion of proinflammatory cytokines, inhibit the function of antigen-presenting cells, and convey regulatory messages to immune cells (Zhou et al., 2019). In contrast, since the ovaries of most POF patients are in inflammatory conditions, the presence of inflammatory cytokines is also crucial for the regulation of MSC immunological and regenerative functions. Beldi et al. proved that the tumor TNF-α-TNFR2 axis is necessary for MSCs to produce anti-inflammatory mediators (such as IL-10, TGFβ and NO) and sustain regenerative functions such as wound healing, complex tube formation and endothelial pro-angiogenic support (Beldi et al., 2020a; Beldi et al., 2020b). IFN-γ and MSCs have a synergistic effect on immunosuppression. They upregulate PGE2, HGF, IL-6 and TGF-1 in MSCs and induce MSCs to express IDO, promoting GC proliferation and increasing the number of follicles (Najar et al., 2016; Liang et al., 2018). Yin et al. showed that the level of proinflammatory IFN-γ increased and the level of anti-inflammatory TGF-β decreased in POF mice, whereas PMSC transplantation reversed this situation and improved ovarian function (Yin et al., 2018a). A study also showed that PMSCs increase the secretion of IL-10 by inhibiting NF-κB-mediated pro-inflammatory reactions and thus promote tissue repair (Wang et al., 2016).
Immune cells (Treg cells, NK cells, Th cells, etc.) are important pathogenic factors in several models of autoimmune diseases (Alvarez Arias et al., 2014; Gianchecchi et al., 2018; Zhang X.-M. et al., 2020; Sakaguchi et al., 2020). These results indicate that the interaction of MSCs and immune cells plays a critical role in regulating the inflammatory microenvironment of POF. Yin et al. showed that PMSC transplantation might restore the ovarian function of POF mice by balancing the ratios of Th17/Tc17 and Th17/Treg cells (Yin et al., 2018b). Lu et al. reported that the serum levels of IL-2 and IFN-γ secreted by Th1 cells increased, while IL-4 secreted by Th2 cells decreased in POF mice; however, after UMSC transplantation, the amounts of these cytokines were reversed (Lu et al., 2019). Yin et al. showed that UCMSC transplantation into POF mice upregulates the ratio of CD8+ Treg cells, which have a typical immunosuppressive function and can reduce immune rejection (Su et al., 2014; Yin et al., 2020).
The Effect of MSCs on Oxidative Stress
Oxidative stress is a phenomenon of imbalance between the oxidative system and the antioxidant system caused by excessive ROS produced in cells. Reduction of ROS can protect the structure and function of ovarian mitochondria, increase the levels of antioxidant and antiapoptotic enzymes, and reduce apoptosis and oxidative damage of the ovary (He et al., 2018). Abumaree et al. indicated that cocultured PMSCs could reverse the destructive effect of OS on H2O2-treated endothelial cells and increase cell proliferation and migration (Abumaree et al., 2017). One study showed that ROS inhibit the expression and activity of TERT and induce POF (Jiang et al., 2018). MSCs can increase the production of antioxidant enzymes and inhibit ROS production through secretion of HGF, IL-6, IL-8, VEGF, BDNF and LIF and activation of the FOXO, NOQ1/MAPK, PI3K/Akt and Nrf2-ARE pathways (Amoroso et al., 2017). One study indicated that fMSCs upregulate MT1, JNK1, PCNA and AMPK levels and enhance antioxidant effects (Huang et al., 2019). Recently, it has been found that PMSC transplantation can reduce the levels of UCP-2, SOD1, reactive oxygen species and 8-hydroxydeoxyguanosine in POF rats, improving mitochondrial function in vivo, inhibiting oxidative stress and improving ovarian function (Zhang et al., 2016).
Using MSCs to treat POF is a sophisticated project. To better understand the mechanism by which MSCs improves ovarian functions, we summarized the cytokines and regulatory factors involved in the homing effect, follicular development, cell proliferation/apoptosis, angiogenesis, immunomodulation and oxidative stress processes, as shown in Table 3.
Perspective
MSCs possess multiple differentiation potentials and homing and immunomodulatory functions. They can be used as seed cells to participate in the regeneration and reconstruction of tissues and organs in various diseases, such as rheumatoid arthritis, amyotrophic lateral sclerosis, systemic lupus erythematosus and other degenerative diseases (spinal cord injury, Parkinson’s disease, Alzheimer’s disease). At present, more than ten kinds of stem cell preparations have been used to treat graft-versus-host disease (Zhao et al., 2019), acute myocardial infarction (Cho et al., 2017), osteoarthritis (Matas et al., 2019), etc. The clinical application of MSCs has brought great hope to the treatment of POF infertility and the improvement of female reproductive health, and a large number of clinical studies are actively being carried out. However, with increasing age, the number and function of MSCs decrease accordingly. The senescence of MSCs may be related to telomere shortening, DNA damage, epigenetics and immunological characteristics (Trachana et al., 2017; Wagner, 2019). At present, senescence of MSC is still the bottleneck of stem cell tissue engineering and clinical applications. Therefore, how to deeply understand the molecular mechanism of MSC senescence and delay or prevent MSC senescence efficiently through reasonable gene manipulation or drug intervention, has crucial practical significance and important economic value.
Conclusion
MSCs derived from different sources have similar curative effects in the treatment of POF through multiple mechanisms. MSCs have attractive clinical transformation and application prospects in the restoration of reproductive function in POF patients, even in older women with POF. Therefore, understanding the molecular mechanism of POF is still a key scientific problem for comprehensively and deeply evaluating the safety and effectiveness of MSC transplantation, especially the long-term impact on parents and offspring.
Author Contributions
XS and JW contributed to the conception and design of the article. JW and WL drafted the article. ZY, DY, and SL drafted the figures. All authors have read and approved the final manuscript.
Funding
This work was supported in part by the National Natural Science Foundation of China Grant (No. #81801227 to XS), the Subject Arrangement Program from Science and Technology Department of Jilin Province (Nos. #20200201123JC to DY and #20190201209JC to SL), and Clinical-Translational Medicine Project from the First Hospital of Jilin University (No. #JDYYJCHX2020013 and #2020-ZL-13 to XS and DY).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Abumaree, M. H., Hakami, M., Abomaray, F. M., Alshabibi, M. A., Kalionis, B., Al Jumah, M. A., et al. (2017). Human Chorionic Villous Mesenchymal Stem/Stromal Cells Modify the Effects of Oxidative Stress on Endothelial Cell Functions. Placenta 59, 74–86. doi:10.1016/j.placenta.2017.05.001
Alvarez Arias, D. A., Kim, H.-J., Zhou, P., Holderried, T. A. W., Wang, X., Dranoff, G., et al. (2014). Disruption of CD8+ Treg Activity Results in Expansion of T Follicular Helper Cells and Enhanced Antitumor Immunity. Cancer Immunol. Res. 2, 207–216. doi:10.1158/2326-6066.cir-13-0121
Amoroso, M. R., Matassa, D. S., Agliarulo, I., Avolio, R., Maddalena, F., Condelli, V., et al. (2017). Stress-Adaptive Response in Ovarian Cancer Drug Resistance. Adv. Protein Chem. Struct. Biol. 108, 163–198. doi:10.1016/bs.apcsb.2017.01.004
Badawy, A., Sobh, M., Ahdy, M., and Abdelhafez, M. (2017). Bone Marrow Mesenchymal Stem Cell Repair of Cyclophosphamide-Induced Ovarian Insufficiency in a Mouse Model. Int. J. women's Health 9, 441–447. doi:10.2147/ijwh.s134074
Bahrehbar, K., Valojerdi, M. R., Esfandiari, F., Fathi, R., Hassani, S.-N., and Baharvand, H. (2020). Human Embryonic Stem Cell-Derived Mesenchymal Stem Cells Improved Premature Ovarian Failure. World J. Stem Cell 12, 857–878. doi:10.4252/wjsc.v12.i8.857
Bedoschi, G., Navarro, P. A., and Oktay, K. (2016). Chemotherapy-Induced Damage to Ovary: Mechanisms and Clinical Impact. Future Oncol. 12, 2333–2344. doi:10.2217/fon-2016-0176
Beilmann, M., Birk, G., and Lenter, M. C. (2004). Human Primary Co-Culture Angiogenesis Assay Reveals Additive Stimulation and Different Angiogenic Properties of VEGF and HGF. Cytokine 26, 178–185. doi:10.1016/j.cyto.2004.03.003
Beldi, G., Bahiraii, S., Lezin, C., Nouri Barkestani, M., Abdelgawad, M. E., Uzan, G., et al. (2020a). TNFR2 Is a Crucial Hub Controlling Mesenchymal Stem Cell Biological and Functional Properties. Front. Cel Dev. Biol. 8, 596831. doi:10.3389/fcell.2020.596831
Beldi, G., Khosravi, M., Abdelgawad, M. E., Salomon, B. L., Uzan, G., Haouas, H., et al. (2020b). TNFα/TNFR2 Signaling Pathway: An Active Immune Checkpoint for Mesenchymal Stem Cell Immunoregulatory Function. Stem Cel Res Ther 11, 281. doi:10.1186/s13287-020-01740-5
Bidarimath, M., Khalaj, K., Kridli, R. T., Kan, F. W., Koti, M., and Tayade, C. (2017). Extracellular Vesicle Mediated Intercellular Communication at the Porcine Maternal-Fetal Interface: A New Paradigm for Conceptus-Endometrial Cross-Talk. Sci. Rep. 7, 40476. doi:10.1038/srep40476
Bukovsky, A., and Caudle, M. R. (2012). Immunoregulation of Follicular Renewal, Selection, POF, and Menopause In Vivo, vs. Neo-Oogenesis In Vitro, POF and Ovarian Infertility Treatment, and a Clinical Trial. Reprod. Biol. Endocrinol. 10, 97. doi:10.1186/1477-7827-10-97
Chen, L., Guo, S., Wei, C., Li, H., Wang, H., and Xu, Y. (2018). Effect of Stem Cell Transplantation of Premature Ovarian Failure in Animal Models and Patients: A Meta-Analysis and Case Report. Exp. Ther. Med. 15, 4105–4118. doi:10.3892/etm.2018.5970
Chernyshov, V. P., Radysh, T. V., Gura, I. V., Tatarchuk, T. P., and Khominskaya, Z. B. (2001). Immune Disorders in Women with Premature Ovarian Failure in Initial Period. Am. J. Reprod. Immunol. 46, 220–225. doi:10.1034/j.1600-0897.2001.d01-5.x
Cho, D. I., Kang, W. S., Hong, M. H., Kang, H. J., Kim, M. R., Kim, M. C., et al. (2017). The Optimization of Cell Therapy by Combinational Application with Apicidin-Treated Mesenchymal Stem Cells after Myocardial Infarction. Oncotarget 8, 44281–44294. doi:10.18632/oncotarget.17471
Cho, J., Kim, T.-H., Seok, J., Jun, J. H., Park, H., Kweon, M., et al. (2021). Vascular Remodeling by Placenta-Derived Mesenchymal Stem Cells Restores Ovarian Function in Ovariectomized Rat Model via the VEGF Pathway. Lab. Invest. 101, 304–317. doi:10.1038/s41374-020-00513-1
Ding, C., Zou, Q., Wang, F., Wu, H., Chen, R., Lv, J., et al. (2018). Human Amniotic Mesenchymal Stem Cells Improve Ovarian Function in Natural Aging through Secreting Hepatocyte Growth Factor and Epidermal Growth Factor. Stem Cel Res Ther 9, 55. doi:10.1186/s13287-018-0781-9
Ding, L., Yan, G., Wang, B., Xu, L., Gu, Y., Ru, T., et al. (2018). Transplantation of UC-MSCs on Collagen Scaffold Activates Follicles in Dormant Ovaries of POF Patients with Long History of Infertility. Sci. China Life Sci. 61, 1554–1565. doi:10.1007/s11427-017-9272-2
Dolmans, M.-M., and Donnez, J. (2021). Fertility Preservation in Women for Medical and Social Reasons: Oocytes vs Ovarian Tissue. Best Pract. Res. Clin. Obstet. Gynaecol. 70, 63–80. doi:10.1016/j.bpobgyn.2020.06.011
Dzafic, E., Stimpfel, M., Novakovic, S., Cerkovnik, P., and Virant-Klun, I. (2014). Expression of Mesenchymal Stem Cells-Related Genes and Plasticity of Aspirated Follicular Cells Obtained from Infertile Women. Biomed. Res. Int. 2014, 508216. doi:10.1155/2014/508216
El-Derany, M. O., Said, R. S., and El-Demerdash, E. (2021). Bone Marrow-Derived Mesenchymal Stem Cells Reverse Radiotherapy-Induced Premature Ovarian Failure: Emphasis on Signal Integration of TGF-β, Wnt/β-Catenin and Hippo Pathways. Stem Cel Rev Rep 17, 1429–1445. doi:10.1007/s12015-021-10135-9
Esfandyari, S., Chugh, R. M., Park, H. S., Hobeika, E., Ulin, M., and Al-Hendy, A. (2020). Mesenchymal Stem Cells as a Bio Organ for Treatment of Female Infertility. Cells 9, 2253. doi:10.3390/cells9102253
Fang, J., Wei, Y., Lv, C., Peng, S., Zhao, S., and Hua, J. (2017). CD61 Promotes the Differentiation of Canine ADMSCs into PGC-like Cells through Modulation of TGF-β Signaling. Sci. Rep. 7, 43851. doi:10.1038/srep43851
Field, S. L., Dasgupta, T., Cummings, M., and Orsi, N. M. (2014). Cytokines in Ovarian Folliculogenesis, Oocyte Maturation and Luteinisation. Mol. Reprod. Dev. 81, 284–314. doi:10.1002/mrd.22285
Fu, X., He, Y., Xie, C., and Liu, W. (2008). Bone Marrow Mesenchymal Stem Cell Transplantation Improves Ovarian Function and Structure in Rats with Chemotherapy-Induced Ovarian Damage. Cytotherapy 10, 353–363. doi:10.1080/14653240802035926
Fu, X., He, Y., Wang, X., Peng, D., Chen, X., Li, X., et al. (2017). Overexpression of miR-21 in Stem Cells Improves Ovarian Structure and Function in Rats with Chemotherapy-Induced Ovarian Damage by Targeting PDCD4 and PTEN to Inhibit Granulosa Cell Apoptosis. Stem Cel Res Ther 8, 187. doi:10.1186/s13287-017-0641-z
Fu, Y. X., Ji, J., Shan, F., Li, J., and Hu, R. (2021). Human Mesenchymal Stem Cell Treatment of Premature Ovarian Failure: New Challenges and Opportunities. Stem Cel Res. Ther. 12, 161. doi:10.1186/s13287-021-02212-0
Gabr, H., Rateb, M. A., El Sissy, M. H., Ahmed Seddiek, H., and Ali Abdelhameed Gouda, S. (2016). The Effect of Bone Marrow-Derived Mesenchymal Stem Cells on Chemotherapy Induced Ovarian Failure in Albino Rats. Microsc. Res. Tech. 79, 938–947. doi:10.1002/jemt.22725
Ge, W., Ma, H. G., Cheng, S. F., Sun, Y. C., Sun, L. L., Sun, X. F., et al. (2015). Differentiation of Early Germ Cells from Human Skin-Derived Stem Cells without Exogenous Gene Integration. Sci. Rep. 5, 13822. doi:10.1038/srep13822
Gianchecchi, E., Delfino, D. V., and Fierabracci, A. (2018). NK Cells in Autoimmune Diseases: Linking Innate and Adaptive Immune Responses. Autoimmun. Rev. 17, 142–154. doi:10.1016/j.autrev.2017.11.018
Golocheikine, A., Tiriveedhi, V., Angaswamy, N., Benshoff, N., Sabarinathan, R., and Mohanakumar, T. (2010). Cooperative Signaling for Angiogenesis and Neovascularization by VEGF and HGF Following Islet Transplantation. Transplantation 90, 725–731. doi:10.1097/tp.0b013e3181ef8a63
Gupta, S., Lodha, P., Karthick, M. S., and Tandulwadkar, S. R. (2018). Role of Autologous Bone Marrow-Derived Stem Cell Therapy for Follicular Recruitment in Premature Ovarian Insufficiency: Review of Literature and a Case Report of World's First Baby with Ovarian Autologous Stem Cell Therapy in a Perimenopausal Woman of Age 45 Year. J. Hum. Reprod. Sci. 11, 125–130. doi:10.4103/jhrs.JHRS_57_18
Han, Y., Ren, J., Bai, Y., Pei, X., and Han, Y. (2019). Exosomes from Hypoxia-Treated Human Adipose-Derived Mesenchymal Stem Cells Enhance Angiogenesis through VEGF/VEGF-R. Int. J. Biochem. Cel Biol. 109, 59–68. doi:10.1016/j.biocel.2019.01.017
He, Y., Chen, D., Yang, L., Hou, Q., Ma, H., and Xu, X. (2018). The Therapeutic Potential of Bone Marrow Mesenchymal Stem Cells in Premature Ovarian Failure. Stem Cel Res Ther 9, 263. doi:10.1186/s13287-018-1008-9
Herraiz, S., Romeu, M., Buigues, A., Martínez, S., Díaz-García, C., Gómez-Seguí, I., et al. (2018). Autologous Stem Cell Ovarian Transplantation to Increase Reproductive Potential in Patients Who Are Poor Responders. Fertil. sterility 110, 496–505. doi:10.1016/j.fertnstert.2018.04.025
Herraiz, S., Pellicer, N., Romeu, M., and Pellicer, A. (2019). Treatment Potential of Bone Marrow-Derived Stem Cells in Women with Diminished Ovarian Reserves and Premature Ovarian Failure. Curr. Opin. Obstet. Gynecol. 31, 156–162. doi:10.1097/gco.0000000000000531
Hua, J., Xu, B., Yang, Y., Ban, R., Iqbal, F., Cooke, H. J., et al. (2015). Follicle Online: an Integrated Database of Follicle Assembly, Development and Ovulation. Database 2015, bav036. doi:10.1093/database/bav036
Huang, B., Qian, C., Ding, C., Meng, Q., Zou, Q., and Li, H. (2019). Fetal Liver Mesenchymal Stem Cells Restore Ovarian Function in Premature Ovarian Insufficiency by Targeting MT1. Stem Cel Res Ther 10, 362. doi:10.1186/s13287-019-1490-8
Huhtaniemi, I., Hovatta, O., La Marca, A., Livera, G., Monniaux, D., Persani, L., et al. (2018). Advances in the Molecular Pathophysiology, Genetics, and Treatment of Primary Ovarian Insufficiency. Trends Endocrinol. Metab. 29, 400–419. doi:10.1016/j.tem.2018.03.010
Igboeli, P., El Andaloussi, A., Sheikh, U., Takala, H., ElSharoud, A., McHugh, A., et al. (2020). Intraovarian Injection of Autologous Human Mesenchymal Stem Cells Increases Estrogen Production and Reduces Menopausal Symptoms in Women with Premature Ovarian Failure: Two Case Reports and a Review of the Literature. J. Med. Case Rep. 14, 108. doi:10.1186/s13256-020-02426-5
Imai, A., Furui, T., and Yamamoto, A. (2008). Preservation of Female Fertility during Cancer Treatment. Reprod. Med. Biol. 7, 17–27. doi:10.1111/j.1447-0578.2007.00197.x
Jalalie, L., Rezaie, M. J., Jalili, A., Rezaee, M. A., Vahabzadeh, Z., Rahmani, M. R., et al. (2019). Distribution of the CM-Dil-Labeled Human Umbilical Cord Vein Mesenchymal Stem Cells Migrated to the Cyclophosphamide-Injured Ovaries in C57BL/6 Mice. Iranian Biomed. J. 23, 200–208. doi:10.29252/ibj.23.3.200
Jiang, H. L., Cao, L. Q., and Chen, H. Y. (2018). Protective Effects ROS Up-Regulation on Premature Ovarian Failure by Suppressing ROS-TERT Signal Pathway. Eur. Rev. Med. Pharmacol. Sci. 22, 6198–6204. doi:10.26355/eurrev_201810_16025
Kim, T. H., Choi, J. H., Jun, Y., Lim, S. M., Park, S., Paek, J. Y., et al. (2018). 3D-Cultured Human Placenta-Derived Mesenchymal Stem Cell Spheroids Enhance Ovary Function by Inducing Folliculogenesis. Sci. Rep. 8, 15313. doi:10.1038/s41598-018-33575-9
Knight, P. G., and Glister, C. (2006). TGF-β Superfamily Members and Ovarian Follicle Development. Reproduction 132, 191–206. doi:10.1530/rep.1.01074
Kupcova Skalnikova, H. (2013). Proteomic Techniques for Characterisation of Mesenchymal Stem Cell Secretome. Biochimie 95, 2196–2211. doi:10.1016/j.biochi.2013.07.015
La Marca, A., Brozzetti, A., Sighinolfi, G., Marzotti, S., Volpe, A., and Falorni, A. (2010). Primary Ovarian Insufficiency: Autoimmune Causes. Curr. Opin. Obstet. Gynecol. 22, 277–282. doi:10.1097/gco.0b013e32833b6c70
Lai, D., Wang, F., Dong, Z., and Zhang, Q. (2014). Skin-Derived Mesenchymal Stem Cells Help Restore Function to Ovaries in a Premature Ovarian Failure Mouse Model. PloS one 9, e98749. doi:10.1371/journal.pone.0098749
Lai, D., Wang, F., Yao, X., Zhang, Q., Wu, X., and Xiang, C. (2015). Human Endometrial Mesenchymal Stem Cells Restore Ovarian Function through Improving the Renewal of Germline Stem Cells in a Mouse Model of Premature Ovarian Failure. J. Transl Med. 13, 155. doi:10.1186/s12967-015-0516-y
Laven, J. (2016). Primary Ovarian Insufficiency. Semin. Reprod. Med. 34, 230–234. doi:10.1055/s-0036-1585402
Lee, A. W., Wu, A. H., Wiensch, A., Mukherjee, B., Terry, K. L., Harris, H. R., et al. (2020). Estrogen Plus Progestin Hormone Therapy and Ovarian Cancer. Epidemiology 31, 402–408. doi:10.1097/ede.0000000000001175
Li, B., Liu, W., Zhuang, M., Li, N., Wu, S., Pan, S., et al. (2016). Overexpression of CD61 Promotes hUC-MSC Differentiation into Male Germ-like Cells. Cell Prolif. 49, 36–47. doi:10.1111/cpr.12236
Li, J., Mao, Q., He, J., She, H., Zhang, Z., and Yin, C. (2017). Human Umbilical Cord Mesenchymal Stem Cells Improve the Reserve Function of Perimenopausal Ovary via a Paracrine Mechanism. Stem Cel. Res. Ther. 8 (1), 55. doi:10.1186/s13287-017-0514-5
Li, Z., Zhang, M., Tian, Y., Li, Q., and Huang, X. (2021). Mesenchymal Stem Cells in Premature Ovarian Insufficiency: Mechanisms and Prospects. Front. Cel Dev. Biol. 9, 718192. doi:10.3389/fcell.2021.718192
Liang, C., Jiang, E., Yao, J., Wang, M., Chen, S., Zhou, Z., et al. (2018). Interferon-γ Mediates the Immunosuppression of Bone Marrow Mesenchymal Stem Cells on T-Lymphocytes In Vitro. Hematology 23, 44–49. doi:10.1080/10245332.2017.1333245
Liao, Z., Liu, C., Wang, L., Sui, C., and Zhang, H. (2021). Therapeutic Role of Mesenchymal Stem Cell-Derived Extracellular Vesicles in Female Reproductive Diseases. Front. Endocrinol. 12, 665645. doi:10.3389/fendo.2021.665645
Lin, W., Xu, L., Zwingenberger, S., Gibon, E., Goodman, S. B., and Li, G. (2017). Mesenchymal Stem Cells Homing to Improve Bone Healing. J. orthopaedic translation 9, 19–27. doi:10.1016/j.jot.2017.03.002
Ling, L., Feng, X., Wei, T., Wang, Y., Wang, Y., Zhang, W., et al. (2017). Effects of Low-Intensity Pulsed Ultrasound (LIPUS)-pretreated Human Amnion-Derived Mesenchymal Stem Cell (hAD-MSC) Transplantation on Primary Ovarian Insufficiency in Rats. Stem Cel Res Ther 8, 283. doi:10.1186/s13287-017-0739-3
Ling, L., Feng, X., Wei, T., Wang, Y., Wang, Y., Wang, Z., et al. (2019). Human Amnion-Derived Mesenchymal Stem Cell (hAD-MSC) Transplantation Improves Ovarian Function in Rats with Premature Ovarian Insufficiency (POI) at Least Partly through a Paracrine Mechanism. Stem Cel Res Ther 10, 46. doi:10.1186/s13287-019-1136-x
Liu, J., Zhang, H., Zhang, Y., Li, N., Wen, Y., Cao, F., et al. (2014). Homing and Restorative Effects of Bone Marrow-Derived Mesenchymal Stem Cells on Cisplatin Injured Ovaries in Rats. Mol. Cell 37, 865–872. doi:10.14348/molcells.2014.0145
Liu, S., Wang, J., Han, R., Meng, M., Wang, W., Zhao, Y., et al. (2019a). Therapeutic Effect of Transplanted Umbilical Cord Mesenchymal Stem Cells in a Cynomolgus Monkey Model of Multiple Sclerosis. Am. J. Transl Res. 11, 2516–2531.
Liu, R., Zhang, X., Fan, Z., Wang, Y., Yao, G., Wan, X., et al. (2019b). Human Amniotic Mesenchymal Stem Cells Improve the Follicular Microenvironment to Recover Ovarian Function in Premature Ovarian Failure Mice. Stem Cel Res Ther 10, 299. doi:10.1186/s13287-019-1315-9
Lu, X., Cui, J., Cui, L., Luo, Q., Cao, Q., Yuan, W., et al. (2019). The Effects of Human Umbilical Cord-Derived Mesenchymal Stem Cell Transplantation on Endometrial Receptivity Are Associated with Th1/Th2 Balance Change and uNK Cell Expression of Uterine in Autoimmune Premature Ovarian Failure Mice. Stem Cel Res Ther 10, 214. doi:10.1186/s13287-019-1313-y
Luo, Q., Yin, N., Zhang, L., Yuan, W., Zhao, W., Luan, X., et al. (2017). Role of SDF-1/CXCR4 and Cytokines in the Development of Ovary Injury in Chemotherapy Drug Induced Premature Ovarian Failure Mice. Life Sci. 179, 103–109. doi:10.1016/j.lfs.2017.05.001
Maleki, M., Ghanbarvand, F., Behvarz, M. R., Ejtemaei, M., and Ghadirkhomi, E. (2014). Comparison of Mesenchymal Stem Cell Markers in Multiple Human Adult Stem Cells. Int. J. Stem Cell 7, 118–126. doi:10.15283/ijsc.2014.7.2.118
Manshadi, M. D., Navid, S., Hoshino, Y., Daneshi, E., Noory, P., and Abbasi, M. (2019). The Effects of Human Menstrual Blood Stem Cells‐derived Granulosa Cells on Ovarian Follicle Formation in a Rat Model of Premature Ovarian Failure. Microsc. Res. Tech. 82, 635–642. doi:10.1002/jemt.23120
Mashayekhi, M., Mirzadeh, E., Chekini, Z., Ahmadi, F., Eftekhari-Yazdi, P., Vesali, S., et al. (2021). Evaluation of Safety, Feasibility and Efficacy of Intra-ovarian Transplantation of Autologous Adipose Derived Mesenchymal Stromal Cells in Idiopathic Premature Ovarian Failure Patients: Non-Randomized Clinical Trial, Phase I, First in Human. J. ovarian Res. 14, 5. doi:10.1186/s13048-020-00743-3
Matas, J., Orrego, M., Amenabar, D., Infante, C., Tapia-Limonchi, R., Cadiz, M. I., et al. (2019). Umbilical Cord-Derived Mesenchymal Stromal Cells (MSCs) for Knee Osteoarthritis: Repeated MSC Dosing Is Superior to a Single MSC Dose and to Hyaluronic Acid in a Controlled Randomized Phase I/II Trial. STEM CELLS Translational Med. 8, 215–224. doi:10.1002/sctm.18-0053
Merino-González, C., Zuñiga, F. A., Escudero, C., Ormazabal, V., Reyes, C., Nova-Lamperti, E., et al. (2016). Mesenchymal Stem Cell-Derived Extracellular Vesicles Promote Angiogenesis: Potencial Clinical Application. Front. Physiol. 7, 24. doi:10.3389/fphys.2016.00024
Mohamed, S. A., Shalaby, S. M., Abdelaziz, M., Brakta, S., Hill, W. D., Ismail, N., et al. (2018). Human Mesenchymal Stem Cells Partially Reverse Infertility in Chemotherapy-Induced Ovarian Failure. Reprod. Sci. 25, 51–63. doi:10.1177/1933719117699705
Mu, Y., Wu, X., and Hao, Z. (2018). Comparative Evaluation of Mesenchymal Stromal Cells from Umbilical Cord and Amniotic Membrane in Xeno-free Conditions. BMC Cel Biol 19, 27. doi:10.1186/s12860-018-0178-8
Najar, M., Raicevic, G., Fayyad-Kazan, H., Bron, D., Toungouz, M., and Lagneaux, L. (2016). Mesenchymal Stromal Cells and Immunomodulation: A Gathering of Regulatory Immune Cells. Cytotherapy 18, 160–171. doi:10.1016/j.jcyt.2015.10.011
Nelson, L. (2001). Autoimmune Ovarian Failure: Comparing the Mouse Model and the Human Disease. J. Soc. Gynecol. Investig. 8, S55–S57. doi:10.1016/s1071-5576(00)00110-6
Noory, P., Navid, S., Zanganeh, B. M., Talebi, A., Borhani-Haghighi, M., Gholami, K., et al. (2019). Human Menstrual Blood Stem Cell-Derived Granulosa Cells Participate in Ovarian Follicle Formation in a Rat Model of Premature Ovarian Failure In Vivo. Cell Reprogramming 21, 249–259. doi:10.1089/cell.2019.0020
Pakravan, K., Babashah, S., Sadeghizadeh, M., Mowla, S. J., Mossahebi-Mohammadi, M., Ataei, F., et al. (2017). MicroRNA-100 Shuttled by Mesenchymal Stem Cell-Derived Exosomes Suppresses In Vitro Angiogenesis through Modulating the mTOR/HIF-1α/VEGF Signaling axis in Breast Cancer Cells. Cell Oncol. 40, 457–470. doi:10.1007/s13402-017-0335-7
Park, B.-W., Pan, B., Toms, D., Huynh, E., Byun, J.-H., Lee, Y.-M., et al. (2014). Ovarian-Cell-Like Cells from Skin Stem Cells Restored Estradiol Production and Estrus Cycling in Ovariectomized Mice. Stem Cell Dev. 23, 1647–1658. doi:10.1089/scd.2014.0029
Park, H. S., Ashour, D., Elsharoud, A., Chugh, R. M., Ismail, N., El Andaloussi, A., et al. (2019). Towards Cell Free Therapy of Premature Ovarian Insufficiency: Human Bone Marrow Mesenchymal Stem Cells Secretome Enhances Angiogenesis in Human Ovarian Microvascular Endothelial Cells. HSOA J. Stem Cell Res Dev Ther 5, 19. doi:10.24966/srdt-2060/100019
Park, H. S., Chugh, R. M., Elsharoud, A., Ulin, M., Esfandyari, S., Aboalsoud, A., et al. (2021). Safety of Intraovarian Injection of Human Mesenchymal Stem Cells in a Premature Ovarian Insufficiency Mouse Model. Cel Transplant. 30, 963689720988502. doi:10.1177/0963689720988502
Peng, J., Xiao, N., and Cheng, L. (2018). Therapeutic Potential of BMSCs for Premature Ovarian Failure in Mice. Zhong nan da Xue Xue Bao Yi Xue ban = J. Cent. South Univ. Med. Sci. 43, 7–13. doi:10.11817/j.issn.1672-7347.2018.01.002
Pers, Y.-M., Rackwitz, L., Ferreira, R., Pullig, O., Delfour, C., Barry, F., et al. (2016). Adipose Mesenchymal Stromal Cell-Based Therapy for Severe Osteoarthritis of the Knee: A Phase I Dose-Escalation Trial. Stem Cell translational Med. 5, 847–856. doi:10.5966/sctm.2015-0245
Sakaguchi, S., Mikami, N., Wing, J. B., Tanaka, A., Ichiyama, K., and Ohkura, N. (2020). Regulatory T Cells and Human Disease. Annu. Rev. Immunol. 38, 541–566. doi:10.1146/annurev-immunol-042718-041717
Sanfins, A., Rodrigues, P., and Albertini, D. F. (2018). GDF-9 and BMP-15 Direct the Follicle Symphony. J. Assist. Reprod. Genet. 35, 1741–1750. doi:10.1007/s10815-018-1268-4
Sheikhansari, G., Aghebati-Maleki, L., Nouri, M., Jadidi-Niaragh, F., and Yousefi, M. (2018). Current Approaches for the Treatment of Premature Ovarian Failure with Stem Cell Therapy. Biomed. Pharmacother. 102, 254–262. doi:10.1016/j.biopha.2018.03.056
Shi, Y., Shi, H., Nomi, A., Lei-Lei, Z., Zhang, B., and Qian, H. (2019). Mesenchymal Stem Cell-Derived Extracellular Vesicles: A New Impetus of Promoting Angiogenesis in Tissue Regeneration. Cytotherapy 21, 497–508. doi:10.1016/j.jcyt.2018.11.012
Song, K., Cai, H., Zhang, D., Huang, R., Sun, D., and He, Y. (2018). Effects of Human Adipose-Derived Mesenchymal Stem Cells Combined with Estrogen on Regulatory T Cells in Patients with Premature Ovarian Insufficiency. Int. Immunopharmacology 55, 257–262. doi:10.1016/j.intimp.2017.12.026
Su, J., Xie, Q., Xu, Y., Li, X. C., and Dai, Z. (2014). Role of CD8(+) Regulatory T Cells in Organ Transplantation. Burns Trauma 2, 18–23. doi:10.4103/2321-3868.126086
Sun, M., Wang, S., Li, Y., Yu, L., Gu, F., Wang, C., et al. (2013). Adipose-Derived Stem Cells Improved Mouse Ovary Function after Chemotherapy-Induced Ovary Failure. Stem Cel Res Ther 4, 80. doi:10.1186/scrt231
Sun, L., Li, D., Song, K., Wei, J., Yao, S., Li, Z., et al. (2017). Exosomes Derived from Human Umbilical Cord Mesenchymal Stem Cells Protect against Cisplatin-Induced Ovarian Granulosa Cell Stress and Apoptosis In Vitro. Sci. Rep. 7, 2552. doi:10.1038/s41598-017-02786-x
Sun, B., Ma, Y., Wang, F., Hu, L., and Sun, Y. (2019). miR-644-5p Carried by Bone Mesenchymal Stem Cell-Derived Exosomes Targets Regulation of P53 to Inhibit Ovarian Granulosa Cell Apoptosis. Stem Cel Res Ther 10, 360. doi:10.1186/s13287-019-1442-3
Taheri, M., Saki, G., Nikbakht, R., and Eftekhari, A. R. (2021). Bone Morphogenetic Protein 15 Induces Differentiation of Mesenchymal Stem Cells Derived from Human Follicular Fluid to Oocyte‐Like Cell. Cell Biol Int 45, 127–139. doi:10.1002/cbin.11475
Takehara, Y., Yabuuchi, A., Ezoe, K., Kuroda, T., Yamadera, R., Sano, C., et al. (2013). The Restorative Effects of Adipose-Derived Mesenchymal Stem Cells on Damaged Ovarian Function. Lab. Invest. 93, 181–193. doi:10.1038/labinvest.2012.167
Thakur, M., Feldman, G., and Puscheck, E. E. (2018). Primary Ovarian Insufficiency in Classic Galactosemia: Current Understanding and Future Research Opportunities. J. Assist. Reprod. Genet. 35, 3–16. doi:10.1007/s10815-017-1039-7
Trachana, V., Petrakis, S., Fotiadis, Z., Siska, E. K., Balis, V., Gonos, E. S., et al. (2017). Human Mesenchymal Stem Cells with Enhanced Telomerase Activity Acquire Resistance against Oxidative Stress-Induced Genomic Damage. Cytotherapy 19, 808–820. doi:10.1016/j.jcyt.2017.03.078
Trombly, D. J., Woodruff, T. K., and Mayo, K. E. (2009). Roles for Transforming Growth Factor Beta Superfamily Proteins in Early Folliculogenesis. Semin. Reprod. Med. 27, 14–23. doi:10.1055/s-0028-1108006
Truman, A. M., Tilly, J. L., and Woods, D. C. (2017). Ovarian Regeneration: The Potential for Stem Cell Contribution in the Postnatal Ovary to Sustained Endocrine Function. Mol. Cell. Endocrinol. 445, 74–84. doi:10.1016/j.mce.2016.10.012
Ulin, M., Cetin, E., Hobeika, E., Chugh, R. M., Park, H.-S., Esfandyari, S., et al. (2021). Human Mesenchymal Stem Cell Therapy and Other Novel Treatment Approaches for Premature Ovarian Insufficiency. Reprod. Sci. 28, 1688–1696. doi:10.1007/s43032-021-00528-z
van Kasteren, Y. M., von Blomberg, M., De Koning, C., Lambalk, N., Van Montfrans, J., Schoemaker, J., et al. (2000). Incipient Ovarian Failure and Premature Ovarian Failure Show the Same Immunological Profile. Am. J. Reprod. Immunol. 43, 359–366. doi:10.1111/j.8755-8920.2000.430605.x
Wagner, W. (2019). The Link Between Epigenetic Clocks for Aging and Senescence. Front. Genet. 10, 303. doi:10.3389/fgene.2019.00303
Wang, H., Chen, L., Liu, Y., Luo, B., Xie, N., Tan, T., et al. (2016). Implantation of Placenta-Derived Mesenchymal Stem Cells Accelerates Murine Dermal Wound Closure through Immunomodulation. Am. J. Transl Res. 8, 4912–4921.
Wang, Z., Wang, Y., Yang, T., Li, J., and Yang, X. (2017). Study of the Reparative Effects of Menstrual-Derived Stem Cells on Premature Ovarian Failure in Mice. Stem Cel Res Ther 8, 11. doi:10.1186/s13287-016-0458-1
Wang, P., Lu, Y., Chen, S., Chen, Y., Hu, C., and Zuo, Y. (2018). Protective Function of Bu Shen Huo Xue Formula on the Immunity of B6AF1 Mice with Experimental Autoimmune Premature Ovarian Failure. Exp. Ther. Med. 15, 3302–3310. doi:10.3892/etm.2018.5804
Wang, Z., Wei, Q., Wang, H., Han, L., Dai, H., Qian, X., et al. (2020). Mesenchymal Stem Cell Therapy Using Human Umbilical Cord in a Rat Model of Autoimmune-Induced Premature Ovarian Failure. Stem Cell Int 2020, 3249495. doi:10.1155/2020/3249495
Webber, L., Webber, L., Davies, M., Anderson, R., Bartlett, J., Braat, D., et al. (2016). ESHRE Guideline: Management of Women with Premature Ovarian Insufficiency. Hum. Reprod. 31, 926–937. doi:10.1093/humrep/dew027
Wei, Y., Fang, J., Cai, S., Lv, C., Zhang, S., and Hua, J. (2016). Primordial Germ Cell-like Cells Derived from Canine Adipose Mesenchymal Stem Cells. Cel Prolif. 49, 503–511. doi:10.1111/cpr.12271
Woods, D. C., and Tilly, J. L. (2012). The Next (Re)generation of Ovarian Biology and Fertility in Women: Is Current Science Tomorrow's Practice? Fertil. Sterility 98, 3–10. doi:10.1016/j.fertnstert.2012.05.005
Xia, X., Yin, T., Yan, J., Yan, L., Jin, C., Lu, C., et al. (2015). Mesenchymal Stem Cells Enhance Angiogenesis and Follicle Survival in Human Cryopreserved Ovarian Cortex Transplantation. Cel Transpl. 24, 1999–2010. doi:10.3727/096368914x685267
Xiang, J., Jiang, T., Zhang, W., Xie, W., Tang, X., and Zhang, J. (2019). Human Umbilical Cord-Derived Mesenchymal Stem Cells Enhanced HK-2 Cell Autophagy through MicroRNA-145 by Inhibiting the PI3K/AKT/mTOR Signaling Pathway. Exp. Cel. Res. 378, 198–205. doi:10.1016/j.yexcr.2019.03.019
Xiao, G. Y., Cheng, C. C., Chiang, Y. S., Cheng, W. T., Liu, I. H., and Wu, S. C. (2016). Exosomal miR-10a Derived from Amniotic Fluid Stem Cells Preserves Ovarian Follicles after Chemotherapy. Sci. Rep. 6, 23120. doi:10.1038/srep23120
Yan, L., Wu, Y., Li, L., Wu, J., Zhao, F., Gao, Z., et al. (2020). Clinical Analysis of Human Umbilical Cord Mesenchymal Stem Cell Allotransplantation in Patients with Premature Ovarian Insufficiency. Cell Prolif 53, e12938. doi:10.1111/cpr.12938
Yang, Z., Du, X., Wang, C., Zhang, J., Liu, C., Li, Y., et al. (2019a). Therapeutic Effects of Human Umbilical Cord Mesenchymal Stem Cell-Derived Microvesicles on Premature Ovarian Insufficiency in Mice. Stem Cel Res Ther 10, 250. doi:10.1186/s13287-019-1327-5
Yang, Y., Lei, L., Wang, S., Sheng, X., Yan, G., Xu, L., et al. (2019b). Transplantation of Umbilical Cord-Derived Mesenchymal Stem Cells on a Collagen Scaffold Improves Ovarian Function in a Premature Ovarian Failure Model of Mice. In Vitro Cell.Dev.Biol.-Animal 55, 302–311. doi:10.1007/s11626-019-00337-4
Yang, M., Lin, L., Sha, C., Li, T., Zhao, D., Wei, H., et al. (2020). Bone Marrow Mesenchymal Stem Cell-Derived Exosomal miR-144-5p Improves Rat Ovarian Function after Chemotherapy-Induced Ovarian Failure by Targeting PTEN. Lab. Invest. 100, 342–352. doi:10.1038/s41374-019-0321-y
Yin, N., Zhao, W., Luo, Q., Yuan, W., Luan, X., and Zhang, H. (2018a). Restoring Ovarian Function with Human Placenta-Derived Mesenchymal Stem Cells in Autoimmune-Induced Premature Ovarian Failure Mice Mediated by Treg Cells and Associated Cytokines. Reprod. Sci. 25, 1073–1082. doi:10.1177/1933719117732156
Yin, N., Wang, Y., Lu, X., Liu, R., Zhang, L., Zhao, W., et al. (2018b). hPMSC Transplantation Restoring Ovarian Function in Premature Ovarian Failure Mice Is Associated with Change of Th17/Tc17 and Th17/Treg Cell Ratios through the PI3K/Akt Signal Pathway. Stem Cel Res Ther 9, 37. doi:10.1186/s13287-018-0772-x
Yin, N., Wu, C., Qiu, J., Zhang, Y., Bo, L., Xu, Y., et al. (2020). Protective Properties of Heme Oxygenase-1 Expressed in Umbilical Cord Mesenchymal Stem Cells Help Restore the Ovarian Function of Premature Ovarian Failure Mice through Activating the JNK/Bcl-2 Signal Pathway-Regulated Autophagy and Upregulating the Circulating of CD8+CD28− T Cells. Stem Cel Res Ther 11, 49. doi:10.1186/s13287-019-1537-x
Yoon, S. Y., Yoon, J. A., Park, M., Shin, E.-Y., Jung, S., Lee, J. E., et al. (2020). Recovery of Ovarian Function by Human Embryonic Stem Cell-Derived Mesenchymal Stem Cells in Cisplatin-Induced Premature Ovarian Failure in Mice. Stem Cel Res Ther 11, 255. doi:10.1186/s13287-020-01769-6
Zaher, W., Harkness, L., Jafari, A., and Kassem, M. (2014). An Update of Human Mesenchymal Stem Cell Biology and Their Clinical Uses. Arch. Toxicol. 88, 1069–1082. doi:10.1007/s00204-014-1232-8
Zhang, J., Xiong, J., Fang, L., Lu, Z., Wu, M., Shi, L., et al. (2016). The Protective Effects of Human Umbilical Cord Mesenchymal Stem Cells on Damaged Ovarian Function: A Comparative Study. Biosci. Trends 10, 265–276. doi:10.5582/bst.2016.01125
Zhang, Y., Xia, X., Yan, J., Yan, L., Lu, C., Zhu, X., et al. (2017). Mesenchymal Stem Cell-Derived Angiogenin Promotes Primodial Follicle Survival and Angiogenesis in Transplanted Human Ovarian Tissue. Reprod. Biol. Endocrinol. 15, 18. doi:10.1186/s12958-017-0235-8
Zhang, H., Luo, Q., Lu, X., Yin, N., Zhou, D., Zhang, L., et al. (2018). Effects of hPMSCs on Granulosa Cell Apoptosis and AMH Expression and Their Role in the Restoration of Ovary Function in Premature Ovarian Failure Mice. Stem Cel Res Ther 9, 20. doi:10.1186/s13287-017-0745-5
Zhang, J., Yin, H., Jiang, H., Du, X., and Yang, Z. (2020a). The Protective Effects of Human Umbilical Cord Mesenchymal Stem Cell-Derived Extracellular Vesicles on Cisplatin-Damaged Granulosa Cells. Taiwanese J. Obstet. Gynecol. 59, 527–533. doi:10.1016/j.tjog.2020.05.010
Zhang, X.-M., Liu, C.-Y., and Shao, Z.-H. (2020b). Advances in the Role of Helper T Cells in Autoimmune Diseases. Chin. Med. J. 133, 968–974. doi:10.1097/cm9.0000000000000748
Zhao, L., Chen, S., Yang, P., Cao, H., and Li, L. (2019). The Role of Mesenchymal Stem Cells in Hematopoietic Stem Cell Transplantation: Prevention and Treatment of Graft-Versus-Host Disease. Stem Cel Res Ther 10, 182. doi:10.1186/s13287-019-1287-9
Zheng, Q., Fu, X., Jiang, J., Zhang, N., Zou, L., Wang, W., et al. (2019). Umbilical Cord Mesenchymal Stem Cell Transplantation Prevents Chemotherapy-Induced Ovarian Failure via the NGF/TrkA Pathway in Rats. Biomed. Res. Int. 2019, 6539294. doi:10.1155/2019/6539294
Zhou, Y., Yamamoto, Y., Xiao, Z., and Ochiya, T. (2019). The Immunomodulatory Functions of Mesenchymal Stromal/Stem Cells Mediated via Paracrine Activity. J. Clin. Med. 8, 1025. doi:10.3390/jcm8071025
Glossary
ADMSC adipose-derived stem cells
AFMSC amniotic fluid mesenchymal stem cells
akt protein kinase B
AMH anti-mullerian hormone
AMPK adenosine 5‘-monophosphate (AMP)-activated protein kinase
AMSC amniotic mesenchymal stem cells
ARE antioxidant response element
AZPAb anti-Zona pellucida antibody
Bax Bcl-2 associated X protein
Bcl-2 B-cell lymphoma-2
b-FGF basic fibroblast growth factor
BDNF brain-derived neurotrophic factor
Bim Bcl-2 interacting mediator of cell death
BMP bone morphogenetic protein
BMSC bone marrow stem cells
CD cluster of differentiation
EGF epidermal growth factor epidermal growth factor
E2 estrogen
EGF epidermal growth factor epidermal growth factor
FGF fibroblast growth factor
FOXO forkhead box O
FSH follicle stimulating hormone
FSHR follicle stimulating hormone receptor
fst homo sapiens follistatin
GC ovarian granulosa cells granulosa cells
GC ovarian granulosa cells granulosa cells
GCSF granulocyte colony stimulating factor
Gdf growth differentiation factor
HGF hepatocyte growth factor
HOVEC human ovarian endothelial cell
HRT hormone replacement therapy
IDO indoleamine 2,3-dioxygenase
IGF-1 insulin-like growth factors-1
IFN-γ interferon γ
IRAK1 interleukin 1 receptor associated Kinase 1
IL interleukin-10
JNK1 jun n-terminal kinase1
LH luteinizing hormone
LIF interleukin 6 family cytokine
MAPK mitogen-activated protein kinase
MCP monocyte chemotactic protein
Mensc menstrual-derived stem cell
MSC mesenchymal stem cells
MVs microvesicles
MT1 melatonine receptor1
Nanos3 nanos C2HC-type Zinc finger 3
NF-κB nuclear factor kappa-light-chain-enhancer of activated B cells
NK natural killer cell
Nobox NOBOX oogenesis homeobox
NO nitric oxide
NOQ1 NAD(P)H quinone dehydrogenase 1
Nrf2 NF-E2-related factor 2
OGCs ovarian granulosa cells
PARP poly ADP-ribose polymerase
PCNA proliferating cell nuclear antigen
PDCD4 programmed cell death 4
PDMSC placenta-derived mesenchymal stem cells
PGF placental growth factor
PGE2 prostaglandin E2
PGC primordial germ cell
PMSC placenta-derived mesenchymal stem cell
POF premature ovarian failure
PTEN phosphatase and tensin homolog
PI3K phosphatidylinositol-3-kinase
ROS reactive oxygen species
SC stem cell
SOD1 superoxide dismutase 1
TERT telomerase reverse transcriptase
TGF transforming growth factor
th helper T cell
TNF-α tumor necrosis factor-α
TRAF632 receptor associated factor 632
UCMSC umbilical cord mesenchymal stem cells
UCP-2 uncoupling protein-2
VEGF vascular endothelial growth factor
VEGFR vascular endothelial growth factor
Keywords: mesenchymal stem cells, fertility, premature ovarian failure (POF), ovarian dysfunction, reproductive medicine
Citation: Wang J, Liu W, Yu D, Yang Z, Li S and Sun X (2021) Research Progress on the Treatment of Premature Ovarian Failure Using Mesenchymal Stem Cells: A Literature Review. Front. Cell Dev. Biol. 9:749822. doi: 10.3389/fcell.2021.749822
Received: 30 July 2021; Accepted: 29 November 2021;
Published: 13 December 2021.
Edited by:
Rebecca Ryznar, Rocky Vista University, United StatesReviewed by:
Sina Naserian, Hôpital Paul Brousse, FranceMohammad Ghasemzadeh-H, University of Glasgow, United Kingdom
Copyright © 2021 Wang, Liu, Yu, Yang, Li and Sun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiguang Sun, eGdzdW5Aamx1LmVkdS5jbg==
 Jing Wang
Jing Wang Wanru Liu
Wanru Liu Dehai Yu
Dehai Yu Zongxing Yang
Zongxing Yang Sijie Li
Sijie Li Xiguang Sun
Xiguang Sun