
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
MINI REVIEW article
Front. Cell Dev. Biol. , 24 November 2020
Sec. Cellular Biochemistry
Volume 8 - 2020 | https://doi.org/10.3389/fcell.2020.584696
This article is part of the Research Topic Developmental Biology and Regulation of Osteoclasts View all 16 articles
Erythropoietin (EPO) is expressed primarily in fetal liver and adult kidney to stimulate red blood cell production. Erythropoietin receptor expression is not restricted to erythroid progenitor cells, and non-erythroid EPO activity includes immune response and bone remodeling. In bone fracture models, EPO administration promotes bone formation and accelerates bone healing. In contrast, in healthy adult mice, exogenous EPO-stimulated erythropoiesis has been concomitant with bone loss, particularly at high EPO, that may be accompanied by increased osteoclast activation. Other EPO-associated responses include reduced inflammation and loss of fat mass with high-fat diet feeding, especially in male mice. While EPO exhibited a sex-dimorphic response in regulation of fat mass and inflammation in obese mice, EPO-stimulated erythropoiesis as well as EPO-associated bone loss was comparable in males and females. EPO administration in young mice and in obese mice resulted in bone loss without increasing osteoclasts, suggesting an osteoclast-independent mechanism, while loss of endogenous EPO decreased bone development and maintenance. Ossicle formation of bone marrow stromal cell transplants showed that EPO directly regulates the balance between osteogenesis and adipogenesis. Therefore, during development, endogenous EPO contributes to normal bone development and in maintaining the balance between osteogenesis and adipogenesis in bone marrow stromal cells, while EPO treatment in mice increased erythropoiesis, promoted bone loss, decreased bone marrow adipogenesis, and increased osteoclast activity. These observations in mouse models suggest that the most prevalent use of EPO to treat anemia associated with chronic kidney disease may compromise bone health and increase fracture risk, especially at a high dose.
Erythropoietin (EPO) regulates red blood cell production, and recombinant EPO is used primarily to treat anemia in chronic kidney disease. EPO can stimulate additional non-erythroid cell response mediated by erythropoietin receptor (EPOR) expression in other hematopoietic cells and non-hematopoietic tissues including white adipose tissue (WAT), brain, and bone (Suresh et al., 2019b). In mice, EPO treatment is associated with anti-inflammatory activity, neuroprotection, cardioprotection, skeletal muscle wound healing, protection against diet-induced obesity (Zhang et al., 2014; Suresh et al., 2019b), and bone loss accompanying EPO-stimulated erythropoiesis (Hiram-Bab et al., 2015; Suresh et al., 2019a). Hormones, cytokines, and growth factors can influence osteoblast and osteoclast differentiation, bone remodeling, and macrophage immune response, and the resultant production of inflammatory cytokines can modulate osteoclast differentiation and bone resorption activity (Sinder et al., 2015; Adamopoulos, 2018; Kubatzky et al., 2018). Here we describe the EPO response of cells derived from the monocyte–macrophage lineage such as the anti-inflammatory EPO response during diet-induced obesity in white adipose tissue and brain and the osteoclasts associated with EPO-stimulated bone loss. We also include a discussion of EPO effects on fat accumulation during diet-induced obesity and on bone marrow stromal cells associated with EPO-stimulated bone loss.
The estrogen-dependent EPO activity was first identified with EPO angiogenic response in the uterus during the mouse estrus cycle (Yasuda et al., 1998). Among non-hematopoietic tissues, EPOR has a relatively high expression in brain and adipose tissue. The EPO-stimulated hypoxic ventilatory response in brain and carotid body is also sex dimorphic and is increased in females compared with males in human and mouse (Soliz et al., 2012). With respect to adipose tissue, mice with erythroid-restricted EPOR expression show a disproportionate accumulation of fat mass that is greater in females that develop obesity and insulin resistance at a younger age compared with their male counterpart (Teng et al., 2011).
C57BL/6 mice fed a high-fat diet develop an obese phenotype and inflammation in WAT. With obesity, the macrophages in WAT stromal vascular fraction shift from an anti-inflammatory toward a pro-inflammatory phenotype, decrease the secretion of the anti-inflammatory cytokine IL-10 that enhances adipocyte insulin sensitivity, and increase the expression of inflammatory cytokines, TNFα, and IL-6, contributing to insulin resistance (Lumeng et al., 2007; Lauterbach and Wunderlich, 2017). The increased WAT inflammation and macrophage infiltration result in crown-like structures, which are macrophages surrounding necrotic or dying adipocytes, indicating the proinflammatory state of adipose tissue.
In mice, EPO contributes directly to metabolic homeostasis by maintenance of WAT. During high-fat-diet feeding, EPO treatment protects against glucose intolerance, insulin resistance, WAT inflammation, and fat mass accumulation, particularly in male mice (Wang et al., 2014; Zhang et al., 2014; Alnaeeli and Noguchi, 2015). In WAT, EPOR is highly expressed in adipocytes and primarily in macrophages in the stromal vascular fraction (Alnaeeli et al., 2014; Alnaeeli and Noguchi, 2015). EPO treatment significantly reduced the inflammation in WAT, macrophage infiltration, and crown-like structures and promoted an anti-inflammatory phenotype (Alnaeeli et al., 2014). EPO directly stimulated EPOR-expressing macrophages by activating STAT3, reducing proinflammatory gene expression and increasing IL-10 expression. The protective effect of endogenous EPO in metabolic control was demonstrated in mice with EPOR restricted to erythroid tissue (Suzuki et al., 2002). Subjected to high-fat-diet-induced obesity, these mice with similar body weight and fat mass as wild-type mice had greater glucose intolerance and insulin resistance, increased WAT inflammation and macrophage infiltration, enhanced crown-like structures, and increased inflammatory cytokine production (Alnaeeli et al., 2014). In the liver, EPO inhibited gluconeogenesis, attenuated obesity-related inflammatory cytokine expression and production of TNF-α and IL-6, reduced the activation of NFκB and inflammatory signaling, and enhanced insulin-related PI3K signaling (Meng et al., 2013). In the pancreas, EPO exerted JAK2-dependent protective effects in pancreatic β-cells and induced proliferative, anti-inflammatory, and angiogenic activity within the islets in diabetic mouse models (Choi et al., 2010).
The expansion of adipose tissue requires increased adipose tissue vasculature to maintain appropriate blood flow to supply oxygen and nutrients. A deficit in adipose tissue angiogenesis may contribute to insulin resistance and metabolic disease (Corvera and Gealekman, 2014). It has been suggested that vascular dysfunction resulting in adipose tissue hypoxia may lead to obesity-associated inflammation and occur before insulin resistance (Ye, 2011). Adipose tissue vasculature has been considered as a potential target for type 2 diabetes (Corvera and Gealekman, 2014). In retinoic acid treatment, activation of the brown fat-associated program in white adipocytes was mediated by vascular endothelial growth factor-stimulated angiogenesis (Wang et al., 2017). With exercise, vascularization in subcutaneous WAT is increased and may mediate an improved metabolic response (Min et al., 2019). EPO exhibits angiogenic and neovascularization activity in animal models (Yasuda et al., 1998; Ribatti et al., 1999; Kertesz et al., 2004; Wang et al., 2004; Li et al., 2007). EPO treatment in patients with Friedreich ataxia suggested the possibility for EPO to increase capillary density in skeletal muscle (Nachbauer et al., 2012). Further investigation is warranted to determine whether EPO treatment promotes vascularization, particularly in white adipose tissue, to contribute to a potentially beneficial metabolic response.
Exogenous EPO treatment for 3 to 4 weeks in male, but not female, C57BL/6 mice reduced fat mass accumulation (Zhang et al., 2017). EPO treatment during high-fat-diet feeding in male mice increased the expression of genes PRDM16 and UCP1 associated with brown adipocyte differentiation in both brown fat and white fat (Wang et al., 2013; Kodo et al., 2017). This sex-dimorphic activity of EPO fat mass regulation is attributed to the anti-obesity effect of estrogen that interferes with EPO regulation of fat mass. In contrast to acute EPO treatment, long-term EPO treatment is able to regulate fat mass and body weight in both genders. Male and female transgenic mice with chronically increased EPO production have decreased body weight (Katz et al., 2010). Increased EPO expression by gene electrotransfer in skeletal muscle resulted in a 100-fold increase in serum EPO. By 12 weeks after the electrotransfer in female obese mice, fat mass was reduced by 28% (Hojman et al., 2009). The transfected muscle showed increased muscle volume and vascularization. However, in mice with mixed strain background, the absence of EPO receptor expression in WAT did not have any effect on adipocyte regulation (Luk et al., 2013).
The interference of estrogen with EPO regulation of fat mass was demonstrated by acute EPO treatment in ovariectomized female mice on high-fat diet that decreased fat mass accumulation, but not when combined with estradiol supplementation (Zhang et al., 2017). EPO regulation of fat mass is associated with increased activity and decreased food intake mediated by EPOR expression in non-hematopoietic tissue, especially in WAT adipocytes and in the brain (Zhang et al., 2017; Dey et al., 2020). EPOR expression in the hypothalamus arcuate nucleus localizes with proopiomelanocortin (POMC) neurons that, when stimulated, produces POMC to suppress appetite (Teng et al., 2011). EPO administration increases POMC expression in the hypothalamus and in POMC neural cell cultures (Teng et al., 2011; Dey et al., 2016). Male mice with EPOR restricted to erythroid cells exhibit increased hematocrit and reduced POMC expression, and EPO administration in these mice does not alter fat mass or POMC expression (Teng et al., 2011).
Erythropoietin is produced in the brain by astrocytes and neurons contributing to intrinsic hypoxic response (Marti et al., 1997; Bernaudin et al., 2000; Shingo et al., 2001). In animal models, a neuroprotective effect is associated with EPO activity in the brain, and EPO reduces neuronal cell death and inflammation associated with brain ischemia, with a decrease in astrocyte activation, recruitment of microglia, and proinflammatory cytokine production (Villa et al., 2003). High-fat-diet-induced obesity in mice also increases inflammation in the hypothalamus, activation of microglial cells, and inflammatory cytokine production. Hypothalamus inflammation is linked to a disruption of energy homeostasis and contributes to obesity, insulin resistance, and glucose intolerance (Jais and Bruning, 2017). Increased EPO in the brain, either by cerebral transgenic EPO expression (Tg21-mice) or by implanted EPO secreting intracerebral ventricular pump in mice, reduced fat mass accumulation during high-fat-diet feeding, reduced hypothalamus inflammation, and prevented myeloid cell recruitment to the hypothalamus in males. The unchanged hematocrit in these mice suggested an insufficient transport of EPO across the blood–brain barrier to affect EPO-stimulated erythropoiesis and showed that cerebral EPO regulation of fat mass and hypothalamus inflammation is independent of EPO-stimulated erythropoiesis (Dey et al., 2020). In contrast, deletion of EPOR in neural cells using the Nestin-Cre transgenic model showed increased weight gain, hypothalamus inflammation, and inflammatory cytokine expression in male mice, indicating that endogenous cerebral EPO also contributes to the protection against weight gain and hypothalamus inflammation during diet-induced obesity (Dey et al., 2020).
A sex-dimorphic response of cerebral EPO regulation during diet-induced obesity resulted from estrogen blocking the protective effects of EPO signaling in the brain on fat mass accumulation and hypothalamus inflammation during high-fat-diet feeding in female mice. In female ovariectomized Tg21-mice, increased EPO levels in the brain regulated body weight and hypothalamus inflammation during high-fat diet, while no such changes were evident in female non-ovariectomized Tg21-mice or in female mice with Nestin-Cre deletion of EPOR in neural cells (Dey et al., 2020). While elevated EPO improves glucose tolerance in both male and female mice, EPO regulation of fat mass accumulation and inflammation during diet-induced obesity, mediated in part via activity in WAT and the hypothalamus, appears to be sex specific.
Lineage tracing studies for EPOR expression using the Epo-R-Cre and yellow fluorescent protein reporter mice showed 75% labeling efficiency of Ter119+ cells. This suggested erythroid specificity for EPOR expression in the bone marrow microenvironment, with no yellow fluorescent protein expression in hematopoietic stem cells, B-lymphoid or myeloid lineages, or mesenchymal- and osteoblastic-enriched populations (Singbrant et al., 2011). However, other reports showed that bone marrow stromal cells (BMSCs) expressed EPOR mRNA and EPOR protein by flow cytometry and were EPO responsive in culture, resulting in induced osteoblastic differentiation with increased mineral deposition and alkaline phosphatase activity. EPO also stimulated osteoclastogenesis of preosteoclasts in culture (Shiozawa et al., 2010; Hiram-Bab et al., 2015). EPOR expression on BMSCs, osteoblasts, and osteoclasts thus adds to the increasing select non-erythroid cells that respond to EPO, mediated via EPOR cell surface expression (Shiozawa et al., 2010; Hiram-Bab et al., 2015; Suresh et al., 2019a, 2020b).
Mice with EPOR restricted to erythroid tissue (ΔEpoRE), generated by rescuing the EPOR knockout mouse with an erythroid EPOR transgene driven by the GATA1 locus hematopoietic regulatory domain, demonstrated the requirement for EPO/EPOR signaling in normal bone development (Suresh et al., 2019a). These ΔEpoRE-mice lacked EPOR expression in BMSCs and osteoblasts, and in cultures, these osteoblasts had reduced differentiation and mineralization. ΔEpoRE-mice had reduced trabecular bone and no significant changes in cortical bone, suggesting that endogenous EPO–EPOR signaling is essential for proper bone development (Table 1). The ΔEpoRE-mice showed excessive marrow adiposity (Suresh et al., 2019a). Enhanced marrow adipogenesis is often observed with reduced osteogenesis, suggesting an imbalance in the differentiation of BMSCs (Muruganandan et al., 2018). Ectopic ossification assays in immunodeficient mice using wild-type BMSCs with intact EPO–EPOR signaling formed ossicles with a defined outer cortical bone, interspersed with trabeculae and marrow containing hematopoietic cells and adipocytes. ΔEpoRE-BMSCs formed ossicles with a cortical bone similar to control cells but with reduced trabecular bone and increased marrow adipocytes. These studies conclusively showed that endogenous EPO–EPOR signaling is essential in regulating normal differentiation and the lineage commitment of BMSCs, with a specific role in the development and the maintenance of the trabecular bone.
Mice with EPOR deletion, specifically in mature osteoblasts, using the Osteocalcin-Cre system demonstrated the contribution of osteoblast direct response to EPO in bone development and remodeling (Suresh et al., 2020b). Both male and female mice had normal hematocrits and a significant reduction in trabecular bone volume, with the cortical bone unaffected (Table 1). The osteoprogenitors derived from calvaria had reduced differentiation and mineralization potential in cultures similar to the ΔEpoRE-mice. This study showed endogenous EPO–EPOR signaling in osteoblasts as an essential mechanism integral for the development of the trabecular bone (Figure 1).
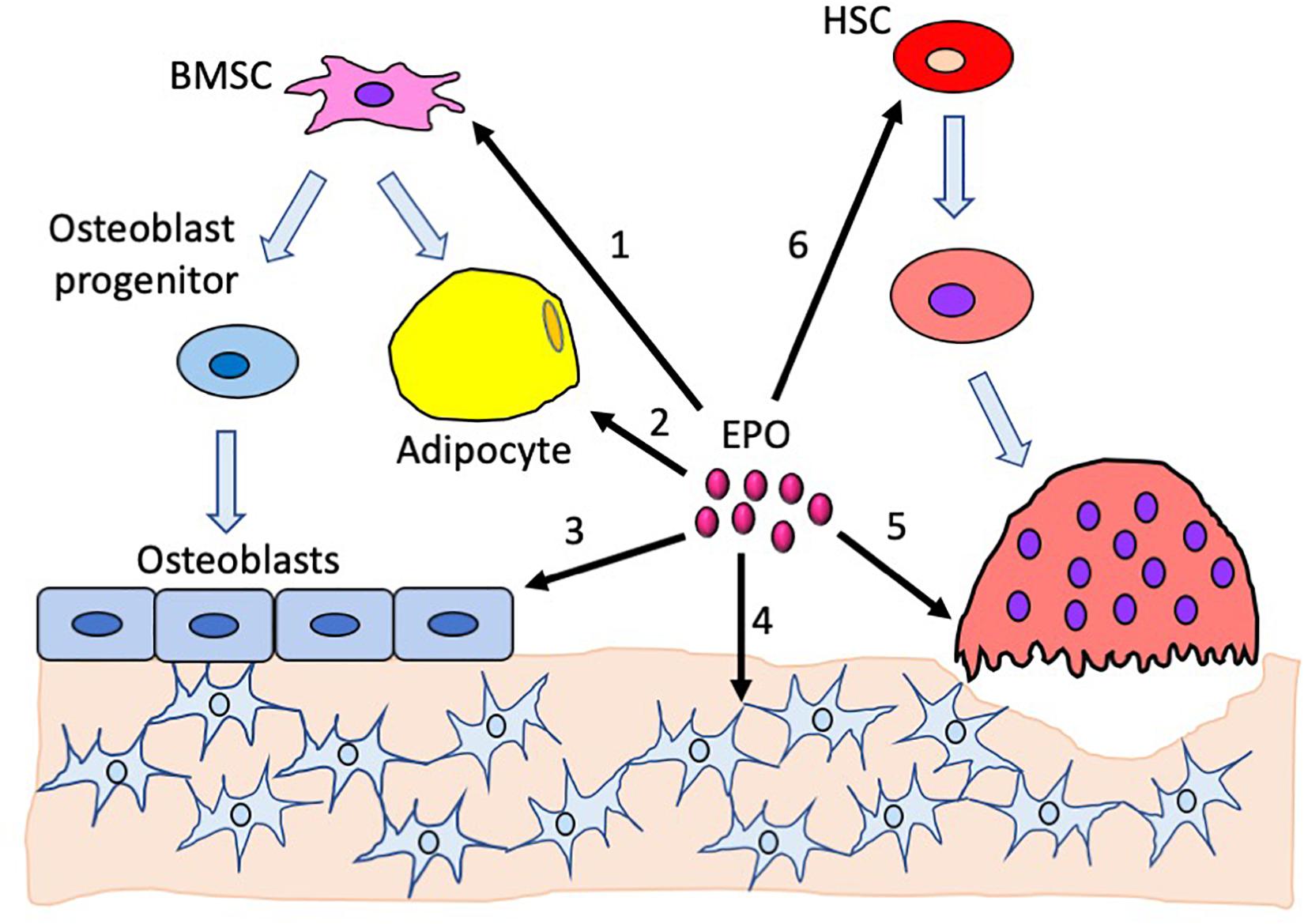
Figure 1. Effects of erythropoietin in the bone and the bone marrow compartment. 1. Endogenous EPO regulates bone marrow stromal cell differentiation to adipocytes and osteoblasts. 2. Increased EPO decreases bone marrow adipocytes. 3. EPO directly regulates osteoblast differentiation; the absence of EPO signaling in osteoblasts reduces their differentiation potential. Elevated EPO has a dose-dependent effect on osteoblasts, with low-dose EPO reducing differentiation and high-dose EPO increasing differentiation. 4. Absence of EPO signaling in mature osteoblasts reduces osteocytes, resulting in empty lacunae. 5. High EPO stimulates differentiation of preosteoclasts into osteoclasts. 6. EPO stimulates hematopoietic stem cells which, in turn, promotes both osteoblast and osteoclast differentiation.
Studies focusing on the role of EPO in bone have utilized mouse models treated with recombinant human EPO either at physiological or elevated doses for acute EPO effects or the transgenic mouse model Tg6 with constitutive overexpression of human EPO to explore the chronic effects of elevated EPO (Singbrant et al., 2011; Hiram-Bab et al., 2015; Suresh et al., 2019a). Modulation of endogenous EPO signaling in mice with Von Hippel–Lindau (VHL) mutation in osteoblasts caused an increase in hypoxia inducible factor-1/2 (HIF), resulting in elevated EPO production in osteoblasts and polycythemia (Rankin et al., 2012). In these mice, even with significant expansion of erythropoiesis, trabecular bone volume was increased. The targeted deletion of prolyl hydroxylase (PHD) in osteoblasts also induced osteoblast production of EPO and increased hematocrit, demonstrating that manipulation of the PHD/VHL/HIF pathway in osteoblasts in mice alters endogenous EPO production, elevates hematocrit, and affects bone formation. In contrast, mice with deletion of VHL, HIF-1, and HIF-2 in osteoblasts exhibited reduced EPO levels and low trabecular bone volume, with HIF-2 being the critical HIF-regulating EPO in bone (Rankin et al., 2012). In mice with PHD2 deletion in renal cells, macrophages, neural cells, and astrocytes, there was a significant reduction of bone volume due to reduced bone formation (Rauner et al., 2016). Increased EPO levels were observed in mice with PHD2 deletion, and the conditional deletion of HIF-2α in this model rescued the loss of bone. These mice exhibit increased hematocrits and elevated EPO; however, the high levels of EPO did not increase osteoclast differentiation or drive bone resorption as seen in the Tg6 mouse model, which also has chronically elevated EPO (Hiram-Bab et al., 2015). PHD2 deletion specifically in osteoblasts, however, increased bone density by reducing osteoclasts, showing that the loss of PHD2 in osteoblasts is not essential for bone reduction (Rauner et al., 2016).
The effects of elevated EPO in bone metabolism appear controversial as EPO treatment has resulted in a gain in bone density and volume in some models while reducing bone in others, suggesting a context-dependent role for EPO in bone remodeling (Hiram-Bab et al., 2017; Suresh et al., 2019b). In animal models of bone fracture, EPO treatment significantly accelerated bone healing (Holstein et al., 2007; Mihmanli et al., 2009; Rolfing et al., 2014b; Omlor et al., 2016). The process of new bone formation occurs in two ways: by endochondral ossification, where cartilage is replaced by bone tissue as seen in long bones, or by intramembranous ossification, where mesenchyme is converted to osteoblasts as seen in the formation of flat bones like the skull and the clavicle (Breeland et al., 2019). Studies done in murine fracture models showed that EPO administration promotes endochondral ossification and aids in the healing process. In cranial bone fracture models where the bone is usually repaired by intramembranous ossification, EPO administration along with bone morphogenetic protein 2 (BMP2) resulted in new bone formation by endochondral process along with increased angiogenesis possibly mediated by EPO (Sun et al., 2012). The HIF signaling pathway has also been shown to be important in EPO-stimulated repair of osteonecrosis in rat models, as EPO administration increased the expression of alkaline phosphatase, HIF-1α, runt-related transcription factor 2, and vascular endothelial growth factor (Li et al., 2018).
While EPO primarily regulates red blood cell production, most of the studies with EPO administration in healthy mouse models of different ages show a reduction in bone volume accompanying the increase in hematocrit (Singbrant et al., 2011; Hiram-Bab et al., 2015; Suresh et al., 2019a). However, in contrast to these reports, another study reported an increase in bone formation in the vertebrae of both newborn and 4–6-week-old mice receiving supraphysiological doses of EPO with a modest increase in hematocrits (Shiozawa et al., 2010; Table 1). Unlike EPO regulation of fat mass and inflammation associated with diet-induced obesity, EPO-stimulated bone loss in mice does not appear to exhibit gender bias. Chronic exposure of EPO severely disrupts bone microarchitecture as demonstrated by Tg6-mice expressing a high level of transgenic human EPO (Hiram-Bab et al., 2015). Tg6-mice show reduced trabecular bone, cortical bone mineral density, cortical bone volume (Oikonomidou et al., 2016; Suresh et al., 2019a), and thickness (Hiram-Bab et al., 2015; Table 1). Excess EPO in these mice reduces osteoblast-dependent mineral apposition and bone formation rate while simultaneously increasing the osteoclast numbers (Hiram-Bab et al., 2015). BMSCs from Tg6-mice had high EPO expression and, in ectopic ossification assays in immunodeficient mice, formed markedly reduced ossicles without a defined structure or significant bone or adipocytes (Suresh et al., 2019a). The direct effects of EPO on BMSCs were shown using culture studies, where adding EPO less than 5 U/ml to primary mouse BMSC cultures inhibited osteogenic differentiation, while elevated doses of EPO between 50 and 250 U/ml increased their osteogenic differentiation potential (Rauner et al., 2016). Osteogenic differentiation assays of BMSCs in the presence of EPO have been reported to activate EphrinB2/EphrinB4 (Li et al., 2015) mTOR (Kim et al., 2012) and JAK2/PI3K pathways (Rolfing et al., 2014a). In BMSC cultures and in vivo, the administration of EPO increased BMP2 expression in hematopoietic stem cells, which have been suggested to increase osteoclasts initially, followed by a rise in osteoblast numbers (Shiozawa et al., 2010). Wnt signaling has been proposed to mediate EPO effects in non-hematopoietic cells. Endothelial cell cultures exposed to elevated glucose suggested that EPO cytoprotection was mediated via Wnt1 and inhibition of glycogen synthase kinase activity (Chong et al., 2007). This led to the suggestion of potential application of EPO and Wnt signaling for the prevention of neurovascular injury associated with diabetes mellitus (Maiese, 2008). In human bone marrow-derived mesenchymal stem cell cultures, EPO induced neurogenic differentiation, especially at reduced oxygen, and stimulated increased Wnt3a- and Wnt3a-mediated EPO neuroprotection against glutamate toxicity (Danielyan et al., 2009). Wnt signaling was also shown to mediate the EPO-stimulated differentiation of mesenchymal stromal cells to osteoblasts. In cultures of human bone marrow mesenchymal stromal cells from young donors, EPO stimulated osteoblast-specific gene expression and osteoblast mineralization, but not in cultures from patients with myelodysplastic syndromes and old healthy donors that exhibited a reduced expression of genes associated with the canonical Wnt pathway. Activation of the Wnt pathway in these cells restored EPO-associated osteoblast differentiation (Balaian et al., 2018).
The polycythemia mouse model with JAK2 V617F mutation in hematopoietic cells gives rise to constitutively active EPOR, low EPO concentrations in the serum, low trabecular bone volume, and reduced osteoblast number (Oikonomidou et al., 2016). Thus, both low and elevated EPO or EPOR activation impaired osteoblast differentiation and function. In patients with thalassemia, low bone mass developing into osteoporosis is a common complication due to a myriad of factors like excess ineffective erythropoiesis, iron overload, or endocrine dysfunction seen during the disease (Wong et al., 2016). A mouse model of β-thalassemia major th3 has high serum EPO levels (Rivella et al., 2003), reduced trabecular bone volume, and thin cortical bone (Vogiatzi et al., 2010). These mice provide examples of increased EPO or EPOR signaling, resulting in increased erythropoiesis and decreased bone formation or bone loss. However, while exogenous EPO administration increased hematocrit in ΔEpoRE-mice, there was no accompanying reduction in trabecular bone (Suresh et al., 2019a), suggesting that EPO-stimulated bone loss is mediated by non-hematopoietic response and independent of increased erythropoiesis. In female mice lacking EPOR signaling in osteoblasts, exogenous EPO administration did not reduce trabecular bone volume, while in male mice a similar treatment resulted in only a trend for reduced trabeculae (Suresh et al., 2020b; Table 1). These findings show that bone loss during EPO-stimulated erythropoiesis is mediated in part by direct EPO–EPOR signaling in osteoblasts.
In cocultures of bone marrow monocytes and calvarial osteoblasts, addition of both EPO and erythroblasts did not stimulate osteoclast differentiation (Singbrant et al., 2011). However, in bone marrow-derived cultures, EPO did not affect preosteoclast proliferation but increased osteoclast differentiation via JAK2 and PI3K pathways (Hiram-Bab et al., 2015). EPO stimulated osteoclastogenesis in culture even at a low dose (Hiram-Bab et al., 2017). Other studies using bone marrow-derived cultures showed that EPO increased the osteoclast numbers, but not activity (Shiozawa et al., 2010). An osteoclast differentiation assay of RAW264.7 mouse monocyte/macrophage cell line similarly shows that EPO increased the osteoclast numbers, but not osteoclast activity (Li et al., 2015). It was suggested that EPO contributes to the communication between differentiation of osteoclasts and osteoblasts through the EphrinB2/EphrinB4 signaling pathway and increases the number of EphrinB2-expressing osteoclasts and EphrinB4 expression in ST2 stromal cells to promote osteoblastic differentiation that may play a role in bone formation (Li et al., 2015). EPO-stimulated osteoclastogenesis in bone marrow mononuclear cell cultures and RAW264.7 cells was mTOR signaling dependent, but the increased expression of the master transcription regulator of osteoclast differentiation NFATC1 in EPO-treated osteoclasts was independent of mTOR signaling in RAW264.7 cells (Kim et al., 2012; Kim and Kim, 2014).
Bone loss with elevated EPO has been associated with EPO-stimulated osteoclastogenesis (Hiram-Bab et al., 2015). Tg6-mice with elevated EPO have an increased bone marrow preosteoclast number, with 25% more osteoclasts per bone surface, and increased serum levels of bone resorption marker TRAP5b. Increased preosteoclast and osteoclast numbers and TRAP5b serum levels were also observed with EPO treatment in wild-type mice (Singbrant et al., 2011; Hiram-Bab et al., 2015). The increase in osteoclasts in mice with EPO stimulation has been reported to be dependent on the duration of EPO exposure, as a 2-week EPO administration increased the osteoclasts which appeared to decline with two more weeks of EPO treatment (Shiozawa et al., 2010). HIF signaling has also been shown to be important in osteoclast function. Inactivation of PHD in osteoblasts, leading to the specific activation of HIF-1α, has been associated with an increased production of osteoprotegerin, which blocks RANKL and RANK interaction to limit osteoclast differentiation (Shao et al., 2015), and increased interleukin-33 to reduce bone marrow-derived monocyte osteoclastic differentiation (Kang et al., 2017). Since PHD inactivation in osteoblasts increased HIF-2α and EPO (Rankin et al., 2012), these observations suggest that hypoxia induction of EPO may also restrict the expansion of osteoclastogenesis in support of other osteoclast-independent mechanisms contributing to EPO-stimulated bone loss.
Studies on the role of EPO signaling in osteoclasts showed elevated EPO directly stimulating osteoclasts in C57BL6/J mice treated with EPO and in Tg6-mice with chronically elevated EPO resulting in bone loss (Hiram-Bab et al., 2015). However, other studies observed reduction in bone volume but without an increase in osteoclast activity in C57BL/6 mice given exogenous EPO (Suresh et al., 2019a) or in C57BL/6 mice transplanted with bone marrow from Tg6-mice to induce polycythemia (Oikonomidou et al., 2016). The polycythemia JAK2V617F mouse model with constitutively active EPOR has reduced bone and normal osteoclast numbers (Oikonomidou et al., 2016). β-Thalassemia major th3 mouse model with high serum EPO and reduced bone exhibits decreased bone formation and resorption, suggesting overall reduction in bone remodeling (Rivella et al., 2003). The reduced osteoclast numbers in these mice show that elevated EPO stimulating osteoclasts is not always required for bone loss.
ΔEpoRE-mice were developed for erythroid-restricted expression of EPOR (Suzuki et al., 2002), but the presence of GATA1 hematopoietic regulatory domain in the preosteoclasts results in EPOR expression in these cells (Suresh et al., 2019a). The presence of EPO–EPOR signaling in osteoclasts and its absence in other key bone regulatory cells like BMSCs and osteoblasts led to some interesting observations of endogenous EPO signaling in osteoclasts depending on the age of the mice. As ΔEpoRE-mice age, accumulation of excess fat mass due to the absence of endogenous EPO signaling in WAT results in increased systemic inflammation (Teng et al., 2011). The body weight of young ΔEpoRE-mice (8 weeks) was comparable to that of wild-type mice, and these young ΔEpoRE-mice did not have any increase in osteoclasts on their bone surface. However, at this age, these mice have a reduced trabecular number with increased spacing, indicating an early disruption of trabecular microarchitecture, but bone mineral density and volume were unaffected (Suresh et al., 2019a). By 11 weeks of age, ΔEpoRE-mice gain substantial body weight due to increased body fat mass and have about 40% reduction in trabecular bone volume and increased osteoclasts, in both male and female mice. Thus, in young ΔEpoRE-mice, reduction in bone is an osteoclast-independent mechanism. This study shows that dysregulation of WAT stemming from lack of EPO signaling results in inflammation and increased osteoclastogenesis with age, which adversely affects the bone.
In mice, the effects of EPO signaling in the bone have been largely studied in the trabecular bone compartment which comprises 20% of bone mass and is interspersed with bone marrow and adipocytes, with a higher remodeling rate than the cortical bone (Singbrant et al., 2011; Hiram-Bab et al., 2015; Suresh et al., 2019a). The cortical bone is stiffer but brittle and is essential for maintaining structure and mechanical loading (Ott, 2018). In C57BL/6J mice fed a high-fat diet, EPO administration showed distinct effects in trabecular and cortical bone compartments (Suresh et al., 2020a). On regular chow diet, daily EPO administration for 10 days reduced the trabecular bone and the cortical bone volumes, with a reduction of cortical bone osteocytes and periosteal osteoblasts surrounding the cortical bone (Suresh et al., 2019a). In contrast, the cortical bone in mice on high-fat diet was unaffected by EPO administration, but excessive marrow fat accumulation in these mice was completely abrogated by EPO administration. High-fat-diet feeding increased the osteoclast numbers but was not further increased with EPO treatment (Suresh et al., 2020a). Therefore, EPO-induced reduction of bone can affect various types of cells in the bone and marrow compartment under different dietary conditions.
Studies in animal models show that, beyond stimulating erythropoiesis, EPO can also regulate fat mass and monocyte–macrophage-derived cell response in obesity-associated inflammation and bone remodeling. The potential for EPO to regulate fat mass and the increase in EPO production at high altitude may contribute to the lower obesity rate observed in humans residing at a high altitude (Voss et al., 2014; Diaz-Gutierrez et al., 2016). Sex-dimorphic EPO response is related to estrogen in female mice, which interferes with EPO protective activity in fat mass regulation and obesity-related inflammation. The relationship between EPO and body weight in humans is suggested in a subset analysis of full-heritage Pima Indians with a high prevalence of obesity and type 2 diabetes. This study showed that endogenous plasma EPO negatively associated with percent weight change per year in males, while the females exhibited a positive association (Reinhardt et al., 2016). In the bone, EPO activity is mediated via osteoclast-dependent and osteoclast-independent mechanisms and can affect bone healing or stimulate bone loss with increased erythropoiesis (Figure 1). Wild-type mice with EPO administration exhibit both increased erythropoiesis and bone loss, while mouse models with EPOR deletion, either in non-hematopoietic cells or specifically in osteoblasts, have increased erythropoiesis but no accompanying bone loss. Consistent with EPO promoting bone healing in animal models of fracture, a pilot study in 60 patients with tibiofibular factures who received either EPO or saline showed patients in the EPO receiving arm having faster union rates by a couple of weeks and reduced nonunion fracture (Bakhshi et al., 2013). However, in a recent study, high EPO level was also associated with higher fracture risk independent of hemoglobin and age in elderly Swedish men (Kristjansdottir et al., 2020), suggesting that, as observed in mice, EPO may also affect bone homeostasis, and chronic EPO treatment may impact on bone health. EPO stimulated FGF23 production in mouse and human, increasing serum FGF23 and reducing serum phosphate, and may contribute to elevated FGF23 in chronic kidney disease patients receiving EPO (Clinkenbeard et al., 2017). Increased FGF23 in response to EPO administration has been suggested as a possible mechanism of EPO-induced bone reduction associated with disrupted mineralization (Clinkenbeard et al., 2017). EPOR expression in non-erythroid tissues, including BMSCs, adipocytes, osteoblasts and osteoclasts, contributes to EPO activity independent of erythropoiesis that regulates bone formation and bone marrow microenvironment (Suresh et al., 2019a, 2020b). These activities demonstrated in animal models suggest that, while some non-hematopoietic EPO responses may be protective, bone health may be adversely affected with chronic EPO treatment such as that associated with chronic kidney disease.
SS, JL, and CN contributed to the planning, writing, and editing of this manuscript. All authors contributed to the article and approved the submitted version.
This work was supported by the Intramural Research Program of the National Institute of Diabetes and Digestive and Kidney Diseases at the National Institutes of Health.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Adamopoulos, I. E. (2018). Inflammation in bone physiology and pathology. Curr. Opin. Rheumatol. 30, 59–64. doi: 10.1097/bor.0000000000000449
Alnaeeli, M., and Noguchi, C. T. (2015). Erythropoietin and obesity-induced white adipose tissue inflammation: redefining the boundaries of the immunometabolism territory. Adipocyte 4, 153–157. doi: 10.4161/21623945.2014.978654
Alnaeeli, M., Raaka, B. M., Gavrilova, O., Teng, R., Chanturiya, T., and Noguchi, C. T. (2014). Erythropoietin signaling: a novel regulator of white adipose tissue inflammation during diet-induced obesity. Diabetes 63, 2415–2431. doi: 10.2337/db13-0883
Bakhshi, H., Kazemian, G., Emami, M., Nemati, A., Karimi Yarandi, H., and Safdari, F. (2013). Local erythropoietin injection in tibiofibular fracture healing. Trauma. Mon. 17, 386–388. doi: 10.5812/traumamon.7099
Balaian, E., Wobus, M., Weidner, H., Baschant, U., Stiehler, M., and Ehninger, G. (2018). Erythropoietin inhibits osteoblast function in myelodysplastic syndromes via the canonical Wnt pathway. Haematologica 103, 61–68. doi: 10.3324/haematol.2017.172726
Bernaudin, M., Bellail, A., Marti, H. H., Yvon, A., Vivien, D., Duchatelle, I., et al. (2000). Neurons and astrocytes express EPO mRNA: oxygen-sensing mechanisms that involve the redox-state of the brain. Glia 30, 271–278. doi: 10.1002/(sici)1098-1136(200005)30:3<271::aid-glia6>3.0.co;2-h
Breeland, G., Sinkler, M. A., and Menezes, R. G. (2019). Embryology, Bone Ossification. Treasure Island, FL: StatPearls Publishing.
Choi, D., Schroer, S. A., Lu, S. Y., Wang, L., Wu, X., Liu, Y., et al. (2010). Erythropoietin protects against diabetes through direct effects on pancreatic beta cells. J. Exp. Med. 207, 2831–2842. doi: 10.1084/jem.20100665
Chong, Z. Z., Shang, Y. C., and Maiese, K. (2007). Vascular injury during elevated glucose can be mitigated by erythropoietin and Wnt signaling. Curr. Neurovasc. Res. 4, 194–204. doi: 10.2174/156720207781387150
Clinkenbeard, E. L., Hanudel, M. R., Stayrook, K. R., Appaiah, H. N., Farrow, E. G., and Cass, T. A. (2017). Erythropoietin stimulates murine and human fibroblast growth factor-23, revealing novel roles for bone and bone marrow. Haematologica 102, 427–430e.
Corvera, S., and Gealekman, O. (2014). Adipose tissue angiogenesis: impact on obesity and type-2 diabetes. Biochim. Biophys. Acta 1842, 463–472. doi: 10.1016/j.bbadis.2013.06.003
Danielyan, L., Schafer, R., Schulz, A., Ladewig, T., Lourhmati, A., and Buadze, M. (2009). Survival, neuron-like differentiation and functionality of mesenchymal stem cells in neurotoxic environment: the critical role of erythropoietin. Cell Death Differ. 16, 1599–1614. doi: 10.1038/cdd.2009.95
Dey, S., Cui, Z., Gavrilova, O., Zhang, X., Gassmann, M., and Noguchi, C. T. (2020). Sex-specific brain erythropoietin regulation of mouse metabolism and hypothalamic inflammation. JCI Insight 5:e134061.
Dey, S., Li, X., Teng, R., Alnaeeli, M., Chen, Z., Rogers, H., et al. (2016). Erythropoietin regulates POMC expression via STAT3 and potentiates leptin response. J. Mol. Endocrinol. 56, 55–67. doi: 10.1530/jme-15-0171
Diaz-Gutierrez, J., Martinez-Gonzalez, M. A., Pons Izquierdo, J. J., Gonzalez-Muniesa, P., Martinez, J. A., and Bes-Rastrollo, M. (2016). Living at Higher Altitude and Incidence of Overweight/Obesity: Prospective Analysis of the SUN Cohort. PLoS One 11:e0164483. doi: 10.1371/journal.pone.0164483
Hiram-Bab, S., Liron, T., Deshet-Unger, N., Mittelman, M., Gassmann, M., Rauner, M., et al. (2015). Erythropoietin directly stimulates osteoclast precursors and induces bone loss. FASEB J. 29, 1890–1900. doi: 10.1096/fj.14-259085
Hiram-Bab, S., Neumann, D., and Gabet, Y. (2017). Context-Dependent Skeletal Effects of Erythropoietin. Vitam. Horm. 105, 161–179. doi: 10.1016/bs.vh.2017.02.003
Hojman, P., Brolin, C., Gissel, H., Brandt, C., Zerahn, B., Pedersen, B. K., et al. (2009). Erythropoietin over-expression protects against diet-induced obesity in mice through increased fat oxidation in muscles. PLoS One 4:e5894. doi: 10.1371/journal.pone.0005894
Holstein, J. H., Menger, M. D., Scheuer, C., Meier, C., Culemann, U., Wirbel, R. J., et al. (2007). Erythropoietin (EPO): EPO-receptor signaling improves early endochondral ossification and mechanical strength in fracture healing. Life Sci. 80, 893–900. doi: 10.1016/j.lfs.2006.11.023
Jais, A., and Bruning, J. C. (2017). Hypothalamic inflammation in obesity and metabolic disease. J. Clin. Invest. 127, 24–32. doi: 10.1172/jci88878
Kang, H., Yang, K., Xiao, L., Guo, L., Guo, C., and Yan, Y. (2017). Osteoblast Hypoxia-Inducible Factor-1alpha Pathway Activation Restrains Osteoclastogenesis via the Interleukin-33-MicroRNA-34a-Notch1 Pathway. Front. Immunol. 8:1312. doi: 10.3389/fimmu.2017.01312
Katz, O., Stuible, M., Golishevski, N., Lifshitz, L., Tremblay, M. L., Gassmann, M., et al. (2010). Erythropoietin treatment leads to reduced blood glucose levels and body mass: insights from murine models. J. Endocrinol. 205, 87–95. doi: 10.1677/joe-09-0425
Kertesz, N., Wu, J., Chen, T. H., Sucov, H. M., and Wu, H. (2004). The role of erythropoietin in regulating angiogenesis. Dev. Biol. 276, 101–110. doi: 10.1016/j.ydbio.2004.08.025
Kim, J. H., and Kim, N. (2014). Regulation of NFATc1 in Osteoclast Differentiation. J. Bone Metab. 21, 233–241. doi: 10.11005/jbm.2014.21.4.233
Kim, J., Jung, Y., Sun, H., Joseph, J., Mishra, A., Shiozawa, Y., et al. (2012). Erythropoietin mediated bone formation is regulated by mTOR signaling. J. Cell Biochem. 113, 220–228. doi: 10.1002/jcb.23347
Kodo, K., Sugimoto, S., Nakajima, H., Mori, J., Itoh, I., Fukuhara, S., et al. (2017). Erythropoietin (EPO) ameliorates obesity and glucose homeostasis by promoting thermogenesis and endocrine function of classical brown adipose tissue (BAT) in diet-induced obese mice. PLoS One 12:e0173661. doi: 10.1371/journal.pone.0173661
Kristjansdottir, H. L., Lewerin, C., Lerner, U. H., Herlitz, H., Johansson, P., and Johansson, H. (2020). High Plasma Erythropoietin Predicts Incident Fractures in Elderly Men with Normal Renal Function: The MrOS Sweden Cohort. J. Bone Miner. Res. 35, 298–305. doi: 10.1002/jbmr.3900
Kubatzky, K. F., Uhle, F., and Eigenbrod, T. (2018). From macrophage to osteoclast - How metabolism determines function and activity. Cytokine 112, 102–115. doi: 10.1016/j.cyto.2018.06.013
Lauterbach, M. A., and Wunderlich, F. T. (2017). Macrophage function in obesity-induced inflammation and insulin resistance. Pflugers Arch. 469, 385–396. doi: 10.1007/s00424-017-1955-5
Li, C., Shi, C., Kim, J., Chen, Y., Ni, S., Jiang, L., et al. (2015). Erythropoietin promotes bone formation through EphrinB2/EphB4 signaling. J. Dent. Res. 94, 455–463. doi: 10.1177/0022034514566431
Li, D., Hu, Q., Tan, G., Xie, X., Yang, Z., and Kang, P. (2018). Erythropoietin Enhances Bone Repair Effects via the Hypoxia-Inducible Factor Signal Pathway in Glucocorticoid-Induced Osteonecrosis of the Femoral Head. Am. J. Med. Sci. 355, 597–606. doi: 10.1016/j.amjms.2018.03.010
Li, Y., Lu, Z., Keogh, C. L., Yu, S. P., and Wei, L. (2007). Erythropoietin-induced neurovascular protection, angiogenesis, and cerebral blood flow restoration after focal ischemia in mice. J. Cereb Blood Flow Metab. 27, 1043–1054. doi: 10.1038/sj.jcbfm.9600417
Luk, C. T., Shi, S. Y., Choi, D., Cai, E. P., Schroer, S. A., and Woo, M. (2013). In vivo knockdown of adipocyte erythropoietin receptor does not alter glucose or energy homeostasis. Endocrinology 154, 3652–3659. doi: 10.1210/en.2013-1113
Lumeng, C. N., Bodzin, J. L., and Saltiel, A. R. (2007). Obesity induces a phenotypic switch in adipose tissue macrophage polarization. J. Clin. Invest. 117, 175–184. doi: 10.1172/jci29881
Maiese, K. (2008). Triple play: promoting neurovascular longevity with nicotinamide, WNT, and erythropoietin in diabetes mellitus. Biomed. Pharmacother. 62, 218–232. doi: 10.1016/j.biopha.2008.01.009
Marti, H. H., Gassmann, M., Wenger, R. H., Kvietikova, I., Morganti-Kossmann, M. C., Kossmann, T., et al. (1997). Detection of erythropoietin in human liquor: intrinsic erythropoietin production in the brain. Kidney Int. 51, 416–418. doi: 10.1038/ki.1997.55
Meng, R., Zhu, D., Bi, Y., Yang, D., and Wang, Y. (2013). Erythropoietin inhibits gluconeogenesis and inflammation in the liver and improves glucose intolerance in high-fat diet-fed mice. PLoS One 8:e53557. doi: 10.1371/journal.pone.0053557
Mihmanli, A., Dolanmaz, D., Avunduk, M. C., and Erdemli, E. (2009). Effects of recombinant human erythropoietin on mandibular distraction osteogenesis. J. Oral. Maxillofac. Surg. 67, 2337–2343. doi: 10.1016/j.joms.2008.06.082
Min, S. Y., Learnard, H., Kant, S., Gealikman, O., Rojas-Rodriguez, R., DeSouza, T., et al. (2019). Exercise Rescues Gene Pathways Involved in Vascular Expansion and Promotes Functional Angiogenesis in Subcutaneous White Adipose Tissue. Int. J. Mol. Sci. 20:2046. doi: 10.3390/ijms20082046
Muruganandan, S., Govindarajan, R., and Sinal, C. J. (2018). Bone Marrow Adipose Tissue and Skeletal Health. Curr. Osteoporos Rep. 16, 434–442. doi: 10.1007/s11914-018-0451-y
Nachbauer, W., Boesch, S., Reindl, M., Eigentler, A., Hufler, K., Poewe, W., et al. (2012). Skeletal muscle involvement in friedreich ataxia and potential effects of recombinant human erythropoietin administration on muscle regeneration and neovascularization. J. Neuropathol. Exp. Neurol. 71, 708–715. doi: 10.1097/nen.0b013e31825fed76
Oikonomidou, P. R., Casu, C., Yang, Z., Crielaard, B., Shim, J. H., Rivella, S., et al. (2016). Polycythemia is associated with bone loss and reduced osteoblast activity in mice. Osteoporos. Int. 27, 1559–1568. doi: 10.1007/s00198-015-3412-7
Omlor, G. W., Kleinschmidt, K., Gantz, S., Speicher, A., Guehring, T., and Richter, W. (2016). Increased bone formation in a rabbit long-bone defect model after single local and single systemic application of erythropoietin. Acta Orthop. 87, 425–431. doi: 10.1080/17453674.2016.1198200
Ott, S. M. (2018). Cortical or Trabecular Bone: What’s the Difference? Am. J. Nephrol. 47, 373–375. doi: 10.1159/000489672
Rankin, E. B., Wu, C., Khatri, R., Wilson, T. L., Andersen, R., Araldi, E., et al. (2012). The HIF signaling pathway in osteoblasts directly modulates erythropoiesis through the production of EPO. Cell 149, 63–74. doi: 10.1016/j.cell.2012.01.051
Rauner, M., Franke, K., Murray, M., Singh, R. P., Hiram-Bab, S., Platzbecker, U., et al. (2016). Increased EPO Levels Are Associated With Bone Loss in Mice Lacking PHD2 in EPO-Producing Cells. J. Bone Miner. Res. 31, 1877–1887. doi: 10.1002/jbmr.2857
Reinhardt, M., Dey, S., Tom Noguchi, C., Zhang, Y., Krakoff, J., and Thearle, M. S. (2016). Non-hematopoietic effects of endogenous erythropoietin on lean mass and body weight regulation. Obesity 24, 1530–1536. doi: 10.1002/oby.21537
Ribatti, D., Presta, M., Vacca, A., Ria, R., Giuliani, R., Dell’Era, P., et al. (1999). Human erythropoietin induces a pro-angiogenic phenotype in cultured endothelial cells and stimulates neovascularization in vivo. Blood 93, 2627–2636. doi: 10.1182/blood.v93.8.2627.408k21_2627_2636
Rivella, S., May, C., Chadburn, A., Riviere, I., and Sadelain, M. (2003). A novel murine model of Cooley anemia and its rescue by lentiviral-mediated human beta-globin gene transfer. Blood 101, 2932–2939. doi: 10.1182/blood-2002-10-3305
Rolfing, J. H., Baatrup, A., Stiehler, M., Jensen, J., Lysdahl, H., and Bunger, C. (2014a). The osteogenic effect of erythropoietin on human mesenchymal stromal cells is dose-dependent and involves non-hematopoietic receptors and multiple intracellular signaling pathways. Stem Cell Rev. Rep. 10, 69–78. doi: 10.1007/s12015-013-9476-x
Rolfing, J. H., Jensen, J., Jensen, J. N., Greve, A. S., Lysdahl, H., Chen, M., et al. (2014b). A single topical dose of erythropoietin applied on a collagen carrier enhances calvarial bone healing in pigs. Acta Orthop. 85, 201–209. doi: 10.3109/17453674.2014.889981
Shao, J., Zhang, Y., Yang, T., Qi, J., Zhang, L., and Deng, L. (2015). HIF-1alpha disturbs osteoblasts and osteoclasts coupling in bone remodeling by up-regulating OPG expression. Vitro. Cell Dev. Biol. Anim. 51, 808–814. doi: 10.1007/s11626-015-9895-x
Shingo, T., Sorokan, S. T., Shimazaki, T., and Weiss, S. (2001). Erythropoietin regulates the in vitro and in vivo production of neuronal progenitors by mammalian forebrain neural stem cells. J. Neurosci. 21, 9733–9743. doi: 10.1523/jneurosci.21-24-09733.2001
Shiozawa, Y., Jung, Y., Ziegler, A. M., Pedersen, E. A., Wang, J., Wang, Z., et al. (2010). Erythropoietin couples hematopoiesis with bone formation. PLoS One 5:e10853. doi: 10.1371/journal.pone.0010853
Sinder, B. P., Pettit, A. R., and McCauley, L. K. (2015). Macrophages: Their Emerging Roles in Bone. J. Bone Miner. Res. 30, 2140–2149. doi: 10.1002/jbmr.2735
Singbrant, S., Russell, M. R., Jovic, T., Liddicoat, B., Izon, D. J., Purton, L. E., et al. (2011). Erythropoietin couples erythropoiesis, B-lymphopoiesis, and bone homeostasis within the bone marrow microenvironment. Blood 117, 5631–5642. doi: 10.1182/blood-2010-11-320564
Soliz, J., Khemiri, H., Caravagna, C., and Seaborn, T. (2012). Erythropoietin and the sex-dimorphic chemoreflex pathway. Adv. Exp. Med. Biol. 758, 55–62. doi: 10.1007/978-94-007-4584-1_8
Sun, H., Jung, Y., Shiozawa, Y., Taichman, R. S., and Krebsbach, P. H. (2012). Erythropoietin modulates the structure of bone morphogenetic protein 2-engineered cranial bone. Tissue Eng. Part A 18, 2095–2105. doi: 10.1089/ten.tea.2011.0742
Suresh, S., Alvarez, J. C., Dey, S., and Noguchi, C. T. (2020a). Erythropoietin-Induced Changes in Bone and Bone Marrow in Mouse Models of Diet-Induced Obesity. Int. J. Mol. Sci. 21:1657. doi: 10.3390/ijms21051657
Suresh, S., de Castro, L. F., Dey, S., Robey, P. G., and Noguchi, C. T. (2019a). Erythropoietin modulates bone marrow stromal cell differentiation. Bone Res. 7:21.
Suresh, S., Lee, J., and Noguchi, C. T. (2020b). Erythropoietin signaling in osteoblasts is required for normal bone formation and for bone loss during erythropoietin-stimulated erythropoiesis. FASEB J. 00, 1–13. doi: 10.1016/s8756-3282(02)00716-0
Suresh, S., Rajvanshi, P. K., and Noguchi, C. T. (2019b). The Many Facets of Erythropoietin Physiologic and Metabolic Response. Front. Physiol. 10:1534. doi: 10.3389/fphys.2019.01534
Suzuki, N., Ohneda, O., Takahashi, S., Higuchi, M., Mukai, H. Y., Nakahata, T., et al. (2002). Erythroid-specific expression of the erythropoietin receptor rescued its null mutant mice from lethality. Blood 100, 2279–2288. doi: 10.1182/blood-2002-01-0124
Teng, R., Gavrilova, O., Suzuki, N., Chanturiya, T., Schimel, D., Hugendubler, L., et al. (2011). Disrupted erythropoietin signalling promotes obesity and alters hypothalamus proopiomelanocortin production. Nat. Commun. 2:520.
Villa, P., Bigini, P., Mennini, T., Agnello, D., Laragione, T., Cagnotto, A., et al. (2003). Erythropoietin selectively attenuates cytokine production and inflammation in cerebral ischemia by targeting neuronal apoptosis. J. Exp. Med. 198, 971–975. doi: 10.1084/jem.20021067
Vogiatzi, M. G., Tsay, J., Verdelis, K., Rivella, S., Grady, R. W., Doty, S., et al. (2010). Changes in bone microarchitecture and biomechanical properties in the th3 thalassemia mouse are associated with decreased bone turnover and occur during the period of bone accrual. Calcif. Tissue Int. 86, 484–494. doi: 10.1007/s00223-010-9365-0
Voss, J. D., Allison, D. B., Webber, B. J., Otto, J. L., and Clark, L. L. (2014). Lower obesity rate during residence at high altitude among a military population with frequent migration: a quasi experimental model for investigating spatial causation. PLoS One 9:e93493. doi: 10.1371/journal.pone.0093493
Wang, B., Fu, X., Liang, X., Deavila, J. M., Wang, Z., Zhao, L., et al. (2017). Retinoic acid induces white adipose tissue browning by increasing adipose vascularity and inducing beige adipogenesis of PDGFRalpha(+) adipose progenitors. Cell Discov. 3:17036.
Wang, L., Di, L., and Noguchi, C. T. (2014). Erythropoietin, a novel versatile player regulating energy metabolism beyond the erythroid system. Int. J. Biol. Sci. 10, 921–939. doi: 10.7150/ijbs.9518
Wang, L., Teng, R., Di, L., Rogers, H., Wu, H., Kopp, J. B., et al. (2013). PPARalpha and Sirt1 mediate erythropoietin action in increasing metabolic activity and browning of white adipocytes to protect against obesity and metabolic disorders. Diabetes 62, 4122–4131. doi: 10.2337/db13-0518
Wang, L., Zhang, Z., Wang, Y., Zhang, R., and Chopp, M. (2004). Treatment of stroke with erythropoietin enhances neurogenesis and angiogenesis and improves neurological function in rats. Stroke 35, 1732–1737. doi: 10.1161/01.str.0000132196.49028.a4
Wong, P., Fuller, P. J., Gillespie, M. T., and Milat, F. (2016). Bone Disease in Thalassemia: A Molecular and Clinical Overview. Endocr. Rev. 37, 320–346. doi: 10.1210/er.2015-1105
Yasuda, Y., Masuda, S., Chikuma, M., Inoue, K., Nagao, M., and Sasaki, R. (1998). Estrogen-dependent production of erythropoietin in uterus and its implication in uterine angiogenesis. J. Biol. Chem. 273, 25381–25387. doi: 10.1074/jbc.273.39.25381
Ye, J. (2011). Adipose tissue vascularization: its role in chronic inflammation. Curr. Diab. Rep. 11, 203–210. doi: 10.1007/s11892-011-0183-1
Zhang, Y., Rogers, H. M., Zhang, X., and Noguchi, C. T. (2017). Sex difference in mouse metabolic response to erythropoietin. FASEB J. 31, 2661–2673. doi: 10.1096/fj.201601223rrr
Keywords: brain, fat, macrophage, osteoclast, osteoblast, bone, erythropoietin, microglial
Citation: Suresh S, Lee J and Noguchi CT (2020) Effects of Erythropoietin in White Adipose Tissue and Bone Microenvironment. Front. Cell Dev. Biol. 8:584696. doi: 10.3389/fcell.2020.584696
Received: 17 July 2020; Accepted: 20 October 2020;
Published: 24 November 2020.
Edited by:
Natalie A. Sims, The University of Melbourne, AustraliaReviewed by:
Martina Rauner, Dresden University of Technology, GermanyCopyright © 2020 Suresh, Lee and Noguchi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Constance Tom Noguchi, Y29ubmllbkBuaWRkay5uaWguZ292
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.