- 1Department of Pediatrics, Rainbow Babies and Children's Hospital, Cleveland, OH, United States
- 2Department of Medicine, University of the Incarnate Word School of Osteopathic Medicine, San Antonio, TX, United States
- 3Department of Pediatric Cardiology, Children's Hospital of San Antonio / Baylor College of Medicine, San Antonio, TX, United States
- 4Department of Pediatric Cardiology, Rainbow Babies and Children's Hospital, Cleveland, OH, United States
Circumflex right aortic arch is a rare aortic arch anomaly where the arch extends in a retro-esophageal pattern with a left-sided descending thoracic aorta. In the setting of circumflex right aortic arch with the ductus arteriosus connecting the left descending aorta and left pulmonary artery, a vascular ring is present and can cause compressive symptoms of the aerodigestive tract. A 33-year-old G4P3 patient underwent fetal echocardiography after obstetric ultrasound showed concern for double aortic arch. Fetal echocardiogram was suspicious for vascular ring with presumptive diagnosis of double aortic arch vs. circumflex right aortic arch. The child was born at 38 weeks gestation via induced vaginal delivery and had an uneventful postnatal course. Post-natal echocardiogram was able to diagnose vascular ring but could not fully assess the arch or branching pattern. Cardiac computed tomography angiography (CCTA) was able to definitively diagnose right aortic arch and characterize the branching pattern. To our knowledge, this is the first case reported in the literature of a circumflex right aortic arch suspected on fetal echocardiogram and postnatal echocardiogram and subsequently confirmed with CCTA. Fetal echocardiogram provides a unique opportunity to assess the aortic arch as the trachea is filled with fluid. However, circumflex aortic arch and double aortic arch can be difficult to delineate on fetal or post-natal echocardiography. CCTA is an effective modality for evaluation of the aortic arch and its branching pattern in the setting of non-diagnostic echocardiography.
Introduction
Circumflex aortic arch is a rare form of aortic arch anomaly where a portion of the arch extends behind the esophagus while the ascending and descending aortic segments are located on the contralateral side of the spine (1). Circumflex right aortic arch refers to a retro-esophageal right aortic arch (passing over the right main bronchus to the right of the trachea and esophagus) and left-sided descending thoracic aorta. A typical vascular ring occurs in the presence of a right circumflex aortic arch with left ductus arteriosus from the descending aorta to the left pulmonary artery. This arch anomaly is extremely rare, particularly when associated with a vascular ring, which results in compressive symptoms of the aerodigestive tract during childhood (2).
In this report, we present a case of a newborn with circumflex right aortic arch first suspected on fetal echocardiogram and confirmed with post-natal imaging. Circumflex retro-esophageal aortic arch poses a diagnostic challenge and can be indistinguishable from a double aortic arch with an atretic segment on both fetal sonography and post-natal echocardiogram (3). Cardiac computed tomography angiography (CCTA) was helpful in the diagnosis as well as evaluation of the aerodigestive tract. From our extensive literature review, there are six reports on cases of a circumflex right aortic arch forming a vascular ring, none of which were diagnosed in-utero. This case is unique for both the rarity of the aortic arch branching pattern and for being the first reported case of a circumflex right aortic arch diagnosed in-utero.
Case presentation
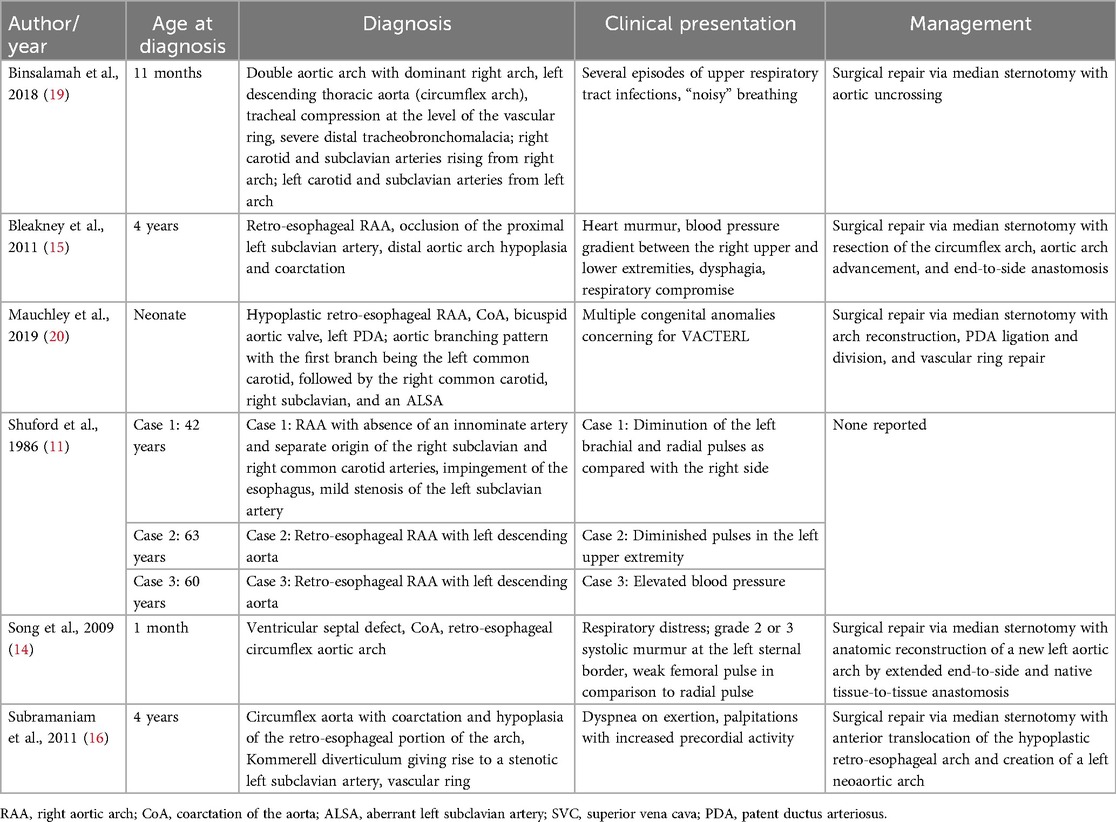
A 33-year-old G4P3 patient was referred for a fetal echocardiogram at 20 weeks gestation for a concerning obstetric ultrasound indicative of a double aortic arch. Fetal echocardiogram performed by a fetal cardiologist was suspicious for a vascular ring with a presumptive diagnosis of double aortic arch vs. circumflex right aortic arch (Figure 1). The child was born at 38 weeks gestation via induced vaginal delivery and had an uneventful postnatal course with no symptoms of airway or esophageal compression.
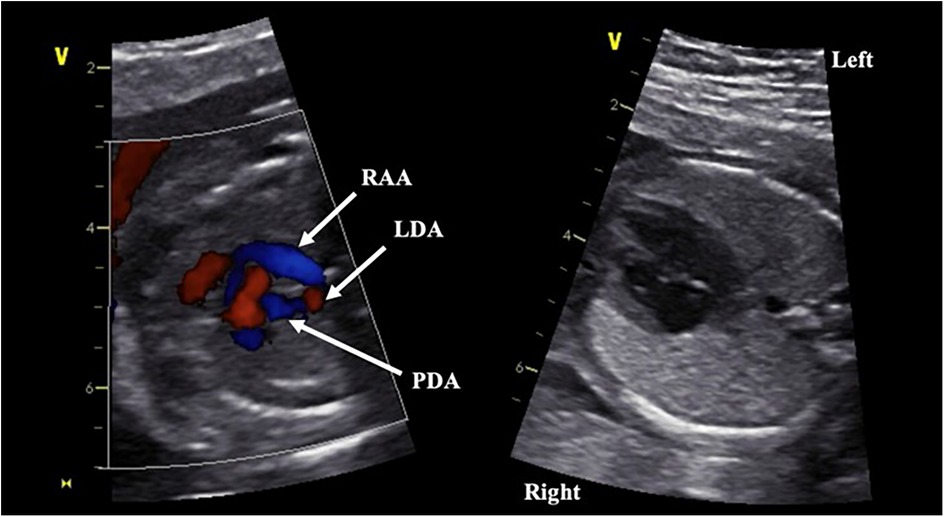
Figure 1. Fetal echocardiographic images at 20 weeks gestation. Panel on the left demonstrates vascular ring formed by the right circumflex aortic arch with left patent ductus arteriosus. Panel on the right demonstrates left sided descending aorta. RAA, right aortic arch; LDA, left descending aorta; PDA, patent ductus arteriosus.
Imaging findings
Fetal echocardiogram identified a right aortic arch with left-sided descending aorta, raising suspicions for a circumflex aortic arch (Figure 1). An aortic arch branching pattern was not well delineated. The differential diagnosis included right circumflex aortic arch with left ductus arteriosus vs. double aortic arch. Post-natal echocardiogram confirmed the presence of a vascular ring, but the arch behind the airway and aortic branching pattern was still not well-defined due to acoustic interface from the tracheobronchial tree and thus could not definitively diagnose the arch anomaly. CCTA was therefore performed, revealing a right aortic arch with a left descending aorta and a portion of the aortic arch extending behind the esophagus. A ductal ampulla was seen on the proximal portion of a left-sided descending aorta, which was suggestive of a right circumflex aortic arch with left ductus arteriosus (now reduced to ligamentum arteriosum). In addition, the first branch of the aortic arch was the left subclavian artery followed by a common trunk bifurcating into the left and right common carotid arteries and lastly the right subclavian artery (Figure 2). There was significant narrowing of the trachea and collapse of the esophagus at the level of the aortic arch, suggesting compression from the vascular ring (Figure 3). However, the patient was largely asymptomatic at birth without respiratory distress.
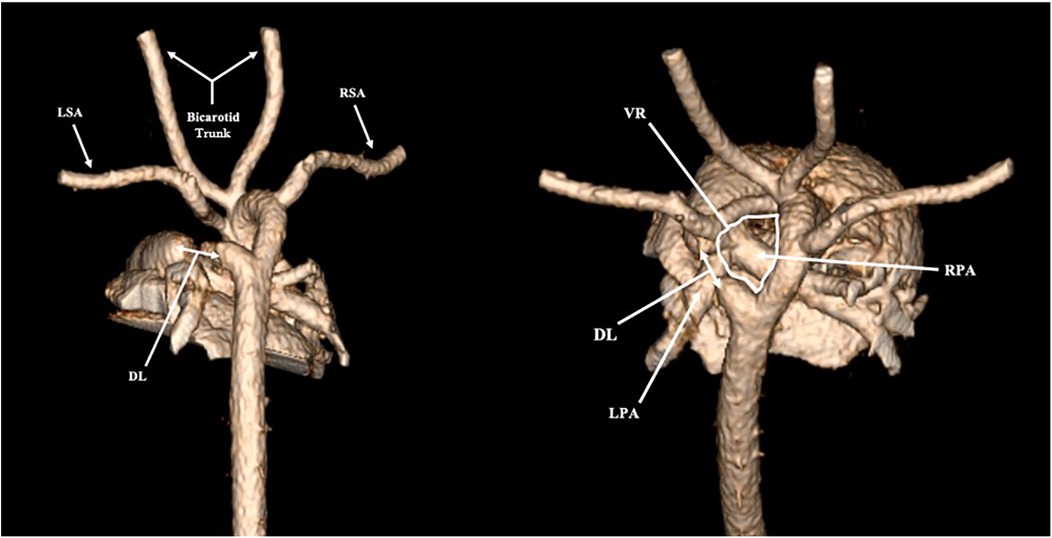
Figure 2. Three-dimensional reconstruction of cardiac computed tomography (CCTA). LSA, left subclavian artery; RSA, right subclavian artery; DL, ductal ligament; VR, vascular ring; LPA, left pulmonary artery; RPA, right pulmonary artery.
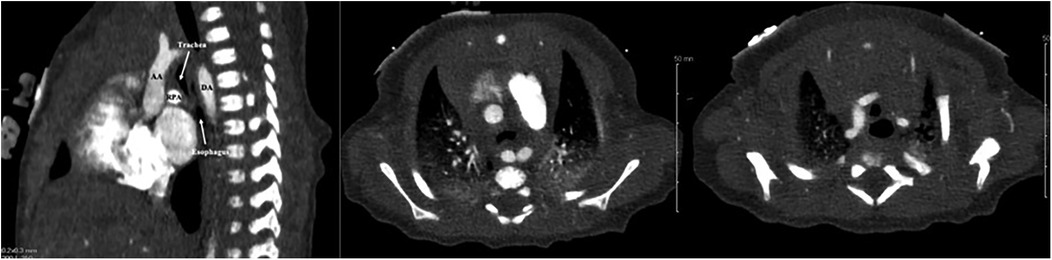
Figure 3. Cardiac computed tomography (CT) images demonstrating sagittal and axial views of the esophageal and tracheal compression caused by the vascular ring (middle panel taken at the level of the aortic arch for comparison to the right panel taken above the level of the aortic arch). AA, ascending aorta; DA, descending aorta; RPA, right pulmonary artery.
Discussion
Several imaging modalities are available for the evaluation of vascular ring anomalies, including radiography, echocardiography, computed tomography (CT), and magnetic resonance imaging (MRI). CT has become the preferred diagnostic modality for both pre- and post-operative evaluations, as it provides excellent spatial and temporal resolution, a wide field of view, multiplanar reconstruction capabilities, and simultaneous evaluation of the airway. Echocardiography is limited in aortic arch imaging due to its two-dimensional nature, acoustic interface from the airway, and interference from bony structures such as the vertebrae (4). Additionally, circumflex retro-esophageal aortic arch can be indistinguishable from a double aortic arch with an atretic segment on both fetal sonography and post-natal echocardiography (3). However, fetal echocardiogram provides a unique opportunity to assess the aortic arch as the trachea is filled with fluid during fetal life, leading to decreased acoustic interface in comparison to a post-natal transthoracic echocardiogram.
In our case, fetal echocardiogram did demonstrate a vascular ring but could not offer a definitive diagnosis of circumflex right aortic arch. Advanced imaging was critical to identify the definitive anatomy of this rare pathology. Though tracheal and esophageal compression were present, our patient did not have any respiratory distress or feeding difficulties.
Congenital aortic arch variants and malformations result from disordered embryogenesis of the branchial arches (2). They are important to recognize as they can be associated with vascular rings, congenital heart disease, and chromosomal abnormalities (5). Vascular rings can result in compression of the tracheobronchial tree and/or esophagus due to vessels, or their atretic portions, completely encircling the trachea and esophagus (6). The vessels forming the vascular ring can include the aortic arch or arches, aortic branch vessels, pulmonary branch arteries, ductus arteriosus, or ligamentum arteriosum (5). One rare form of a vascular ring is a circumflex aorta, which occurs when the distal aortic arch courses behind the esophagus, usually at the level of T4 or T5 vertebral body, to form a descending aorta that is contralateral to the aortic arch (5–7). The aortic arch can arise on the right or left side. The vascular ring is formed from the ductus arteriosus arising from the descending aorta on the contralateral side of the arch (7, 8). In rare cases, there is a ductus arteriosus or a diverticulum of Kommerell with an aberrant subclavian artery (7, 9).
A rare type of vascular ring is formed by a circumflex retro-esophageal right aortic arch (7, 10). A circumflex right aortic arch consists of a right-sided aortic arch with a left descending aorta and left ductus arteriosus or ligamentum arteriosum (5, 11). After the distal aortic arch passes behind the esophagus, it gives rise to a left diverticulum where the left ductus arteriosus or ligamentum arteriosum arises and connects to the left pulmonary artery, forming the complete vascular ring (5). Clinical manifestations as a result of the vascular ring compressing the trachea and/or esophagus include wheezing, stridor, dysphagia, feeding difficulty, cyanosis, vomiting, and arterial insufficiency (12). Circumflex right aortic arches have been rarely reported in the pediatric population in both asymptomatic and symptomatic patients with tracheal and esophageal compression (7, 13–20). Circumflex right aortic arches have been associated with a markedly hypoplastic retro-esophageal aortic segment (7), hypoplasia and coarctation of the aorta (15, 16, 20), double aortic arch (19), ventricular septal defect with bicuspid aortic valve (15), and ventricular septal defect with coarctation of the aorta (13).
There are two typical aortic branching patterns associated with a circumflex right aortic arch, depending on the presence of an aberrant left subclavian artery (5). One pattern consists of the first aortic arch vessel as the left innominate artery followed by the right carotid artery and then the right subclavian artery (5). The other typical branching pattern consists of the following order of aortic branches from proximal to distal: left carotid artery, right carotid artery, right subclavian artery and aberrant left subclavian artery, which arises from aortic diverticulum after the aorta has crossed midline behind the esophagus (5, 7, 21). In our patient, the first branch of the aorta was the left subclavian artery, followed by a common trunk bifurcating into the left and right common carotid arteries, and lastly the right subclavian artery.
Circumflex right aortic arch with vascular ring in a symptomatic patient is managed with surgical intervention, which typically includes median sternotomy, ligation and division of the ductal ligament, and resection of the retro-esophageal portion of the aortic arch with reconstruction or anterior translocation of the aortic arch. From our extensive literature review, we were able to identify only six reports of cases of a circumflex right aortic arch forming a vascular ring, none of which were diagnosed in-utero (Table 1).
Binsalamah and colleagues identified a double aortic arch with dominant right arch and a left descending thoracic aorta (circumflex arch) creating a vascular ring with tracheal compression (19). The patient subsequently underwent surgical repair via a median sternotomy with aortic uncrossing.
Bleakney and associates reported on a patient with a retro-esophageal right aortic arch with distal aortic arch hypoplasia and coarctation, for which the patient underwent surgical repair via a median sternotomy with resection of the circumflex arch, aortic arch advancement, and end-to-side anastomosis (15). Song and colleagues similarly performed a median sternotomy with reconstruction of a new left aortic arch via end-to-side and native tissue-to-tissue anastomosis on a patient with a retro-esophageal circumflex aortic arch (14). Additionally, Subramaniam and associates described a patient with a circumflex aorta with retro-esophageal coarctation who underwent surgical repair via median sternotomy with anterior translocation of the hypoplastic arch and creation of a left neoaortic arch (16).
Shuford and colleagues reported on three adult patients who were diagnosed with retro-esophageal right aortic arch (11). The patients were being evaluated for varying causes (chest pain, urinary retention, and elevated blood pressures) at the time of their diagnosis. None of the patients underwent surgical intervention at the time.
Following surgical intervention, patients were reported to recover without complications and post-operative imaging revealed successful repair. Of note, Mauchley and colleagues reported the development of an increasing gradient through the parachute mitral valve, but confirmed the patient continued to do well clinically (20).
Conclusion
To our knowledge, this is the first case reported in the literature of a circumflex right aortic arch suspected on fetal echocardiogram and postnatal echocardiogram and subsequently confirmed with CCTA. This case is particularly unique for its atypical aortic branching pattern and due to circumflex right aortic arches being a rare cause of a complete vascular ring. Vascular ring due to circumflex retro-esophageal aortic arch can be difficult to distinguish from a double aortic arch with an atretic segment on both fetal sonography and post-natal echocardiography. Fetal echocardiogram provides a unique opportunity to assess the aortic arch as the trachea is filled with fluid allowing for decreased acoustic interface in comparison to a post-natal transthoracic echocardiogram. Additionally, CCTA has become the preferred diagnostic modality for both pre- and post-operative evaluations as it provides excellent spatial and temporal resolution, a wide field of view, multiplanar reconstruction capabilities, and simultaneous evaluation of the airway. Clinical presentation may vary, but this anomaly is important to recognize due to its potential to cause severe symptoms.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the individual(s), and minor(s)' legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
Author contributions
TL: Writing – review & editing. YA: Writing – original draft. CS: Writing – original draft. AA: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Agarwal AK. Vascular Rings and Slings. Springer eBooks (2021). p. 181–96. doi: 10.1007/978-3-030-74822-7_26
2. Priya S, Thomas R, Nagpal P, Sharma A, Steigner M. Congenital anomalies of the aortic arch. Cardiovasc Diagn Ther. (2018) 8(Suppl 1):S26–44. doi: 10.21037/cdt.2017.10.15
3. Yoo SJ, Min JY, Lee YH, Roman K, Jaeggi E, Smallhorn J. Fetal sonographic diagnosis of aortic arch anomalies. Ultrasound Obstet Gynecol. (2003) 22:535–46. doi: 10.1002/uog.897
4. Bader V, Knight WB, Danton MH, Peng E. Congenital arch malformation: a review of morphology and surgical management of circumflex aortic arch. Vessel Plus. (2020) 4:34. doi: 10.20517/2574-1209.2020.36
5. Hanneman K, Newman B, Chan F. Congenital variants and anomalies of the aortic arch. Radiographics. (2017) 37(1):32–51. doi: 10.1148/rg.2017160033
6. Gould SW, Rigsby CK, Donnelly LF, McCulloch M, Pizarro C, Epelman M. Useful signs for the assessment of vascular rings on cross-sectional imaging. Pediatr Radiol. (2015) 45(13):2004–16; quiz 2–3. doi: 10.1007/s00247-015-3424-7
7. Hilmes M, Hernandez R, Devaney E. Markedly hypoplastic circumflex retroesophageal right aortic arch: mR imaging and surgical implications. Pediatr Radiol. (2007) 37(1):63–7. doi: 10.1007/s00247-006-0343-7
8. Kellenberger CJ. Aortic arch malformations. Pediatr Radiol. (2010) 40(6):876–84. doi: 10.1007/s00247-010-1607-9
9. Weinberg PM. Aortic arch anomalies. J Cardiovasc Magn Reson. (2006) 8(4):633–43. doi: 10.1080/10976640600713756
10. Ramos-Duran L, Nance JW Jr., Schoepf UJ, Henzler T, Apfaltrer P, Hlavacek AM. Developmental aortic arch anomalies in infants and children assessed with CT angiography. AJR Am J Roentgenol. (2012) 198(5):W466–74. doi: 10.2214/AJR.11.6982
11. Shuford WH, Sybers RG, Gordon IJ, Baron MG, Carson GC. Circumflex retroesophageal right aortic arch simulating mediastinal tumor or dissecting aneurysm. AJR Am J Roentgenol. (1986) 146(3):491–6. doi: 10.2214/ajr.146.3.491
12. Philip S, Chen SY, Wu MH, Wang JK, Lue HC. Retroesophageal aortic arch: diagnostic and therapeutic implications of a rare vascular ring. Int J Cardiol. (2001) 79(2–3):133–41. doi: 10.1016/S0167-5273(01)00402-8
13. Planche C, Lacour-Gayet F. Aortic uncrossing for compressive circumflex aorta. 3 cases. Presse Med. (1984) 13(21):1331–2.6233555
14. Song J, Kim WH, Kim H, Koh J, Kwak JG, Kim KB, et al. Repair of coarctation in right circumflex retroesophageal arch. Ann Thorac Surg. (2009) 87(1):307–9. doi: 10.1016/j.athoracsur.2008.05.050
15. Bleakney CA, Zafar F, Fraser CD Jr. Circumflex right aortic arch with associated hypoplasia and coarctation: repair by aortic arch advancement and end-to-side anastomosis. Ann Thorac Surg. (2011) 91(2):624–6. doi: 10.1016/j.athoracsur.2010.05.056
16. Subramaniam KG, Marimuthu K, Manohar K, Verma S, Cherian KM. Anterior arch translocation for coarctation of circumflex aorta using median sternotomy without cardiopulmonary bypass. J Thorac Cardiovasc Surg. (2011) 141(6):1543–5. doi: 10.1016/j.jtcvs.2010.10.020
17. Backer CL, Monge MC, Russell HM, Popescu AR, Rastatter JC, Costello JM. Reoperation after vascular ring repair. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. (2014) 17(1):48–55. doi: 10.1053/j.pcsu.2014.01.001
18. Tissot C, Didier D, Beghetti M, Kalangos A, Myers PO. Asymptomatic right circumflex aortic arch associated with ventricular septal defect and biscuspid aortic valve. Heart Surg Forum. (2015) 18(3):E114–5. doi: 10.1532/hsf.1313
19. Binsalamah ZM, Chacon-Portillo MA, Sanyahumbi A, Adachi I, Heinle JS, Fraser CD Jr., et al. Circumflex aorta with double aortic arch in an infant. J Card Surg. (2018) 33(5):292–5. doi: 10.1111/jocs.13604
20. Mauchley DC, Stiegler JM, Padilla LA, Aburjania Z, Dabal R, Cleveland D. Repair of rare vascular ring: circumflex aortic arch with associated hypoplasia and coarctation. World J Pediatr Congenit Heart Surg. (2020) 11(2):235–7. doi: 10.1177/2150135119828387
Keywords: case report, circumflex aortic arch, vascular ring, fetal echo and fetal echocardiography, cardiac CT
Citation: Langenfeld T, Ali Y, Sharma C and Agarwal A (2025) Case report and literature review: fetal diagnosis of vascular ring with circumflex right aortic arch and unique aortic arch branching pattern. Front. Cardiovasc. Med. 12:1523356. doi: 10.3389/fcvm.2025.1523356
Received: 5 November 2024; Accepted: 18 February 2025;
Published: 10 March 2025.
Edited by:
Mauro Lo Rito, IRCCS San Donato Polyclinic, ItalyReviewed by:
Mila Stajevic, University of Belgrade, SerbiaRandy Stevens, St. Christopher's Hospital for Children, United States
Copyright: © 2025 Langenfeld, Ali, Sharma and Agarwal. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Arpit Agarwal, YXJwaXQuYWdhcndhbEB1aGhvc3BpdGFscy5vcmc=
 Tyler Langenfeld
Tyler Langenfeld Yumna Ali
Yumna Ali Chetan Sharma
Chetan Sharma Arpit Agarwal
Arpit Agarwal