
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med. , 19 February 2025
Sec. Lipids in Cardiovascular Disease
Volume 12 - 2025 | https://doi.org/10.3389/fcvm.2025.1493271
Background: Limited evidence exists regarding the association between oxidative stress induced by dietary and lifestyle factors and cardiovascular diseases (CVDs).
Methods: We conducted a weighted analysis using data from 13,530 adults in the National Health and Nutrition Examination Survey (NHANES), covering the period from 2003 to 2018. The total oxidative balance score (OBS) was derived from 20 oxidative stress-related exposures, including dietary and lifestyle factors. Survey-weighted multivariable logistic regression and stratified analyses were performed to examine the association between OBS and CVDs. To further investigate the nonlinear relationship, we employed restricted cubic spline analysis and threshold effect analysis. Additionally, we assessed whether hepatic function and blood lipid levels mediate the OBS-CVDs relationship.
Results: This study included 13,530 participants, representing a weighted population of 81,006,649.2 individuals. After adjusting for potential confounders, a linear relationship was observed between total OBS, dietary OBS, and CVDs, while lifestyle OBS exhibited a nonlinear association, with a significant threshold effect at a score of 4. When the lifestyle OBS exceeded this threshold, a marked negative correlation with CVDs was observed. Furthermore, albumin (Alb) mediated 23.59% of the relationship between the total OBS and CVDs.
Conclusions: Lower levels of total OBS were inversely associated with CVDs. This association was partially mediated by blood lipid levels and hepatic function. Interventions focusing on antioxidant-rich dietary and lifestyle modifications may play a pivotal role in reducing the possibility of CVDs.
Oxidative stress results from the accumulation of reactive oxygen species (ROS), which can damage cellular structures and disrupt their functions. When the body's antioxidant defenses are overwhelmed by an excess of free radicals, oxidative stress develops, potentially leading to damage to proteins, lipids, and DNA, and contributing to the pathogenesis of various diseases (1). Prolonged exposure to ultraviolet radiation, chronic stress, intense physical activity, unhealthy dietary habits, and exposure to irritants can lead to excessive production of ROS (2). Unhealthy lifestyle behaviors are significant contributors to the global prevalence of cardiovascular diseases (CVDs). Smoking, alcohol consumption, excess body weight, high fat intake, and iron are potential pro-oxidants, while dietary antioxidants such as fiber, carotene, riboflavin, certain vitamins, and physical exercise, serve as common antioxidant factors. The Oxidative Balance Score (OBS) offers a new approach by integrating multiple dietary and lifestyle exposures, assessing an individual's overall antioxidant status by considering both antioxidant and pro-oxidant factors. A higher OBS reflects a greater exposure to antioxidants.
Previous studies have shown that a higher OBS is associated with reduced all-cause and cardiovascular mortality in individuals with diabetes and prediabetes (3). The mechanisms through which the OBS influences CVDs require further investigation. Evidence suggests that oxidative stress is closely associated with hepatotoxicity, disrupting the intracellular oxidative balance in liver cells and impairing both their structure and function (4). This disruption often leads to liver dysfunction, which is a well-established precursor to dyslipidemia (5, 6). Building on this understanding, we hypothesize that low OBS levels may exacerbate oxidative stress, potentially affecting serum markers such as albumin (Alb), total cholesterol (TC), and alkaline phosphatase (ALP), thereby increasing the possibility of developing CVDs.
To address these concerns, we analyzed cross-sectional data from eight cycles of the National Health and Nutrition Examination Survey (NHANES), including 13,530 participants, to examine the relationship between OBS and both general and specific CVDs. Additionally, this study aims to conduct a mediation analysis to explore whether the effects of OBS on CVDs are mediated through hepatic function and lipid levels, with the ultimate goal of providing novel intervention strategies for clinical application.
The NHANES is an ongoing cross-sectional survey designed to assess the health and nutritional status of non-institutionalized civilians across the United States. Employing a complex multistage probability sampling design, NHANES ensures national representativeness. Participants undergo household interviews, physical examinations, and laboratory tests every two years. The survey is administered by the National Center for Health Statistics (NCHS), which operates under the Centers for Disease Control and Prevention (CDC). All participants provide written informed consent prior to participation.
This study utilized publicly available NHANES data from 2003 to 2018 and initially included 80,313 adults. A total of 67,708 individuals were excluded from the analysis for various reasons: 62,731 had incomplete OBS data, 397 were under the age of 20, 275 were pregnant women, 3,295 had missing covariate data, and another group had unreliable energy intake values (less than 800 kcal/day or more than 4,200 kcal/day for males, and less than 500 kcal/day or more than 3,500 kcal/day for females). After excluding 85 individuals with missing data on CVDs, the final analysis included 13,530 participants with complete interview and examination data (Figure 1). Sociodemographic information was collected, including age, gender, race, education levels, poverty-income ratio (PIR), and body mass index (BMI). Additionally, covariates such as total energy intake, blood lipid levels, liver and kidney function indicators, and self-reported chronic conditions, including diabetes and hypertension, were gathered (3).
The OBS is a comprehensive metric that represents the overall oxidative balance, derived from 16 dietary nutrients and 4 lifestyle components, encompassing both pro-oxidant and antioxidant factors. Pro-oxidant factors include total fat and iron intake, smoking and alcohol habits, and BMI, while antioxidant factors include dietary fiber, calcium, zinc, copper, selenium, magnesium, vitamins C, E, B12, B6, carotenoids, riboflavin, niacin, total folate intake, and physical activity. Each component was categorized into three groups based on gender-specific tertiles. Antioxidant components in Groups 1 to 3 were assigned scores from 0 to 2, with higher scores indicating greater antioxidant levels. Conversely, pro-oxidant components were scored inversely, with lower scores indicating higher pro-oxidant levels. Specific scoring for each component is as follows:
- Physical activity levels were categorized based on the 2018 Physical Activity Guidelines for Americans (HHS, 2018): low activity (<150 min per week) was assigned a score of 0, moderate activity (150–300 min per week) was assigned a score of 1, and high activity (>300 min per week) was assigned a score of 2.
- Alcohol consumption was classified as follows: non-drinkers were assigned a score of 2, moderate drinkers (0–15 g per day for females or 0–30 g per day for males) were assigned a score of 1, and heavy drinkers (≥15 g per day for females or ≥30 g per day for males) were assigned a score of 0.
- Smoking status was assessed based on lifetime cigarette consumption: individuals who smoked fewer than 100 cigarettes scored 2, those with at least 100 cigarettes but who were no longer smoking scored 1, and current smokers scored 0.
- BMI was calculated as weight (kg) divided by height squared (m2): individuals with normal weight (<25 kg/m2) received a score of 2, those who were overweight (25–29.9 kg/m2) received a score of 1, and individuals with obesity (≥30 kg/m2) received a score of 0.
The dietary OBS was obtained by totaling the scores of the 16 dietary components, while the lifestyle OBS was determined by summing the scores of the 4 lifestyle components. The total OBS was obtained by adding together the scores of each individual component. In our investigation, total OBS ranged from 5 to 38, with higher scores denoting greater levels of antioxidant exposure. Participants were stratified into quartiles according to their total OBS, with Quartiles 1 and 2 categorized as pro-oxidant groups, and Quartiles 3 and 4 classified as antioxidant groups.
The diagnosis of CVDs was established through a comprehensive medical history questionnaire conducted via individual interviews. This questionnaire comprised five distinct inquiries, such as: “Has a doctor or other healthcare professional ever informed you that you have congestive heart failure (HF)/coronary heart disease (CHD)/angina/heart attack/stroke?” An affirmative response to any of these queries indicated a positive CVDs status for the individual. Participants who provided affirmative answers to specific CVD-related questions were categorized accordingly.
To assess the relationship between OBS and CVDs, survey-weighted multivariable logistic regression analysis was performed. Given the complex sampling design of NHANES, sample data were weighted using the “survey” package in R. To account for the eight cycles of NHANES, the original two-year sample weights were divided by eight and assigned to each participant. Subsequent regression analyses utilized these weighted models. Three covariate-adjusted models were employed to assess potential confounding effects. Stratified analyses were performed to evaluate the robustness of the relationship between OBS and CVDs. Dose-response associations were explored using restricted cubic splines with a smoothing function. Additionally, mediation analyses were conducted using the “mediation” package in R to estimate the potential mediating effects of TC, Alb, ALP on the OBS-CVDs association. Statistical analyses were performed using R software (version 4.3.2), with statistical significance set at P < 0.05.
This study involved 13,530 participants, weighted to represent a population of 81,006,649.2 individuals. The mean age was 45.77 ± 16.19 years, comprising 41,673,433.2 males (51.4%) and 39,333,216.0 females (48.6%). Among the participants, 5,031,828.7 individuals (6.2%) were diagnosed with CVDs (Table 1). Individuals with CVDs tended to be male, older, non-Hispanic white, and exhibited higher BMI, hypertension, lower levels of TC, HDL, Alb, and calorie intake, while showing elevated levels of ALP and creatinine. Notably, CVDs patients had lower total, lifestyle, and dietary OBS.
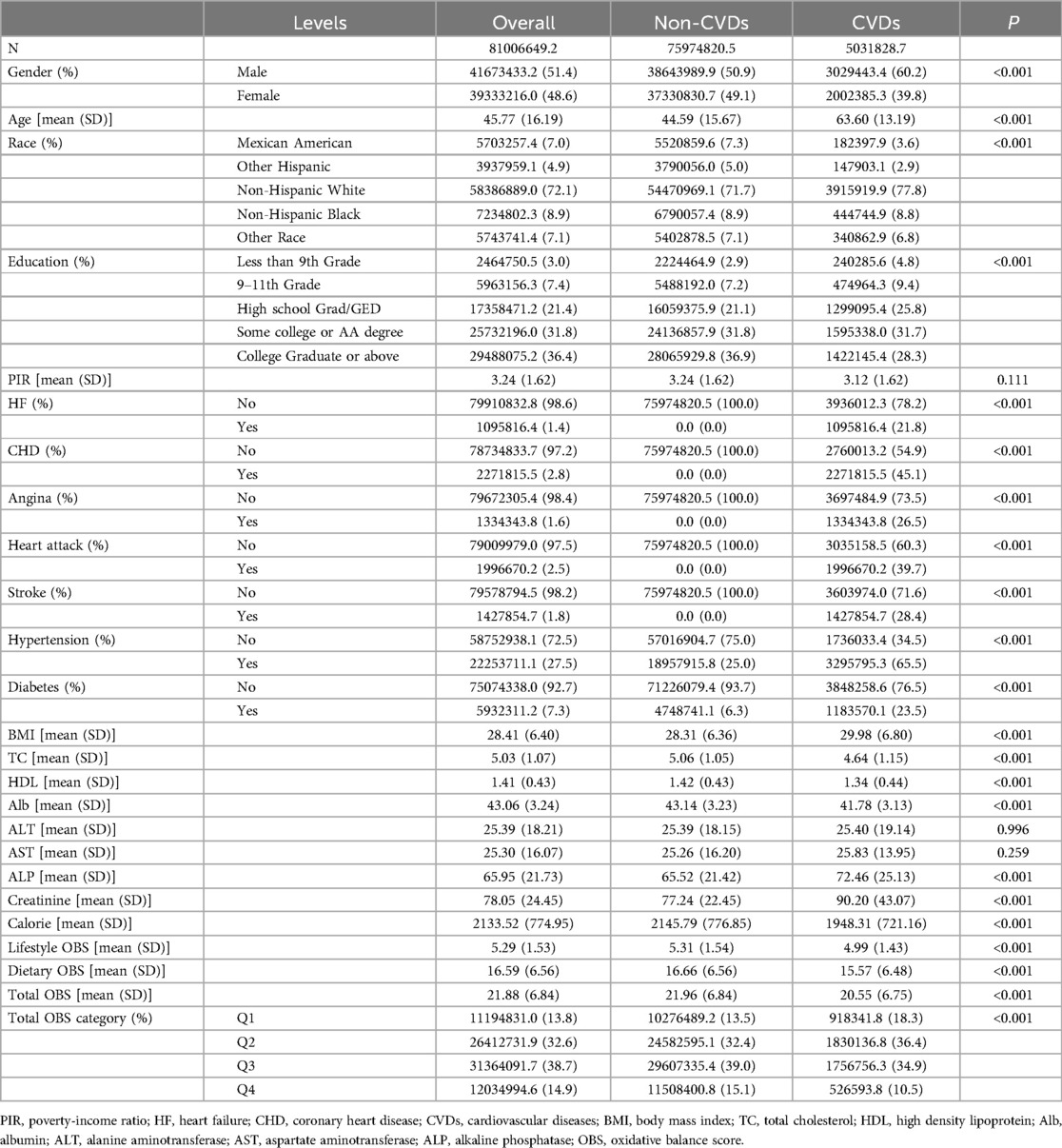
Table 1. Survey-weighted baseline characteristics of the U.S. Adult Population, NHANES 2003–2018 Cohort.
Table 2 presents the association between total OBS and CVDs as determined by logistic regression analysis. After adjusting for potential confounders, a significant association was observed. In Model 3, participants in the highest total OBS Quartile had a reduced likelihood of CVDs occurrence (Q4 vs. Q1: OR=−0.51; 95%CI = −0.89 to −0.12, P < 0.01). Similarly, individuals in the third total OBS Quartile also showed a lower likelihood of developing CVDs, with an OR of −0.34 (95%CI = −0.60 to −0.09; P < 0.01). Further investigation revealed a significant negative correlation between total OBS subgroups and HF, whereas no statistically significant associations were detected with CHD, angina pectoris, heart attack, or stroke. Subgroup analysis (Figure 2) comparing individuals with and without CVDs indicated that age and gender modulated the OBS-CVDs relationship. That is to say, this relationship was more prominent in elderly and male patient groups (P < 0.05).
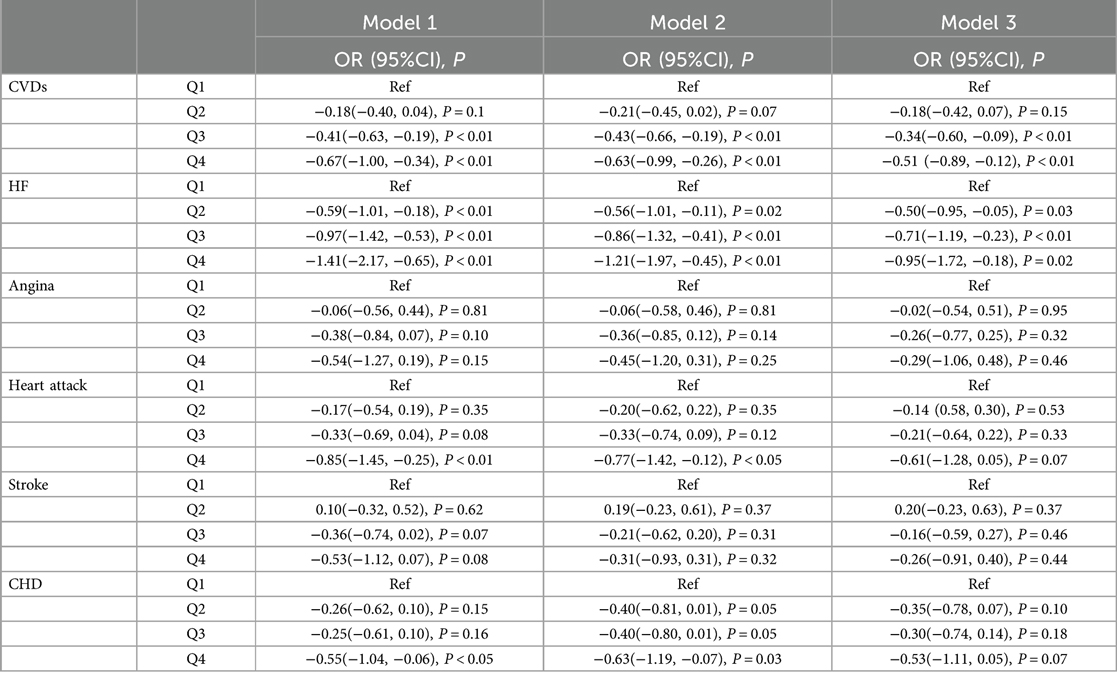
Table 2. Weighted multivariate logistic regression analysis of the association between OBS and overall CVDs and specific CVD subtypes.
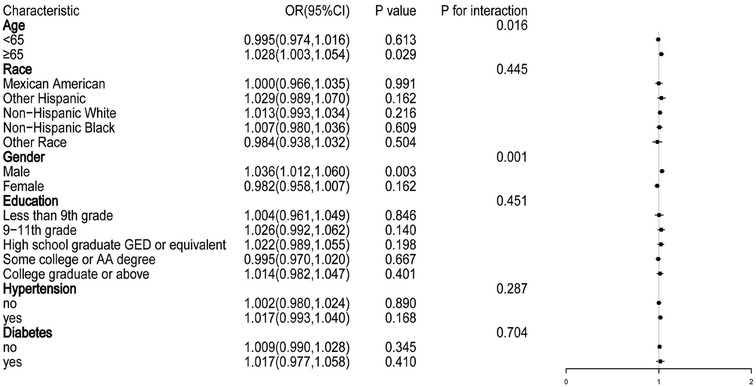
Figure 2. Subgroup analysis of the relationship between total OBS and CVDs. Adjusted for age, gender, education levels, race, hypertension, diabetes, TC, Alb, ALP, creatinine, and caloric intake.
The restricted cubic spline curves revealed a linear trend in the relationship between total OBS (P for non-linearity = 0.647) and dietary OBS (P for non-linearity = 0.551) with CVDs, as illustrated in Figure 3. Specifically, the association between lifestyle OBS and CVDs exhibited a non-linear trend (P for non-linearity < 0.01; Table 3). Threshold effect analysis indicated that when lifestyle OBS was below 4, no statistically significant association was observed. However, when lifestyle OBS exceeded 4, a significant negative correlation emerged, with an OR of 0.813 (P < 0.01). A likelihood ratio test comparing segmented models with linear models yielded a P = 0.014, suggesting that a segmented model with a significant turning point at lifestyle OBS = 4 was more appropriate.
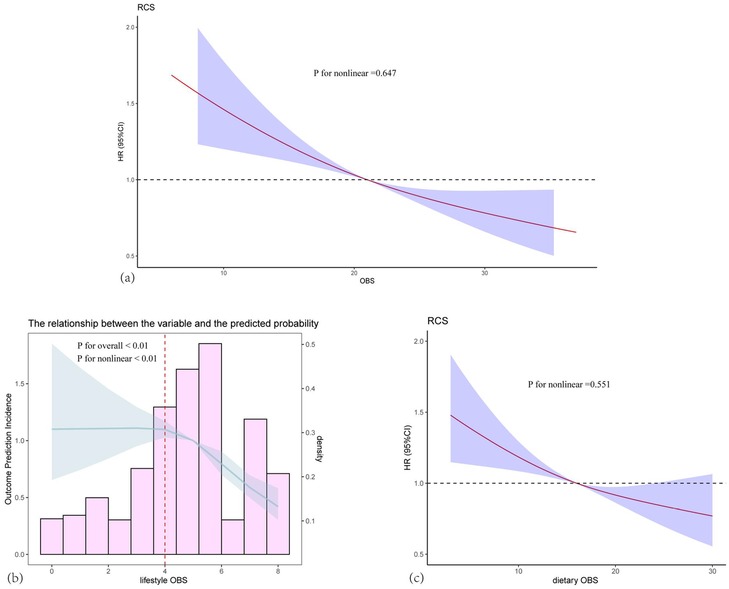
Figure 3. Dose-Response associations between total OBS, dietary OBS, and lifestyle OBS and CVDs. (a) Total OBS; (b) Lifestyle OBS; (c) Dietary OBS. The Solid lines and shaded areas represent the central risk estimates and 95% CIs. Logistic regression based on restricted cubic splines shows a linear association between dietary OBS and CVDs (P for nonlinearity = 0.647), and a nonlinear association between lifestyle OBS and CVDs (P for nonlinearity < 0.01). Models were adjusted for age, gender, race, and education levels.
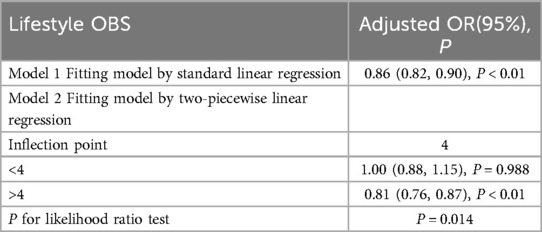
Table 3. Threshold effect of lifestyle OBS on CVDs analyzed using a Two-stage logistic regression model.
We further examined whether liver function-related markers mediate the negative correlation between OBS and CVDs. Based on the significant results from multivariable logistic regression analysis, we selected Alb, TC, and ALP as the variables for mediation analysis. As depicted in Table 4, Alb mediated 23.59% of the association between OBS and CVDs, TC mediated −8.29%, and ALP mediated 7.68% (all P < 0.05).
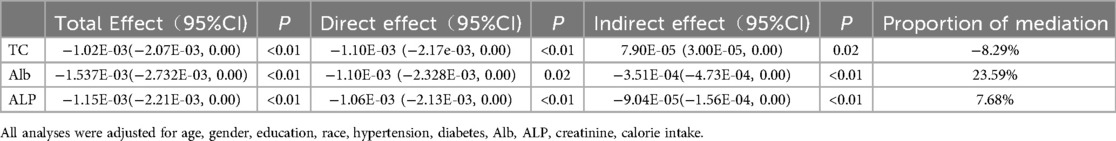
Table 4. Estimated proportion of the association between tital OBS and CVDs mediated by Serum parameters.
In this nationwide prospective cohort study utilizing NHANES data spanning up to 16 years, we observed a negative correlation between total OBS and CVDs. Participants with a pro-oxidative OBS exhibited a significantly higher possibility of overall CVDs, with a particularly pronounced association observed in HF. Subgroup analysis revealed a more pronounced correlation in elderly and male patients (P < 0.05). A linear relationship was identified between total and dietary OBS with CVDs, while lifestyle OBS exhibited a non-linear relationship. Notably, Alb played a significant mediating role in this association.
While the precise mechanism by which OBS affects CVDs remains unclear, oxidative stress appears to play a central role in this association. ROS are oxygen-containing molecules characterized by their chemical reactivity, functioning both as signaling molecules and as harmful agents when present in excess. Excessive accumulation of ROS within cells can trigger cellular stress responses, including the activation of antioxidant defense mechanisms or programmed cell death pathways (7). OBS may exacerbate CVDs progression by promoting ROS production. Atherosclerosis, with its multifactorial etiology, highlights the central role of inflammation (8). From endothelial dysfunction to clinical manifestations, both systemic and local inflammation play pivotal roles in the onset and progression of CVDs. Monocytes recruited to sites of inflammation differentiate into macrophages, which exhibit either pro-inflammatory or anti-inflammatory phenotypes based on microenvironment cues (9).
The linear relationship between total and dietary OBS with CVDs suggests that dietary antioxidant status may have a predictable impact on cardiovascular health. This finding could inform dietary guidelines or interventions aimed at reducing CVDs possibility by emphasizing antioxidant-rich diets. In contrast, the non-linear relationship observed with lifestyle OBS indicates that lifestyle factors may influence CVDs in a more complex manner, suggesting the need for personalized lifestyle modifications rather than a one-size-fits-all approach. When lifestyle OBS is below the threshold of 4, changes in lifestyle OBS may not significantly impact CVDs. However, once lifestyle OBS exceeds this threshold, a notable reduction in CVDs possibility is observed, suggesting that specific lifestyle factors may have a more pronounced effect on CVDs prevention once they reach a certain level. Clinicians should consider assessing patients' total, dietary, and lifestyle OBS and tailor their recommendations accordingly.
Our study further explored the pathways linking OBS to CVDs through mediation analysis, identifying Alb, TC, and ALP as partial mediators. Alb alone accounted for 23.59% of the observed association, suggesting that reduced OBS may worsen CVDs symptoms by promoting oxidative stress and affecting lipid levels and liver function. A study by Andreas Ronit et al. also found a strong, independent link between low Alb and an increased risk of CVDs, with hazard ratios ranging from 1.17 to 1.46 across different CVDs subtypes. Meta-analysis revealed a risk ratio of 1.85 for each 10 g/L decrease in Alb, partly due to Alb's role as a negative acute-phase reactant (10). The Mediterranean diet, rich in antioxidants and anti-inflammatory compounds, helps alleviate intracellular oxidative stress and consistently benefits overall health, well-being, and mental state. It is believed to modulate genes related to oxidative stress, contributing to its health advantages (11). Panagiotakos et al. reported a significant negative correlation between adherence to the Mediterranean diet and blood lipid levels (12). Additionally, oxidative stress is associated with hepatotoxicity. Diets high in methionine can induce hyperhomocysteinemia, leading to multi-organ damage and inflammation. Research by Derouiche F found that methionine supplementation correlates with oxidative stress and disrupts proteasome function, resulting in hepatotoxicity and inflammation, as evidenced by elevated liver enzymes, bilirubin, and decreased Alb levels (4).
Notably, total OBS demonstrates a strong negative correlation with HF, but not with other subtypes like CHD, angina, heart attack, or stroke. This disparity likely reflects the distinct pathophysiological mechanisms underlying each CVD subtype, suggesting that the effects of antioxidants are not uniform across diseases. Additionally, antioxidants, particularly at high concentrations or when interacting with other substances, may act as pro-oxidants (13). Several factors may contribute to this variation, including differing baseline oxidative stress levels in each disease, the context-dependent effects of antioxidants, and the potential disruption of oxidative balance when antioxidant levels become excessive (14). In the case of HF, the pathogenesis involves complex processes such as myocardial remodeling, impaired contractility, neurohormonal activation, inflammation, and oxidative stress, all regulated by various genes (15).
This study has several limitations. Firstly, patients' self-reported CVDs history is prone to recall and information biases, as well as misclassification, which could compromise the reliability of the results. Secondly, residual and unmeasured confounding factors may introduce bias into the analysis. Thirdly, the observational design of our study limits our ability to establish a causal relationship between OBS and CVDs. Fourthly, despite our large sample size, the participants are limited to voluntary U.S. residents, which raises concerns about the generalizability of our findings to other countries. Given these limitations, the results should be interpreted with caution, and further research is needed to confirm our findings.
Total OBS is negatively associated with both overall CVDs and HF, with total and dietary OBS demonstrating a linear negative correlation with CVDs, while lifestyle OBS exhibits a nonlinear relationship. Interventions promoting antioxidant-rich diets and healthy lifestyles could significantly reduce the likelihood of CVDs. Furthermore, our findings suggest that blood lipids and liver function may mediate the association between OBS and CVDs. Prospective and experimental studies are needed to confirm these associations and elucidate the underlying mechanisms. We recommend that clinical practice and public health initiatives focus on promoting antioxidant-rich diets, such as the Mediterranean diet, to mitigate oxidative stress and enhance cardiovascular health. Regular monitoring of liver function and lipid profiles should be incorporated into routine check-ups, especially for high-risk individuals.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
The studies involving humans were approved by the Research Ethics Review Board of the National Center for Health Statistics. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
YH: Conceptualization, Formal Analysis, Methodology, Software, Writing – original draft. YL: Conceptualization, Investigation, Methodology, Supervision, Validation, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declare that no Generative AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Chaudhary P, Janmeda P, Docea A, Yeskaliyeva B, Abdull Razis A, Modu B, et al. Oxidative stress, free radicals and antioxidants: potential crosstalk in the pathophysiology of human diseases. Front Chem. (2023) 11:1158198. doi: 10.3389/fchem.2023.1158198
2. Lushchak VI. Free radicals, reactive oxygen species, oxidative stresses and their classifications. Ukr Biochem J. (2015) 87:11–8. doi: 10.15407/ubj87.06.011
3. Xu Z, Liu D, Zhai Y, Tang Y, Jiang L, Li L, et al. Association between the oxidative balance score and all-cause and cardiovascular mortality in patients with diabetes and prediabetes. Redox Biol. (2024) 76:103327. doi: 10.1016/j.redox.2024.103327
4. Derouiche F, Djemil R, Sebihi FZ, Douaouya L, Maamar H, Benjemana K. High methionine dietary mediated oxidative stress and proteasome impairment causes toxicity in liver. Sci Rep. (2024) 14(1):5555. doi: 10.1038/s41598-024-55857-1
5. Lakkur S, Judd S, Bostick RM, McClellan W, Flanders WD, Stevens VL, et al. Oxidative stress, inflammation, and markers of cardiovascular health. Atherosclerosis. (2015) 243(1):38–43. doi: 10.1016/j.atherosclerosis.2015.08.032
6. Xiao J, Wei H, Gao Z, Chen L, Ye W, Huang W. Differential age-specific associations of LDL cholesterol and body mass index with coronary heart disease. Atherosclerosis. (2024) 393:117542. doi: 10.1016/j.atherosclerosis.2024.117542
7. Schieber M, Chandel NS. ROS Function in redox signaling and oxidative stress. Curr Biol. (2014) 24:R453–62. doi: 10.1016/j.cub.2014.03.034
8. Legein B, Temmerman L, Biessen EA, Lutgens E. Inflammation and immune system interactions in atherosclerosis. Cell Mol Life Sci. (2013) 70(20):3847–69. doi: 10.1007/s00018-013-1289-1
9. Henein MY, Vancheri S, Longo G, Vancheri F. The role of inflammation in cardiovascular disease. Int J Mol Sci. (2022) 23(21):12906. doi: 10.3390/ijms232112906
10. Ronit A, Kirkegaard-Klitbo DM, Dohlmann TL, Lundgren J, Sabin CA, Phillips AN, et al. Plasma albumin and incident cardiovascular disease: results from the CGPS and an updated meta-analysis. Arterioscler Thromb Vasc Biol. (2020) 40(2):473–82. doi: 10.1161/ATVBAHA.119.313681
11. Di Renzo L, Gualtieri P, Frank G, De Santis GL, Cianci R, Bigioni G, et al. Sex differences in the efficacy of Mediterranean dietary treatment: a nutrigenomics pilot study. Genes (Basel). (2023) 14(11):1980. doi: 10.3390/genes14111980
12. Panagiotakos DB, Pitsavos C, Stefanadis C. Stefanadis, dietary patterns: a Mediterranean dietary score and its relation to clinical and biological markers of cardiovascular disease risk. Nutr Metabol Cardiovasc Dis. (2006) 16:559–68. doi: 10.1016/j.numecd.2005.08.006
13. Carocho M, Ferreira IC. A review on antioxidants, prooxidants and related controversy: natural and synthetic compounds, screening and analysis methodologies and future perspectives. Food Chem Toxicol. (2013) 51:15–25. doi: 10.1016/j.fct.2012.09.021
14. Jia J, Sun Z, Tao X, Tong Y, Feng H, Yang J, et al. Association between oxidative balance score and heart failure in the older adults: results from the NHANES 2005–2018. Heart Lung. (2024) 68:107–15. doi: 10.1016/j.hrtlng.2024.06.006
Keywords: cardiovascular diseases, heart failure, hepatic function, lipid level, oxidative balance score
Citation: He Y and Lan Y (2025) Dietary and lifestyle oxidative balance scores and their impact on cardiovascular diseases: exploring the mediating influence of hepatic function and blood lipid levels. Front. Cardiovasc. Med. 12:1493271. doi: 10.3389/fcvm.2025.1493271
Received: 16 December 2024; Accepted: 5 February 2025;
Published: 19 February 2025.
Edited by:
Mohamad Navab, UCLA Health System, United StatesReviewed by:
Lin Xia, Northern Theater General Hospital, ChinaCopyright: © 2025 He and Lan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ying Lan, bGFueWluZzQ0NzQzMTc2NkAxNjMuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.