Abstract
Objective:
To quantify the risk of heart diseases (HD) and determine the relationship between physical activity (PA) dimensions and HD among Chinese middle-aged and older individuals.
Methods:
Using data from the China Health and Retirement Longitudinal Study (CHARLS, 2018), 16,927 participants were included in this study. Multivariate logistic regression was performed to determine the association between HD risk and PA dimensions, including volume, intensity, frequency, and duration. Restricted cubic spline analysis was conducted to assess the dose-response relationship between PA and HD risk.
Results:
Compared to the least active participants, a low risk of HD was significantly associated with a higher PA volume. With regards to frequency, a lower HD risk was associated with performing vigorous PA except for 3–5 days/week. The frequency and duration of light as well as moderate PA had no significant associations with HD risk after adjusted by using covariates. A non-linear association was also noted, with increased PA being associated with decreased HD risk, with steeper reductions in HD risk at low activity levels than at high activity levels. There was a non-linear association between PA and HD risk in participants in male and aged older than 65 years.
Conclusions:
An inverse non-linear dose-response association was detected between the total volume of PA and HD risk. As PA increased to 4,000 METs-min/week, HD risk in the overall population decreased by approximately 26%, while further increases in PA did not produce any further marked reduction in the risk. A vigorous intensity of PA was associated with a reduced risk of HD and is strongly recommended.
1 Introduction
Globally, cardiovascular diseases (CVD) are the leading causes of death. According to the World Health Organization, 17.9 million people die from CVD each year, representing 32% of global deaths (1). It has been postulated that by 2030, this number will increase to ∼23.3 million (1). Heart diseases (HD) include myocardial infarction, coronary heart disease, angina pectoris, and congestive heart failure among others. Myocardial infarction (MI) is associated with 15% of global mortality (2), while heart failure (HF) affects >26 million people globally (3). Cardiovascular disease-associated mortality as well hospitalization rates keep increasing (4). Coupled with increasing health care costs for HD (5), the already overburdened traditional health care model is a cause for concern.
Lifestyle changes are closely associated with fitness (6, 7). Among the least physically active adults, sitting is correlated with all-cause and CVD-associated mortality risk (6), while physical activity (PA) contributes to lowering the risks of CVD in all-age stages (8, 9). PA can reduce the risk of developing MI, moreover, self-reported regular PA is associated with a 45% lower case fatality in MI with a dose-response association between increasing levels of PA and decreased same-day fatality (10). Higher physical activities are associated with low mortality outcomes for coronary heart disease patients (11). PA interventions are effective as therapeutic options for heart failure patients after invasive treatment of angina pectoris (12). However, Bahls et al. denied the causal relationship between PA and sedentary behaviors with the risk of coronary artery disease, myocardial infarction, and ischemic stroke (13). Thus, the bias of the relationship between PA and HD may be influenced by multiple factors.
The characteristics of PA play key roles in HD-associated morbidity and mortality. A higher level of PA has been noted for coronary heart disease (11), while a dose-dependent protective effect of PA on CVD mortality has been reported in older adults (8). Different intensities of PA are recommended to lower HD risk (6, 10). The duration and frequency of PA can also affect the relationship between PA and HD. We aimed at determining the association between PA and the risk of HD morbidity among Chinese middle-aged and older individuals. We used the China Health and Retirement Longitudinal Study (CHARLS) data from 2018, which is the newest version of nationally representative investigation among Chinese population aged ≥45 years. Moreover, associations between various PA dimensions (intensity, frequency, duration, and volume) and HD-associated morbidity were assessed to establish a better PA protocol for HD prevention.
2 Methods
2.1 Study design
This cross-sectional study was based on the CHARLS, which assessed the health, social and economic status of nationally representative samples covering 450 villages and 150 counties in 28 provinces (14). This survey involved Chinese community-dwelling adults aged 45 or older and their spouses. Multi-stage stratified probability-proportional-to-size sampling method was used for sample size determination. The data adopted in this study was the latest version of CHARLS (Wave 4) data available. CHARLS was approved by the Biomedical Ethics Review Committee of Peking University (Approval no. IRB00001052-11015). Written informed consents were obtained from all participants.
2.2 Outcome variables
Participants were asked: “Have you been diagnosed with heart attack, coronary heart disease, angina, congestive heart failure, or other heart problems by a doctor?” We considered that the individual had HD when the response was “yes”.
2.3 Assessment of physical activities
Respondents were asked to finish a questionnaire about weekly PA in three predefined intensity categories. Indications and examples of intensity were: (1) Vigorous physical activities (VPA): Activities that cause shortness of breath, including carrying heavy stuff, digging, hoeing, aerobic workout, bicycling at a fast speed, and riding a cargo bike/motorcycle among others; (2) Moderate physical activities (MPA): Activities that make one breath faster than usual, including carrying light stuff, bicycling at a normal speed, mopping, Tai-Chi, and speed walking; (3) Light physical activities (LPA) such as walking at home and work. Each intensity category of PA was asked to choose the frequency (times per week) and how much time of PA was conducted in one day (<10 min, 10–30 min, 30 min–2 h, 2–4 h, ≥4 h). The median daily PA time was used to calculate PA volume. The highest category for daily PA time was open-ended, then the width of the interval was obtained by referring to other intervals.
Metabolic equivalent of task (MET) was cited to calculate the volume of PA with considerations of intensity. Resting energy expenditure during quiet sitting was defined as one MET. According to the Physical Activity Guidelines Advisory Committee Scientific Report of 2018 (15), we assigned 6.0 METs, 3.1 METs, and 1.6 METs for VPA, MPA, and LPA, respectively. The weekly PA volume for each intensity category equals the product of PA frequency, the daily duration of PA, and the value assigned for each category. The total volume of PA (TPA) equals the sum of VPA, MPA, and LPA. The TPA volume was classified by quartiles.
2.4 Covariates
Demographic characteristics, including age, sex (male/female), marital status (married/separated/divorced/widowed, and never married), education level (below junior high school, senior high school and vocational school, college and above), and place of residence (rural, urban) were self-reported. Health-related behaviors included smoking status (never smoked, quit smoking, current smoker), drinking frequency in the past (never, ≤1/month, >1/month), and sleep duration (≤7 h, 7–8 h, ≥8 h). Possible confounding variables and effect modifiers were identified through a review of the literature and integrated into a directed acyclic graph that was used to guide the modeling strategy (16–22) (Figure 1). These covariates included age, sex, marital status, education and residency. Considering potential reverse causation, smoking status, drinking frequency, and sleep duration were not included as confounders in the adjusted models.
Figure 1
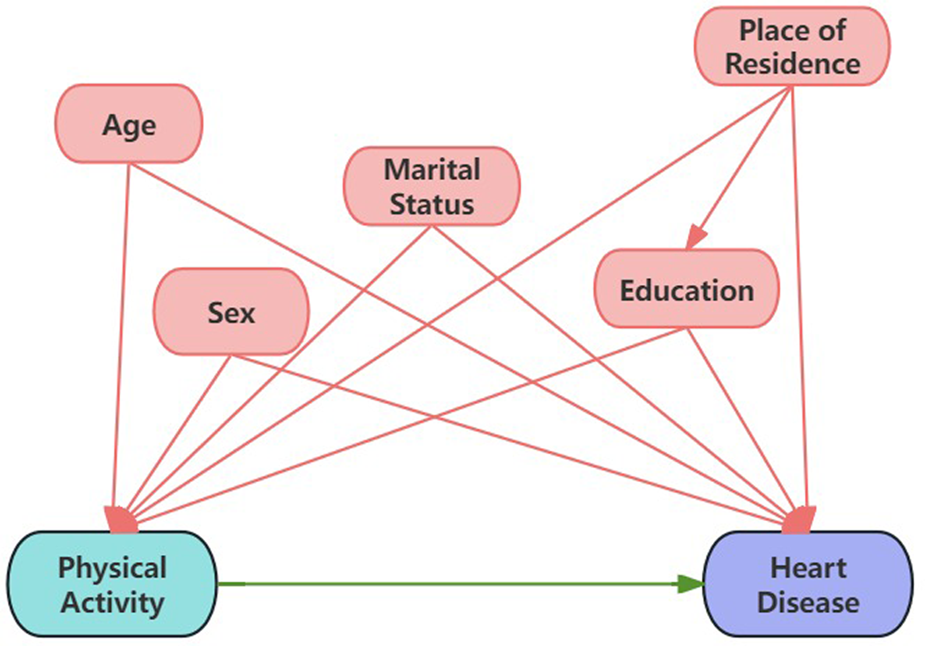
Directed acyclic graph (DAG) illustrating the causal effect of physical activity on heart disease.
2.5 Statistical analysis
STATA 16.0 was used for statistical analyses. Descriptive statistics for participant characteristics are presented according to the self-reported doctor diagnosis of HD. Continuous data are expressed as mean ± SD and analyzed with student's t-test. Categorical variables were expressed as counts and percentages and were compared using the chi-square test. Multiple logistic regression analysis was used to explore the association between various dimensions of PA and the risk of HD. Model building started with univariate analyses. Multivariate Model was adjusted for potential confounding factors (including age, sex, marital status, education and residency). Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated to show the associations between PA and HD-associated morbidity. A restricted cubic spline (RCS) was used to assess the dose-response relationship between PA and HD risk with three knots at the 25th, 50th and 75th percentiles of PA levels. The RCS models were adjusted for age, sex, marital status, education and residency. The dose-response relationships between PA and HD for different ages and sex were also determined. Multiple imputation was used to impute missing data, and sensitivity analysis was performed on the imputed data. All tests were two-tailed, and p < 0.05 was considered significant.
3 Results
3.1 Demographic characteristics
Baseline parameters for demographics, lifestyle behaviors, and living conditions of cases and controls are shown in Table 1. Based on inclusion criteria, 16,927 participants from CHARLS 2018 were included in this study, of whom 8,267 (48.84%) were male, and 1,350 (7.98%) were HD patients. Age, sex, marital status, drinking frequency, smoking status, residency, education, and sleep duration were associated with HD risk.
Table 1
| Characteristic | Total | Heart disease | Normal | P-value |
|---|---|---|---|---|
| (N = 16,927) | (N = 1,350) | (N = 15,577) | ||
| Age, year, mean (SD) | 61.17 (10.27) | 60.96 (10.26) | 63.59 (9.99) | 0.001 |
| Sex, n (%) | 0.001 | |||
| Male | 8,267 | 7,700 (45.49%) | 567 (3.35%) | |
| Female | 8,660 | 7,877 (46.54%) | 783 (4.63%) | |
| Marital status, n (%) | 0.022 | |||
| Married or cohabiting | 14,577 | 13,444 (79.42%) | 1,133 (6.69%) | |
| Separated, divorced or widowed | 2,247 | 2,036 (12.03%) | 211 (1.25%) | |
| Never married | 103 | 97 (0.57%) | 6 (0.04%) | |
| Drinking frequency, n (%) | 0.001 | |||
| ≤1/month | 4,656 | 4,381 (25.8%8) | 275 (1.62%) | |
| >1/month | 1,300 | 1,199 (7.08%) | 101 (0.6%) | |
| Never | 10,971 | 9,997 (59.06%) | 974 (5.75%) | |
| Smoking status, n (%) | 0.001 | |||
| Current smoker | 4,732 | 4,438 (26.22%) | 294 (1.74%) | |
| Quit | 2,318 | 2,089 (12.34%) | 229 (1.35%) | |
| Never | 9,877 | 9,050 (53.46%) | 827 (4.89%) | |
| Residency, n (%) | 0.001 | |||
| Urban | 4,641 | 4,188 (24.74%) | 453 (2.68%) | |
| Rural | 12,286 | 11,389 (67.28%) | 897 (5.3%) | |
| Education, n (%) | 0.051 | |||
| Junior high school or less | 14,778 | 13,627 (80.5%) | 1,151 (6.8%) | |
| Senior high school and vocational school | 2,009 | 1,825 (10.78%) | 184 (1.09%) | |
| College or higher | 140 | 125 (0.74%) | 15 (0.09%) | |
| Sleep duration, hours, n (%) | 0.001 | |||
| <7 | 4,732 | 4,438 (26.22%) | 294 (1.74%) | |
| 7–8 | 2,318 | 2,089 (12.34%) | 229 (1.35%) | |
| ≥8 | 9,877 | 9,050 (53.46%) | 827 (4.89%) | |
Participants’ characteristics stratified by HD.
3.2 Multiple logistic regression analysis of PA and HD
3.2.1 Volume of PA
Multivariate logistic regression results for associations between TPA and HD are presented in Table 2. In univariate model, compared to the first quartile of TPA, a low onset risk of HD was significantly associated with a high TPA in the 3rd and 4th quartiles of TPA. After adjustment by age, sex, marital status, education, and residency, multivariate model showed the same trend of association between TPA and HD risk. Compared to the least active individuals, the risk of HD in most active participants was lower by 23% (OR 0.77 95% CI 0.65–0.92). In addition, an inverse association was detected between TPA and HD risk (p-trend <0.001) in both two models.
Table 2
| Total PA score | Univariate model | Multivariate model | ||
|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | |
| Q1 | 1 | 1 | ||
| Q2 | 0.87 (0.75, 1.01) | 0.074 | 0.89 (0.77, 1.04) | 0.143 |
| Q3 | 0.75 (0.63, 0.88) | 0.001 | 0.82 (0.69, 0.97) | 0.019 |
| Q4 | 0.62 (0.52, 0.73) | 0.001 | 0.77 (0.65, 0.92) | 0.004 |
| P-trend | 0.001 | 0.001 | ||
Logistic regression analyses of associations between TPA and HD status.
OR, odds ratio; CI, confidence interval. Univariate Model was unadjusted; multivariate model was adjusted for age, sex, marital status, education and place of residence.
3.2.2 Frequency of PA
The onset risk of HD was analyzed by the frequency of each intensity category. Compared to participants with no activity, a higher frequency of VPA was associated with a lower risk of HD, as shown in univariate model (Table 3). However, after adjusted by confounding factors, participants who performed VPA for 3–5 days per week had no significant difference in HD risk, relative to those of no activity (Table 3). After adjusting for potential confounding factors, multivariate model demonstrated a 30% lower risk of HD (OR 0.70, 95% CI 0.52–0.94) for individuals engaging in 1–2 days of VPA per week. Similarly, participants engaging in 6–7 days of VPA per week exhibited a 28% lower risk of HD (OR 0.72, 95% CI 0.61–0.85). Before adjustment, a frequency of 6–7 days MPA per week was associated with a lower risk of HD (OR 0.88, 95% CI 0.77–0.99), but it was not significant after adjustment. A higher frequency of LPA was not associated with decreased HD risk (Table 3).
Table 3
| Variables | Univariate model | Multivariate model | ||
|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | |
| Frequency | ||||
| VPA | ||||
| No activity | 1 | 1 | ||
| 1–2 day/week | 0.61 (0.45, 0.81) | 0.001 | 0.70 (0.52, 0.94) | 0.017 |
| 3–5 day/week | 0.72 (0.58, 0.90) | 0.004 | 0.87 (0.69, 1.09) | 0.223 |
| 6–7 day/week | 0.59 (0.50, 0.69) | 0.001 | 0.72 (0.61, 0.85) | 0.001 |
| MPA | ||||
| No activity | 1 | 1 | ||
| 1–2 day/week | 0.88 (0.69, 1.11) | 0.271 | 0.92 (0.73, 1.17) | 0.487 |
| 3–5 day/week | 0.84 (0.69, 1.02) | 0.085 | 0.90 (0.74, 1.10) | 0.316 |
| 6–7 day/week | 0.88 (0.77, 0.99) | 0.041 | 0.91 (0.80, 1.04) | 0.163 |
| LPA | ||||
| No activity | 1 | 1 | ||
| 1–2 day/week | 0.72 (0.51, 1.04) | 0.077 | 0.74 (0.51, 1.06) | 0.097 |
| 3–5 day/week | 0.89 (0.70, 1.13) | 0.336 | 0.92 (0.72, 1.18) | 0.516 |
| 6–7 day/week | 0.96 (0.83, 1.11) | 0.556 | 0.99 (0.85, 1.15) | 0.860 |
| Duration | ||||
| VPA | ||||
| Inactive | 1 | 1 | ||
| 10–29 min/day | 0.49 (0.24, 1.00) | 0.050 | 0.55 (0.27, 1.13) | 0.106 |
| 30–119 min/day | 0.72 (0.56, 0.92) | 0.010 | 0.80 (0.62, 1.04) | 0.093 |
| ≥120 min/day | 0.61 (0.52, 0.70) | 0.001 | 0.75 (0.64, 0.87) | 0.001 |
| MPA | ||||
| Inactive | 1 | 1 | ||
| 10–29 min/day | 0.88 (0.68, 1.12) | 0.291 | 0.87 (0.68, 1.11) | 0.260 |
| 30–119 min/day | 0.95 (0.82, 1.10) | 0.504 | 0.96 (0.82, 1.11) | 0.559 |
| ≥120 min/day | 0.80 (0.69, 0.92) | 0.002 | 0.88 (0.76, 1.02) | 0.096 |
| LPA | ||||
| Inactive | 1 | 1 | ||
| 10–29 min/day | 0.93 (0.74, 1.17) | 0.536 | 0.95 (0.75, 1.19) | 0.627 |
| 30–119 min/day | 1.00 (0.85, 1.17) | 0.972 | 1.00 (0.85, 1.17) | 0.984 |
| ≥120 min/day | 0.87 (0.74, 1.03) | 0.104 | 0.94 (0.79, 1.11) | 0.473 |
Associations between HD risk and PA frequency, duration, and intensity.
VPA, vigorous physical activity; MPA, moderate physical activity; LPA, light physical activity; OR, odds ratio; CI, confidence interval. Univariate model was unadjusted; multivariate model was adjusted for age, sex, marital status, education and place of residence.
3.2.3 Duration of physical activity
The logistic regression results for the duration of different intensity PA and the risk of HD were presented in Table 3. In univariate model, a longer duration of VPA was associated with a lower risk of HD compared to inactive participants. Participants engaging in VPA for more than 30 min per day had a lower risk of HD (p < 0.05), as did those engaging in MPA for more than 120 min per day (p < 0.05). However, there was no difference in the risk of HD among different durations of LPA. After adjusting for multiple variables in multivariate model, participants engaging in VPA for more than 120 min per day had a lower risk of HD (p < 0.05). There was no significant association found between the duration of MPA and LPA and the risk of HD (p > 0.05).
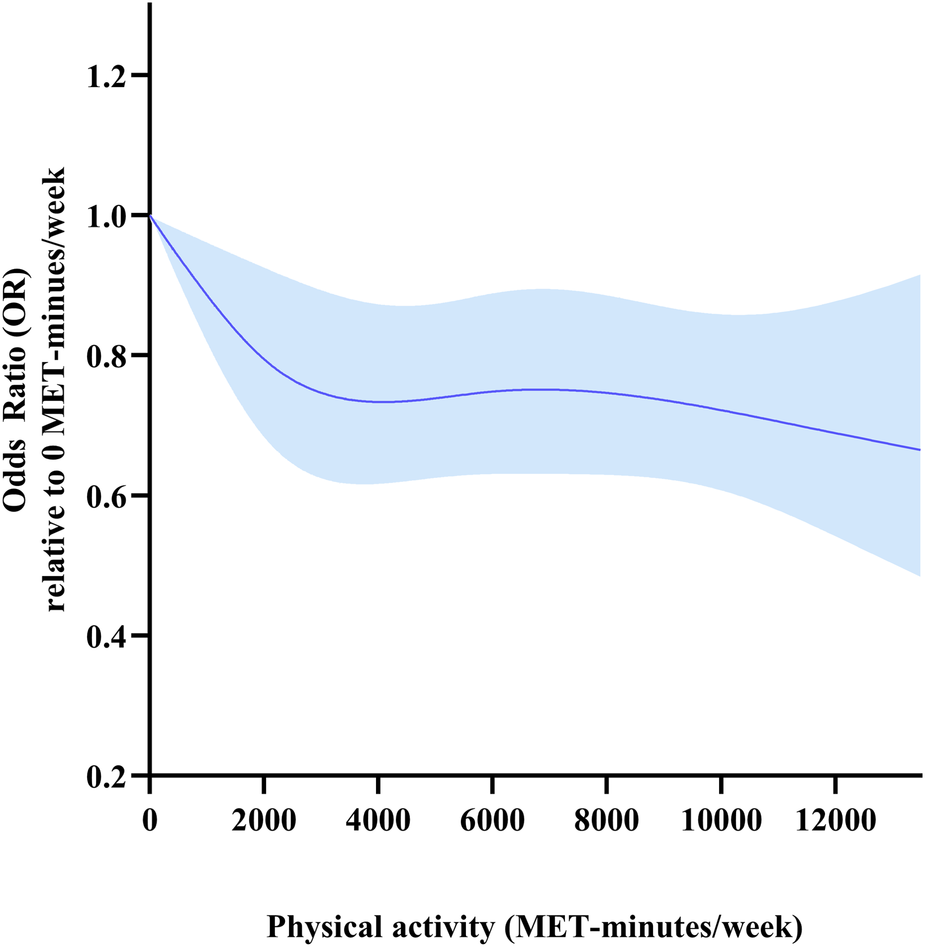
3.2.4 Dose-response relationship between PA and HD risk
The dose-response relationship between TPA and HD risk is shown in Figure 2. A nonlinear dose-response relationship with steeper reductions in HD risk at low TPA levels than at high TPA levels was detected (p overall < 0.001, p for non-linearity = 0.014). The risk of HD decreased rapidly as TPA level increased from 0 to 4,000 METs-min/week, but more slowly for those with TPA above 4,000 METs-min/week. The risk of HD was 26% lower in participants with TPA of 4,000 METs-min/week than in those with no physical activity (OR 0.74, 95% CI 0.62–0.89).
Figure 2
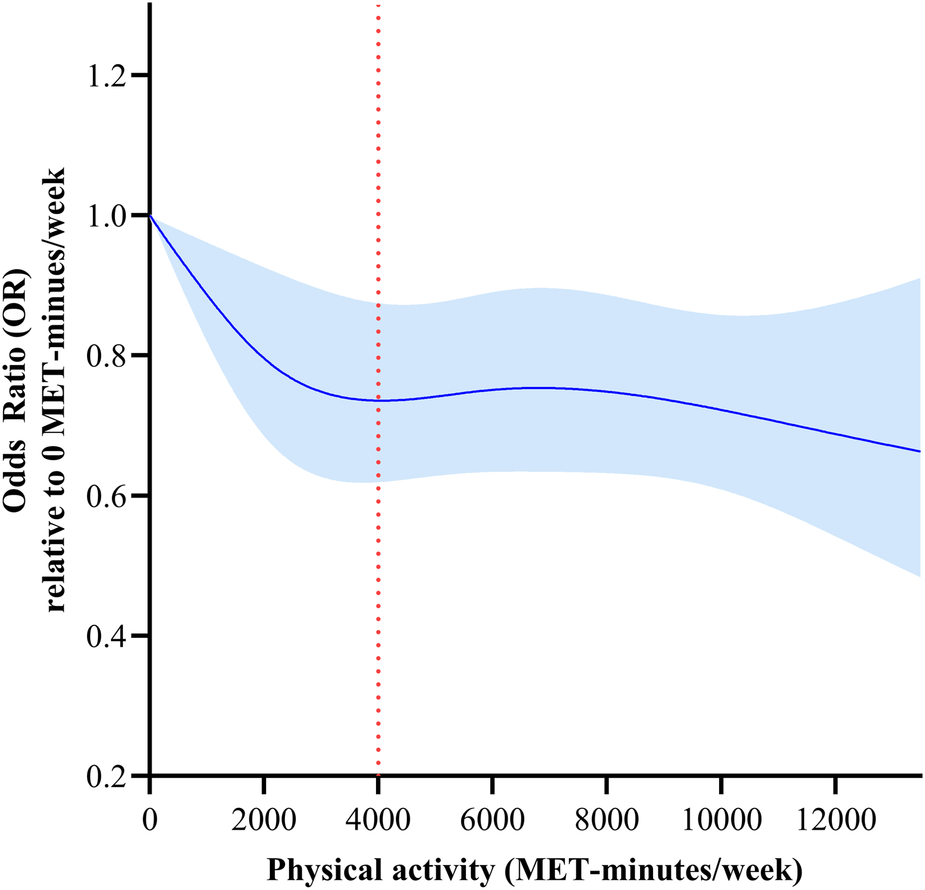
Dose-response relationships between total physical activity (METs-min/week) and HD risk. Models were adjusted for age, sex, marital status, education, residency, smoking status, drinking frequency and sleep duration. This graph shows ORs (solid line) with 95% CI (shaded area).
3.2.5 Interaction and subgroup analysis
To interpret the potential heterogenous effect in people with different demographic characteristics, we ran the statistical models to examine the interaction of age and physical activity. There was a significant interaction between age and PA variability on HD (p for interaction = 0.049). Age-stratified analysis was conducted to interpret associations among participants with different ages. The risk of HD decreased with increasing TPA. A reverse linear dose-response relationship was found between TPA and HD for participants aged <65 years (p for non-linearity >0.05, Figure 3a), while a nonlinear dose-response relationship between TPA and HD was observed in participants aged ≥65 years (p for non-linearity < 0.05, Figure 3b). Among participants aged ≥65 years, a 36% lower risk of HD was associated with a TPA level of about 4,000 METs-min/week (OR 0.64, 95% CI 0.50–0.81).
Figure 3
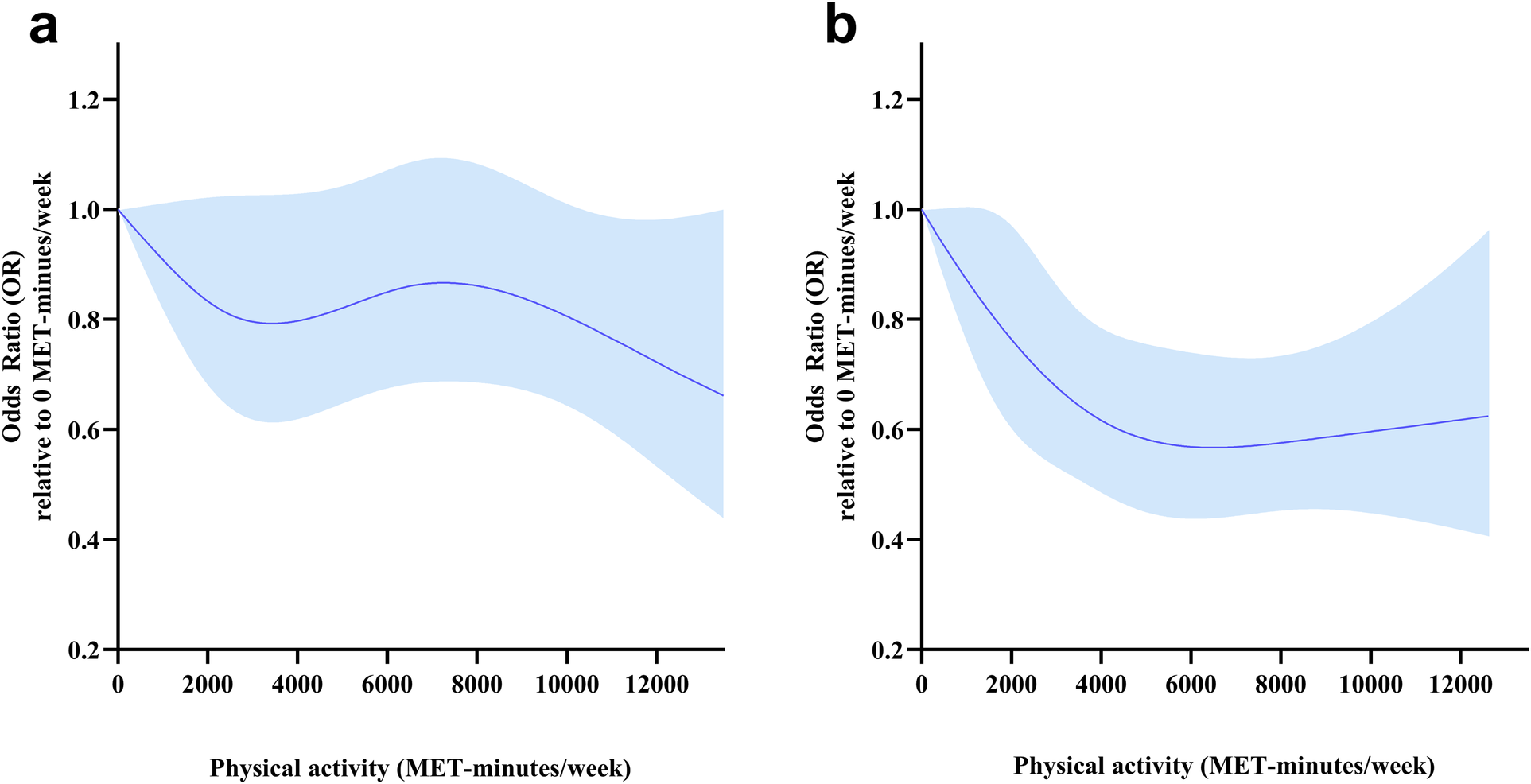
Dose-response relationships between total physical activity (METs-min/week) and HD risk for different age groups. Models were adjusted for sex, marital status, education, residency, smoking status, drinking frequency and sleep duration. This graph shows ORs (solid line) with 95% CI (Shaded area). (a) Participants aged <65 years. (b) Participants aged ≥65 years.
There was no significant interaction between sex and physical activity variability on HD (p for interaction = 0.234). Given the observed sex-specific variability in HD as indicated by the results of the chi-square test, further subgroup analyses were conducted to elucidate the potential dose-response relationship between PA and HD within the context of sex. In the sex-stratified analysis (Figure 4), there was a linear dose-response relationship between TPA and HD risk in males (pnon-linearity > 0.05), and the OR for HD decreased sharply as the PA increased. However, the dose-response relationship between TPA and HD risk was not statistically significant in women.
Figure 4
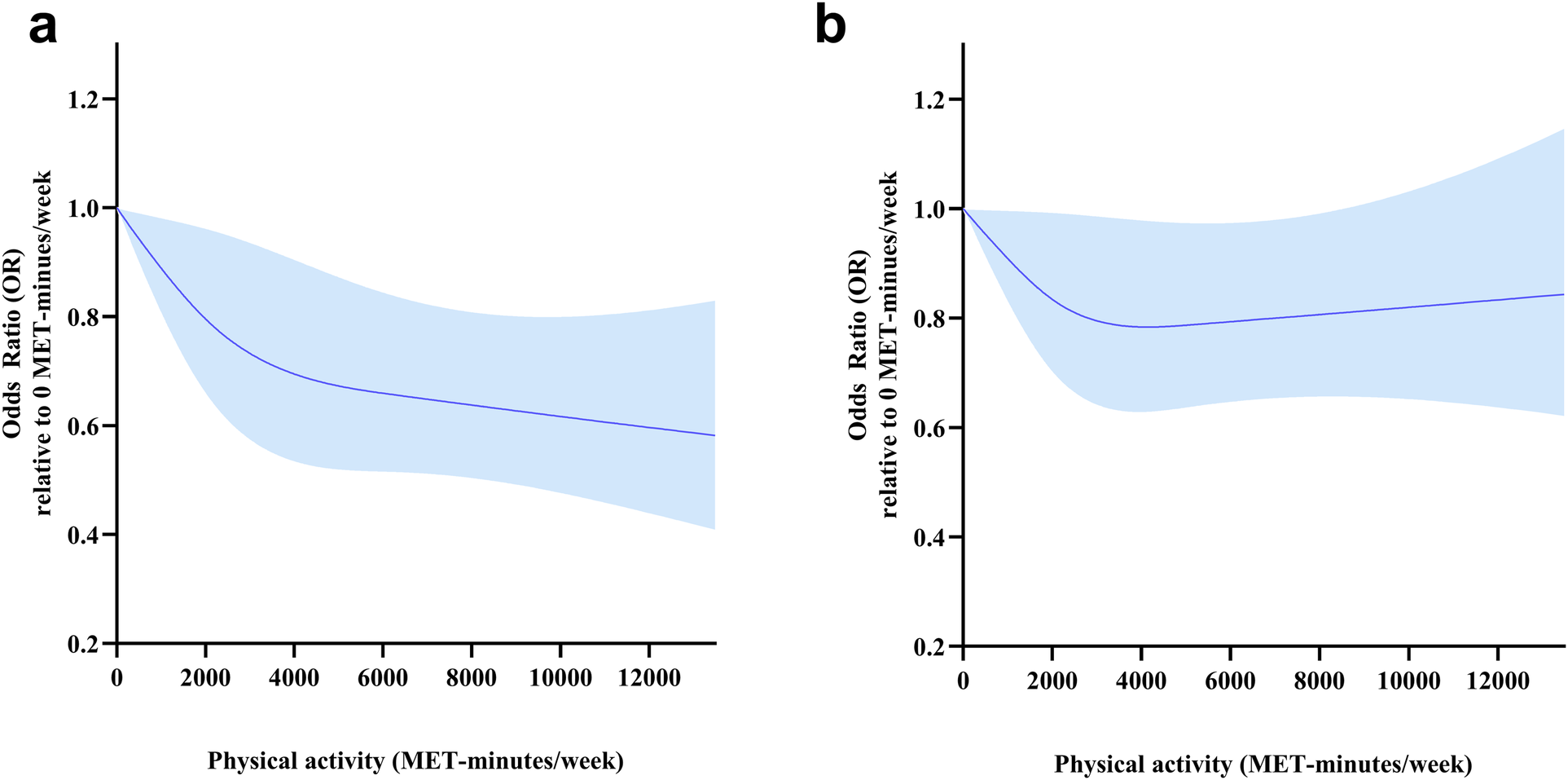
Dose-response relationships between total physical activity (METs-min/week) and HD risk for different sex groups. Models were adjusted for age, marital status, education, residency, smoking status, drinking frequency and sleep duration. This graph shows ORs (solid line) with 95% CI (shaded area). (a) Males. (b) Females.
Missing values were imputed using multiple imputation, 19,498 participants were included in the sensitivity analysis. A similar nonlinear dose-response relationship between TPA and HD risk was observed in the sensitivity analysis (poverall < 0.001, pnon-linearity = 0.025), and the shape of the dose-response curve was similar to the main analysis (Figure 5).
Figure 5
Sensitivity analyses of dose-response relationships between total physical activity (METs·min/week) and risk of heart diseases. Models were adjusted for age, sex, marital status, education, residency, smoking status, drinking frequency and sleep duration. This graph shows ORs (solid line) with 95% CI (shaded area).
4 Discussion
We established that a higher TPA was associated with a low HD risk, and an inverse non-linear dose-response relationship was detected. The plateau of TPA was 4,000 METs-min/week, with a 26% reduction in HD risk. A higher frequency and longer duration of VPA were associated with a low HD risk, while the association was insignificant in both MPA and LPA after adjustment of demographics, lifestyle behaviors, and living conditions. Subgroup analysis revealed an inverse nonlinear dose-response relationship between TPA and HD for participants aged ≥65 years, and a 36% lower risk of HD was associated with a TPA level of 4,000 METs-min/week in participants aged ≥65 years. A linear dose-response relationship between TPA and HD risk was detected in males instead of females.
TPA was inversely associated with HD risk. Insufficient PA increases the risk for cardiovascular diseases, especially coronary arterial disease, and myocardial infarction (23). Exercise training should be part of cardiac rehabilitation programs. Cattadori et al. (24) reported that PA protects against the onset of HF and provides secondary prevention for HF patients. Moreover, exercise impairment is a prognostic factor for HF (24). PA is recommended for congenital heart disease patients (25). We found that the higher the TPA levels, the lower the HD risk, thus we postulated that a lack of PA is a risk factor for HD, and TPA volume is a prospective indicator for HD risk.
The intensity of PA is a vital indicator for preventing HD risk. Previous studies reported an inverse association between relative intensities of physical activity (an individual's perceived level of exertion) and coronary heart disease risk, and moderate-intensity physical activity was recommended to reduce coronary heart disease risks (26). Regular vigorous exercises also reduce the risk of developing cardiovascular diseases, compared to moderate-intensity activity (27). Lee et al. (28) reported an inverse association between PA and coronary heart disease-associated morbidity while light-to-moderate activity was associated with decreased coronary heart disease morbidity among women. Sesso et al. (29) found a nonsignificant inverse association between PA and coronary heart disease occurrence. We established that VPA is correlated with a lower HD risk, even when performed at a low frequency or for a short duration. Importantly, compared to participants without physical activity, vigorous-intensity activity was associated with reduced risk of independent of the volume of TPA, which is in accordance with the conclusion that sedentary people can benefit from regular short activity periods of as little as 1 min (30). Higher intensity activities provide greater health benefits with a dose-response relationship (31). Although light intensity PA can confer accumulating health benefits (32), and moderate-intensity PA is recommended in several physical activity guidelines (33, 34), our findings indicate that the benefits of accumulating light-moderate intensity PA for reducing the risk of HD may be dismissed by other covariates. Thus, vigorous-intensity PA is strongly recommended to reduce the risk of HD. The recommendation of intensity for HD patients has not been fully confirmed. Light to moderate intensity PA has been suggested in some guidelines (35), but, habitual vigorous activities are not associated with increased risk of subsequent myocardial infarctions in coronary heart disease patients (36). Patients with specific lesions or complications may require counseling regarding precautions and recommendations.
There was a nonlinear dose-response relationship between HD risk and TPA levels. Low TPA levels were associated with steeper reductions in HD risk, and the percentage of risk reduction was less with the increase in TPA. According to physical activity guidelines for Americans, benefits begin with a moderate PA volume, but greater amounts of PA result in further reductions in cardiovascular disease risks (37). This theory was in accordance with our results. A plateau was reached at 4,000 METs-min/week. Assuming causality, PA levels should be increased to reduce HD risk. There is an economical level of TPA that is necessary to reduce the risk of HD, rather than “the more, the better”. An economical level of TPA to reduce the risk of HD by 36% for participants aged than 65 years was established to be 4,000 METs-min/week, which is higher than some physical activity guidelines (33, 34), it would need a higher TPA to prevent instead of improving HD (37). Interestingly, the risk reduction of HD was more sensitive in males than females. Consistently, the strength of association between daily step count and CVD risk appeared to be stronger in men than in women (38). Sex difference in the recommendation of PA also exists, and it was encouraged to perform a higher TPA for women compared to men to prevent HD. Overall, higher TPA levels are recommended to prevent HD risks, and a basic TPA score was recommended for the best economic protection effect.
This study has some strengths, including the use of a nationwide representative sample covering 28 provinces in mainland China and the use of the CHARLS database, which has proven its validity and reliability in a large number of studies (14). This study also has some limitations. First, causal association between PA and the risk of HD cannot be interpreted by a cross-sectional study. Second, recall bias is not avoidable in self-reported questionnaires, and the species of HD were not distinguished in the questionnaire. Third, leisure-time PA and work-related PA were mixed so that the PA paradox may be neglected (39). Finally, the PA data were collected using self-reported questionnaires, which means that PA was not strictly continuous when categorized into different intensities. The various intensities of physical activity were somewhat isolated from each other, and sedentary behavior was not accounted for in the analysis, which restricted our ability to analyze one domain of PA intensity while adjusting for the effects of other intensities based on 24-h activities. This limitation may introduce bias when interpreting the differential effects of various intensities. In future studies, more consideration should be given to using accelerometers to obtain physical activity data, comprehensively considering physical activity, sedentary behavior and sleep, and conducting more in-depth analysis based on isochronous substitution and other models.
5 Conclusion
An inverse non-linear dose-response association was detected between total volume of physical activity and HD risk. As physical activity increased to 4,000 METs-min/week, HD risk in the overall population decreased by approximately 26%, while further increases in physical activity did not produce any further marked reduction in the risk. A vigorous intensity of physical activity was associated with a reduced risk of HD and is strongly recommended.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
YL: Data curation, Formal Analysis, Funding acquisition, Writing – original draft, Writing – review & editing. CY: Data curation, Formal Analysis, Methodology, Writing – original draft. TC: Methodology, Software, Writing – original draft. LZ: Data curation, Methodology, Writing – original draft. GZ: Data curation, Writing – original draft. YC: Conceptualization, Funding acquisition, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This analysis was based upon work funded by Humanities and Social Science Fund of Ministry of Education of China (Grant No. 23YJC890005); China Postdoctoral Science Foundation (Grant No. 2021M693736); the Fundamental Research Funds for the Central Universities (Grant NO. 2022CDSKXYTY003 and 2024CDJSKXYTY03); Natural Science Foundation of the Jiangsu Education Institutions of China (Grant No. 22KJB180017) and Xuzhou Natural Science Foundation (Grant No. KC21029).
Acknowledgments
We would like to acknowledge the China Health and Retirement Longitudinal Study (CHARLS) team for providing high-quality, nationally representative data.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Aalami OO Lin J Savage D Ho V Bertges D Corriere M . Use of an app-based exercise therapy program including cognitive-behavioral techniques for the management of intermittent claudication. J Vasc Surg. (2022) 76(6):1651–6.e. 10.1016/j.jvs.2022.06.087
2.
Allen JD Stabler T Kenjale A Ham KL Robbins JL Duscha BD et al Plasma nitrite flux predicts exercise performance in peripheral arterial disease after 3months of exercise training. Free Radical Biol Med. (2010) 49(6):1138–44. 10.1016/j.freeradbiomed.2010.06.033
3.
Savarese G Lund LH . Global public health burden of heart failure. Card Fail Rev. (2017) 3(1):7–11. 10.15420/cfr.2016:25:2
4.
Zou Z Cini K Dong B Ma Y Ma J Burgner DP et al Time trends in cardiovascular disease mortality across the BRICS: an age-period-cohort analysis of key nations with emerging economies using the global burden of disease study 2017. Circulation. (2020) 141(10):790–9. 10.1161/CIRCULATIONAHA.119.042864
5.
Xie P Li X Guo F Zhang D Zhang H . Direct medical costs of ischemic heart disease in urban Southern China: a 5-year retrospective analysis of an all-payer health claims database in Guangzhou City. Front Public Health. (2023) 11:1146914. 10.3389/fpubh.2023.1146914
6.
Stamatakis E Gale J Bauman A Ekelund U Hamer M Ding D . Sitting time, physical activity, and risk of mortality in adults. J Am Coll Cardiol. (2019) 73(16):2062–72. 10.1016/j.jacc.2019.02.031
7.
Liang ZD Zhang M Wang CZ Yuan Y Liang JH . Association between sedentary behavior, physical activity, and cardiovascular disease-related outcomes in adults-A meta-analysis and systematic review. Front Public Health. (2022) 10:1018460. 10.3389/fpubh.2022.1018460
8.
Barengo NC Antikainen R Borodulin K Harald K Jousilahti P . Leisure-time physical activity reduces total and cardiovascular mortality and cardiovascular disease incidence in older adults. J Am Geriatr Soc. (2017) 65(3):504–10. 10.1111/jgs.14694
9.
Saint-Maurice PF Coughlan D Kelly SP Keadle SK Cook MB Carlson SA et al Association of leisure-time physical activity across the adult life course with all-cause and cause-specific mortality. JAMA Netw Open. (2019) 2(3):e190355. 10.1001/jamanetworkopen.2019.0355
10.
Peytz NC Jabbari R Bojesen SE Nordestgaard B Schnohr P Prescott E . Physical activity and risk of instant and 28-day case-fatality in myocardial infarction. PLoS One. (2019) 14(5):e0217398. 10.1371/journal.pone.0217398
11.
Stewart RAH Held C Hadziosmanovic N Armstrong PW Cannon CP Granger CB et al Physical activity and mortality in patients with stable coronary heart disease. J Am Coll Cardiol. (2017) 70(14):1689–700. 10.1016/j.jacc.2017.08.017
12.
Irzmański R Kapusta J Kowalski J . [Role of controlled physical activity as a method of therapy in patients with heart failure after invasive treatment of angina pectoris]. Pol Merkur Lekarski. (2014) 37(218):77–81.
13.
Bahls M Leitzmann MF Karch A Teumer A Dorr M Felix SB et al Physical activity, sedentary behavior and risk of coronary artery disease, myocardial infarction and ischemic stroke: a two-sample Mendelian randomization study. Clin Res Cardiol. (2021) 110(10):1564–73. 10.1007/s00392-021-01846-7
14.
Zhao Y Hu Y Smith JP Strauss J Yang G . Cohort profile: the China health and retirement longitudinal study (CHARLS). Int J Epidemiol. (2014) 43(1):61–8. 10.1093/ije/dys203
15.
Pescatello LS Buchner DM Jakicic JM Powell KE Kraus WE Bloodgood B et al Physical activity to prevent and treat hypertension: a systematic review. Med Sci Sports Exerc. (2019) 51(6):1314–23. 10.1249/MSS.0000000000001943
16.
Molanorouzi K Khoo S Morris T . Motives for adult participation in physical activity: type of activity, age, and gender. BMC Public Health. (2015) 15:66. 10.1186/s12889-015-1429-7
17.
Yuan S Elam KK Johnston JD Chow A . The influence of marriage and cohabitation on physical activity among middle-aged and older people. J Appl Gerontol. (2024) 43(2):139–48. 10.1177/07334648231203124
18.
Dhindsa DS Khambhati J Schultz WM Tahhan AS Quyyumi AA . Marital status and outcomes in patients with cardiovascular disease. Trends Cardiovasc Med. (2020) 30(4):215–20. 10.1016/j.tcm.2019.05.012
19.
Sun Y . Physical activity’s impact on rural older adult health: the multiple mediating effects of education, income, and psychological capital. Front Public Health. (2023) 11:1173217. 10.3389/fpubh.2023.1173217
20.
Schultz WM Kelli HM Lisko JC Varghese T Shen J Sandesara P et al Socioeconomic status and cardiovascular outcomes: challenges and interventions. Circulation. (2018) 137(20):2166–78. 10.1161/CIRCULATIONAHA.117.029652
21.
Okuyama K Abe T Li X Toyama Y Sundquist K Nabika T . Neighborhood environmental factors and physical activity status among rural older adults in Japan. Int J Environ Res Public Health. (2021) 18(4):1450. 10.3390/ijerph18041450
22.
Clark AM DesMeules M Luo W Duncan AS Wielgosz A . Socioeconomic status and cardiovascular disease: risks and implications for care. Nat Rev Cardiol. (2009) 6(11):712–22. 10.1038/nrcardio.2009.163
23.
Yusuf S Hawken S Ounpuu S Dans T Avezum A Lanas F et al Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. (2004) 364(9438):937–52. 10.1016/S0140-6736(04)17018-9
24.
Cattadori G Segurini C Picozzi A Padeletti L Anza C . Exercise and heart failure: an update. ESC Heart Fail. (2018) 5(2):222–32. 10.1002/ehf2.12225
25.
Takken T Giardini A Reybrouck T Gewillig M Hovels-Gurich HH Longmuir PE et al Recommendations for physical activity, recreation sport, and exercise training in paediatric patients with congenital heart disease: a report from the exercise, basic & translational research section of the European Association of Cardiovascular Prevention and Rehabilitation, the European Congenital Heart and Lung Exercise Group, and the Association for European Paediatric Cardiology. Eur J Prev Cardiol. (2012) 19(5):1034–65. 10.1177/1741826711420000
26.
Lee IM Sesso HD Oguma Y Paffenbarger RS Jr . Relative intensity of physical activity and risk of coronary heart disease. Circulation. (2003) 107 (8):1110–6. 10.1161/01.CIR.0000052626.63602.58
27.
Swain DP Franklin BA . Comparison of cardioprotective benefits of vigorous versus moderate intensity aerobic exercise. Am J Cardiol. (2006) 97(1):141–7. 10.1016/j.amjcard.2005.07.130
28.
Lee IM Rexrode KM Cook NR Manson JE Buring JE . Physical activity and coronary heart disease in women: is “no pain, no gain” passe?JAMA. (2001) 285(11):1447–54. 10.1001/jama.285.11.1447
29.
Sesso HD Paffenbarger RS Jr Lee IM . Physical activity and coronary heart disease in men: the Harvard alumni health study. Circulation. (2000) 102 (9):975–80. 10.1161/01.CIR.102.9.975
30.
Healy GN Dunstan DW Salmon J Cerin E Shaw JE Zimmet PZ et al Breaks in sedentary time: beneficial associations with metabolic risk. Diabetes Care. (2008) 31(4):661–6. 10.2337/dc07-2046
31.
McPhee JS French DP Jackson D Nazroo J Pendleton N Degens H . Physical activity in older age: perspectives for healthy ageing and frailty. Biogerontology. (2016) 17(3):567–80. 10.1007/s10522-016-9641-0
32.
Fuzeki E Engeroff T Banzer W . Health benefits of light-intensity physical activity: a systematic review of accelerometer data of the national health and nutrition examination survey (NHANES). Sports Med. (2017) 47(9):1769–93. 10.1007/s40279-017-0724-0
33.
Piercy KL Troiano RP Ballard RM Carlson SA Fulton JE Galuska DA et al The physical activity guidelines for Americans. JAMA. (2018) 320(19):2020–8. 10.1001/jama.2018.14854
34.
Bull FC Al-Ansari SS Biddle S Borodulin K Buman MP Cardon G et al World health organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. (2020) 54(24):1451–62. 10.1136/bjsports-2020-102955
35.
Pelliccia A Sharma S Gati S Back M Borjesson M Caselli S et al 2020 ESC guidelines on sports cardiology and exercise in patients with cardiovascular disease. Eur Heart J. (2021) 42(1):17–96. 10.1093/eurheartj/ehaa605
36.
Yu S Patterson CC Yarnell JW . Is vigorous physical activity contraindicated in subjects with coronary heart disease? Evidence from the caerphilly study. Eur Heart J. (2008) 29(5):602–8. 10.1093/eurheartj/ehn012
37.
Rejeski WJ Spring B Domanchuk K Tao H Tian L Zhao L et al A group-mediated, home-based physical activity intervention for patients with peripheral artery disease: effects on social and psychological function. J Transl Med. (2014) 12(1):29. 10.1186/1479-5876-12-29
38.
Lin H Sardana M Zhang Y Liu C Trinquart L Benjamin EJ et al Association of habitual physical activity with cardiovascular disease risk. Circ Res. (2020) 127(10):1253–60. 10.1161/CIRCRESAHA.120.317578
39.
Holtermann A Schnohr P Nordestgaard BG Marott JL . The physical activity paradox in cardiovascular disease and all-cause mortality: the contemporary Copenhagen general population study with 104 046 adults. Eur Heart J. (2021) 42(15):1499–511. 10.1093/eurheartj/ehab087
Summary
Keywords
physical activity, heart disease, middle-aged and older individuals, dose-response relationship, intensity
Citation
Liu Y, Yuan C, Chen T, Zhou L, Zhu G and Chen Y (2025) Associations between physical activity and heart disease among middle-aged and older Chinese adults. Front. Cardiovasc. Med. 12:1383888. doi: 10.3389/fcvm.2025.1383888
Received
29 February 2024
Accepted
13 January 2025
Published
24 January 2025
Volume
12 - 2025
Edited by
Klaus-Dieter Schlüter, University of Giessen, Germany
Reviewed by
Stefan Gross, University Medicine Greifswald, Germany
Heather-Jean Foulds, University of Saskatchewan, Canada
Updates
Copyright
© 2025 Liu, Yuan, Chen, Zhou, Zhu and Chen.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Yu Chen chenyu157@cqu.edu.cn
†These authors have contributed equally to this work
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.