- Department of Biomedical Science, Debre Markos University, Debre Markos, Ethiopia
Introduction: Dyspepsia is a group of symptoms located in the gastroduodenal area of the upper gastrointestinal tract characterized by epigastric pain, postprandial completeness, or early satiety and occasionally related to heartburn. Helicobacter pylori is the major causative agent of dyspepsia and gastric-related disorders; besides, it alters different metabolic processes in the human body, such as lipid metabolism and inflammatory processes. Even though dyslipidemia and inflammation are independent risk factors for cardiovascular disorders, we are assessing the interaction between serum lipids and highly sensitive C reactive protein levels among dyspeptic patients to predict potential cardiovascular disorders.
Objectives: To assess serum high sensitive C reactive protein levels and its correlation with lipid profile among dyspeptic patients.
Methods: A hospital-based comparative cross-sectional study was conducted from May 2022 to March 2023 in East Gojjam, Ethiopia. One hundred Helicobacter pylori-positive and 100 Helicobacter pylori-negative dyspeptic patients were included. Data were checked for completeness and entered into SPSS version 26.0 software and analyzed. The association between variables was determined by Pearson correlation analysis. A p-value <0.05 was considered statistically significant.
Result: The mean serum high sensitive C reactive protein was 8.09 ± 7.84 mg/L, and serum high-density lipoprotein, low-density lipoprotein, total cholesterol, and triglyceride were (35.35 ± 7.5, 105.07 ± 87.63, 142.31 ± 71.31, 160.07 ± 43.06) mg/dl, respectively, for Helicobacter pylori positive dyspeptic patients. Among these values, high-density lipoprotein is negatively correlated with high sensitive C reactive and total cholesterol is positively correlated with high sensitive C reactive levels among Helicobacter pylori-infected dyspeptic patients with a p-value < 0.05, but in Helicobacter pylori negative dyspeptic patients, there is no significant correlation between lipid profile and high sensitive C reactive levels.
Conclusion: Serum high sensitive C reactive levels had a negative correlation with high-density lipoprotein and a positive correlation with total cholesterol among Helicobacter pylori-positive dyspeptic patients. Therefore, the significant interaction between serum lipid levels and inflammation exacerbates the potential risk of cardiovascular disorders among Helicobacter pylori-positive dyspeptic patients.
Introduction
Dyspepsia is a group of symptoms located in the gastroduodenal area of the upper gastrointestinal tract characterized by epigastric pain, postprandial completeness, or early satiety and occasionally related to heartburn (1).
Different factors aggravate the disease process of dyspepsia. These are Helicobacter pylori (H. pylori) infection, delayed gastric emptying, hypersensitivity, enteric pathogen, impaired accommodation of the stomach, and diet. Besides, lifestyle factors such as cigarette smoking, alcohol drinking, and khat chewing, and psychosocial factors like stress, anxiety, and depression (2).
Helicobacter pylori is the major causative agent of dyspepsia and gastric-related disorders such as peptic ulcer disease, stomach cancer, and primary stomach lymphoma. These disorders are common community health problems both in industrialized and unindustrialized countries, with greater effect in economically deprived countries due to poor hygienic circumstances. Different studies have shown that half of adults in industrialized countries are infected by Helicobacter pylori bacteria, but in developing countries, the severity is higher, with 90% of adults being infected by H. pylori (3).
Even though H. Pylori is the major causative agent of gastric and gastric-related disorders; it is also linked to extra-gastric complications such as cardiovascular diseases, diabetes mellitus, neurological disorders, gynecological disorders, eye diseases, dermatology, oral mucosa disorders, lung diseases, ear disorders, nose disorders, throat disorders, and blood disorders (4).
H. Pylori infection alters different metabolic processes in the human body. For example, it alters serum lipid levels; alterations in serum lipid levels are the greatest potential risk factors for cardiovascular disorders and metabolic syndrome (5).
Atherosclerosis, the leading cause of mortality worldwide, is the primary factor that contributes to cardiovascular disease (CVD). A well-known atherogenic lipoprotein, low-density lipoprotein, kickstarts vascular inflammation. Inflammation is an independent risk factor for manifestations of atherosclerosis and plays an important role in the underlying pathological process of atherosclerosis (6).
Different studies show the various mechanisms used by H. pylori bacteria to alter the serum lipid profile. Gastric colonization and attack by H. Pylori initiate aggravations in the lipid profile because of debilitated coagulation overflow enactment and autoimmunity because of antigenic sub-atomic mimicry between human epitopes and that of H. pylori, the disability of nutritional absorption, and by triggering an inflammatory reaction to the contamination (7).
H. pylori infection increases the circulating inflammatory markers, especially high-sensitive C-reactive protein (CRP). hs-CRP, produced in the liver and released into the blood, is a representative marker reflecting systemic inflammation. This protein is increased not only in acute but also in chronic diseases, and its slight change in chronic diseases at a low-grade subclinical level has pathophysiological relevance (5).
Various studies focused on the relationship between H. pylori infection and lipid profile, as well as the association between H. pylori infection and different inflammatory markers. However, this study aims to determine the interaction between lipid metabolism and inflammatory processes among dyspeptic patients with or without H. pylori infection to predict potential cardiovascular risk, even though dyslipidemia and inflammation are well-known independent risk factors for the onset of cardiovascular disease (CVD).
Numerous complex biological pathways are involved in the relationship between lipid metabolism and inflammation. Initially, significant pro-inflammatory cytokines, like TNF-α and interleukin 6 (IL-6), are crucial for controlling lipid metabolism (4, 8). Tumor-necrotizing factor alpha (TNF-α) can increase the amount of free fatty acids in the bloodstream by impairing lipoprotein lipase's function and aggravating adipocytes' fat breakdown process. The pro-inflammatory cytokine IL-6 modifies lipoprotein function and raises hepatic triglyceride synthesis (9, 10). However, inflammation suppresses nuclear receptors like peroxisome proliferator-activated receptor (PPAR), which is important for controlling lipid metabolism and hence upsets lipid homeostasis. When inflammatory signals activate the transcription factor nuclear factor kappa (NF-κB), they down regulate genes related to fat metabolism while enhancing the expression of pro-inflammatory genes (11). Furthermore, eicosanoids, lipid mediators sourced from arachidonic acid, have the ability to affect insulin sensitivity and adipocyte activity, thus establishing a connection between lipid metabolism and inflammation (10).
Besides, lipoproteins have the ability to control inflammation and immune cell activity. Due to its ability to transport bioactive lipids, anti-inflammatory and antioxidant proteins, and regulate immune cell activation by mediating cellular cholesterol efflux and reorganizing pattern recognition receptor (PRR) and related co-receptors in membrane lipid rafts, high-density lipoproteins (HDL) in particular are known to possess a variety of immune-modulatory and anti-inflammatory properties (10, 12).
The pro-oxidative enzyme myeloperoxidase (MPO) and its subsequent formation of malondialdehyde (MDA) can be inhibited by paraoxonase 1 (PON1), an HDL-associated antioxidant enzyme known to neutralize oxidized phosphatidylcholine moieties and prevent the accumulation of lipid hydroperoxides in lipoproteins. MDA has the ability to covalently crosslink HDL-associated apolipoprotein A1 (apoA1) and impede the positive effects of HDL on inflammation and cholesterol-effluxing properties (11).
Low-grade inflammation is characterized by a slight chronic elevation of inflammatory markers in the blood, but not to the same degree as acute inflammation. High-sensitivity C-reactive protein (hs-CRP), known as a classic indicator for low-grade inflammation, has undergone extensive research among diverse groups of inflammatory biomarkers and has drawn the greatest attention because of its potential as a reliable and affordable predictor for CVD (13–17).
Materials and methods
A hospital-based cross-sectional study was conducted at Dejen Primary Hospital, Debre Markos Referral Hospital, and Lumamie Primary Hospital from May 2022 to March 2023, East Gojjam, Ethiopia. In this study, 100 H. pylori-positive and 100 H. pylori-negative dyspeptic patients were selected during a health check-up in the outpatient department (OPD) by the purposive sampling technique as those who fulfilled inclusion criteria. All dyspeptic patients attending the three hospitals during the data collection period were included in the study, but subjects with liver disease, renal dysfunction, obesity, diabetes, cardiovascular disorders, malignancy, rheumatoid arthritis, and gouty arthritis who received the antihyperlipidemic drug and patients with a history of H. Pylori eradication therapy were excluded from the study. After we obtained informed consent from the study participants, 5 ml of blood was drawn, and the blood was allowed to stand for 30 min for complete clotting, centrifuged at 3,000 rpm for 15 min to extract serum, and stored at −70°C before the day of analysis.
Laboratory tests
Using a chromatographic immunoassay for the qualitative detection of H. Pylori antigen in the human fecal material [Joaquim Costa 18 2a planta. 08390 Montgat (Barcelona) SPAIN], H. Pylori was found using a linear H. Pylori Ag cassette. The Friedwald formula was used to determine the serum levels of low-density lipoprotein (LDL), while the Cobas C 501 chemical analyzer (Roche Diagnostic, USA) was used to assess the levels of total cholesterol, high-density lipoprotein (HDL), triglycerides (TG), and high sensitive C reactive protein (hs-CRP). At the Ethiopian Public Health Institute in Addis Ababa, Ethiopia, all biochemical analyses were completed. HDL (40–60 mg/dl), TG (<130 mg/dl), TC (<200 mg/dl), LDL (<130 mg/dl), and hs-CRP (<5 mg/L) were the reference ranges for adults.
Data processing and analysis
Version 26.0 of the SPSS software suite was used to analyze the data. The socio-demographic information is presented using basic descriptive statistics. However, the relationship between the variables was described using Pearson chi-square and Pearson correlation. The mean ± standard deviation is used to represent continuous variables having a normal distribution. To compare the variables, an independent student t-test was employed. A 95% confidence level p-value of less than 0.05 designates a statistically significant result.
Result
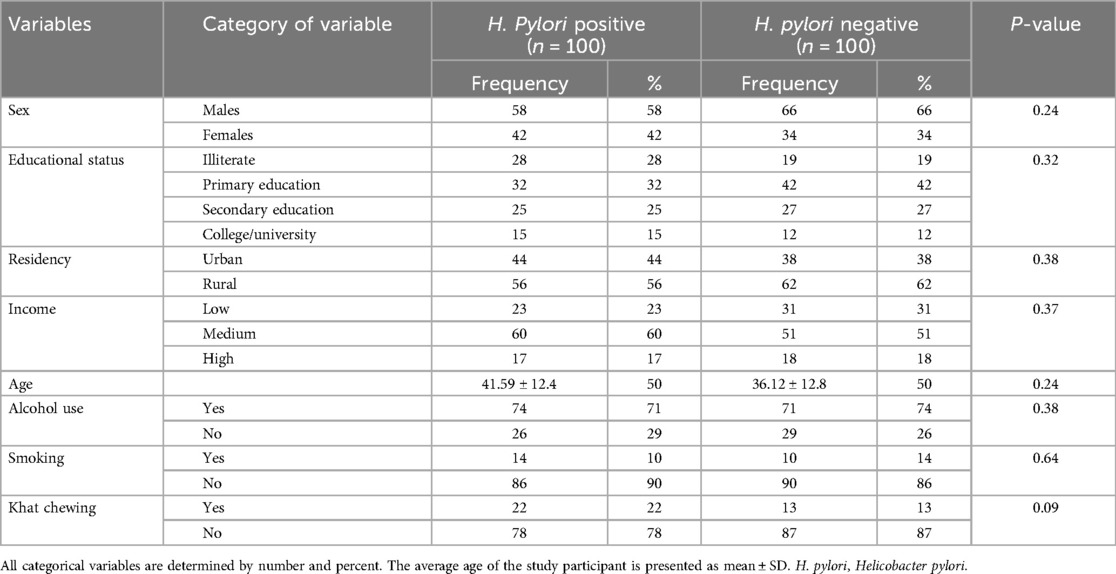
Socio-demographic data of dyspeptic patients: This study was conducted on 100 H. pylori-positive and 100 H. pylori- negative dyspeptic patients. The average age of H. pylori-positive dyspeptic patients was 41.59 ± 12.4 and 35.54 ± 12.59. Of the total dyspeptic patients included in this study, 76 participants were female and the remaining 126 participants were male. The majority of dyspeptic patients were alcohol users 74 participants in H. pylori positive and 71 participants in H. pylori-negative dyspeptic patients. The socio-demographic variables are summarized in Table 1.
The average serum hs-CRP levels and lipid profile among dyspeptic patients with and without H. pylori infection:
The average serum hs-CRP levels of H. pylori positive and negative dyspeptic patients were 8.09 ± 7.84 mg/L and 2.71 ± 2.51 mg/L respectively with a standard range of hs-CRP (<5 mg/L) in adults. The average serum HDL levels of H. pylori positive and negative dyspeptic patients were 35.35 ± 7.5 mg/dl and 44.64 ± 6.69 mg/dl respectively with a standard range of HDL (40–60 mg/dl) in adults.
An independent t-test was also conducted to compare the mean serum hs-CRP levels and lipid profiles (TG, TC, HDL, and LDL) between H. pylori-positive and negative dyspeptic patients. All serum lipid profiles and hs-CRP levels were significantly different between H. pylori-positive and H. pylori-negative dyspeptic patients with P-value <0.05. The summary is presented in Table 2.
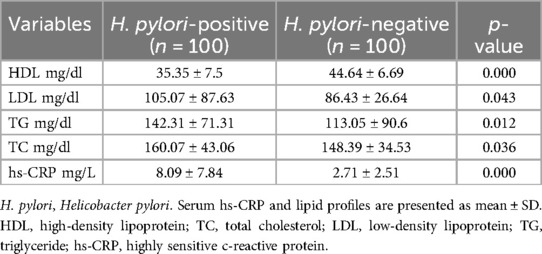
Table 2. The comparison of serum lipid profile and hs-CRP between H. pylori-positive and H. pylori-negative dyspeptic patients.
The correlation between serum hs-CRP levels and lipid profile among dyspeptic patients: Pearson correlation analysis was conducted to evaluate the association between hs-CRP and lipid profile (TG, HDL, LDL, and TC) among dyspeptic patients with and without H. pylori infection. In H. pylori-positive dyspeptic patients, serum TC levels were found positive, moderate in strength, and a statistically significant relationship with serum hs-CRP levels (r = 0.293, p < 0.05), and serum HDL levels were also found statistically significant but had a negative relationship with serum hs-CRP levels (r = −0.64, p < 0.01) (Figures 1, 2). This finding suggests that the higher hs-CRP levels in H. pylori-infected dyspeptic patients are more likely to have higher TC and lower HDL levels. However, in H. pylori-negative dyspeptic patients’ hs-CRP levels have an insignificant correlation with lipid profiles with P-value >0.05. The correlation between serum hs-CRP levels and lipid profile among dyspeptic patients is summarized in Table 3.
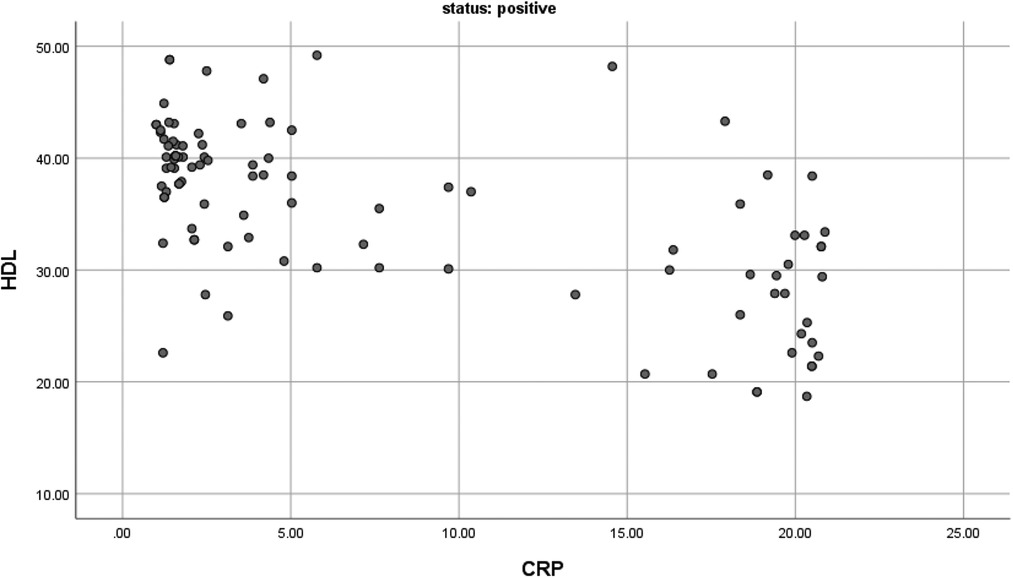
Figure 1. The correlation between HDL and CRP among H. Pylori positive dyspeptic patients (r = −0.64 and P-value <0.01 with n = 100).
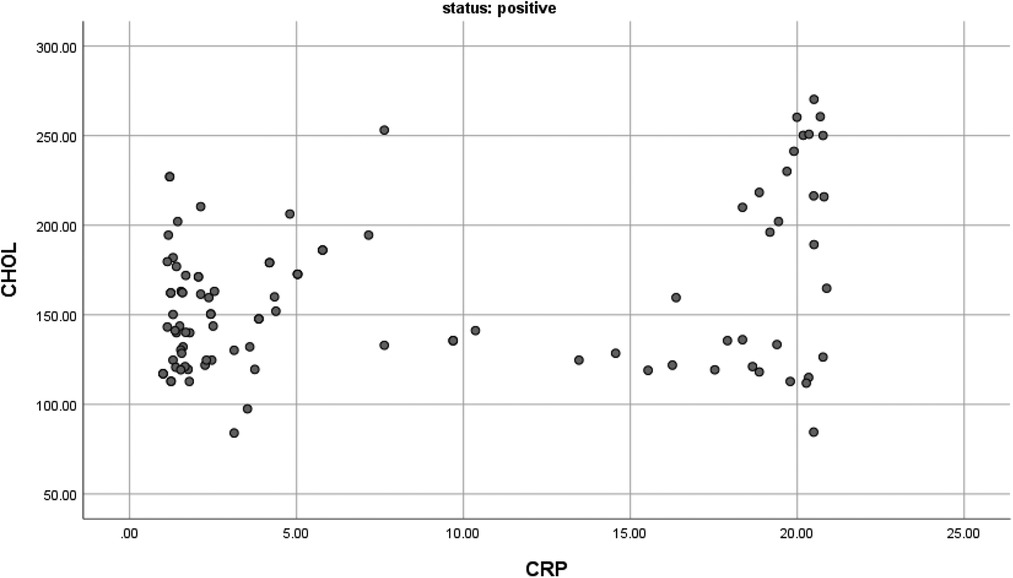
Figure 2. The correlation between CHOL and CRP among H. Pylori positive dyspeptic patients (r = 0.29 and P-value <0.01 with n = 100).
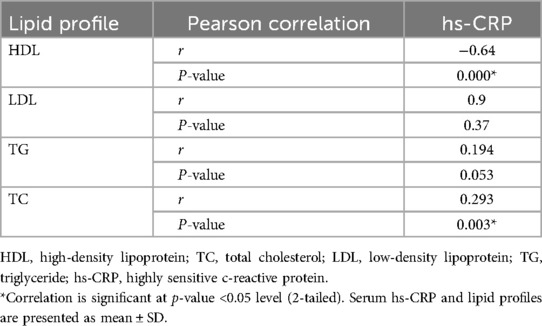
Table 3. The correlation between serum hs-CRP levels and lipid profile among H. pylori-positive dyspeptic patients.
Discussion
In our study, the average age of H. pylori-positive dyspeptic patients was 41.56 years, which was higher than the average age of H. pylori-negative dyspeptic patients (36.1 years). This was in line with a study conducted in Indonesia (18) and Jimma (19). The possible explanation for this age-related correlation between H. pylori infection and susceptibility to infectious diseases is the weakened immune system that accompanies aging. One reason the immune system is unable to effectively defend the body against a foreign body is that aging causes several immune system components to become dysregulated. In addition, a longer life expectancy raises the risk of developing an H. pylori infection because of increased exposure to the germs (20).
The majority of dyspeptic participants in our study—both those with and without H. pylori infection—were alcohol consumers. A study that was comparable to this one was published in Similar conclusions were drawn from research conducted in West Africa (21), and Hosanna (22). This could be because drinking alcohol increases the risk of developing an H. pylori infection and increases the prevalence of dyspepsia in a number of ways. First, alcohol causes inflammation by weakening the gastric mucosal membrane and increasing the mucosa's permeability. Interleukin-8 (IL-8), a cytokine released by neutrophils and macrophages during inflammation, binds with its receptor to promote further inflammation. Interleukin-8 is linked to HP0638, an external inflammatory protein virulence factor that makes H. pylori more adherence-prone and so promotes bacterial colonization (23).
The serum lipid profile (HDL, LDL, TC, and TG) was a statically difference between H. pylori positive and negative dyspeptic patients. In H. pylori-positive dyspeptic patients, the serum levels of LDL, TC, and TG were higher than in H. pylori-negative dyspeptic patients but for HDL the value is vice versa. A similar study was reported in the studies conducted in Jimma, Iraq, and China (19, 24, 25). This may result from changes in lipid metabolism after infection with H. pylori, which produces numerous virulence factors, including cytotoxic-associated genes (CagA) and vacuolating cytotoxic A (VacA). These virulence factors generate host factors such as interleukins, interferon-gamma, tumor necrosis factor, T and B lymphocytes, and phagocytic cells, as well as inflammation and cellular damage to host cells (26). In particular, TNF-α inhibits lipoprotein lipase, which causes lipids from tissues to be mobilized into the blood and raises serum levels of TG, TC, and LDL (11). Additionally, the lipid and protein composition of HDL are significantly altered by inflammation brought on by an H. pylori infection, which lowers the concentration of HDL (27).
In our investigation, we found that in H. pylori-positive dyspeptic patients, there was a substantial link between the lipid profile, notably HDL and TC, and the inflammatory markers, specifically hs-CRP levels. Analogous research and reviews demonstrating this correlation have been published in different countries (9, 11, 28, 29). This could be because a variety of lipid species, such as sterols, complex lipids, lipoproteins, fatty acids, and their metabolites have been shown to have immunomodulatory and pro- and anti-inflammatory qualities (12).
Due to its ability to transport bioactive lipids, anti-inflammatory and anti-oxidant proteins, and regulate immune cell activation by mediating cellular cholesterol efflux and reorganizing pathogen recognition receptors (PRRs) and related coreceptors in membranes lipid rafts, higher-density lipoproteins (HDL) in particular are known to possess a variety of immunomodulatory and anti-inflammatory properties (30).
Various research works have documented the significance of HDL in maintaining anti-inflammatory and cholesterol-accepting capacities. They discovered that pro-oxidative enzyme myeloperoxidase (MPO) can be inhibited by paraoxonase 1 (PON1), an HDL-associated antioxidant enzyme known to neutralize oxidized phosphatidylcholine moieties and prevent the accumulation of lipid hydroperoxides in lipoproteins. Besides, HDL inhibits the formation of malondialdehyde (MDA), which can covalently crosslink HDL-associated apolipoprotein A1 (apoA1) and impair the positive anti-inflammatory and cholesterol-effluxing properties of HDL (12, 31).
Conclusion
Different studies focus on the effect of H. pylori infection on lipid profile and inflammatory markers rather than the interaction between lipid profile and inflammation among dyspeptic patients (5, 26, 32, 33). However, our study focuses on the correlation between lipid profiles and inflammatory markers among dyspeptic patients. Based on our study result we can conclude that dyslipidemia and inflammation interact with each other, so provoking the potential risk of cardiovascular disorders.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Departmental Research and Ethics Review Committee, Department of Biochemistry, College of Health Sciences, Addis Ababa University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
GB: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Software, Supervision, Validation, Writing – original draft, Writing – review & editing. BW: Investigation, Software, Writing – original draft, Writing – review & editing. BA: Data curation, Formal Analysis, Methodology, Writing – original draft, Writing – review & editing. MJ: Conceptualization, Methodology, Software, Writing – original draft, Writing – review & editing. TB: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We express our gratitude to the Addis Ababa University Department of Medical Biochemistry, School of Medicine, and College of Health Sciences for their unwavering support in the research and provision of any required items. We also extend our sincere gratitude to the EPHI crew for their invaluable technical assistance with the serum laboratory analysis. It gives us great pleasure to express our gratitude to the staff members of Lumamie Primary Hospital, Dejen Primary Hospital, and Debre Markos Referral Hospital, who assisted us with sample collection at the study site.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Almeida AM, Martins LA, Cunha PL, Brasil VW, Felix LG, Passos MD. Prevalence of dyspeptic symptoms and heartburn of adults in Belo Horizonte, Brazil. Arq Gastroenterol. (2017) 54(1):46–50. doi: 10.1590/S0004-2803.2017v54n1-09
2. Koduru P, Irani M, Quigley EMM. Definition, pathogenesis, and management of that cursed dyspepsia. Clin Gastroenterol Hepatol. (2018) 16(4):467–79. doi: 10.1016/j.cgh.2017.09.002
3. Alebie G. Prevalence of Helicobacter pylori infection and associated factors among gastritis students in Jigjiga University, Jigjiga, Somali regional state of Ethiopia. J Bacteriol Mycol. (2016) 3(2):1–7. doi: 10.15406/jbmoa.2016.03.00060
4. Begolli-Stavileci G, Begolli G, Begolli L. Interleukin-6, tumor necrosis factor-α, and high-sensitivity C-reactive protein in diabetic patients with Helicobacter pylori in Kosovo. Maced J Med Sci. (2020) 8(B):172–5. doi: 10.3889/oamjms.2020.3199
5. Watanabe J, Kotani K. The effect of Helicobacter pylori eradication on C-reactive protein: results from a meta-analysis. Arch Med Sci. (2022) 18(4):958–64. doi: 10.5114/aoms/130288
6. Yang W, Cai X, Lin C, Lv F, Zhu X, Han X, et al. Reduction of C-reactive protein, low-density lipoprotein cholesterol, and its relationship with cardiovascular events of different lipid-lowering therapies: a systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore). (2022) 101(37):e30563. doi: 10.1097/MD.0000000000030563
7. Izhari MA, Al Mutawa OA, Mahzari A, Alotaibi EA, Almashary MA, Alshahrani JA, et al. Helicobacter pylori (H. pylori) infection-associated dyslipidemia in the Asir region of Saudi Arabia. Life (Basel). (2023) 13(11):2206. doi: 10.3390/life13112206
8. Glass CK, Olefsky JM. Inflammation and lipid signaling in the etiology of insulin resistance. Cell Metab. (2012) 15(5):635–45. doi: 10.1016/j.cmet.2012.04.001
9. Dias IHK, Milic I, Heiss C, Ademowo OS, Polidori MC, Devitt A, et al. Inflammation, lipid (per)oxidation, and redox regulation. Antioxid Redox Signal. (2020) 33(3):166–90. doi: 10.1089/ars.2020.8022
10. Sukhorukov VN, Orekhov AN. Molecular aspects of inflammation and lipid metabolism in health and disease: the role of the mitochondria. Int J Mol Sci. (2024) 25(12):6299. doi: 10.3390/ijms25126299
11. van Diepen JA, Berbee JF, Havekes LM, Rensen PC. Interactions between inflammation and lipid metabolism: relevance for efficacy of anti-inflammatory drugs in the treatment of atherosclerosis. Atherosclerosis. (2013) 228(2):306–15. doi: 10.1016/j.atherosclerosis.2013.02.028
12. Andersen CJ. Lipid metabolism in inflammation and immune function. Nutrients. (2022) 14(7):1414. doi: 10.3390/nu14071414
13. Bafei SEC, Zhao X, Chen C, Sun J, Zhuang Q, Lu X, et al. Interactive effect of increased high sensitive C-reactive protein and dyslipidemia on cardiovascular diseases: a 12-year prospective cohort study. Lipids Health Dis. (2023) 22(1):95. doi: 10.1186/s12944-023-01836-w
14. Liu C, Li C. C-reactive protein and cardiovascular diseases: a synthesis of studies based on different designs. Eur J Prev Cardiol. (2023) 30(15):1593–6. doi: 10.1093/eurjpc/zwad116
15. Fu Y, Wu Y, Liu E. C-reactive protein and cardiovascular disease: from animal studies to the clinic (review). Exp Ther Med. (2020) 20(2):1211–9. doi: 10.3892/etm.2020.8840
16. Shrivastava AK, Singh HV, Raizada A, Singh SK. C-reactive protein, inflammation and coronary heart disease. Egypt Heart J. (2015) 67(2):89–97. doi: 10.1016/j.ehj.2014.11.005
17. Amezcua-Castillo E, Gonzalez-Pacheco H, Saenz-San Martin A, Mendez-Ocampo P, Gutierrez-Moctezuma I, Masso F, et al. C-reactive protein: the quintessential marker of systemic inflammation in coronary artery disease-advancing toward precision medicine. Biomedicines. (2023) 11(9):2444. doi: 10.3390/biomedicines11092444
18. Winarta J, Waleleng BJ, Wenas NT, Fujiyanto , Miguna O, Rahardja M. Correlation between interleukin-17, high sensitivity C-reactive protein and pepsinogen in Helicobacter pylori infected gastritis. Gastroenterol Insights. (2024) 15(1):32–41. doi: 10.3390/gastroent15010003
19. Abdu A, Cheneke W, Adem M, Belete R, Getachew A. Dyslipidemia and associated factors among patients suspected to have Helicobacter pylori infection at Jimma university medical center, Jimma, Ethiopia. Int J Gen Med. (2020) 13:311–21. doi: 10.2147/IJGM.S243848
20. Castelo-Branco C, Soveral I. The immune system and aging: a review. Gynecol Endocrinol. (2014) 30(1):16–22. doi: 10.3109/09513590.2013.852531
21. Ofori EG, Adinortey CA, Bockarie AS, Kyei F, Tagoe EA, Adinortey MB. Helicobacter pylori infection, virulence genes’ distribution and accompanying clinical outcomes: the West Africa situation. Biomed Res Int. (2019) 2019:7312908. doi: 10.1155/2019/7312908
22. Kahase D, Haile K. Helicobacter pylori infection and predictors among dyspeptic adult patients in Southwest Ethiopia: cross-sectional study. Res Rep Trop Med. (2020) 11:141–7. doi: 10.2147/RRTM.S282557
23. Zhang L. Relationship between alcohol consumption and active Helicobacter pylori infection. Alcohol Alcohol. (2009) 45(1):89–94. doi: 10.1093/alcalc/agp068
24. Maountor. Lipid profile in patients with gastritis. World J Pharm Pharm Sci. (2016) 5(7):74–90. doi: 10.20959/wjpps20167-6122
25. AlFawaeir S, Zaid M, Awad A, Alabedallat B. Serum lipid profile in Helicobacter pylori infected patients. J Investig Biochem. (2013) 2(2):123–35. doi: 10.5455/jib.20130603084538
26. Temesgen GB, Menon M, Gizaw ST, Yimenu BW, Agidew MM. Evaluation of lipid profile and inflammatory marker in patients with gastric Helicobacter pylori infection, Ethiopia. Int J Gen Med. (2022) 15:271–8. doi: 10.2147/IJGM.S345649
27. He C, Yang Z, Lu NH. Helicobacter pylori-an infectious risk factor for atherosclerosis? J Atheroscler Thromb. (2014) 21(12):1229–42. doi: 10.5551/jat.25775
28. Rathore V, Singh N, Rastogi P, Mahat RK, Mishra MK, Shrivastava R. Lipid profile and its correlation with C-reactive protein in patients of acute myocardial infarction. Int J Res Med Sci. (2017) 5(5):2182–6. doi: 10.18203/2320-6012.ijrms20171866
29. Bale BF, Doneen AL, Leimgruber PP, Vigerust DJ. The critical issue linking lipids and inflammation: clinical utility of stopping oxidative stress. Front Cardiovasc Med. (2022) 9:1042729. doi: 10.3389/fcvm.2022.1042729
30. Andersen CJ. Impact of dietary cholesterol on the pathophysiology of infectious and autoimmune disease. Nutrients. (2018) 10(6):764. doi: 10.3390/nu10060764
31. Huang J, Yancey PG, Tao H, Borja MS, Smith LE, Kon V, et al. Reactive dicarbonyl scavenging effectively reduces MPO-mediated oxidation of HDL and restores PON1 activity. Nutrients. (2020) 12(7):1937. doi: 10.3390/nu12071937
32. Watanabe J, Hamasaki M, Kotani K. The effect of Helicobacter pylori eradication on lipid levels: a meta-analysis. J Clin Med. (2021) 10(5):904. doi: 10.3390/jcm10050904
Keywords: Helicobacter pylori, dyspepsia, lipid profile, high sensitive C reactive, inflammation, cardiovascular diseases
Citation: Baye G, Wondmneh B, Ashenef B, Jemal M and Baylie T (2024) Serum high sensitive C-reactive protein level and its correlation with lipid profile among dyspeptic patients with or without Helicobacter pylori infection in East Gojjam zone, Ethiopia. Front. Cardiovasc. Med. 11:1470993. doi: 10.3389/fcvm.2024.1470993
Received: 26 July 2024; Accepted: 16 September 2024;
Published: 26 September 2024.
Edited by:
Hongxue Shi, Columbia University, United StatesReviewed by:
Hong Yu, The University of Texas Health Science Center at San Antonio, United StatesLi Li, University of California, San Francisco, United States
Yujie Ye, Wistar Institute, United States
Copyright: © 2024 Baye, Wondmneh, Ashenef, Jemal and Baylie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gelagey Baye, Z2VsYWdheWJheWVAZ21haWwuY29t
 Gelagey Baye
Gelagey Baye Bayu Wondmneh
Bayu Wondmneh Baye Ashenef
Baye Ashenef Mohammed Jemal
Mohammed Jemal Temesgen Baylie
Temesgen Baylie