- 1Department of Diagnostic Ultrasound & Echocardiography, Sir Run Run Shaw Hospital, Zhejiang University College of Medicine, Technical Guidance Center for Fetal Echocardiography of Zhejiang Province and Sir Run Run Shaw Institute of Clinical Medicine of Zhejiang University, Hangzhou, China
- 2Department of ECG, Sir Run Run Shaw Hospital, Sir Run Run Shaw Institute of Clinical Medicine of Zhejiang University, Hangzhou, China
- 3Department of Radiology, Sir Run Run Shaw Hospital, Sir Run Run Shaw Institute of Clinical Medicine of Zhejiang University, Hangzhou, China
Intracardiac bronchogenic cysts (IBCs) are very rare. To date, only a few cases of IBC have been reported in the literature. We report a case of a bronchogenic cyst that arose from the interatrial septum in a 42-year-old man who presented with symptoms of palpitation. A unilocular cystic lesion of the heart was found initially on echocardiography and subsequently on computed tomography and magnetic resonance imaging. The diagnosis was further confirmed by histopathology after surgical resection. Multimodality imaging played a crucial role in the diagnosis and treatment of such rare lesions.
Background
A bronchogenic cyst is considered a rare congenital lesion that originates from the ventral foregut during embryogenesis (1, 2). It can usually be found in the mediastinum or lung (3). Intracardiac bronchogenic cysts (IBCs) are very rare, accounting for only 1.3% of all primary cardiac and pericardial tumors. The majority of bronchogenic cysts are either asymptomatic and discovered incidentally through imaging or they present with symptoms caused by the compression of surrounding structures, such as dyspnea, atrioventricular block, or superior vena cava syndrome. This case was assessed using multimodal imaging and underwent successful resection.
Case presentation
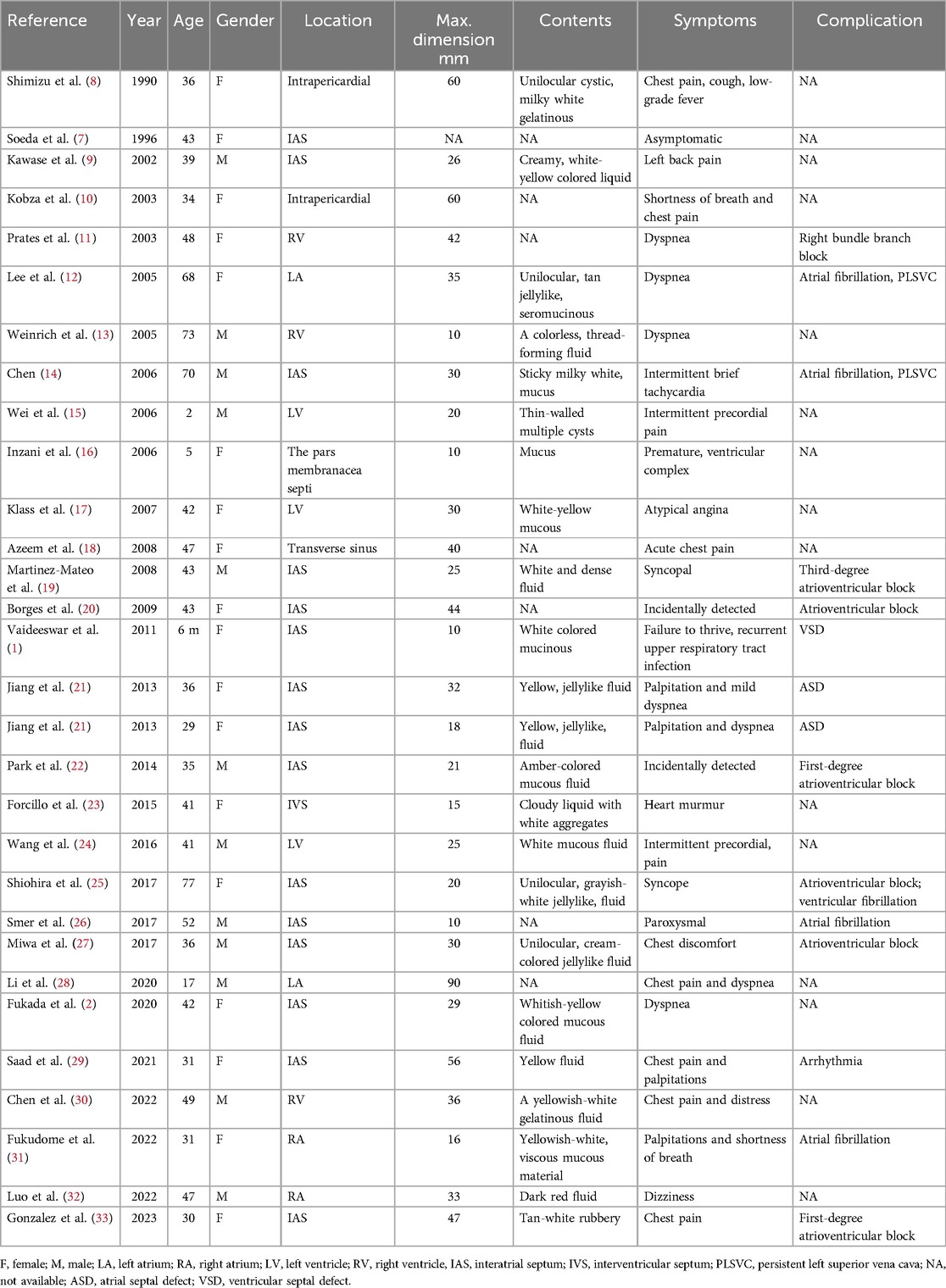
A 47-year-old man presented to a local clinic with complaints of palpitation. Physical examination and chest radiography were unremarkable; however, a 12-lead electrocardiogram (ECG) showed a third-degree atrioventricular block (Figure 1A). Transthoracic echocardiography (TTE) revealed normal ventricular and valve function; however, a well-demarcated hypoechoic ovoid mass measuring 29.9 mm × 25.6 mm was identified in the interatrial septum (IAS) (Figure 2A). In addition, transesophageal echocardiography (TEE) revealed a large, homogeneous, hypoechoic mass in the near field on mid-esophageal views (Figure 2B). The mass had no stalk, and color Doppler echocardiography revealed no color flow signal within the mass. Myocardial contrast echocardiography (MCE) revealed a hypoechogenic mass in the atrial septum, with clear and regular boundaries and no obvious contrast agent perfusion (Figure 2C). Three-dimensional TEE demonstrated the relationship between the mass and surrounding structures (Figure 2D). Subsequent computed tomography (CT) (SOMATOM Definition Flash) coronary angiography revealed no obvious stenosis in the left main coronary artery, anterior descending branch, circumflex branch, or right coronary arteries. A low-density ovoid mass was found in the atrial septum, with well-defined borders, no significant enhancement, and an absence of feeding vessels from the coronary arteries (Figure 3A). Magnetic resonance imaging (MRI) (SIGNA EXCITE HD 1.5 T) identified a mass in the atrioventricular septal region (Figure 3B). Neither fat deposition nor late gadolinium enhancement were observed in the tumor. Based on multimodality imaging, the mass was most likely consistent with a cyst.
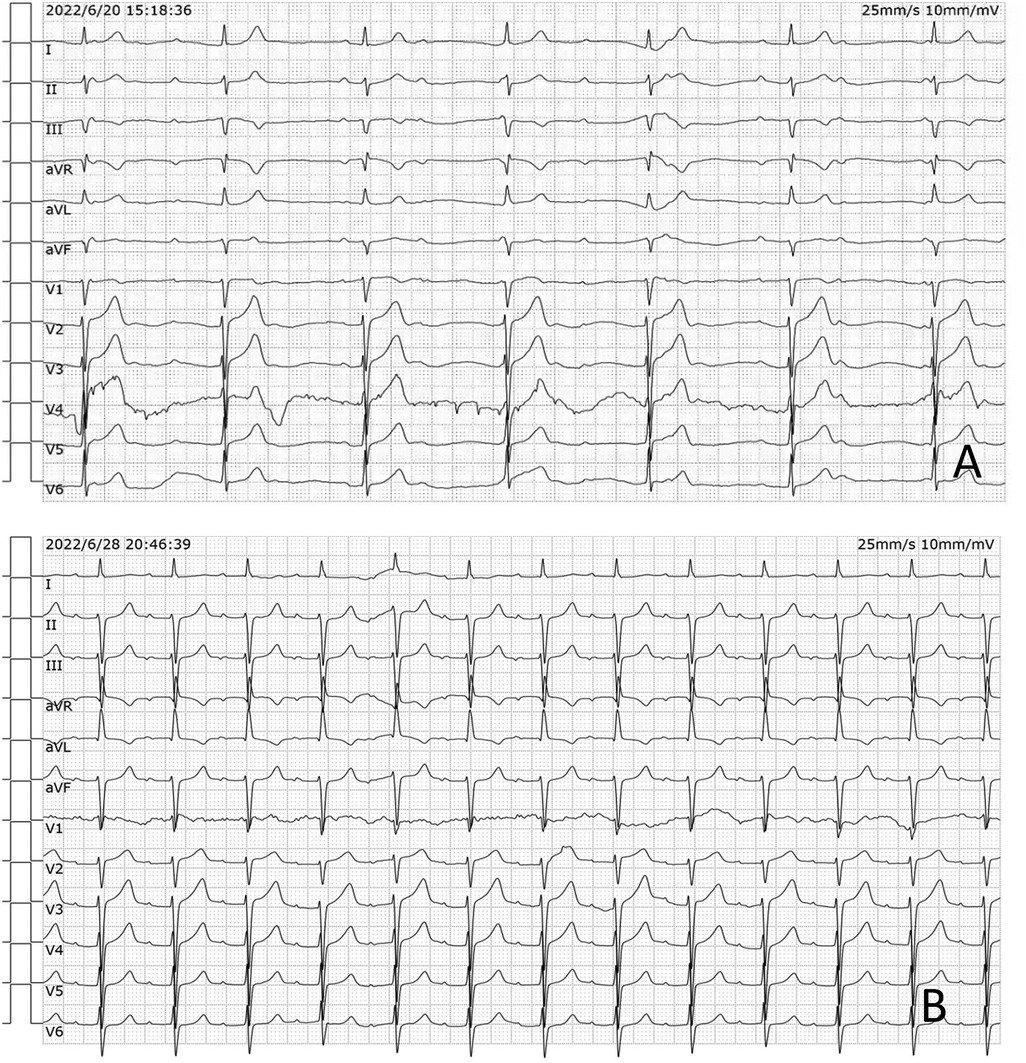
Figure 1. (A) The preoperative 12-lead ECG showed a third-degree atrioventricular block. (B) The postoperative ECG showed a first-degree atrioventricular block.
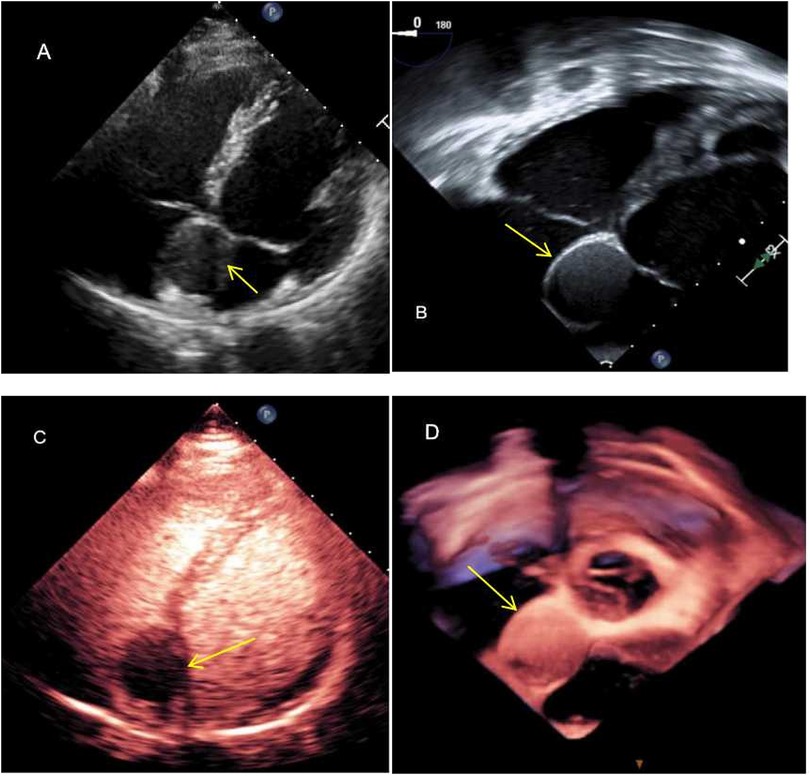
Figure 2. Echocardiography showing the well-defined ovoid interatrial lesion (arrow). (A) Transthoracic echocardiography showing a well-demarcated hypoechoic ovoid mass embedded in the interatrial septum in the apical four-chamber view; (B) TEE showing a homogeneous, isoechoic mass at the interatrial septum—the mass is well-defined and has a smooth surface; (C) the mass was not enhanced by the use of a contrast agent; and (D) three-dimensional TEE illustrating the relationship between the mass and surrounding structures.
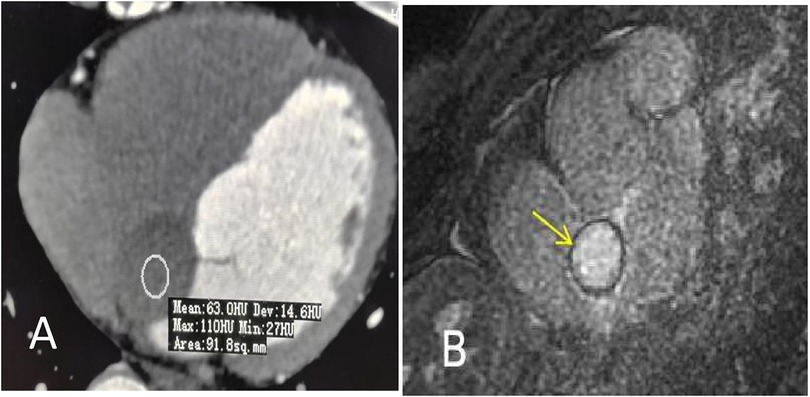
Figure 3. (A) Contrast-enhanced CT shows a low-intensity ovoid nodule without obvious enhancement at the interatrial septum (arrow). The mean attenuation value was approximately 63 Hu. (B) Cardiac MRI shows a round mass in the interatrial septum measuring 30 mm × 20 mm (arrow). Neither fat deposition nor late gadolinium enhancement were identified in the tumor.
Given the above information, surgical resection of the cystic tumor was planned via median sternotomy. The position of the heart and great vessels was normal. A round mass measuring approximately 40 mm × 30 mm, with a smooth surface, was identified in the middle of the atrial septum and was completely resected. The mass was a cyst containing muddy, milky mucous liquid. Histology revealed that the cyst wall was composed of stratified ciliated columnar epithelium, with smooth muscle cells also observed within the wall. The final diagnosis, based on histopathologic examination, was a bronchogenic cyst (Figure 4). The patient's recovery was uneventful. The postoperative ECG showed a first-degree atrioventricular block (Figure 1B). The patient was asymptomatic without recurrence during the 2 years of follow-up.
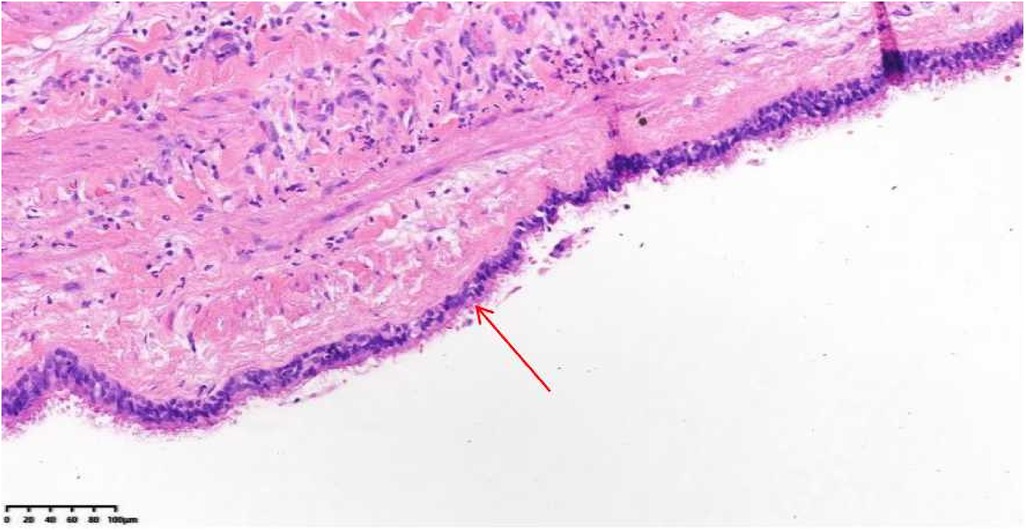
Figure 4. Histology shows the surface of the cystic lesion lined by pseudostratified ciliated columnar epithelium (arrow), smooth muscle cells within the fibrous tissue wall of the cyst, and acute inflammatory cells.
Discussion
The occurrence of cardiac masses is rare. They are mostly diagnosed as an incidental finding during various imaging examinations. Echocardiography is typically the first-line diagnostic technique used to evaluate patients with suspected cardiac tumors as it is widely available and free of ionizing radiation (4). However, echocardiography is limited owing to its dependence on the echogenic window and its limited ability for tissue characterization. MRI has been proven to be superior to echocardiography owing to its excellent soft tissue contrast, high temporal and spatial resolution, and lack of ionizing radiation (5). Thus, the diagnostic and therapeutic planning for patients with suspected cardiac tumors is primarily dependent on multimodal imaging tools.
When evaluating a cardiac mass, several differential diagnoses need to be considered, such as cardiac thrombus, cardiac tumor, and normal anatomical variants. Cardiac thrombi are more commonly seen in patients with a reduced left ventricular (LV) ejection fraction, and their presence is often associated with a lack of first pass prussian and late gadolinium enhancement (LGE). Cardiac tumors are rare and are typically classified as benign tumors or malignant tumors. Malignant tumors tend to be larger, have a predilection for the right heart, are more often infiltrative, and are more likely to be isointense on T1 black-blood weighted images. They also exhibit higher proportions of LGE (6). Three-quarters of cardiac tumors are benign. The most common types of benign tumors are myxomas (42%), papillary fibroelastomas (23%), and cysts (22%). Myxomas present themselves as mostly mobile masses attached to the left atrial side of the IAS, are heterogeneous, perfused, and show LGE. Papillary fibroelastoma, which rarely occurs, is typically pedunculated and frequently involves the cardiac valves. However, none of these show any enhancement after gadolinium injection. For intracardiac cysts, echinococcal cysts, congenital blood cysts, and bronchogenic cysts should be included in the list of possible diagnoses. The diagnosis of echinococcal cysts requires a history of travel to endemic areas or a medical history of a visceral hydatid cyst. Echinococcal cysts frequently involve the left ventricular myocardial wall and interventricular septum. Specific imaging features include calcification of the cyst wall, the presence of daughter cysts, and membrane detachment. Congenital blood cysts, which are most commonly observed in infants, are typically located along the lines of closure of the valvular endocardium.
IBCs were first described by Jöel in 1890 during an autopsy. However, the first surgical removal of an interatrial bronchogenic cyst was reported by Soeda et al. a century later, in 1996 (7). To the best of our knowledge, approximately 30 cases of intrapericardial bronchogenic cysts have been published in the literature. We reviewed the relevant studies and summarized our findings in Table 1.
The mean age of onset of bronchogenic cysts is 39, ranging from newborns to 77 years, with a female-to-male ratio of 2:1. The cysts are usually described as round or oval-shaped, unilocular masses that are either milky white or yellowish in color. The mean maximum size is 31 mm (range 10–90 mm). In general, the cysts grow slowly in the absence of complications (34). The most frequent location of the cysts is the IAS, accounting for more than half of the reported cases (1). Although the majority may be asymptomatic, many may present with syncope, dyspnea, chest pain, or palpitations (35, 36), as well as symptoms related to compression of surrounding structures (10–12). Associated congenital defects reported include atrial septal defects, ventricular septal defects, and persistent left superior vena cava.
Our patient, who presented with a third-degree atrioventricular block, was initially assessed using echocardiography and this was later confirmed through multimodality imaging. Due to the limitations associated with cardiac mass biopsy in clinical practice, diagnosis, and treatment of cardiac masses remain extremely challenging. The clinical diagnosis mainly relies on the comprehensive evaluation of echocardiography, CT, MRI, and other imaging techniques (36). Compared with cardiac CT and MRI, echocardiography can qualitatively assess and localize the cyst, and analyze its impact on hemodynamics, which is important for diagnosis and treatment planning. In this case, TTE showed a well-demarcated hypoechoic ovoid mass on the atrial septum, and TEE showed a well-defined mass with a regular shape, suggesting the possibility of a benign mass. MCE showed cystic wall-like enhancement around the mass, without internal perfusion, suggesting the possibility of a cystic lesion, and CT imaging also showed a well-defined non-enhancing spheroid or ovoid thin-walled lesion. MRI confirmed the absence of enhancement and intralesional fat, suggesting that the mass occupying the atrial septum was more likely to be benign. The characteristics of the mass seen on multimodality imaging were indicative of a benign atrial septal cystic mass. In addition, the patient’s atrioventricular block was due to the mass’s impact on myocardial electrophysiology, providing strong evidence for clinical decision-making. This was also confirmed after surgery.
Here, we presented a rare case of new-onset third-degree atrioventricular block that was initially found using echocardiography and subsequently confirmed by TEE, MCE, CT, and MRI. We also reviewed the imaging findings and highlighted the characteristic features of IBCs on multimodal imaging that are essential for appropriate diagnosis and management.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
MM: Writing – original draft. ZY: Data curation, Investigation, Writing – review & editing. CR: Supervision, Validation, Writing – review & editing. ZQ: Data curation, Visualization, Writing – original draft. ZB: Funding acquisition, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by funds from the National Key Research and Development Program of China (2023YFC2705700) and the General Cooperative Research Program of the Sci-Tech Academy of Zhejiang University (ZJU Cooperation No. 2021-KYY-518053-0055).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Vaideeswar P, Agnihotri MA, Patwardhan AM. Intracardiac bronchogenic cyst. J Card Surg. (2011) 26:266–8. doi: 10.1111/j.1540-8191.2011.01206.x
2. Fukada Y, Endo Y, Nakanowatari H, Kitagawa A, Tsuboi E, Irie Y. Bronchogenic cyst of the interatrial septum. Fukushima J Med Sci. (2020) 66:41–3. doi: 10.5387/fms.2019-29
3. Ogunkunle OO, Animashaun D. Intracardiac bronchogenic cyst in a 2-year-old Nigerian boy. BMJ Case Rep. (2012):bcr0920114785. doi: 10.1136/bcr.09.2011.4785
4. Bhattacharyya S, Khattar RS, Gujral DM, Senior R. Cardiac tumours: the role of cardiovascular imaging. Expert Rev Cardiovasc Ther. (2014) 12:37–43. doi: 10.1586/14779072.2014.872031
5. Shenoy C, Grizzard JD, Shah DJ, Kassi M, Reardon MJ, Zagurovskaya M, et al. Cardiovascular magnetic resonance imaging in suspected cardiac tumour: a multicentre outcomes study. Eur Heart J. (2021) 43(1):71–80. doi: 10.1093/eurheartj/ehab635
6. Giusca S, Mereles D, Ochs A, Buss S, André F, Seitz S, et al. Incremental value of cardiac magnetic resonance for the evaluation of cardiac tumors in adults: experience of a high volume tertiary cardiology centre. Int J Cardiovasc Imaging. (2017) 33(6):879–88. doi: 10.1007/s10554-017-1065-7
7. Soeda T, Matsuda M, Fujioka Y, Doui K, Maruhashi H. A case report of huge bronchogenic cyst originated in the atrial septum. Nippon Kyobu Geka Gakkai Zasshi. (1996) 44:1781–6.8911056
8. Shimizu M, Takeda R, Mifune J, Tanaka T. Echocardiographic features of intrapericardial bronchogenic cyst. Cardiology. (1990) 77:322–6. doi: 10.1159/000174616
9. Kawase Y, Takahashi M, Takemura H, Tomita S, Watanabe G. Surgical treatment of a bronchogenic cyst in the interatrial septum. Ann Thorac Surgery. (2002) 74:1695–7. doi: 10.1016/s0003-4975(02)03863-8
10. Kobza R, Oechslin E, Jenni R. An intrapericardial bronchogenic cyst. Interact Cardiovasc Thorac Surg. (2003) 2:279–80. doi: 10.1016/S1569-9293(03)00044-6
11. Prates PR, Lovato L, Homsi-Neto A, Barra M, Sant'Anna JR, Kalil RA, et al. Right ventricular bronchogenic cyst. Texas Heart Inst J. (2003) 30:71–3.
12. Lee T, Tsai IC, Tsai WL, Jan YJ, Lee CH. Bronchogenic cyst in the left atrium combined with persistent left superior vena cava: the first case in the literature. AJR. (2005) 185:116–9. doi: 10.2214/ajr.185.1.01850116
13. Weinrich M, Lausberg HF, Pahl S, Schäfers HJ. A bronchogenic cyst of the right ventricular endocardium. Ann Thorac Surg. (2005) 79:e13–4. doi: 10.1016/j.athoracsur.2004.09.032
14. Chen CC. Bronchogenic cyst in the interatrial septum with a single persistent left superior vena cava. J Chin Med Assoc. (2006) 69:89–91. doi: 10.1016/S1726-4901(09)70120-0
15. Wei X, Omo A, Pan TC, Li J, Liu LG, Hu M. Left ventricular bronchogenic cyst. Ann Thorac Surg. (2006) 81:e13–5. doi: 10.1016/j.athoracsur.2005.12.038
16. Inzani F, Recusani F, Agozzino M, Cavallero A, De Siena PM, D'Armini A, et al. Bronchogenic cyst: unexpected finding in a large aneurysm of the pars membranacea septi. J Thorac Cardiovasc Surg. (2006) 132(4):972–4. doi: 10.1016/j.jtcvs.2006.06.022
17. Klass O, Hoffmann MH, Ludwig B, Leithäuser F, Hannekum A. Images in cardiovascular medicine. Left ventricular bronchogenic cyst. Circulation. (2007) 116(16):e385–7. doi: 10.1161/CIRCULATIONAHA.107.713420
18. Azeem F, Rathwell C, Awad WI. A near fatal presentation of a bronchogenic cyst compressing the left main coronary artery. J Thorac Cardiovasc Surg. (2008) 135:1395–6. doi: 10.1016/j.jtcvs.2007.09.082
19. Martínez-Mateo V, Arias MA, Juárez-Tosina R, Rodríguez-Padial L. Permanent third- degree atrioventricular block as clinical presentation of an intracardiac bronchogenic cyst. Europace. (2008) 10:638–40. doi: 10.1093/europace/eun056
20. Borges AC, Knebel F, Lembcke A, Panda A, Komoda T, Hiemann NE, et al. Bronchogenic cyst of the in- teratrial septum presenting as atrioventricular block. Ann Thorac Surg. (2009) 87:1920–3. doi: 10.1016/j.athoracsur.2008.10.051
21. Jiang H, Wang H, Wu H, Li X. Bronchogenic cyst of the interatrial septum. J Cardiothorac Surg. (2013) 8:171–4. doi: 10.1186/1749-8090-8-171
22. Park J, Cho G-Y, Park K-H, Oh I-Y. Intracardiac bronchogenic cyst. Circulation. (2014) 130:1107–9. doi: 10.1161/CIRCULATIONAHA.114.010992
23. Forcillo J, Dion D, Sauvageot C, Jeanmart H. Intraventricular bronchogenic cyst: a rare congenital anomaly. Ann Thorac Surg. (2015) 100:1101–3. doi: 10.1016/j.athoracsur.2014.11.059
24. Wang J, Zhu Q, Liang B, Shi H, Han P, Kong X. Left ventricular bronchogenic cyst. Ann Thorac Surg. (2016) 101(2):744–6. doi: 10.1016/j.athoracsur.2015.03.083
25. Shiohira S, Sasaki T, Maeda S, Kawabata M, Goya M, Hirao K. Bronchogenic cyst of the atrioventricular septum presenting with ventricular fibrillation. HeartRhythm Case Rep. (2017) 3:389–91. doi: 10.1016/j.hrcr.2017.05.005
26. Smer A, Alla VM, Abuissa H. A 50-year-old man with incidental cardiac mass. Heart. (2017) 103(3):189. doi: 10.1136/heartjnl-2016-310337
27. Miwa E, Tani T, Okada Y, Furukawa Y. A rare cardiac tumor: bronchogenic cyst of interatrial septum. Echocardiography. (2017) 34:474–5. doi: 10.1111/echo.13445
28. Li Z, Xiang D, Gao L, Tan J, Zeng X. Resection of a giant bronchogenic cyst in the left atrium. Can J Cardiol. (2020) 36:967.e13–15. doi: 10.1016/j.cjca.2020.02.078
29. Saad E, Singh P, Iskandar M. Atypical chest pain in a young woman with an interatrial bronchogenic cyst. BMJ Case Rep. (2021) 14:241736. doi: 10.1136/bcr-2021-241736
30. Chen Y, Zhu Y, Xu Y, Zhou X, Zhu X. Multimodality imaging toward diagnosis of an intraventricular bronchogenic cyst presenting with complex components: a case report with literature review. J Radiol Case Rep. (2022) 16(2):1–11. doi: 10.3941/jrcr.v16i2.4109
31. Fukudome Y, Hieda M, Masui S, Yokoyama T, Futami S, Moriyama S, et al. Case report: bronchogenic cyst in the right atrium of a young woman. Front Cardiovasc Med. (2022) 9:915876. doi: 10.3389/fcvm.2022.915876
32. Luo Y, Chen D, Yang X. Bronchogenic cyst in the right atrium: a case report. Asian J Surg. (2022) 45:1162–64. doi: 10.1016/j.asjsur.2021.12.072
33. Gonzalez J, Batlle JC, Maroules C, Cury RC, Peña CS, Ma C, et al. Multimodality imaging of a rare intracardiac bronchogenic cyst. Radiol Case Rep. (2023) 19(3):1035–9. doi: 10.1016/j.radcr.2023.11.072
34. Maurin S, Hery G, Bourliere B, Potier A, Guys JM, Lagausie PD. Bronchogenic cyst: clinical course from antenatal diagnosis to postnatal thoracoscopic resection. J Minim Access Surg. (2013) 9:25–8. doi: 10.4103/0972-9941.107132
35. Aktoğu S, Yuncu G, Halilçolar H, Ermete S, Buduneli T. Bronchogenic cysts: clinicopathological presentation and treatment. Eur Respir J. (1996) 9:2017–21. doi: 10.1183/09031936.96.09102017
Keywords: congenital anomaly, bronchogenic cyst, interatrial septum, diagnosis, therapy
Citation: Mingming M, Yana Z, Ran C, Qingqing Z and Bowen Z (2024) Case Report: Multimodality imaging of a bronchogenic cyst in the interatrial septum. Front. Cardiovasc. Med. 11:1466016. doi: 10.3389/fcvm.2024.1466016
Received: 17 July 2024; Accepted: 18 September 2024;
Published: 9 October 2024.
Edited by:
Grigorios Korosoglou, GRN Klinik Weinheim, GermanyReviewed by:
Sorin Giusca, GRN Klinik Weinheim, GermanyAlexandros Kallifatidis, St. Luke’s Hospital, Greece
Copyright: © 2024 Mingming, Yana, Ran, Qingqing and Bowen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhao Bowen, emJ3Y2pwQHpqdS5lZHUuY24=
 Ma Mingming
Ma Mingming Zhao Yana2
Zhao Yana2 Zhu Qingqing
Zhu Qingqing