- 1Department of Public Health and Institute of Public Health, Chung Shan Medical University, Taichung, Taiwan
- 2Division of Cardiovascular Surgery, Department of Surgery, E-Da Cancer Hospital, I-Shou University, Kaohsiung, Taiwan
- 3Department of Medical Imaging, Chung Shan Medical University Hospital, Taichung, Taiwan
- 4Institute of Medicine, Chung Shan Medical University, Taichung, Taiwan
Background: Varicose veins are a common issue for employees in jobs that require prolonged standing compared with all other employees. However, its relationship with presentations of traditional Chinese medicine constitution is unknown. This study aimed to investigate their association.
Material and methods: Data in the study were obtained from questionnaires of patients in Taiwan Biobank, enrolled from 2008 to 2020. The responses to the statement “I can see distorted blood vessels on my four limbs (varicose veins).” were categorized into none, mild, moderate, severe. and more severe, and the same scale was also used to classify breathing difficulties and hypotension.
Results: A total of 11,293 participants were enrolled in the study. The prevalence of women was higher in the studied group compared with the control. Patients complained of breathing difficulties with moderate (30.49%) and severe discomfort (12.44%) in the diseased group. Regarding hypotension, 28.81% and 9.82% of the patients presented with moderate and severe hypotension, respectively. The cofactor odds ratio was 1.775 for severe breathing difficulty/moderate hypotension and 2.235 for severe breathing difficulty/severe hypotension, with statistical significance. The combined impact of breathing difficulties and hypotension increased with severity.
Conclusions: Varicose veins had a higher association with breathing difficulties and hypotension as the severity of the condition worsened. The combined impact of breathing difficulties and hypotension increased as the disease progressed. Therefore, self-reported assessments can be a useful tool for evaluating patients with asymptomatic varicose veins before the development of “heart-failure-like symptoms” to reduce the risk of underdiagnosis.
1 Introduction
Varicose veins (VVs) are a common and important issue, with an incidence of 29.5%–39.0% in women and 10.4%–23.0% in men (1). The CEAP (Clinical-Etiology-Anatomy-Pathophysiology) clinical score is the most widely used tool to determine the severity of chronic venous insufficiency (CVI), with the range from C0 (absolutely no venous disease) to C6 (an open and active venous leg ulcer), and VVs are classified as C2 severity (2). Recent research indicated that females and people residing in urban areas were more susceptible to CVI, with the predominant age group being middle-aged adults, between 41 and 65 years (3). Moreover, various aspects related were associated with varicose veins, including marital status, weight and body mass index, also educational impacts. People who were married, had a normal body mass index, and possessed a moderate or higher educational background, were more likely to develop CVI (3). In addition, patient perception and beliefs about varicose veins, particularly among those who have inherited the condition, contributed to the progress of CVIs due to multifaceted factors (3). VVs, classified as C2 by the CEAP scale, are the most common issue of venous disease, followed by CVI, affecting more than 25 million people in the United States (4, 5). As a chronic venous disease, VVs occur in superficial veins with a diameter greater than 3 mm, and the vast major pathetic vessels are caused by damage to valves, leading to blood stagnation in the low-pressure vascular network vessels and resulting in varicose veins (6).
The constitution of traditional Chinese medicine is one of the oldest medical theories in traditional Chinese medicine (7). There is harmony and equilibrium within the human body (8, 9), and some fundamental substances, such as blood, body fluids, and spirit and vital organs, including the liver, spleen, lung, heart, and kidney, are closely associated and interacted with each other to form the body's constitution (7). Impaired blood circulation and dysregulation of fundamental substances lead to several physiological and psychological disorders (7). Various types of the constitution have been reported, such as physical muscular weakness, dizziness, weak voice, easily feeling tired, short breath, and sweating spontaneously (10, 11). The unspecified constitution symptoms have been noted to resemble the presentations of heart failure (12). However, the association between VVs and the constitution of traditional Chinese medicine symptoms, which could be “heart-failure-like,” remain unclear. This study aimed to investigate the relationship between VVs and the constitution of traditional Chinese medicine symptoms.
2 Materials and methods
2.1 Data resource
The data for this study were obtained from Taiwan Biobank. Taiwan Biobank is a population-based database that recruited volunteers from Taiwan aged 30–70 without a cancer history. The enrollment was from 2008 to 2020. All volunteers were required to sign an informed consent before enrollment. The information from physical examination, bioinformatics, and a questionnaire were collected during the recruitment procedure. Participants were enrolled after excluding the incomplete and missing data.
2.2 Definition of variables
In the Taiwan Biobank, VVs were assessed using a questionnaire. The responses were classified into five categories, as none, mild, moderate, severe, and more severe. In response to the statement “I can see distorted blood vessels on my four limbs (varicose veins),” we categorized the answer into no varicose veins (none) and with varicose veins (mild, moderate, severe, and more severe). Similarly, breathing difficulties and hypotension were categorized as no (none), moderate (mild), and severe (moderate, severe, and more severe). Moreover, the statement for breathing difficulties was, “I feel hard to breathe, need to breathe deeply” and hypotension was “I will feel the darkness in front of my eyes when I stand up suddenly.” Covariates in the models included gender (Women/Men), age (Age < 50/50 ≤ Age ≤ 70), vegetarian diet (No/Yes), cigarette smoking (No/Yes), alcohol intake (No/Yes), exercise (No/Yes), body mass index (BMI) (Normal weight/Underweight/Overweight Obesity), education level (Elementary and below/Junior and senior school/University and above), job type (non-prolonged standing/Prolonged standing), hypertension (No/Yes), and diabetes (No/Yes).
2.3 Ethics statement
This study was approved by the Institutional Review Board of Chung Shan Medical University Hospital (CSMUH No: CS1-20009). Taiwan Biobank participants provided written informed consent during enrollment.
2.4 Data analysis
The data was analyzed using SAS version 9.4 (SAS Institute, Cary, NC, USA). Patients were divided into two groups, with one cohort of patients without varicose veins (control cohort) and the other one of patients with varicose veins (diseased cohort). The logistic regression models were used to determine the relation of breathing difficulty, hypotension, and varicose veins. The results were presented as odds ratio (OR) and 95% confidence interval (95% CI). For demographic characteristics analysis, Student's t-test was used to examine the difference between varicose veins status and categorical variables (gender, age, breathing difficulty, hypotension, vegetarian diet, cigarette smoking, alcohol intake, exercise, BMI, job type, hypertension, and diabetes). The results were presented as numbers (n) and percentages (%). The significance level used for the analysis was 0.05.
3 Results
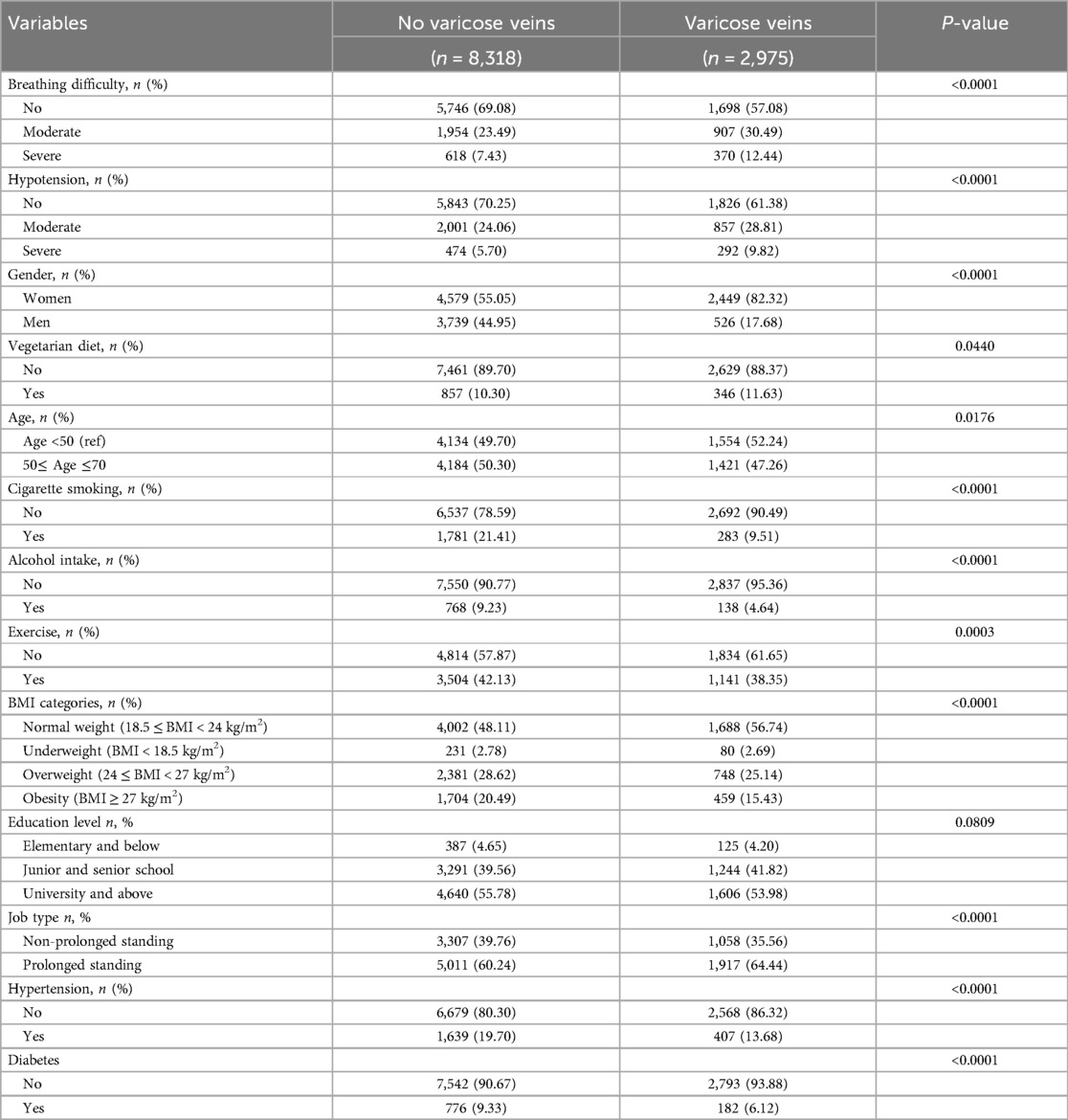
A total of 11,293 participants were enrolled in the study. The basic characteristics stratified by varicose vein status are reported in Table 1. VVs had a higher prevalence in women compared with men (82.32 vs. 17.68%). Among patients without varicose veins (control cohort), they reported no symptoms (n = 5,746, 69.08%), moderate (n = 1,954, 3.49%), and severe (n = 618, 7.43%) breathing difficulties. In a subgroup of patients with varicose veins (diseased cohort), 1,698 (57.08%), 907 (30.49%), and 370 (12.44%) patients presented with no, moderate, and severe discomfort, respectively. The proportion of moderate and severe symptoms of breathing difficulty was higher in the diseased cohort than in the control cohort (P < 0.0001). Regarding hypotension, there were 5,843 (70.25%), 2,001 (24.06%), and 474 (5.70%) patients presenting with no, moderate, and severe symptoms in the control group, respectively, while the diseased cohort had 1,826 (61.38%), 857 (28.81%), and (9.82%) patients the reported no, moderate, and severe hypotension, respectively. Hypotension was more common in the diseased compared to the control cohort (P < 0.0001).
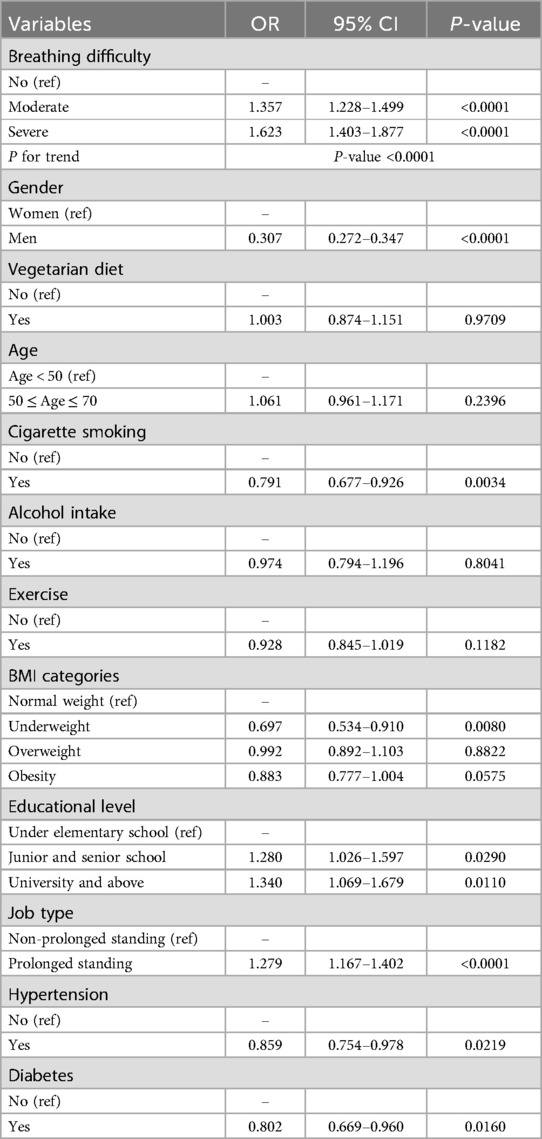
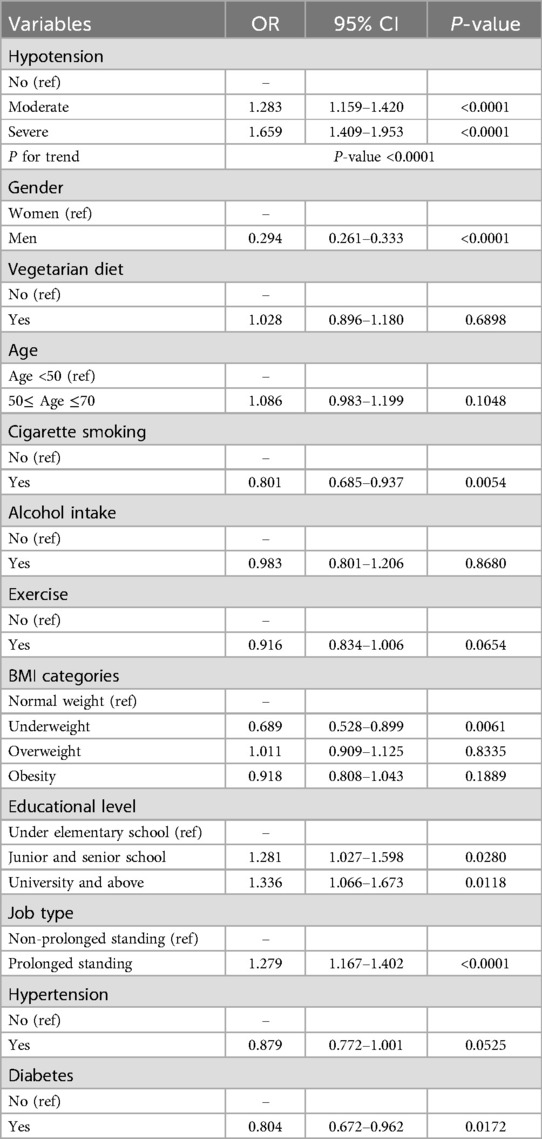
The association between breathing difficulties and VVs was determined using logistic regression (Table 2). When using no breathing difficulty as the reference group, the OR of moderate breathing difficulty was 1.357 (95% CI = 1.228–1.499) and 1.623 (95% CI = 1.403–1.877) for severe breathing difficulty, with statistical significance in P trend test (P < 0.0001). Moreover, the result of the association between hypotension and VVs is shown in Table 3. The OR of moderate hypotension was 1.283 (95% CI = 1.159–1.420) and 1.659 (95% CI = 1.409–1.953) in severe hypotension when compared with patients without hypotension. The trend was statistically significant (P < 0.0001).
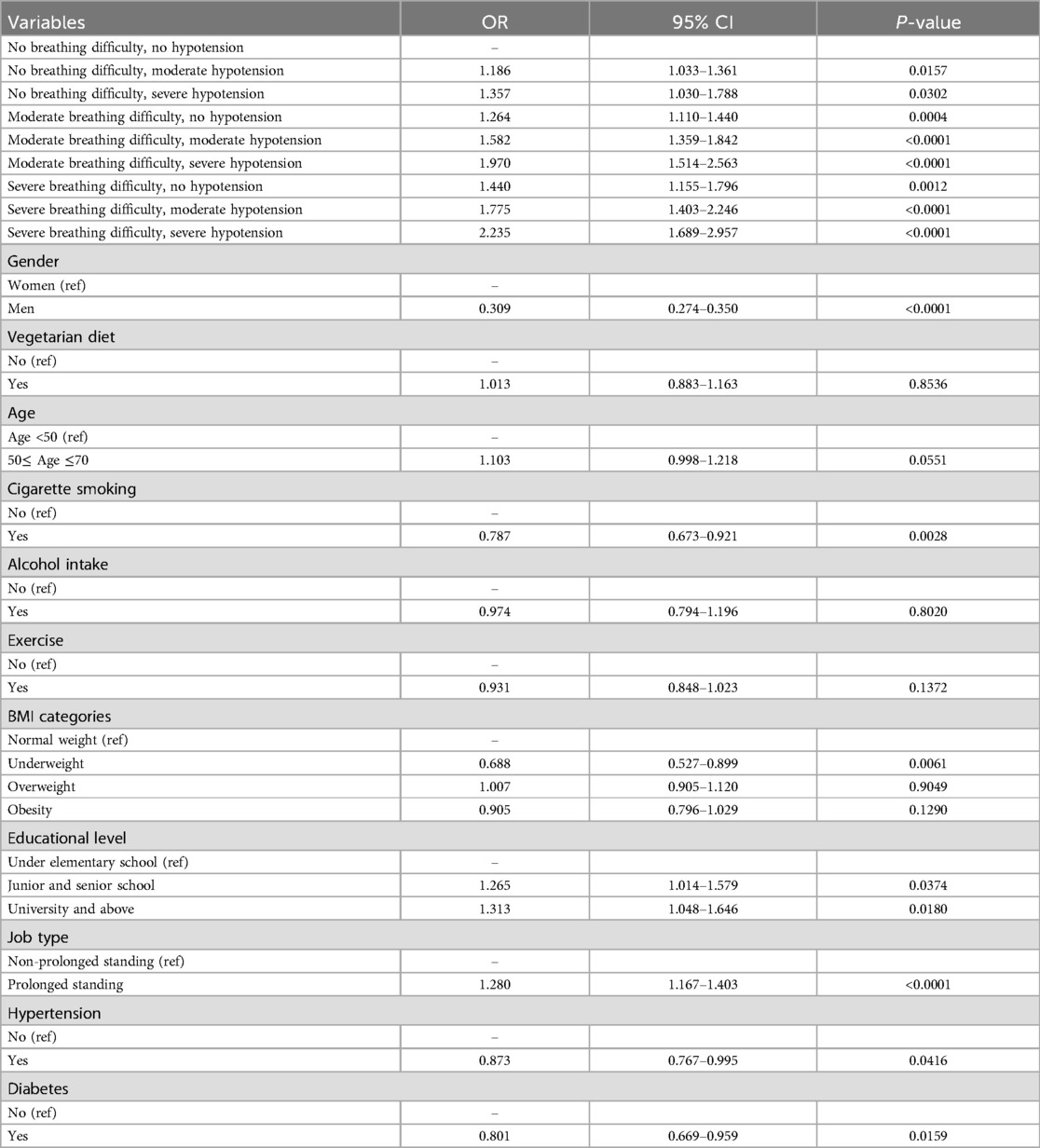
Furthermore, the results of logistic regression analysis of the association between breathing difficulties, hypotension, and VVs are illustrated in Table 4. When taking patients with no breathing difficulty/no hypotension as a reference, the cofactor OR of patients with no breathing difficulty/moderate hypotension was 1.186 (95% CI = 1.033–1.361), while no breathing difficulty/severe hypotension was 1.357 (95% CI = 1.030–1.788). Furthermore, the cofactor OR of moderate breathing difficulty/no hypotension was 1.264 (95% CI = 1.110–1.440), moderate breathing difficulty/moderate hypotension was 1.582 (95% CI = 1.359–1.842), and 1.970 (95% CI = 1.514–2.563) in moderate breathing difficulty/severe hypotension. Additionally, the cofactor OR was 1.440 (95% CI = 1.155–1.796) for patients with severe breathing difficulty/no hypotension, 1.775 (95% CI = 1.403–2.246) for severe breathing difficulty/moderate hypotension, and 2.235 for severe breathing difficulty/severe hypotension (95% CI = 1.689–2.957).
4 Discussion
There are shared risk factors between VVs and cardiovascular diseases, including obesity, aging, smoking, and diabetes. Both conditions also share the pathophysiology of endothelial dysfunction, inflammation, and thrombosis (13). Diagnosis of both heart failure and chronic venous disease rely on typical physical examination; however, given that leg edema was the most common manifestation of CVI, there could be confusion or coexistence between VVs and undetected heart failure. Risk factor prediction is extremely important to enhance the diagnosis in VV patients with “hear-failure-like symptoms” or the so-called “Constitution of Traditional Chinese Medicine.” The present study demonstrated that females had a higher prevalence of VVs, and prolonged standing jobs were more prevalent in patients with VVs compared with the control group (Table 1). The proportion of moderate and severe symptoms of breathing difficulties and hypotension were more common in the VV cohort. The combined impact of breathing difficulties and hypotension increased with severity (Table 4).
A study including 10,423 adult participants used self-reported venous symptoms to define the CEAP and classify CVI (14). Compared with men, women had a higher burden of chronic venous disease, which is compatible with the results in the present study, with a higher prevalence of VVs in women compared with men (82.32 vs. 17.68%) (14). The present study also reported that being male was a negative risk factor compared with being female (OR = 0.309, 95% CI = 0.274–0.350, P < 0.001, Table 4). Prior studies have explored the risk factors for CVI, including age, female sex, and smoking (15–17), which supported the findings in the present study (Table 1). Obesity affects up to one-quarter of lower limb venous disease, is an important risk factor for VVs, and is more likely to be symptomatic because of their lower limb venous disease (18, 19). However, there was no remarkably higher prevalence of obesity in the diseased group compared to the control (Table 1). The reporting bias could be due to the invisibility of distorted blood vessels on the limbs of patients with obesity when the study was based on self-reported assessments. The present study reported that jobs needing prolonged standing were more common in patients with VVs (Table 1), which is consistent with a previous study showing a higher risk of VV of employees with jobs requiring prolonged standing compared with other employees (1.75 for men and 1.82 for women) (20). Diabetes is a risk factor for VVs (21–23); however, antidiabetic medication, such as metformin, could reduce the risk of VVs in patients with diabetes (24). The present study also demonstrated that diabetes was a negative predictor for VVs (OR = 0.801, 95% CI = 0.669–0.959, P = 0.0159, Table 4).
There were two main symptoms of the constitution of traditional Chinese medicine in this study, including breathing difficulty and hypotension. The association between each symptom with VVs varied according to its severity. (1) If patients presented with only one symptom, the contribution of breathing difficulty was higher than hypotension in the association with VVs (if there was no breathing difficulty, the cofactor OR of moderate hypotension = 1.186; severe hypotension = 1.357, while cofactor OR of moderate breathing difficulty = 1.264 and severe breathing difficulty = 1.440 when there was no hypotension). (2) If one of the two symptoms was moderate in severity, the cofactor of hypotension had a greater association with VVs than with breathing difficulties (under moderate breathing difficulty situations, respective cofactor ORs of moderate and severe hypotension = 1.582 and 1.970, respectively, while under moderate hypotension situation, cofactor ORs of moderate and severe breathing difficulty = 1.583 and 1.775, respectively, Table 4). However, (3) If one of the two symptoms was severe, the cofactor of breathing difficulties was more associated with VV than hypotension (under severe breathing difficulty situation, respective cofactor ORs of moderate and severe hypotension were 1.775 and 2.235, respectively, while under severe hypotension situation, cofactor ORs of moderate and severe breathing difficulty = 1.970 and 2.235, respectively, Table 4). Moreover, when patients complained of both symptoms, the risk of VVs was higher if the severity of any one of the symptoms was worse.
Previous evidence demonstrated a higher prevalence of clinical conditions of cardiovascular comorbidities (such as atrial fibrillation, congestive heart failure, and myocardial infarction) as CVI progressed (25). The reason for the variant association between symptoms and VVs could be explained by the insufficient preload and the complications of stationary flow in VVs. As VVs progressed, reduced venous return to the heart and pooling of blood below the inferior vena cava led to hypotension, tachycardia, and lower extremity edema (26). As the severity gets worse, venous stasis or turbulent flow predisposes to thrombotic events (27). Previous evidence has indicated that a history of deep vein thrombosis (DVT) increases the incidence of VVs with a hazard ratio of 2.6 (14, 15). Moreover, a retrospective cohort study investigating >400,000 patients in Asia demonstrated that VV increased the incidence of DVT drastically with a hazard ratio of 5.3 (28). Additionally, patients with VVs had a higher incidence of DVT than the control group (6.55 vs. 1.23 per 1,000 person-years) (28). In a study with 1.2 million people, 40% of patients had pulmonary embolism with or without DVT (29), As one criteria of Virchow's triad, venous stasis contributes to thromboembolic events and pulmonary embolism. The present study reported that breathing difficulties revealed a tighter association with VVs compared with hypotension when there were severe symptoms, which could be attributed to coexisting impacts from inadequate preload and potential thromboembolic events.
There was a 36.5% prevalence of chronic venous diseases in patients with any cardiovascular disease, with the highest prevalence of 30% in patients with lower extremity edema and the lowest prevalence in patients with ulceration (13). However, even in C3–C6 severity, 2.8–32.2% of patients were symptomatic, while 14.0–37.6% of patients were asymptomatic. In C2 patients, there were only 1.2%–4.9% symptomatic patients, compared with 6.4%–8.8% asymptomatic patients (25). As the patients were younger, more asymptomatic patients were reported, which could lead to underdiagnosis of VVs (25). Less than 50% of patients were older than 50 years in the present study, and the prevalence of asymptomatic patients with VV may mask the accurate diagnosis of VVs. In addition to congestive heart failure and pulmonary hypertension, VVs have also been characterized by unspecified “heart-failure-like symptoms,” such as fatigue, dizziness, anorexia, palpitations, and shortness of breath on exertion (26). Self-report by self-observation could elevate the diagnosis of VVs in the early stages before symptoms develop. In terms of therapy, intermittent use or full compliance of compression stockings have been recommended by European Society for Vascular Surgery as one of the conservative treatment modalities for chronic venous disease (30). It has been reported to be effective in relieving symptoms in patients with chronic venous disease by decreasing pain, heaviness, cramps, and oedema (30). Unfortunately, the present study has opted for a questionnaire approaching database with self-reported venous assessment, which was lacking in the documentation on whether elastic compression stockings were used for symptom relief.
Since VVs disease has been a crucial issue, many evidences have reported that chronic venous disease is relevant to cardiovascular disorders (30). Patients are prone to developing venous diseases and symptoms, such as edema, leg pain, and cutaneous changes. Therefore, history-taking and physical assessment are clinchers to identify coexisting cardiovascular diseases (30). Moreover, patients with VVs have two-fold increase in the risk of major adverse cardiovascular events, including congestive heart failure, ischaemic stroke, DVT and pulmonary embolism (30). Fortunately, both Wells score and D-dimer levels could be considerable options used to evaluate the possibility of venous thrombosis and the necessity for advanced diagnostic imaging such as ultrasonography or computed tomography venography (31). Furthermore, recent article also indicated the gene correlation between varicose vein and heart failure, suggesting that people with varicose veins might have a higher risk of heart failure (31). One practical hint of the edema relevant to CVI is pitting pattern, originating in the peri-malleolar region, progresses up the leg in a dependent manner but spares the forefoot (32). Since more and more evidences have highlighted the crosstalk between VVs and heart failure, self-report assessment focusing on leg is a simple and quick check-up regarding the concerns of both VVs, early heart failure sign, or concomitant events.
5 Strengths and limitations
Despite limitations of lacking of objective information, such as electrocardiography, echocardiography, or biochemistry data, the present study gathered objective questionnaire data from a substantial cohort of 11,293 participants. This approach offered an efficient and practical tool that closely mimicked real-world applications for both primary care providers and specialists. This study reinforced the idea of educating patients and clinical practitioners to observe their legs, and further useful information could be acquired to reduce the risk of thrombosis and avoid misdiagnosis of other cardiovascular diseases.
6 Conclusions
VVs had a tight association with breathing difficulty and hypotension as the disease progressed, and the combined impact of the two symptoms also increased their association with VVs as the severity increased. For asymptomatic patients with VVs, it can be a simple method to assess the severity of VV by self-reported observation before it progresses to “heart-failure-like symptoms.”
Data availability statement
The datasets presented in this article are not publicly accessible due to restrictions on their usage. Requests for data access should be directed to Cheng-Ken Tsai atbTg3MTM3M0BnbWFpbC5jb20=.
Author contributions
C-KT: Conceptualization, Data curation, Methodology, Project administration, Resources, Writing – original draft, Writing – review & editing. ON: Data curation, Formal Analysis, Software, Writing – original draft, Writing – review & editing. W-YL: Funding acquisition, Project administration, Resources, Writing – review & editing. Y-PL: Funding acquisition, Project administration, Supervision, Validation, Visualization, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Leopardi D, Hoggan BL, Fitridge RA, Woodruff PW, Maddern GJ. Systematic review of treatments for varicose veins. Ann Vasc Surg. (2009) 23(2):264–76. doi: 10.1016/j.avsg.2008.10.007
2. Lurie F, Passman M, Meisner M, Dalsing M, Masuda E, Welch H, et al. The 2020 update of the CEAP classification system and reporting standards. J Vasc Surg Venous Lymphat Disord. (2020) 8(3):342–52. doi: 10.1016/j.jvsv.2019.12.075
3. Mulita F, Dimopoulos P, Verras GI, Mustaqe P, Jaho J, Leivaditis V, et al. Demographic and clinical characteristics of patients with varicose veins in Albania: a retrospective, single-centre analysis. Arch Med Sci Atheroscler Dis. (2024) 9:e41–6. doi: 10.5114/amsad/183653
4. Sassaki VS, Fukaya E. Varicose veins: approach, assessment, and management to the patient with chronic venous disease. Med Clin North Am. (2023) 107(5):895–909. doi: 10.1016/j.mcna.2023.05.002
5. Beebe-Dimmer JL, Pfeifer JR, Engle JS, Schottenfeld D. The epidemiology of chronic venous insufficiency and varicose veins. Ann Epidemiol. (2005) 15(3):175–84. doi: 10.1016/j.annepidem.2004.05.015
6. Gawas M, Bains A, Janghu S, Kamat P, Chawla P. A comprehensive review on varicose veins: preventive measures and different treatments. J Am Nutr Assoc. (2022) 41(5):499–510. doi: 10.1080/07315724.2021.1909510
7. Yap SY, Ng FL, Subramaniam M, Lim YM, Foo CN. Traditional Chinese medicine body constitutions as predictors for depression: a systematic review and meta-analysis. Behav Sci (Basel). (2022) 12(11). doi: 10.3390/bs12110423
8. Marshall AC. Traditional Chinese medicine and clinical pharmacology. In: Drug Discovery and Evaluation: Methods in Clinical Pharmacology. 2nd ed. Springer International Publishing (2020). p. 455–82. doi: 10.1007/978-3-319-68864-0_60
9. Lu AP, Jia HF, Xiao C, Fau XC, Lu Q-P, Lu QP. Theory of traditional Chinese medicine and therapeutic method of diseases. (1007-9327 (Print)).
10. Jiang Q-Y, Li J, Zheng L, Wang G-H, Wang J. Constitution of traditional Chinese medicine and related factors in women of childbearing age. J Chin Med Assoc. (2018) 81(4):358–65. doi: 10.1016/j.jcma.2018.01.005
11. Sun Y, Zhao Y, Xue SA, Chen J. The theory development of traditional Chinese medicine constitution: a review. J Tradit Chin Med Sci. (2018) 5(1):16–28. doi: 10.1016/j.jtcms.2018.02.007
12. Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Circulation. (2022) 145(18):e895–e1032. doi: 10.1161/cir.0000000000001063
13. Hamburg NM. The legs are a pathway to the heart: connections between chronic venous insufficiency and cardiovascular disease. Eur Heart J. (2021) 42(40):4166–8. doi: 10.1093/eurheartj/ehab589
14. Baylis RA, Smith NL, Klarin D, Fukaya E. Epidemiology and genetics of venous thromboembolism and chronic venous disease. Circ Res. (2021) 128(12):1988–2002. doi: 10.1161/CIRCRESAHA.121.318322
15. Fukaya E, Flores AM, Lindholm D, Gustafsson S, Zanetti D, Ingelsson E, et al. Clinical and genetic determinants of varicose veins. Circulation. (2018) 138(25):2869–80. doi: 10.1161/circulationaha.118.035584
16. Criqui MH, Jamosmos M, Fronek A, Denenberg JO, Langer RD, Bergan J, et al. Chronic venous disease in an ethnically diverse population: the San Diego Population Study. Am J Epidemiol. (2003) 158(5):448–56. doi: 10.1093/aje/kwg166
17. Lee AJ, Evans CJ, Allan PL, Ruckley CV, Fowkes FG. Lifestyle factors and the risk of varicose veins: Edinburgh vein study. J Clin Epidemiol. (2003) 56(2):171–9. doi: 10.1016/s0895-4356(02)00518-8
18. Davies HO, Popplewell M, Singhal R, Smith N, Bradbury AW. Obesity and lower limb venous disease—the epidemic of phlebesity. Phlebology. (2017) 32(4):227–33. doi: 10.1177/0268355516649333
19. Davies HO, Popplewell M, Singhal R, Smith N, Bradbury AW. Obesity and lower limb venous disease—The epidemic of phlebesity. (1758-1125 (Electronic)).
20. Tüchsen F, Hannerz H, Burr H, Krause N. Prolonged standing at work and hospitalisation due to varicose veins: a 12 year prospective study of the Danish population. Occup Environ Med. (2005) 62(12):847–50. doi: 10.1136/oem.2005.020537
21. Hu H, Hu L, Deng Z, Jiang Q. A prognostic nomogram for recurrence survival in post-surgical patients with varicose veins of the lower extremities. Sci Rep. (2024) 14(1):5486. doi: 10.1038/s41598-024-55812-0
22. Komsuoğlu B, Göldeli O, Kulan K, Cetinarslan B, Komsuoğlu SS. Prevalence and risk factors of varicose veins in an elderly population. Gerontology. (1994) 40(1):25–31. doi: 10.1159/000213571
23. Ali SA, Najmi WK, Hakami FM, Almubarak AA, Alhassan RA, Maafa SH, et al. Prevalence of varicose veins among nurses in different departments in jazan public hospitals, Saudi Arabia: a cross-sectional study. Cureus. (2022) 14(4):e24462. doi: 10.7759/cureus.24462
24. Tseng CH. Metformin reduces risk of varicose veins in patients with type 2 diabetes. Diabetes Metab Res Rev. (2020) 36(2):e3206. doi: 10.1002/dmrr.3206
25. Prochaska JH, Arnold N, Falcke A, Kopp S, Schulz A, Buch G, et al. Chronic venous insufficiency, cardiovascular disease, and mortality: a population study. Eur Heart J. (2021) 42(40):4157–65. doi: 10.1093/eurheartj/ehab495
27. Shaydakov ME, Comerota AJ, Lurie F. Primary venous insufficiency increases risk of deep vein thrombosis. J Vasc Surg Venous Lymphat Disord. (2016) 4(2):161–6. doi: 10.1016/j.jvsv.2015.09.008
28. Chang SL, Huang YL, Lee MC, Hu S, Hsiao YC, Chang SW, et al. Association of varicose veins with incident venous thromboembolism and peripheral artery disease. JAMA. (2018) 319(8):807–17. doi: 10.1001/jama.2018.0246
29. Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2020 update: a report from the American heart association. Circulation. (2020) 141(9):e139–596. doi: 10.1161/cir.0000000000000757
30. De Maeseneer MG, Kakkos SK, Aherne T, Baekgaard N, Black S, Blomgren L, et al. Editor’s choice – European society for vascular surgery (ESVS) 2022 clinical practice guidelines on the management of chronic venous disease of the lower limbs. Eur J Vasc Endovasc Surg. (2022) 63(2):184–267. doi: 10.1016/j.ejvs.2021.12.024
31. Guo P, Fang Q, Wang Y. Associations between varicose veins and heart failure: a genetic correlation and Mendelian randomization study. Medicine (Baltimore). (2024) 103(20).
Keywords: constitution of traditional Chinese medicine, chronic venous insufficiency, heart failure, heart-failure-like symptoms, varicose vein
Citation: Tsai C-K, Nfor ON, Lu W-Y and Liaw Y-P (2024) Association between varicose veins and constitution of traditional Chinese medicine plus heart-failure-like symptoms. Front. Cardiovasc. Med. 11:1465843. doi: 10.3389/fcvm.2024.1465843
Received: 3 August 2024; Accepted: 24 September 2024;
Published: 23 October 2024.
Edited by:
Francesk Mulita, General Hospital of Eastern Achaia- Unit of Aigio, GreeceReviewed by:
Andreas Antzoulas, General University Hospital of Patras, GreeceAngelis Peteinaris, University of Patras, Greece
Christos Pitros, General University Hospital of Patras, Greece
Spyros Papadoulas, General University Hospital of Patras, Greece
Copyright: © 2024 Tsai, Nfor, Lu and Liaw. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yung-Po Liaw, TGlhd2xpYXd5cEBjc211LmVkdS50dw==
 Cheng-Ken Tsai
Cheng-Ken Tsai Oswald Ndi Nfor
Oswald Ndi Nfor Wen-Yu Lu
Wen-Yu Lu Yung-Po Liaw
Yung-Po Liaw