- 1Department of Pharmacy, Institute of Health Science, Wallaga University, Nekemte, Ethiopia
- 2Department of Health Informatics, College of Health Science, Mattu University, Mattu, Ethiopia
- 3Department of Infectious Diseases and Public Health, Jockey Club College of Veterinary Medicine and Life Sciences, City University of Hong Kong, Hong Kong, Hong Kong SAR, China
Background: Heart failure (HF) is a leading cause of morbidity and mortality worldwide. Various factors can exacerbate disease progression in patients with HF and negatively impact treatment outcomes. This study aims to evaluate the pooled prevalence and contributing factors associated with poor heart failure treatment outcomes in Ethiopia.
Methods: A systematic review and meta-analysis were conducted using five databases: Google Scholar, ScienceDirect, Hinari, PubMed, and Scopus. In total, 12 studies met the eligibility criteria for inclusion in this analysis. The review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses 2020 guidelines. Data extraction was performed using a Microsoft Excel spreadsheet, and statistical analysis was conducted with STATA 14. The Joanna Briggs Institute Meta-analysis of Statistics Assessment and Review Instrument was utilized for quality assessment. Heterogeneity among the studies was evaluated using the I2 statistic and the Cochrane Q test. Publication bias was assessed using Begg's test, Egger's weighted regression, and funnel plots.
Results: The pooled prevalence of poor HF treatment outcomes was found to be 16.67% [95% confidence interval (CI): 10.67–22.67]. No significant heterogeneity was observed across the included studies (I2 = 0.0%, p = 0.962). Significant predictors of a poor treatment outcome were smoking cigarettes [adjusted odds ratio (AOR) = 10.74; 95% CI: 3.24–35.63] and medication-related problems (AOR = 3.99; 95% CI: 1.90–8.37).
Conclusion: The prevalence of poor HF treatment outcomes in Ethiopia was found to be high. Smoking cigarettes and medication-related problems are significant predictors of these adverse outcomes. Comprehensive health education and improved clinical pharmacy services are essential for addressing these issues.
Systematic Review Registration: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42023437397, PROSPERO (CRD42023437397).
Background
Heart failure (HF) is a clinical syndrome characterized by the heart's diminished capacity to pump and/or fill with blood (1). It occurs when the body's metabolic needs are not met by the heart's ability to pump a sufficient volume of blood (2). Clinical signs of HF include dyspnea, fatigue, exercise intolerance, and fluid retention (3).
Globally, HF impacted over 64.3 million people in 2017 (4). The incidence of heart failure rises sharply with age; it affects 1%–2% of individuals in the 40–59 years age group and up to 12% of those older than 80 years. Heart failure is a leading cause of morbidity and mortality worldwide (5–7). Within a year of diagnosis, 30%–40% of patients succumb to the condition globally (8). Hospitalization for HF is associated with a high risk of mortality, both in the short and long term (9). The prognosis for HF remains dire, with a 50% 5-year mortality risk upon diagnosis—higher than that of several cancer types (10).
Many variables contribute to an accelerated progression of the disease and diminished treatment responsiveness in patients with HF (6). Approximately two out of every three Asian patients with widespread HF have at least two comorbidities. Poorer outcomes are linked to multimorbidity patterns in patients with HF (10).
Most patients, regardless of symptom severity, require lifelong optimal medical treatment, which includes angiotensin-converting enzyme inhibitors (ACEIs), beta-blockers (BB), and mineralocorticoid receptor antagonists (MRAs) to reduce hospitalization and mortality (11). Despite advancements in pharmaceutical therapy, HF morbidity and mortality remain high. Therefore, non-pharmacological management, primarily focusing on self-care, deserves increased attention (12).
Management of HF encompasses both lifestyle modifications and pharmacological interventions. Hospitalization rates within 6 months of discharge between 30% and 40%, and morbidity and mortality rates remain elevated, with quality of life still low despite breakthroughs in prevention and therapy (8, 11, 13–15). It has been observed that older, male, and African-American patients experience higher mortality rates (9, 14). Urgent interventions should be prioritized to address the underlying causes of HF, halt its progression, and redesign healthcare delivery, infrastructure, and treatment options (16).
In Ethiopia, heart failure-related mortality rates range from 10.2% to 32.6% (6, 7, 11, 13–17). Several risk factors, including comorbidity, advanced HF class, lower left ventricular ejection fraction (LVEF), male sex, and adverse medication events, have been associated with poor treatment outcomes (6, 13, 17, 18).
Furthermore, in Ethiopia, the management and outcomes of HF are particularly concerning due to limited healthcare resources and access to specialized care. The healthcare system often faces challenges such as inadequate diagnostic facilities, a shortage of trained healthcare professionals, and limited availability of essential medications. These factors contribute to suboptimal treatment adherence and poorer health outcomes for patients with HF. Furthermore, cultural perceptions and stigma associated with chronic illnesses may deter individuals from seeking timely medical care, exacerbating the burden of HF in the population.
This study aims to summarize recent findings on the prevalence of, and factors related to, poor treatment outcomes to inform appropriate interventions. Despite inconsistent reports on the prevalence and predictors of HF treatment outcomes in Ethiopia, no systematic review and meta-analysis has been conducted.
Methods
Search strategy
This systematic review and meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guidelines (19). Five databases—PubMed, Science Direct, Scopus, HINARI, and Google Scholar—were utilized for the literature search. The review was conducted from 12 November to 11 December 2023, with the final search conducted on 8 December 2023. The search strategy employed the following MeSH terms: [(Burden) OR (Mortality) AND (Predictors) AND (HF) AND (Ethiopia)]. The review protocol was registered with PROSPERO (CRD42023437397).
Data collection process, items, and extraction
Two authors (FB and LT) were responsible for collecting relevant literature. Reference management software (EndNote X7.2) was used to combine the results and eliminate duplicates. Three data extractors (GD, GF, and DS) utilized a standardized data extraction checklist on Microsoft Excel. For the primary outcome (burden), the checklist included the author's name, publication year, study area, study design, sample size, and the number of individuals with the outcome. For the secondary outcome (predictors), data were extracted in the form of two-by-two tables to calculate the log odds ratio (OR) based on the original research results. Any disagreements between the two independent reviewers were resolved through discussion, with a third reviewer (DD) involved if consensus was not reached.
Eligibility criteria
Studies were included if they reported primary outcomes and full texts were accessible, specifically focusing on the burden and determinants of poor HF treatment outcomes in Ethiopia. Excluded articles included systematic reviews, meta-analyses, preprints, brief communications, letters to the editor, and articles with unclear primary outcomes. Qualitative and non-observational studies were excluded; however, cross-sectional studies were retained. The Condition, Context, and Population (CoCoPop) framework was employed to assess study eligibility: the population consisted of patients with HF, the condition was defined as treatment outcomes for HF, and the setting was Ethiopia.
Outcome measurement
Two primary outcomes were assessed. The burden of poor HF treatment outcomes was defined as the total number of patients with poor outcomes divided by the total number of HF patients, multiplied by 100. The second outcome involved determining factors associated with poor treatment outcomes, using ORs and binary outcomes from the included studies. Poor outcomes were operationally defined as hospital mortality related to HF, self-discharge, and HF sequelae (17).
Quality assessment
Quality assessment was conducted using the Joanna Briggs Institute Meta-Analysis of Statistics Assessment and Review Instrument (JBI-MAStARI) (20) which is tailored for cross-sectional studies and has more univocal items for observational studies. This tool can be used without modifying its domains, unlike other tools such as the Newcastle–Ottawa Scale. The Newcastle–Ottawa Scale tool is only validated for case–control and longitudinal studies. The quality of the included studies was assessed based on several criteria: clarity in the definition of inclusion criteria for the sample, a detailed description of the study subjects and setting, the validity and reliability of exposure measurement, use of objective, standard criteria to measure the condition, identification of confounding factors, articulation of strategies to address these confounding factors, the validity and reliability of the outcome measurement, and the appropriateness of the statistical analysis utilized. Two authors (FB and GD) conducted the quality assessment and any disagreements were resolved by a third reviewer (DS). Articles were classified as high quality if the score was greater than 80%, moderate if between 65% and 80%, and low if below 65%.
Data analysis and synthesis
Data were exported to STATA V. 14 to determine the pooled effect size with 95% confidence intervals (CIs). The Cochran Q test (chi-squared statistic) and I2 statistic were computed to assess heterogeneity among the included studies. A p-value of <0.05 indicated statistically significant heterogeneity. I2 values were interpreted as follows: 0% (no heterogeneity), 25% (minimal), 50% (moderate), and 75% (high). A funnel plot was employed to assess publication bias, with asymmetry indicating potential bias. In addition, Egger's weighted regression and Begg's test were conducted to evaluate publication bias, with statistical significance set at p < 0.05.
Results
A total of 4,010 articles were identified from initial searches conducted in PubMed, ScienceDirect, Hinari, Scopus, and Google Scholar. After removing 3,746 duplicate articles, 241 additional articles were excluded based on title and abstract screening. Consequently, 23 articles underwent full-text review, and ultimately, 12 articles were selected for inclusion in this review (Figure 1).
Characteristics of the included studies
The articles included in our systematic review and meta-analysis were observational studies. The majority of participants were female, as reported in seven of the articles (6, 7, 13, 17, 21–23). The total sample size was 3,002 patients with HF, with individual study sample sizes ranging from 96 to 496. Regarding study settings, five articles originated from Amhara (6, 13, 21–23) and five from Oromia (7, 11, 24–26), while two articles were based in Addis Ababa (17, 27) (Table 1).
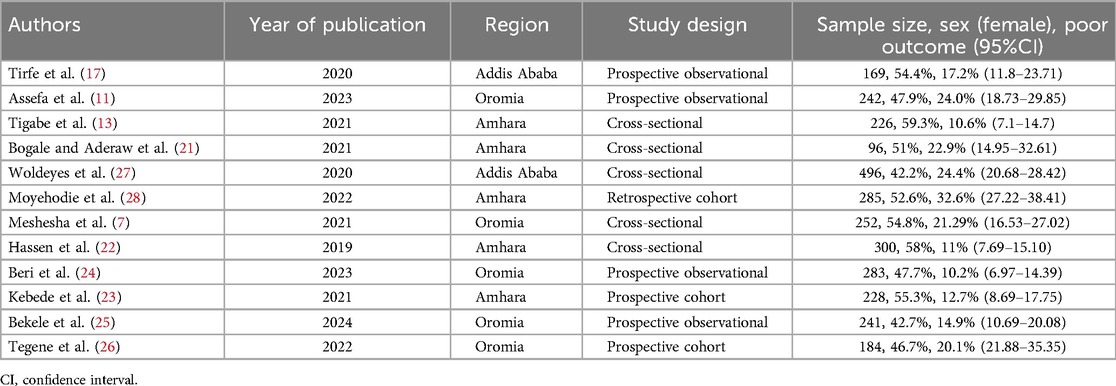
Table 1. Summary of included studies on the burden and associated factors of poor treatment outcomes among patients with HF in Ethiopia, 2024.
Quality assessment of included studies
In our systematic review and meta-analysis, eight articles (7, 11, 13, 17, 23–25, 27) were classified as high quality, while the remaining four articles (6, 21, 22, 26) were categorized as moderate quality according to the JBI-MAStARI.
The magnitude of poor heart failure treatment outcome
The pooled magnitude of poor heart failure treatment outcomes was found to be 16.67% (95% CI: 10.67–22.67). No heterogeneity was observed across the included studies (I2 = 0.0%, p = 0.962). This lack of heterogeneity suggests that the true underlying effect size was consistent across all the included studies, which were drawn from similar populations. The highest reported rate of poor heart failure treatment outcomes was 32.6% in Amhara (6), while the lowest was 10.2% in Oromia (24) (Figure 2).
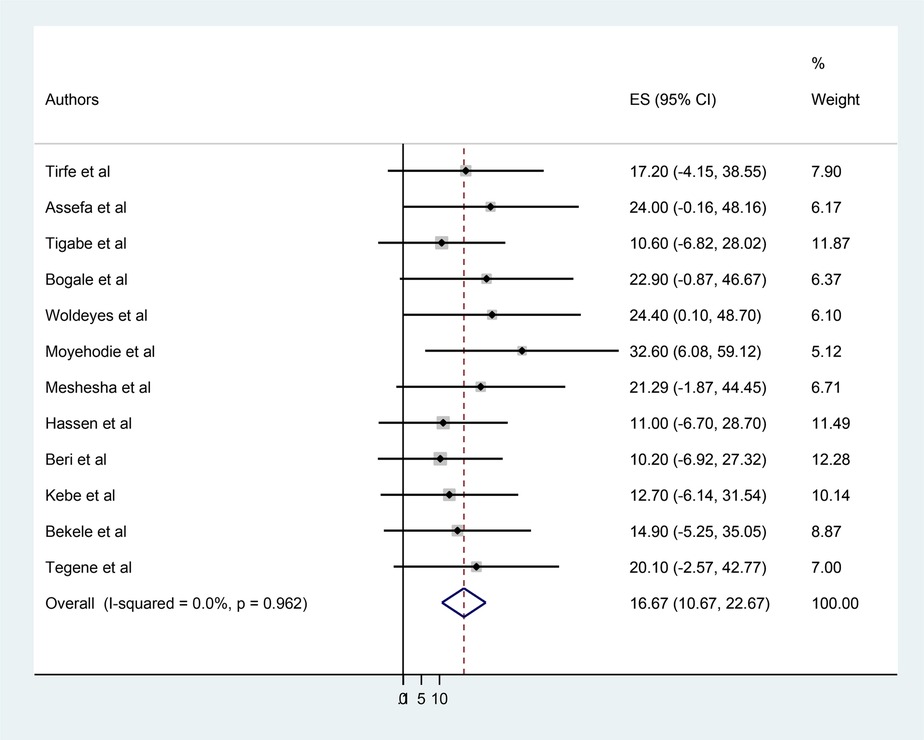
Figure 2. Forest plot of the pooled prevalence of poor heart failure treatment outcomes in Ethiopia, 2024.
Publication bias
To assess the presence of publication bias, a funnel plot, Egger's test, and Begg's test were conducted at a 5% significance level. The funnel plot appeared symmetrical, and both the Egger test and Begg's test indicated no statistically significant evidence of publication bias, with p-values of 0.539 and 0.174, respectively (Figure 3).
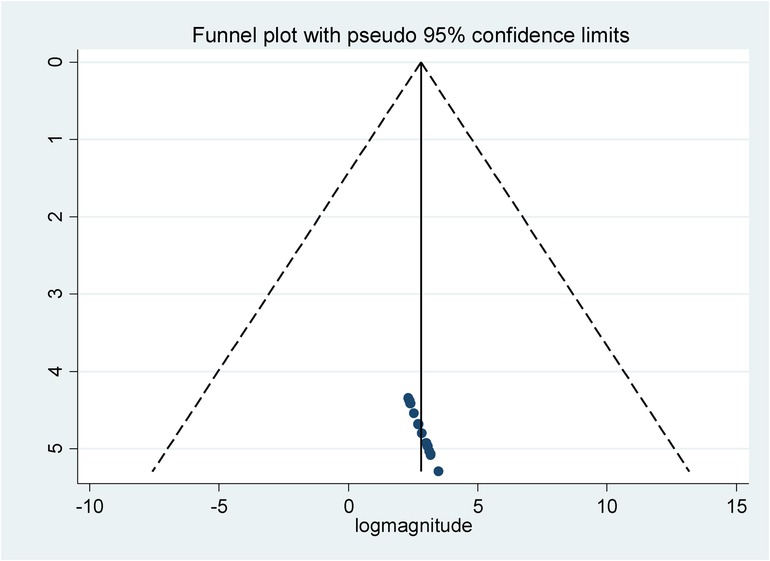
Figure 3. Funnel plot to test for publication bias in the included studies conducted in Ethiopia, 2024.
Factors associated with poor heart failure treatment outcomes
Six studies were included in the meta-analysis to identify pooled predictors of poor heart failure treatment outcomes. The pooled effect of the odds ratios was assessed using the command “metanlogor selogor, xlab(0.1,1,10) label(namevar=authors) by (factors) random texts(180)eform.” Patients with HF who smoked cigarettes were found to be 10.74 times more likely to experience poor treatment outcomes compared to their non-smoking counterparts [adjusted odds ratio (AOR) = 10.74; 95% CI, 3.24–35.63]. Similarly, patients who experienced medication-related problems were four times more likely to develop poor treatment outcomes than those without such problems (AOR = 3.99; 95% CI, 1.90–8.37) (Figure 4).
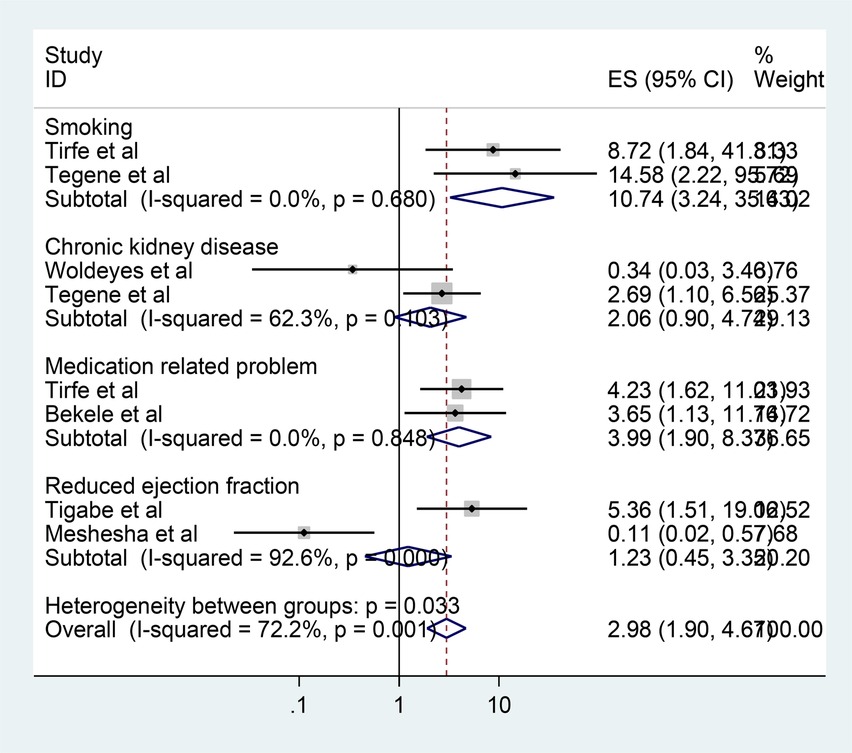
Figure 4. Forest plot of the factors associated with poor heart failure treatment outcomes in Ethiopia, 2024.
Discussion
HF has been recognized as a significant contributor to the cardiovascular disease burden in sub-Saharan Africa for many decades (29). Therefore, our study aimed to assess the predictors of poor HF treatment outcomes in Ethiopia.
The pooled prevalence of poor HF treatment outcomes in Ethiopia was 16.67%, which was higher than studies conducted in Kenya (30) and Uganda (31). Compared to these previous studies, we found a higher incidence of in-hospital mortality. This may be attributable to the fact that these studies were carried out in highly specialized cardiac centers with superior diagnostic, therapeutic, and human resources, resulting in lower in-hospital mortality rates. In contrast, the current study was performed in the general medicine ward of a regional hospital, which reflects the level of care where the majority of patients with HF seek treatment in low-income countries such as Ethiopia.
The burden of HF was lower than that reported in studies conducted in Tanzania (6), Angola (32), and Burkina Faso (15). The variability in HF burden might be due to differences in patient characteristics, study designs, settings, duration, and the etiology of HF.
Patients with HF who smoked cigarettes were 10.74 times more likely to experience poor treatment outcomes compared to their counterparts. This finding aligns with studies conducted in Uganda and Tikur Anbessa Specialized Hospital in Addis Ababa, Ethiopia (17, 31). This correlation may be due to the cardiovascular risks associated with nicotine, which adversely affects the heart vessels and valves of tobacco smokers.
Patients with heart failure who had medication-related problems were 3.99 times more likely to have poor treatment outcomes than those who did not experience such problems. This finding is consistent with a study conducted in Angola, where medication non-compliance was identified as a precipitating factor of decompensated HF (32). Similar reports were noted in the study conducted in Tikur Anbessa Specialized Hospital (17). These issues may stem from the negative effects of drug therapy problems when attempting to optimize HF management. Drug-related problems (DRPs) are events involving medications that can impact a patient's desired therapeutic goals (33, 34).
The absence of clinical pharmacy services in Ethiopia may contribute to the prevalence of medication-related problems that adversely affect the treatment outcomes of patients with HF. In addition, insufficient interventions to reduce cigarette smoking persist, as smoking is often viewed as a social norm in Ethiopia. This cultural perception may contribute significantly to HF-associated mortality. Implementing pharmaceutical care services, including involving clinical pharmacists in patient rounds and establishing drug information services to address adverse drug effects, is essential. Furthermore, incorporating pharmacist assessment sheets into patient charts for evaluation and follow-up of drug therapy would be beneficial.
Interestingly, reduced ejection fraction was not identified as a predictor of HF mortality in our study. However, lower LVEF has been associated with poor HF treatment outcomes in Angola (32). This discrepancy may be related to differences in cut-off points for LVEF and the etiologies of HF across countries, which can influence mortality rates beyond just reduced ejection fraction. In our study, the three most common causes of HF were hypertensive heart disease, coronary artery disease, and dilated cardiomyopathy (25). In addition, patients with reduced ejection fraction often receive special attention in clinical practice, which may contribute to a lower mortality rate in Ethiopia.
The implications of these findings underscore the need for a multifaceted approach to managing HF in Ethiopia. Addressing the social determinants of health, such as smoking cessation and access to medications, is crucial for improving patient outcomes. Public health campaigns that aim to educate the community about the risks of smoking and the importance of medication adherence could significantly improve HF management. Moreover, enhancing healthcare infrastructure to improve access to specialized care and training healthcare providers could lead to better treatment adherence and outcomes.
This review calls for both governmental and non-governmental interventions to reduce mortality associated with HF. The study aims to assist policymakers by providing evidence to assist in the planning of various interventions specific to decreasing mortality from HF. Moreover, it will aid the government in developing standard treatment guidelines and evaluating the effectiveness of their programs for HF patients. This review will also guide clinical practice by providing appropriate treatments and addressing factors associated with poor HF outcomes, such as mortality. Finally, our study will serve as a benchmark for future researchers conducting interventional studies aimed at reducing HF hospitalization and mortality.
This systematic review and meta-analysis has several limitations that should be acknowledged. First, the included studies varied in design, sample size, and methodology, which may affect the generalizability of the findings. For instance, many studies were conducted in specific regions or hospitals, potentially limiting the applicability of the results to the broader Ethiopian population. In addition, the reliance on observational studies may introduce biases related to data collection and reporting, particularly regarding self-reported measures of smoking and medication adherence.
Moreover, the quality of the included studies varied, as indicated by the quality assessment. While most studies were deemed high quality, some were assessed as moderate quality, which may influence the robustness of the pooled estimates. Furthermore, the potential for publication bias exists as studies with negative results may be less likely to be published. This could skew the overall prevalence and predictors of poor HF treatment outcomes. Finally, the cross-sectional nature of some of the studies limited the ability to establish causal relationships between the identified predictors and treatment outcomes, suggesting that further longitudinal research is needed to clarify these associations.
Conclusion
In this systematic review and meta-analysis, the prevalence of poor HF treatment outcomes in Ethiopia was found to be concerningly high. This study identified that smoking cigarettes and the presence of medication-related problems were significantly associated with adverse HF treatment outcomes. To address these critical issues, it is essential to implement educational interventions through community outreach programs aimed at raising awareness about the detrimental impact of smoking on mortality among patients with HF. In addition, healthcare workers should receive training focused on rational drug use to enhance treatment adherence and optimize patient outcomes. Furthermore, establishing pharmaceutical care services in Ethiopia is vital to effectively manage the adverse effects of medications and improve the overall care for patients with HF. By addressing these factors, we can significantly improve treatment outcomes and reduce mortality associated with HF in the region.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
FB: Investigation, Methodology, Writing – original draft, Writing – review & editing. LT: Investigation, Writing – review & editing. GF: Methodology, Writing – review & editing. GD: Software, Writing – original draft. DD: Supervision, Writing – review & editing. DS: Data curation, Investigation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We would like to thank all the authors of the studies included in this systematic review and meta-analysis.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ACEI, angiotensin-converting enzyme inhibitors; AOR, adjusted odds ratio; BB, beta-blocker; CI, confidence interval; HF, heart failure; LVEF, left ventricular ejection fraction; MRA, mineralocorticoid receptor antagonists; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
References
1. Savarese G, Lund LH. Global public health burden of heart failure. Card Fail Rev. (2017) 3(1):7. doi: 10.15420/cfr.2016:25:2
2. Abdulkadir MB, Ibraheem RM, Issa A, Suberu HD, Owolabi BI, Alabi K. Prevalence, etiology, and fatality rates of childhood heart failure in Nigeria: a systematic review and meta-analysis. Int J Health Sci. (2023) 17(1):53.
3. Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. (2013) 62(16):e147–239. doi: 10.1016/j.jacc.2013.05.019
4. James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national incidence, prevalence and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990 2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2018) 392(10159):1789–858. doi: 10.1016/S0140-6736(18)32279-7
5. Tukeni KN, Regassa RJ, Abera EG, Geleta MN. The prevalence and correlates of hospital admission of patients with heart failure admitted to Jimma Medical Center, Ethiopia. PAMJ Clinical Medicine. (2023) 12:28. doi: 10.11604/pamjcm.2023.12.28.40297
6. Prattipati S, Sakita FM, Kweka GL, Tarimo TG, Peterson T, Mmbaga BT, et al. Heart failure care and outcomes in a Tanzanian emergency department: a prospective observational study. PLoS One. (2021) 16(7):e0254609. doi: 10.1371/journal.pone.0254609
7. Meshesha MD, Kabthymer RH, Abafogi MM. Mortality and its associated factors among hospitalized heart failure patients: the case of South West Ethiopia. Cardiol Res Pract. (2021) 2021:1–8. doi: 10.1155/2021/5951040
8. Kimani KN, Murray SA, Grant L. Multidimensional needs of patients living and dying with heart failure in Kenya: a serial interview study. BMC Palliat Care. (2018) 17(1):1–8. doi: 10.1186/s12904-018-0284-6
9. Buddeke J, Valstar GB, Van Dis I, Visseren FL, Rutten FH, Den Ruijter HM, et al. Mortality after hospital admission for heart failure: improvement over time, equally strong in women as in men. BMC Public Health. (2020) 20(1):36. doi: 10.1186/s12889-019-7934-3
10. Ang N, Chandramouli C, Yiu K, Lawson C, Tromp J. Heart failure and multimorbidity in Asia. Curr Heart Fail Rep. (2023) 20(1):24–32. doi: 10.1007/s11897-023-00585-2
11. Assefa E, Tegene E, Abebe A, Melaku T. Treatment outcomes and associated factors among chronic ambulatory heart failure patients at Jimma Medical Center, South West Ethiopia: prospective observational study. BMC Cardiovasc Disord. (2023) 23(1):26. doi: 10.1186/s12872-023-03055-8
12. Bekele F, Tafese L, Demsash AW, Tesfaye H, Labata BG, Fekadu G. Adherence to selfcare practices and associated factors among heart failure patients in Ethiopia: a systematic review and meta-analysis. PLoS One. (2023) 18(8):e0288824. doi: 10.1371/journal.pone.0288824
13. Tigabe M, Fentahun A, Getawa S, Gelaye KA, Gebreyohannes EA. Clinical characteristics and in-hospital outcome of acute heart failure patients admitted to the medical ward of university of Gondar Comprehensive Specialized Hospital, Northwest Ethiopia. Vasc Health Risk Manag. (2021) 17:581–90. doi: 10.2147/VHRM.S322493
14. Bytyçi I, Bajraktari G. Mortality in heart failure patients. Anatol J Cardiol. (2015) 15(1):63–68. doi: 10.5152/akd.2014.5731
15. Mandi DG, Bamouni J, Yaméogo RA, Naïbé DT, Kaboré E, Kambiré Y, et al. Spectrum of heart failure in sub-Saharan Africa: data from a tertiary hospital-based registry in the eastern center of Burkina Faso. Pan Afr Med J. (2020) 36(1):30. doi: 10.11604/pamj.2020.36.30.19321
16. Lippi G, Sanchis-Gomar F. Global epidemiology and future trends of heart failure. AME Med J. (2020) 5:15. doi: 10.21037/amj.2020.03.03
17. Tirfe M, Nedi T, Mekonnen D, Berha AB. Treatment outcome and its predictors among patients of acute heart failure at a tertiary care hospital in Ethiopia: a prospective observational study. BMC Cardiovasc Disord. (2020) 20(1):16. doi: 10.1186/s12872-019-01318-x
18. Bekele F, Tafese L, Garbessa B, Tadasa S, Fekadu G. Burden and predictors of heart failure treatment outcomes in Ethiopia: a systematic review and meta-analysis protocol. PLoS One. (2023) 18(12):e0291686. doi: 10.1371/journal.pone.0291686
19. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br Med J. (2021) 372:n71. doi: 10.1136/bmj.n71
20. JBI. Meta-Analysis of Statistics. Assessment and Review Instrument (JBI Mastari). Adelaide: Joanna Briggs Institute (2006). p. 20032007.
21. Bogale K, Aderaw A. Clinical characteristics and in-hospital mortality in patients with acute heart failure at Dessie Referral Hospital, northeast Ethiopia. Abyssinia J Sci Technol. (2021) 6(1):33–7.
22. Hassen A, Assen M, Tadese M. Treatment outcome of heart failure patients admitted in Kemissie general hospital, northeast Ethiopia: retrospective study. Int J Curr Res. (2019) 11(10):7469–71. doi: 10.24941/ijcr.36842.10.2019
23. Kebede B, Getachew M, Molla Y, Bahiru B, Dessie B. Management, survival, and predictors of mortality among hospitalized heart failure patients at Debre Markos comprehensive specialized hospital, Northwest Ethiopia: prospective cohort study. SAGE Open Med. (2021) 9:20503121211057336. doi: 10.1177/20503121211057336
24. Beri B, Fanta K, Bekele F, Bedada W. Management, clinical outcomes, and its predictors among heart failure patients admitted to tertiary care hospitals in Ethiopia: prospective observational study. BMC Cardiovasc Disord. (2023) 23(1):4. doi: 10.1186/s12872-022-03008-7
25. Bekele F, Sheleme T, Tsegaye T, Parameswari SA, Syed MA, Tafese L, et al. Prevalence and risk factors of mortality among heart failure patients in low resource setting hospitals. A multicenter prospective observational study. Front Cardiovasc Med. (2024) 11:1429513. doi: 10.3389/fcvm.2024.1429513
26. Tegene E, Mekonin G, Dukessa G, Dube L, Tadesse I. Acute heart failure outcome and predictors of outcome among patients admitted to Jimma University Medical Center, Southwest Ethiopia (2024). doi: 10.21203/rs.3.rs-1906685/v1
27. Woldeyes E, Zewdu H, Abera H, Bayissa T, Sirgu S. Clinical characteristics and in hospital outcome of acute heart failure: a five-year experience at a tertiary care hospital in Ethiopia. Ethiop Med J. (2020) 58(1):21–8.
28. Moyehodie YA, Muluneh MW, Belay AT, Fenta SM. Time to death and its determinant factors among patients with chronic heart failure in Northwest Ethiopia: a retrospective study at selected referral hospitals. Front Cardiovasc Med. (2022) 9:817074.35600464
29. Bloomfield GS, Barasa FA, Doll JA, Velazquez EJ. Heart failure in sub-Saharan Africa. Curr Cardiol Rev. (2013) 9(2):157–73. doi: 10.2174/1573403X11309020008
30. Ogeng'o JA, Gatonga PM, Olabu BO, Nyamweya DK, Ong'era D. Pattern of congestive heart failure in a Kenyan paediatric population: cardiovascular topics. Cardiovasc J Afr. (2013) 24(4):117–20. doi: 10.5830/CVJA-2013-015
31. Abeya FC, Lumori BA, Akello SJ, Annex BH, Buda AJ, Okello S. Incidence and predictors of 6 months mortality after an acute heart failure event in rural Uganda: the Mbarara Heart Failure Registry (MAHFER). Int J Cardiol. (2018) 264:113–7. doi: 10.1016/j.ijcard.2018.03.110
32. Morais H, Alfredo A, Lopes I, Gonçalves MA. Etiology, clinical features, comorbidities and mortality in patients with acute heart failure. Experience of a tertiary public hospital in Angola. Cardiospace. (2023) 2(1):1. doi: 10.55976/cds.2202311211-11
33. Bekele F, Tsegaye T, Negash E, Fekadu G. Magnitude and determinants of drugrelated problems among patients admitted to medical wards of southwestern Ethiopian hospitals: a multicenter prospective observational study. PLoS One. (2021) 16(3):e0248575. doi: 10.1371/journal.pone.0248575
Keywords: treatment outcome, associated factors, Ethiopia, heart failure, prevalence
Citation: Bekele F, Tafese L, Fekadu G, Dube GN, Dugassa D and Samuel D (2024) Prevalence and predictors of poor heart failure treatment outcomes in Ethiopia: a systematic review and meta-analysis. Front. Cardiovasc. Med. 11:1434265. doi: 10.3389/fcvm.2024.1434265
Received: 6 June 2024; Accepted: 2 December 2024;
Published: 24 December 2024.
Edited by:
Pietro Scicchitano, ASLBari—Azienda Sanitaria Localedella provincia di Bari (ASL BA), ItalyReviewed by:
Marcellino Monda, University of Campania Luigi Vanvitelli, ItalyAdeseye Abiodun Akintunde, Ladoke Akintola University of Technology, Nigeria
Cristina Florescu, University of Medicine and Pharmacy of Craiova, Romania
Copyright: © 2024 Bekele, Tafese, Fekadu, Dube, Dugassa and Samuel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Firomsa Bekele, Zmlyb21zYWJla2VsZTIxQGdtYWlsLmNvbQ==
 Firomsa Bekele
Firomsa Bekele Lalise Tafese2
Lalise Tafese2 Ginenus Fekadu
Ginenus Fekadu Geleta Nenko Dube
Geleta Nenko Dube Dinka Dugassa
Dinka Dugassa