- Department of Nursing, The First Affiliated Hospital of Soochow University, Suzhou, China
Background: Venous thromboembolism (VTE) is a common complication after major orthopedic surgery. The venous foot pump (VFP) is an effective mechanical preventive measure against VTE in patients. However, the differences in effectiveness based on varying usage times of VFP remain unclear.
Objective: To explore the effectiveness of VFP with different usage times in preventing VTE in patients undergoing major orthopedic surgery.
Methods: Nine databases (PubMed, Web of Science, CINAHL, Embase, Cochrane Library, CBM, VIP, CNKI, and Wanfang) were searched to identify randomized controlled trials (RCTs) evaluating VFP interventions for VTE prevention in major orthopedic surgery patients. The risk of bias in each study was assessed using the Cochrane Collaboration tool. Meta-analysis was conducted using RevMan 5.3.
Results: A total of 36 RCTs involving 3,791 patients undergoing major orthopedic surgery were included. Meta-analysis revealed significant differences in VTE incidence between the VFP and blank control groups (RR = 0.27, 95% confidence interval CI: 0.19–0.38, P < 0.001) and between the VFP plus chemoprophylaxis and chemoprophylaxis alone groups (RR 0.39, 95% CI: 0.29–0.53, P < 0.001). However, no statistically significant difference was observed between the VFP and the LMWH groups (RR = 0.93, 95% CI: 0.54–1.61, P = 0.8). Subgroup analysis showed no significant difference in effectiveness based on different VFP usage durations (VFP vs. Blank: Chi-square = 0.54, P = 0.46, I2 = 0%; VFP Plus chemoprophylaxis vs. chemoprophylaxis alone: Chi-square = 1.93, P = 0.86, I2 = 0%).
Conclusion: The current evidence indicates that VFP significantly reduces the incidence of postoperative VTE in patients undergoing major orthopedic surgery. VFP can be considered an add-on strategy to LMWH for patients at low risk of bleeding and an alternative strategy to LMWH in patients at high risk of bleeding. This study found no significant difference in effectiveness between various VFP usage interventions. Future research should focus on economic cost-effectiveness and patient acceptance to help policymakers determine the most efficient usage duration, providing practical guidance for thromboprophylaxis.
1 Introduction
Venous thromboembolism (VTE) contains deep vein thrombosis (DVT) and pulmonary thromboembolism (PTE). DVT refers to abnormal blood clotting in the deep veins, usually in the lower limbs (1), leading to potential dysfunction or disability. PTE occurs when a blood clot dislodges and travels through the bloodstream to the pulmonary artery. According to risk assessments for VTE in orthopedic surgery patients (2), those undergoing major orthopedic surgeries, such as hip arthroplasty (HA), knee arthroplasty (KA), and hip fracture surgery (HFS) (3), are at high risk for VTE. Studies (4) have revealed that without preventive measures, the incidence of DVT after total HA ranges from 20.6% to 47.1% and from 30.8% to 58.2% after total KA. VTE often lacks typical clinical symptoms but significantly impacts patients’ quality of life and can result in perioperative mortality (2). Therefore, early screening and prevention are crucial in VTE prevention (5, 6).
The guidelines (2) strongly recommend implementing effective preventive measures in patients undergoing major orthopedic surgery to reduce the incidence and mortality of VTE, alleviate patient suffering, and reduce healthcare costs. Current preventive measures for VTE in major orthopedic patients mainly include physical and drug prevention and basic preventive measures. Physical prevention is an essential strategy, serving as a necessary supplement and alternative to drug prevention in specific situations. The combination of physical and drug prevention addresses multiple aspects of Virchow's triad, thus synergistically reducing the occurrence of VTE (7). Drug prevention primarily involves using anticoagulant drugs such as LMWH, Xa factor inhibitors, and vitamin K antagonists, which can inhibit the coagulation process and reduce blood hypercoagulability. Physical prevention measures use pressure to accelerate blood flow in the lower limbs, reducing blood stasis and significantly reducing the occurrence of postoperative lower limb DVT while minimizing bleeding risks. The guidelines for the prevention and treatment of VTE recommend physical prevention methods for thrombosis prevention in patients categorized as moderate and high risk for VTE, highlighting the generalizability and importance of physical prevention.
Similarly, venous foot pump (VFP) is a common mechanical precaution, and compared to graduated compression stockings (GCS) and intermittent pneumatic compression devices (IPCD), it offers the advantages of better effectiveness and ease of wear (8–13). While research on the effectiveness of VFP in preventing VTE in major orthopedic surgery patients continues to be published, there remains some controversy over the conclusions. Numerous studies have demonstrated that VFP can effectively prevent VTE in orthopedic surgery patients (14–16). However, Pitto and colleagues (17, 18) have revealed that compared to Low molecular weight heparin (LMWH), VFP does not significantly differ in preventing postoperative VTE in these patients. Moreover, the differences in the effects of VFP intervention at different usage times remain unclear, and researchers hold varying views on the optimal duration of VFP use (14, 16, 19, 20). For example, the consensus among experts in the mechanical prevention of VTE (9) suggests that IPCD should be used for at least 18 h per day. For patients who are completely immobilized, the daily usage time should be extended as much as possible. However, the usage time of VFP is not specified. Windish and colleagues (17, 19) demonstrated that continuous VFP application for 24 h can reduce the incidence of postoperative VTE in orthopedic surgery patients. Conversely, several studies (16, 20, 21) have used VFP intervention at a usage time of 30 min twice a day, showing an effective reduction of postoperative VTE in these patients. Based on the current studies, the effectiveness of VFP in postoperative VTE prevention in patients undergoing major orthopedic surgery and the optimal usage time of intervention remains to be further examined.
Therefore, this study used a systematic evaluation method to assess the effectiveness of VFP in preventing postoperative VTE in orthopedic surgery patients. It also compared and analyzed studies on VFP intervention at different usage times to provide a reference basis for clinical decision-making.
2 Methods
This study followed the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) statement. The PRISMA checklist is shown in Supplementary File 1 (22).
2.1 Search strategy
The following electronic databases were systematically searched from their inception until September 2023: PubMed, Embase, CINAHL, Cochrane Library, Web of Science, and four Chinese databases (CBM, CNKI, VIP, and WanFang). Searches in each database were performed using a combination of subject terms and free terms. The search terms included VTE (“venous thromboembolism,” “venous thrombosis,” “phlebothrombosis,” “deep venous thrombosis,” “DVT”), major orthopedic surgery (“arthroplasty,” “replacement,” “hip fracture surgery,” “orthopedic/orthopaedic,” “fracture,” “joint prosthesis implantation,” “orthopedic surgery”), VFP (“venous foot pump,” “A-V impulse system”), and RCT (“randomized controlled trial,” “randomized”). The complete search strategy for the PubMed database is provided in the Supplementary File 2).
2.2 Inclusion and exclusion criteria
The inclusion criteria for the literature were as follows: (1) Study population (P): patients undergoing major orthopedic surgery (including hip/knee arthroplasty and surgeries for hip fractures such as intertrochanteric fractures, subtrochanteric fractures, femoral neck fractures, femoral head fractures, and acetabular fractures); (2) intervention (I): the experimental group receiving VFP therapy; (3) control (C): the group receiving only anticoagulant therapy or serving as the blank control group; (4) outcome measures (O): incidence of DVT/PTE; (5) study type (S): randomized controlled trials (RCTs).
The exclusion criteria for the literature were as follows: (1) Studies with duplicate outcomes; (2) studies with incomplete or unextractable data; (3) studies with low quality.
2.3 Study selection and data extraction
Two researchers independently screened the literature based on the inclusion and exclusion criteria and extracted data from articles that met the inclusion criteria. The extracted data primarily included the first author, country, publication year, sample size, gender and age of the study subjects, intervention measures (intervention content and usage time), and outcome indicators. In case of any disagreements, they consulted a third researcher to reach the final decision.
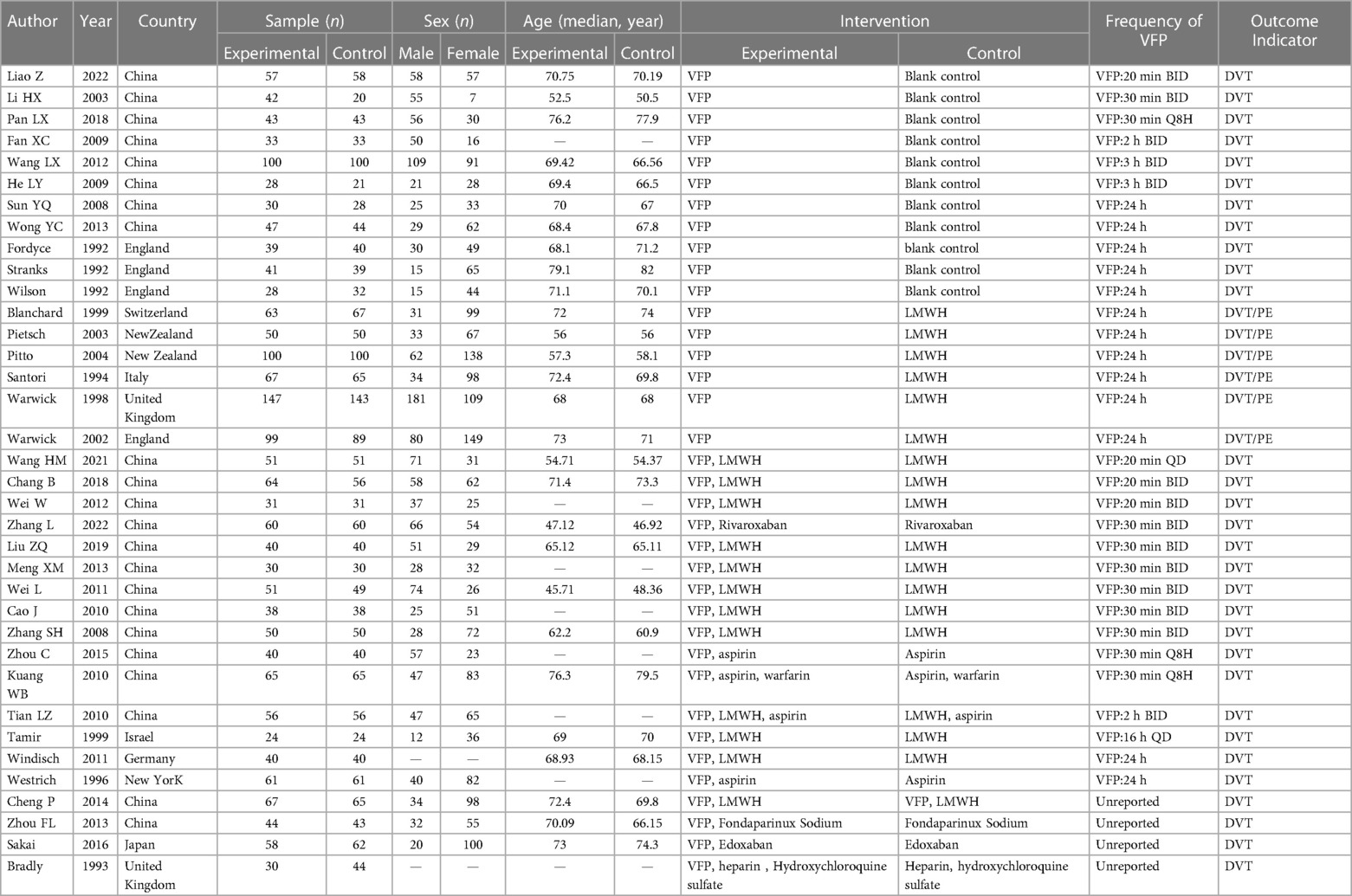
2.4 Quality appraisal
The two researchers used the Cochrane risk of bias assessment tool (23) to evaluate the quality in seven aspects: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessors, completeness of outcome data, selective outcome reporting, and other biases. Each aspect was evaluated as low risk of bias, unclear risk of bias, or high risk of bias.
2.5 Data analysis
Data analysis was performed using the RevMan 5.3 software provided by the Cochrane Library. The relative risk (RR) and a 95% confidence interval (CI) from different studies were synthesized. Heterogeneity among the included studies was assessed using the Cochrane Q test and the calculation of the I2 value. If there was no statistically significant heterogeneity among the studies (I2 ≤ 50%, P ≥ 0.10), a fixed-effects model was selected for the meta-analysis. Otherwise, a random-effects model was used. If there was statistically significant heterogeneity (I2 > 50%, P < 0.10), subgroup analysis and sensitivity analysis will be used to explore the potential sources of heterogeneity. Publication bias was assessed using a funnel plot and Egger's test for studies with a sample size of 10 or more (24). A p-value of less than 0.05 was considered significant.
3 Results
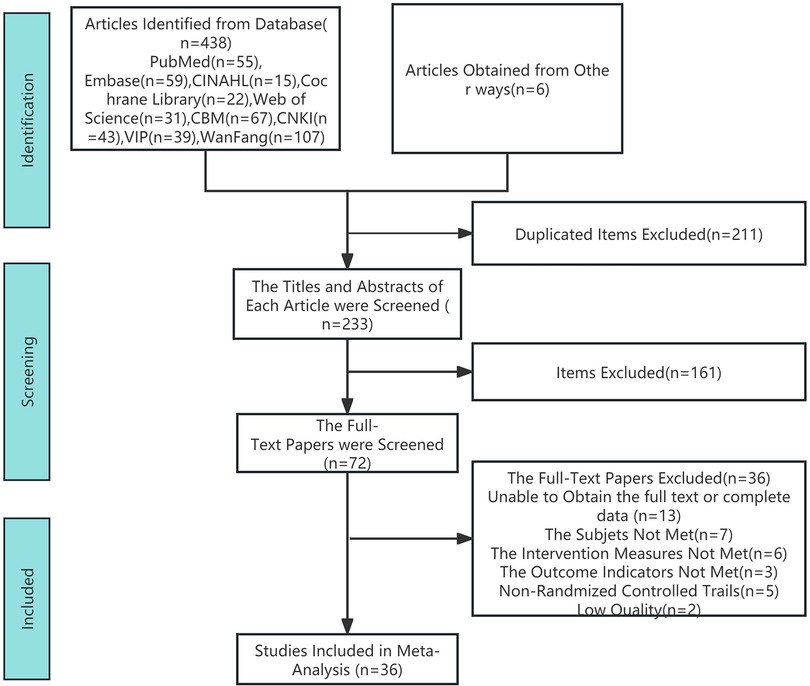
3.1 Search outcomes
After reviewing the full texts, 36 articles were included in the final analysis (Figure 1).
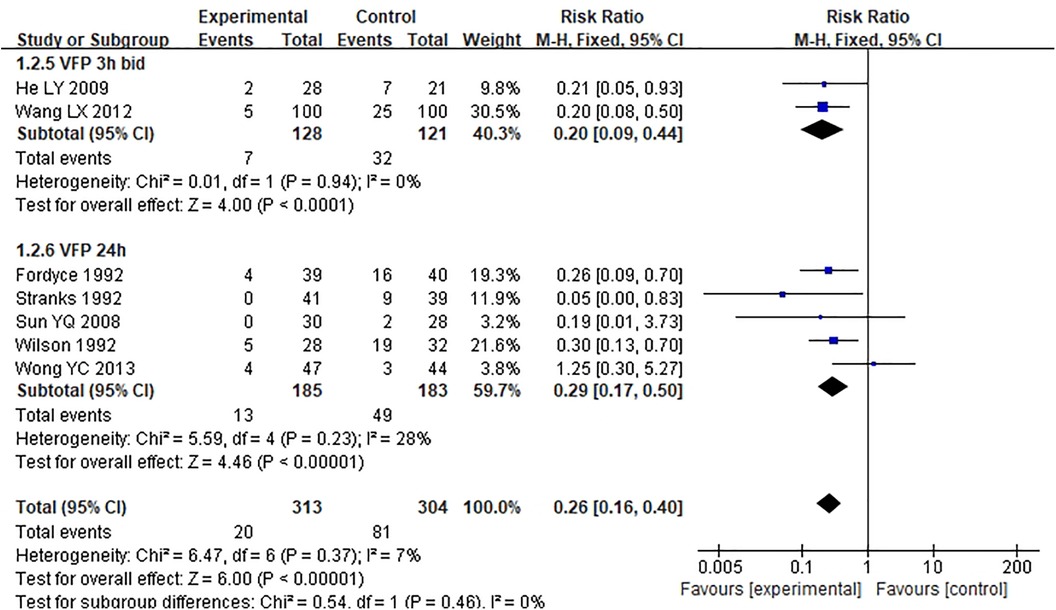
3.2 Characteristics of included studies
The basic characteristics of the 36 included articles are shown in Table 1. A total of 3,791 patients undergoing major orthopedic surgery were included in the studies. The methodological quality and risk of bias assessment of the included studies are displayed in Figure 2.
3.3 Meta-analysis results
3.3.1 Comparison of the incidence of DVT in patients with VFP alone group and blank control group
Eleven studies (15, 25–34) compared the DVT incidence between VFP and blank control group. The results depicted a significant difference in the incidence of postoperative DVT between the two groups of orthopedic surgery patients (pooled RR = 0.27, 95% CI: 0.19–0.38, P < 0.001; I2 = 0%, P = 0.59) (Figure 3A).
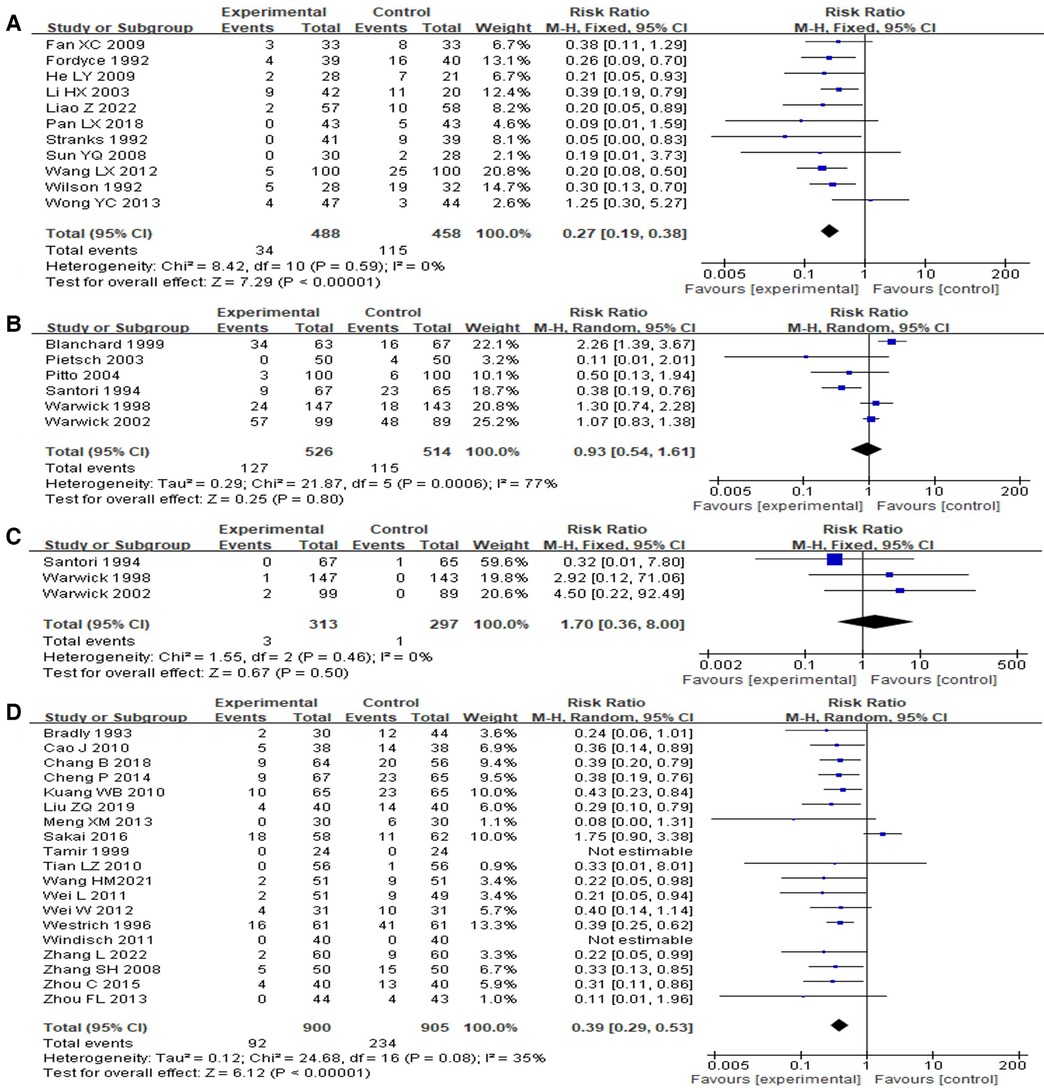
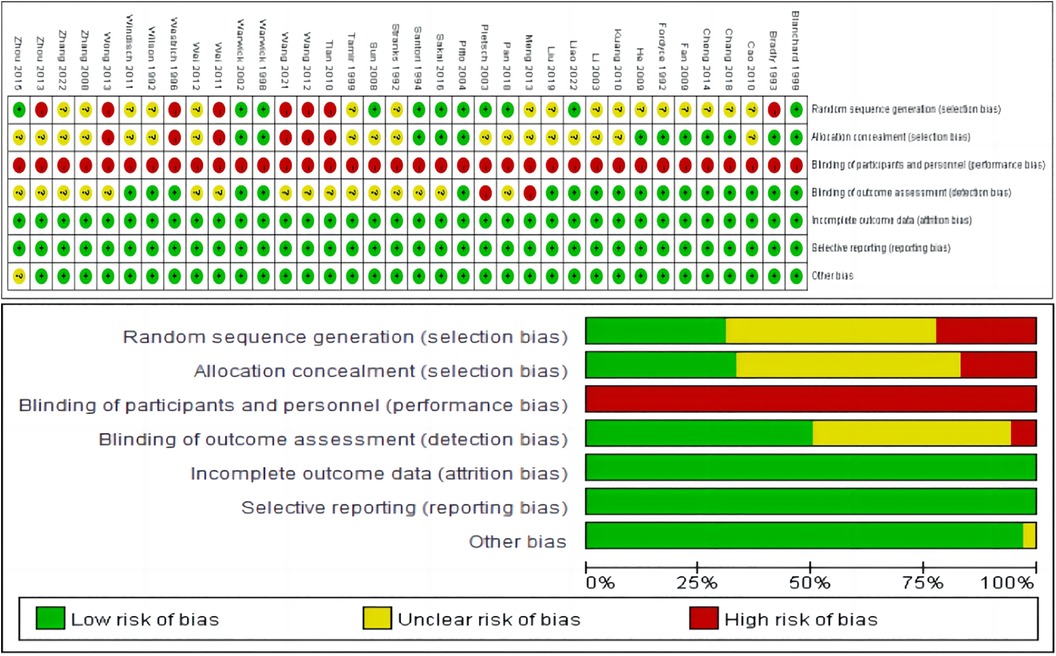
Figure 3. Forest map of VTE prevention effect between VFP group and control group [(A) VFP versus blank control; (B) VFP versus LMWH (outcome: DVT); (C) VFP versus LMWH (outcome: PTE); (D) VFP plus chemoprophylaxis versus chemoprophylaxis alone].
Among the 11 studies, there were 2 different VFP intervention usage times (3 h BID, 24 h). Subgroup analysis of the two usage times showed that the RR values were 0.20 (3 h BID), 0.29 (24 h) in order from low to high. However, there was no statistical significance among the subgroups (Chi-square = 0.54, P = 0.46, I2 = 0%) (Figure 4).
3.3.2 Comparison of the incidence of DVT in patients with VFP group and LMWH group
Six studies (17, 18, 35–38) compared the incidence of DVT between the VFP group (24 h) and the LMWH group. The results indicated a non-significant difference in the incidence of postoperative DVT between the VFP group and the LMWH group in orthopedic surgery patients (RR = 0.93, 95% CI: 0.54–1.61, P = 0.8; I2 = 77%, P = 0.0006) (Figure 3B).
Three of the six studies (36–38) compared the incidence of PTE between the VFP group (24 h) and the LMWH group. The results revealed a non-significant difference in the incidence of postoperative PTE between the VFP group and the LMWH group in orthopedic surgery patients (pooled RR = 1.7, 95% CI: 0.36–8.00, P = 0.5; I2 = 0%, P = 0.46) (Figure 3C).
3.3.3 Comparison of the incidence of DVT in patients with VFP plus chemoprophylaxis group and chemoprophylaxis alone group
A total of 19 studies (14, 16, 19–21, 39–52) were included in the meta-analysis comparing the incidence of DVT between the group receiving VFP combined with anticoagulant drugs and the group receiving anticoagulant drugs alone. The results showed a significant difference in the incidence of postoperative DVT between the two groups of orthopedic patients [RR = 0.39, 95% CI (0.29, 0.53), P < 0.001; I2 = 35%, P = 0.08] (Figure 3D).
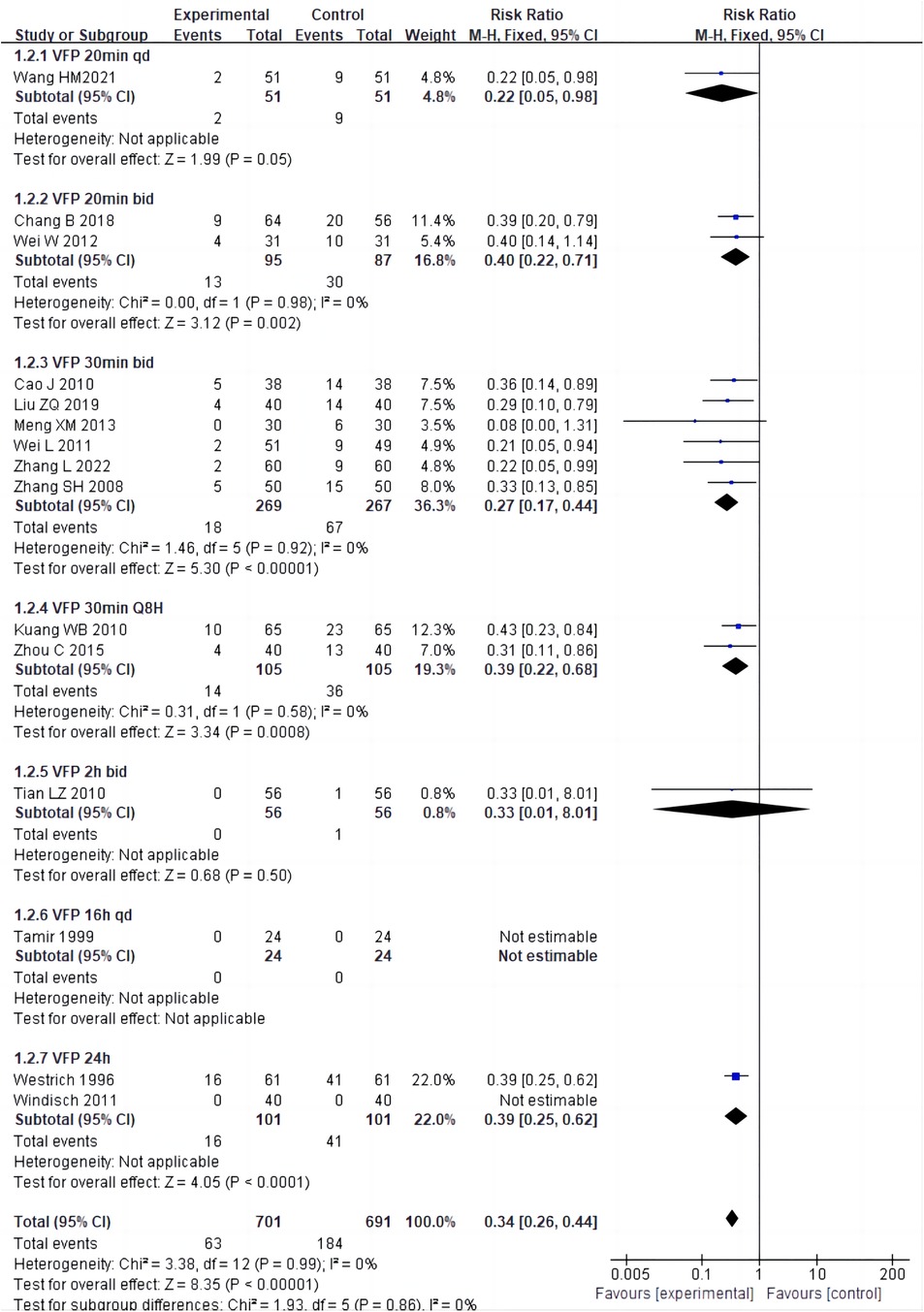
Among the 15 studies (16, 19–21, 40, 41, 43–51), there were 7 different usage times of VFP intervention (20 min once daily, 20 min twice daily, 30 min twice daily, 30 min every eight hours, two hours twice daily, 16 h once daily, 24 h). Subgroup analysis of the seven usage times showed that the RR values were 0.22 (20 min QD), 0.27 (30 min BID), 0.33 (2 h BID), 0.39 (30 min Q8 H), 0.39 (24 h), 0.40 (20 min BID) and “not estimable” (16 h QD). However, there was a non-significant difference among the subgroups (Chi-square = 1.93, P = 0.86, I2 = 0%) (Figure 5).
3.3.4 Sensitivity analysis and publication bias
Sensitivity analysis disclosed that the results were robust. Funnel plot and Egger's test were performed to analyze publication bias for the 11 studies comparing the VFP group with the blank control group and the 19 studies comparing the VFP combined with the anticoagulant drugs group with the anticoagulant drugs only group. The results were non-significant in publication bias for the VFP vs. control group (t = –1.21, P = 0.258, P > 0.05) and the VFP combined with anticoagulant drugs vs. anticoagulant drugs only group (t = –2.02, P = 0.062, P > 0.05) (Figure 6).

Figure 6. Funnel plot [(A) VFP versus blank control; (B) VFP plus chemoprophylaxis versus chemoprophylaxis alone].
4 Discussion
4.1 Effectiveness of VFP
The meta-analysis results of this study indicated that VFP has significantly prevented postoperative VTE in patients undergoing major orthopedic surgery. This finding is consistent with Zhang and colleagues (53) and emphasizes the critical role of VFP in reducing postoperative VTE risk in orthopedic surgery patients. VFP stimulates the body's “physiological foot pump” and generates high-speed pulsatile blood flow similar to cardiac function. This mechanism rapidly impacts the plantar region, creating a pulsatile acceleration state similar to walking. It increases blood flow velocity, prevents clotting, and avoids blood stasis and thrombus formation in the vascular endothelium. Given its low risk of bleeding, VFP can be an effective alternative to pharmacological prevention (54).
4.2 Effect of combined use of VFP and anticoagulant drugs
The research findings highlighted that combining VFP with anticoagulant drugs provides better prevention of postoperative DVT in orthopedic surgery. VFP not only promotes blood flow in the lower extremities but also stimulates the synthesis and release of plasminogen activators in endothelial cells, activating plasmin and facilitating fibrinolysis, preventing blood coagulation (55). Anticoagulant drugs such as rivaroxaban prevent thrombosis by directly inhibiting the activity of clotting factor Xa to prevent platelet activation and cross-binding of clotting proteins (56). When used with anticoagulant drugs, VFP complements their mechanisms, jointly preventing venous thrombosis and more effectively reducing the incidence of VTE than anticoagulant drugs alone. Therefore, the combination of VFP and anticoagulant drugs may effectively reduce postoperative VTE in orthopedic surgery patients (57), with VFP serving as a necessary complement to drug prevention.
4.3 Comparison between VFP and LMWH
Meta-analysis results show no significant difference in the effectiveness of VFP and LMWH in preventing postoperative VTE in orthopedic surgery patients. Although VFP and LMWH may operate through different mechanisms, their ultimate goal is to reduce blood stasis and promote blood circulation. LMWH reduces thrombus formation by inhibiting coagulation factor activity and increasing the activity of anticoagulant protein C (58). Conversely, VFP promotes blood flow through movement and pressure application, preventing venous blood stasis (59). Due to these similar mechanisms, VFP and LMWH are comparably effective in preventing postoperative VTE. Therefore, VFP can be considered as an alternative strategy to LMWH in patients at high risk of bleeding.
4.4 Comparison of effects between different usage times of VFP intervention
Subgroup analysis revealed non-significant differences in the effects of different VFP usage times, whether combined with anticoagulant drugs or not. This may be linked to the small number of studies with varied VFP usage durations included in this analysis. Among these, the frequencies of “30 min BID” and “24 h” were represented in about six studies, while other VFP durations were included in only one to two studies. Moreover, individual patient differences, implementation of the intervention, and duration may contribute to variability in the results, affecting their statistical significance.
5 Limitations
The scope and variety of VFP intervention times included in this study were not comprehensive, and the impact of the VFP intervention duration was not thoroughly examined. Additionally, the quality of the included literature was mostly moderate. Therefore, a more comprehensive multicenter, large sample, high-quality studies of VFP intervention with varying usage durations are needed to verify these findings.
6 Conclusions
Based on the current evidence, VFP can effectively prevent the occurrence of postoperative VTE in patients undergoing major orthopedic surgery. Combining VFP with drugs provides even better prevention. VFP can be considered an add-on strategy to LMWH for patients at low risk of bleeding and an alternative strategy to LMWH in patients at high risk of bleeding. Subgroup analysis revealed a non-significant difference in the effectiveness of VFP interventions with different usage durations. Future studies should conduct more comprehensive comparative research on VFP intervention with varying use times to help decision-makers choose the most effective treatment duration with limited resources, providing reference and practical guidance for thromboprophylaxis.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
YT: Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Writing – original draft, Writing – review & editing. RY: Data curation, Formal Analysis, Writing – original draft, Writing – review & editing. MN: Writing – review & editing. LX: Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
This work was supported by research project of Suzhou Municipal Health Commission (KJXW-2022003), The National Natural Science Foundation of China (No. 72104168), and Suzhou 32nd Batch of Science and Technology Development Plan (Medical and Health Technology Innovation) (2021) (No. SKJY2021036).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2024.1408334/full#supplementary-material
References
1. Giuliano KK, Pozzar R, Hatch C. Thromboprophylaxis after hospitalization for joint replacement surgery. J Healthc Qual. (2019) 41:384–91. doi: 10.1097/JHQ.0000000000000204
2. Chinese Orthopaedic Association. Prevention of venous thromboembolism after major orthopaedic surgery. Chin J Orthopaed. (2016) 2:65–71. doi: 10.3760/cma.j.issn.0253-2352.2016.02.001
3. Commission OEGO, Association OEPC, Promotion OEPC. Expert consensus on the prevention and treatment of perioperative venous thromboembolism in major orthopaedic surgery in enhanced recovery after surgery program. Chin J Bone Joint Surg. (2022) 15:754–62. doi: 10.3969/j.issn.2095-9958.2022.10.06
4. Mengchun Z, Yujin Y, Ping W, Xingwei Y, Huanhuan Z, Sumin W, et al. Effcacy of intermittent pneumatic compression devices with different treatment duration on proventing deep vein thrombosis after joint replacement. Chinese Nurs Res. (2020) 34:329–32. doi: 10.12102/j.issn.1009-6493.2020.02.032
5. Segon YS, Summey RD, Slawski B, Kaatz S. Surgical venous thromboembolism prophylaxis: clinical practice update. Hosp Pract (1995). (2020) 48:248–57. doi: 10.1080/21548331.2020.1788893
6. Speth J. Guidelines in practice: prevention of venous thromboembolism. AORN J. (2023) 118:321–8. doi: 10.1002/aorn.14019
7. Douketis JD, Spyropoulos AC, Murad MH, Arcelus JI, Dager WE, Dunn AS, et al. Perioperative management of antithrombotic therapy: an American college of chest physicians clinical practice guideline. Chest. (2022) 162(5):e207–43. doi: 10.1016/j.chest.2022.07.025
8. Sachdeva A, Dalton M, Lees T. Graduated compression stockings for prevention of deep vein thrombosis (review. Cochrane Database Syst Rev. (2018) 11:CD1484. doi: 10.1002/14651858.CD001484.pub4
9. China Health Promotion Foundation Committee. Chinese Expert consensus on mechanical prevention of venous thromboembolism. Nat Med J Chin. (2020) 100:484–92. doi: 10.3760/cma.j.issn.0376-2491.2020.07.002
10. Kakkos S, Kirkilesis G, Caprini JA, Geroulakos G, Nicolaides A, Stansby G, et al. Combined intermittent pneumatic leg compression and pharmacological prophylaxis for prevention of venous thromboembolism. Cochrane Database Syst Rev. (2022) 1:CD005258. doi: 10.1002/14651858.CD005258.pub4
11. Liu P, Liu J, Chen L, Xia K, Wu X. Intermittent pneumatic compression devices combined with anticoagulants for prevention of symptomatic deep vein thrombosis after total knee arthroplasty: a pilot study. Ther Clin Risk Manag. (2017) 13:179–83. doi: 10.2147/TCRM.S129077
12. Pitto RP, Young S. Foot pumps without graduated compression stockings for prevention of deep-vein thrombosis in total joint replacement: efficacy, safety and patient compliance: a comparative, prospective clinical trial. Int Orthop. (2008) 32:331–6. doi: 10.1007/s00264-007-0326-9
13. Wang LQ, Zhang HY, Ning N, Chen JL, Zhou ZK, Liao X, et al. Application of transient pulse plantar venous pump in the prevention of deep venous thrombosis after hip and knee arthroplasty. Orthopedics. (2022) 13:441–6. doi: 10.3969/j.issn.1674-8573.2022.05.012
14. Sakai T, Izumi M, Kumagai K, Kidera K, Yamaguchi T, Asahara T, et al. Effects of a foot pump on the incidence of deep vein thrombosis after total knee arthroplasty in patients given edoxaban: a randomized controlled study. Medicine (Baltimore). (2016) 95:e2247. doi: 10.1097/MD.0000000000002247
15. Liao Z. Effect of plantar vein pump combined with predictive nursing in prevention of deep vein thrombosis in elderly patients with hip fracture after operation. Med Equip. (2022) 35:140–2. doi: 10.3969/j.issn.1002-2376.2022.16.054
16. Wang H, Jin H, Huang Y. Preventive effect of planar arteriovenous pump on lower extremity dvt after artificial femoral head replacement. J Vasc Endovasc Surg. (2021) 7:571–5. doi: 10.19418/j.cnki.issn2096-0646.2021.05.15
17. Pitto RP, Hamer H, Heiss-Dunlop W, Kuehle J. Mechanical prophylaxis of deep-vein thrombosis after total hip replacement a randomised clinical trial. J Bone Joint Surg Br. (2004) 86:639–42. doi: 10.1302/0301-620x.86b5.14763
18. Pietsch M, Kühle J, Hamer H, Pitto RP. Mechanical versus drug prevention of thrombosis after total hip endoprosthesis implantation. A randomized, controlled clinical study. Biomed Tech (Berl). (2003) 48:207–12. doi: 10.1515/bmte.2003.48.7-8.207
19. Windisch C, Kolb W, Kolb K, Grutzner P, Venbrocks R, Anders J. Pneumatic compression with foot pumps facilitates early postoperative mobilisation in total knee arthroplasty. Int Orthop. (2011) 35:995–1000. doi: 10.1007/s00264-010-1091-8
20. Zhang L, Wu WT. Effect of plantar vein pump on preventing deep vein thrombosis of lower extremity after artificial joint replacement. Med Equip. (2022) 35:126–7. doi: 10.3969/j.issn.1002-2376.2022.12.051
21. Liu ZQ, Zhu XP. Study on preventive nursing of deep vein thrombosis using plantar vein pump after orthopedic lower extremity joint replacement. Feet Health Care. (2019) 28:157–8. doi: 10.19589/j.cnki.issn1004-6569.2019.18.157
22. Page MJ, Mckenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The prisma 2020 statement: an updated guideline for reporting systematic reviews. Br Med J. (2021) 372:n71. doi: 10.1136/bmj.n71
23. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The cochrane collaboration’s tool for assessing risk of bias in randomised trials. Br Med J. (2011) 343:d5928. doi: 10.1136/bmj.d5928
24. Yin YK, Wang JL, Sun JZ. Therapeutic effect of different-frequency repetitive transcranial magnetic stimulations on post-stroke cognitive impairment: a meta-analysis. Chin J Tissue Eng Res. (2023) 27:3274–80. doi: 10.12307/2023.150
25. Fan X, Zhou D, Sun Z, Dong J. Preventive effect of foot a-v pump on lower limb dvt formation after acetabular fracture. Shandong Med J. (2009) 49:57–8. doi: 10.3969/j.issn.1002-266X.2009.14.026
26. Fordyce MJF, Ling RSM. A venous foot pump reduces thrombosis after total hip replacement. J Bone Joint Surg Br. (1992) 74:45–9. doi: 10.1302/0301-620x.74b1.1732264
27. He LY, Zeng ZF, Shen CH, He F. Effect of plantar arteriovenous pump in preventing venous embolization of lower extremities after total hip arthroplasty. Nurs Rehab J. (2009) 8:676–7. doi: 10.3969/j.issn.1671-9875.2009.08.021
28. Li HX, Jia WW, Qiu YM, Zou R. Clinical study of prevention of deep vein thrombsis by a foot sole pump. J Prac Med Tech. (2003) 10:486–7. doi: 10.3969/j.issn.1671-5098.2003.05.069
29. Pan L, Wu J. Observation of nursing intervention effect of plantar vein pump in preventing deep vein thrombosis after hip fracture in elderly patients. Elect J Pract Clin Nurs. (2018) 3:95. doi: 10.3969/j.issn.2096-2479.2018.41.075
30. Stranks GJ, Mackenzie NA, Grover ML, Fail T. The a-v impulse system reduces deep-vein thrombosis and swelling after hemiarthroplasty for hip fracture. J Bone Joint Surg Br. (1992) 74:775–8. doi: 10.1302/0301-620X.74B5.1527133
31. Sun YQ, Yang J. Effect of plantar dynamic pulse system on reducing swelling of affected limb after total hip/total knee arthroplasty. J Nurs. (2008) 15:59–61. doi: 10.3969/j.issn.1008-9969.2008.08.022
32. Wilson NV, Das SK, Kakkar VV, Maurice HD, Smibert JG, Thomas EM, et al. Thromboembolic prophylaxis in total knee replacement evaluation of the av impulse system. J Bone Joint Surg Br. (1992) 74:50–2. doi: 10.1302/0301-620X.74B1.1732265
33. Wong YC, Cheung HY, Li PH, Lee QJ, Wai YL, Wong CW. A prospective study of venous thromboembolic prophylaxis using foot pumps following total knee replacement in a Chinese population. J Orthop Trau Rehab. (2013) 17:9–12. doi: 10.1016/j.jotr.2012.04.002
34. Wang LX, Tang L, Tang Y, Zhou MY, Wei C. Application and effect of plantar arteriovenous pump in patients with hip fracture. J Nurs Adm. (2012) 12:835–6. doi: 10.3969/j.issn.1671-315X.2012.11.033
35. Blanchard J, Meuwly JY, Leyvraz PF, Miron MJ, Bounameaux H, Hoffmeyer P, et al. Prevention of deep-vein thrombosis after total knee replacement. Randomised comparison between a low-molecular-weight heparin (nadroparin) and mechanical prophylaxis with a foot-pump system. J Bone Joint Surg Br. (1999) 81:654–9. doi: 10.1302/0301-620x.81b4.9464
36. Santori FS, Vitullo A, Stopponi M, Santori N, Ghera S. Prophylaxis against deepvein thrombosis in total hipreplacement comparison of heparin and foot impulse pump. J Bone Joint Surg Br. (1994) 76B:579–83. doi: 10.1302/0301-620X.76B4.8027144
37. Warwick D, Harrison J, Glew D, Mitchelmore A, Peters TJ, Donovan J. Comparison of the use of a foot pump with the use of low-molecular-weight heparin for the prevention of deep-vein thrombosis after total hip replacement. A prospective, randomized trial. J Bone Joint Surg Am. (1998) 80:1158–66. doi: 10.2106/00004623-199808000-00009
38. Warwick D, Harrison J, Whitehouse S, Mitchelmore A, Thornton M. A randomised comparison of a foot pump and low-molecular-weight heparin in the prevention of deep-vein thrombosis after total knee replacement. J Bone Joint Surg Br. (2002) 84B:344–50. doi: 10.1302/0301-620x.84b3.12372
39. Bradley JG, Krugener GH, Jager HJ. The effectiveness of intermittent plantar venous compression in prevention of deep venous thrombosis after total hip arthroplasty. J Arthroplasty. (1993) 8:57–61. doi: 10.1016/s0883-5403(06)80108-7
40. Cao J, Wang JL, Zhang H, Wang LL. The combination of dynamic pulse system and low molecular weight heparin calcium for prevention of deep vein thrombosis after total knee arthroplasty. Chin J Restor Recons Surg. (2010) 24:538–40.
41. Chang B, Zhao JQ. Plantar vein pump prevents perioperative deep vein thrombosis in elderly patients with hip fractures. Zhejiang J Trau Surg. (2018) 23:151–3. doi: 10.3969/j.issn.1009-7147.2018.01.075
42. Cheng P, Zheng YB, Li L. Comparison of treatment methods for preventing thromboembolism after total hip arthroplasty. Zhejiang J Trau Surg. (2014) 19:479–80. doi: 10.3969/j.issn.1009-7147.2014.03.076
43. Kuang WB, Hou WM. Nursing care of plantar vein pump for prevention of deep vein thrombosis after hip fracture in elderly patients. Guangdong Med J. (2010) 31:1631–2. doi: 10.3969/j.issn.1001-9448.2010.12.054
44. Meng X, Wang DF. Nursing of plantar venous pump in the prevention of deep venous thrombosis after lower limb arthroplasty in department of orthopedics. J Clin Med Prac. (2013) 17:85–6. doi: 10.7619/jcmp.201302032
45. Tamir L, Hendel D, Neyman C, Eshkenazi AU, Ben-Zvi Y, Zomer R. Sequential foot compression reduces lower limb swelling and pain after total knee arthroplasty. J Arthroplasty. (1999) 14:333–8. doi: 10.1016/s0883-5403(99)90060-8
46. Tian LZ. Clinical observation of plantar dynamic pulse system for preventing deep vein thrombosis after lower limb joint replacement surgery. Mod Hosp. (2010) 10:46–8. doi: 10.3969/j.issn.1671-332X.2010.04.021
47. Wei L, Ouyang ZL, Chen YH, Chen WL, Yuan SQ, Ju CF. Observation on the effect of plantar vein pump in preventing deep venous thrombosis of lower extremity after major orthopaedic surgery. J Nurs. (2011) 18:50–1. doi: 10.3969/j.issn.1008-9969.2011.10.019
48. Wei W. Application of plantar vein pump in postoperative nursing of elderly hip fracture. Morden Nurse. (2012) 19:59–60. doi: 10.3969/j.issn.1006-6411-B.2012.06.034
49. Westrich GH, Sculco TP. Prophylaxis against deep venous thrombosis after total knee arthroplasty. Pneumatic plantar compression and aspirin compared with aspirin alone. J Bone Joint Surg Am. (1996) 78:826–34. doi: 10.2106/00004623-199606000-00004
50. Zhang SH, Wu XX, Lu YH. Efficacy of low molecular weight heparin combined with plantar pump in prevention of deep vein thrombosis after knee joint surface replacement. Nurs Prac Res. (2008) 5:62–3. doi: 10.3969/j.issn.1672-9676.2008.09.046
51. Zhou C. Evaluation of nursing effect of plantar vein pump for prevention of deep vein thrombosis in elderly patients after hip fracture. Guid China Med. (2015) 13:279. doi: 10.15912/j.cnki.gocm.2015.03.217
52. Zhou F, Xu G, Ren M, Shan J, Jiang H. Prevention of deep vein thrombosis of lower limbs after hip and knee arthroplasty with fonda hepatodecane sodium combined with plantar venous pump. Zhejiang J Trau Surg. (2013) 18:469–71. doi: 10.3969/j.issn.1009-7147.2013.04.008
53. Zhang HY, Ning N, Chen JL, Li PF, Liu Y, He CM. Meta analysis on effectiveness of venous foot pump in preventing deep vein thrombosis after hip and knee arthroplasty. Chongqing Med. (2021) 50:3713–9. doi: 10.3969/j.issn.1671-8348.2021.21.024
54. Fan D, Ouyang Z, Ying Y, Huang S, Tao P, Pan X, et al. Thromboelastography for the prevention of perioperative venous thromboembolism in orthopedics. Clin Appl Thromb Hemost. (2022) 28:10760296221077975. doi: 10.1177/10760296221077975
55. Pour AE, Keshavarzi NR, Purtill JJ, Sharkey PF, Parvizi J. Is venous foot pump effective in prevention of thromboembolic disease after joint arthroplasty: a meta-analysis. J Arthroplasty. (2013) 28:410–7. doi: 10.1016/j.arth.2012.08.003
56. Duggan ST, Scott LJ, Plosker GL. Rivaroxaban: a review of its use for the prevention of venous thromboembolism after total hip or knee replacement surgery. Drugs. (2009) 69(13):1829–51. doi: 10.2165/11200890-000000000-00000
57. Fey B, Meurer A. Thromboembolic prophylaxis in orthopaedics: update on the current S3 guideline, effective 2015. Orthopade. (2019) 48:629–42. doi: 10.1007/s00132-019-03759-w
58. Nimerta F, Faisal S, Reyaz N, Shah SU, Gurajala S, Khenhrani RR, et al. Comparison of the efficacy and safety of aspirin and low-molecular-weight heparin in patients with a fracture: a meta-analysis. Curēus. (2023) 15:e39025. doi: 10.7759/cureus.39025
Keywords: venous foot pump, major orthopedic surgery, venous thromboembolism, systematic review, meta-analysis
Citation: Tong Y, Ying R, Niu M and Xu L (2024) Effect of venous foot pump intervention on prevention of venous thromboembolism in patients with major orthopedic surgery: a systematic review and meta-analysis. Front. Cardiovasc. Med. 11:1408334. doi: 10.3389/fcvm.2024.1408334
Received: 1 April 2024; Accepted: 16 July 2024;
Published: 2 August 2024.
Edited by:
Emanuele Valeriani, Umberto 1 Hospital, ItalyReviewed by:
Ilaria Maria Palumbo, Sapienza University of Rome, ItalyArianna Pannunzio, Sapienza University of Rome, Italy
© 2024 Tong, Ying, Niu and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lan Xu, c3pzZ2tobHp3aDIwMjBAMTI2LmNvbQ==
†These authors have contributed equally to this work
 Yahui Tong†
Yahui Tong† Lan Xu
Lan Xu