- 1Cardiology Department, Bouake Teaching Hospital, Alassane Ouattara University, Bouake, Cote d'Ivoire
- 2Cardiology Department, Institute of Cardiology of Abidjan, Felix Houphouet-Boigny University, Abidjan, Cote d'Ivoire
Introduction: Normalization of blood pressure in hypertensive patients is a major challenge for practitioners. Knowledge of the factors associated with normalization of blood pressure could help optimize management of these hypertensive patients. In this study, we analysed the factors predictive of this in a population of hypertensive patients followed as outpatients in a specialised department.
Patients and methods: Retrospective and analytic study (January 2021–May 2022) of adult hypertensive patients over 40 years old who had been receiving antihypertensive treatment as outpatients in the Cardiology Department of the Bouake Teaching Hospital for at least 6 months. We studied the epidemiological and clinical parameters as well as the factors involved in the normalization of blood pressure in this population. Statistical analysis was performed using SPPS version 26 software (SPSS Inc., Chicago, IL, USA).
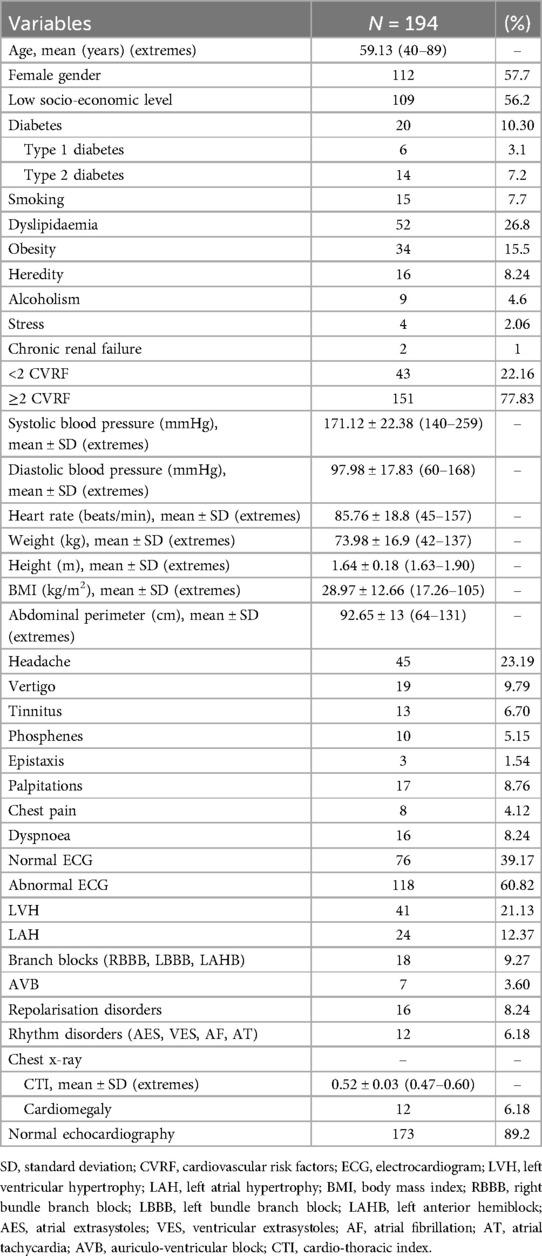
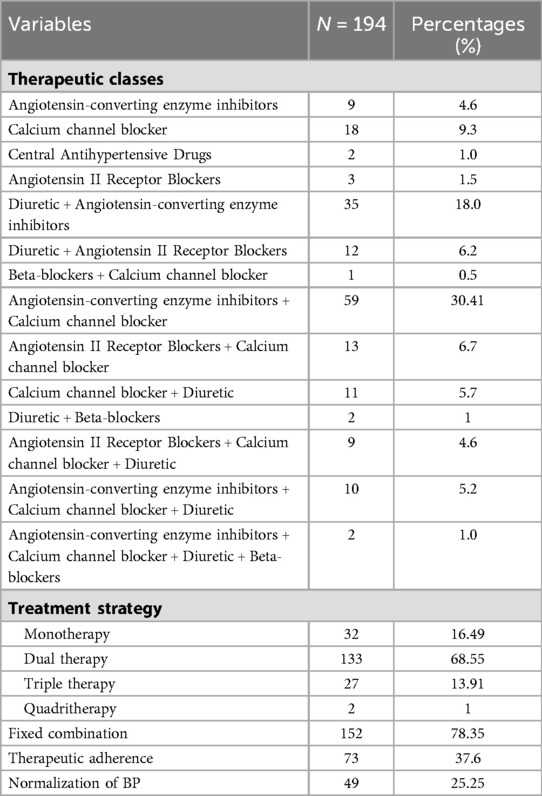
Results: We collected 194 patients records (57.7% women). The mean age was 59.13 years [extremes: 40–89 years]. One hundred and nine (56.2%) patients had a low socioeconomic status and 151 (77.83%) had at least 2 cardiovascular risk factors. The mean systolic blood pressure on admission was 171.12 ± 22.38 mmHg [extremes: 140–259 mmHg] and the mean diastolic blood pressure was 97.98 ± 17.83 mmHg [extremes: 60–168 mmHg]. First-line treatment consisted of dual anti-hypertensive therapy (n = 133; 68.55%) and fixed combination (n = 152; 78.35%). Only 25.25% (n = 49) of patients achieved normalization of blood pressure with therapeutic adherence estimated at 37.62% (n = 73). In multivariate analysis adjusted for anti-hypertensive treatment adherence, age (OR = 1.03; 95% CI = 1.002–1.059; p = 0.039), absence of alcoholism (OR = 9.48; 95% CI = 2.13–42.11; p = 0.003), number of cardiovascular risk factors <2 (OR = 1.52; 95% CI = 1.06–2.16; p = 0.021), normalization of uricemia (OR = 1.05; 95% CI = 1.00–1.11; p = 0.039) and natraemia (OR = 1.01; 95% CI = 1.00–1.03; p = 0.021), dual therapy (OR = 0.40; 95% CI = 0.18–0.90; p = 0.027), change in treatment for optimization (OR = 4.22; 95% CI = 1.71–10.37; p = 0.002), intellectual education (OR = 10.40; 95% CI = 4.31–25.10; p < 0.001) and health insurance (OR = 0.09; 95% CI = 0.04–0.21; p < 0.001) were the main factors predicting normalization of blood pressure.
Conclusion: Control of cardiovascular risk factors and compliance with treatment are the main factors in normalizing blood pressure.
Introduction
Worldwide, approximately 1.39 billion people have hypertension (1). Hypertension is a major public health problem and one of the main modifiable risk factors for cardiovascular disease (1–3). In recent decades, in the era of epidemiological transition, we have witnessed an upsurge in this global scourge in our developing countries, with increased morbidity and mortality (4, 5). The annual mortality rate from hypertension worldwide is estimated at around 10.4 million people (6, 7). This mortality is partly due to uncontrolled high blood pressure levels, which are responsible for multiple complications such as stroke, ischaemic heart disease, congestive heart failure, kidney disease and hypertensive emergencies (6, 8, 9). According to learned societies, normalized blood pressure (BP) is only achieved when the target BP of less than 130/80 mmHg is reached (10–13). In current medical practice, this target is difficult to achieve and blood pressure in general is not optimally controlled (4, 14). Only 1/3 of patients on pharmacological treatment achieve the recommended blood pressure targets (4). In addition, it has been shown that a prolonged and effective reduction in blood pressure (BP) of 2 mmHg in hypertensive patients significantly reduces the risk of cardiovascular events by up to 10%, and a reduction in systolic blood pressure of 20 mmHg reduces coronary heart disease and stroke mortality by 50% (15). Thus, normalizing blood pressure levels in hypertensive patients should be a major challenge for practitioners (1), and identifying the factors associated with normalization could help optimize the management of hypertension. In this study, we analysed the predictive factors of normalization of blood pressure in a population of hypertensive patients followed up on an outpatient basis.
Patients and methods
This was a retrospective and transversal study conducted over a 15-month period from January 01, 2021 to May 31, 2022. We included consecutively, adult hypertensive patients over 40 years of age, followed up on a short-term basis and receiving antihypertensive treatment on an outpatient basis in the cardiology department of Bouake University Hospital. These patients had undergone 3 successive consultations: (1) Initial consultation (M0), (2) Consultation at 3rd month (M3) and (3) Consultation at 6th month (M6). Short-term follow-up is defined as follow-up during the first year outside the 3-month initiation phase, in accordance with the ESH international guidelines (16). Patients with secondary arterial hypertension, hypertensive pregnant women and pregnant arterial hypertension were not included. Hypertension was defined as a BP ≥140/90 mmHg. For Patients aged 18–64 years old and 65–79 years old, the office Blood pressure (BP) was considered normalized when it's <130/80 mmHg and <140/80 mmHg respectively. For Patients aged ≥80 years old, the office Systolic Blood pressure (SBP) was considered normalized when it's in the 140–150 mmHg range (16). Blood pressure was measured using an OMRON M6 automatic electronic blood pressure monitor (15). Measurements were taken in the sitting position, using a cuff adapted to the patients' morphology. An average of 02 measurements was considered for analysis (17). The body mass index used as an index of obesity was calculated from the weight in kilograms divided by the square of the height in meters. Secondary education or above was considered intellectual education. Anyone living on less than $2.15 a day was considered in low socioeconomic status (18). We analyzed the epidemiological and clinical parameters and the factors influencing the normalization of blood pressure. To evaluate the therapeutic adherence, we used the indirect method (Self report) based on patient interview (19). Our therapeutic strategy was based on the decision-making algorithm recommended by the 2018 ESH guidelines (12). The data were collected on an individual survey form, filled in according to the various parameters studied, from the medical records. Statistical analysis was performed using Epi info 7 software and SPPS version 26 (SPSS Inc., Chicago, IL, USA). Qualitative values were expressed as percentages and quantitative variables as mean ± standard deviation. We used the Kolmogorov–Smirnov to assess the normally distribution of the different continous variables. Comparisons were made using ANOVA for quantitative variables and the Chi2 test for qualitative variables. The multivariate analysis consisted of a logistic regression analysis with adjustment of the variables studied for therapeutic adherence. A p-value < 0.05 was considered statistically significant.
Results
Epidemiological and clinical aspects
We collected 194 records from adult hypertensive patients. The mean age was 59.13 years [extremes: 40–89 years] and 57.7% were women. Epidemiological and clinical characteristics are listed in Table 1. One hundred and nine (56.18%) patients were in low socioeconomic status and 151 (77.83%) had at least 2 cardiovascular risk factors. Dyslipidaemia (26.8%), obesity (17.52%), diabetes (10.30%) and smoking (7.73%) were the most common cardiovascular risk factors in addition to hypertension. Blood pressure on admission averaged 171.12 (140–259) mmHg for systolic blood pressure and 97.46 (60–168) mmHg for diastolic blood pressure. The high blood pressure symptoms were present in 44.84%, including the headache (23.19%), vertigo (9.79%), tinnitus (6.70%) and phosphenes (5.15%).
The electrocardiogram was abnormal in 60.82% of cases, and the most common electrical abnormalities were left ventricular hypertrophy and left atrial hypertrophy in 21.13% and 12.37% of cases respectively.
Therapeutic aspects
First-line treatment consisted of dual antihypertensive therapy (n = 133; 68.55%) in fixed dose combination (n = 152; 78.35%). The therapeutic classes of antihypertensive agents most commonly used were the combination of Angiotensin-converting enzyme (ACE) inhibitors (ACE inhibitors) and calcium channel blockers (30.41%), followed by the combination of ACE inhibitors and diuretics (18%). Adherence was good in 37.62% of cases. The initial treatment was modified for optimization in 32.98% of cases (Table 2).
Factors predicting normalization of blood pressure
Only 25.25% of patients achieved normalization of blood pressure within 6 months, with therapeutic adherence estimated at 37.62%. About thirty-three percent (33%) of patients had their initial antihypertensive treatment modified for optimization (Figure 1).
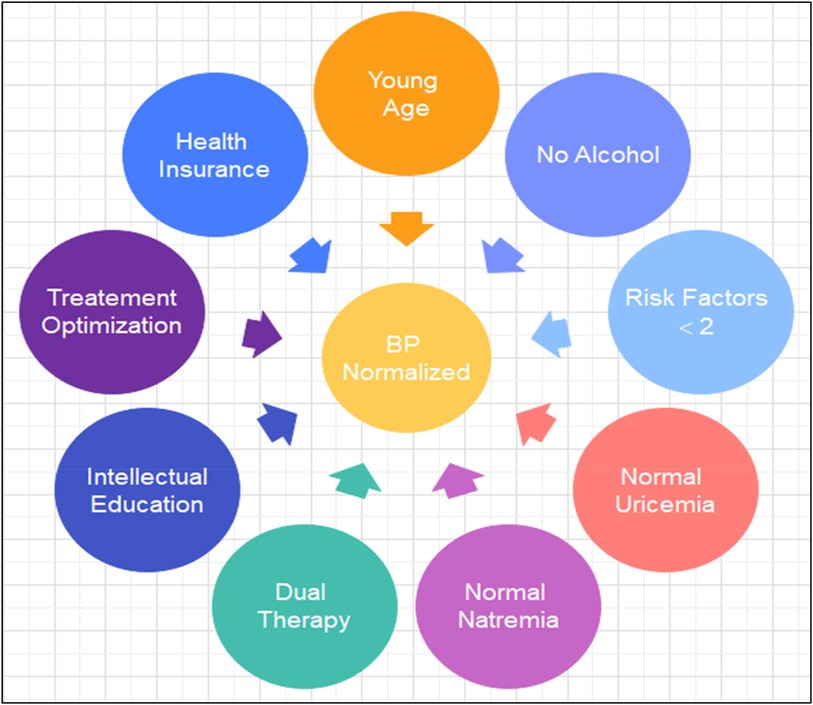
Figure 1. Illustrating Factors of Blood Pressure (BP) Normalization in Hypertensive Patients after short-term follow-up.
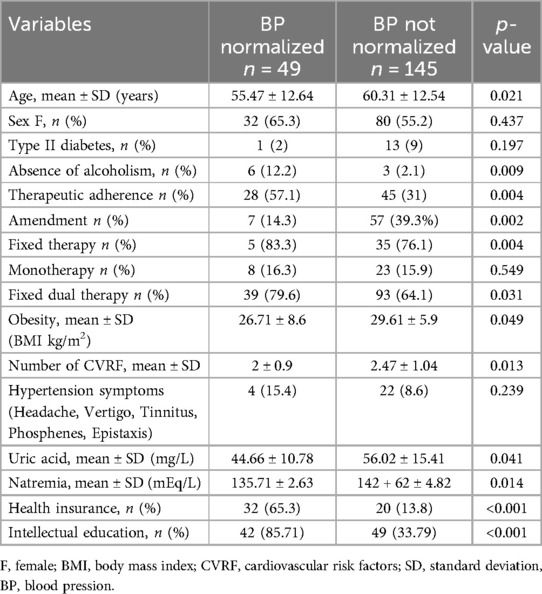
In univariate analysis, age (p = 0.021), absence of obesity (p = 0.049), alcoholism (p = 0.009), number of cardiovascular risk factors <2 (p = 0.013), normalization of uricemia (p = 0.041), natraemia (p = 0.014), fixed dose combination therapy (p = 0.004), dual anti-hypertensive therapy (p = 0, 031), modification of treatment for optimization (p = 0.002), health insurance (p < 0.001), good level of intellectual education (p < 0.001) and anti-hypertensive treatment adherence (p = 0.004) were the main factors predicting normalization of blood pressure (Table 3).
In multivariate analysis adjusted for anti-hypertensive treatment adherence, age (OR = 1.03; 95% CI = 1.002–1.059; p = 0.039), absence of alcoholism (OR = 9.48; 95% CI = 2.13–42.11; p = 0.003), number of cardiovascular risk factors < 2 (OR = 1.52; 95% CI = 1.06–2.16; p = 0.021), normalization of uricemia (OR = 1.05; 95% CI = 1.00–1.11; p = 0.039), natraemia (OR = 1.01; 95% CI = 1.00–1.03; p = 0.021), dual therapy (OR = 0.40; 95% CI = 0.18–0.90; p = 0.027), modification of treatment (OR = 4.22; 95% CI = 1.71–10.37; p = 0.002), good level of intellectual education (OR = 10.40; 95% CI = 4.31–25.10; p < 0.001) and health insurance (OR = 0.09; 95% CI = 0.04–0.21; p < 0.001) were the main factors predicting normalization of blood pressure (Table 4).
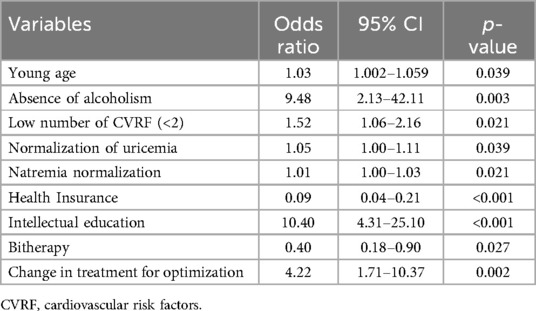
Table 4. Predictive factors for normalization of blood pressure figures in multivariate analysis adjusted for therapeutic compliance.
Discussion
Normalization rate of blood pressure and ideal blood pressure target
Recent American and European guidelines on the therapeutic strategy for hypertension recommend a significant reduction in blood pressure (BP) to below 130/80 mmHg as the blood pressure target for most hypertensive patients on treatment (10–13, 16, 20–22). Initially, the first blood pressure target when treating patients with antihypertensive drugs should be a blood pressure below 140/90 mmHg (6, 22). Secondly, an optimal BP of less than 130/80 mmHg could be aimed for (10, 16, 23). However, caution should be the rule, as lowering blood pressure too severely to below 120/70 mmHg may be harmful to the hypertensive patient, exposing him or her to systemic organ hypoperfusion (10). In our series, out of 194 hypertensive patients, only 49 patients (25.3%) achieved normalization of blood pressure within 6 months of starting anti-hypertensive treatment. Clara K et al, in 2013, in Canada, in a cross-sectional study of a multinational, multicentre population, found a rate of BP control varying between 20.7% and 40% in treated hypertensives. The lowest rates of BP normalization were found in developing countries in Africa, and the highest rates in developed countries and South Africa (3). These rates are lower than those of Lucinda Calas et al. in Mayotte (24) in 2019, Al-Saadi R in Greece in 2011 (25), Donna Shelley in the USA in 2011 (26) and Onwukwe in South Africa in 2012 (27), who respectively found a control rate of 30.2%, 55.6%, 49.8% and 57% in hypertensive patients on pharmacological treatment (4).
Predictive factors for normalization of blood pressure
The factors involved in normalizing BP are numerous and vary according to the authors. Our data are similar to those in the literature, which found that good control of blood pressure was associated with young age, absence of obesity and alcohol consumption, low number of cardiovascular risk factors, correction of uricemia and natremia, use of anti-hypertensive therapies in fixed combinations, modification of treatment, health insurance, adherence with anti-hypertensive treatment and a good level of intellectual education (3, 9, 28–32). In our study, normalized blood pressure was significantly associated with a younger age, less than 60 years. Sheleme T et al. in 2022 (1) made the same observation and explained this phenomenon by the fact that comorbidities increase with ageing and do not facilitate the taking of medication. These results contrast with those of Teshome et al. in Ethiopia (28) in 2018, who found better control of blood pressure in hypertensive patients aged over 60 compared with younger subjects. This could be explained in part by young people's refusal to accept the disease and subsequent therapy. Correction of hyperuricaemia was a predictive factor for normalization of blood pressure in treated hypertensive patients. These results have been corroborated by other authors such as Borghi et al. (33) in 2022 in Italy. As in our series, non-adherence to anti-hypertensive treatment has been recognized as a major problem associated with uncontrolled severe arterial hypertension and is thought to be responsible for approximately 50% of therapeutic failures of anti-hypertensive drugs (9, 34–36). Currently, learned societies (16) strongly recommend the use of a fixed combination of dual therapy during initial treatment for most patients in order to achieve greater efficacy, good adherence with treatment and more rapid attainment of the ideal blood pressure target. Almost 65% of our patients with normalized blood pressure were covered by health insurance. Similar studies have reported the absence of health insurance as a factor associated with poor blood pressure control (9, 37). As reported by other authors (9), our results demonstrate that blood pressure control requires a good level of intellectual literacy on the part of the patient.
Reasons of nonadherence to antihypertensive treatment
Adherence is defined as the extent to which the patient follows prescriptions or oral recommendations from a health care provider (16). It is reported that only approximately one-fourth (25%) are adherent to antihypertensive treatment (38–40). In our series, 37.62% of patients were adherent. The reasons for this low adherence rate in our series overlap with those mentioned by the WHO (41), namely: problems with drug reimbursements, side-effects, complexity of drug regime or interference with daily routine, lack of symptoms or presence of comorbidities with a long list of medications to ingest, low self-efficacy or inaccurate beliefs about medications, poverty with high cost of medications, lack of family support or unemployment. The generally asymptomatic nature of hypertension is likely to increase the risk of this nonadherence.
Strenghs and potential limitations of our study
This analytical study allowed us to clearly predicting Factors of Blood Pressure Normalization and its methodology was based on recent Hypertension management guidelines. However it was a single-center retrospective study with possible lack of representativity of patients group; sport and eating habits were not evaluated. The indirect method (Self report) we used to measure the medication adherence was simple, easy, inexpensive method, integrated into the care relationship. However, it is known to presente a low reliability, an overestimation of adherence and a risk of focusing the relationship on adherence (19, 42). Also, the lack of quantitative data on the reasons why patients were non-adherent is a limitation.
Perspectives
Only 25.25% of our patients achieved normalization of blood pressure. These results are consistent with regional data. Indeed, since 2017, several studies have confirmed suboptimal blood pressure control in sub-Saharan Africa countries (9%–47.3%) (43–45).
The normalization of blood pressure is a major challenge for the practitioner. It is a health emergency which requires the implementation as a priority of a national health program aimed at has:
• Promote 100% comprehensive health insurance, allowing our patients to have health security and improve therapeutic compliance.
• Promote literacy courses to improve the educational level of our populations.
• Promote therapeutic education and strict compliance with the health and diet regime with priority given to the low-sodium diet.
• Make antihypertensive treatment available at lower cost and accessibility for all our populations.
• Develop a system of continuing medical training with a view to updating practitioners' knowledge.
Conclusion
The rate of blood pressure normalization remains poor worldwide and even more worrying in our context. Control of cardiovascular risk factors, fixed dual therapy, adherence with treatment, appropriate modification of antihypertensive treatment, normal uraemia and natraemia, health insurance and an intellectual education are the main factors in normalizing blood pressure levels.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
FS: Conceptualization, Data curation, Formal Analysis, Methodology, Supervision, Writing – original draft, Writing – review & editing. GM: Data curation, Formal Analysis, Writing – review & editing. BS: Writing – review & editing. M-PN: Writing – review & editing. Y-HK: Data curation, Writing – review & editing. IN: Data curation, Writing – review & editing. VA: Data curation, Writing – review & editing. FD: Data curation, Writing – review & editing. AA: Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Sheleme T, Jilo O, Bekele F, Olika W, Safera B, Babu Y. Uncontrolled blood pressure and contributing factors among patients with hypertension at outpatient care of Bedele general hospital, southwest Ethiopia: a cross-sectional study. SAGE Open Med. (2022) 10:20503121221126333. doi: 10.1177/20503121221126333
2. Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. (2016) 134:441–50. doi: 10.1161/CIRCULATIONAHA.115.018912
3. Chow CK, Teo KK, Rangarajan S, Islam S, Gupta R, Avezum A, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. (2013) 310:959–68. doi: 10.1001/jama.2013.184182
4. Amare F, Nedi T, Berhe DF. Blood pressure control practice and determinants among ambulatory hypertensive patients attending primary health care facilities in Addis Ababa. SAGE Open Med. (2020) 8:2050312120946521. doi: 10.1177/2050312120946521
5. Bharatia R, Chitale M, Saxena GN, Kumar RG, Chikkalingaiah TA, Dalvi K, et al. Management practices in Indian patients with uncontrolled hypertension. J Assoc Physicians India. (2016) 64:14–21.27759337
6. Fentaw Z, Adamu K, Wedajo S. Blood pressure control status of patients with hypertension on treatment in Dessie city northeast Ethiopia. BMC Public Health. (2022) 22:917. doi: 10.1186/s12889-022-13368-6
7. Stanaway JD, Afshin A, Gakidou E, Lim SS, Abate D, Abate KH, et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2018) 392:1923–94. doi: 10.1016/S0140-6736(18)32225-6
8. Modey Amoah E, Esinam Okai D, Manu A, Laar A, Akamah J, Torpey K. The role of lifestyle factors in controlling blood pressure among hypertensive patients in two health facilities in urban Ghana: a cross-sectional study. Int J Hypertens. (2020):9379128. doi: 10.1155/2020/9379128
9. Shea S, Misra D, Ehrlich MH, Field L, Francis CK. Predisposing factors for severe, uncontrolled hypertension in an inner-city minority population. N Engl J Med. (1992) 327:776–81. doi: 10.1056/NEJM199209103271107
10. Park S. Ideal target blood pressure in hypertension. Korean Circ J. (2019) 49:1002–9. doi: 10.4070/kcj.2019.0261
11. Reboussin DM, Allen NB, Griswold ME, Guallar E, Hong Y, Lackland DT, et al. Systematic review for the 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol. (2018) 71:2176–98. doi: 10.1016/j.jacc.2017.11.004
12. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Cardiology and the European society of hypertension: the task force for the management of arterial hypertension of the European Society of Cardiology and the European society of hypertension. J Hypertens. (2018) 36:1953–2041. doi: 10.1097/HJH.0000000000001940
13. Martínez-Ibáñez P, Marco-Moreno I, Peiró S, Martínez-Ibáñez L, Barreira-Franch I, Bellot-Pujalte L, et al. Home blood pressure self-monitoring plus self-titration of antihypertensive medication for poorly controlled hypertension in primary care: the ADAMPA randomized clinical trial. J Gen Intern Med. (2023) 38:81–9. doi: 10.1007/s11606-022-07791-z
14. Mancia G, Fagard R, Narkiewicz K, Redón J, Zanchetti A, Böhm M, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European society of hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. (2013) 31:1281–357. doi: 10.1097/01.hjh.0000431740.32696.cc
15. Topouchian JA, El Assaad MA, Orobinskaia LV, El Feghali RN, Asmar RG. Validation of two automatic devices for self-measurement of blood pressure according to the international protocol of the European society of hypertension: the omron M6 (HEM-7001-E) and the omron R7 (HEM 637-IT). Blood Press Monit. (2006) 11:165–71. doi: 10.1097/01.mbp.0000209078.17246.34
16. Mancia G, Kreutz R, Brunström M, Burnier M, Grassi G, Januszewicz A, et al. 2023 ESH guidelines for the management of arterial hypertension the task force for the management of arterial hypertension of the European society of hypertension: endorsed by the international society of hypertension (ISH) and the European renal association (ERA). J Hypertens. (2023) 41:1874–2071. doi: 10.1097/HJH.0000000000003480
17. Pires JE, Sebastião YV, Langa AJ, Nery SV. Hypertension in northern Angola: prevalence, associated factors, awareness, treatment and control. BMC Public Health. (2013) 13:90. doi: 10.1186/1471-2458-13-90
18. The World Bank. Fact Sheet: An Adjustment to Global Poverty Lines. Available on Fact Sheet: An Adjustment to Global Poverty Lines. Available online at: worldbank.org (accessed March 17, 2024)
19. Hawkshead J, Krousel-Wood MA. Techniques for measuring medication adherence in hypertensive patients in outpatient settings: advantages and limitations. Dis Manag Health Outcomes. (2007) 15:109–18. doi: 10.2165/00115677-200715020-00006
20. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Himmelfarb CD, et al. 2017ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol. (2018) 71:e127–248. doi: 10.1016/j.jacc.2017.11.006
21. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. (2018) 39:3021–104. Erratum in: Eur Heart J. 2019;40:475. doi: 10.1093/eurheartj/ehy339
22. Weber MA, Schiffrin EL, White WB, Mann S, Lindholm LH, Kenerson JG, et al. Clinical practice guidelines for the management of hypertension in the community: a statement by the American society of hypertension and the international society of hypertension. J Clin Hypertens (Greenwich). (2014) 16:14–26. doi: 10.1111/jch.12237
23. Beddhu S, Chertow GM, Greene T, Whelton PK, Ambrosius WT, Cheung AK, et al. Effects of intensive systolic blood pressure lowering on cardiovascular events and mortality in patients with type 2 diabetes mellitus on standard glycemic control and in those without diabetes mellitus: reconciling results from ACCORD BP and SPRINT. J Am Heart Assoc. (2018) 18(7):e009326. doi: 10.1161/JAHA.118.009326
24. Calas L, Subiros M, Ruello M, Hassani Y, Gabet A, Angue M, et al. Hypertension prevalence, awareness, treatment and control in 2019 in the adult population of Mayotte. Eur J Public Health. (2022) 32:408–14. doi: 10.1093/eurpub/ckac015
25. Al-Saadi R, Al-Shukaili S, Al-Mahrazi S, Al-Busaidi Z. Prevalence of uncontrolled hypertension in primary care settings in Al Seeb Wilayat, Oman. Sultan Qaboos Univ Med J. (2011) 11:349–56.22087376
26. Shelley D, Tseng TY, Andrews H, Ravenell J, Wu D, Ferrari P, et al. Predictors of blood pressure control among hypertensives in community health centers. Am J Hypertens. (2011) 24:1318–23. doi: 10.1038/ajh.2011.154
27. Onwukwe SC, Omole OB. Drug therapy, lifestyle modification and blood pressure control in a primary care facility, South of Johannesburg, South Africa: an audit of hypertension management. S Afr Fam Pract. (2012) 54:156–61. doi: 10.1080/20786204.2012.10874196
28. Teshome DF, Demssie AF, Zeleke BM. Determinants of blood pressure control amongst hypertensive patients in Northwest Ethiopia. PLoS One. (2018) 13(5):e0196535. doi: 10.1371/journal.pone.0196535
29. Cushman WC, Ford CE, Cutler JA, Margolis KL, Davis BR, Grimm RH, et al. Success and predictors of blood pressure control in diverse north American settings. J Clin Hypertens (Greenwich). (2002) 4:393–404. doi: 10.1111/j.1524-6175.2002.02045.x
30. Joshi R, Chow CK, Raju PK, Raju KR, Gottumukkala AK, Reddy KS, et al. The rural Andhra Pradesh cardiovascular prevention study (RAPCAPS). J Am Coll Cardiol. (2012) 59:1188–96. doi: 10.1016/j.jacc.2011.10.901
31. Zaman MJ, Patel A, Jan S, Hillis GS, Raju PK, Neal B, et al. Socio-economic distribution of cardiovascular risk factors and knowledge in rural India. Int J Epidemiol. (2012) 41:1302–14. doi: 10.1093/ije/dyr226
32. Axon RN, Bradford WD, Egan BM. The role of individual time preferences in health behaviors among hypertensive adults: a pilot study. J Am Soc Hypertens. (2009) 3:35–41. doi: 10.1016/j.jash.2008.08.005
33. Borghi C, Agnoletti D, Cicero AFG, Lurbe E, Virdis A. Uric acid and hypertension: a review of evidence and future perspectives for the management of cardiovascular risk. Hypertension. (2022) 79:1927–36. doi: 10.1161/HYPERTENSIONAHA.122.17956
34. McManus RJ, Mant J, Franssen M, Nickless A, Schwartz C, Hodgkinson J, et al. Efficacy of self-monitored blood pressure, with or without telemonitoring, for titration of antihypertensive medication (TASMINH4): an unmasked randomised controlled trial. Lancet. (2018) 391:949–59. doi: 10.1016/S0140-6736(18)30309-X
35. Hossain A, Ahsan GU, Hossain MZ, Hossain MA, Sultana ZZ, Arefin A, et al. A prospective longitudinal study with treated hypertensive patients in northern Bangladesh (PREDIcT-HTN) to understand uncontrolled hypertension and adverse clinical events: a protocol for 5-years follow-up. PLoS One. (2022) 17:e0269240. doi: 10.1371/journal.pone.0269240
36. Kolandaivelu K, Leiden BB, O’Gara PT, Bhatt DL. Non-adherence to cardiovascular medications. Eur Heart J. (2014) 35:3267–76. doi: 10.1093/eurheartj/ehu364
37. Yang L, Xu X, Yan J, Yu W, Tang X, Wu H, et al. Analysis on associated factors of uncontrolled hypertension among elderly hypertensive patients in southern China: a community-based, cross-sectional survey. BMC Public Health. (2014) 14:903. doi: 10.1186/1471-2458-14-903
38. Mancia G, Rea F, Corrao G, Grassi G. Two-drug combinations as first-step antihypertensive treatment. Circ Res. (2019) 124:1113–23. doi: 10.1161/CIRCRESAHA.118.313294
39. Tomaszewski M, White C, Patel P, Masca N, Damani R, Hepworth J, et al. High rates of non-adherence to antihypertensive treatment revealed by high-performance liquid chromatography-tandem mass spectrometry (HP LC-MS/MS) urine analysis. Heart. (2014) 100:855–61. doi: 10.1136/heartjnl-2013-305063
40. Gupta P, Patel P, Strauch B, Lai FY, Akbarov A, Gulsin GS, et al. Biochemical screening for nonadherence is associated with blood pressure reduction and improvement in adherence. Hypertension. (2017) 70:1042–8. doi: 10.1161/HYPERTENSIONAHA.117.09631
41. Sabaté E. Adherence to Long-Term Therapies: Evidence for Action. Geneva: World Health Organization (2003). ISBN: 9241545992.
42. Benoit M, Pon J, Zimmermann MA. Comment évaluer la qualité de l’observance? L'encéphale. (2009) 35:S87–90. doi: 10.1016/S0013-7006(09)75542-3
43. Gafane-Matemane LF, Craig A, Kruger R, Alaofin OS, Ware LJ, Jones ESW, et al. Hypertension in Sub-Saharan Africa: the current profile, recent advances, gaps, and priorities. J Hum Hypertens. (2024). doi: 10.1038/s41371-024-00913-6
44. Zhou B, Carrillo-Larco RM, Danaei G, Riley LM, Paciorek CJ, Stevens GA, et al. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. (2021) 398:957–80. doi: 10.1016/S0140-6736(21)01330-1
Keywords: normalization, arterial hypertension, cardiology, predicting factors, follow-up
Citation: Sall F, Meneas GC, Siransy BAE, N’cho Mottoh M-P, Kpi Y-H, N’guessan I, Assi VM, Diby F and Adoubi A (2024) Predicting factors of blood pressure normalization in hypertensive patients after short-term follow-up. Front. Cardiovasc. Med. 11:1403214. doi: 10.3389/fcvm.2024.1403214
Received: 19 March 2024; Accepted: 30 July 2024;
Published: 27 August 2024.
Edited by:
Guido Iaccarino, Federico II University Hospital, ItalyReviewed by:
Michel Burnier, Université de Lausanne, SwitzerlandAlessandra Cuomo, University of Naples Federico II, Italy
Copyright: © 2024 Sall, Meneas, Siransy, N'cho Mottoh, Kpi, N'guessan, Assi, Diby and Adoubi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fatouma Sall, ZmF0b3VzYWxsNDVAeWFob28uZnI=
†ORCID:
Fatouma Sall
orcid.org/0000-0002-8571-9684
 Fatouma Sall
Fatouma Sall Gueu Christophe Meneas
Gueu Christophe Meneas Balayssac Ahou Edwige Siransy
Balayssac Ahou Edwige Siransy Marie-Paule N’cho Mottoh
Marie-Paule N’cho Mottoh Yannik-Hermann Kpi1
Yannik-Hermann Kpi1