- 1Department of Preventive and Social Medicine, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand
- 2Cardiac Center and Division of Cardiovascular Disease, Department of Medicine, King Chulalongkorn Memorial Hospital, Chulalongkorn University, Bangkok, Thailand
Background: In Thailand, access to specific pharmaceuticals and medical devices for ST-elevation myocardial infarction (STEMI) patients is restricted within certain healthcare systems, leading to inequalities in the quality of medical care among different healthcare systems. This study aims to compare mortality rates within one year of STEMI patients among the public health insurance schemes of Thailand.
Methodology: This study is a single-center retrospective analysis of patients with STEMI treated with primary percutaneous coronary intervention (pPCI). It involves patients utilizing various state health insurance schemes in Thailand from January 1, 2010, to December 31, 2020. Data collection occurred through the hospital's computerized management system and the registration administration office of the Department of Provincial Administration.
Results: The study involved 1,077 patients, categorized into three groups based on their state health insurance: Universal Health Coverage (UC) (546 patients, 50.7%), Social Security System (SS) (199 patients, 18.5%), and Civil Service Reimbursement (CS) (332 patients, 30.8%). The one-year mortality rates in these groups were 10.57%, 4.21%, and 6.47%, respectively (p = 0.010). In the unadjusted model, the SS group showed a lower risk of one-year mortality [Hazard Ratio (HR) 0.38, 95% CI 0.18–0.80, p = 0.011], and the CS group also demonstrated a lower risk (HR 0.59, 95% CI 0.35–0.99, p = 0.047) compared to the UC group. In the adjusted model, only the CS group significantly reduced the risk of one-year mortality. Other factors that affected one-year mortality were age ≥65 years, prior coronary artery diseases, Killip class 3–4, pre-discharge prescription of angiotensin-converting enzyme inhibitors, occlusion in the left anterior descending artery, multivessel disease, in-hospital atrial fibrillation/flutter and in-hospital pericardial effusion.
Conclusion: Healthcare schemes play a significant role in influencing one-year mortality rates among STEMI patients treated with pPCI. This information would be crucial for developing strategies and programs to aid healthcare policymakers at both regional and international levels in reducing morbidity and mortality.
1 Introduction
ST-segment elevation myocardial infarction (STEMI) presents a major public health challenge worldwide, including in Thailand (1). The prevalence of STEMI within the nation exhibits an ascending trend, leading to significant rates of morbidity and mortality (2–4). As recommended by international guidelines, primary percutaneous coronary intervention (pPCI) is currently the preferred therapeutic intervention for STEMI patients when performed by experts within an optimal timeframe (5, 6). Compared with traditional intervention, thrombolytic therapy, pPCI demonstrates superior efficacy, significantly reducing short-term and long-term mortality rates, the incidence of recurrent arterial occlusions, the risk of cerebrovascular events, and the occurrence of abnormal bleeding (7).
In Thailand, most healthcare services are predominantly provided by the government sector. Healthcare services in Thailand are divided into three distinct systems: Universal Health Coverage (UC), Social Security System (SS), and Civil Service Reimbursement (CS), which cover 75%, 16%, and 9% of the population, respectively. The UC's objective is to provide healthcare services without incurring personal financial costs for Thai citizens. The SS is intended for private sector employees, providing a safety net for life sustenance through contributions from employers, employees, and the state. The CS is a privilege for active and retired civil servants, representing one of the welfare benefits provided by the government (8).
Each system has its own conceptual underpinnings, leading to inequalities in public health service access among the three types of health coverage. This results in discrepancies in access to medications and variations in the quality of treatments, leading to a potential significant impact on the quality of life of patients, both in the short and long term. The authors sought to determine the differences in patients' characteristics, procedure variations, in-hospital outcomes, and long-term outcomes among the healthcare systems. Therefore, this study aims to compare mortality rates within one year of STEMI patients among the public health insurance schemes of Thailand. This information would be crucial for developing strategies and programs to aid healthcare policymakers at both regional and international levels in reducing morbidity and mortality.
2 Methods
2.1 Study design
This study is a descriptive, retrospective research on patients diagnosed with ST-elevation myocardial infarction (STEMI), who received primary percutaneous coronary intervention (pPCI), at the King Chulalongkorn Memorial Hospital, a tertiary referral center. The data for this study was compiled from the King Chulalongkorn Memorial Hospital's database management system, utilizing International Classification of Diseases, Tenth Revision, Clinical Modification codes I21.0–I21.4, and the Ninth Revision, Clinical Modification codes 00.40–0048, 00.6, and 36.06–36.07. The period under review in this study extends from January 1, 2010, through December 31, 2020.
We identified and recorded the total number of patients who met the pre-defined inclusion criteria: patients who received the pPCI strategy as the initial treatment, and whose age was equal to or greater than 18 years. We excluded patients with missing data on national identification number, health insurance coverage under the Thai national health insurance scheme, or no history in the civil registration system, patients who received the pharmacoinvasive strategy, and patients who underwent coronary artery bypass grafting (CABG) surgery. Patients were followed for mortality from the time of procedure initiation. However, the analysis exclusively included deaths that occurred post-procedure. Demographic and clinical information, including laboratory test results and procedural data, were retrospectively collected by well-trained critical care nurses and cardiologists, and documented from both outpatient and inpatient database records. Routine follow-up data collection included hospital visits and assessments at 12 months via file review for specific clinical measures, patient-reported outcomes, or hospitalizations.
For verifying the timing of deaths, our study was granted access to the civil registration system through the Bureau of Registration Administration (BORA) of Thailand. We performed a matching process using the patient's national identification number and date of birth against entries in the civil registration system. A match was confirmed when an entry in the Index corresponded exactly to a patient's national identification number and date of birth with a patient recorded in our study registry. ChatGPT 4.0 is applied to check and correct grammatical errors during writing process. The contents produced by AI technology were finally reviewed and edited by the authors.
This study was conducted in adherence to the principles of Good Clinical Practice, adhering to all relevant Thai legislation and data protection regulations. No individual specific consent forms for the study were obtained. The protocol was reviewed and approved by an ethics committee from the Institutional Review Board of the Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand (COA No. 1742/2022).
2.2 Statistical analysis
The primary objective is to compare mortality rates within one year of STEMI patients after treatment of pPCI among the public health insurance schemes of Thailand. The secondary objectives are to study prognostic determinants for both in-hospital and one-year mortality rates among patients diagnosed with STEMI who have undergone pPCI at King Chulalongkorn Memorial Hospital.
Categorical variables are presented as frequency and proportion using the Pearson Chi-square test or Fisher's exact test, while continuous variables are expressed through mean, standard deviations (SD), medians, or interquartile ranges (IQR) analyzed with the independent t-test, one-way analysis of variance (ANOVA), or Kruskal-Wallis test. The study aims to conduct a comparative analysis of one-year mortality rates across different healthcare entitlements in Thailand, including the Universal Health Coverage, Social Security System, and Civil Service Reimbursement. To assess differences in mortality outcomes among these groups, Kaplan-Meier curve and log-rank testing methodologies are utilized. Multiple logistic regression analyses were executed to determine the predictors of in-hospital outcomes, while multiple Cox regression models to compute crude hazard ratios are utilized to examine the individual relation between each predictor and death during one-year follow-up. Variables selected for inclusion in the final multivariate models were those demonstrating a significance level of less than 0.05 in the univariate analyses (Supplementary Tables S1, S2), unless otherwise stated. All statistical tests were conducted as two-sided, with the threshold for statistical significance established at a P-value of less than 0.05. All statistical analyses will be performed using StataCorp. 2023. Stata Statistical Software: Release 18. College Station, TX: StataCorp LLC.
3 Results
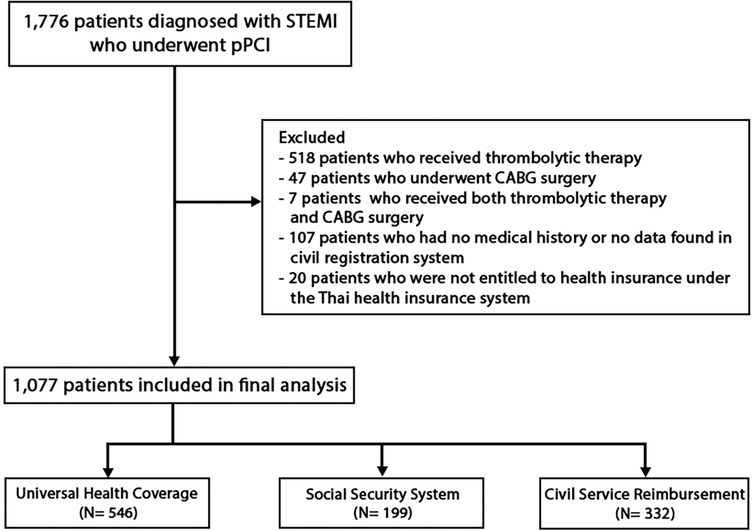
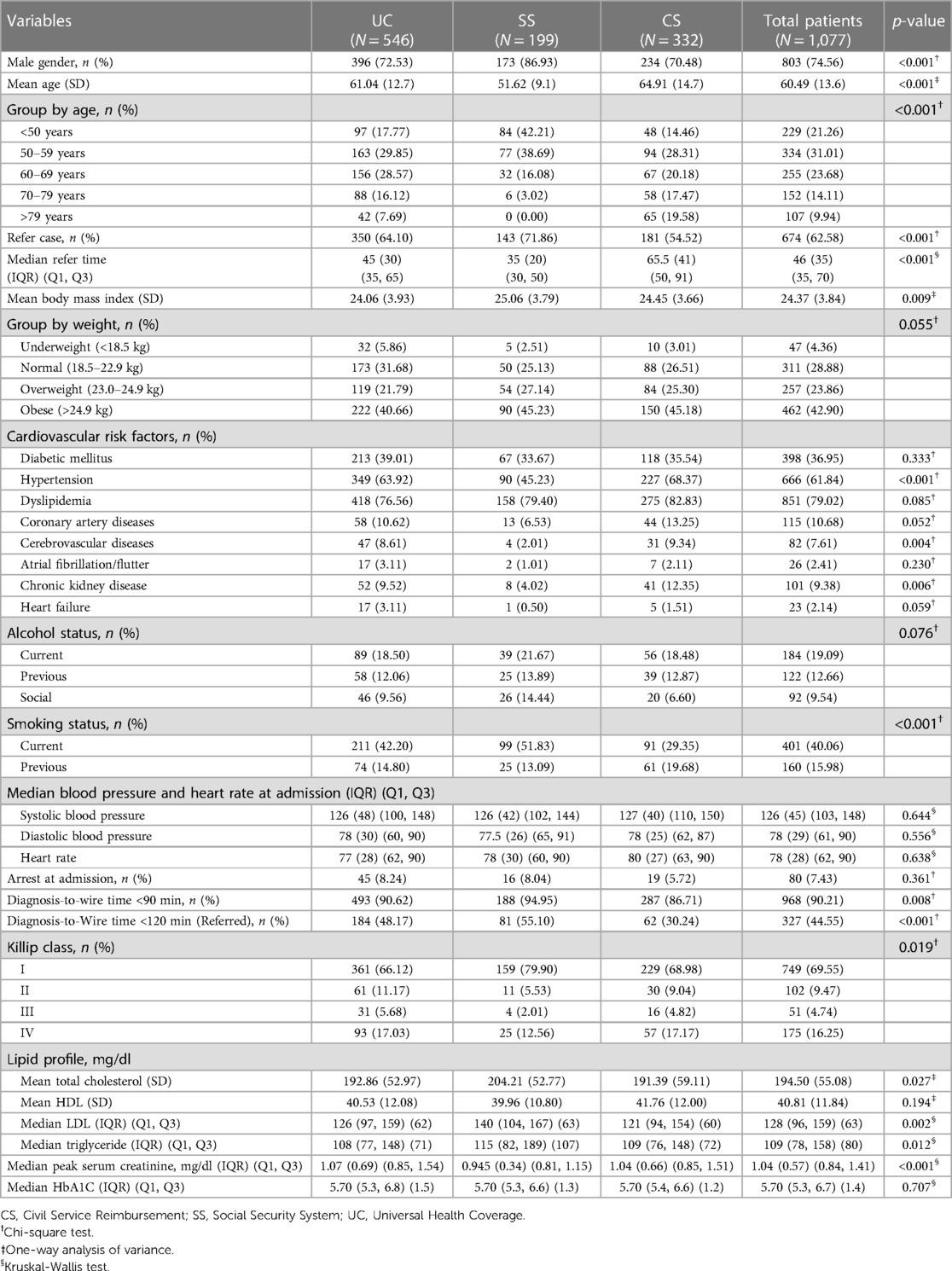
In this study, we examined data from 1,776 STEMI patients who underwent PCI for STEMI from January 1, 2010, to December 31, 2020. Following the application of exclusion criteria, which led to the removal of 699 patients as depicted in Figure 1, our analysis focused on the remaining 1,077 participants. These individuals were stratified into three distinct groups based on their enrollment in public health insurance schemes of Thailand: 546 patients in the Universal Health Coverage (UC) group (50.69%), 199 patients in the Social Security System (SS) group (18.48%), and 332 patients in the Civil Service Reimbursement (CS) group (30.83%). Baseline demographic and clinical characteristics, presented in Table 1, reveal that the SS cohort exhibited a higher male predominance (86.90%), the youngest mean age (51.62 years), and the most significant proportion of transferred patients (71.90%). Notably, this group also reported the highest proportion of Killip class I at hospital admission (79.90%). Laboratory findings showed the lowest mean serum creatinine levels in the SS group at 0.945 mg/dl and the lowest LDL levels in the CS group at 121 mg/dl.
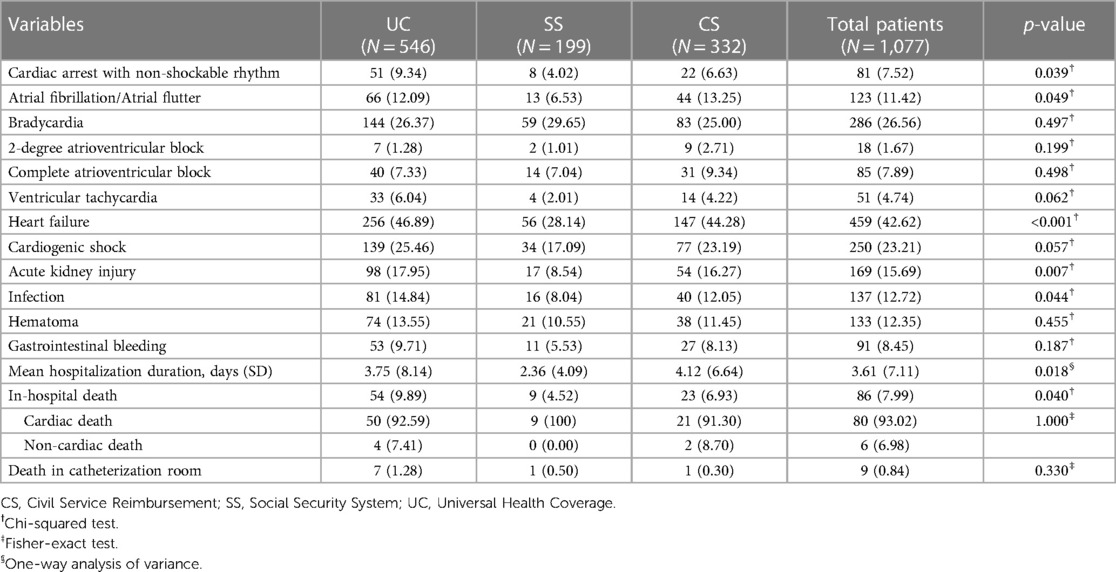
Significant statistical differences between groups were observed in hospital complications (Table 2), including cardiac arrest with non-shockable rhythm, atrial fibrillation/atrial flutter, heart failure, acute kidney injury, and infections. Remarkably, these complications were least prevalent in the SS group, with in-hospital mortality also lowest in this cohort. Through multiple logistic regression analysis (Table 3), variables for in-hospital mortality were identified, including age more than or equal to 65, cardiac arrest upon admission, advanced Killip class 3–4, multivessel disease, left main artery occlusion, alongside complications such as bradycardia, pericardiac effusion, atrial fibrillation/flutter, ventricular tachycardia, and acute kidney failure. In contrast, the use of drug-eluting stents represented a protective factor against in-hospital mortality.
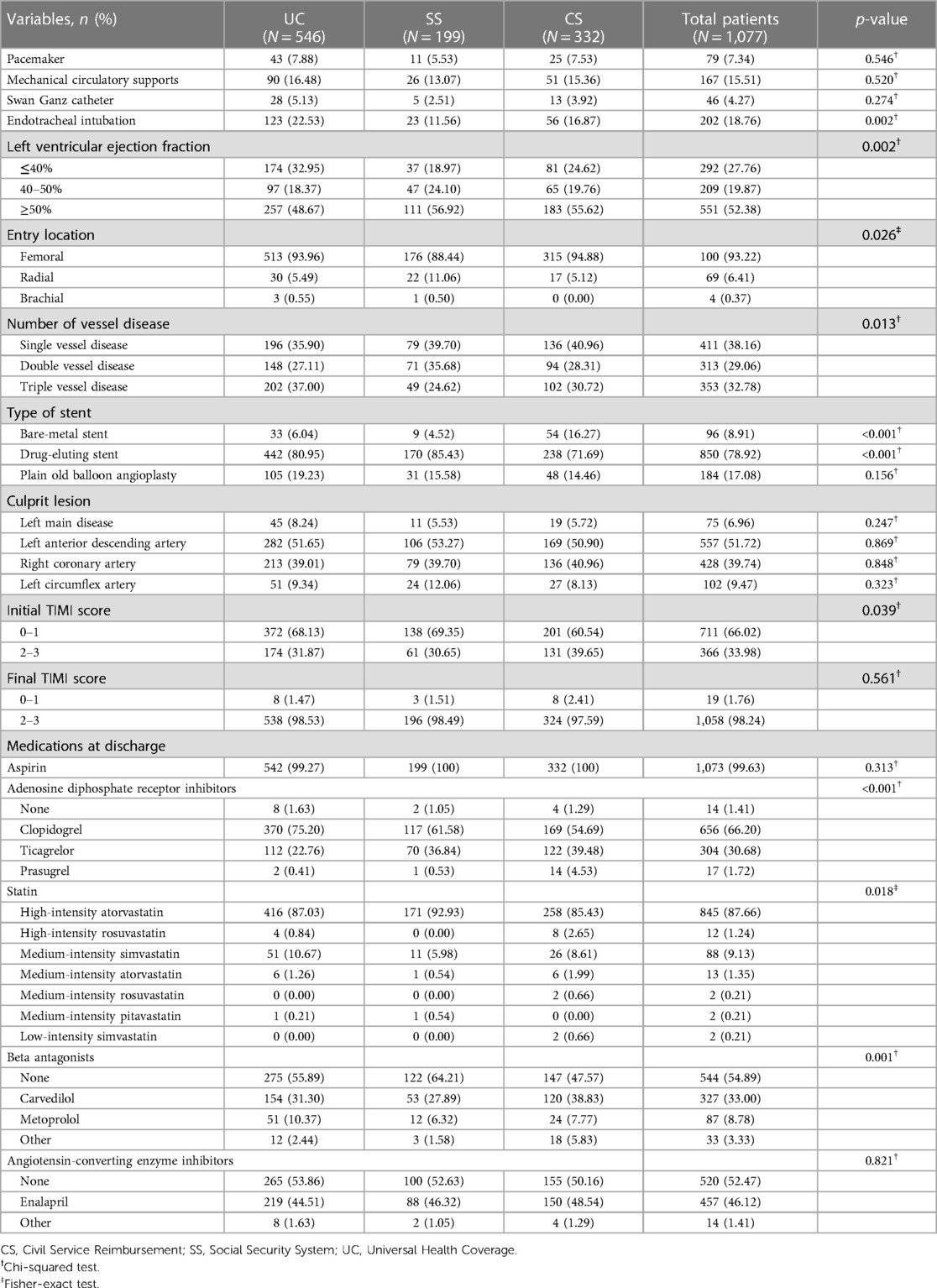
In terms of cardiac catheterization procedures, as presented in Table 4, the SS group had the highest proportion of procedures completed within the Diagnosis-to-Wire time of less than 90 min (94.95%), and also achieved the highest proportion within <120 min (55.10%) drug-eluting stents (DES) appeared to be the predominant choice (78.92%), followed by plain old balloon angioplasty (POBA) and bare-metal stents (BMS) at 17.08% and 8.91%, respectively. The SS cohort led in DES utilization (85.43%), with the UC and CS groups behind at 80.95% and 71.69%, respectively.
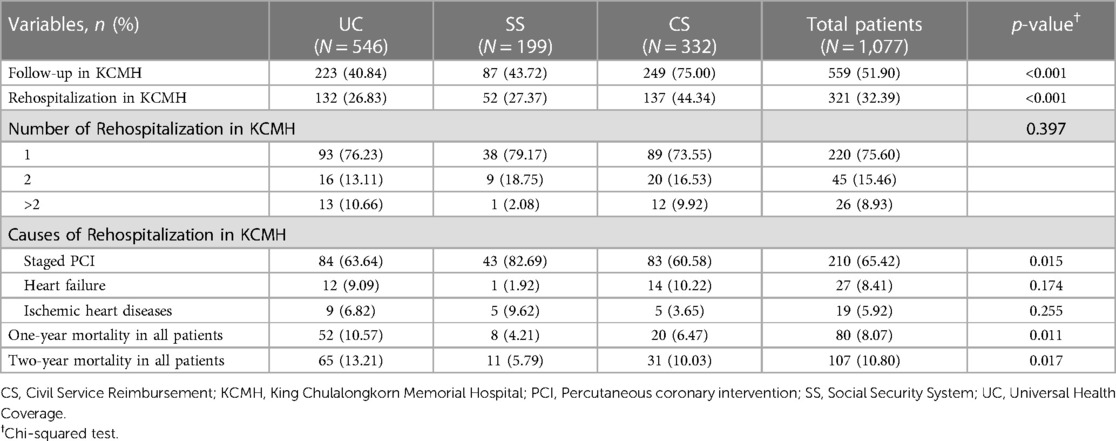
One-year follow-up observations, detailed in Table 5, indicated the CS group had the highest follow-up (75.00%) and readmission rate within one year (44.34%), primarily for staged PCI. Mortality rate at one- and two-years post-discharge revealed the highest death rates in the UC group, with the SS group recording the lowest figures. Kaplan–Meier curve was used to evaluate one- and two-year mortality rates across the public health insurance schemes (Figure 2) which revealed significant differences, with both the SS and CS groups demonstrating notably lower mortality rates at one-year compared to the UC group (p = 0.0083 and p = 0.0446, respectively). Also, the SS group maintained a significantly lower mortality rate at two-years compared to the UC group (p = 0.0055).
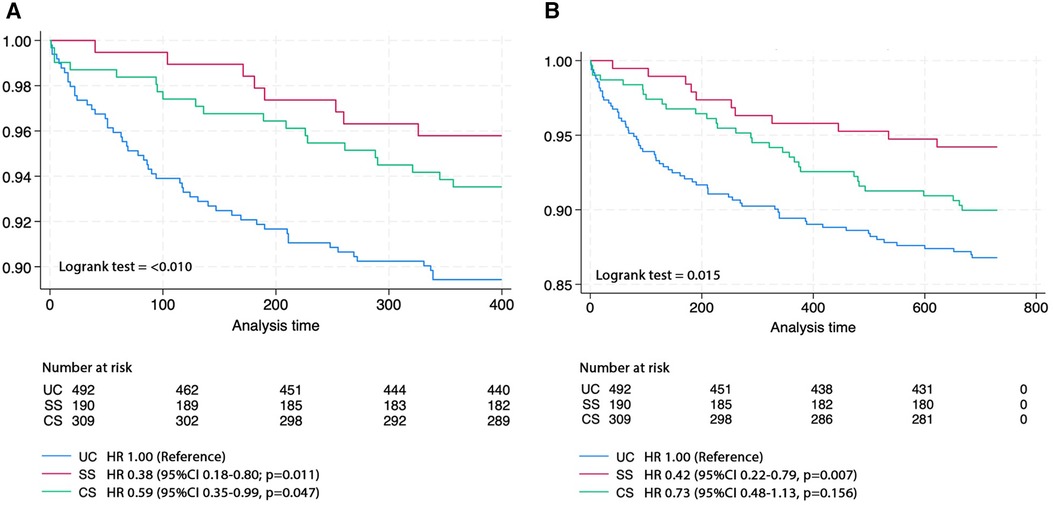
Figure 2. Kaplan-Meier curve of (A) one- and (B) two-year survival rates across the public health insurance schemes.
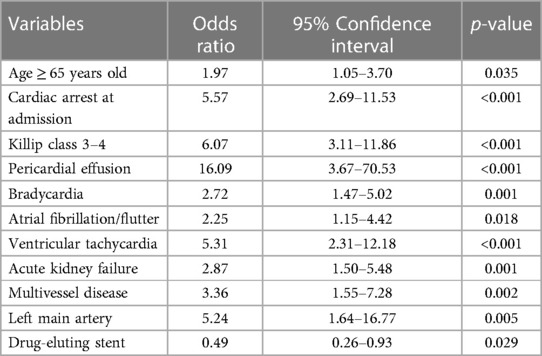
Utilizing a multiple Cox regression model (Table 6), several predictors are associated with an increased risk of mortality within one-year post-discharge, including age equal to or more than 65 years, prior coronary artery diseases, Killip class 3–4, multivessel disease, occlusion at the left anterior descending artery, in-hospital atrial fibrillation/flutter and in-hospital pericardial effusion. Moreover, patients covered by the CS insurance and received pre-discharge angiotensin-converting enzyme inhibitor administration demonstrated a decreased risk of one-year post-discharge mortality.
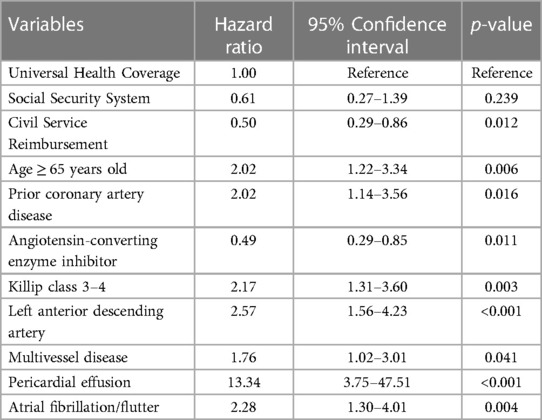
Table 6. Cox proportional hazard multivariate analysis of predictors of one-year post-discharge mortality after pPCI.
4 Discussion
This study represents the first national investigation into the correlation between public health insurance schemes in Thailand and the long-term mortality rates among STEMI patients receiving pPCI treatment. Our findings reveal that different health insurance schemes have a statistically significant impact on mortality rates. Specifically, the SS group demonstrated the lowest one-year mortality rate at 4.21%, followed by the CS group at 6.47%. Furthermore, a longitudinal analysis extending to two years supported that the SS cohort consistently showed the lowest mortality rate. Additionally, international studies underscore that the entitlement to treatment profoundly influences both the management and outcomes of patients (9–12).
Upon examining the basic characteristics, the SS group was found to have the youngest average age. We observed that patients aged 65 years or older had nearly twice the risk of mortality within one year, which aligns with previous research indicating that age is a significant predictor of mortality (13, 14). When comparing the basic characteristics of patients in other studies, the SS group was found to be younger than the sample groups in other studies (3, 9–11). In terms of comorbidities, the SS patient group had the lowest number of diabetes mellitus, which is a predictive factor for short-term and long-term mortality (15, 16). Regarding smoking history, a higher proportion of SS patients were smokers. This finding is consistent with observations in smokers with acute myocardial infarction where the paradoxical protective effect of smoking may be attributed to smoking being a confounding variable (17). When assessing the severity at hospital admission using the Killip classification, other studies have indicated that higher scores are associated with an increased risk of mortality in both the short-term and long-term (18), which is consistent with our findings. The SS patient group had a lower proportion of high Killip class.
Upon further examination of laboratory blood values, the SS patient group exhibited the lowest peak creatinine levels. Previous research has established that elevated creatinine levels are indicative of an increased risk of mortality (13). Our study similarly found that patients with acute kidney injury faced a heightened risk of in-hospital mortality. Additionally, the highest levels of LDL in the SS group were observed in comparison to other groups. This phenomenon can be elucidated by the LDL paradox, where it has been documented those patients with elevated LDL levels during myocardial ischemia experienced reduced mortality and morbidity, likely attributed to younger age and fewer comorbidities (19).
Shortening the treatment delay time significantly influences mortality rates (20). In our research, the SS patient group exhibited the shortest diagnosis-to-wire time, yet, regrettably, this time frame did not appear as a protective factor. Nonetheless, we encourage that reducing pre-hospital time presents a critical opportunity to enhance treatment outcomes and should be prioritized for additional attention and resource allocation (21).
In terms of procedures, SS patients received DES more frequently than BMS, with DES being the preferred choice of stent used in the procedure (22). This results in superior outcomes in terms of reducing the rate of re-occlusion of the stents (6). The final TIMI score does not differ among the three groups, along with the mortality rate in the catheterization room being similar.
In the comparison between the Civil Servant (CS) and Universal Coverage (UC) groups, both exhibit similar baseline characteristics and receive similar treatment during hospitalization. However, the CS group demonstrates a lower one-year mortality rate. Being covered under the CS scheme serves as a protective factor against one-year mortality. This can be attributed to the extensive coverage offered by the CS insurance, which grants patients access to treatment at any public hospital, in contrast to the UC and SS schemes that limit treatment to registered hospitals only. Additionally, patients under the CS scheme have access to a wider range of medications, including those not on the National List of Essential Medicine (NLEM), original drugs, and those with higher prices. Notably, Clopidogrel, an ADP inhibitor, is available to all CS patients without additional cost (8). Furthermore, CS patients are more likely to receive the predischarge non-Clopidogrel medications, such as Ticagrelor or Prasugrel, which may result in a lower recurrence of myocardial infarctions in CS group.
When reviewing the medications provided at discharge, it shows that patients in the CS group are more likely to receive angiotensin converting enzyme inhibitors and beta-blockers compared to other health insurance groups. Renin-angiotensin system inhibitors and beta-antagonists are associated with enhanced outcomes in both short-term and long-term cardiovascular diseases (5, 6). The administration of angiotensin-converting enzyme inhibitors to the CS patients prior to discharge, which is a protective factor, may lead to a lower mortality rate among the CS patients compared to others. However, nearly half of the patients still did not receive beta-antagonists or angiotensin-converting enzyme inhibitors, a continuing issue from previous research (3). Improving the administration of these medications could present an opportunity to reduce morbidity and mortality in STEMI patients.
Moreover, follow-up data indicates that the CS group have the highest rate of one-year treatment adherence. This may be crucial for secondary prevention of STEMI patients. Additionally, CS group have a higher rate of hospitalizations, with more than half of these patients scheduled for staged PCI. The CS group shows a significantly higher rate of hospitalization compared to other groups. However, the greater number of CS patients who undergo follow-up at KCMH ensures that the rehospitalization data pertaining to this group is more precise and accurate. Nonetheless, future studies should aim to collect data on patient follow-ups from all hospitals where treatment is received.
In addition, the reason the CS group has a higher rate of hospitalizations may possibly be due to the direct effects of hospital payments and patient demand for services. The CS scheme reimburses hospitals based on the actual costs of services rendered. This contrasts with other systems that use capitation or Diagnosis-Related Groups (DRG), which may result in hospitals receiving less than their expenditures (8). It is interesting that despite the higher incidence of in-hospital complications among UC group, they experience a less hospitalization duration compared to the CS group. This may be explained by the fact that CS patients tend to request more services since they are aware that the hospital is entitled to full reimbursement of expenses by the government. Although the SS group cohort showed lower in-hospital and one-year mortality rates, upon conducting a multivariable analysis, it was determined that this factor did not serve as a protective variable against mortality. This may be attributed to the younger age demographic, lower Killip class, and lower in-hospital complications.
Our research indicates that healthcare schemes play a significant role in influencing mortality rates among patients. Health equity implies the equitable and appropriate access to high-quality health services for all individuals. Also, distributing equity across different regions is crucial (23). The government aims to evolve the health insurance system to augment quality and extend coverage nationwide, particularly through the UC scheme, which covers most of the population (24). The assessment of PCI treatment in UC patients has been increasing, resulting in a noticeable reduction in mortality rates (25).
4.1 Limitations
Cost-effectiveness was not presented in this study as some patients were transferred out of the hospital before recovery, making it difficult to track expenses. In searching for mortality data in the civil registration system, information on the cause of death was not provided. The study was conducted on data from only one tertiary care hospital, resulting in limited patient data distribution which may not accurately represent the treatment outcomes in general. Therefore, further prospective research is required to gather data on a national level.
5 Conclusion
We found that the one-year mortality rate of patients with STEMI treated with pPCI in Thailand tends to be lower. Patients using the SS scheme had the lowest one-year and two-year mortality rates, followed by patients with the CS scheme, which is consistent with the in-hospital mortality rate. The CS schemes and the pre-discharge administration of angiotensin-converting enzyme inhibitors independently serve as protective factors against one-year mortality. In contrast, advanced age, a Killip class of 3–4 at hospital admission, multivessel disease, occlusion in the left anterior descending artery, and the presence of atrial fibrillation/flutter and pericardial effusion independently elevate the risk of one-year mortality. The improvement of the UC scheme may reduce morbidity and mortality in Thailand.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Institutional Review Board of the Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand (COA No. 1742/2022). The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
SC: Conceptualization, Investigation, Writing – original draft, Writing – review & editing, Data curation, Formal Analysis, Methodology. SL: Conceptualization, Formal Analysis, Methodology, Writing – review & editing. TR: Conceptualization, Formal Analysis, Methodology, Writing – review & editing. VL: Conceptualization, Data curation, Writing – review & editing. SA: Conceptualization, Data curation, Writing – review & editing. CW: Conceptualization, Data curation, Writing – review & editing. SS: Conceptualization, Data curation, Investigation, Methodology, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
Ratchadapiseksompotch Fund, Graduate Affairs, Faculty of Medicine, Chulalongkorn University, Grant number GA66/053.
Acknowledgments
The authors would like to express our gratitude to the patients whose participation was vital to this study. We deeply appreciate the Emergency department/Catheterization laboratory/ICU/CCU personnel, and the research nurses for their assistance in patient care data collection. Finally, we appreciate the guidance of our investigator, which is crucial to this research. During the preparation of this work the authors used ChatGPT 4.0 to check and correct grammatical errors during writing process. After using this tool/service, the authors reviewed and edited the content as needed and take full responsibility for the content of the publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2024.1397015/full#supplementary-material
Abbreviations
BMS, bare-metal stent; BORA, the Bureau of Registration Administration; CABG, coronary artery bypass grafting; CS, Civil Service Reimbursement; DES, Drug-eluting stent HR, hazard ratio; KCMH, King Chulalongkorn Memorial Hospital; POBA, plain old balloon angioplasty; PCI, percutaneous coronary intervention; pPCI, primary percutaneous coronary intervention; SS, Social Security System; STEMI, ST-segment elevation myocardial infarction; UC, Universal Health Coverage.
References
1. Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the global burden of disease study 2010. Lancet. (2012) 380(9859):2095–128. doi: 10.1016/S0140-6736(12)61728-0
2. Srimahachota S, Kanjanavanit R, Boonyaratavej S, Boonsom W, Veerakul G, Tresukosol D, et al. Demographic, management practices and in-hospital outcomes of Thai acute coronary syndrome registry (TACSR): the difference from the western world. J Med Assoc Thai. (2007) 90(Suppl 1):1–11.18431881
3. Srimahachota S, Boonyaratavej S, Kanjanavanit R, Sritara P, Krittayaphong R, Kunjara-Na-Ayudhya R, et al. Thai Registry in acute coronary syndrome (TRACS)-an extension of Thai acute coronary syndrome registry (TACS) group: lower in-hospital but still high mortality at one-year. J Med Assoc Thail. (2012) 95(4):508.
4. Sansanayudh N, Chandavimol M, Srimahachota S, Limpijankit T, Hutayanon P, Kiatchoosakun S, et al. Patient characteristics, procedural details, and outcomes of contemporary percutaneous coronary intervention in real-world practice: insights from nationwide Thai PCI registry. J Interv Cardiol. (2022) 2022:5839834. doi: 10.1155/2022/5839834
5. Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. (2018) 39(2):119–77. doi: 10.1093/eurheartj/ehx393
6. Writing Committee Members; Lawton JS, Tamis-Holland JE, Bangalore S, Bates ER, Beckie TM, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: executive summary: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. J Am Coll Cardiol. (2022) 79(2):197–215. doi: 10.1016/j.jacc.2021.09.005
7. Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. (2003) 361(9351):13–20. doi: 10.1016/S0140-6736(03)12113-7
8. World Health Organization. Regional Office for the Western P. the Kingdom of Thailand Health System Review. Manila: WHO Regional Office for the Western Pacific (2015).
9. Chakraborty S, Bandyopadhyay D, Amgai B, Sidhu JS, Paudel R, Koirala S, et al. Does insurance effect the outcome in patients with acute coronary syndrome?: an insight from the most recent national inpatient sample. Curr Probl Cardiol. (2021) 46(1):100411. doi: 10.1016/j.cpcardiol.2019.02.003
10. Arazi HC, Higa C, Blanco P, Nani S, Fernandez H, Hirschson A, et al. Mortality in myocardial infarction remains high in Argentina: the association with health insurance coverage. IJC Metab Endocr. (2014) 4:18–22. doi: 10.1016/j.ijcme.2014.08.004
11. Pancholy S, Patel G, Pancholy M, Nanavaty S, Coppola J, Kwan T, et al. Association between health insurance status and in-hospital outcomes after ST-segment elevation myocardial infarction. Am J Cardiol. (2017) 120(7):1049–54. doi: 10.1016/j.amjcard.2017.06.041
12. Patel N, Gupta A, Doshi R, Kalra R, Bajaj NS, Arora G, et al. In-Hospital management and outcomes after ST-segment-elevation myocardial infarction in medicaid beneficiaries compared with privately insured individuals. Circ Cardiovasc Qual Outcomes. (2019) 12(1):e004971. doi: 10.1161/CIRCOUTCOMES.118.004971
13. Newby LK, Bhapkar MV, White HD, Topol EJ, Dougherty FC, Harrington RA, et al. Predictors of 90-day outcome in patients stabilized after acute coronary syndromes. Eur Heart J. (2003) 24(2):172–81. doi: 10.1016/S0195-668X(02)00325-1
14. Hosseiny AD, Moloi S, Chandrasekhar J, Farshid A. Mortality pattern and cause of death in a long-term follow-up of patients with STEMI treated with primary PCI. Open Heart. (2016) 3(1):e000405. doi: 10.1136/openhrt-2016-000405
15. Otter W, Kleybrink S, Doering W, Standl E, Schnell O. Hospital outcome of acute myocardial infarction in patients with and without diabetes mellitus. Diabet Med. (2004) 21(2):183–7. doi: 10.1111/j.1464-5491.2004.01114.x
16. Miettinen H, Lehto S, Salomaa V, Mahonen M, Niemela M, Haffner SM, et al. Impact of diabetes on mortality after the first myocardial infarction. The FINMONICA myocardial infarction register study group. Diabetes Care. (1998) 21(1):69–75. doi: 10.2337/diacare.21.1.69
17. Barbash GI, Reiner J, White HD, Wilcox RG, Armstrong PW, Sadowski Z, et al. Evaluation of paradoxic beneficial effects of smoking in patients receiving thrombolytic therapy for acute myocardial infarction: mechanism of the “smoker’s paradox” from the GUSTO-I trial, with angiographic insights. Global utilization of streptokinase and tissue-plasminogen activator for occluded coronary arteries. J Am Coll Cardiol. (1995) 26(5):1222–9. doi: 10.1016/0735-1097(95)00299-5
18. DeGeare VS, Boura JA, Grines LL, O'Neill WW, Grines CL. Predictive value of the killip classification in patients undergoing primary percutaneous coronary intervention for acute myocardial infarction. Am J Cardiol. (2001) 87(9):1035–8. doi: 10.1016/S0002-9149(01)01457-6
19. Schubert J, Lindahl B, Melhus H, Renlund H, Leosdottir M, Yari A, et al. Elevated low-density lipoprotein cholesterol: an inverse marker of morbidity and mortality in patients with myocardial infarction. J Intern Med. (2023) 294(5):616–27. doi: 10.1111/joim.13656
20. Rollando D, Puggioni E, Robotti S, De Lisi A, Ferrari Bravo M, Vardanega A, et al. Symptom onset-to-balloon time and mortality in the first seven years after STEMI treated with primary percutaneous coronary intervention. Heart. (2012) 98(23):1738–42. doi: 10.1136/heartjnl-2012-302536
21. Farshid A, Allada C, Chandrasekhar J, Marley P, McGill D, O'Connor S, et al. Shorter ischaemic time and improved survival with pre-hospital STEMI diagnosis and direct transfer for primary PCI. Heart Lung Circ. (2015) 24(3):234–40. doi: 10.1016/j.hlc.2014.09.015
22. Bental T, Assali A, Vaknin-Assa H, Lev EI, Brosh D, Fuchs S, et al. A comparative analysis of major clinical outcomes using drug-eluting stents versus bare-metal stents in a large consecutive patient cohort. Catheter Cardiovasc Interv. (2010) 76(3):374–80. doi: 10.1002/ccd.22507
23. Braveman P. Health disparities and health equity: concepts and measurement. Annu Rev Public Health. (2006) 27(2006):167–94. doi: 10.1146/annurev.publhealth.27.021405.102103
24. Sumriddetchkajorn K, Shimazaki K, Ono T, Kusaba T, Sato K, Kobayashi N. Universal health coverage and primary care, Thailand. Bull World Health Organ. (2019) 97(6):415–22. doi: 10.2471/BLT.18.223693
25. Limwattananon C, Jaratpatthararoj J, Thungthong J, Limwattananon P, Kitkhuandee A. Access to reperfusion therapy and mortality outcomes in patients with ST-segment elevation myocardial infarction under universal health coverage in Thailand. BMC Cardiovasc Disord. (2020) 20(1):121. doi: 10.1186/s12872-020-01379-3
Keywords: STEMI, ST-elevation myocardial infarction, healthcare, percutaneous coronary intervention, Thailand, mortality, PCI
Citation: Chumsantivut S, Lertmaharit S, Rattananupong T, Lertsuwunseri V, Athisakul S, Wanlapakorn C and Srimahachota S (2024) Mortality rate of percutaneous coronary interventions in ST-segment elevation myocardial infarction patients under the public health insurance schemes of Thailand. Front. Cardiovasc. Med. 11:1397015. doi: 10.3389/fcvm.2024.1397015
Received: 6 March 2024; Accepted: 7 May 2024;
Published: 4 October 2024.
Edited by:
Rajeev Gupta, Emirates International Hospital, United Arab EmiratesReviewed by:
Mohammed Najeeb Osman, University Hospitals Cleveland Medical Center, United StatesGhada Youssef, Cairo University, Egypt
Copyright: © 2024 Chumsantivut, Lertmaharit, Rattananupong, Lertsuwunseri, Athisakul, Wanlapakorn and Srimahachota. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Suphot Srimahachota, c19zcmltYWhhY2hvdGFAeWFob28uY28udGg=
 Suppavit Chumsantivut
Suppavit Chumsantivut Somrat Lertmaharit1
Somrat Lertmaharit1 Thanapoom Rattananupong
Thanapoom Rattananupong