
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med. , 07 May 2024
Sec. Cardiovascular Surgery
Volume 11 - 2024 | https://doi.org/10.3389/fcvm.2024.1393921
 Ryohei Ushioda1,2
Ryohei Ushioda1,2 Aina Hirofuji2*
Aina Hirofuji2* Dit Yoongtong1
Dit Yoongtong1 Boonsap Sakboon1
Boonsap Sakboon1 Jaroen Cheewinmethasiri1
Jaroen Cheewinmethasiri1 Thanin Lokeskrawee3
Thanin Lokeskrawee3 Jayanton Patumanond4
Jayanton Patumanond4 Suppachai Lawanaskol5
Suppachai Lawanaskol5 Hiroyuki Kamiya2
Hiroyuki Kamiya2 Nuttapon Arayawudhikul1
Nuttapon Arayawudhikul1
Introduction: The procedure called the “aorta no-touch” (NT) or anaortic technique in off-pump coronary artery bypass grafting (OPCAB) is designed to reduce the perioperative risk of stroke. We have observed an increased frequency of anaortic OPCAB procedures at our institution. The main purpose of the present study is to investigate the effectiveness of anaortic OPCAB in reducing the perioperative risk of stroke.
Methods: From April 2011 to July 2023, a total of 2,236 patients underwent isolated OPCAB at our single center. The patients were divided into the anaortic group (NT, n = 762) and the aortic group (A, n = 1,474). The NT group was propensity score-matched (PSM) with the A group at a 1:1 ratio (NT n = 640; A n = 640), and matching was performed based on 26 covariates with preoperative clinical characteristics.
Results: In both the unmatched and matched cohorts of the NT and A groups, there were no significant differences observed in new stroke rates (NT vs. A; unmatched, 1.0% vs. 1.2%, p = 0.624; matched, 0.9% vs. 1.3%, p = 0.789). The univariable logistic analysis did not identify the anaortic technique as an independent factor negatively associated with new stroke events (OR = 0.81, 95% CI = 0.35–1.86, p = 0.624).
Conclusion: The present study did not find the anaortic technique to reduce the perioperative risk of stroke in OPCAB. Hence, further large studies are needed to identify patient cohorts in which anaortic OPCAB is significantly beneficial.
Numerous studies have investigated the outcomes, advantages, and challenges associated with off-pump coronary artery bypass grafting (OPCAB) performed with the aorta no-touch (anaortic) technique (1, 2). This strategic approach notably reduces the perioperative risk of stroke (3), yet it demands advanced techniques such as harvesting skeletonized arterial grafts to ensure sufficient length, the creation of composite grafts, and precise graft alignment during sequential bypass. Despite its patient-centric advantages, the adoption of this technically demanding procedure remains limited, with only a handful of cardiac surgeons venturing into this style of operation, likely owing to its significant learning curve (4). Our department has routinely performed OPCAB for patients with coronary artery diseases since 2011 and recently shifted to performing anaortic OPCAB with more frequency in cases that appear theoretically and anatomically reasonable. This study investigated whether anaortic OPCAB was more effective for stroke reduction.
From April 2011 to July 2023, a total of 2,236 patients underwent isolated OPCAB in our center. These patients were divided into two groups based on the presence or absence of aortic manipulation, namely, the anaortic group [“aorta no-touch” (NT), n = 762] and the aortic group (A, n = 1,474). Univariable or multivariable logistic regression analyses were used to identify independent prognostic factors of a new stroke. In addition, the NT group was propensity score-matched (PSM) with the A group at a 1:1 ratio (NT, n = 640; A, n = 640), and matching was performed based on 26 covariates of preoperative clinical characteristics. After matching, patient characteristics, preoperative evaluation details, operative procedures, and postoperative outcomes were compared between both groups. The institutional review board of Lampang Hospital approved this retrospective study and waived the need for written patient consent. A new stroke was defined as the development of a new focal neurologic deficit confirmed by clinical findings and a computed tomography (CT) scan within the duration of the patient’s hospital stay. Strokes occurring after discharge were defined as long-term stroke events. In postoperative management, dual antiplatelet therapy was prescribed as discharge medication.
All patients in the present study underwent OPCAB. Our institution has a total of five surgeons, each of whom performed anaortic OPCAB. The operative procedures were as follows. The approach was through median sternotomy or left mini-thoracotomy, and the target vessel for each anastomosis was appropriately exposed using a tissue stabilizer (Octopus tissue stabilizer, Medtronic, Minneapolis, MN, USA) with or without a deep pericardial stitch or a heart positioner such as the Starfish heart positioner (Medtronic). Graft selection and bypass design were determined by the primary surgeon, and complete revascularizations of the major coronary artery branches were achieved in every case. Prior to arteriotomy, stitches were placed in both the proximal and distal regions of the target vessels using elastic silicone tubing or monofilament suture material. 8-0 polypropylene sutures were used for anastomosis with the internal thoracic artery, while 7-0 polypropylene sutures were used for anastomosis with the gastroepiploic or radial artery. Our institution prioritizes the anaortic approach for OPCAB when it appears theoretically and anatomically suitable. Anaoritc OPCAB was performed in 34.1% (n = 762) of all OPCAB cases, mainly in patients with all arterial revascularisation, left mini-thoracotomy including minimally invasive direct coronary artery bypass grafting (MIDCAB), and preoperative CT showing severe aortic calcification. In OPCAB with aortic manipulation (n = 1,414), aortic side clamping was mainly utilized for proximal anastomosis onto the ascending aorta, and an anastomosis assist device (Guidant Heartstring, Guidant Corporation, Santa Clara, CA, USA, n = 5; Enclose II, Novare Surgical Systems, Cupertino, CA, USA, n = 55) was used sporadically. In patients who present with poor preoperative conditions or require multiple distal anastomoses, we consider performing the aorta-coronary bypass technique by saphenous vein. However, in patients with a history of cerebrovascular events, we actively opt for the anaortic approach.
Preoperative CT scans were only performed in patients aged over 75 years and those suspected of aortic risk based on their x-rays. In postoperative management, dual antiplatelet therapy was prescribed as discharge medication. The use of anticoagulants was not standard practice in our study population. However, in patients who developed atrial fibrillation (AF) a few days postoperatively, warfarin was prescribed, and prothrombin time international normalized ratio (PT INR) levels were monitored and maintained within the range of 2–3.
The patients were followed up every 6 months at our outpatient clinic. Information on all causes of death and cardiac complications during the follow-up period was obtained from Lampang Hospital's database. We achieved a 100% follow-up rate by contacting both the patients and their families for any missing data.
Group assignments were not randomized because the operative approach was a matter of subjective choice. Therefore, we calculated standardized mean differences before and after PSM to assess the balance of variables between the groups. The propensity score (PS) was obtained from a logistic regression model, including 23 covariables presented in Table 1, excluding the European System for Cardiac Operative Risk Evaluation (Euro SCORE) Ⅱ, Society of Thoracic Surgeons (STS) score, and emergent case (Table 2). Patients were matched at a 1:1 ratio using the nearest neighbor matching method without replacement and a caliper width of 0.2 of the standard deviation of the logit of the estimated PS. The continuous variables exhibiting a normal distribution were tested using the t-test, and the continuous variables exhibiting a non-normal distribution were tested using the Mann–Whitney U-test. For the categorical variables, McNemar's test was conducted in the matched cohort, while Fisher's exact test and chi-square test were performed in the unmatched cohort. Statistical significance was set at p < 0.05. The Kaplan–Meier method was used to demonstrate survival rate and freedom from major adverse cardiac or cerebrovascular events (MACCE). The STATA software/MP version 17.0 (Stata Corporation, College Station, TX, USA) was used for the statistical analyses.
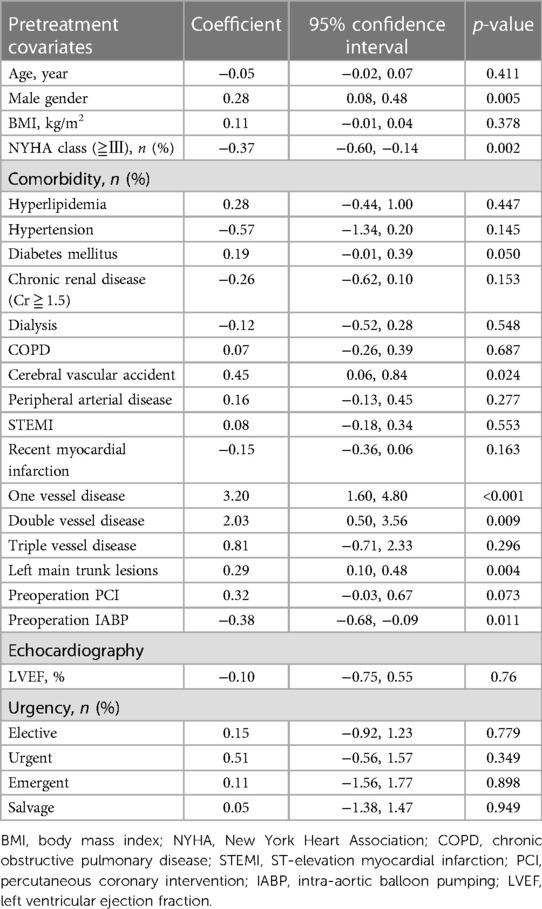
Table 2. Derivation of propensity score equation from pretreatment covariates under multivariable binary logistic regression.
Preoperative patient characteristics before and after matching are presented in Table 1. In the order of NT group and A group, there were 481 (63.1%) and 850 (57.7%) males, with mean ages of 64.4 ± 8.6 and 65.0 ± 8.4 years in the unmatched cohort, and 403 (63.0%) and 403 (63.0%) males, with mean ages of 64.5 ± 8.5 and 64.7 ± 8.3 years in the matched cohort. After matching, all categories showed a standardized mean difference below 0.1.
Intraoperative results between the two groups are presented in Table 3. After matching, the use of intraoperative blood transfusion was significantly higher in the A group (65.8% vs. 77.7%, p < 0.001).
The period from April 2011 to March 2017 was defined as the early-term operation, which was significantly higher in the NT group (86.7% vs. 66.9%, p < 0.001). The number of distal anastomoses (3.0 ± 1.1 vs. 3.3 ± 0.9, p < 0.001) and graft number (2.7 ± 0.9 vs. 2.9 ± 0.8, p < 0.001) were significantly higher in the A group compared to the NT group. Multiple arterial grafting rate was higher in the NT group (NT vs. A; more than two arterial grafts, 77.3% vs. 43.8%, p < 0.001; total arterial revascularization, 67.7% vs. 6.1%, p < 0.001). The use of the left internal thoracic artery (98.8% vs. 95.5%, p < 0.001), right internal thoracic artery (66.4% vs. 12.3%, p < 0.001), and gastroepiploic artery (26.8% vs. 0.6%, p < 0.001) were respectively significantly higher in the NT group, whereas the use of the saphenous vein (30.0% vs. 93.9%, p < 0.001) was higher in the A group.
Table 4 shows the postoperative results between NT and A groups. There was no difference in new stroke rates: 1.0% vs. 1.2% (p = 0.624) in the before-matched cohort and 0.9% vs. 1.3% (p = 0.789) in the matched cohort in the NT and A groups, respectively. There was also no difference in 30-day mortality; 1.7% vs. 2.9% (p = 0.069) in the before-matched cohort and 1.7% vs. 2.0% (p = 0.837) in the matched cohort in NT and A groups, respectively. After PSM, the rates of new-onset AF (18.6% vs. 24.4%, p = 0.012) and median drain contents (IQR) [400 (300–500) ml vs. 400 (320–550) ml, p = 0.021] were significantly lower in the NT group compared to the A group. There were no statistically significant differences in the duration of intensive care unit (ICU) or hospital stay, other major complications, or MACCE event rates between the two groups.
After PSM, the Kaplan–Meier curves of the postoperative MACCE-free rate and survival rate are shown in Figure 1. There were no significant differences in each item between the two groups (MACCE-free rate, p = 0.228; survival rate, p = 0.783). Additionally, the anaortic technique did not show a difference in long-term stroke events after OPCAB (p = 0.948, Figure 2).
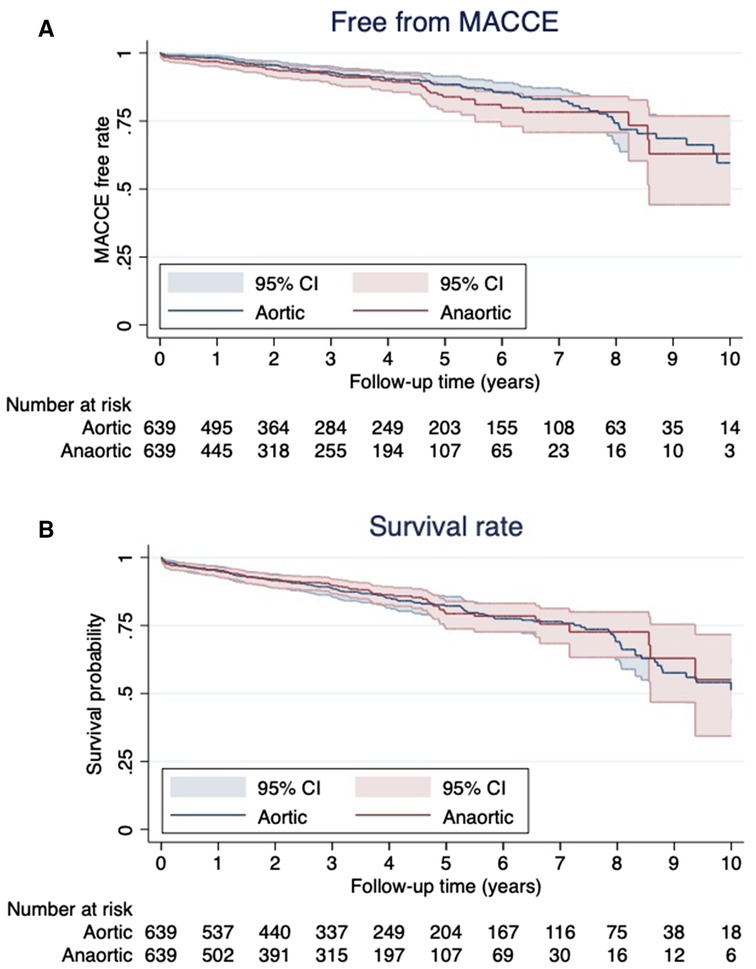
Figure 1. Kaplan–Meier analysis for major adverse cardiac or cerebrovascular event (MACCE)-free rate (A) and survival rate (B).
The univariable and multivariable risk regression analyses performed to identify risk factors for new stroke are presented in Table 5. The univariable analysis indicated that the risk factors for new strokes included a history of cerebral vascular accident (CVA), peripheral vessel disease (PVD), salvage operative status, reoperation due to postoperative bleeding, and postoperative new-onset AF. However, the anaortic technique was not identified as an independent factor negatively associated with new stroke events (OR = 0.81, 95% CI = 0.35–1.86, p = 0.624). The history of PVD (OR = 2.38, 95% CI = 1.02–5.56, p = 0.045) and new-onset AF (OR = 4.45, 95% CI = 1.98–10.01, p < 0.001) were significant risk factors in the multivariable analysis of these factors.
Contrary to previous reports (1–3), there was no association observed between postoperative stroke and aortic manipulation in OPCAB surgery in our single-center study. Moreover, anaortic OPCAB had no positive impact on long-term stroke prevention.
Recent reports have claimed that there is little difference in outcome for most patients between OPCAB and conventional CABG (5, 6). However, it is also well accepted that OPCAB is valuable in reducing the risk of stroke and preserving the heart and renal function in higher-risk patients and that the most reliable tactics for avoiding perioperative stroke are the maintenance of blood pressure and the avoiding aortic manipulation (7–9). For these reasons, the anaortic technique OPCAB has been hailed for preventing the incidence of new stroke events. Pawliszak et al. (3) reported a meta-analysis comparing anaortic technique and proximal anastomosis devices with side-clamp OPCAB3 involving 25,163 patients across 18 studies. The anaortic technique demonstrated a decrease in postoperative cerebrovascular events of nearly 60%, compared to side-clamp OPCAB, and this benefit was consistent across different patient risk levels. In another study, Zhao et al. (9) conducted a meta-analysis comparing post-CABG outcomes, incorporating data from 13 studies with 37,720 patients. They concluded that anaortic OPCAB was the most effective treatment for decreasing the postoperative risk of stroke. However, it was not evident in our study that anaortic OPCAB reduces the incidence of perioperative strokes (NT 0.9% vs. A 1.3%, p = 0.789). In addition, the univariable analysis indicated that the risk factors for new strokes were not associated with the aortic technique. Generally, the important and major risk factors for stroke after CABG were as follows: old age, aortic atheromatous disease, aortic manipulation, diabetes, female sex, hypertension, PVD, previous neurological injury, symptomatic carotid stenosis, and use of cardiopulmonary bypass (CPB) (10, 11). Our study demonstrated that a history of PVD (OR = 2.38, 95% CI = 1.02–5.56, p = 0.045) and new-onset AF (OR = 4.45, 95% CI = 1.98–10.01, p < 0.001) were significant risk factors in the multivariable analysis. This implies that adopting the anaortic technique may not be universally consequential in averting the onset of new strokes. While the anaortic technique need not be performed routinely for the sake of reducing perioperative stroke risk, it should always remain a viable option when performing OPCAB for patients with a high risk of stroke.
When anaortic techniques are performed, the internal thoracic arteries are commonly used, and reap the benefits of multiple artery grafts or total arterial reconstruction (TAR) (12–14). However, it has not been reported that the anaortic technique improves the long-term survival rate or the incidence of MACCE. Furukawa et al. (15) reported a prospective study comparing mid-term outcomes of anaortic OPCAB (n = 1,233), clampless OPCAB (n = 2,310), and conventional CABG (n = 1,879). Their study showed no difference in MACCE nor mortality in mid-term outcomes between the three groups. In our study, despite multiple arterial grafting rates being higher in the NT group than in the A group (aortic manipulation group), there were no significant differences in either the MACCE-free (p = 0.228) rates or survival rates (p = 0.783) between the two groups. In addition, the anaortic technique did not reduce long-term stroke events after OPCAB (p = 0.948). Albert et al. (16) elucidated the impact of the anaortic technique on post-CABG strokes (n = 4,485) compared with on-pump CABG (n = 8,794). They reported anaortic OPCAB resulted in a significant reduction of the overall postoperative risk of stroke (0.45% vs. 1.28% in CPB patients; p = 0.0001), but delayed strokes were not significantly reduced [0.37% (95% CI, 0.18%–0.57%) vs. 0.46% (95% CI, 0.24%–0.67%)] in anaortic OPCAB vs. CPB patients, respectively (p = 0.5749). These results show that although anaortic OPCAB is not beneficiary in preventing long-term strokes, it reduces the risk of strokes caused by acute perioperative embolism from the thoracic aorta. However, anaortic techniques may supply long-term benefits to patients in other aspects.
According to recent guidelines (17, 18), multiple arterial revascularizations, application of different appropriate modalities, and unclamping the ascending aorta to avoid stroke are all recommended strategies. The whole operation requires various procedures: (1) a skeletonized technique for harvesting the arterial conduits, (2) a traction technique to create the best exposure without hemodynamic compromise using appropriate instruments, (3) generation of composite grafts followed by optimal alignment of the conduits without kinking, and (4) a technique with a high level of anastomoses. All of these procedures must be performed with the heart still beating, which is not the case in conventional CABG. Due to the high level of technicality required, it is challenging for a surgeon who is not familiar with the knacks and pitfalls of anaortic OPCAB to perform and complete the procedure in its entirety safely. To perform anaortic technique reproducibly and with satisfactory outcomes, it is important to incorporate OPCAB into regular practice, to enable not only the surgeons but also the medical staff, to acquire abundant experience of OPCAB procedures (19). In our institution, the anaortic technique has been established as a method of choice for all OPCAB patients, so operation times and major complication rates were not significantly different.
To point out some important limitations, first, this is a retrospective, non-randomized analysis from a single medical center. Second, PSM was based on preoperational patient characteristics, with several unmeasured confounders. In addition, although we included many patients in this study, it remains underpowered to properly assess the true effect of anaortic OPCAB on the studied outcome because the new stroke rate was a rare complication (approximately 1%). Third, there was a selection bias in favor of choosing the anaortic technique, which tended to be more frequently employed in patients with aortic disease. In this study, procedures in the A group utilized anastomosis assist devices while all anastomoses were done purely manually in the NT group. Additionally, the application of anastomosis assist devices was constrained, primarily due to a lack of insurance reimbursement in Thailand. Fourth, we did not conduct consistent preoperative assessments, such as head lack of magnetic resonance imaging (MRI) or CT scans, for brain imaging in many patients. Consequently, the information regarding previous CVA may not be accurate. Finally, the asymptomatic strokes were not included in our analysis due to the lack of routine postoperative head CT scans.
The present study did not find the anaortic technique to reduce the perioperative risk of stroke in OPCAB. Hence, further large studies are needed to identify patient cohorts in which anaortic OPCAB is significantly beneficial.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Dr. Artit Wongpaliboonwatana/Chairman of the Lampang Human Research Ethics Committee. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
RU: Data curation, Writing – original draft. AH: Writing – review & editing. DY: Resources, Writing – review & editing. BS: Resources, Writing – review & editing. JC: Resources, Writing – review & editing. TL: Formal Analysis, Writing – review & editing. JP: Formal Analysis, Writing – review & editing. SL: Formal Analysis, Writing – review & editing. HK: Conceptualization, Methodology, Project administration, Writing – review & editing. NA: Conceptualization, Methodology, Resources, Writing – review & editing.
The authors declare that no financial support was received for the research, authorship, and/or publication of this article.
We would like to express our sincere gratitude to the faculty and team of Chiang Mai University and Lampang Hospital for their valuable assistance in the statistical analysis of this research. Their expertise and support played a crucial role in ensuring the accuracy of our data analysis.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Börgermann J, Hakim K, Renner A, Parsa A, Aboud A, Becker T, et al. Clampless off-pump versus conventional coronary artery revascularization: a propensity score analysis of 788 patients. Circulation. (2012) 126(11 Suppl 1):S176–82. doi: 10.1161/CIRCULATIONAHA.111.084285
2. Vallely MP, Yan TD, Edelman JJ, Hayman M, Brereton RJ, Ross DE. Anaortic, total-arterial, off-pump coronary artery bypass surgery: how to do it. Heart Lung Circ. (2010) 19(9):555–60. doi: 10.1016/j.hlc.2010.04.078
3. Pawliszak W, Kowalewski M, Raffa GM, Malvindi PG, Kowalkowska ME, Szwed KA, et al. Cerebrovascular events after no-touch off-pump coronary artery bypass grafting, conventional side-clamp off-pump coronary artery bypass, and proximal anastomotic devices: a meta-analysis. J Am Heart Assoc. (2016) 5(2):e002802. doi: 10.1161/JAHA.115.002802
4. Smith TA, Asimakopoulos G. How safe is it to train residents to perform off-pump coronary artery bypass surgery? Interact Cardiovasc Thorac Surg. (2015) 20(5):658–61. doi: 10.1093/icvts/ivu447
5. Lamy A, Devereaux PJ, Prabhakaran D, Taggart DP, Hu S, Straka Z, et al. Five-year outcomes after off-pump or on-pump coronary-artery bypass grafting. N Engl J Med. (2016) 375(24):2359–68. doi: 10.1056/NEJMoa1601564
6. Quin JA, Wagner TH, Hattler B, Carr BM, Collins J, Almassi GH, et al. Ten-year outcomes of off-pump vs. on-pump coronary artery bypass grafting in the Department of Veterans Affairs: a randomized clinical trial. JAMA Surg. (2022) 157(4):303–10. doi: 10.1001/jamasurg.2021.7578
7. Emmert MY, Seifert B, Wilhelm M, Grünenfelder J, Falk V, Salzberg SP. Aortic no-touch technique makes the difference in off-pump coronary artery bypass grafting. J Thorac Cardiovasc Surg. (2011) 142(6):1499–506. doi: 10.1016/j.jtcvs.2011.04.031
8. Falk V. Stay off-pump and do not touch the aorta!. Eur Heart J. (2010) 31(3):278–80. doi: 10.1093/eurheartj/ehp527
9. Zhao DF, Edelman JJ, Seco M, Bannon PG, Wilson MK, Byrom MJ, et al. Coronary artery bypass grafting with and without manipulation of the ascending aorta: a network meta-analysis. J Am Coll Cardiol. (2017) 69(8):924–36. doi: 10.1016/j.jacc.2016.11.071
10. Bergman P, Hadjinikolaou L, Dellgren G, van der Linden J. A policy to reduce stroke in patients with extensive atherosclerosis of the ascending aorta undergoing coronary surgery. Interact Cardiovasc Thorac Surg. (2004) 3(1):28–32. doi: 10.1016/S1569-9293(03)00219-6
11. Raja SG. Total arterial off-pump coronary revascularization: the holy grail? Curr Opin Cardiol. (2019) 34(5):552–6. doi: 10.1097/HCO.0000000000000645
12. Zacharias A, Schwann TA, Riordan CJ, Durham SJ, Shah AS, Habib RH. Late results of conventional versus all-arterial revascularization based on internal thoracic and radial artery grafting. Ann Thorac Surg. (2009) 87(1):19–26.e2. doi: 10.1016/j.athoracsur.2008.09.050
13. Buxton BF, Shi WY, Tatoulis J, Fuller JA, Rosalion A, Hayward PA. Total arterial revascularization with internal thoracic and radial artery grafts in triple-vessel coronary artery disease is associated with improved survival. J Thorac Cardiovasc Surg. (2014) 148(4):1238–43; discussion 1243–4. doi: 10.1016/j.jtcvs.2014.06.056
14. Locker C, Schaff HV, Daly RC, Dearani JA, Bell MR, Frye RL, et al. Multiple arterial grafts improve survival with coronary artery bypass graft surgery versus conventional coronary artery bypass grafting compared with percutaneous coronary interventions. J Thorac Cardiovasc Surg. (2016) 152(2):369–79.e4. doi: 10.1016/j.jtcvs.2016.03.089
15. Furukawa N, Kuss O, Preindl K, Renner A, Aboud A, Hakim-Meibodi K, et al. Anaortic off-pump versus clampless off-pump using the PAS-Port device versus conventional coronary artery bypass grafting: mid-term results from a matched propensity score analysis of 5422 unselected patients. Eur J Cardiothorac Surg. (2017) 52(4):760–7. doi: 10.1093/ejcts/ezx235
16. Albert A, Ennker J, Hegazy Y, Ullrich S, Petrov G, Akhyari P, et al. Implementation of the aortic no-touch technique to reduce stroke after off-pump coronary surgery. J Thorac Cardiovasc Surg. (2018) 156(2):544–54.e4. doi: 10.1016/j.jtcvs.2018.02.111
17. Benedetto U, Amrani M, Gaer J, Bahrami T, de Robertis F, Simon AR, et al. The influence of bilateral internal mammary arteries on short- and long-term outcomes: a propensity score matching in accordance with current recommendations. J Thorac Cardiovasc Surg. (2014) 148(6):2699–705. doi: 10.1016/j.jtcvs.2014.08.021
18. Kelly R, Buth KJ, Légaré JF. Bilateral internal thoracic artery grafting is superior to other forms of multiple arterial grafting in providing survival benefit after coronary bypass surgery. J Thorac Cardiovasc Surg. (2012) 144(6):1408–15. doi: 10.1016/j.jtcvs.2012.01.030
Keywords: anaortic, aorta no-touch technique, off-pump coronary artery bypass grafting, stroke, propensity score matching
Citation: Ushioda R, Hirofuji A, Yoongtong D, Sakboon B, Cheewinmethasiri J, Lokeskrawee T, Patumanond J, Lawanaskol S, Kamiya H and Arayawudhikul N (2024) Assessing the benefits of anaortic off-pump coronary artery bypass grafting. Front. Cardiovasc. Med. 11:1393921. doi: 10.3389/fcvm.2024.1393921
Received: 29 February 2024; Accepted: 22 April 2024;
Published: 7 May 2024.
Edited by:
Giuseppe Gatti, Azienda Sanitaria Universitaria Giuliano Isontina, ItalyReviewed by:
Thierry Caus, University of Picardie Jules Verne, France© 2024 Ushioda, Hirofuji, Yoongtong, Sakboon, Cheewinmethasiri, Lokeskrawee, Patumanond, Lawanaskol, Kamiya and Arayawudhikul. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Aina Hirofuji bmVvbGVub3JlNzhAZ21haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.