- Department of Peripheral Vascular Diseases, The First Affiliated Hospital of Xi’an Jiaotong University, Xi’an, Shaanxi, China
Background: Behcet's disease (BD) is a systematic vasculitis that affects vessels with various sizes, presenting as venous thrombosis and arterial pseudoaneurysms. The most severe manifestation in BD is ascending aortic pseudoaneurysm, which is associated with high risks of rupture and mortality.
Case presentation: We present a case of ascending aortic pseudoaneurysm in a 50-year-old patient with BD. After preoperative evaluation, coil embolization was successfully performed to treat the pseudoaneurysm, resulting in a satisfactory outcome at the 1-year follow-up.
Conclusion: Coil embolization serves as an effective treatment option for ascending aortic pseudoaneurysm in BD when open surgical repair and stent graft placement are unsuitable.
1 Introduction
Pseudoaneurysm of the ascending aorta represents a rare vascular complication in patients with Behcet's disease (BD) and carries a potentially fatal risk (1). Given the heightened threat of rupture and mortality, these individuals often necessitate either open surgical or endovascular repair. While traditional open surgical repair remains a viable option for select patients, the presence of anastomotic complications contributes to an unfavorable outcome, including issues such as leakage, occlusion, and pseudoaneurysm formation (2). Recently, mounting evidence has underscored the efficacy of endovascular repair (3, 4).
In this report, we present a case of ascending aortic pseudoaneurysm in a patient with BD, successfully managed through coil embolization, leading to a favorable outcome at the one-year follow-up. Consent was obtained from the patient for the publication of this data.
2 Case presentation
The patient, a 50-year-old man with a confirmed 16-year diagnosis of BD, was referred to our hospital because a recent computed tomography angiogram (CTA) conducted at another facility had shown a pseudoaneurysm of the ascending aorta. He had reported left-sided chest pain since 2 weeks prior. The patient was known with visual impairment, which was attributed to recurrent episodes of ocular inflammation, and over the last several years, he had experienced approximately 10–20 oral ulcers per year. Prior treatment with colchicine proved ineffective. Consequently, rheumatologists had adjusted the treatment regimen to incorporate glucocorticoids, cyclosporine, and adalimumab. However, during the tapering of adalimumab, the patient had experienced recurrent erythema nodosum in the extremities. The patient had discontinued adalimumab for 10 days upon admission to our center.
Additionally, the patient had comorbidities including hypertension and type II diabetes mellitus, for which long-term telmisartan 40 mg once daily and metformin 500 mg twice daily were prescribed. Upon admission, the patient reported mild left-sided chest pain, without accompanying compressive symptoms such as shortness of breath, dysphagia, stridor, or hoarseness. This subtle clinical presentation may be attributed to the pseudoaneurysm of the ascending aorta associated with BD, which can exhibit slow growth or even remain stable for a prolonged period, resulting in a lack of overt symptoms during chronic progression. The patient presented with a blood pressure of 117/53 mmHg and a heart rate of 65 beats/minute. A comprehensive physical examination revealed normal heart rhythm and apical position, absence of abnormal pulsations in the precordial region, and no pathological murmurs in the valve area. Electrocardiogram findings and biomarkers for cardiac injury were within normal ranges, excluding acute coronary syndrome.
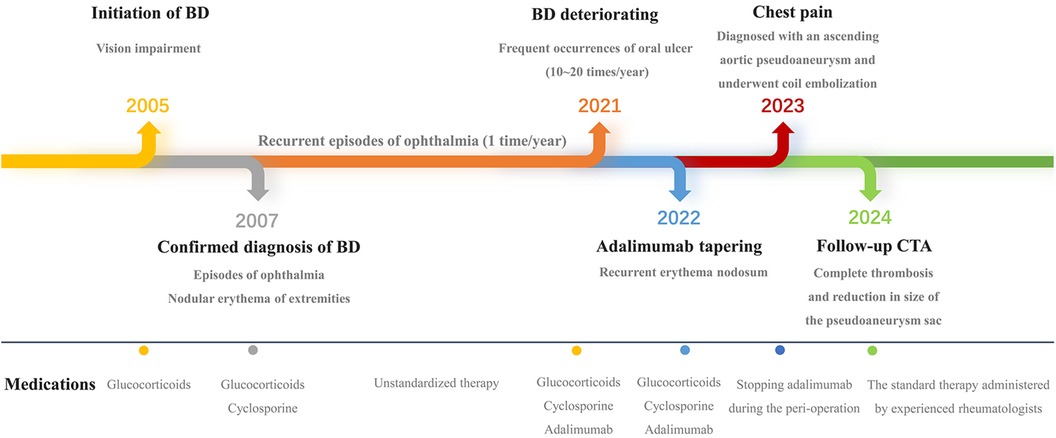
The patient had a hemoglobin level of 124 g/L (reference range 130–175 g/L), a high-sensitive C-reactive protein level of 8.08 mg/L (reference range 0–3 mg/L), and an erythrocyte sedimentation rate of 28 mm/h (reference range 0–15 mm/h). CTA revealed an ascending aortic pseudoaneurysm with a patchy hypodense opacity along the irregular wall of the aortic arch, indicative of an inflammatory condition. Preoperative CTA was used to evaluate morphology and size of the pseudoaneurysm. The aortic pseudoaneurysm was situated in the anterior wall of the ascending aorta, approximately 39 mm from the aortic sinus. The diameter of the neck of the pseudoaneurysm measured 6 mm, whereas its maximum sac diameter reached up to 18 mm, with an adhered thrombus with a maximum thickness of 23 mm observed on its external surface (Figure 1).
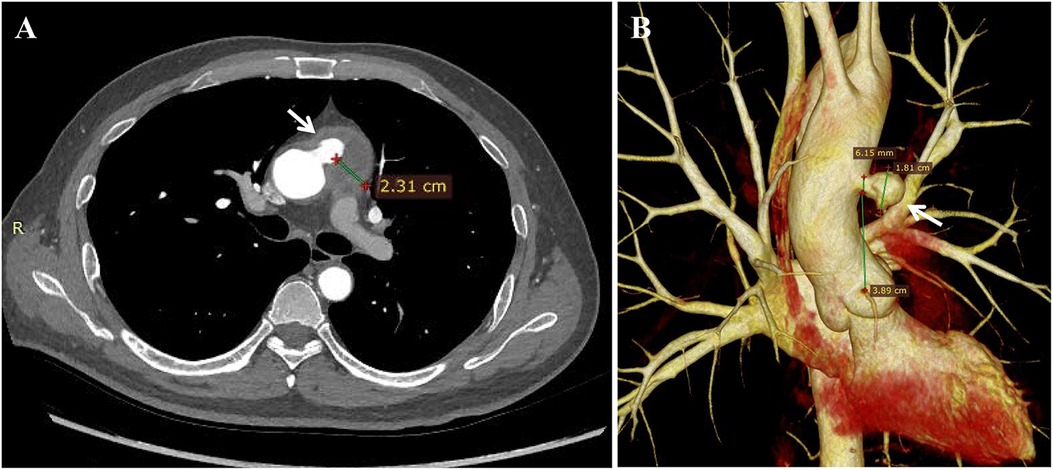
Figure 1. Preoperative CT angiography revealed (A) the pseudoaneurysm located at the anterior wall of the ascending aorta (indicated by the white arrow), with an adhered thrombus of maximum thickness 23 mm observed on its external surface. (B) Morphological measurements of the lesion were obtained from 3D reconstructed images, showing a maximum pseudoaneurysm neck diameter of 6 mm, maximum pseudoaneurysm sac diameter of 18 mm, and a distance of 39 mm from the aortic sinus to the pseudoaneurysm.
After multidisciplinary consultation, decision was made to perform coil embolization. Under local anesthesia, a pigtail catheter was introduced into the proximal end of the ascending aorta via the right femoral artery. Angiography revealed the presence of the pseudoaneurysm, located at the anterior wall of the aorta, with a maximum sac diameter of 20 mm, and a neck diameter of 6.7 mm. Subsequently, the pigtail catheter was replaced with a 5F multifunctional catheter (Terumo, Tokyo, Japan) enclosed in a 6F long sheath (COOK, Bloomington, IN, USA). Five Interlock coils of varying sizes were introduced into the pseudoaneurysm cavity, including one measuring 20–400 mm, two measuring 15–400 mm, and two measuring 10–250 mm. Intraoperative angiography confirmed complete occlusion of the pseudoaneurysm sac with coils, effectively excluding it from arterial blood flow (Figure 2). The procedure duration was 40 min. The patient remained admitted for 6 days and was subsequently discharged. Successful treatment was confirmed by a follow-up CTA scan 1-month postoperatively, which revealed no evidence of endoleak. Subsequent assessment by CTA 1-year postoperatively demonstrated complete thrombosis and reduction in the size of the pseudoaneurysm sac (Figure 3). Meanwhile, the erythrocyte sedimentation rate and high-sensitivity C-reactive protein levels remained within normal ranges with drug treatment. Currently, the patient is being followed up at regular intervals. Cardiac surgery will only be considered in case of occurrence serious, late postoperative complications (The timeline with relevant data from the episode of care is presented in Figure 4).
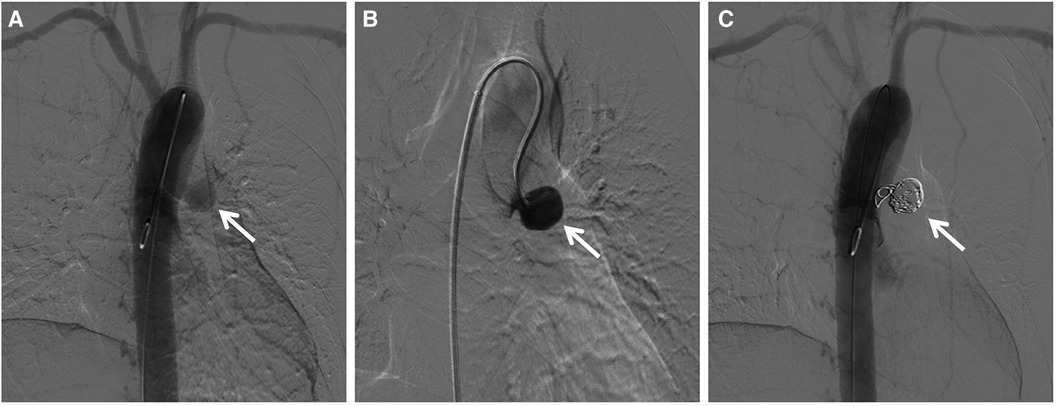
Figure 2. Intraoperative angiogram displayed (A) the anterior wall location of the aortic pseudoaneurysm and (B) clear visualization upon contrast administration. Following coil embolization, the angiogram demonstrated (C) complete occlusion of the pseudoaneurysm sac with coils, leading to exclusion from arterial blood flow (indicated by the white arrow).
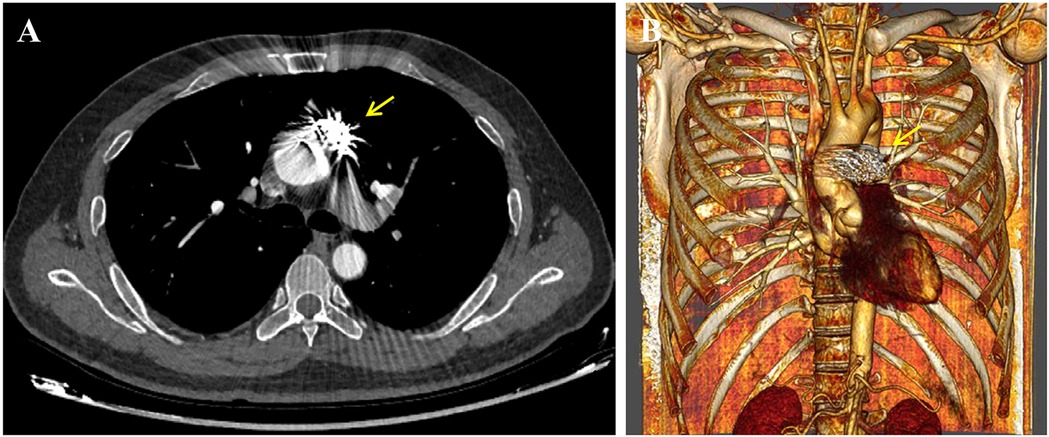
Figure 3. Postoperative CT angiography at the 1-year follow-up depicted (A) complete thrombosis and reduction in the size of the pseudoaneurysm sac. (B) 3D reconstructed image showed secure positioning of the coils without any evidence of migration (indicated by the yellow arrow).
3 Discussion
In addition to oral and genital ulcerations, and relapsing ocular inflammation, BD also affects vessels, including venous thrombosis and arterial pseudoaneurysm (5). Ascending aortic involvement represents one of the most serious complications of BD, with aortic rupture emerging as the leading cause of mortality in patients with vascular involvement (1, 6). The pathogenesis of pseudoaneurysm formation in BD is associated with the occlusion of nutrient vessels within the arterial wall due to pan vasculitis. Chronic inflammation leads to proliferation of fibroblast and smooth muscle cells within the intimal layer, along with deposition in the arterial wall, resulting in destruction of the medial and outer layers. Pseudoaneurysms in patients with BD are highly prone to rupture and necessitate emergency open surgical or endovascular repair.
Open surgical repair has traditionally been considered the gold standard for treating ascending aortic pseudoaneurysms in patients with BD. However, this procedure is associated with high mortality rates and recurrent anastomotic pseudoaneurysms, leading to unfavorable outcomes. A meta-analysis demonstrated that the mortality rate following open surgical repair ranged from 10% to 30%, and 10% to 50% of patients with BD experienced recurrent pseudoaneurysms at the site of anastomosis (7). Moreover, because of the extensive trauma induced by sternotomy, and the deep hypothermic circulatory arrest, patients with major-comorbidities are often poor candidates for surgery.
Recently, endovascular repair has emerged as a novel option for treating pseudoaneurysms of the ascending aorta (3). The three most prevalent procedures include stent graft placement (8), vascular occlusion, and coil embolization (9), all of which have demonstrated reduced invasiveness and considerable efficiency. However, several unresolved questions hinder the widespread adoption of these interventions. Regarding stent graft placement, several challenges exist. Firstly, there is currently no stent graft specifically designed for ascending aortic lesions, limiting the options to off-label use of stent grafts designed for thoracic or abdominal aortic lesions. Secondly, the commercially available delivery systems used in our medical center are primarily designed for descending aortic lesions and may not provide sufficient length to effectively guide the stent graft from the femoral artery to the ascending aorta. Although using either the ventricular apex or axillary artery can reduce the delivery distance, it is unsuitable for patients with BD due to its high invasiveness (10). Lastly, mechanical stimulation and foreign body reactions caused by the stent graft may induce inflammation in the aortic wall (11), potentially leading to the recurrence of pseudoaneurysms at the edge of the stent graft. Several studies have also reported the successful use of endovascular occluders. Tarantini et al. (12) employed two Amplatzer septal occluder devices for percutaneous repair of ascending aortic pseudoaneurysm and aortopulmonary fistula. Komanapalli et al. (13) performed percutaneous repair of an ascending aortic pseudoaneurysm with a septal occluder device. When anatomically suitable, a less invasive approach using a vascular plug or septal occluder is an attractive option (14). However, the precise implantation of occluder devices at the neck of the pseudoaneurysm may pose technical challenges due to the variable location and size of these lesions. Currently, there is a lack of commercially available endovascular occluder devices in many medical centers. While coil embolization has become the preferred treatment for aneurysms in specific locations (15), its efficacy in the ascending aorta, particularly in patients with BD, remains uncertain. D'Ortenzio et al. (16) employed coil embolization to successfully address an aortic root pseudoaneurysm in a patient diagnosed with Loeys-Dietz syndrome. Dziekiewicz et al. (17) utilized coil embolization to treat a patient with post-traumatic pseudoaneurysm of the ascending aorta, demonstrating its efficacy as a safe and viable alternative for managing cases at high-risk for hemorrhage, where heparinization is unfeasible, both as a bridge procedure and as a long-term solution. Kim et al. (9) used coil embolization to address the pseudoaneurysm at the aortic sinotubular junction following multiple aortic operations and achieved a good outcome. Moreover, coil embolization can be used in combination with other endovascular techniques for the management of these patients. Wu et al. (3) combined bare stents with coil embolization to treat patients with vascular BD, resulting in an unsatisfactory outcome. Lyen et al. (18) utilized endovascular treatment to manage thoracic aortic pseudoaneurysms and proposed a novel treatment strategy that combined the use of occluder devices and coils as an effective treatment strategy for these patients. However, the efficacy of using coil embolization technology exclusively as an endovascular treatment option for ascending aortic pseudoaneurysm in patients with BD remains unclear.
To our knowledge, our procedure represents the pioneering use of coil embolization for treating ascending aortic pseudoaneurysms in patients with BD. The decision to employ coil embolization for managing this patient was based on several factors: firstly, the anatomical characteristics of an anterior wall location of the ascending aortic pseudoaneurysm with a narrow neck provided favorable endovascular conditions for coil embolization; secondly, considering the presence of BD in this patient, which renders the aortic wall more vulnerable to damage, we aimed to minimize iatrogenic injury caused by devices such as catheters and wires during the endovascular procedure. However, the utilization of coil embolization in ascending aortic pseudoaneurysms entails potential risks, including intraoperative aortic rupture and incomplete pseudoaneurysm filling, as well as postoperative endoleak and coil migration. To mitigate these adverse events, several key considerations were taken into account during the procedure: (i) gradual release of coils is essential to minimize the risk of pseudoaneurysm rupture; (ii) the combination of different sizes of coils can be employed to achieve complete filling and appropriate oversizing; (iii) precise positioning of coils is crucial to prevent distal migration, therefore we employed controlled-release coils that could be retracted multiple times, adjusted for correct orientation, and subsequently redeployed within the pseudoaneurysm cavity. Pseudoaneurysm at the puncture site is a commonly encountered complication following endovascular repair in patients with BD and vascular involvement. In this case, meticulous attention to the management of the puncture site led to the absence of post-operative pseudoaneurysm at the right femoral artery.
In strict accordance with the European League Against Rheumatism (EULAR) recommendations for the management of BD (19), the patient received regular immunosuppressant and glucocorticoid treatment pre-operatively, with coil embolization scheduled 2 weeks after adalimumab administration in this case, in order to mitigate the risk of postoperative complications such as enlargement or recurrence of pseudoaneurysm. Additionally, experienced rheumatologists adjusted perioperative and postoperative drug dosages to effectively control disease activity. The ESR and hsCRP levels remained within normal ranges during the 1-year postoperative period, indicating that this satisfactory outcome of coil embolization may also be attributed to the sustained administration of immunosuppressants. Therefore, we suggest that standardized continuation of immunosuppressive therapy is strongly recommended following endovascular treatment in patients with vascular BD. Many questions remain unaddressed regarding the long-term durability and safety of transcatheter coil embolization. Nevertheless, this technique seems to serve as a viable alternative for ascending aortic pseudoaneurysm in patients with BD, when open surgical repair or stent graft placement entails a significant risk of postoperative complications.
4 Conclusion
Ascending aortic pseudoaneurysm represents a rare and potentially fatal complication of BD. Coil embolization may present a viable alternative to sternotomy in patients with suitable anatomical characteristics.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
MK: Writing – original draft, Conceptualization, Writing – review & editing. BZ: Writing – review & editing, Resources. HP: Writing – review & editing, Resources. HH: Writing – review & editing, Resources. JZ: Writing – review & editing, Conceptualization, Resources, Supervision.
Funding
The authors declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Bettiol A, Alibaz-Oner F, Direskeneli H, Hatemi G, Saadoun D, Seyahi E, et al. Vascular Behçet syndrome: from pathogenesis to treatment. Nat Rev Rheumatol. (2023) 19(2):111–26. doi: 10.1038/s41584-022-00880-7
2. Gaudric J, Jayet J, Saadoun D, Couture T, Ferfar Y, Davaine JM, et al. Factors influencing the recurrence of arterial involvement after surgical repair in Behçet disease. J Vasc Surg. (2020) 72(5):1761–9. doi: 10.1016/j.jvs.2020.01.076
3. Wu L, Li F, Sun X, Liu Z, Zhou J, Zheng W, et al. Long term outcomes and potential risk factors for endovascular repair of aortic pseudoaneurysms in vascular Behçet’s disease. Eur J Vasc Endovasc Surg. (2023) 66(2):169–77. doi: 10.1016/j.ejvs.2023.04.009
4. Duan L, Lu X, Pan R, Cao D. Recurrent aortic-arch pseudoaneurysm eroding into the left main bronchus following descending thoracic aortic stent repair. J Cardiothorac Surg. (2023) 18(1):11. doi: 10.1186/s13019-023-02112-9
5. Yazici Y, Hatemi G, Bodaghi B, Cheon JH, Suzuki N, Ambrose N, et al. Behçet syndrome. Nature Reviews Disease Primers. (2021) 7(1):67. doi: 10.1038/s41572-021-00301-1
6. Marone EM, Diaco DA, Brioschi C, Argenteri A. Emergent endovascular treatment of thoracoabdominal aortic rupture in Behcet’s disease. Ann Vasc Surg. (2018) 47:282.e7–.e11. doi: 10.1016/j.avsg.2017.09.014
7. Liu CW, Ye W, Liu B, Zeng R, Wu W, Dake MD. Endovascular treatment of aortic pseudoaneurysm in Behçet disease. J Vasc Surg. (2009) 50(5):1025–30. doi: 10.1016/j.jvs.2009.06.009
8. Ohira S, Masuda S, Matsushita T. Nine-year experience of recurrent anastomotic pseudoaneurysms after thoracoabdominal aneurysm graft replacement in a patient with Behçet disease. Heart Lung Circ. (2014) 23(10):e210–3. doi: 10.1016/j.hlc.2014.05.009
9. Kim CH, So YH, Ok YJ, Choi JS. Bail-out coil embolization for a pseudoaneurysm of aortic sinotubular junction in a patient with Behcet’s disease after receiving multiple aortic operations. J Card Surg. (2022) 37(5):1410–2. doi: 10.1111/jocs.16304
10. Roselli EE, Idrees J, Greenberg RK, Johnston DR, Lytle BW. Endovascular stent grafting for ascending aorta repair in high-risk patients. J Thorac Cardiovasc Surg. (2015) 149(1):144–51. doi: 10.1016/j.jtcvs.2014.07.109
11. Kim SW, Lee DY, Kim MD, Won JY, Park SI, Yoon YN, et al. Outcomes of endovascular treatment for aortic pseudoaneurysm in Behcet’s disease. J Vasc Surg. (2014) 59(3):608–14. doi: 10.1016/j.jvs.2013.09.052
12. Tarantini G, Cucchini U, Nai Fovino L. Percutaneous repair of ascending aorta pseudoaneurysm and aortopulmonary fistula with two amplatzer septal occluder devices. Eur Heart J. (2017) 38(37):2853–4. doi: 10.1093/eurheartj/ehw579
13. Komanapalli CB, Burch G, Tripathy U, Slater MS, Song HK. Percutaneous repair of an ascending aortic pseudoaneurysm with a septal occluder device. J Thorac Cardiovasc Surg. (2005) 130(2):603–4. doi: 10.1016/j.jtcvs.2005.02.044
14. Hussain J, Strumpf R, Wheatley G, Diethrich E. Percutaneous closure of aortic pseudoaneurysm by amplatzer occluder device-case series of six patients. Catheter Cardiovasc Interv. (2009) 73(4):521–9. doi: 10.1002/ccd.21833
15. Obara H, Kentaro M, Inoue M, Kitagawa Y. Current management strategies for visceral artery aneurysms: an overview. Surg Today. (2020) 50(1):38–49. doi: 10.1007/s00595-019-01898-3
16. D'Ortenzio R, Cardarelli-Leite L, Dhatt R, Saw J, Heran M. Transarterial coil embolization of an aortic root pseudoaneurym in a patient with loeys-dietz syndrome: a case report. CVIR endovascular. (2020) 3(1):94. doi: 10.1186/s42155-020-00184-5
17. Dziekiewicz MA, Makowski K, Maciąg RB. Coil embolization of post-traumatic pseudoaneurysm of the ascending aorta. Am J Case Rep. (2021) 22:e931844. doi: 10.12659/ajcr.931844
18. Lyen SM, Rodrigues JC, Manghat NE, Hamilton MC, Turner M. Endovascular closure of thoracic aortic pseudoaneurysms: a combined device occlusion and coil embolization technique in patients unsuitable for surgery or stenting. Catheter Cardiovasc Interv. (2016) 88(7):1155–69. doi: 10.1002/ccd.26558
Keywords: Behcet’s disease, ascending aortic pseudoaneurysm, coil embolization, thoracic endovascular repair, computed tomography angiography
Citation: Kang M, Zhang B, Pang H, Hu H and Zhang J (2024) Case Report: Coil embolization of ascending aortic pseudoaneurysm in patient with Behcet's disease. Front. Cardiovasc. Med. 11:1392236. doi: 10.3389/fcvm.2024.1392236
Received: 27 February 2024; Accepted: 24 May 2024;
Published: 6 June 2024.
Edited by:
Gianni Angelini, University of Bristol, United KingdomReviewed by:
Eustaquio Maria Onorato, U.O. Cardiologia Universitaria, Ospedale Galeazzi—Sant’Ambrogio, Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS), ItalyStijn Lochy, University Hospital Brussels, Belgium
© 2024 Kang, Zhang, Pang, Hu and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Junbo Zhang, emhhbmdqdW5ib0B4anR1ZmguZWR1LmNu
 Mengyang Kang
Mengyang Kang Bo Zhang
Bo Zhang Honggang Pang
Honggang Pang Huishe Hu
Huishe Hu Junbo Zhang
Junbo Zhang