
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med. , 23 October 2024
Sec. Coronary Artery Disease
Volume 11 - 2024 | https://doi.org/10.3389/fcvm.2024.1382374
Objective: This study aims to explore the association between risk stratification and total occlusion (TO) of the culprit artery and multivessel disease (MVD) in patients with non-ST-segment-elevation myocardial infarction (NSTEMI) and to obtain more data on clinical decision-making in addition to risk stratification.
Methods: We retrospectively collected data from 835 patients with NSTEMI admitted to our hospital between 1 January 2016 and 1 August 2022. All patients underwent percutaneous coronary intervention (PCI) within 72 h of admission. We excluded patients with a history of cardiac arrest, myocardial infarction, coronary artery bypass grafting, or PCI. Univariate and multivariate regression analyses were performed to determine the predictors of acute TO and MVD.
Results: A total of 349 (41.8%) patients presented with a TO culprit vessel, whereas 486 (58.2%) had a patent culprit vessel. Thrombolysis in myocardial infarction (TIMI) and Global Registry of Acute Coronary Events (GRACE) risk stratifications were similar between the two groups of patients (P = 0.712 and 0.991, respectively). The TO infarct vessel was more commonly observed in the left circumflex artery. Patients with TO were more likely to develop MVD (P = 0.004). Univariate and multivariate linear regression analyses were performed to evaluate the role of variables in the presence of TO and MVD in patients with NSTEMI. Regional wall motion abnormalities (RWMAs) [odds ratio (OR) = 4.022; confidence interval (CI): 2.782–5.813; P < 0.001] were significantly linked to TO after adjusting for potentially related variables. Furthermore, age (OR = 1.032; CI: 1.018–1.047; P < 0.001), hypertension (OR = 1.499; CI: 1.048–2.144; P = 0.027), and diabetes mellitus (OR = 3.007; CI: 1.764–5.125; P < 0.001) were independent predictors of MVD in patients with NSTEMI. TIMI and GRACE risk scores were related to MVD prevalence in the multivariate logistic regression model. Patients with a TO culprit vessel had a higher risk of out-of-hospital cardiac death after a 2-year follow-up compared with those without a TO culprit vessel (P = 0.022).
Conclusion: TIMI and GRACE risk scores were not associated with a TO of the culprit artery; however, they correlated with the prevalence of MVD in patients with NSTEMI. RWMA is an independent predictor of acute TO in patients with NSTEMI. Patients with a TO culprit vessel had worse clinical outcomes than those without a TO culprit vessel.
Acute coronary syndrome (ACS) is a prevalent cause of mortality worldwide (1). ACS is categorized into ST-segment-elevation myocardial infarction (STEMI), non-ST-segment-elevation myocardial infarction (NSTEMI), and unstable angina (UA) based on electrocardiogram (ECG) findings and cardiac markers. ST-segment elevation in two or more contiguous leads denotes total or near-total occlusion (TO) of the culprit artery, an indication for immediate coronary angiography and revascularization (2). Emergency intervention is recommended only for high-risk patients with NSTEMI, as assessed by the thrombolysis in myocardial infarction (TIMI) or Global Registry of Acute Coronary Events (GRACE) risk score (3). The reason for such a recommendation for this patient category is that the absence of ST-segment elevation is interpreted as a lack of TO. However, in clinical practice, coronary angiography reveals that up to 30% of patients with NSTEMI have total coronary occlusion (4, 5). Growing evidence suggests that NSTEMI patients with TO have a higher risk of mortality and major adverse cardiac events (6). However, only a limited number of dependable markers or methods are available to predict the occurrence of TO in individuals with NSTEMI. This delays the provision of reperfusion therapy for many patients. In addition, multivessel disease (MVD) in patients with NSTEMI also confers a poor prognosis on them (7, 8). Furthermore, information about the predictors of MVD in patients with NSTEMI is limited. Therefore, this study aims to explore the association of risk stratification with TO and MVD and to find more data on clinical decision-making in patients with NSTEMI in addition to risk stratification.
This retrospective study was conducted on consecutive patients with NSTEMI who were admitted to our emergency room between 1 January 2016 and 1 August 2022. The inclusion criteria were as follows: established diagnosis of NSTEMI and a need for interventional treatment within 72 h of admission, as recommended by the relevant guidelines. Exclusion criteria were as follows: previous myocardial infarction, coronary artery bypass grafting, or percutaneous coronary intervention (PCI). This study was approved by the Institutional Ethics Committee of the Sir Run Run Shaw Hospital. Informed consent was obtained from all patients enrolled in this study.
The demographic features of all patients, such as age, gender, body mass index (BMI), history of hypertension or diabetes, smoking, and family history of coronary artery disease (CAD), were obtained from electronic medical records. Blood samples were drawn from the patients upon their arrival at the emergency department via a peripheral venous line and processed immediately. ECG data on ST-segment depression, flat T waves or T-wave inversion, and pathological Q wave and echocardiographic data consisting of ejection fraction (EF), regional wall motion abnormalities (RWMAs), and left ventricular end-diastolic dimension (LVEDD) were extracted. Moreover, the TIMI (http://www.timi.org/index.php?page=calculators) and GRACE scores (https://www.outcomes-umassmed.org/grace/acs_risk/) were calculated separately for all patients.
Two experienced interventional cardiologists identified the culprit vessel using coronary angiography, ECG, and echocardiogram. TO was defined as a culprit vessel with a TIMI flow of 0–1, indicating no dye penetration or minimal dye penetration without complete vessel opacification. MVD was defined as significant stenosis (>70%) in two or more major coronary arteries of 2.5 mm diameter or more. NSTEMI was defined as elevated troponin levels and the absence of ST elevation at the time of diagnosis according to 2014 NSTEMI guidelines (3). According to the guidelines of the American Society of Echocardiography (9), longitudinal shortening or radial thickening of the myocardium after aortic valve closure (postsystolic shortening or thickening, sometimes referred to as tardokinesis) of >20% of the total deformation during the cardiac cycle is a consistent sign of regional functional inhomogeneity. And also, RWMAs were defined as the occurrence of hypokinetic (reduced thickening), akinetic (absent or negligible thickening), and dyskinetic (systolic thinning or stretching) which were detected by experienced sonographers and confirmed by trained cardiologists. According to the severity of RWMAs, we defined the RWMA score as normal = 1, hypokinetic = 2, akinetic = 3, and dyskinetic = 4.
Detailed in-hospital and follow-up data were recorded and entered into a database. Patients were followed up through clinical visits or telephone calls to the referring physician. The clinical endpoint was cardiac death, which included death due to myocardial infarction, ventricular tachycardia/ventricular fibrillation, sudden cardiac arrest, or heart failure.
Categorical variables were expressed as percentages and compared using the chi-square test. Continuous variables were expressed as a mean ± SD or median with interquartile ranges and were compared using Student's t-test or the Wilcoxon rank-sum test as appropriate. The independent predictors of acute TO and MVD were confirmed by using the multivariate logistic regression model after adjusting for the potentially related variables (P < 0.2 and P < 0.05, respectively) identified in the univariate analysis. Kaplan–Meier survival curves were compared using the log-rank test. SPSS V.26.0 was used for all analyses, and a value of P < 0.05 was considered statistically significant.
The study population comprised 835 patients with NSTEMI: 349 (41.8%) presented with a TO culprit vessel and 486 (58.2%) had a patent culprit vessel. Baseline characteristics according to the patency of the culprit artery are listed in Table 1. The two groups showed similarities with respect to demographic characteristics and clinical data, and there were no significant differences between them, although differences were noticed with regard to BMI, white blood cell (WBC) count, neutrophil count, low-density lipoprotein cholesterol (LDL-C) level, high-sensitivity C-reactive protein (hs-CRP) level, heart rate (HR), and RWMAs, which were all higher or more commonly detected in patients with TO. TIMI and GRACE risk stratification were similar in both groups (P = 0.712 and 0.991, respectively). The proportion of patients with a TO of the culprit artery divided by different types of risk stratification is shown in Figures 1A,B.
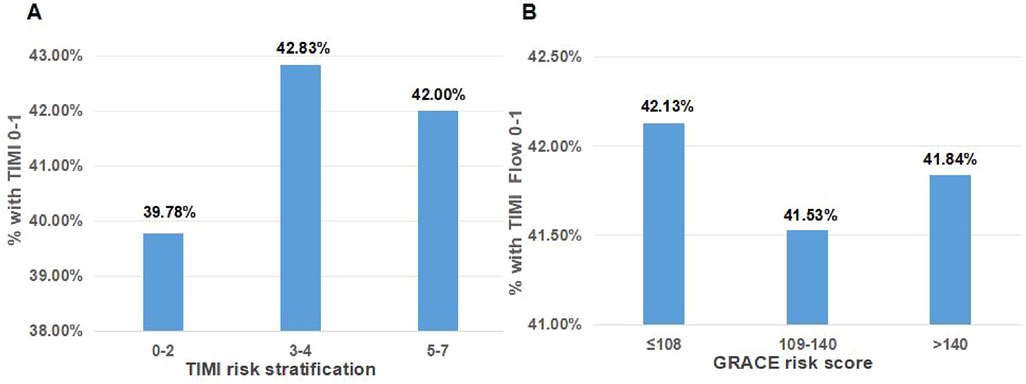
Figure 1. The proportion of patients with an occluded culprit artery by TIMI risk stratification (A) and the GRACE risk score (B).
The angiographic characteristics of the patient groups are presented in Table 1. TO was more commonly observed in the left circumflex artery (LCX). Patients with a TO of the culprit artery had a higher incidence of MVD (P = 0.004), a greater number of thrombotic culprit lesions (P < 0.001), high levels of collateral circulation (P < 0.001), and fewer calcified lesions (P = 0.008). In the TO group, glycoprotein IIb/IIIa inhibitors were used more frequently.
Univariate and multivariate linear regression analyses were performed to evaluate the role of variables in NSTEMI patients with a TO of the culprit artery. RWMA [odds ratio (OR) = 4.022, confidence interval (CI): 2.782–5.813; P < 0.001] was significantly associated with TO after adjusting for potentially related variables (Table 2). We also examined the variables through univariate and multivariate regression analyses and found that age (OR = 1.032, CI: 1.018–1.047; P < 0.001), hypertension (OR = 1.499, CI: 1.048–2.144; P = 0.027), and diabetes mellitus (OR = 3.007, CI: 1.764–5.125; P < 0.001) were independent predictors of MVD in patients with NSTEMI (Table 3). An assessment of the predictive value of MVD by risk stratification revealed that the TIMI and GRACE risk scores were associated with the prevalence of MVD in the multivariate logistic regression model (Table 4).
The outcomes of the 2-year follow-up period were compared between the TO and the non-TO groups of patients. A Kaplan–Meier analysis showed similar rates of in-hospital, 6-month out-of-hospital, and 1-year out-of-hospital cardiac deaths within the two groups (P = 0.727, 0.393, and 0.407, Figures 2A–C). However, patients with a TO culprit vessel had a higher rate of out-of-hospital cardiac death after the 2-year follow-up compared with those without a TO culprit vessel (P = 0.022, Figure 2D).
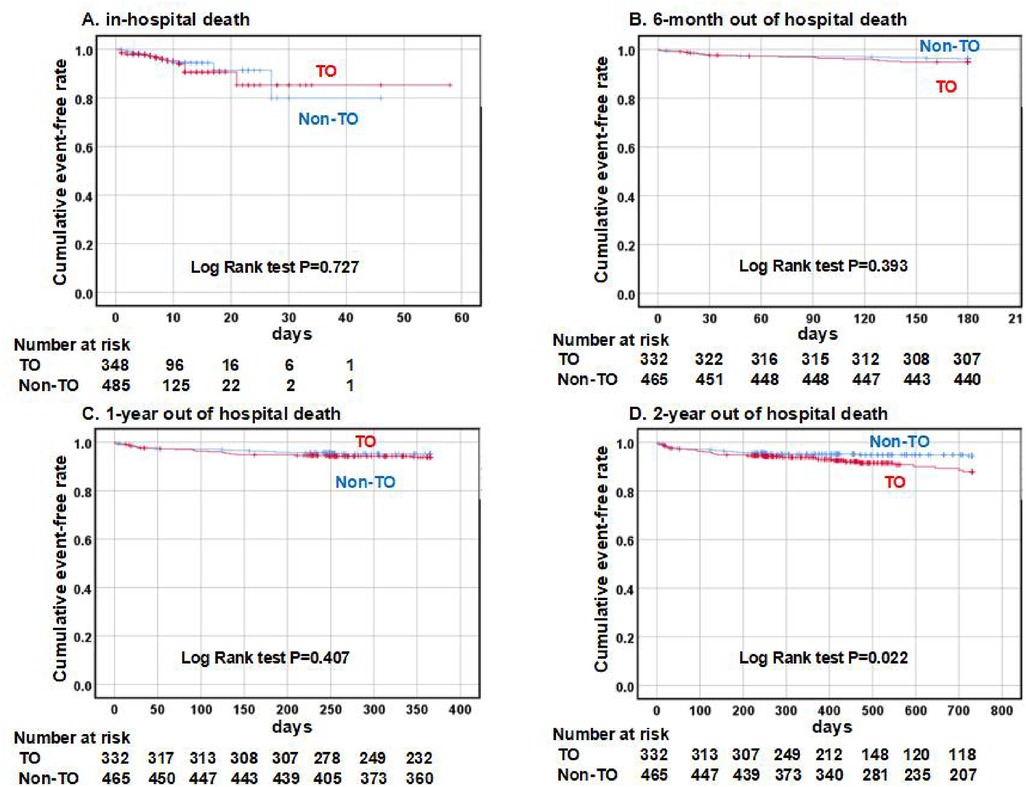
Figure 2. A comparison of cardiac death between patients belonging to the TO and the non-TO groups. A Kaplan–Meier analysis of cardiac death demonstrated similar outcomes in the TO group (red line) and the non-TO group (blue line) in terms of in-hospital, 6-month, and 1-year follow-ups (A–C). The TO group had a higher rate of cardiac death after a 2-year follow-up compared with the non-TO group (D). TO indicates total occlusion of the culprit artery.
The principal findings of this study are as follows: (1) the rate of prevalence of acute TO in patients with NSTEMI was 41.8%; (2) the LCX culprit vessel had the highest likelihood of TO in the setting of NSTEMI; (3) TIMI and GRACE risk stratification did not correlate with a TO of the culprit vessel but correlated with the prevalence of MVD; (4) RWMA was an independent predictor of TO in patients with NSTEMI; (5) patients with a TO of the culprit vessel had worse clinical outcomes at the mid-term follow-up compared with those without a TO of the culprit vessel.
The reported rates of prevalence of acute TO in patients with NSTEMI ranged from 24.0% to 37.2% (4, 10–12). In our study, the frequency was higher than that reported in previous studies, which may be explained by the differences in patient selection and variation in the risk stratification of the patients. Our study found that the vessel most likely occluded in NSTEMI is the LCX, which is consistent with the results of previous trials (13, 14). This finding is perhaps attributed to the fact ischemia in the LCX territory is difficult to detect since 38%–47% of patients do not show ST-segment shifts in any standard ECG lead (15). At our center, we routinely obtained an 18-lead electrocardiogram for patients presenting to the emergency department with ACS. STEMI due to occlusion of the LCX was typically manifested on ECG as ST-segment elevations in lateral, inferior, and posterior leads, while NSTEMI due to occlusion of the LCX was defined as elevated troponin levels and the absence of ST-segment elevations in any standard ECG lead at the time of diagnosis.
In patients with NSTEMI, a quantitative assessment of ischemic risk employing scores such as the GRACE risk score and TIMI risk stratification proved to be superior to clinical assessment alone. Current clinical practice guidelines for non-ST-segment-elevation acute coronary syndrome (NSTE-ACS) recommend different treatment strategies and timings for intervention according to the initial risk stratification (16). However, we demonstrated that the proportion of TO in different risk stratifications of TIMI and GRACE was similar, which accounted for the inability of the TIMI and GRACE risk scores to indicate whether the culprit vessel was totally occluded. This may result in delayed revascularization in non-high-risk patients. Prior studies have shown that the outcomes for NSTEMI patients with TO who do not receive timely revascularization are poorer than those for STEMI patients (17, 18). Moreover, a meta-analysis suggested that NSTEMI patients with totally occluded culprit vessels on coronary angiography were at a higher risk of mortality and major adverse cardiac events (19). Our findings were comparable but not identical to those of previous studies regarding the outcomes for patients with a TO culprit vessel. Patients with a TO culprit vessel had a similar rate of cardiac death in the hospital and at the short-term follow-up, while these patients had a higher risk of mortality in the mid-term follow-up compared with those without a TO culprit vessel. This could be attributed to the following: (1) all patients with NSTEMI received timely revascularization and proper medication in our center, contributing to a reduction in mortality after PCI and at the short-term follow-up. (2) Patients with a TO culprit vessel usually suffered a complete infarction of a part of the myocardium, requiring better treatment for myocardial remodeling. Some patients had a higher mortality rate due to poor drug adherence at the mid-term follow-up. Hence, finding reliable predictors of TO in patients with NSTEMI is of great significance.
Echocardiography is a feasible tool for TO detection. Eek et al. (20) found that detection of contractile abnormalities by strain or conventional echocardiography might be a very useful method to identify acute TO in NSTEMI. In our study, RWMA was also shown to be an effective predictor of acute TO in patients with NSTEMI. The possible mechanism is that acute persistent coronary occlusion can cause more severe ischemia and impaired systolic function in large regions of the myocardium.
The prognosis of NSTEMI in the presence of MVD is poor (3). Although risk factors for coronary heart disease are included in risk stratification, the association between the above-mentioned risk scores and coronary severity in NSTEMI has rarely been studied. A few studies have reported on the relationship between risk stratification and the extent of disease (21–25). Our study further evaluated the novel role of existing risk stratification. Identifying the predictors of severe NSTEMI is necessary for preoperative evaluation and developing postoperative preventive strategies based on risk factors.
Our study had some limitations. First, this was a retrospective, single-center study; therefore, a larger sample size with cross-center comparisons is required to validate the results further. Second, the outcome of the patients stratified into two groups in our study was recorded only in terms of cardiac death; it was not recorded by also taking into account other major adverse cardiac and cerebrovascular events, such as recurrent angina, heart failure, and stroke. Detailed records of the causes of adverse events can help make better decisions.
The TIMI and GRACE risk scores could not independently predict the TO of the culprit artery but were associated with the prevalence of MVD in patients with NSTEMI. RWMA was an independent predictor of acute TO in these patients. Patients with a TO culprit vessel had worse clinical outcomes at the mid-term follow-up compared with their non-TO counterparts.
The raw data supporting the conclusions of this article will be made available by the authors without undue reservation.
The studies involving humans were approved by the Ethics Committee of Sir Run Run Shaw Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
GX: Conceptualization, Formal Analysis, Methodology, Writing – original draft, Writing – review & editing, Software. GC: Data curation, Formal Analysis, Software, Writing – review & editing. MG: Data curation, Investigation, Software, Writing – review & editing. TH: Data curation, Investigation, Writing – review & editing. WH: Data curation, Investigation, Software, Writing – review & editing. CG: Data curation, Investigation, Writing – review & editing. XH: Conceptualization, Investigation, Methodology, Supervision, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by the Zhejiang Traditional Chinese Medicine Science and Technology Project (2023ZL496).
We thank our medical staff for their contribution to data entry and monitoring.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Writing Group Members, Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics—2016 update: a report from the American Heart Association. Circulation. (2016) 133(4):e38–360. doi: 10.1161/CIR.0000000000000350
2. Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, et al. 2015 ACC/AHA/SCAI focused update on primary percutaneous coronary intervention for patients with ST-elevation myocardial infarction: an update of the 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention and the 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation. (2016) 133(11):1135–47. doi: 10.1161/CIR.0000000000000336
3. Amsterdam EA, Wenger NK, Brindis RG, Casey DE Jr., Ganiats TG, Holmes DR, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. (2014) 64(24):e139–228. doi: 10.1016/j.jacc.2014.09.017
4. Dixon WCT, Wang TY, Dai D, Shunk KA, Peterson ED, Roe MT, et al. Anatomic distribution of the culprit lesion in patients with non-ST-segment elevation myocardial infarction undergoing percutaneous coronary intervention: findings from the National Cardiovascular Data Registry. J Am Coll Cardiol. (2008) 52(16):1347–8. doi: 10.1016/j.jacc.2008.07.029
5. Wang TY, Zhang M, Fu Y, Armstrong PW, Newby LK, Gibson CM, et al. Incidence, distribution, and prognostic impact of occluded culprit arteries among patients with non-ST-elevation acute coronary syndromes undergoing diagnostic angiography. Am Heart J. (2009) 157(4):716–23. doi: 10.1016/j.ahj.2009.01.004
6. Khan AR, Golwala H, Tripathi A, Bin Abdulhak AA, Bavishi C, Riaz H, et al. Impact of total occlusion of culprit artery in acute non-ST elevation myocardial infarction: a systematic review and meta-analysis. Eur Heart J. (2017) 38(41):3082–9. doi: 10.1093/eurheartj/ehx418
7. Corpus RA, House JA, Marso SP, Grantham JA, Huber KC Jr., Laster SB, et al. Multivessel percutaneous coronary intervention in patients with multivessel disease and acute myocardial infarction. Am Heart J. (2004) 148(3):493–500. doi: 10.1016/j.ahj.2004.03.051
8. Sorajja P, Gersh BJ, Cox DA, McLaughlin MG, Zimetbaum P, Costantini C, et al. Impact of multivessel disease on reperfusion success and clinical outcomes in patients undergoing primary percutaneous coronary intervention for acute myocardial infarction. Eur Heart J. (2007) 28(14):1709–16. doi: 10.1093/eurheartj/ehm184
9. Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. (2015) 28(1):1–39.e14. doi: 10.1016/j.echo.2014.10.003
10. Koyama Y, Hansen PS, Hanratty CG, Nelson GI, Rasmussen HH. Prevalence of coronary occlusion and outcome of an immediate invasive strategy in suspected acute myocardial infarction with and without ST-segment elevation. Am J Cardiol. (2002) 90(6):579–84. doi: 10.1016/S0002-9149(02)02559-6
11. Bahrmann P, Rach J, Desch S, Schuler GC, Thiele H. Incidence and distribution of occluded culprit arteries and impact of coronary collaterals on outcome in patients with non-ST-segment elevation myocardial infarction and early invasive treatment strategy. Clin Res Cardiol. (2011) 100(5):457–67. doi: 10.1007/s00392-010-0269-9
12. Kim MC, Ahn Y, Rhew SH, Jeong MH, Kim JH, Hong YJ, et al. Impact of total occlusion of an infarct-related artery on long-term mortality in acute non-ST-elevation myocardial infarction patients who underwent early percutaneous coronary intervention. Int Heart J. (2012) 53(3):160–4. doi: 10.1536/ihj.53.160
13. Karwowski J, Polonski L, Gierlotka M, Ciszewski A, Hawranek M, Beckowski M, et al. Total coronary occlusion of infarct-related arteries in patients with non-ST-elevation myocardial infarction undergoing percutaneous coronary revascularisation. Kardiol Pol. (2017) 75(2):108–16. doi: 10.5603/KP.a2016.0130
14. Ayad SW, El Zawawy TH, Lotfy MI, Naguib AM, El Amrawy AM. Incidence and impact of totally occluded culprit coronary artery in patients with non-ST segment elevation myocardial infarction acute coronary syndrome. Egypt Heart J. (2021) 73(1):36. doi: 10.1186/s43044-021-00160-x
15. Haeberlin A, Studer E, Niederhauser T, Stoller M, Marisa T, Goette J, et al. Electrocardiographic ST-segment monitoring during controlled occlusion of coronary arteries. J Electrocardiol. (2014) 47(1):29–37. doi: 10.1016/j.jelectrocard.2013.10.003
16. Roffi M, Patrono C, Collet JP, Mueller C, Valgimigli M, Andreotti F, et al. 2015 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: task force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. (2016) 37(3):267–315. doi: 10.1093/eurheartj/ehv320
17. Menon V, Ruzyllo W, Carvalho AC, de Sousa JMA, Forman SA, Jaworska K, et al. Infarct artery distribution and clinical outcomes in occluded artery trial subjects presenting with non-ST-segment elevation myocardial infarction (from the long-term follow-up of Occluded Artery Trial [OAT]). Am J Cardiol. (2013) 111(7):930–5. doi: 10.1016/j.amjcard.2012.12.009
18. Hochman JS, Lamas GA, Buller CE, Dzavik V, Reynolds HR, Abramsky SJ, et al. Coronary intervention for persistent occlusion after myocardial infarction. N Engl J Med. (2006) 355(23):2395–407. doi: 10.1056/NEJMoa066139
19. de Silva R, Steg PG. Identifying patients with acute total coronary occlusion in NSTEACS: finding the high-risk needle in the haystack. Eur Heart J. (2017) 38(41):3090–3. doi: 10.1093/eurheartj/ehx520
20. Eek C, Grenne B, Brunvand H, Aakhus S, Endresen K, Smiseth OA, et al. Strain echocardiography predicts acute coronary occlusion in patients with non-ST-segment elevation acute coronary syndrome. Eur J Echocardiogr. (2010) 11(6):501–8. doi: 10.1093/ejechocard/jeq008
21. Lakhani MS, Qadir F, Hanif B, Farooq S, Khan M. Correlation of thrombolysis in myocardial infarction (TIMI) risk score with extent of coronary artery disease in patients with acute coronary syndrome. J Pak Med Assoc. (2010) 60(3):197–200.20225777
22. Mahmood M, Achakzai AS, Akhtar P, Zaman KS. Comparison of the TIMI and the GRACE risk scores with the extent of coronary artery disease in patients with non-ST-elevation acute coronary syndrome. J Pak Med Assoc. (2013) 63(6):691–5.23901666
23. Santos ES, Aguiar Filho Lde F, Fonseca DM, Londero HJ, Xavier RM, Pereira MP, et al. Correlation of risk scores with coronary anatomy in non-ST-elevation acute coronary syndrome. Arq Bras Cardiol. (2013) 100(6):511–7. doi: 10.5935/abc.20130088
24. Acet H, Ertas F, Bilik MZ, Aydin M, Yuksel M, Polat N, et al. The relationship of TIMI risk index with SYNTAX and Gensini risk scores in predicting the extent and severity of coronary artery disease in patients with STEMI undergoing primary percutaneous coronary intervention. Ther Adv Cardiovasc Dis. (2015) 9(5):257–66. doi: 10.1177/1753944715574814
Keywords: ACS—ACS/NSTEMI, total occlusion, percutaneous coronary intervention (PCI), multivessel disease (MVD), regional wall motion abnormalities (RWMAs)
Citation: Xiang G, Cao G, Gao M, Hu T, He W, Gu C and Hong X (2024) Clinical decision-making in patients with non-ST-segment-elevation myocardial infarction: more than risk stratification. Front. Cardiovasc. Med. 11:1382374. doi: 10.3389/fcvm.2024.1382374
Received: 5 February 2024; Accepted: 4 October 2024;
Published: 23 October 2024.
Edited by:
Istvan Szokodi, University of Pécs, HungaryReviewed by:
Alessia D’Aiello, Agostino Gemelli University Polyclinic (IRCCS), ItalyCopyright: © 2024 Xiang, Cao, Gao, Hu, He, Gu and Hong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xulin Hong, MTAyODM0NjYwNEB6anUuZWR1LmNu; Guangze Xiang, Z3Vhbmd6ZXhAZm94bWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.