
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med. , 26 April 2024
Sec. Thrombosis and Haemostasis
Volume 11 - 2024 | https://doi.org/10.3389/fcvm.2024.1381391
This article is part of the Research Topic Insights in Thrombosis and Haemostasis: From a Biological, Clinical and Genetic Perspective View all 14 articles
Background: The incidence of deep vein thrombosis (DVT) in the lower extremities is increasing in the younger population. However, there are fewer reported comparisons in the literature for lower extremity DVT.
Methods: Patients aged <40 years admitted with lower-extremity DVT between January 2018 and December 2023 were retrospectively analyzed and followed up for 1 year.
Results: A total of 61 patients were included in the study and divided into two groups: 33 patients over 30 years of age (middle-aged group) and 28 patients under 30 years of age (young group). A significant gender difference was observed, with a higher proportion of males in the young group compared to the middle-aged group (P < 0.001). Five patients in the young group were treated with anticoagulation alone, whereas all patients in the middle-aged group underwent endovascular therapy. A higher prevalence of inferior vena cava thrombosis in the young group compared to the middle-aged group (60.71% vs. 33.3%, P = 0.032). The proportion of iliac vein stenosis was significantly higher in the middle-aged groups than in the young group (P = 0.002). There was no statistically significant difference in venous function scores (Villalta and rVCSS) between the two groups during both the preoperative period and the postoperative follow-up (P > 0.05). The incidence of lower-extremity DVT post-thrombotic syndrome and thrombus recurrence was higher in the young group than in the middle-aged group at 1 year postoperatively (PTS: 78.57% vs. 33.3%, P < 0.001, and thrombus recurrence: 28.57% vs. 9.09%, P < 0.05). Univariate and multivariate analyses revealed that inferior vena cava thrombosis was an independent risk factor for severe DVT post-thrombotic syndrome and recurrent DVT (P < 0.05), whereas gender was an independent risk factor for recurrent DVT (P < 0.05).
Conclusions: This study suggests differences in the clinical characteristics and prognosis of lower-extremity DVT.
The prevalence of lower extremity deep vein thrombosis (DVT) is primarily attributed to factors that affect blood flow, such as tumors, aging, hypercoagulability and prolonged immobilization (1, 2). These factors traditionally result in a lower incidence of DVT in younger individuals. However, in recent years, the prevalence of DVT has been on the rise among the younger population in China (3). The formation of DVT can easily lead to post-thrombotic syndrome (PTS), a condition with later symptoms that significantly impact the patient's quality of life. This is particularly challenging for younger patients to accept. PTS, stemming from DVT in the lower extremities, inevitably diminishes the patient's quality of life, posing an unacceptable burden for the younger demographic. Recent literature suggests that DVT characteristics in young adults differ from those in older patients (4–6). However, detailed comparisons of DVT in China are scarce. Therefore, this study aims to conduct a retrospective analysis of 61 patients under the age of 40 admitted to our center. The analysis provides a preliminary exploration of DVT in the younger age group.
A retrospective analysis was conducted on 61 patients under 40 years of age who were diagnosed with lower extremity deep vein thrombosis (DVT) from January 2018 to December 2023. The study was conducted at the Department of Vascular Surgery, Affiliated Hospital of Chengdu University of Traditional Chinese Medicine. Enrolled participants were confirmed to have venous thrombosis above the popliteal vein through lower extremity venous ultrasound. Only patients who were first-time diagnosed with lower extremity DVT and received anticoagulation therapy or underwent venography were included in the study. Exclusion criteria included patients who did not receive anticoagulation therapy or undergo venography.
All admitted patients received standard anticoagulation therapy using low molecular weight heparin sodium or rivaroxaban tablets (anticoagulant course >3 months). Additionally, all enrolled patients underwent lower extremity venography. For patients with acute iliofemoral vein thrombosis (onset within 14 days with markedly elevated D2 polymers), after communication with the patients and their families, the inferior vena cava filter is implanted and Angiojet thrombus is aspirated (7, 8). For cases with refractory thrombus, the surgeon will perform catheter contact thrombolysis (CDT) according to the situation. Balloon dilatation was performed for patients with iliac vein compression, and the decision to implant a stent was made by the surgeon as needed. Compression therapy was applied at the end of the procedure to alleviate lower limb swelling.
In addition to basic information such as age, gender, and weight, the study collected indicators related to the increased risk of venous thrombosis, tumors, marital history, history of prolonged braking, and various biochemical indexes (hemoglobin, leukocytes, neutrophil counts, D2 polymorphisms, protein C, protein S, etc.). The location of lower extremity DVT was recorded by imaging, and the intraoperative Angiojet documented the thrombus location. The use of Angiojet thrombus aspiration catheter, CDT, balloon, and thrombus clearance were also indicated.
All patients underwent follow-up at the hospital and were contacted by telephone at 6 and 12 months postoperatively. Follow-up included lower extremity venous ultrasound, Villalta score assessment, and Revised venous clinical severity scores (rVCSS). A Villalta score exceeding 15 indicated severe lower extremity post-DVT syndrome.
Normality of the quantitative data was assessed, and descriptive statistics were applied accordingly. To compare the young and middle-aged groups, t-tests were used for normally distributed data, Wilcoxon rank sum tests for non-normally distributed data, and chi-square tests/exact tests for categorical data. Risk factors for post-thrombotic syndrome (PTS) and thrombosis recurrence were analyzed using univariate and multivariate logistic regression. Statistical significance was determined at a significance level of P < 0.05. All analyses were performed using SAS statistical software (version 9.4, Cary, NC).
This study included patients diagnosed with lower extremity deep vein thrombosis (DVT), 33 of whom were over 30 years old and 28 under 30. The proportion of males with lower extremity DVT was significantly higher in the younger population compared to the middle-aged and young adult population (78.57% vs. 33.3%, P < 0.001). The analysis of listed risk factors (Table 1) showed no history of tumors in either group. Family history was observed in only one case in each group. The young group had more case of recent hormone use, trauma, and history of deep vein thrombosis compared to the middle-aged group. On the other hand, the young group had fewer cases of history of braking, infections, and surgeries than in the middle-aged group. Table 2 show thathemoglobin levels were slightly higher in the young group (4.29 ± 0.67 vs. 4.35 ± 0.53, P = 0.705) among the listed blood indices, Fibrinogen was elevated in the middle-aged group (4.19 ± 1.36 vs. 4.84 ± 2.62, P = 0.244). Protein C deficiency was found in two cases, and protein S deficiency was found in one case in the young group, while none were found in the middle-aged group. As shown in Table 3, the analysis of the lesions showed a significantly higher incidence of inferior vena cava thrombosis among individuals under 30 years of age. Additionally, this group had a lower rate of iliac vein stenosis in this group (57.14% vs. 90.19%, P = 0.002).
The mean Villalta scores improved at the 6-month and 12-month follow-ups for the young (baseline, 15.60; 6 months, 6.32; 12 months, 6.60; P < .0001), and middle age (baseline, 16.60; 6 months, 6.21; 12 months, 5.60; P < .0001) groups (Figure 1A). No difference in 6-month and 12-month Villalta score improvement was observed between the groups (P > 0.05). The mean rVCSS at baseline, 6 months, and 12 months was 10.14, 4.39, and 5.67, respectively, (6 months, P < 0.001; 12 months, P < 0.001; each follow up compared with baseline) for patients in the young group and 11.42, 5.82, and 0.15, respectively, (P < .0001 for each follow-up) for patients in the middle-aged group. Figure 1 illustrate variation in Villalta and rVCSS distribution between the groups. Improvement in 6-month and 12-month rVCSS was not significantly different between the groups. The young group had higher scores. A Villalta score exceeding 15 points indicatS severe PTS. The incidence of PTS was significantly higher in the young group than in the middle-aged group (78.57% vs. 33.3%, P < 0.001). Furthermore, the recurrence rate of lower extremity DVT was significantly higher in the youth group than in the middle-aged group (28.57% vs. 9.09%, P < 0.05, Table 4). The study conducted univariate and multivariate logistic regression analyses to determine the relationship between PTS and recurrence of lower extremity DVT. The results showed that inferior vena cava thrombosis was an independent risk factor for both PTS and recurrence of lower extremity DVT (Tables 5, 6). Additionally, Males were identified as an independent risk factor for the recurrence of lower extremity DVT (Table 6).
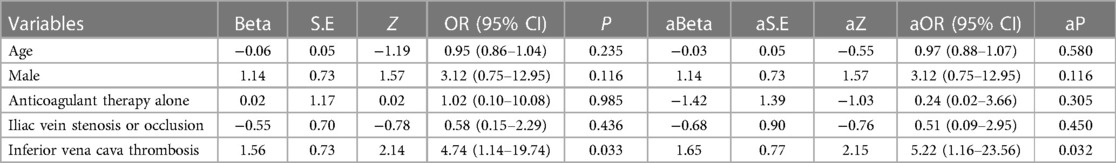
Table 5. Univariate and multifactor logistic regression analysis of clinically relevant risk factors for PTS.
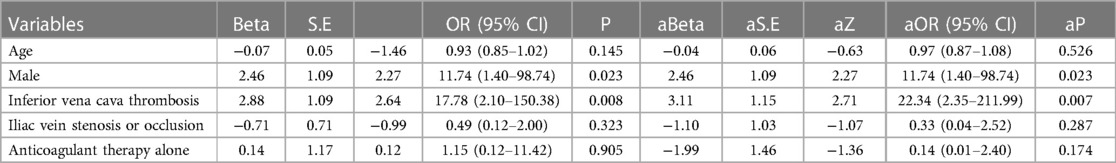
Table 6. Univariate and multifactor logistic regression analysis of clinically relevant risk factors for venous thrombosis recurrence.
The literature suggests that younger patients with lower-extremity DVT are not common in clinical practice. However, in recent years, the incidence of patients with lower-extremity DVT has increased compared with the past, and although the management of lower extremity DVT has gained a lot of diagnostic and therapeutic experience in the clinic, there is still a lack of more evidence-based medical evidence regarding the clinical characteristics of younger patients with DVTas well as their postoperative conditions. In this study, a preliminary attempt was made to gain a better understanding of the younger DVT patient population by retrospectively comparing the differences in lower extremity DVT between young and middle-aged patients.
The pathogenesis and recurrence of the first episode of DVT are multifactorial, depending on the severity and number of genetic and indirect factors (9). Venous thrombosis is caused by hypercoagulable state, venous stasis, and endothelial damage. The main conditions associated with these three pathological processes are tumors, trauma, immobility, and childbirth younger patients are less likely to develop DVT due to these underlying factors. Kuo DJ's reports that- prolonged repetitive squatting position required by- baseball catchers may compress the blood vessels in the pelvic, inguinal, and popliteal regions, leading to the development of lower extremity DVT in younger baseball patients (5). In the Raymundo SRO report a patient with inferior vena cava malformation was found to have developed lower extremity DVT (10). Additionally, genetic factors such as abnormalities in blood proteins C and S and coagulation factor V can contribute to the development of lower extremity DVT. The study found elevated levels of protein C and S in patients under 30 years old, with less variation in other factors such as tumors. In the present study, it was found that males were more common among patients with DVT under 30 years of age, while females were more common among patients with DVT over 30 years of age. This difference was statistically significant.
The occurrence of post-thrombotic syndrome (PTS) and recurrent deep vein thrombosis (DVT) in young patients can have disastrous consequences. Long-term chronic venous hypertension can cause significant discomfort, and localized itching and ulceration of the lower extremities can affect the quality of life of patients. Therefore, in addition to preventing fatal pulmonary embolism in young patients with DVT, it is crucial to prevent recurrence of DVT and PTS in the lower extremities. According to the literature, severe post-thrombotic syndrome (PTS) occurs in 5%–10% of cases (11). However, this study found a significantly higher incidence of severe PTS in young and middle-aged patients. Additionally, patients under 30 years old with DVT had a significantly higher incidence of recurrent DVT and severe PTS within 1 year compared to young and middle-aged patients (Table 4). These findings warrant attention.
In 2017, an article published in the New England Journal of Medicine found no significant difference between anticoagulation alone and surgery in the management of lower extremity DVT with regards to the development of PTS in the later stages of the disease (12). However, the study's methodology suggests that different treatment modalities may impact the prognosis of lower extremity DVT (13–15). The discrepancy may be due to the previous study's prospective design, which introduced confounding factors, such as being conducted in the early stages of the disease. To ensure a meaningful comparison, it may be necessary to conduct a randomized controlled clinical trial, as there are several confounding factors to consider, such as the surgical procedure and type of thrombus. However, the study found no statistically significant difference in the rates of post-thrombotic syndrome (PTS) and lower extremity deep vein thrombosis (DVT) between the two treatment groups. It should be noted that the study had a small sample size and included age-specific patients, which limits the ability to draw conclusions about the effect of different treatment modalities on the occurrence of PTS and recurrence of thrombosis. Statin use has been shown (15) to reduce the incidence of PTS, and statins were not included in this study because the population consisted of young and middle-aged patients who were less likely to use lipid-lowering drugs.
Lower extremity DVT complicated by inferior vena cava thrombosis is rare and has a high mortality rate. Patients with untreated inferior vena cava thrombosis have a 90% risk of developing post-thrombotic syndrome (PTS), and up to 15% may develop severe PTS with chronic leg ulcers (16). Similarly, the incidence of inferior vena cava thrombosis was found to be as high as 60% in the young group in this study, with a significantly higher rate of PTS and recurrent thrombosis later in life than in the middle-aged group. Correlation analysis showed that the presence of inferior vena cava thrombosis in patients with lower-extremity DVT was an independent risk factor for PTS and recurrent venous thrombosis.
Regarding DVT recurrence, a prospective study by Dr. Legese Chelkeba et al. in an Ethiopian population showed that a history of previous DVT was an independent factor for DVT recurrence (2). In contrast, the patients enrolled in this study were all first diagnosed with thrombosis, which makes the two studies not comparable considering the age and ethnicity of the cohort in this study population. However, we found that male sex was an independent risk factor for recurrence in patients with lower-extremity DVT. This has been less reported in previous literature and further studies are needed to confirm this.
However, this study is a small retrospective analysis of rejuvenated lower extremity DVT patients, comparing those over 30 years old with those under 30 years old. While there are differences between the two age groups, the age difference is not significant enough to highlight the characteristics of rejuvenated DVT in certain factors. Therefore, multicenter prospective studies or randomized clinical controlled trials are needed to investigate the rejuvenation of deep vein thrombosis (DVT) in the lower extremities. This will increase awareness of young DVT and provide a more evidence-based approach to treatment at a later stage.
Our study examines the unique characteristics of deep vein thrombosis (DVT) in young adults vs. middle-aged individuals. We found that young adults have higher rates of post-thrombotic syndrome (PTS) and recurrent DVT. We also identified inferior vena cava thrombosis as a potential independent risk factor for both PTS and DVT. Furthermore, gender was found to be a significant risk factor for recurrent thrombosis. These findings emphasize the necessity of customized approaches to comprehend and manage DVT in young adults. It is important to focus on factors that may increase the risk of PTS and recurrence.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
The requirement of ethical approval was waived by the Medical Ethics Committee of Chengdu University of Traditional Chinese Medicine Hospital for the studies involving humans because this is a retrospective analysis. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
YZ: Data curation, Investigation, Writing – original draft. HW: Data curation, Supervision, Writing – original draft. YL: Formal Analysis, Supervision, Writing – review & editing. QW: Conceptualization, Data curation, Validation, Writing – review & editing. CH: Conceptualization, Methodology, Software, Supervision, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Vrints CJM. Deep venous thrombosis and endothelial dysfunction in cancer: prevention and early initiated rehabilitation should be integral to a cardio-oncology programme. Eur J Prev Cardiol. (2022) 29:1244–7. doi: 10.1093/eurjpc/zwab117
2. Mulatu A, Melaku T, Chelkeba L. Deep venous thrombosis recurrence and its predictors at selected tertiary hospitals in Ethiopia: a prospective cohort study. Clin Appl Thromb Hemost. (2020) 26:1076029620941077. doi: 10.1177/1076029620941077
3. Stein PD, Matta F, Hughes MJ. In-hospital mortality with deep venous thrombosis. Am J Med. (2017) 130:596–600. doi: 10.1016/j.amjmed.2016.10.030
4. Cohen CT, Sartain SE, Sangi-Haghpeykar H, Kukreja KU, Desai SB. Clinical characteristics and outcomes of combined thrombolysis and anticoagulation for pediatric and young adult lower extremity and inferior vena cava thrombosis. Pediatr Hematol Oncol. (2021) 38:528–42. doi: 10.1080/08880018.2021.1889729
5. Abood KK, Paul MR, Kuo DJ. Deep vein thrombosis in a young, healthy baseball catcher: a case report and review of the literature. J Pediatr Hematol Oncol. (2019) 41:321–3. doi: 10.1097/MPH.0000000000001113
6. Rosenthal J, Kilburn T, Jackson W, Lune PV, Nutting A, Pacheco L. Double trouble: a young female with extensive deep venous thrombosis. Am J Med. (2023) 136:e113–4. doi: 10.1016/j.amjmed.2023.01.040
7. McLafferty RB. Endovascular management of deep venous thrombosis. Perspect Vasc Surg Endovasc Ther. (2008) 20:87–91. doi: 10.1177/1531003507313304
8. Kim KA, Choi SY, Kim R. Endovascular treatment for lower extremity deep vein thrombosis: an overview. Korean J Radiol. (2021) 22:931–43. doi: 10.3348/kjr.2020.0675
9. Vorob’eva NM, Panchenko EP, Dobrovol’skiĭ AB, Titaeva EV, Khasanova ZB, Konovalova NV, et al. Independent predictors of deep vein thrombosis (results of prospective 18 months study). Kardiologiia. (2010) 50:52–8.. PMID: 21591393.
10. Raymundo SRO, Cabral VS, Cavalieri RF, Reis Neto F. Thrombolysis for deep venous thrombosis associated with inferior vena cava agenesis in a young patient. BMJ Case Rep. (2019) 12(5):e229840. doi: 10.1136/bcr-2019-229840
11. Kahn SR. The post-thrombotic syndrome. Hematology Am Soc Hematol Educ Program. (2016) 2016:413–8. doi: 10.1182/asheducation-2016.1.413
12. Vedantham S, Goldhaber SZ, Julian JA, Kahn SR, Jaff MR, Cohen DJ, et al. Pharmacomechanical catheter-directed thrombolysis for deep-vein thrombosis. N Engl J Med. (2017) 377:2240–52. doi: 10.1056/NEJMoa1615066
13. Huang CY, Hsu HL, Kuo TT, Lee CY, Hsu CP. Percutaneous pharmacomechanical thrombectomy offers lower risk of post-thrombotic syndrome than catheter-directed thrombolysis in patients with acute deep vein thrombosis of the lower limb. Ann Vasc Surg. (2015) 29:995–1002. doi: 10.1016/j.avsg.2015.01.014
14. Kuo TT, Huang CY, Hsu CP, Lee CY. Catheter-directed thrombolysis and pharmacomechanical thrombectomy improve midterm outcome in acute iliofemoral deep vein thrombosis. J Chin Med Assoc. (2017) 80:72–9. doi: 10.1016/j.jcma.2016.08.012
15. Hager E, Yuo T, Avgerinos E, Naddaf A, Jeyabalan G, Marone L, et al. Anatomic and functional outcomes of pharmacomechanical and catheter-directed thrombolysis of iliofemoral deep venous thrombosis. J Vasc Surg Venous Lymphat Disord. (2014) 2:246–52. doi: 10.1016/j.jvsv.2014.02.003
Keywords: lower extremity deep vein thrombosis, young, PTS, thrombus recurrence, inferior vena cava thrombosis
Citation: Zhang Y, Wei H, Liu Y, Wang Q and He C (2024) Clinical characteristics of lower extremity deep vein thrombosis in young vs. middle-aged adults: a single-center retrospective study. Front. Cardiovasc. Med. 11:1381391. doi: 10.3389/fcvm.2024.1381391
Received: 3 February 2024; Accepted: 4 April 2024;
Published: 26 April 2024.
Edited by:
Gabor Erdoes, University Hospital of Bern, SwitzerlandReviewed by:
Yung-Wei Chi, University of California, Davis, United States© 2024 Zhang, Wei, Liu, Wang and He. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qiqi Wang d2FuZ3FpcWlfY3p5ZnlAMTYzLmNvbQ== Chunshui He Y2h1bnNodWlfaGVAMTYzLmNvbQ==
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.