
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med. , 28 June 2024
Sec. Cardiovascular Epidemiology and Prevention
Volume 11 - 2024 | https://doi.org/10.3389/fcvm.2024.1379871
Background: Oxidative stress is a known pathogenic mechanism in cardiovascular disease (CVD), yet the association between dietary antioxidants and CVD in the general population remains underexplored. This study leverages data from the National Health and Nutrition Examination Survey (NHANES) to investigate the association of a composite dietary antioxidant index with CVD in US adults.
Methods: Analyzing data from 25,997 adults (2011–2020 NHANES), we employed weighted generalized linear models, subgroup analysis, threshold effect analyses, and sensitivity analysis to assess the association between dietary antioxidants and CVD. Nonlinear associations were explored through a restricted cubic spline, with gender-specific stratification and threshold effect analysis to identify critical inflection points.
Results: Increasing levels of the composite dietary antioxidant index corresponded with decreased CVD prevalence (P < 0.001). In all models, weighted generalized linear models revealed a consistent negative association between CVD prevalence. And in Model 3, Quartile 4 had a 29% lower CVD prevalence than Quartile 1[0.71 (0.59, 0.85), P < 0.001]. Meanwhile, the findings of the unweighted logistic regression model demonstrated stability. Various characteristics such as sex, age, race, PIR, education, BMI, alcohol consumption, hypertension, hyperlipidemia, and diabetes did not influence this inverse association (P for interaction >0.05). Notably a nonlinear association was observed, with a significant inflection point at 3.05 among women.
Conclusion: This study demonstrates a strong negative association between the composite dietary antioxidant index and CVD prevalence, suggesting the potential protective role of dietary antioxidants. These findings underscore the need for prospective studies to further understand the impact of oxidative stress on cardiovascular health.
Cardiovascular disease (CVD) stands as the predominant cause of mortality among adults globally, accounting for approximately one-third of all deaths each year (1). The impact of CVD on public health is profound, directing significant attention towards understanding how to reduce its morbidity and mortality (2). Consequently, there is an urgent need to delve deeper into identifying additional risk factors and preventive measures for CVD.
Central to the progression of CVD is oxidative stress (OS), which impairs endothelial cell function through increased production of reactive oxygen species (ROS) (3). Nitric oxide (NO) interacts with these reactive oxygen species (ROS), which lowers the bioavailability of NO. This reduction in NO levels affects the vasodilatory response, which is essential for preserving vascular homeostasis and degrades endothelial function (4). Concurrently, inflammation synergizes with OS, exacerbating atherosclerosis progression (5). Emerging research highlights oxidative stress as a key player in the pathogenesis and progression of diseases such as pulmonary arterial hypertension (PAH), atherosclerosis (AS), and myocardial infarction (MI) (6–8). Despite this, the clinical application of antioxidant drugs in CVD prevention and treatment remains limited, shifting focus to the potential of antioxidant nutrients obtained from daily diets.
The Composite Dietary Antioxidant Index (CDAI) is established as a scientifically valid and reliable instrument for evaluating the overall antioxidant capacity in daily diets (9–11). This index intricately amalgamates a multifaceted score derived from six pivotal antioxidant nutrients, encompassing vitamins A, E, C, zinc, selenium, and carotenoids (12, 13). The CDAI highlights its importance in the assessment of nutrition. Recent studies underscore the significance of the CDAI. Investigations have revealed CDAI's role in reducing lung cancer risk in male smokers (14), protecting against osteoporosis in individuals aged 40–85 years (15), and mitigating depression development in U.S. adults (16). A study by Yang found that individuals with type 2 diabetes mellitus who consumed a diet rich in antioxidants experienced notably lower mortality rates from cardiovascular diseases (17). Additionally, a negative association between CDAI and various cardiovascular conditions, including hypertension, coronary heart disease, and heart failure, has been observed (18–20). However, we have found no studies that directly explore the association between the CDAI and the overall prevalence of cardiovascular diseases in the general population. To address this gap, our study utilizes data from the National Health and Nutrition Examination Survey (NHANES), aiming to enrich our understanding of antioxidant nutrients in CVD prevention and management.
The primary objective of our study is to investigate the potential association between CDAI and cardiovascular disease in U.S. adults. This exploration aims to contribute valuable insights into future strategies for the prevention and treatment of CVD.
The National Health and Nutrition Examination Survey (NHANES), a pivotal initiative of the National Center for Health Statistics (NCHS), plays a crucial role in evaluating the health and nutritional status of the United States' adult and child populations. This comprehensive program combines detailed interviews with thorough physical examinations to gather its data. Ethical compliance is a cornerstone of the NHANES methodology; the NCHS Research Ethics Review Board has rigorously approved all research protocols. Additionally, we ensured strict adherence to ethical standards by meticulously securing written informed consent from every individual. For transparency and public engagement, the NHANES has made its exhaustive research methodologies and datasets publicly accessible at www.cdc.gov/nchs/nhanes/, facilitating further research and analysis.
In the study, we analyzed data from 45,462 participants from the NHANES database covering the years 2011 to 2020. To focus the research on adults, individuals under 20 years of age, totaling 19,182, were omitted. Furthermore, the analysis excluded 236 participants due to incomplete questionnaire data, which was essential for diagnosing cardiovascular diseases. Additionally, 47 participants with missing information on education and smoking were excluded. Consequently, the final sample size for the study comprised 25,997 participants.
Figure 1 illustrates the process of participant selection for the study through a detailed flow diagram.
In this analysis, the derivation of CDAI data was executed via a 24-h dietary recall interview. This method involved detailed documentation of all foods and beverages consumed by the participants in the 24 h preceding the interview, facilitating an accurate estimation of the nutrients. However, they do not include nutrients obtained from dietary supplement intakes, antacids, or medications. We used a modified version of the CDAI formula in our investigation to precisely measure the total amount of dietary antioxidant consumption (14, 21, 22). The six essential antioxidant vitamins included in this improved CDAI formula are carotenoids, zinc, selenium, vitamin A, vitamin C, and vitamin E. The formula for calculating the CDAI is as follows:
The antioxidant intake was denoted by , a mean of the entire cohort was represented by , and the showed the standard deviation (SD).
In this study, the classification of CVD was based on participant responses to the survey questionnaire. A diagnosis of CVD was considered if participants reported any of the following conditions: angina, myocardial infarction (MI), stroke, congestive heart failure (CHF), or coronary heart disease (CHD). Consequently, any affirmative response to these specific conditions was interpreted as an indication of the presence of CVD.
In this study, a comprehensive array of covariates was analyzed, including age, gender, racial background, educational attainment, the ratio of family income to poverty (PIR), body mass index (BMI), estimated Glomerular Filtration Rate (eGFR), and consumption patterns of alcohol and tobacco. Additionally, clinical conditions such as hyperlipidemia, hypertension, and diabetes mellitus were considered. Educational levels were categorized into three groups: less than high school, high school or equivalent, and college education or higher. PIR was stratified into low (PIR < 1.3), middle (≥1.3 and <3.5), and high-income (PIR ≥ 3.5) brackets (23). Alcohol consumption was defined as excessive at four or more drinks per day for men and three or more for women, moderate at two drinks per day for women and three for men, with any additional intake considered minimal (24). Smoking status was determined by a history of consuming over a hundred cigarettes in a year (25). Hyperlipidemia was defined using specific thresholds: total cholesterol ≥200 mg/dl, triglycerides ≥150 mg/dl, high-density lipoprotein ≤40 mg/dl in men and ≤50 mg/dl in women, or low-density lipoprotein ≥130 mg/dl (26, 27). Hypertension was identified by the use of antihypertensive medications, a systolic blood pressure of 140 mmHg or higher, diastolic blood pressure of 90 mmHg or higher, or a documented history of hypertension. Diabetes diagnosis was based on a fasting plasma glucose level of 126 mg/dl or higher, glycated hemoglobin (HbA1c) values of 6.5% or higher, or the use of insulin or hypoglycemic medications. All measured clinical parameters and laboratory data were meticulously collected for the research.
We conducted a comprehensive weighting of the study data, adhering to the NHANES guidelines for complex sampling weight calculations, to ensure robust and representative statistical analysis. Continuous variables were presented as means [95% confidence intervals (CI)], and categorical variables were presented as proportions (95% CI). The method of multiple imputation was utilized for the variables that lacked data. Individuals were stratified into quartiles based on their weighted CDAI for baseline characteristic analysis. Using weighted generalized linear models to analyze the linear association between CVD and CDAI. Model 1 was unadjusted; Model 2 accounted for sex, age, and race; Model 3 further controlled for education, PIR, smoking status, alcohol consumption, hypertension, hyperlipidemia, and diabetes. Additionally, we employed restricted cubic spline curves to assess the nonlinear association between the CDAI and CVD. We stratified the analysis by gender and performed threshold effect analysis to identify critical inflection points in this association. Weighted subgroup analyses were conducted to assess the stability of the association between CDAI and cardiovascular disease. Ultimately, we corroborated our findings through an unweighted logistic regression analysis. The R studio (Version 4.2.2) and Empower Stats (version 4.1) were used for all statistical analyses. A two-sided P < 0.05 was used to establish statistical significance.
This study encompassed 25,997 participants, characterized by an average age of 49.72 ± 17.69 years, with a slight majority of females (51.65%) over males (48.35%). The median CDAI is −0.66, with a cardiovascular disease prevalence of 11.01%. As shown in Table 1, the participants were divided into quartiles based on CADI values. A notable trend emerged, showing a decreasing prevalence of cardiovascular disease with increasing CDAI quartiles, a difference that proved to be statistically significant (Quartile 1: 11.57%, Quartile 2: 8.76%, Quartile 3: 8.96%, Quartile 4: 6.79%, P < 0.001). Furthermore, statistically significant variations were observed among the four quartiles in terms of age, gender, race, education level, PIR, BMI, smoking habits, alcohol consumption level, eGFR, hyperlipidemia, hypertension, and diabetes mellitus (P < 0.05).
The generalized linear regression weighted model of CDAI and CVD is displayed in Table 2. This negative correlation association is evident when CDAI is treated as a continuous variable, manifesting in unadjusted, partially adjusted models with statistical significance (P < 0.001). Specifically, in Model 1, Model 2, and Model 3, the fourth quartile exhibited a lower prevalence of cardiovascular disease compared to the first quartile, when CDAI was segmented into quartiles (P < 0.001). Notably, in Model 3, the prevalence in Quartile 4 was 29% lower than in Quartile 1 [0.71 (0.59, 0.85), P < 0.001], and the trend test was also significant (P for trend <0.05). Furthermore, Figure 2 illustrates a nonlinear association between CDAI and cardiovascular disease. Figure 3 shows the base on gender nonlinear association between cardiovascular disease and CDAI. Additionally, Table 3 demonstrates a statistically significant negative association between the prevalence of CVD and the CDAI, particularly in both women and the overall population (P < 0.05). Specifically, in women, when the CDAI is less than 3.05, and for every unit increase in CDAI, the prevalence of CVD decreased by 6% (OR = 0.94, 95% CI: 0.90–0.98, P = 0.005).
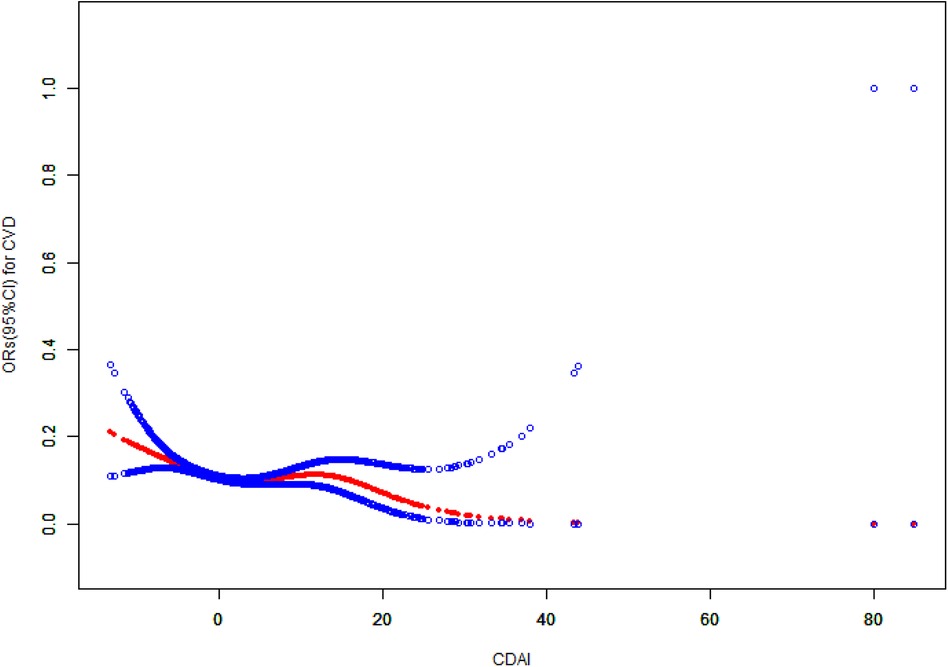
Figure 2 The association between CDAI and cardiovascular disease. CDAI, composite dietary antioxidant index; CVD, cardiovascular disease; CI, confidence interval; OR, odds ratio.
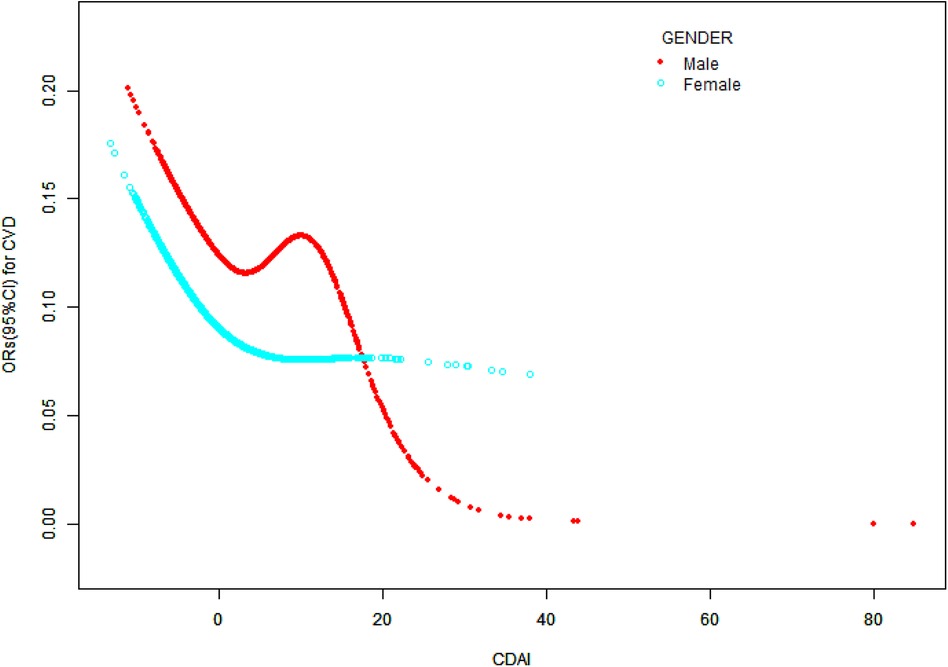
Figure 3 The association between CDAI and cardiovascular disease stratified by sex CDAI, composite dietary antioxidant index; CVD, cardiovascular disease; CI, confidence interval; OR, odds ratio.
According to Table 4, in our subgroup analysis, which considered variables such as gender, age, race, education level, PIR, BMI, and habits like smoking and drinking, along with hyperlipidemia, diabetes, and hypertension, the negative association between CDAI and cardiovascular disease persisted across all categories. Nevertheless, there was a significant interaction between the CDAI and CVD in the smoking subgroup analysis (P for interaction <0.05).
Sensitivity analyses conducted with unweighted logistic regression, as presented in Table 5, reveal a consistent negative association between CDAI and CVD prevalence across Model 1, Model 2, and Model 3. These findings align with those obtained from the weighted logistic regression analysis.
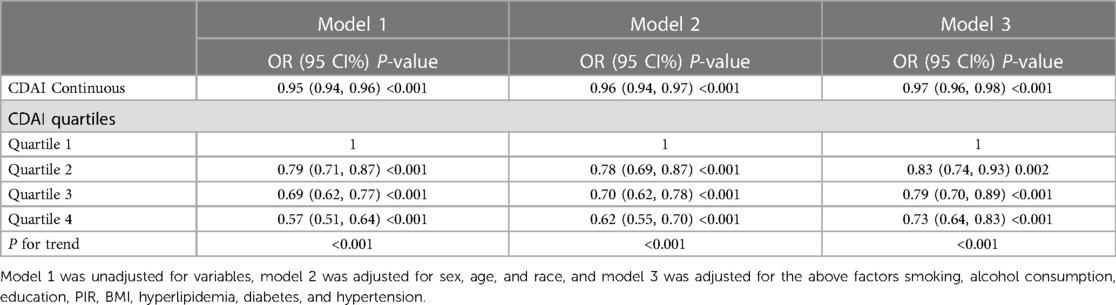
Table 5 The association between CDAI and cardiovascular disease in sensitivity analysis using unweighted logistic regression analysis.
To the best of our knowledge, our investigation represents the inaugural study exploring the association between CDAI values and the prevalence of cardiovascular disease. This study encompassed a cohort of 25,997 individuals from the 2011 to 2020 NHANES database. Our findings reveal a nonlinear association between CDAI and CVD prevalence. This negative association appeared robust and unaffected by variables such as gender, age, race, education level, PIR, BMI, alcohol consumption, hyperlipidemia, hypertension, and diabetes (P > 0.05). This consistency underlines the reliability and stability of the negative association between CDAI and CVD prevalence. Furthermore, our analysis of women identified an inflection point in the CDAI and cardiovascular disease association at a CDAI value of 3.05. Intriguingly, below this threshold, each unit increase in CDAI corresponded to a 6.0% decrease in CVD prevalence (P < 0.05).
OS has been recognized as one of the risk factors for cardiovascular disease. However, single antioxidant nutrients do not exhibit uniform associations with cardiovascular disease. A meta-analysis indicated that vitamin C, vitamin E, and β-carotene may potentially reduce the risk of cardiovascular disease mortality (28). Another meta-analysis of 884 randomized controlled intervention trials showed that individual vitamins C, D, E, and selenium did not impact cardiovascular disease incidence significantly. In contrast, β-carotene supplementation increased all-cause mortality, CVD mortality, and stroke risk (29). A study by Nazari suggests that zinc supplementation may increase the risk of coronary atherosclerosis (30), but further investigation is needed to understand the exact mechanism. A randomized controlled trial confirms that vitamin A and vitamin D supplementation improves clinical prognosis in patients with ischemic stroke (31). It is important to note that maintaining normal cellular function depends on the balance between OS and antioxidant capacity, and excessive intake of antioxidant nutrients may have adverse effects (32). The amount of antioxidants needed for protection may vary among individuals, influenced by factors such as gender, age, and lifestyle habits (33). Our study demonstrates that the U-shaped association between CDAI and cardiovascular disease exists only in women, consistent with the findings of Liu, who reported a similar L-shaped association between CDAI levels and atherosclerotic cardiovascular disease in postmenopausal women (34).
There was a significant interaction between CDAI quartiles and CVD prevalence in the smoking subgroup analysis. (P for interaction = 0.003). This may be because smoking exacerbates cardiovascular disease risk via mechanisms such as heightened oxidative stress, inflammatory responses, and impaired endothelial function (35). In concert with CDAI, these factors intensify the association in smokers. Higher CDAI levels appeared to have a more significant impact on cardiovascular health in smoking populations compared to non-smoking populations. Smoking may serve as an amplifying factor for the effects of CDAI on cardiovascular health. However, further prospective research is needed to determine the exact mechanism underlying this behavior. Meanwhile, the pathogenesis of cardiovascular disease due to oxidative stress is complex, and further research is warranted to confirm these conclusions. Different antioxidants may exhibit synergistic or antagonistic effects on cardiovascular disease, influencing its development through its ability to combat OS (36). In contrast, CDAI is an indicator that combines six antioxidant nutrients, providing a comprehensive assessment of their impact on cardiovascular health (37, 38).
Our study has several strengths: firstly, it is the first to investigate the association between CDAI and cardiovascular disease in the general population; secondly, our model adjusted for potential confounders as comprehensively as possible; and thirdly, our study utilized the NHANES database, which provided health- and nutrition-related data on 25,997 participants, enhancing the reliability of our results. Nevertheless, our study has certain limitations. First of all, Variations across different periods might influence the CDAI, variables, and the prevalence of cardiovascular disease. Although we adhered to NHANES guidelines for calculating complex sample weights, we cannot entirely dismiss the potential impact on our findings. And because the study is cross-sectional, it is more challenging to determine the causative links between CDAI and CVD risks. Additional prospective research is required to validate our results. Secondly, we may not have accounted for all potential confounders despite adjusting for multiple covariates. Thirdly, the results mainly apply to the American population because racial dietary patterns range significantly, and further multiethnic research is required to investigate the association between CDAI and cardiovascular disease.
In conclusion, our study confirms the negative association between CDAI and CVD prevalence in the general population, and women, the inflection point was 3.05. However, we need more prospective studies to explore further.
Publicly available datasets were analyzed in this study. This data can be found: https://wwwn.cdc.gov/nchs/nhanes/.
The studies involving humans were approved by the ethical review board for the National Health and Nutrition Examination Survey is currently known as the “NCHS Ethics Review Board.” It is affiliated with the National Center for Health Statistics, which is part of the Centers for Disease Control and Prevention. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
RW: Investigation, Methodology, Software, Writing – original draft, Writing – review & editing. WT: Investigation, Methodology, Writing – review & editing. XC: Funding acquisition, Supervision, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
This research was funded by the Anhui Medical University Research of China (Grant no. 2023xkj238) and the Municipal Health and Wellness Committee 2023 Applied Medical Research Program of Hefei (Grant no. Hwk2023yb024).
We are thankful to the National Health and Nutrition Examination Survey (NHANES) for providing the database that enriched our research. Their valuable data contribution was a cornerstone in the development of our study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. (2020) 396(10258):1223–49. doi: 10.1016/S0140-6736(20)30752-2
2. Tsao CW, Aday AW, Almarzooq ZI, Anderson CAM, Arora P, Avery CL, et al. Heart disease and stroke statistics-2023 update: a report from the American heart association. Circulation. (2023) 147(8):e93–621. doi: 10.1161/CIR.0000000000001123
3. Shaito A, Aramouni K, Assaf R, Parenti A, Orekhov A, Yazbi AE, et al. Oxidative stress-induced endothelial dysfunction in cardiovascular diseases. Front Biosci (Landmark Ed). (2022) 27(3):105. doi: 10.31083/j.fbl2703105
4. Incalza MA, D’Oria R, Natalicchio A, Perrini S, Laviola L, Giorgino F. Oxidative stress and reactive oxygen species in endothelial dysfunction associated with cardiovascular and metabolic diseases. Vascul Pharmacol. (2018) 100:1–19. doi: 10.1016/j.vph.2017.05.005
5. Yang X, Li Y, Li Y, Ren X, Zhang X, Hu D, et al. Oxidative stress-mediated atherosclerosis: mechanisms and therapies. Front Physiol. (2017) 8:600. doi: 10.3389/fphys.2017.00600
6. Poyatos P, Gratacós M, Samuel K, Orriols R, Tura-Ceide O. Oxidative stress and antioxidant therapy in pulmonary hypertension. Antioxidants (Basel). (2023) 12(5):1006. doi: 10.3390/antiox12051006
7. Batty M, Bennett MR, Yu E. The role of oxidative stress in atherosclerosis. Cells. (2022) 11(23):3843. doi: 10.3390/cells11233843
8. Orellana-Urzúa S, Briones-Valdivieso C, Chichiarelli S, Saso L, Rodrigo R. Potential role of natural antioxidants in countering reperfusion injury in acute myocardial infarction and ischemic stroke. Antioxidants (Basel). (2023) 12(9):1760.
9. Li Y, Ling GC, Ni RB, Ni SH, Sun SN, Liu X, et al. Association of dietary total antioxidant capacity with all-cause and cardiovascular mortality in patients with chronic kidney disease: based on two retrospective cohort studies of NHANES. Ren Fail. (2023) 45(1):2205950. doi: 10.1080/0886022X.2023.2205950
10. Wang L, Yi Z. Association of the composite dietary antioxidant index with all-cause and cardiovascular mortality: a prospective cohort study. Front Cardiovasc Med. (2022) 9:993930. doi: 10.3389/fcvm.2022.993930
11. Barchitta M, Maugeri A, La Mastra C, Rosa MC, Favara G, Lio RMS, et al. Dietary antioxidant intake and human papillomavirus infection: evidence from a cross-sectional study in Italy. Nutrients. (2020) 12(5):1384. doi: 10.3390/nu12051384
12. Zhang J, Lu X, Wu R, Ni H, Xu L, Wu W, et al. Associations between composite dietary antioxidant index and estimated 10-year atherosclerotic cardiovascular disease risk among U.S. adults. Front Nutr. (2023) 10:1214875. doi: 10.3389/fnut.2023.1214875
13. Xu Q, Qian X, Sun F, Liu H, Dou Z, Zhang J. Independent and joint associations of dietary antioxidant intake with risk of post-stroke depression and all-cause mortality. J Affect Disord. (2023) 322:84–90. doi: 10.1016/j.jad.2022.11.013
14. Wright ME, Mayne ST, Stolzenberg-Solomon RZ, Li Z, Pietinen P, Taylor PR, et al. Development of a comprehensive dietary antioxidant index and application to lung cancer risk in a cohort of male smokers. Am J Epidemiol. (2004) 160(1):68–76. doi: 10.1093/aje/kwh173
15. Chen Y, Tang W, Li H, Lv J, Chang L, Chen S. Composite dietary antioxidant index negatively correlates with osteoporosis among middle-aged and older US populations. Am J Transl Res. (2023) 15(2):1300–8.36915799
16. Zhao L, Sun Y, Cao R, Wu X, Huang T, Peng W. Non-linear association between composite dietary antioxidant index and depression. Front Public Health. (2022) 10:988727. doi: 10.3389/fpubh.2022.988727
17. Yang C, Yang Q, Peng X, Li X, Rao G. Associations of composite dietary antioxidant index with cardiovascular disease mortality among patients with type 2 diabetes. Diabetol Metab Syndr. (2023) 15(1):131. doi: 10.1186/s13098-023-01109-7
18. Wu M, Si J, Liu Y, Kang L, Xu B. Association between composite dietary antioxidant index and hypertension: insights from NHANES. Clin Exp Hypertens. (2023) 45(1):2233712. doi: 10.1080/10641963.2023.2233712
19. Ma R, Zhou X, Zhang G, Wu H, Lu Y, Liu F, et al. Association between composite dietary antioxidant index and coronary heart disease among US adults: a cross-sectional analysis. BMC Public Health. (2023) 23(1):2426. doi: 10.1186/s12889-023-17373-1
20. Ma Y, Liu J, Sun J, Cui Y, Wu P, Wei F, et al. Composite dietary antioxidant index and the risk of heart failure: a cross-sectional study from NHANES. Clin Cardiol. (2023) 46(12):1538–43. doi: 10.1002/clc.24144
21. Luu HN, Wen W, Li H, Dai Q, Yang G, Cai Q, et al. Are dietary antioxidant intake indices correlated to oxidative stress and inflammatory marker levels? Antioxid Redox Signal. (2015) 22(11):951–9. doi: 10.1089/ars.2014.6212
22. Tan Z, Meng Y, Li L, Wu Y, Liu C, Dong W, et al. Association of dietary fiber, composite dietary antioxidant Index and risk of death in tumor survivors: national health and nutrition examination survey 2001–2018. Nutrients. (2023) 15(13):2968. doi: 10.3390/nu15132968
23. Jackson SL, Yang EC, Zhang Z. Income disparities and cardiovascular risk factors among adolescents. Pediatrics. (2018) 142(5):e20181089. doi: 10.1542/peds.2018-1089
24. Phillips JA. Dietary guidelines for Americans, 2020–2025. Workplace Health Saf. (2021) 69(8):395. doi: 10.1177/21650799211026980
25. Eke PI, Dye BA, Wei L, Slade GD, Thornton-Evans GO, Borgnakke WS, et al. Update on prevalence of periodontitis in adults in the United States: NHANES 2009 to 2012. J Periodontol. (2015) 86(5):611–22. doi: 10.1902/jop.2015.140520
26. Mahemuti N, Jing X, Zhang N, Liu C, Li C, Cui Z, et al. Association between systemic immunity-inflammation index and hyperlipidemia: a population-based study from the NHANES (2015–2020). Nutrients. (2023) 15(5):1177. doi: 10.3390/nu15051177
27. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III) final report. Circulation. (2002) 106(25):3143–421. doi: 10.1161/circ.106.25.3143
28. Jayedi A, Rashidy-Pour A, Parohan M, Zargar MS, Shab-Bidar S. Dietary and circulating vitamin C, vitamin E, β-carotene and risk of total cardiovascular mortality: a systematic review and dose-response meta-analysis of prospective observational studies. Public Health Nutr. (2019) 22(10):1872–87. doi: 10.1017/S1368980018003725
29. An P, Wan S, Luo Y, Luo J, Zhang X, Zhou S, et al. Micronutrient supplementation to reduce cardiovascular risk. J Am Coll Cardiol. (2022) 80(24):2269–85. doi: 10.1016/j.jacc.2022.09.048
30. Nazari M, Ashtary-Larky D, Nikbaf-Shandiz M, Goudarzi K, Bagheri R, Dolatshahi S, et al. Zinc supplementation and cardiovascular disease risk factors: a GRADE-assessed systematic review and dose-response meta-analysis. J Trace Elem Med Biol. (2023) 79:127244. doi: 10.1016/j.jtemb.2023.127244
31. Kadri A, Sjahrir H, Juwita Sembiring R, Ichwan M. Combination of vitamin A and D supplementation for ischemic stroke: effects on interleukin-1ß and clinical outcome. Med Glas (Zenica). (2020) 17(2):425–32. doi: 10.17392/1137-20
32. Senoner T, Dichtl W. Oxidative stress in cardiovascular diseases: still a therapeutic target? Nutrients. (2019) 11(9):2090. doi: 10.3390/nu11092090
33. Biesalski HK, Grune T, Tinz J, Zöllner I, Blumberg JB. Reexamination of a meta-analysis of the effect of antioxidant supplementation on mortality and health in randomized trials. Nutrients. (2010) 2(9):929–49. doi: 10.3390/nu2090929
34. Liu C, Lai W, Zhao M, Zhang Y, Hu Y. Association between the composite dietary antioxidant index and atherosclerotic cardiovascular disease in postmenopausal women: a cross-sectional study of NHANES data, 2013–2018. Antioxidants (Basel). (2023) 12(9):1740. doi: 10.3390/antiox12091740
35. Messner B, Bernhard D. Smoking and cardiovascular disease: mechanisms of endothelial dysfunction and early atherogenesis. Arterioscler Thromb Vasc Biol. (2014) 34(3):509–15. doi: 10.1161/ATVBAHA.113.300156
36. Schiffrin EL. Antioxidants in hypertension and cardiovascular disease. Mol Interv. (2010) 10(6):354–62. doi: 10.1124/mi.10.6.4
37. Wang T, Liu H, Wei X. Association between the composite dietary antioxidant index and stroke: a cross-sectional study. Biol Trace Elem Res. (2023). doi: 10.1007/s12011-023-04011-5
Keywords: oxidative stress, composite dietary antioxidant index, cardiovascular disease, NHANES, cross-sectional studies
Citation: Wang R, Tao W and Cheng X (2024) Association of composite dietary antioxidant index with cardiovascular disease in adults: results from 2011 to 2020 NHANES. Front. Cardiovasc. Med. 11:1379871. doi: 10.3389/fcvm.2024.1379871
Received: 31 January 2024; Accepted: 13 June 2024;
Published: 28 June 2024.
Edited by:
Monica Trif, Centre for Innovative Process Engineering, GermanyReviewed by:
Mihai Domnutiu Suciu, University of Medicine and Pharmacy Iuliu Hatieganu, Romania© 2024 Wang, Tao and Cheng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaobing Cheng, ZG9jY3hiQDEyNi5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.