
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med. , 08 March 2024
Sec. Atherosclerosis and Vascular Medicine
Volume 11 - 2024 | https://doi.org/10.3389/fcvm.2024.1353945
 Yuanping Wang1,†
Yuanping Wang1,† Cheng Chen2,†
Cheng Chen2,† Qiaofen Lin1,†
Qiaofen Lin1,† Qingling Su1
Qingling Su1 Yiquan Dai2
Yiquan Dai2 Hongyu Chen2
Hongyu Chen2 Tianmin He2
Tianmin He2 Xiantao Li2
Xiantao Li2 Ruimei Feng3
Ruimei Feng3 Wuqing Huang1
Wuqing Huang1 Zhijian Hu1
Zhijian Hu1 Jun Chen1
Jun Chen1 Shanshan Du1*
Shanshan Du1* Pingfan Guo2*
Pingfan Guo2* Weimin Ye1,4*
Weimin Ye1,4*
Background: Although the impact of hypertension on carotid intima-media thickness (IMT) and plaques has been well established, its association with femoral IMT and plaques has not been extensively examined. In addition, the role of the ratio of systolic and diastolic pressure (SDR) in the subclinical atherosclerosis (AS) risk remains unknown. We assessed the relationship between SDR and carotid and femoral AS in a general population.
Methods: A total of 7,263 participants aged 35–74 years enrolled from January 2019 to June 2021 in a southeast region of China were included in a cross-sectional study. Systolic and diastolic blood pressure (SBP and DBP) were used to define SDR. Ultrasonography was applied to assess the AS, including thickened IMT (TIMT) and plaque in the carotid and femoral arteries. Logistic regression and restricted cubic spline (RCS) models were the main approaches.
Results: The prevalence of TIMT, plaque, and AS were 17.3%, 12.4%, and 22.7% in the carotid artery; 15.2%, 10.7%, and 19.5% in the femoral artery; and 23.8%, 17.9% and 30.0% in either the carotid or femoral artery, respectively. Multivariable logistic regression analysis found a significant positive association between high-tertile SDR and the higher risk of overall TIMT (OR = 1.28, 95% CI = 1.10–1.49), plaques (OR = 1.36, 95%CI = 1.16–1.61), or AS (OR = 1.36, 95% CI = 1.17–1.57), especially in the carotid artery. RCS analysis further revealed the observed positive associations were linear. Further analyses showed that as compared to the low-tertile SDR and non-hypertension group, high-tertile SDR was associated with increased risks of overall and carotid TIMT, plaques, or AS in both groups with or without hypertension.
Conclusions: SDR is related to a higher risk of subclinical AS, regardless of hypertension or not, suggesting that as a readily obtainable index, SDR can contribute to providing additional predictive value for AS.
Peripheral artery disease (PAD) is an atherosclerotic disease of the arteries, which is always underappreciated due to being symptomless in its early stages. As a predecessor of cardiovascular diseases (CVD), it confers an elevated risk of various adverse outcomes. It has been recognized as an increasing global public health issue, receiving more and more attention in recent years (1–3). It is known that the intima of middle- and large-sized arteries are most vulnerable to atherosclerosis (AS), especially the sites of vessel branching, due to the nature of the blood flow (4). Thus, AS screening in carotid and femoral arteries is of great importance to CVD prevention, especially in the general population. However, early AS detection in the general population has mainly focused on the carotid artery (3), while femoral AS is still underrecognized (2).
Hypertension is defined by systolic and diastolic blood pressure (SBP and DBP), referring to the pressure produced by arteries during systolic and diastolic activities of the heart, which could reflect the early hemodynamic changes, perfusion of organs, and heart systolic function. Lower SBP/DBP levels have been strictly recommended to decrease CVD risk (5–7). It can also greatly reduce the risk of atherosclerotic CVD and death (8). However, there is a dearth of studies distinguishing the role of BP in the AS across different sites. In addition to the absolute value of SBP or DBP, recent studies proposed a novel index, the ratio of SBP and DBP (SDR) (9). Some studies have shown that hypertensive subjects with proper SDR may suffer from less severe forms of end-organ damage than those with ratios significantly deviating from the mean ratio (10), indicating the potentially additional predictive value of SDR in cardiovascular outcomes. However, its implication in AS risk has previously not been evaluated.
In the current study, we conducted a cross-sectional study in southeastern China to explore the association between SDR and AS in arteries, including carotid and femoral arteries.
Data for this cross-sectional study were collected from the baseline survey of the Fuqing Cohort Study (11–13), conducted in Fuqing City, Fujian Province, China. Native residents aged 35–74 years were recruited, and a total of 10,193 residents participated in the baseline survey of the cohort from January 2019 to June 2021. Participants were excluded from the analyses if they met the criteria below:
1. individuals aged <35 or ≥75 years (n = 88);
2. incomplete questionnaire survey on disease history (n = 591);
3. missing data on BP measurements (n = 151);
4. a self-reported history of coronary heart disease, stroke, or malignant tumor (n = 19);
5. without measurement of peripheral AS (n = 2,081).
After excluding 2,930 participants, a total of 7,263 individuals were included in the final study. Permission for the cohort study was obtained from the Ethics Committee of Fujian Medical University (approval number: [2017–07] and [2020–58]) before data collection. Written informed consent was obtained from all the participants prior to the enrollment of this study.
The details of data collection have been described in previous studies (13, 14). Briefly, a structured questionnaire compiled by the Fujian Cohort Research Center was used to collect information on demographic and sociological characteristics (age, gender, occupation, and education), disease and medication history, family history of disease, and lifestyles (smoking, drinking, and physical activity). Anthropometric measurements were taken to determine height (cm) and weight (kg), and body mass index (BMI) was calculated and classified into underweight, normal weight, overweight, and obese groups according to the recommendations of the Working Group on Obesity in China (15). Fasting venous blood was taken to determine fasting blood glucose (FBG), glucose hemoglobin A1c (HbA1c), total cholesterol, triglyceride, high density lipoprotein cholesterol and low density lipoprotein cholesterol. Diabetes refers to a measured FBG ≥ 7.0 mmol/L or HbA1c ≥ 6.5%, self-reported history of diabetes, and/or taking antidiabetic drugs. Hyperlipidemia was defined as present if ≥1 of the following criteria are satisfied: total cholesterol >6.2 mmol/L, triglyceride >2.3 mmol/L, high-density lipoprotein cholesterol <1.0 mmol/L, or low-density lipoprotein cholesterol >4.1 mmol/L. Treatment of AS was referred to using drugs that could act on the vascular wall.
SDR was defined as the ratio between SBP and DBP. BP measurements were taken on the right upper arm at the heart level by trained employees using an electronic blood pressure monitor (OMRON, U30, Japan). SBP and DBP were recorded twice. A third measurement was taken if there was a difference of more than 5 mmHg between the two measurements. The average of the two closest measurements was used to define the value of BP.
Hypertension was referred to SBP ≥ 140 mmHg or/and DBP ≥ 90 mmHg, self-reported history of hypertension (HT), or taking antihypertensive drugs. Normotension was defined as averaged SBP ranging from 90 to 119, or/and DBP ranging from 60 to 79 mmHg without self-reported diagnosis or treatment of HT; prehypertension (PreHT) was defined as averaged SBP ranging from 120 to 139, or/and DBP ranging from 80 to 89 mmHg without self-reported diagnosis or treatment of HT.
AS was the primary outcome, defined as the presence of thickened intima-media thickness (TIMT) or/and plaques in the carotid or/and femoral arteries. TIMT and plaques in the carotid or/and femoral arteries were the secondary outcomes. B-mode ultrasound imaging (EDGEII, Sono Sound, America) was performed to determine IMT and plaques in the carotid and femoral arteries synchronously by qualified surgeons, as previously reported (11, 12).
Briefly, TIMT was reported if there exists an IMT ≥ 1.0 mm at any one of the four arteries. IMT ≥1.5 mm, or a focal structure encroaching into the arterial lumen by at least 0.5 mm, or >50% of the surrounding IMT value was regarded as the presence of plaque (16). According to the specific vascular location of TIMT, plaques, and AS, participants were diagnosed as only carotid TIMT, plaques, and AS (C-TIMT, C-P, and C-AS), only femoral TIMT, plaques, and AS (F-TIMT, F-P, and F-AS), and either carotid or femoral TIMT, plaques, and AS (CF-TIMT, CF-P, and CF-AS).
All statistical analyses were performed using SAS 9.4 statistical software, and a P-value < 0.05 was considered statistically significant. Individuals were divided into low-, medium-, and high-SDR groups according to their tertiles. Continuous variables were expressed as mean and standard deviations (SD), and compared using one-way ANOVA among three groups. Categorical variables were reported as numbers and proportions, and compared using the Chi-squared tests across groups. The correlation coefficients between SDR and SBP or DBP were determined using the Spearman correlation test and displayed with a scatter plot. The joint effect of SBP and DBP on AS risk was first clarified by univariable logistic regression, the estimates of which were shown as heat maps. Univariable and multivariable logistic regression analyses were used to generate odds ratios (ORs) and 95% confidential intervals (CIs) for the association between SDR groups and TIMT, plaques, or AS in carotid, femoral, or both arteries, respectively. Multivariable models included age- and sex-adjusted models and a fully-adjusted model, and the fully-adjusted model included age, sex, BMI, occupation, education, alcohol drinking, smoking, diabetes, dyslipidemia, SBP, and treatment of AS. A restricted cubic spline (RCS) plot with five knots was used to present the linear or nonlinear relationship between continuous SDR level and AS risk.
Considering the joint effects of HT and SDR on AS risk, we regrouped all participants into six subgroups according to SDR and HT, and they were low-SDR and non-HT (L-SDR & non-HT), medium-SDR and non-HT (M-SDR & non-HT), high-SDR and non-HT (H-SDR & non-HT), low-SDR and HT (L-SDR & HT), medium-SDR and HT (M-SDR & HT), and high-SDR and HT (H-SDR & HT). Multivariable adjusted logistic regression analyses were used to estimate the ORs of joint effects of SDR and HT for AS risk, with L-SDR & non-HT group as the reference.
The ORs of preHT and HT (normotension, PreHT, and HT) for AS risk were also calculated in fully adjusted logistic regression analyses. The absolute SBP value was categorized into <110 mmHg, 110 mmHg–119 mmHg, 120 mmHg–124 mmHg, 125 mmHg–129 mmHg, 130 mmHg–139 mmHg, and ≥140 mmHg, while DBP was categorized into <75 mmHg, 75 mmHg–79 mmHg, 80 mmHg–84 mmHg, 85 mmHg–89 mmHg, and ≥90 mmHg. A heat map from GraphPad Prism was applied to display the ORs between each BP subgroup and AS risk. Considering the significant differences in BP and SDR levels between hypertensive and non-hypertensive populations, we performed a stratified analysis. The relationship between SDR and AS risk in these two groups was discussed respectively. In addition, we also conducted an RCS analysis of the risk of SDR and AS to explore the potential linear and non-linear association between them, and to explore whether the potential optimal SDR for non-hypertensive and hypertensive populations was similar or not.
To further explore the association between SDR and AS risk, we also performed a sensitivity analysis. Participants with antihypertensive medicine were excluded, and the association between SDR, HT, and their six subgroups and AS risk were reanalyzed, considering the potential effect of the medicine on BP values and AS risk.
The average SBP and DBP of 7,263 participants were 134.41 (±20.71) mmHg and 84.55 (±11.22) mmHg, respectively. The prevalence of HT was 46.3%. The SDR ranged from 1.17 to 2.93 (Mean: 1.59, SD: 0.17). According to its tertiles, low-, medium-, and high-SDR groups were defined as SDR < 1.506, 1.506–1.643, and > 1.643 (Table 1). The SDP, DBP, and HT prevalence rates were significantly higher in high-SDR groups. Participants with high SDR were more likely to be older, female, obese, receiving treatment for AS, less educated, more likely to be farmers or unemployed, less likely to be current smokers or alcohol drinkers, and have diabetes and dyslipidemia. The distribution of SBP and DBP across SDR is depicted in Figure 1. The scatter plots reveal a notable positive correlation between SDR and SBP, and a moderate inverse correlation between SDR and DBP. The correlation coefficients between SDR-SBP and SDR-DBP were 0.515 and −0.197, respectively.
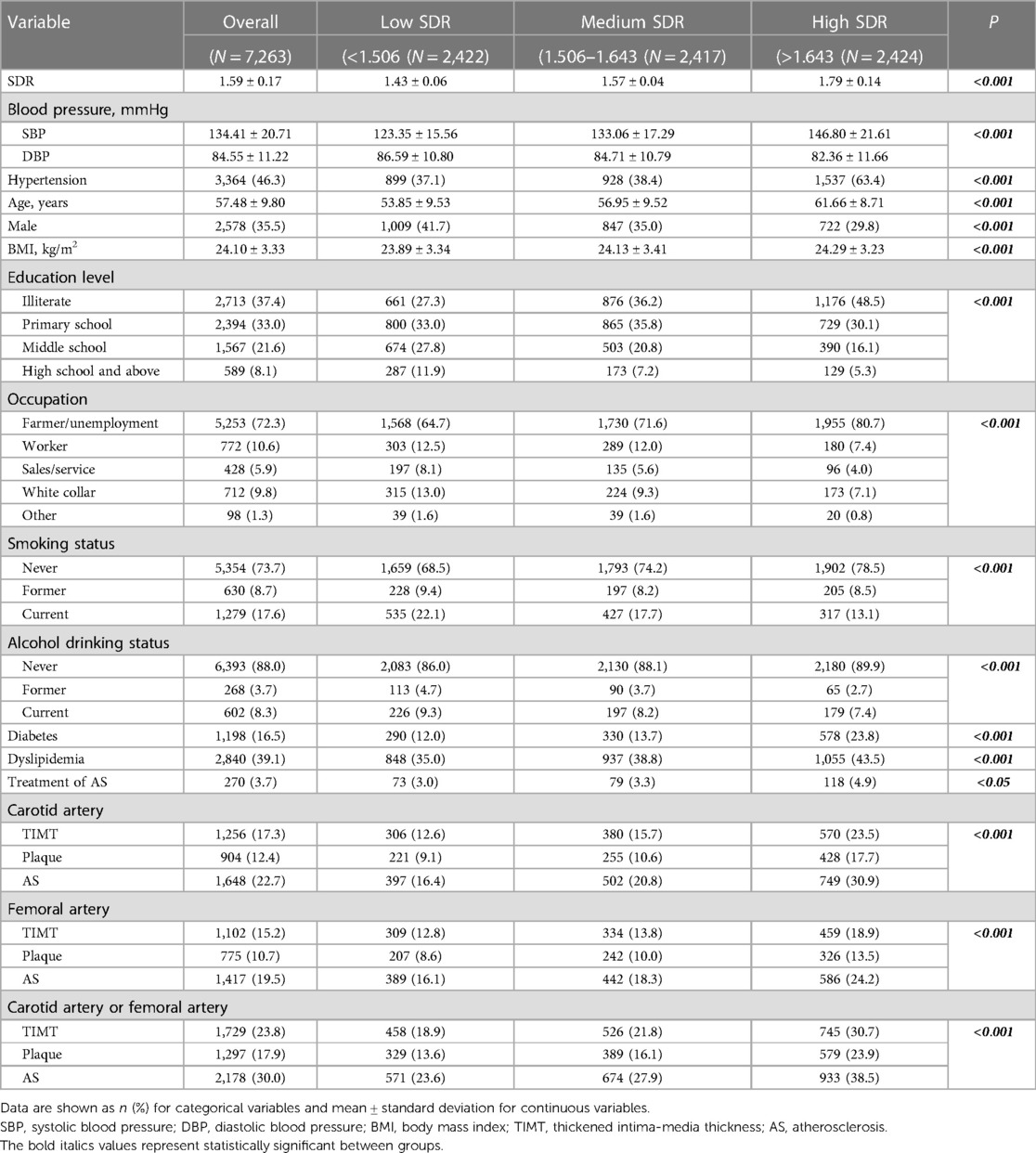
Table 1. Characteristics of the study population by systolic/diastolic ratio (SDR) of blood pressure.
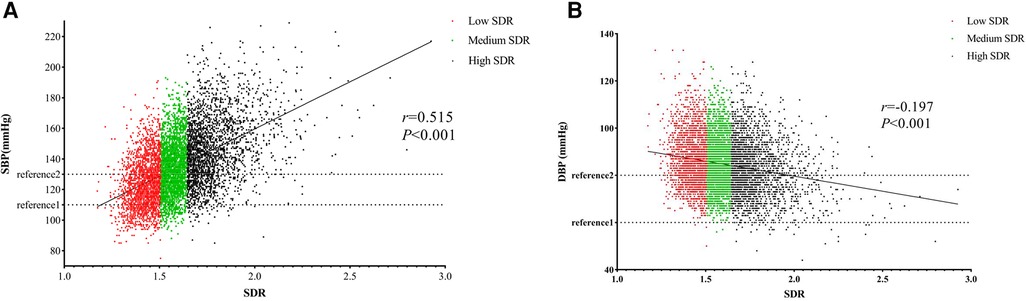
Figure 1. Distribution of SDR with SBP (A) and DBP (B) SDR, the ratio of systolic and diastolic pressure; SBP, systolic blood pressure; DBP, diastolic blood pressure.
In the whole population, the prevalence rates of TIMT, plaques, and AS were 17.3%, 12.4%, and 22.7% in the carotid artery, and 15.2%, 10.7%, and 19.5% in the femoral artery, respectively. When defining AS in either carotid or femoral artery, the prevalence rates of TIMT, plaques, and AS were 23.8%, 17.9%, and 30.0%. From the low- to high-SDR group, the prevalence of TIMT, plaques, and AS in carotid and/or femoral arteries all increased gradually.
The heatmap of the ORs in Figure 2 shows the joint effects of SBP and DBP on CF-AS risk, in which the blank in white was the reference group (SBP 110–119 mmHg and DBP 75–79 mmHg), the red blank marked an OR > 1.0, the blue marked an OR < 1.0, and the OR became higher as the color deepened. Overall, with the increasing SBP, the ORs for AS became higher, but the values at a given SBP group varied by DBP groups. As compared to the reference, both lower and higher DBP seemed to be associated with a higher prevalence of AS. These findings suggested that an index combining SBP and DBP, such as SDR, might provide more information.
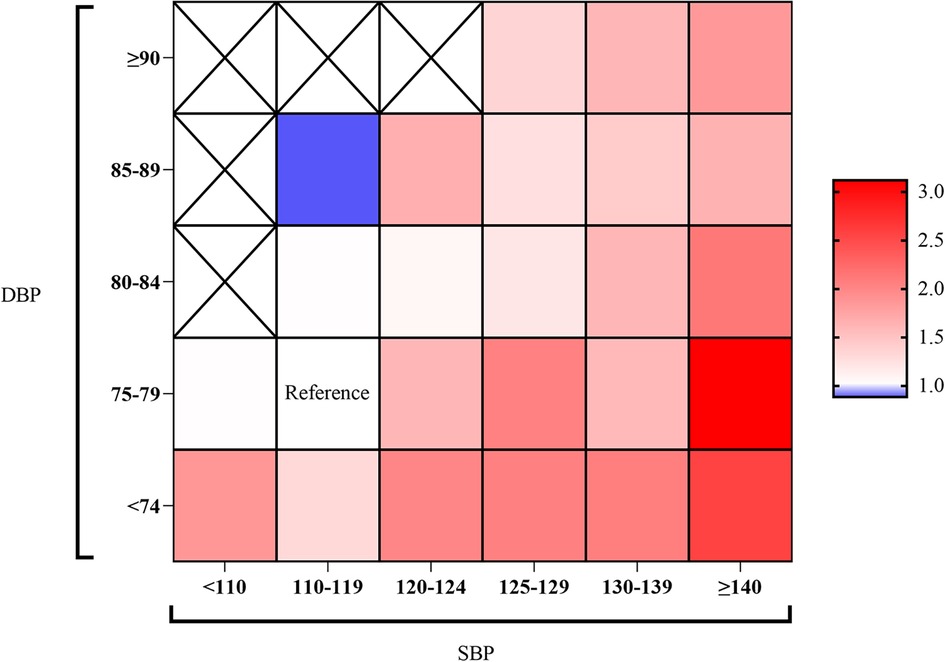
Figure 2. Heat map of the association between BP levels and carotid and femoral AS risk. SBP level was at the x-axis, and DBP level was at the y-axis. The color represents the odds ratio of AS risk at a given SBP/DBP level. SBP/DBP at 110–119/75–79 mmHg was set as a reference group. The blanks with “×” indicated missing OR values due to the small sample size.
The low-SDR group was set as a reference in logistic regression models. As shown in Table 2, after adjusting for covariates, the ORs (95% CIs) of high-SDR for C-TIMT, and C-AS were significant, with values of 1.39 (1.15,1.68), and 1.38 (1.16,1.63), respectively. On the contrary, the ORs of medium-SDR for C-TIMT, C-P, and C-AS were all non-significant. In the femoral artery, neither medium- nor high-SDR was associated with F-TIMT, F-P, and F-AS risk. Combining the carotid and femoral arteries, a significantly higher risk for CF-TIMT, CF-AS could be observed in high-SDR, and the ORs (95%CI) were 1.29 (1.09,1.53), and 1.26 (1.07,1.48), respectively. The associations between medium-SDR and CF-TIMT, CF-P, and CF-AS were not significant.
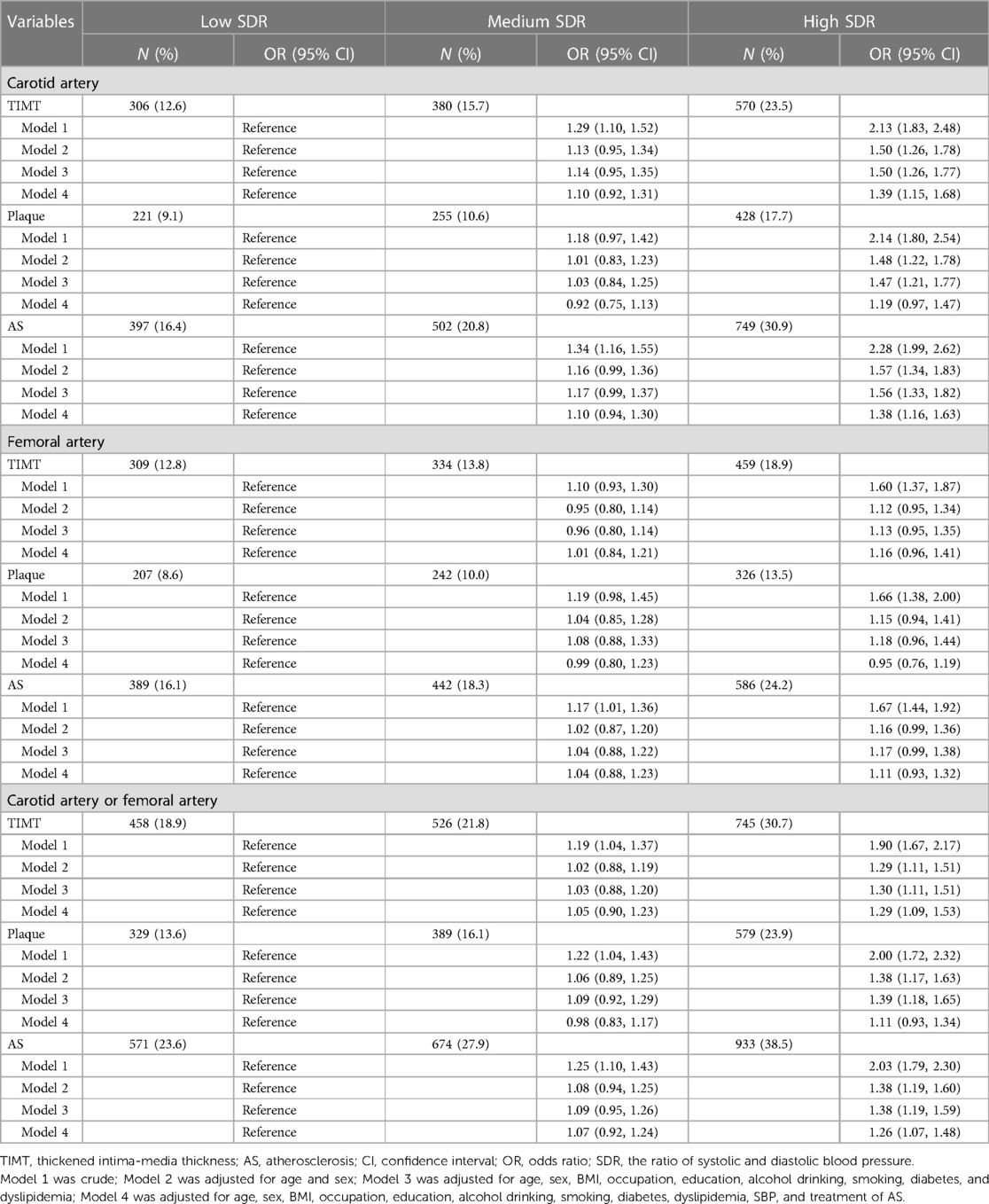
Table 2. ORs and 95% CIs for prevalence of atherosclerosis subgroup by the systolic/diastolic ratio (SDR) of blood pressure.
Results from RCS regression are shown in Figure 3. Positive linear relationships were observed between SDR and CF-TIMT, CF-AS, C-TIMT, C-P, and C-AS.
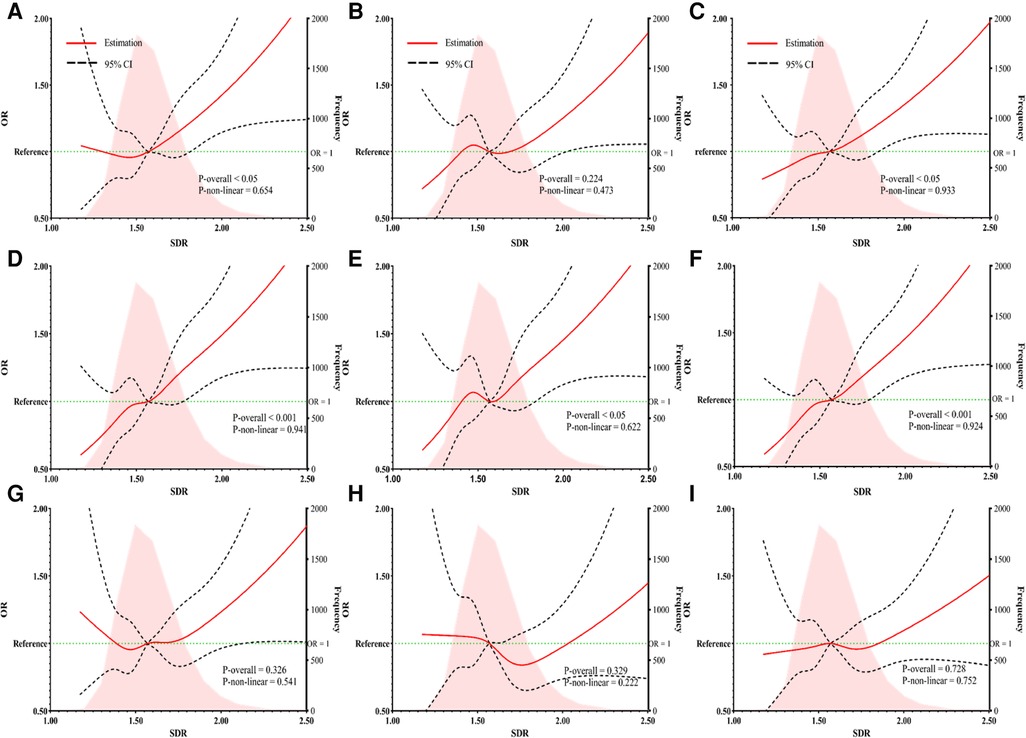
Figure 3. The RCS regression between SDR and the risk of carotid or femoral TIMT (A), plaque (B), and AS (C) the RCS regression between SDR and the risk of carotid TIMT (D), plaque (E), and AS (F) the RCS regression between SDR and the risk of femoral TIMT (G), plaque (H), and AS (I). SDR, the ratio of systolic and diastolic blood pressure; OR, odds ratio; CI, confidence interval.
As compared with normotension, HT was only positively associated with F-P in fully adjusted logistic regression models (Table 3). Thus, we then explored the joint effects of SDR and HT on AS risk. Taking the group with L-SDR and non-HT as the reference, the ORs of M-SDR and non-HT, H-SDR and non-HT, L-SDR and HT, M-SDR and HT, and H-SDR and HT for AS risk were calculated from fully adjusted logistic regression models (Supplementary Table S1), and shown in forest plots (Figure 4). For carotid artery, H-SDR and non-HT, and H-SDR and HT were associated with higher C-TIMT risk, and the ORs of H-SDR and non-HT, L-SDR and HT, M-SDR and HT, and H-SDR and HT for C-AS were all significant and higher than 1.0, suggesting the additional predictive value of SDR for carotid AS in both HT and non-HT population (Figure 4A). For femoral artery, L-SDR and HT, and H-SDR and HT were associated with higher F-TIMT risk, and H-SDR and non-HT, L-SDR and HT, M-SDR and HT, and H-SDR and HT were associated with higher F-AS risk, suggesting that although no association of SDR with femoral AS in overall population, SDR could provide more predictive value for femoral AS in HT population (Figure 4B). In either carotid or femoral artery, H-SDR and non-HT, L-SDR and HT, M-SDR and HT, and H-SDR and HT were associated with CF-TIMT and CF-AS risk (Figure 4C).
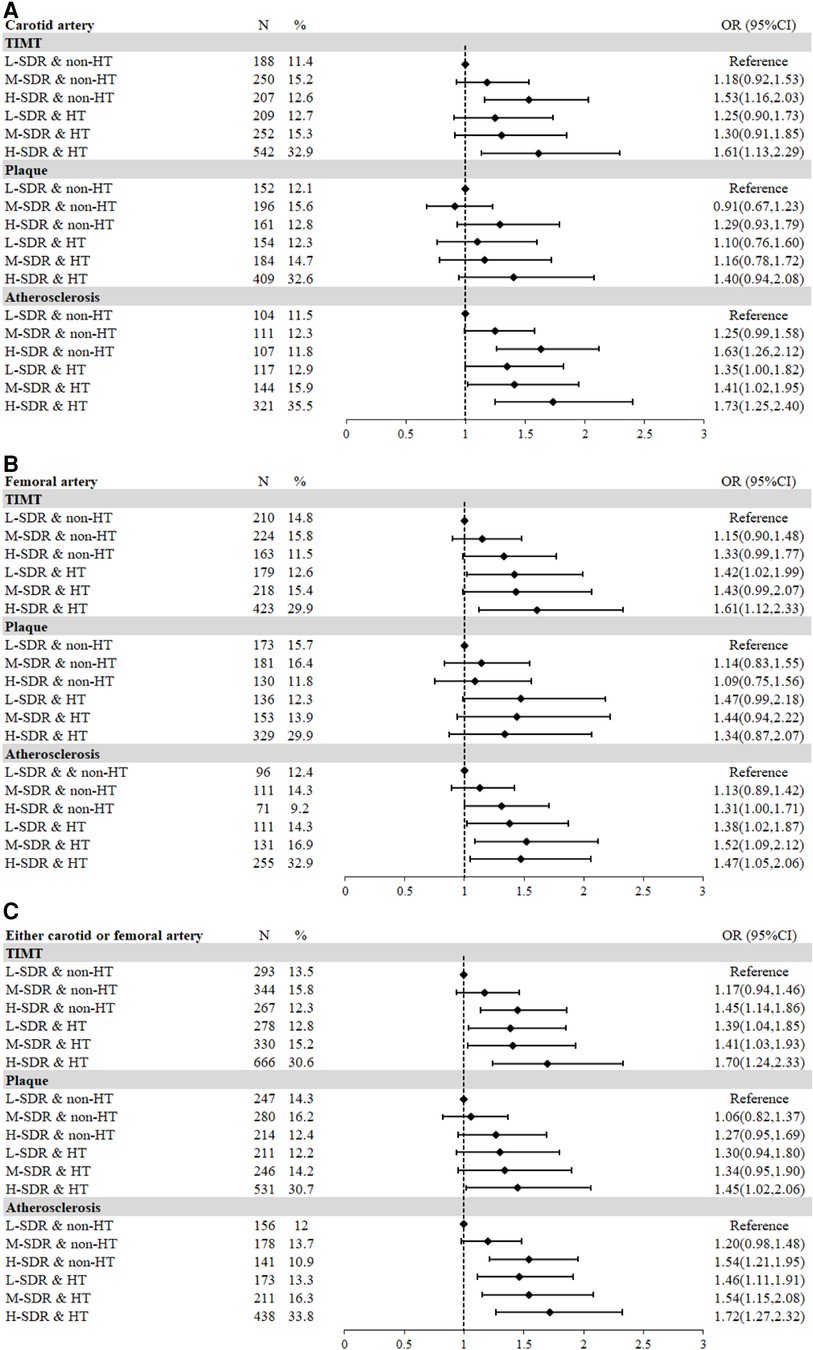
Figure 4. The joint effects of SDR and hypertension on AS risk. (A) Carotid artery; (B) Femoral artery; (C) Carotid or femoral arteries. TIMT, thickened intima-media thickness; AS, atherosclerosis; SDR, the ratio of systolic and diastolic blood pressure, OR, odds ratio; CI, confidence interval.
In fully adjusted logistic models, compared to L-SDR, H-SDR was associated with increased risks of C-TIMT, C-AS, CF-TIMT, and CF-AS in the non-hypertensive population (Supplementary Table S2), while only C-TIMT, C-AS in the HT stratum (Supplementary Table S3). In the hypertensive population, the RCS between SDR and TIMT, plaque, or AS showed a significant linear trend, and P values for non-linear trend were 0.558, 0.168 and 0.361 (Supplementary Figures S1D–S1F). The risks of CF-TIMT, CF-P, and CF-AS increased with the rise of the SDR level. In the non-hypertensive population, RCS between SDR and CF-AS also showed the same results (Supplementary Figure S1I), but not for TIMT and plaque (Supplementary Figures S1G,H).
To exclude the potential effect of medication, we reanalyzed the association of SDR-AS among participants without taking any antihypertensive medicine. The increased risk of C-TIMT, C-AS, CF-TIMT, and CF-AS could also be observed in high-SDR when compared with low-SDR in multivariable-adjusted logistic models (Supplementary Table S4). The RCS between SDR and CF-AS also showed a significant linear trend, with SDR = 1.56 when OR = 1.0 (Supplementary Figure S2). In BP subgroups, both HT and PreHT were not associated with any risk of AS when compared with normotension (Supplementary Table S5). We also regrouped the population into six subgroups according to SDR tertiles and HT status, and their associations with risk for AS in logistic models are shown in Supplementary Table S6. H-SDR and non-HT were associated with increased risks of C-TIMT, C-AS, CF-TIMT, and CF-AS. H-SDR and HT were associated with higher C-AS, CF-TIMT, and CF-AS risks. On the contrary, this association was only significant among the non-hypertensive population (Supplementary Table S7), not among the hypertensive population (Supplementary Table S8). The RCSs in non-hypertensive and hypertensive populations were both linear, with SDR at 1.54 and 1.62 when OR = 1.0 (Supplementary Figure S3).
The present study reported an AS screening project among native residents from a prospective cohort study in southeastern China and comprehensively investigated the association between BP and peripheral AS, including carotid and femoral arteries. The prevalence of AS, including TIMT and plaque, was 22.7% in the carotid artery, and 19.5% in the femoral artery. Of note, the total prevalence of AS was as high as 30.0% in either the carotid or femoral artery. The high SDR led to increased risks of TIMT, plaque, and AS, especially in the carotid artery. These findings suggested that SDR could provide additional predictive value for AS, regardless of hypertension or not. As a readily obtainable index, the clinical implication of SDR for AS or AS-related diseases is calling for further studies.
In the process of AS formation, the lesion from the fatty streak develops in the intima of the artery wall, thickening intima, which is an early sign of AS. Then the fatty streak evolves into a fibrous plaque. Thus, both TIMT and plaque were included in AS definition (17, 18). The sites of vessel branching in large-sized arteries are most vulnerable to AS (4). To date, the carotid artery is most frequently reported in previous studies (3), while the femoral artery has been less studied in a general population setting. In such cases, a screening program was launched among rural residents aged 35–74 years in southeastern China, and the IMT and presence of plaques were measured at the far wall of the left and right carotid arteries and femoral arteries concurrently (11, 12). Carotid AS, defined as TIMT and plaque, was reported among 22.7% of the current population, which was similar to the results of a meta-analysis using global datasets (3). As for femoral AS, it was diagnosed among 19.5% of the whole population, suggesting the AS screen in femoral arteries cannot be neglected. Previous studies, mostly from hospitalized populations, also showed the importance of additional femoral AS in cardiovascular risk assessment (19–21), and a study among factory workers in Spain found AS in 72% of the study population, with the prevalence of plaques in the femoral artery (54%), higher than that in the carotid artery (34%) (19). However, the importance of femoral AS in the general population is always underestimated. We highlighted more carotid and femoral AS screening programs in more generalized, larger sample-sized populations to address the burden of AS at finer levels.
HT could affect the arterial system by thickening artery walls, involving atherosclerotic plaques, and even increasing the vulnerability to rupture. Also, it has been widely recognized as an important, modifiable risk factor in CVD prevention (22). Previous observational studies have reported the significant positive association of HT with TIMT, plaque, and AS in carotid arteries (3, 23–25). Then we uniquely assessed these in the femoral artery, which was underdiagnosed. HT was positively associated with femoral plaque as previously reported (19, 26). Furthermore, a population-based cohort also reported the effect of elevated BP on hospitalized peripheral artery disease risk (27). Results from our study in the Chinese population provided supportive evidence regarding the role of HT on AS. In addition, we found that the risks of carotid or femoral TIMT, plaque, and AS were comparable between normotension and PreHT. Then a heatmap of ORs for AS risk in different SBP and DBP levels suggests there might be a complex interaction between SBP and DBP on AS prevalence. Thus, we inferred that an index combining SBP and DBP may provide more information on the role of blood pressure on AS.
SBP is mainly determined by cardiac output and proximal arterial capacity, while DBP is more likely to be affected by peripheral vascular volume and resistance (28, 29). Major arteries can store part of the stroke volume during systolic ejection, and drain this volume during diastole, which could ensure continuous perfusion of organs and tissues (30). A study on ambulatory BP monitoring (ABPM) assessment showed that SDR had a similar number to the “gold ratio" (31) with a value of 1.62 (32). In the present study, the mean of SDR was 1.59 ± 0.17, also around the “gold ratio”. The SDR was significantly, positively correlated to SBP with a coefficient of 0.515, and negatively to DBP but with a much lower coefficient (−0.197). Then we found that high tertile of SDR was significantly, and positively associated with TIMT, plaque, and AS risk in the carotid artery and carotid and/or femoral artery, but only AS in the femoral artery. In RCS analysis, a significant linear trend between SDR and HT was observed, and an SDR < 1.57 shared a relatively lower risk than those higher SDR. Given the effect of HT on AS, we regrouped all participants according to the tertiles of SDR and HT or not. It is noteworthy that increased risks for TIMT, plaque, and AS in the carotid artery and carotid and/or femoral artery were also observed in the high-SDR group in the absence of HT, indicating high-SDR may be a risk factor for AS independent of HT.
SDR is a readily obtainable index, and our study first provided epidemiological evidence regarding the association between SDR and AS in carotid and femoral arteries. But the results should be interpreted with caution since the limitations were inevitable. First, although multiple statistical analyses and sensitivity analyses were used to confirm the association between SDR and AS, our cross-sectional design and sample size still limited the temporal interpretation or casual interference, thus further validation in populations with larger sample-sized longitudinal cohort studies is needed. Second, considering the variation of BP in different situations, BP readings in two or more days were recommended in HT diagnosis and BP evaluation in 2017 ACC/AHA guidelines (33). In the current study, two BP measurements in a single visit were conducted, which may lead to some false diagnoses of HT and BP evaluation. Third, the misclassification of TIMT, plaque, and AS could not be avoided due to the ultrasound subjective judgment of examiners. However, a total of five vascular surgeons with 3–5 years of clinical experience from the same department were trained to conduct all measurements, which we believe could increase the accuracy of AS measurement and reduce the probability of biased association as much as possible. However, residual bias from some other factors cannot be totally excluded, such as diet, physical activity, and so on.
AS is prevalent in middle-aged adults, with a prevalence of 30.0% in our current study population in southeastern China, and femoral AS consists of an important part of AS burden. SDR is linearly associated with the risk of AS, which is stronger in the carotid artery than in the femoral artery. These findings suggest that SDR can provide additional predictive value for AS, independent of hypertension.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
The studies involving humans were approved by the Ethics Committee of Fujian Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
YW: Writing – original draft, Investigation, Formal Analysis, Conceptualization. CC: Writing – original draft, Investigation. QL: Writing – original draft, Investigation. QS: Writing – original draft, Investigation. YD: Writing – original draft, Investigation. HC: Writing – original draft, Investigation. TH: Writing – original draft, Investigation. XL: Writing – original draft, Investigation. RF: Writing – original draft, Data curation. WH: Writing – original draft, Methodology. ZH: Writing – original draft, Funding acquisition. JC: Writing – original draft, Funding acquisition. SD: Writing – original draft, Supervision, Methodology, Data curation, Conceptualization. PG: Writing – original draft, Supervision, Investigation. WY: Writing – review & editing, Writing – original draft, Supervision, Resources, Project administration, Funding acquisition, Conceptualization.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article.
This study was jointly supported by the Ministry of Science and Technology of the People’s Republic of China [grant number: 2017YFC0907102], the Government of Fuqing City [grant number: 2019B003], Special funds of Fujian Provincial Finance Department (No. 2020czbz01), and High-level Talents Research Start-up Project of Fujian Medical University (No. XRCZX2017035, No. XRCZX2020034 and XRCZX2022001). The funders had no role in study design, data collection, and interpretation, or the decision to submit the work for publication.
The research team would like to thank the participants, interviewers, nurses of the Fuqing cohort study, and local government officers, doctors, and other healthcare professionals, who all have been providing generous support for the day-to-day research fieldwork operation.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2024.1353945/full#supplementary-material
1. Aday AW, Matsushita K. Epidemiology of peripheral artery disease and polyvascular disease. Circ Res. (2021) 128:1818–32. doi: 10.1161/CIRCRESAHA.121.318535
2. Criqui MH, Matsushita K, Aboyans V, Hess CN, Hicks CW, Kwan TW, et al. Lower extremity peripheral artery disease: contemporary epidemiology, management gaps, and future directions: a scientific statement from the American heart association. Circulation. (2021) 144:e171–91. doi: 10.1161/CIR.0000000000001005
3. Song P, Fang Z, Wang H, Cai Y, Rahimi K, Zhu Y, et al. Global and regional prevalence, burden, and risk factors for carotid atherosclerosis: a systematic review, meta-analysis, and modelling study. Lancet Glob Health. (2020) 8:e721–9. doi: 10.1016/S2214-109X(20)30117-0
4. Libby P. The changing landscape of atherosclerosis. Nature. (2021) 592:524–33. doi: 10.1038/s41586-021-03392-8
5. Wan EYF, Fung WT, Schooling CM, Au Yeung SL, Kwok MK, Yu EYT, et al. Blood pressure and risk of cardiovascular disease in UK biobank: a Mendelian randomization study. Hypertension. (2021) 77:367–75. doi: 10.1161/HYPERTENSIONAHA.120.16138
6. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet (London, England). (2002) 360:1903–13. doi: 10.1016/S0140-6736(02)11911-8
7. Jung MH, Yi SW, An SJ, Yi JJ. Age-specific associations between systolic blood pressure and cardiovascular mortality. Heart (British Cardiac Society). (2019) 105:1070–7. doi: 10.1136/heartjnl-2019-314697
8. Sudano I, Osto E, Ruschitzka F. Blood pressure-lowering therapy. Handb Exp Pharmacol. (2022) 270:25–45. doi: 10.1007/164_2020_372
9. Gibson CM, Gibson WJ, Murphy SA, Marble SJ, McCabe CH, Turakhia MP, et al. Association of the fibonacci cascade with the distribution of coronary artery lesions responsible for st-segment elevation myocardial infarction. Am J Cardiol. (2003) 92:595–7. doi: 10.1016/S0002-9149(03)00731-8
10. Yetkin E, Topbaş U, Yanik A, Yetkin G. Does systolic and diastolic blood pressure follow golden ratio? Int J Cardiol. (2014) 176:1457–9. doi: 10.1016/j.ijcard.2014.08.065
11. Su Q, Chen H, Du S, Dai Y, Chen C, He T, et al. Association between serum bilirubin, lipid levels, and prevalence of femoral and carotid atherosclerosis: a population-based cross-sectional study. Arterioscler, Thromb, Vasc Biol. (2023) 43:136–45. doi: 10.1161/ATVBAHA.122.318086
12. Feng R, Dai Y, Du S, Liang W, Chen H, Chen C, et al. Leukocyte and platelet related inflammatory indicators and risk of carotid and femoral plaques: a population-based cross-sectional study in southeast China. Angiology. (2022) 75:79–89. doi: 10.1177/00033197221129723
13. Su W, Chen M, Xiao L, Du S, Xue L, Feng R, et al. Association of metabolic dysfunction-associated fatty liver disease, type 2 diabetes mellitus, and metabolic goal achievement with risk of chronic kidney disease. Front Public Health. (2022) 10:1047794. doi: 10.3389/fpubh.2022.1047794
14. Huang W, Feng R, Xu X, Ma M, Chen J, Wang J, et al. Loss of anthropometry-lipids relationship in obese adults: a cross-sectional study in Southern China. Clin Epidemiol. (2023) 15:191–201. doi: 10.2147/CLEP.S400150
15. Zhou BF. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults–study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomedical and Environmental Sciences: BES. (2002) 15:83–96. 12046553.12046553
16. Wang X, Li W, Song F, Wang L, Fu Q, Cao S, et al. Carotid atherosclerosis detected by ultrasonography: a national cross-sectional study. J Am Heart Assoc. (2018) 7:e008701. doi: 10.1161/JAHA.118.008701
17. Usman A, Ribatti D, Sadat U, Gillard JH. From lipid retention to immune-mediate inflammation and associated angiogenesis in the pathogenesis of atherosclerosis. J Atheroscler Thromb. (2015) 22:739–49. doi: 10.5551/jat.30460
18. Xie W, Wu Y, Wang W, Zhao D, Liang L, Wang M, et al. A longitudinal study of carotid plaque and risk of ischemic cardiovascular disease in the Chinese population. J Am Soc Echocardiogr. (2011) 24:729–37. doi: 10.1016/j.echo.2011.02.011
19. Laclaustra M, Casasnovas JA, Fernandez-Ortiz A, Fuster V, Leon-Latre M, Jimenez-Borreguero LJ, et al. Femoral and carotid subclinical atherosclerosis association with risk factors and coronary calcium: the AWHS study. J Am Coll Cardiol. (2016) 67:1263–74. doi: 10.1016/j.jacc.2015.12.056
20. Chaubey S, Nitsch D, Altmann D, Ebrahim S. Differing effect of modifiable cardiovascular risk factors on intima-media thickening and plaque formation at different sites of the arterial vasculature. Heart. (2010) 96:1579–85. doi: 10.1136/hrt.2009.188219
21. Lopez-Melgar B, Fernandez-Friera L, Oliva B, Garcia-Ruiz JM, Penalvo JL, Gomez-Talavera S, et al. Subclinical atherosclerosis burden by 3D ultrasound in mid-life: the PESA study. J Am Coll Cardiol. (2017) 70:301–13. doi: 10.1016/j.jacc.2017.05.033
22. Libby P, Buring JE, Badimon L, Hansson GK, Deanfield J, Bittencourt MS, et al. Atherosclerosis. Nat Rev Dis Primers. (2019) 5:56. doi: 10.1038/s41572-019-0106-z
23. Lu SX, Wu TW, Chou CL, Cheng CF, Wang LY. Combined effects of hypertension, hyperlipidemia, and diabetes mellitus on the presence and severity of carotid atherosclerosis in community-dwelling elders: a community-based study. J Chin Med Assoc. (2023) 86:220–6. doi: 10.1097/JCMA.0000000000000839
24. Mancusi C, Manzi MV, de Simone G, Morisco C, Lembo M, Pilato E, et al. Carotid atherosclerosis predicts blood pressure control in patients with hypertension: the campania salute network registry. J Am Heart Assoc. (2022) 11:e022345. doi: 10.1161/JAHA.121.022345
25. Song P, Xia W, Zhu Y, Wang M, Chang X, Jin S, et al. Prevalence of carotid atherosclerosis and carotid plaque in Chinese adults: a systematic review and meta-regression analysis. Atherosclerosis. (2018) 276:67–73. doi: 10.1016/j.atherosclerosis.2018.07.020
26. Noflatscher M, Schreinlechner M, Sommer P, Kerschbaum J, Berggren K, Theurl M, et al. Influence of traditional cardiovascular risk factors on carotid and femoral atherosclerotic plaque volume as measured by three-dimensional ultrasound. J Clin Med. (2019) 8(1):32. doi: 10.3390/jcm8010032
27. Lu Y, Ballew SH, Tanaka H, Szklo M, Heiss G, Coresh J, et al. 2017 ACC/AHA blood pressure classification and incident peripheral artery disease: the atherosclerosis risk in communities (ARIC) study. Eur J Prev Cardiol. (2020) 27:51–9. doi: 10.1177/2047487319865378
28. Romano SM, Pistolesi M. Assessment of cardiac output from systemic arterial pressure in humans. Crit Care Med. (2002) 30:1834–41. doi: 10.1097/00003246-200208000-00027
29. McEniery CM, Yasmin Wallace S, Maki-Petaja K, McDonnell B, Sharman JE, et al. Increased stroke volume and aortic stiffness contribute to isolated systolic hypertension in young adults. Hypertension. (2005) 46:221–6 doi: 10.1161/01.HYP.0000165310.84801.e0
30. Safar ME. Systolic blood pressure, pulse pressure and arterial stiffness as cardiovascular risk factors. Curr Opin Nephrol Hypertens. (2001) 10:257–61. doi: 10.1097/00041552-200103000-00015
31. Yetkin G, Sivri N, Yalta K, Yetkin E. Golden ratio is beating in our heart. Int J Cardiol. (2013) 168:4926–7. doi: 10.1016/j.ijcard.2013.07.090
32. Henein MY, Zhao Y, Nicoll R, Sun L, Khir AW, Franklin K, et al. The human heart: application of the golden ratio and angle. Int J Cardiol. (2011) 150:239–42. doi: 10.1016/j.ijcard.2011.05.094
33. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APHA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. Hypertension. (2018) 71:e13–e115. doi: 10.1161/HYP.0000000000000065
Keywords: SDR, carotid, femoral, atherosclerosis, hypertension
Citation: Wang Y, Chen C, Lin Q, Su Q, Dai Y, Chen H, He T, Li X, Feng R, Huang W, Hu Z, Chen J, Du S, Guo P and Ye W (2024) The ratio of systolic and diastolic pressure is associated with carotid and femoral atherosclerosis. Front. Cardiovasc. Med. 11:1353945. doi: 10.3389/fcvm.2024.1353945
Received: 11 December 2023; Accepted: 21 February 2024;
Published: 8 March 2024.
Edited by:
José Tuñón, University Hospital Fundación Jiménez Díaz, SpainReviewed by:
Liying Xing, CDC of Liaoning Province, China© 2024 Wang, Chen, Lin, Su, Dai, Chen, He, Li, Feng, Huang, Hu, Chen, Du, Guo and Ye. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shanshan Du ZHVzaGFuc2hhbjEwMDdAMTYzLmNvbQ== Pingfan Guo Zmp4Z2d1b0AxMjYuY29t Weimin Ye eXdtQGZqbXUuZWR1LmNu
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.