- 1Guang’anmen Hospital, Chinese Academy of Chinese Medical Sciences, Beijing, China
- 2Guang'anmen Hospital, Beijing University of Chinese Medicine, Beijing, China
Objective: It is advised that patients engage in physical activity to enhance their quality of life and achieve better results. The purpose of the current study was to measure the efficacy of exercise on the physical ability, cardiac function and cardiopulmonary fitness of patients with AF.
Method: A comprehensive systematic literature search was performed in PubMed, Embase, and Web of Science from 1991 to 2023 for RCTs comparing physical exercise combined with AF routine treatments to routine treatments alone. The meta-analysis was conducted following PRISMA guidelines. Our main outcomes were physical ability (measured by the 6-min walk test, 6MWT), cardiac function (measured by left ventricular ejection fraction, LVEF) and cardiopulmonary fitness (measured by peak oxygen uptake and resting heart rate). Quality assessments were conducted using the Cochrane Collaboration tool.
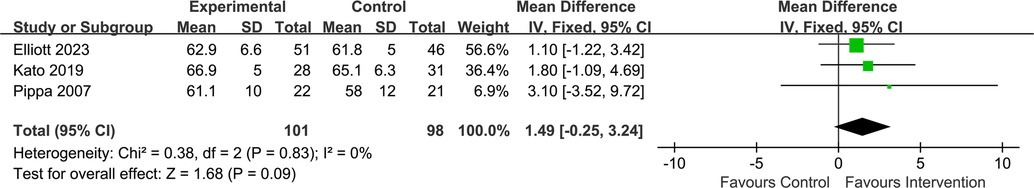
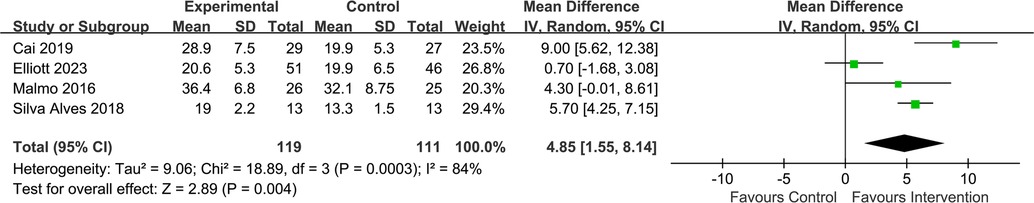
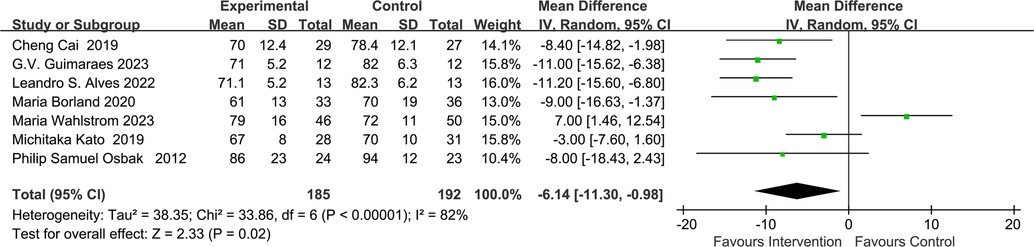
Results: Thirteen trials involving 672 patients met the criteria for analysis. The results showed that physical exercise increased physical ability by improving the 6MWT (m) performance (MD = 96.99, 95% CI: 25.55–168.43; Z = 2.66; p = 0.008); and enhanced peak VO2 (ml/kg per min) (MD = 4.85, 95% CI: 1.55–8.14; Z = 2.89; p = 0.004) while reducing resting heart rate (beats per minute, bpm) (MD = −6.14, 95% CI: −11.30 to −0.98; Z = 2.33; p = 0.02). However, the results showed that regular exercise could improve LVEF (%) inpatients clinically, which had no statistic difference between experimental and control group (MD = 1.49, 95% CI: −0.25–3.24; Z = 1.68; p = 0.09).
Conclusion: Our meta-analysis shows that physical exercise is an effective intervention to improve the exercise ability and cardiopulmonary fitness for AF patients. Meanwhile, we also do not exclude the positive effect of exercise on the improvement of cardiac function (LVEF) in patients with AF. To this end, doctors should consider the positive impact of exercise on patients and give advice on exercise limits in practical clinical practice.
Introduction
The most prevalent prolonged heart arrhythmia, atrial fibrillation (AF), is linked to significant morbidity, mortality, and healthcare utilization (1). The incidence and prevalence of atrial fibrillation (AF) have reached the level of a cardiovascular disease (CVD) epidemic in the twenty-first century due to rising average worldwide life expectancy and extended survival with chronic diseases (2). Preventing atrial fibrillation (AF) and its associated consequences remains problematic despite extensive research efforts (3). The aging of our population and the rise in obesity are two factors that are strongly linked to and may even be the cause of AF, and they may be contributing to its incidence. Modifiable cardiovascular risk factors, including obesity, hypertension (HTN), diabetes mellitus, obstructive sleep apnea (OSA), alcohol consumption, smoking, and sedentary lifestyles, have been proposed as possible contributors to the development and progression of AF (4). Significant decreases in the burden of AF were observed with effective weight loss and enhanced physical activity (1).
As a result, studying the connection between exercise and AF is a highly worthwhile endeavor. Physical exercise can effectively assist in the therapy of various types of cardiovascular diseases, and the potential benefits of moderate regular physical exercise in reducing the risk of AF are considerable (5). Several studies show that regular physical activity positively benefits AF prevention (3). Participation in an exercise-based intervention over 6 months reduced arrhythmia recurrence and improved symptom severity among patients with AF (6). Research has demonstrated that consistent physical activity has an inverse and independent relationship with the advancement of clinical AF (7). We aim to see if exercise can help atrial fibrillation patients live longer and have better prognoses.
Fewer types of AF patients were included in the study (8, 9), and the effect of exercise on cardiac function in patients with AF is unclear despite previous meta-analyses in this area. After searching relevant experiments, we found some controversy about whether exercise can improve the LVEF in patients with atrial fibrillation. While some randomized trials (10) found that exercise enhanced left cardiac function, others (6, 11) found no significant changes. Thus, we gathered these data for analysis. We also need to revise the results in light of the new study reports.
Thus, this meta-analysis aims to investigate areas that remain unclear and update the existing findings. Our responsibility is to clarify how exercise affects an AF patient's physical capacity, heart function, and cardiopulmonary fitness. Furthermore, we broadened the scope of the research participants to provide a more thorough framework for the clinic.
Methods
This present meta-analysis was conducted following by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The data used in this study are all secondary and do not require ethical approval.
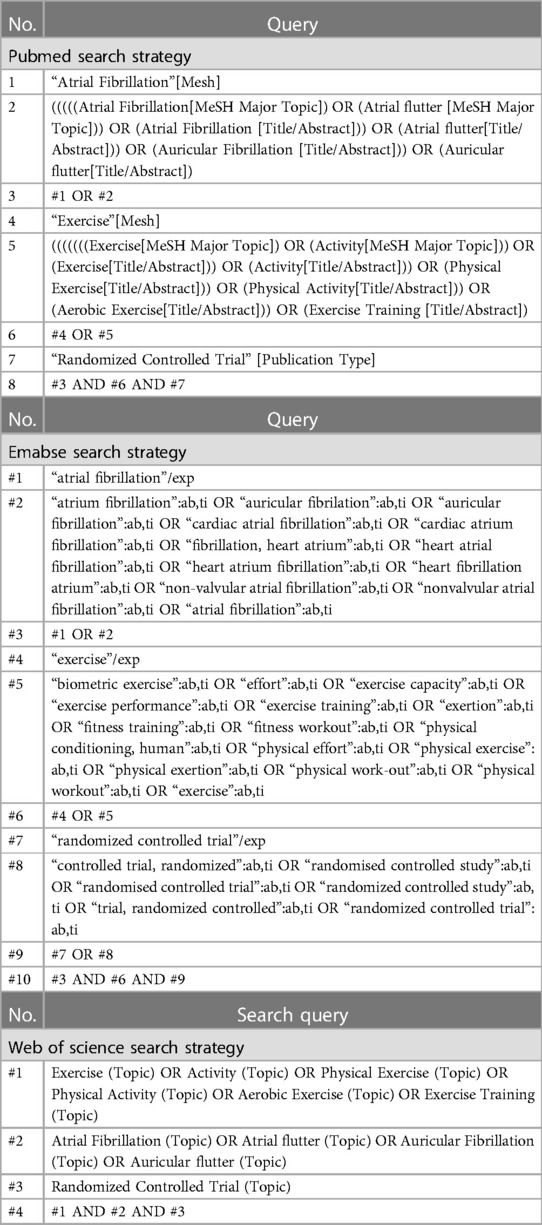
Search strategy
A systematic literature search was conducted in five electronic databases, including PubMed, Embase and Web of Science from 1991 to 2023 for RCTs studying the effects of physical exercise on the physical ability, cardiac function and cardiopulmonary fitness of patients with AF. Keywords and their medical subject headings (MeSH) or Embase subject headings (EMTREE) were used for the search strategy. Table 1 shows the details of the search strategy.
Inclusion criteria
Eligible studies were identified if they met all the following criteria:
(1) Population: adults with AF (aged 18 and over with no upper age limit), including paroxysmal AF patients, persistent AF patients, permanent AF patients, chronic AF (a longstanding chaotic and irregular atrial arrhythmia) patients, patients with atrial fibrillation who underwent the radiofrequency ablation and permanent AF in HF patients.
(2) Intervention: studies reporting the effects of physical ability, cardiac function and cardiopulmonary fitness of AF patients.
(3) Comparison: treatment as usual or daily exercise (not participated in any organized sports programs).
(4) Outcome(s): physical ability measured by the 6MWT, cardiac function measured by LVEF and cardiopulmonary fitness measured by peak oxygen uptake (peak VO2) and resting heart rate.
(5) Study type: RCT.
Exclusion criteria
(1) Animal studies, case reports, reviews, abstracts, conference proceedings and editorials.
(2) Non-RCTs.
(3) Studies without sufficient data to calculate WMD.
Data extraction
WPS Office was used to set up the data extraction table. The main components of the extracted information were classified as:
(1) Publication information: first author and publication year.
(2) General characteristics of patients: sample size, gender and age.
(3) Details of intervention and control therapy: training period, session duration, training mode and number of sessions per week.
(4) Details of outcomes.
(5) Bias risk assessment information: quality of included studies.
Statistical analyses
Review Manager 5.4 was used for all statistical analyses. We used the WMD with the corresponding 95% confidence intervals (CI) as the effect size (ES). If the data (including the sample size, mean value and standard deviation) extracted from the RCTs met the needs of the analyses, the analyses were conducted directly (12). If the data (including the standard error, 95% CI or p-values) in the RCTs could not be used now for analyses, they were analyzed after data conversion (13–15). Cochran's Q-test and I2 test were used to evaluate heterogeneity. A p-value <0.1 or I2 value >50% indicated significant heterogeneity between RCTs, and the random-effect model was used. Otherwise, a fixed-effect model was used.
Assessment of the risk of bias
The Cochrane Collaboration tool was used to assess the risk of bias. Two authors independently extracted data and assessed the quality of the included studies. The data were recorded on a special data form. The differences between data extraction and quality evaluation were determined through discussion.
Results
Search results
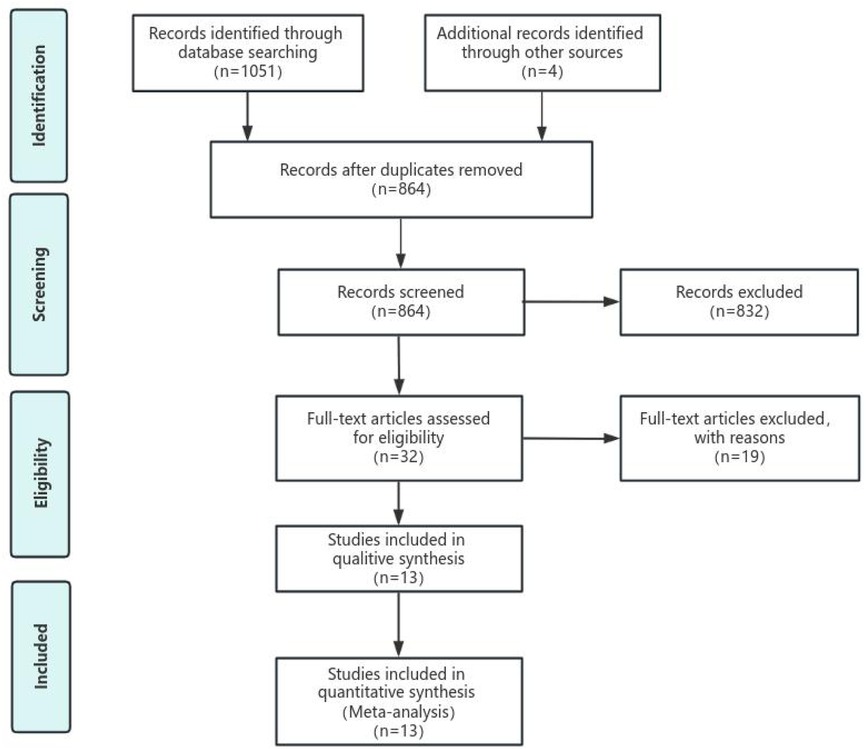
Initially, 1,070 potential studies were retrieved. After deleting duplicates, 864 studies were screened. After scanning the titles and abstracts, the inconsistencies were eliminated, and 32 papers remained. After carefully reading the full text using pre-established inclusion and exclusion criteria, 19 articles were excluded, and the remaining 13 were included in the meta-analysis. The flow chart of the search process is shown in Figure 1. The bias condition of selected studies is shown in Figures 2A,B.
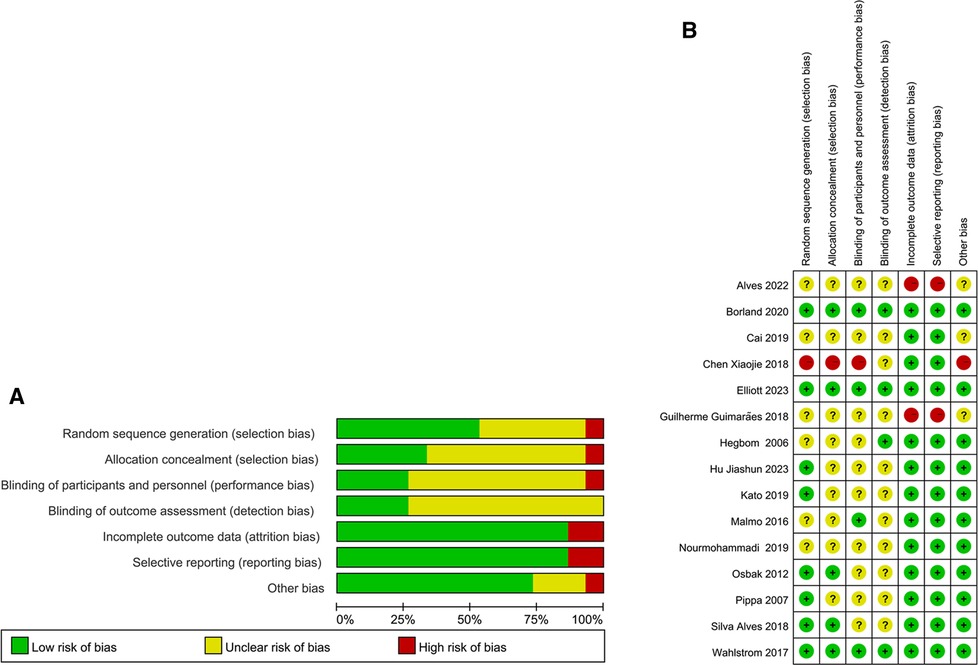
Figure 2. (A) The risk of bias. A review of the authors’ judgments about each risk of bias items are presented as percentages across all of the included studies. The quality of the selected is assessed according to the Cochrane criteria. (B) The risk of bias summary. A review of the authors’ judgments about the risk of bias are included in each study.
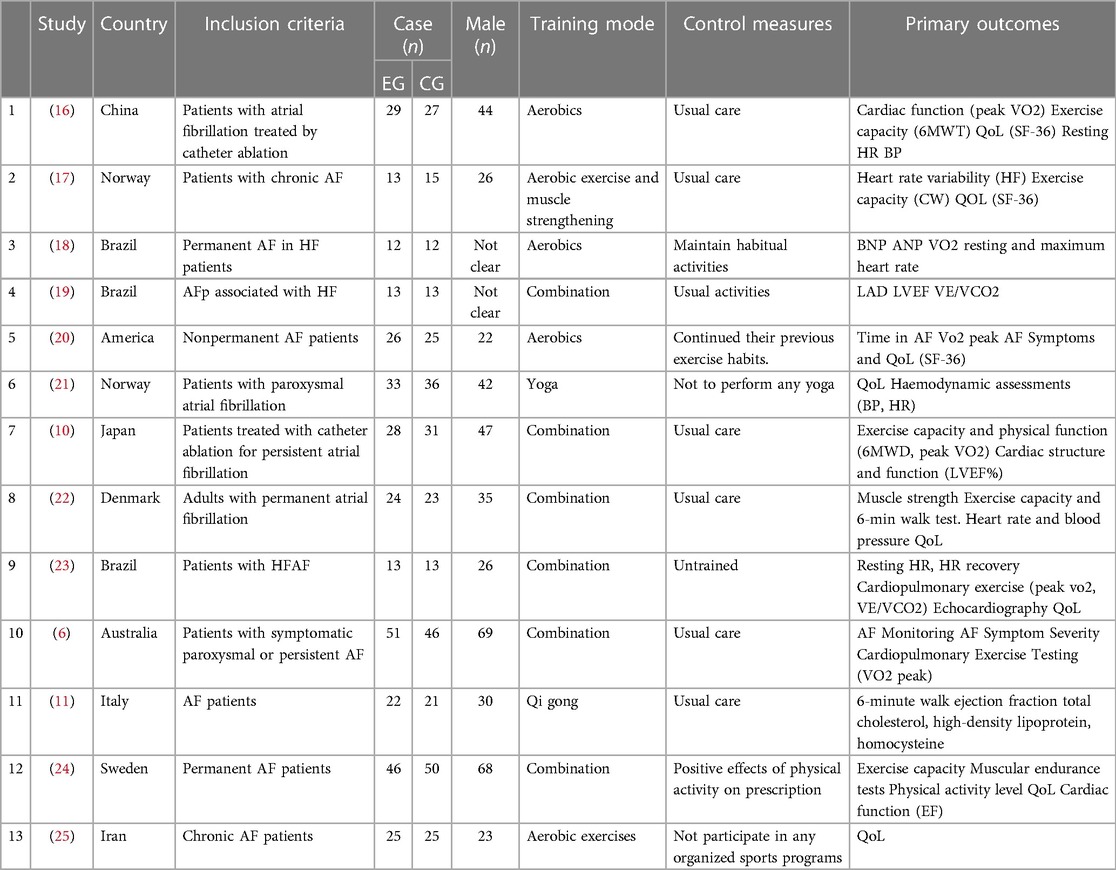
Trial and patient characteristics
The 13 RCTs included 672 patients (335 allocated to experimental groups and 337 allocated to control groups). Four RCT exercise interventions were aerobic, six were aerobic combined with anaerobic, one was Qigong and one was Yoga. The details of all included studies are shown in Table 2.
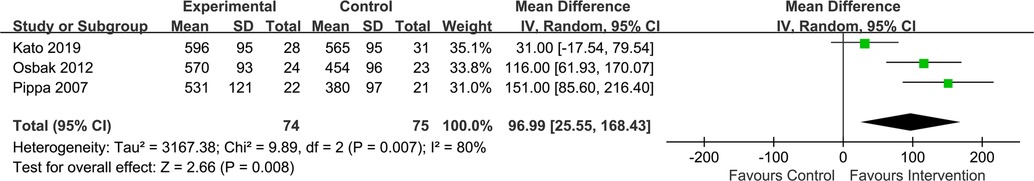
Effects of physical exercise on exercise ability in patients with AF
The effect of physical exercise on exercise ability was measured by the 6MWT. Three RCTs (10, 11, 22) reported the results of 6MWTs, which had statistic difference between experimental and control group (MD = 96.99, 95% CI: 25.55–168.43; Z = 2.66; p = 0.008) (Figure 3).
Effects of physical exercise on cardiac function in patients with AF
The effect of physical exercise on cardiac function was measured by LVEF. Three RCTs (6, 10, 11) reported the results of LVEF, which had no statistic difference between experimental and control group (MD = 1.49, 95% CI: −0.25–3.24; Z = 1.68; p = 0.09) (Figure 4).
Effects of physical exercise on cardiopulmonary fitness in patients with AF
The effect of physical exercise on cardiopulmonary fitness was measured by the peak VO2 and resting heart rate. Four RCTs (6, 16, 20, 23) reported peak VO2 values, which had statistical differences between the experimental and control groups (MD = 4.85, 95% CI: 1.55–8.14; Z = 2.89; p = 0.004) (Figure 5). Seven RCTs (10, 16, 18, 21–24) reported resting heart rates, which had statistic difference between experimental and control group (MD = −6.14, 95% CI: −11.30 to −0.98; Z = 2.33; p = 0.02) (Figure 6).
Publication bias
Review Manager 5.4 was used to draw the funnel plots to analyze the data related to the individual outcome indicators. From the figure, the publication bias of each group is not apparent, and the figure roughly shows the symmetry of the centreline concentrated in the upper part (Figure 7).
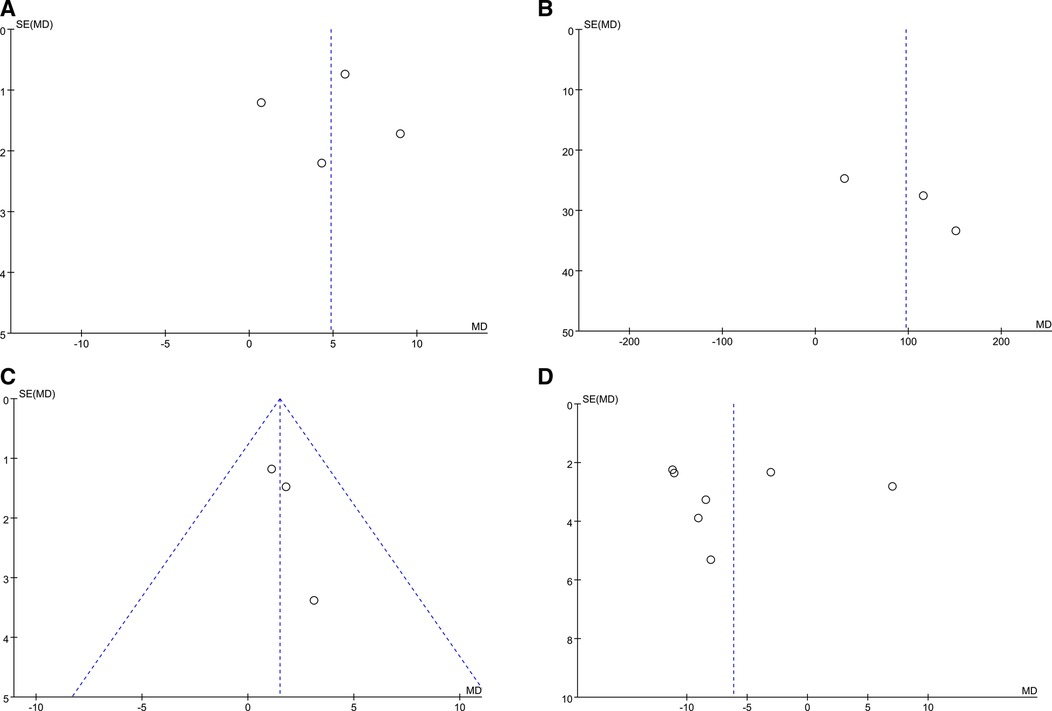
Figure 7. Funnel plots shows the publication bias of physical exercise on peak vo2 (A), 6MWT (B), LVEF (C), resting HR (D) in AF patients.
Discussion
From all the results above, we found that physical exercise positively affected the exercise ability and cardiopulmonary fitness in patients with AF. Statistics did not indicate the difference between exercise and the control group of cardiac function.
Compared with the previous analysis (8, 9), our study included more types of patients with AF, such as patients with AF after radiofrequency ablation and patients with heart failure with AF (10, 16, 18, 19, 23). The reason why we do so is mainly to consider that the clinical condition of some AF patients is more complex. Therefore, we included as many patients with various types of AF as possible. This has important implications for our patient education in the clinic. Secondly, we focused on the efficacy of exercise on the physical ability, cardiac function and cardiopulmonary fitness of patients with AF. What we included more than the previous meta was the outcome “LVEF”, which helped to respond to the controversy about the aspect. This reminded us that we could pay attention to the LVEF of AF patients during exercise. In addition, our study was an updated analysis, including statistics according to inclusion criteria from 1991 to 2023. We are committed to presenting the latest research results to readers to guide clinical and life better.
There were similar reports in the previous analysis for the results of improvement on 6MWT and peak VO2 (8, 9). This suggests that we could improve patients' physical quality and exercise ability with AF through effective and appropriate exercise methods. There appeared to be no differences in outcomes between exercise at high and lower intensity (26).
Resting heart rate is a relatively simple and direct indicator of understanding heart function. The decrease in resting heart rate after exercise intervention also suggests that exercise benefits cardio respiratory fitness in patients with AF. At the same time, resting heart rate is often used to measure the patient's exercise limit (70%–90% of maximal heart rate usually), which is very beneficial for clinical patient exercise monitoring (17).
We were skeptical about whether exercise could improve the ejection fraction in patients with AF. Even if the results of our analysis showed no statistically significant difference between the two groups, we could believe that exercise in patients with AF is clinically significant. After all, several studies have shown that patients' ejection fraction increases significantly after exercise (6, 10, 11). The number of sample sizes and the study subjects' baseline characteristics were considered relevant factors. We hope that more studies will be done to support the relationship between exercise and ejection fraction in patients with AF.
As for the exercise duration, the 2018 Physical Activity Guidelines Advisory Committee Report recommends 150 min/per week of moderate-intensity or 75 min/per week of vigorous-intensity aerobic exercise for all adults because this exercise volume improves cardiovascular health (1). American Heart Association recommends moderate-intensity aerobic exercise for about 60 min every day for several months to reduce the risk of cardiovascular disease (8). Most importantly, this higher risk of AF has been observed only with exercise doses that far exceed recommendations of the Physical Activity Guidelines Advisory Committee Report and are therefore achieved by only <1% of Americans (1). But in real life, only a subset of patients can achieve the above standards due to the differences in personal physical quality or other reasons. We recommend that patients choose exercise limitation based on the degree of physical fatigue, which is consistent with our clinical patient education.
Strengths and limitations
We believe this is the latest analysis of AF patients exercise, which has a broad range population, including paroxysmal AF patients, permanent AF patients, chronic AF patients, patients with atrial fibrillation who underwent radiofrequency ablation, and permanent AF in HF patients. At the same time, we conducted statistical analysis for previous studies with inconsistent results on LVEF to guide clinical practice better. However, we recognize that there are some limitations to this study. First, the large number of types of patients with AF may lead to differences between different populations. Second, the small sample size in multiple studies may make the results less representative. Otherwise, individual studies have differences in baseline patient characteristics, which may affect the final study results. Thirdly, our study did not focus on the effect of exercise on AF recurrence, which also plays an essential role in clinical guidance. In the future, we expect to collect more studies with larger sample sizes for analysis and group them according to different baseline characteristics. And we hope that more researchers will work to study the effects of exercise on the recurrence of AF.
Conclusions
Our meta-analysis shows that physical exercise is an effective intervention to improve AF patients' exercise ability and cardiopulmonary fitness. Meanwhile, we also do not exclude exercise's positive effect on improving cardiac function (LVEF) in patients with AF. To this end, doctors should consider the positive impact of exercise on patients and advise on exercise limits in practical clinical practice. We should continue to expand the accumulation amount of related studies in the future to help patients with different types of AF better.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
CY: Data curation, Methodology, Writing – original draft, Writing – review & editing. QW: Data curation, Methodology, Writing – review & editing. QL: Formal Analysis, Methodology, Writing – review & editing. XH: Supervision, Writing – review & editing. XY: Data curation, Methodology, Writing – original draft. YY: Data curation, Methodology, Writing – original draft. LL: Formal Analysis, Investigation, Writing – original draft. WZ: Formal Analysis, Writing – original draft. SW: Supervision, Writing – review & editing.
Funding
The authors declare financial support was received for the research, authorship, and/or publication of this article.
This research was supported by Beijing Municipal Natural Science Foundation (grant no. 7232311), Chinese Academy of Traditional Chinese Medicine's Major Tackling Project of Science and Technology Innovation ((grant no. CI2021A00921) and National Natural Science Foundation of China (grant no. 82374421).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2024.1352643/full#supplementary-material
References
1. Chung MK, Eckhardt LL, Chen LY, Ahmed HM, Gopinathannair R, Joglar JA. Lifestyle and risk factor modification for reduction of atrial fibrillation: a scientific statement from the American heart association. Circulation. (2020) 141(16):e750–72. doi: 10.1161/cir.0000000000000748
2. Mensah GA, Fuster V, Murray CJL, Roth GA, Mensah GA, Abate YH, et al. Global burden of cardiovascular diseases and risks, 1990–2022. J Am Coll Cardiol. (2023) 82(25):2350–473. doi: 10.1016/j.jacc.2023.11.007
3. Kornej J, Börschel CS, Benjamin EJ, Schnabel RB. Epidemiology of atrial fibrillation in the 21st century. Circ Res. (2020) 127(1):4–20. doi: 10.1161/circresaha.120.316340
4. Shamloo AS, Dagres N, Arya A, Hindricks G. Atrial fibrillation: a review of modifiable risk factors and preventive strategies. Rom J Intern Med. (2019) 57(2):99–109. doi: 10.2478/rjim-2018-0045
5. Eckel RH, Jakicic JM, Ard JD, De Jesus JM, Houston Miller N, Hubbard VS, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American college of cardiology/American heart association task force on practice guidelines. Circulation. (2014) 129:S76–99. doi: 10.1161/01.cir.0000437740.48606.d1
6. Elliott AD, Verdicchio CV, Mahajan R, Middeldorp ME, Gallagher C, Mishima RS. An exercise and physical activity program in patients with atrial fibrillation: the ACTIVE-AF randomized controlled trial. JACC Clin Electrophysiol. (2023a) 9(4):455–65. doi: 10.1016/j.jacep.2022.12.002
7. Blum S, Aeschbacher S, Meyre P, Zwimpfer L, Reichlin T, Beer JH, et al. Incidence and predictors of atrial fibrillation progression. J Am Heart Assoc. (2019) 8(20):e012554. doi: 10.1161/jaha.119.012554
8. Shi S, Shi J, Jia Q, Shi S, Yuan G, Hu Y. Efficacy of physical exercise on the quality of life, exercise ability, and cardiopulmonary fitness of patients with atrial fibrillation: a systematic review and meta-analysis. Front Physiol. (2020) 11:740. doi: 10.3389/fphys.2020.00740
9. Zhang Y, Ren P, Tang A-L, Li D, Hu X, Wang H, et al. Efficacy of exercise rehabilitation in patients with atrial fibrillation after radiofrequency ablation: a meta-analysis of randomized controlled trials. Evidence-Based Complementary Altern Med. (2022) 2022:1–10. doi: 10.1155/2022/9714252
10. Kato M, Ogano M, Mori Y, Kochi K, Morimoto D, Kito K, et al. Exercise-based cardiac rehabilitation for patients with catheter ablation for persistent atrial fibrillation: a randomized controlled clinical trial. Eur J Prev Cardiol. (2019) 26(18):1931–40. doi: 10.1177/2047487319859974
11. Pippa L, Manzoli L, Corti I, Congedo G, Romanazzi L, Parruti G. Functional capacity after traditional Chinese medicine (Qi Gong) training in patients with chronic atrial fibrillation: a randomized controlled trial. Prev Cardiol. (2007) 10(1):22–5. doi: 10.1111/j.1520-037x.2007.05721.x
12. Higgins JP, Green S, Collaboration TC. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.0.0 (Hoboken, NJ: The Cochrane Collaboration). Available online at: www.cochrane-handbook.org (2008a).
13. Higgins JP, White IR, Anzures-Cabrera J. Meta-analysis of skewed data: combining results reported on log-transformed or raw scales. Stat Med. (2008b) 27:6072–92. doi: 10.1002/sim.3427
14. Morris SB. Estimating effect sizes from pretest-posttest control group designs. Organ Res Methods. (2008) 11:364–86. doi: 10.1177/1094428106291059
15. Guilera G, Gómez-Benito J, Hidalgo MD, Sánchez-Meca J. Type I error and statistical power of the Mantel-Haenszel procedure for detecting DIF: a meta-analysis. Psychol Methods. (2013) 18:553–71. doi: 10.1037/a0034306
16. Cai C, Yang G, Bao Z, Zhang F, Ju W, Chen H. Home-based cardiac rehabilitation versus conventional care for patients with atrial fibrillation treated with catheter ablation: a randomized controlled trial. J Arrhythm. (2019) 35(S1):95–6. doi: 10.1002/joa3.12267
17. Hegbom F, Sire S, Heldal M, Orning OM, Stavem K, Gjesdal K. Short-term exercise training in patients with chronic atrial fibrillation. J Cardiopulm Rehabil. (2006) 26(1):24–9. doi: 10.1097/00008483-200601000-00005
18. Guimarães G, Alves LS, Sarà M, Chizzola PR, Castro RE, Bocchi EA. P6236 permanent atrial fibrillation in heart failure: impact of exercise training on biomarkers. A randomized controlled trial. Eur Heart J. (2018) 39(suppl_1):ehy566–P6236. doi: 10.1093/eurheartj/ehy566.p6236
19. Alves LS, Bocchi EA, Chizzola PR, Castro RE, Salemi VMC, de Melo MDT, et al. Exercise training in heart failure with reduced ejection fraction and permanent atrial fibrillation: a randomized clinical trial. Heart Rhythm. (2022) 19(7):1058–66. doi: 10.1016/j.hrthm.2022.03.1217
20. Malmo V, Nes BM, Amundsen BH, Tjonna A-E, Stoylen A, Rossvoll O, et al. Aerobic interval training reduces the burden of atrial fibrillation in the short term. Circulation. (2016) 133(5):466–73. doi: 10.1161/circulationaha.115.018220
21. Wahlstrom M, Rydell Karlsson M, Medin J, Frykman V. Effects of yoga in patients with paroxysmal atrial fibrillation - a randomized controlled study. Eur J Cardiovasc Nurs. (2017) 16(1):57–63. doi: 10.1177/1474515116637734
22. Osbak P, Mourier M, Henriksen J, Kofoed K, Jensen G. Effect of physical exercise training on muscle strength and body composition, and their association with functional capacity and quality of life in patients with atrial fibrillation: a randomized controlled trial. J Rehabil Med. (2012) 44(11):975–9. doi: 10.2340/16501977-1039
23. Silva Alves L, Salemi VMC, Rocon C, Melo MDT, Chizzola PR, Amato JF, et al. P6059 echocardiography parameters, respiratory eficiency, and quality of life in patients with permanent atrial fibrillation and heart failure: effect of exercise training. A randomized controlled trial. Eur Heart J. (2018) 39(suppl_1):hy566–P6059. doi: 10.1093/eurheartj/ehy566.p6059
24. Borland M, Bergfeldt L, Nordeman L, Bollano E, Andersson L, Rosenkvist A, et al. Exercise-based cardiac rehabilitation improves physical fitness in patients with permanent atrial fibrillation – A randomized controlled study. Transl Sports Med. (2020) 3(5):415–25. doi: 10.1002/tsm2.166
25. Nourmohammadi Z, Khalifehzadeh-Esfahani A, Mehdi E, Sanei H. The effect of aerobic physical rehabilitation on the quality of life in patients with chronic atrial fibrillation; A randomized controlled clinical trial study. ARYA Atheroscler. (2019) 15(1):1. doi: 10.22122/arya.v15i1.1705
26. Smart NA, King N, Lambert JD, Pearson MJ, Campbell JL, Risom SS, et al. Exercise-based cardiac rehabilitation improves exercise capacity and health-related quality of life in people with atrial fibrillation: a systematic review and meta-analysis of randomised and non-randomised trials. Open Heart. (2018) 5(2):e000880. doi: 10.1136/openhrt-2018-000880
Keywords: atrial fibrillation, physical exercise, cardiopulmonary fitness, cardiac function, physical ability
Citation: Yang C, Wu Q, Lv Q, Hou X, Ye X, Yang Y, Li L, Zuo W and Wang S (2024) Efficacy of physical exercise on the physical ability, cardiac function and cardiopulmonary fitness of patients with atrial fibrillation: a systematic review and meta-analysis. Front. Cardiovasc. Med. 11:1352643. doi: 10.3389/fcvm.2024.1352643
Received: 13 December 2023; Accepted: 29 January 2024;
Published: 23 February 2024.
Edited by:
Konstantinos Athanasios Gatzoulis, National and Kapodistrian University of Athens, GreeceReviewed by:
Nikolaos Fragakis, Aristotle University of Thessaloniki, GreeceLaura Stefani, University of Florence, Italy
© 2024 Yang, Wu, Lv, Hou, Ye, Yang, Li, Zuo and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shihan Wang d2FuZ3NoaWhhbjkxQDEyNi5jb20=
 Chenyan Yang
Chenyan Yang Qian Wu
Qian Wu Qianyu Lv
Qianyu Lv Xinzheng Hou
Xinzheng Hou Xuejiao Ye
Xuejiao Ye Yingtian Yang
Yingtian Yang Lanlan Li
Lanlan Li Wenxi Zuo2
Wenxi Zuo2 Shihan Wang
Shihan Wang