- 1Inova Scar Heart and Vascular, Inova Health System, Falls Church, VA, United States
- 2University of Virginia School of Medicine, Charlottesville, VA, United States
- 3Inova Pride Clinic, Inova Health System, Falls Church, VA, United States
Cardiovascular disease (CVD) is the leading cause of morbidity and mortality in the United States. Data shows that social drivers of health (SDOH), including economic stability, racial/cultural identity, and community, have a significant impact on cardiovascular morbidity and mortality. LGBTQ+ (lesbian, gay, bisexual, transgender, queer, and other gender and sexual minority) patients face a variety of unique health risk factors and bear a disproportionate burden of CVD compared to cis-gender, heterosexual peers. There is a paucity of research assessing the etiologies of CVD health disparities within the LGBTQ+ community. Herein, we seek to explore existing literature on LGBTQ+ health disparities with a focus on cardiovascular disease, examine trends impacting LGBTQ+ health equity, and identify strategies and interventions that aim to promote LGBTQ+ cardiovascular health equity on a regional and national level.
1 Introduction to LGBTQ+ health
The lesbian, gay, bisexual, transgender, queer, and other gender and sexual minority population represents roughly 7.1% of the population in the United States (1). This heterogeneous community includes individuals who identify as lesbian, gay, bisexual, transgender, and queer, along with others who may identify with a different sexual orientation or gender identity (SOGI). On a whole, SOGI minority patients report lower overall self-reported rates of health compared to cis-gender heterosexual controls (2); a patient's SOGI intersect with other aspects of their identity including race, ethnicity, and other social drivers of health (SDOH) which can impact health outcomes. Over the past several decades, SDOH have been increasingly recognized as drivers of health inequity nationally (3).
Health equity refers to the concept of attaining the highest levels of health and wellness for all peoples; to understand one's set of unique set of health needs, data must exist which explore the intersection of SDOH and epidemiologic health data. Until recently, such data for LGBTQ+ patients were lacking. In 2011, the National Academy of Medicine released a report identifying these research gaps and called for research focused at better understanding LGBTQ+ specific health issues (4). More recently, the American Heart Association (AHA) released a statement in 2020 outlining ways to better understand LGBTQ+ cardiovascular health disparities, identify research gaps, while also providing a framework for research aimed at better understanding LGBTQ+ CV health equity (5).
2 LGBTQ+ health disparities
LGBTQ+ patients face health disparities on a regional and national level compared to their cis-gender peers in the United States. Many of these disparities are driven by inequities related to the community's SDOH. One of the most unifying long-term risk factors for adverse health outcomes in LGBTQ+ patients is related to minority stress (6). Minority stress is broadly driven by pervasive and chronic forms of stress borne by individuals who live in a society which marginalizes and discriminates against them (2, 6). Contributors to minority stress are multifactorial and include increased rates of discrimination at the familial, social, cultural, and employer level (7–9), amongst other sets of internal pressures, which result in higher rates of mental health disorders in the LGBTQ+ population and, putatively, higher rates of physiologic stress (2, 6, 10, 11). SOGI minority patients living in states which practice institutionalized discrimination against LGBTQ+ peoples face higher rates of mental illness compared to those living in states without such policies (12). Increased levels of psychosocial stressors result in increased physiological stress, an adverse impact on the immune system, and hypertension (13–15). The physiological impact of minority stress on the LGBTQ+ population have not been well studied (16), although it has been extensively studied in non-LGBTQ+ minority populations.
While minority stress is a common unifier of health inequity within the LGBTQ+ community, subgroups within the LGBTQ+ community face unique risk factors that impact overall health and well-being. Gay and bisexual men have higher rates of human immunodeficiency virus (HIV) (17). HIV contributes to chronic inflammation, and some drugs used in the treatment of HIV adversely affect cardiometabolic risk (18). Certain non-nucleoside reverse transcriptase inhibitors (NNRTIs) including stavudine and zidovudine have been shown to promote lipoatrophy (19). Protease inhibitors, including ritonavir, and other NNRTIs such as efavirenz and nevirapine, have been shown to promote dyslipidemia (19). Tenofovir lowers levels of high-density lipoproteins, low-density lipoproteins, and total cholesterol, but whether this translates into lower cardiovascular risk in setting of a chronic inflammatory milieu driven by HIV, is unknown (19). Highly active antiretroviral therapy also increases the risk for developing type 2 diabetes mellitus roughly four-fold (20).
Bisexual men face higher rates of substance abuse compared to both gay and straight men, and rates of substance abuse are generally higher in SOGI adults compared to the general population (21, 22). Lesbian women have higher rates of obesity and alcohol use compared to their heterosexual peers (23, 24). Moreover, lesbian women are more likely to engage in tobacco use compared to heterosexual women (25). Lesbian and bisexual women also have high rates of depression, anxiety, asthma and arthritis compared to heterosexual women (26, 27). Transgender patients are more likely to experience physical violence and have higher rates of housing instability and homelessness compared to heterosexual peers (28).
SOGI minority people of color (POC), particularly those with African ancestry, face increased rates of discrimination compared to white LGBTQ+ patients; this includes higher rates of social discrimination, racism, employment discrimination, and housing discrimination (29). This has led to higher rates of depression in LGBTQ+ POC compared to white LGBTQ+ peoples (30). Structural racism was associated with higher rates of anxiety and alcohol abuse for SOGI minority men of color, but not for white SOGI minority men (31). Gay and bisexual men who are black also face significantly higher rates of HIV and decreased utilization of pre-exposure prophylaxis compared to white gay and bisexual men (32). Roughly half (47%) of all SOGI patients of color live in a low-income household compared to 36% for white SOGI patients (33).
3 LGBTQ+ cardiovascular health disparities
LGBTQ+ patients also face increased risk for cardiovascular disease compared to the general population (34). Risk factors for cardiovascular disease generally exhibit wide variation across LGBTQ+ subgroups, and risk factors shared by one SOGI group may not be observed in other SOGI groups. However, on a whole, cardiovascular disease tends to develop at an earlier age for LGBTQ+ patients compared to heterosexual peers (35).
Observational studies have consistently shown that LGBTQ+ patients have higher rates of hypertension compared to their heterosexual peers (15, 35). Sexual minority women are diagnosed with hypertension roughly a decade earlier than heterosexual women, or between the ages of 35–44 (compared to 45–54 for heterosexual women) (35). Gay and bisexual men experience increased rates of hypertension compared to heterosexual men, but age at onset to diagnosis does not differ when compared to heterosexual men (35, 36). Transgender men also experience increases in blood pressure following gender affirming hormone therapy (GAHT), while for transgender women, blood pressure decreases with GAHT (37).
No concrete data exists as to the extent and mechanisms driving this observed risk of hypertension for SOGI minority patients. One hypothesis is that physiologic mediators of chronic stress (minority stress theory) may drive this disparity, which has been observed and studied in other cis-gender minority communities adversely impacted by chronic stress (38).
Gay and bisexual men, as well as lesbian and bisexual women, have higher rates of dyslipidemia compared to their heterosexual peers (35). Gender affirming hormone therapy (GAHT) has been shown to promote dyslipidemia in transgender patients, but evidence is mixed as to whether this translates into worse long-term cardiovascular outcomes (39, 40). HAART therapy in HIV + patients can promote dyslipidemia, and there are numerous drug-drug interactions between HAART and statin medications; the recent REPRIEVE trial showed that for patients with HIV and moderate or greater risk of cardiovascular disease, pitavastatin reduced rates of major adverse cardiovascular outcomes (41).
Lesbian, gay, and bisexual patients have higher rates of stroke compared to their heterosexual peers (35). Gay and bisexual men have roughly twice the adjusted risk of myocardial infarction and heart failure compared to heterosexual men (35). Transgender men face higher rates of myocardial infarction compared to both to cis-gender men and women (42). Clear mechanisms explaining this increased have not been identified. Despite having higher rates of heart disease, LGBTQ+ patients are less likely to be treated for primary prevention of heart disease with statin medications compared to their heterosexual peers, even after controlling for a variety of social and economic risk factors (43). The authors speculated that the residual disparities may be the result of “bias, stereotyping, and mistrust” (43).
The effects of GAHT on cardiac remodeling remains unknown, and robust data does not exist on the topic (44). Older data had suggested that transgender women had higher rates of venous thromboembolism (VTE) compared to the general population, but this observation was only with an estradiol no longer used with GAHT (39). More recent studies have not observed an increased risk of VTE in transgender men or women on GAHT under the age of 37 years old (45). Prospective cohort studies are needed to better understand what, if any, long term effects on cardiac remodeling or VTE are associated with GAHT.
Our current understanding of the unique health risks that affect LGBTQ+ patients is summarized in Figure 1. While there is some commonality to health disparities affecting LGBTQ+, there is significant heterogeneity within each community subgroup. Even within subgroups, there is significant variation in terms of health inequities, some of these being driven by one's SDOH (Figure 1).
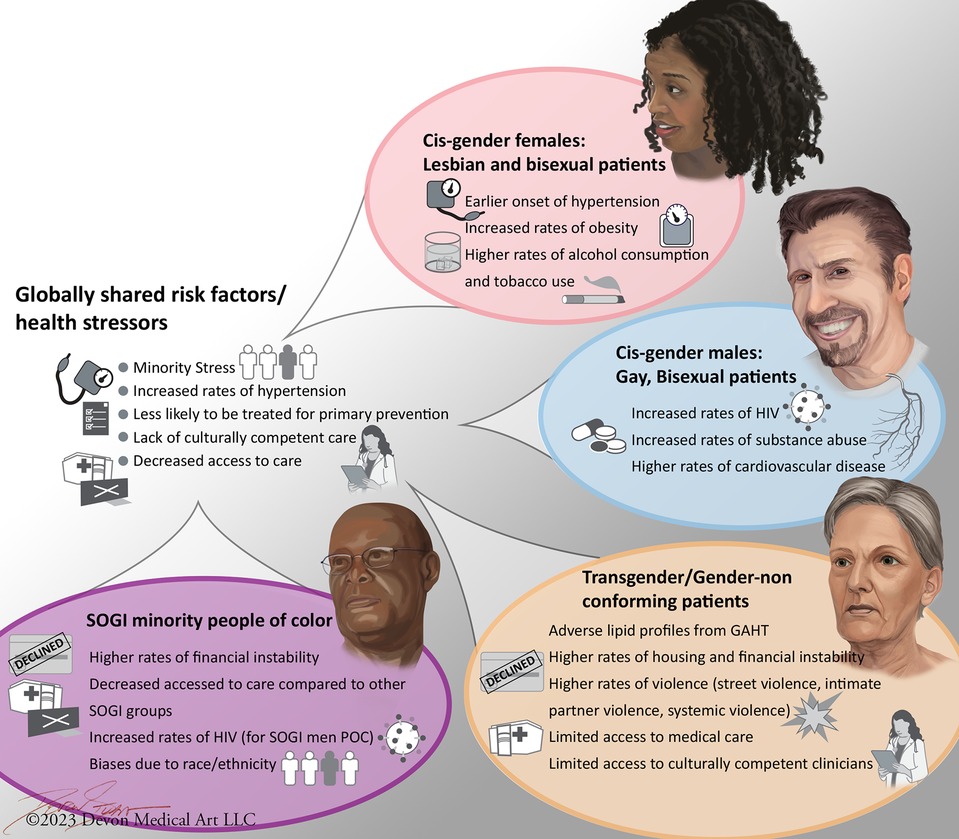
Figure 1. Heterogeneity of social drivers of health and health disparities within the LGBTQ+ population. Cis-gender refers to a patient whose gender identity corresponds with the sex assigned at birth. SOGI refers to sexual orientation and gender identity. While LGBTQ+ patients share some similar risk factors which increase their risk of cardiovascular disease, these disparities are not consistently observed between different LGBTQ+ subgroups.
4 LGBTQ+ barriers to care
Having access to quality, culturally competent health care is paramount component of SDOH. Numerous barriers to care for LGBTQ+ patients have been identified. These include structural discrimination, financial barriers to care, and lack of access to culturally competent care for LGBTQ+ patients in the United States.
SOGI minority patients have increasingly faced sociopolitical systemic discrimination in the United States, where a growing social milieu in areas of the United States has evolved to limit LGBTQ+ access to care (46, 47). This sociopolitical discrimination has been rising across the United States in recent years (48). For example, in Texas and Mississippi, LGBTQ+ focused University-based health centers were forced to close under political duress (49, 50). Prescribing GAHT, a treatment which reduces rates of depression and suicide attempts in transgender adolescents, is currently a felony in 5 US states (48). In 3 other states, it is illegal to provide GAHT although it is not considered a felony (48). 19 states within the US restrict GAHT care for adolescents, and 16 of the 19 state laws restricting access to GAHT have been passed within the past year (48). The United States House of Representatives recently passed a bill in July of 2023 which would eliminate fundings for LGBTQ+ health centers nationally (51). The number of bills and legislation introduced at the federal and state level continues to steadily increase, and the future health impact of the present political climate on LGBTQ+ patients, particularly younger LGBTQ+ patients, remains to be seen.
Access to health insurance had previously been a barrier for LGBTQ+ patients, but after the Affordable Care Act was passed in 2016, coverage rates between LGBTQ+ patients and their cis-gender peers were observed to be comparable (52). However, disparities exist within the LGBTQ+ community, where LGBTQ+ POC are more like to be uninsured compared to white LGBTQ+ patients (53). LGBTQ+ patients also have higher rates of self-reported financial stressors when accessing healthcare compared non-SOGI minority peers (54).
Despite the growing body of literature demonstrating poorer health outcomes for LGBTQ+ patients, there is wide variation in how medical schools in the United States educate students on these topics (55). Roughly one third of allopathic and osteopathic medical schools in the United States and Canada reported having zero hours of clinical education for students on LGBTQ+ related health issues; the median national average for Canadian and US medical schools was 5 h of training over four years (55). Growing data has begun to emerge that both undergraduate and graduate medical education related to LGBTQ+ is not sufficient to address the unique health needs of LGBTQ+ patients (56). For example, a recent survey of internal medicine residents in 120 programs across the Unites States showed that nearly half of trainees have very limited knowledge of basic knowledge related to LGBTQ+ patients (57). Moreover, medical residents and fellows in the US feel less comfortable discussing LGBTQ+ patient related concerns compared to US medical students (58), which is somewhat concerning. It’s noteworthy that LGBTQ+ medical residents in the US face higher levels of discrimination and bullying by peers and attendings during their medical training compared to their non-SOGI minority peers (59). Some have advocated for a broader commitment by the Accreditation Council for Graduate Medical Education (ACGME) to better incorporate LGBTQ+ health issues pertinent to the residency specialties during graduate medical education training (56).
5 LGBTQ+ health in Northern Virginia
The DMV (Washington, District of Columbia, Maryland, and Virginia) area has historically been home to a large and vibrant LGBTQ+ community. However, many health resources dedicated to this population are located within the District of Columbia for several reasons, including geographical concentration of people and centralized distribution of care. As the DMV region continues to grow and expand, it became clear that the LGBTQ+ community in Northern Virginia was lacking in resources specifically dedicated to them within the Virginia region. This need has been a well-known fact highlighted in the findings of several population needs surveys conducted by health departments and local health systems. In June of 2022, Inova Health System opened its first LGBTQ+ clinic named the Inova Pride Clinic (60). The Inova Pride clinic serves LGBTQ+ youths (ages 12 and greater) and adults alike, with over 1,000 new patients in its first calendar year of opening. The purpose of this specialized clinic is to provide comprehensive holistic primary care with an LGBTQ+ focus—to expand the scope of service of primary care to include specific needs for the LGBTQ+ population including gender affirming care, robust mental health services, sexual health, HIV prevention and treatment, and management of chronic diseases.
The clinic has met great success—surpassing initial projections for growth and highlighting the dire need and desire for these services in Virginia and beyond. The Pride Clinic houses medical specialties including internal medicine, pediatrics, obstetrics and gynecology, as well as behavioral health services. Our primary patient population resides in Northern Virginia, Washington, DC, and Maryland. As our clinic continues to grow, we have started to see patients well outside of our geographical location, including the Deep South. Not all patients have the means or resources to travel out of state for medical care, if such medical care is limited in their home state.
At Inova Schar Heart and Vascular, we are working to build a partnership with the Inova Pride Clinic in an effort to enhance cardiovascular care for this community. One of the largest present limitations of cardiovascular research on LGBTQ+ patient's unique health profiles is a lack of SOGI data incorporated into electronic medical records. Going forward, we hope to leverage this robust, comprehensive patient dataset to better understand unique cardiovascular factors impacting LGBTQ+ patients. Long term, we seek to develop the first prospective cardiovascular cohort study of LGBTQ+ patients specifically focused on both clinical and physiologic stressors of health to better understand cardiovascular disease risk factors in this community. Ultimately, we see this as a step towards a broader promotion of community-level LGBTQ+ cardiovascular health equity in the DMV, and especially Northern Virginia.
6 Conclusions
Research has only begun to reveal the disparities that LGBTQ+ identifying individuals may face, limiting our understanding of mechanisms underlying these disparities. The purpose of this review was to frame our current understanding of these risks and to consider how to fill existing gaps in knowledge. By having a dedicated LGBTQ+ center of care, we are building a platform which directly allows us to promote community health equity and reduce barriers to care (to the extent that we, as a health system, have control over said barriers). More research, both in the basic science and longitudinal clinical studies, needs to be performed to community to continue using such venues to partner with the community and better learn about their specific needs and most successful strategies to improve their health and improve equity. Our current understanding of the unique health factors impacting LGBTQ+ cardiovascular health will likely change as more data becomes available. The long-term effects of the current political on current and future LGBTQ+ health remains to be seen.
Author contributions
JB: Writing – review & editing. KL: Writing – review & editing. JR: Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors are thankful for their support from Inova Health System for their commitment to health equity for all those in our community, and especially KB, MSW, LCSW, CSAC who made the Inova Pride Clinic a reality. We are grateful to Bill and CK for their philanthropic support of health equity in our community.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Gallop. (2022). Available online at: https://news.gallup.com/poll/389792/lgbt-identification-ticks-up.aspx (accessed July 20, 2023).
2. Liu M, Sandhu S, Reisner SL, Gonzales G, Keuroghlian AS. Health status and health care access among lesbian, gay, and bisexual adults in the US, 2013 to 2018. JAMA Intern Med. (2023) 183(4):380–3. doi: 10.1001/jamainternmed.2022.6523
3. Jilani MH, Javed Z, Yahya T, Valero-Elizondo J, Khan SU, Kash B, et al. Social determinants of health and cardiovascular disease: current state and future directions towards healthcare equity. Curr Atheroscler Rep. (2021) 23(9):55. doi: 10.1007/s11883-021-00949-w
4. Institute of Medicine (US) Committee on Lesbian, Gay, Bisexual, and Transgender Health Issues and Research Gaps and Opportunities. The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for better Understanding. Washington, DC: National Academies Press (US) (2011). doi: 10.17226/13128 Available online at: https://www.ncbi.nlm.nih.gov/books/NBK64806/ (accessed June 7, 2023).
5. Caceres BA, Streed CG Jr, Corliss HL, Lloyd-Jones DM, Matthews PA, Mukherjee M, et al. American heart association council on cardiovascular and stroke nursing; council on hypertension; council on lifestyle and cardiometabolic health; council on peripheral vascular disease; and stroke council. Assessing and addressing cardiovascular health in LGBTQ adults: a scientific statement from the American heart association. Circulation. (2020) 142(19):e321–32. doi: 10.1161/CIR.0000000000000914
6. Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. (2003) 129(5):674–97. doi: 10.1037/0033-2909.129.5.674
7. Eliason MJ, Dibble SL, Robertson PA. Lesbian, gay, bisexual, and transgender (LGBT) physicians’ experiences in the workplace. J Homosex. (2011) 58(10):1355–71. doi: 10.1080/00918369.2011.614902
8. Hoy-Ellis CP. Minority stress and mental health: a review of the literature. J Homosex. (2023) 70(5):806–30. doi: 10.1080/00918369.2021.2004794
9. Ryan C, Huebner D, Diaz RM, Sanchez J. Family rejection as a predictor of negative health outcomes in white and latino lesbian, gay, and bisexual young adults. Pediatrics. (2009) 123(1):346–52. doi: 10.1542/peds.2007-3524
10. Choi KR, Wisk LE, Zima BT. Availability of LGBTQ mental health services for US youth, 2014 to 2020. JAMA Pediatr. (2023) 177(8):865–7. doi: 10.1001/jamapediatrics.2023.1473
11. Hatzenbuehler ML, Pachankis JE. Stigma and minority stress as social determinants of health among lesbian, gay, bisexual, and transgender youth: research evidence and clinical implications. Pediatr Clin North Am. (2016) 63(6):985–97. doi: 10.1016/j.pcl.2016.07.003
12. Hatzenbuehler ML, McLaughlin KA, Keyes KM, Hasin DS. The impact of institutional discrimination on psychiatric disorders in lesbian, gay, and bisexual populations: a prospective study. Am J Public Health. (2010) 100(3):452–9. doi: 10.2105/AJPH.2009.168815
13. Segerstrom SC, Miller GE. Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry. Psychol Bull. (2004) 130(4):601–30. doi: 10.1037/0033-2909.130.4.601
14. Spruill TM. Chronic psychosocial stress and hypertension. Curr Hypertens Rep. (2010) 12(1):10–6. doi: 10.1007/s11906-009-0084-8
15. Taweh O, Moreira JD. Proposed mechanisms of hypertension and risk of adverse cardiovascular outcomes in LGBT communities. Am J Physiol Heart Circ Physiol. (2023) 325(3):H522–8. doi: 10.1152/ajpheart.00346.2023
16. Caceres BA, Sharma Y, Doan D. Hypertension risk in sexual and gender minority individuals. Expert Rev Cardiovasc Ther. (2022) 20(5):339–41. doi: 10.1080/14779072.2022.2075345
17. Sullivan PS, Satcher Johnson A, Pembleton ES, Stephenson R, Justice AC, Althoff KN, et al. Epidemiology of HIV in the USA: epidemic burden, inequities, contexts, and responses. Lancet. (2021) 397(10279):1095–106. doi: 10.1016/S0140-6736(21)00395-0
18. Reyskens KM, Essop MF. HIV protease inhibitors and onset of cardiovascular diseases: a central role for oxidative stress and dysregulation of the ubiquitin-proteasome system. Biochim Biophys Acta. (2014) 1842(2):256–68. doi: 10.1016/j.bbadis.2013.11.019
19. Brown TT, Glesby MJ. Management of the metabolic effects of HIV and HIV drugs. Nat Rev Endocrinol. (2011) 8(1):11–21. doi: 10.1038/nrendo.2011.151
20. Brown TT, Cole SR, Li X, Kingsley LA, Palella FJ, Riddler SA, et al. Antiretroviral therapy and the prevalence and incidence of diabetes mellitus in the multicenter AIDS cohort study. Arch Intern Med. (2005) 165(10):1179–84. Erratum in: Arch Intern Med. 2005 Nov 28;165(21):2541. doi: 10.1001/archinte.165.10.1179
21. Roth EA, Cui Z, Wang L, Armstrong HL, Rich AJ, Lachowsky NJ, et al. Substance use patterns of gay and bisexual men in the momentum health study. Am J Mens Health. (2018) 12(5):1759–73. doi: 10.1177/1557988318786872
22. Williams ND, Fish JN. The availability of LGBT-specific mental health and substance abuse treatment in the United States. Health Serv Res. (2020) 55(6):932–43. doi: 10.1111/1475-6773.13559
23. Azagba S, Latham K, Shan L. Cigarette, smokeless tobacco, and alcohol use among transgender adults in the United States. Int J Drug Policy. (2019) 73:163–9. doi: 10.1016/j.drugpo.2019.07.024
24. Boehmer U, Bowen DJ, Bauer GR. Overweight and obesity in sexual-minority women: evidence from population-based data. Am J Public Health. (2007) 97(6):1134–40. doi: 10.2105/AJPH.2006.088419
25. Taylor MNL, Gonzales G. Health disparities among women by sexual orientation identity and same-sex or different-sex cohabiting partnership status. Womens Health Issues. (2022) 32(1):80–6. doi: 10.1016/j.whi.2021.07.001
26. Lewis RJ, Ehlke SJ, Shappie AT, Braitman AL, Heron KE. Health disparities among exclusively lesbian, mostly lesbian, and bisexual young women. LGBT Health. (2019) 6(8):400–8. doi: 10.1089/lgbt.2019.0055
27. Simoni JM, Smith L, Oost KM, Lehavot K, Fredriksen-Goldsen K. Disparities in physical health conditions among lesbian and bisexual women: a systematic review of population-based studies. J Homosex. (2017) 64(1):32–44. doi: 10.1080/00918369.2016.1174021
28. James SE, Herman JL, Rankin S, Keisling M, Mottet L, Anafi M. The Report of the 2015 U.S. Transgender Survey. Washington, DC: National Center for Transgender Equality (2016).
29. Whitefield DL, Walls NE, Langendferfer-Magruder L. Queer is the new black? Not so much: racial disparities in an anti-LGBTQ discrimintation. J Gay Lesbian Soc Serv. (2014) 26:426–40. doi: 10.1080/10538720.2014.955556
30. Kertzner RM, Meyer IH, Frost DM, Stirratt MJ. Social and psychological well-being in lesbians, gay men, and bisexuals: the effects of race, gender, age, and sexual identity. Am J Orthopsychiatry. (2009) 79(4):500–10. doi: 10.1037/a0016848
31. English D, Carter JA, Boone CA, Forbes N, Bowleg L, Malebranche DJ, et al. Intersecting structural oppression and black sexual minority men’s health. Am J Prev Med. (2021) 60(6):781–91. doi: 10.1016/j.amepre.2020.12.022
32. Mayer KH, Nelson L, Hightow-Weidman L, Mimiaga MJ, Mena L, Reisner S, et al. The persistent and evolving HIV epidemic in American men who have sex with men. Lancet. (2021) 397(10279):1116–26. doi: 10.1016/S0140-6736(21)00321-4
34. Caceres BA, Brody A, Luscombe RE, Primiano JE, Marusca P, Sitts EM, et al. A systematic review of cardiovascular disease in sexual minorities. Am J Public Health. (2017) 107(4):e13–21. doi: 10.2105/AJPH.2016.303630
35. Sherman J, Dyar C, McDaniel J, Funderburg NT, Rose KM, Gorr M, et al. Sexual minorities are at elevated risk of cardiovascular disease from a younger age than heterosexuals. J Behav Med. (2022) 45(4):571–9. doi: 10.1007/s10865-021-00269-z
36. Sharma Y, Taylor JY, Hughes T, Caceres BA. Cardiovascular stroke nursing best abstract award: investigating sexual identity disparities in hypertension and hypertension treatment among adults. Circulation. (2021) 144:A9744. doi: 10.1161/circ.144.suppl_1.9744
37. Banks K, Kyinn M, Leemaqz SY, Sarkodie E, Goldstein D, Irwig MS. Blood pressure effects of gender-affirming hormone therapy in transgender and gender-diverse adults. Hypertension. (2021) 77(6):2066–74. doi: 10.1161/HYPERTENSIONAHA.120.16839
38. Spruill TM, Butler MJ, Thomas SJ, Tajeu GS, Kalinowski J, Castañeda SF, et al. Association between high perceived stress over time and incident hypertension in black adults: findings from the Jackson heart study. J Am Heart Assoc. (2019) 8(21):e012139. doi: 10.1161/JAHA.119.012139
39. Aranda G, Halperin I, Gomez-Gil E, Hanzu FA, Seguí N, Guillamon A, et al. Cardiovascular risk associated with gender affirming hormone therapy in transgender population. Front Endocrinol (Lausanne). (2021) 12:718200. doi: 10.3389/fendo.2021.718200
40. Masumori N, Nakatsuka M. Cardiovascular risk in transgender people with gender-affirming hormone treatment. Circ Rep. (2023) 5(4):105–13. doi: 10.1253/circrep.CR-23-0021
41. Grinspoon SK, Fitch KV, Zanni MV, Fichtenbaum CJ, Umbleja T, Aberg JA, et al. REPRIEVE investigators. Pitavastatin to prevent cardiovascular disease in HIV infection. N Engl J Med. (2023) 389(8):687–99. doi: 10.1056/NEJMoa2304146
42. Alzahrani T, Nguyen T, Ryan A, Dwairy A, McCaffrey J, Yunus R, et al. Cardiovascular disease risk factors and myocardial infarction in the transgender population. Circ Cardiovasc Qual Outcomes. (2019) 12(4):e005597. doi: 10.1161/CIRCOUTCOMES.119.005597
43. Frank DA, Johnson AE, Hausmann LRM, Gellad WF, Roberts ET, Vajravelu RK. Disparities in guideline-recommended statin use for prevention of atherosclerotic cardiovascular disease by race, ethnicity, and gender: a nationally representative cross-sectional analysis of adults in the United States. Ann Intern Med. (2023) 176(8):1057–66. doi: 10.7326/M23-0720
44. Mahowald MK, Maheshwari AK, Lara-Breitinger KM, Adel FW, Pellikka PA, Davidge-Pitts CJ, et al. Characteristics of transgender women referred to women’s heart clinic. Am J Prev Cardiol. (2021) 7:100223. doi: 10.1016/j.ajpc.2021.100223
45. Totaro M, Palazzi S, Castellini C, Parisi A, D'Amato F, Tienforti D, et al. Risk of venous thromboembolism in transgender people undergoing hormone feminizing therapy: a prevalence meta-analysis and meta-regression study. Front Endocrinol (Lausanne). (2021) 12:741866. doi: 10.3389/fendo.2021.741866
46. Casey LS, Reisner SL, Findling MG, Blendon RJ, Benson JM, Sayde JM, et al. Discrimination in the United States: experiences of lesbian, gay, bisexual, transgender, and queer Americans. Health Serv Res. (2019) 54(Suppl 2):1454–66. doi: 10.1111/1475-6773.13229
47. Jaffe S. LGBTQ discrimination in US health care under scrutiny. Lancet. (2020) 395(10242):1961. doi: 10.1016/S0140-6736(20)31446-X
48. Movement Advancement Project. Equality Maps: Bans on Best Practice Medical Care for Transgender Youth. (2023). Available online at: www.mapresearch.org/equalitymaps/healthcare/youth_medical_care_bans (accessed July 6, 2023)
49. WLBT. “UMMC to shut down LGBTQ+ clinic amid political pressure” (2023). Available online at: https://www.wlbt.com/2023/06/01/ummc-shut-down-lgbtq-clinic-amid-political-pressure/ (accessed June 7, 2023).
50. Rummler O. “Political pressure led to shutdown of Texas' largest gender-affirming care program”. The Texas Tribune (2022). Available online at: https://www.texastribune.org/2022/03/11/texas-genecis-closure-transgender/ (accessed June 7, 2023).
51. The Hill. Available online at: https://thehill.com/homenews/house/4104634-house-republicans-eliminate-funding-to-lgbtq-community-centers-after-tense-hearing/ (accessed August 16, 2023)
52. Bolibol A, Buchmueller TC, Lewis B, Miller S. Health insurance coverage and access to care among LGBT adults, 2013–19. Health Aff (Millwood). (2023) 42(6):858–65. doi: 10.1377/hlthaff.2022.01493
53. Macapagal K, Bhatia R, Greene GJ. Differences in healthcare access, use, and experiences within a community sample of racially diverse lesbian, gay, bisexual, transgender, and questioning emerging adults. LGBT Health. (2016) 3(6):434–42. doi: 10.1089/lgbt.2015.0124
54. Fredriksen-Goldsen KI, Romanelli M, Jung HH, Kim HJ. Health, economic, and social disparities among lesbian, gay, bisexual, and sexually diverse adults: results from a population-based study. Behav Med. (2023):1–12. doi: 10.1080/08964289.2022.2153787
55. Obedin-Maliver J, Goldsmith ES, Stewart L, White W, Tran E, Brenman S, et al. Lesbian, gay, bisexual, and transgender-related content in undergraduate medical education. JAMA. (2011) 306(9):971–7. doi: 10.1001/jama.2011.1255
56. Pregnall AM, Churchwell AL, Ehrenfeld JM. A call for LGBTQ content in graduate medical education program requirements. Acad Med. (2021) 96(6):828–35. doi: 10.1097/ACM.0000000000003581
57. Streed CG Jr, Hedian HF, Bertram A, Sisson SD. Assessment of internal medicine resident preparedness to care for lesbian, gay, bisexual, transgender, and queer/questioning patients. J Gen Intern Med. (2019) 34(6):893–8. doi: 10.1007/s11606-019-04855-5
58. Hayes V, Blondeau W, Bing-You RG. Assessment of medical student and resident/fellow knowledge, comfort, and training with sexual history taking in LGBTQ patients. Fam Med. (2015) 47(5):383–7. 25905882
59. Heiderscheit EA, Schlick CJR, Ellis RJ, Cheung EO, Irizarry D, Amortegui D, et al. Experiences of LGBTQ+ residents in US general surgery training programs. JAMA Surg. (2022) 157(1):23–32. doi: 10.1001/jamasurg.2021.5246
60. Washington Post. “Inova opens LGBTQ+ ‘pride clinic,’ a first for Northern Virginia” (2022). Available online at: https://www.washingtonpost.com/dc-md-va/2022/06/08/pride-clinic-inova-northern-virginia/ (accessed June 7, 2023).
Keywords: LGBTQ+ cardiovascular health, health equity, social drivers of health, SOGI, cardiovascular risk
Citation: Bonomo JA, Luo K and Ramallo JA (2024) LGBTQ+ cardiovascular health equity: a brief review. Front. Cardiovasc. Med. 11:1350603. doi: 10.3389/fcvm.2024.1350603
Received: 5 December 2023; Accepted: 15 February 2024;
Published: 6 March 2024.
Edited by:
Lauren Cooper, Northwell Health, United StatesReviewed by:
Carolina Dalmasso, University of Kentucky, United States© 2024 Bonomo, Luo and Ramallo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jason A. Bonomo amFzb24uYm9ub21vQGlub3ZhLm9yZw==
 Jason A. Bonomo
Jason A. Bonomo Kate Luo2
Kate Luo2