- 1Department of Internal Medicine, School of Medicine, University of Zagreb, Zagreb, Croatia
- 2Division of Clinical Pharmacology, Department of Internal Medicine, University Hospital Centre Zagreb, Zagreb, Croatia
- 3School of Medicine, University of Zagreb, Zagreb, Croatia
- 4Department of Internal Medicine, University Hospital Centre Zagreb, Zagreb, Croatia
- 5Department of Cardiology and Congenital Diseases of Adults, Polish Mother’s Memorial Hospital Research Institute, Lodz, Poland
Dyslipidaemia is a complex disorder characterised by abnormal lipid levels in the blood, including cholesterol and triglycerides, and plays an important role in the development of atherosclerotic cardiovascular disease. Most risk factors for cardiovascular disease are modifiable, and dyslipidaemia is a key factor among them. It can result from a combination of genetic and environmental factors. A distinction is made between primary dyslipidaemia, which is mainly caused by inherited genetic changes, and secondary dyslipidaemia, which is due to underlying diseases or certain medications. The treatment of dyslipidaemia has evolved over the years. In the past, statins were the first choice, but newer drugs, such as proprotein convertase subtilisin-kexin type 9 (PCSK9) inhibitors, have gained prominence due to their effectiveness in lowering lipids. Although recent guidelines recommend PCSK9 inhibitors for high-risk patients and patients who cannot tolerate statins, their widespread use is limited because of cost. Several meta-analyses have confirmed the efficacy and safety of PCSK9 inhibitors and have shown a significant reduction in low-density lipoprotein (LDL) cholesterol levels. However, the long-term side effects and interactions with other risk factors for cardiovascular disease remain uncertain. In addition, cost-effectiveness analyses have shown mixed results, with some countries considering PCSK9 inhibitors to be cost-effective for certain patient groups, while others consider them less economical. Meanwhile, initial data from patients using PCSK9 inhibitors support the results of the clinical trials. To summarise, PCSK9 inhibitors represent a revolutionary solution for lowering LDL cholesterol, but their cost-effectiveness remains controversial. Despite the controversy, they offer clear benefits for high-risk patients and should therefore be considered in the treatment of dyslipidaemia.
Introduction
Dyslipidaemia is a heterogeneous disorder characterised by abnormal lipid levels in the blood. These disorders are characterised by changes in the quantity, quality, or both of various lipid components, including cholesterol and triglycerides (1). They play an important role in the development of atherosclerotic cardiovascular diseases (CVD), such as coronary heart disease, acute myocardial infarction (MI), ischaemic stroke, peripheral arterial disease, and heart failure. The vast majority of risk factors for CVD are modifiable risk factors, such as diabetes mellitus, smoking, hypertension, obesity, and physical inactivity, with dyslipidaemia being one of the most important (2). Dyslipidaemia can result from a combination of genetic and environmental factors. A distinction is usually made between primary and secondary dyslipidaemia. Primary dyslipidaemia, of which familial hypercholesterolaemia is the most important and common, refers to lipid disorders that are primarily caused by inherited genetic changes. Traditionally, they are categorised into types I–V according to Frederickson's classification, based on the particles that show elevated levels in the blood. However, Frederickson's classification was first published in the 1960s. Today, patients in the 21st century need modern and updated classifications based on all aspects of cardiovascular risk and not just elevated lipid particles in the blood (3). Secondary dyslipidaemia or acquired dyslipidaemia occurs due to underlying diseases, lifestyle factors, or the use of certain medications. The most important risk factors for the development of secondary dyslipidaemia are obesity, diabetes mellitus, chronic kidney disease, chronic liver disease, and certain medications such as corticosteroids and diuretics taken over a long period of time (4). Even the new checkpoint inhibitors for oncological treatment have been observed to increase cholesterol levels, as indicated in the summary of product characteristics. Dyslipidaemia is therefore an increasingly attractive topic for the medical community, especially with the development of new therapeutic approaches (5). Until relatively recently, treatment with statins was the first choice for the treatment of dyslipidaemia. Nowadays, new drugs are being developed. The first new drug to come on the market was ezetimibe, which binds to the NPC1L1 transporter protein and thus inhibits fat absorption in the intestine (5). Proprotein convertase subtilisin-kexin type 9 (PCSK9) inhibitors were also developed: alirocumab and evolocumab as monoclonal antibodies, followed by the small RNA-interfering molecule inclisiran (6). All of these agents inhibit PCSK9, prolong low-density lipoprotein (LDL) receptor activation and lower LDL cholesterol levels (6).
In view of these therapeutic approaches, the European Atherosclerosis Society has published guidelines for the treatment of dyslipidaemia. The latest edition is from 2019 and the major innovation in these guidelines is the stratification of CVD risk for patients with primary dyslipidaemia using the revised SCORE system, called SCORE2 and SCORE-OP (7). In addition, these guidelines have revised the nomenclature of statin intolerance and place a strong emphasis on increasing statin treatment in patients previously discontinued due to non-specific, possibly statin-related symptoms. However, an important addition to the guidelines was also the inclusion of treatment recommendations based on new studies of PCSK9 inhibition that demonstrate the efficacy and safety profile of these drugs (8).
Although recent guidelines recommend their use in patients with a very high cardiovascular risk and in patients who cannot tolerate statins (which is not uncommon), PCSK9 inhibitors are not as widely used as statin treatment because of their cost (9). The aim of this review was to present the results of several meta-analyses conducted in the field of dyslipidaemia over the last 5 years, with a focus on PCSK9 inhibition. Another important aim of this paper was to discuss the results of the various studies in which PCSK9 inhibitors have been analysed in the context of cost-effectiveness with other lipid-lowering (LL) drugs. Instead of the 5-year period used for the aforementioned meta-analyses on safety and efficacy, we have chosen a shorter 3-year period (2020–2023) to get the best possible overview of the current market situation.
Methods
For this literature review, PubMed, Scopus, Embase, and Web of Science were searched between October 2022 and 5 May 2023 using the keywords “PCSK9 inhibitors”, “efficacy”, “safety” and “cost-effectiveness”. We considered articles published in the 5-year period before the search. After a thorough assessment by two independent reviewers, we included 30 publications focusing on the efficacy and cost-effectiveness of PCSK9 inhibitors in the treatment of dyslipidaemia.
Results
Safety and efficacy of PCSK9 inhibitor treatment
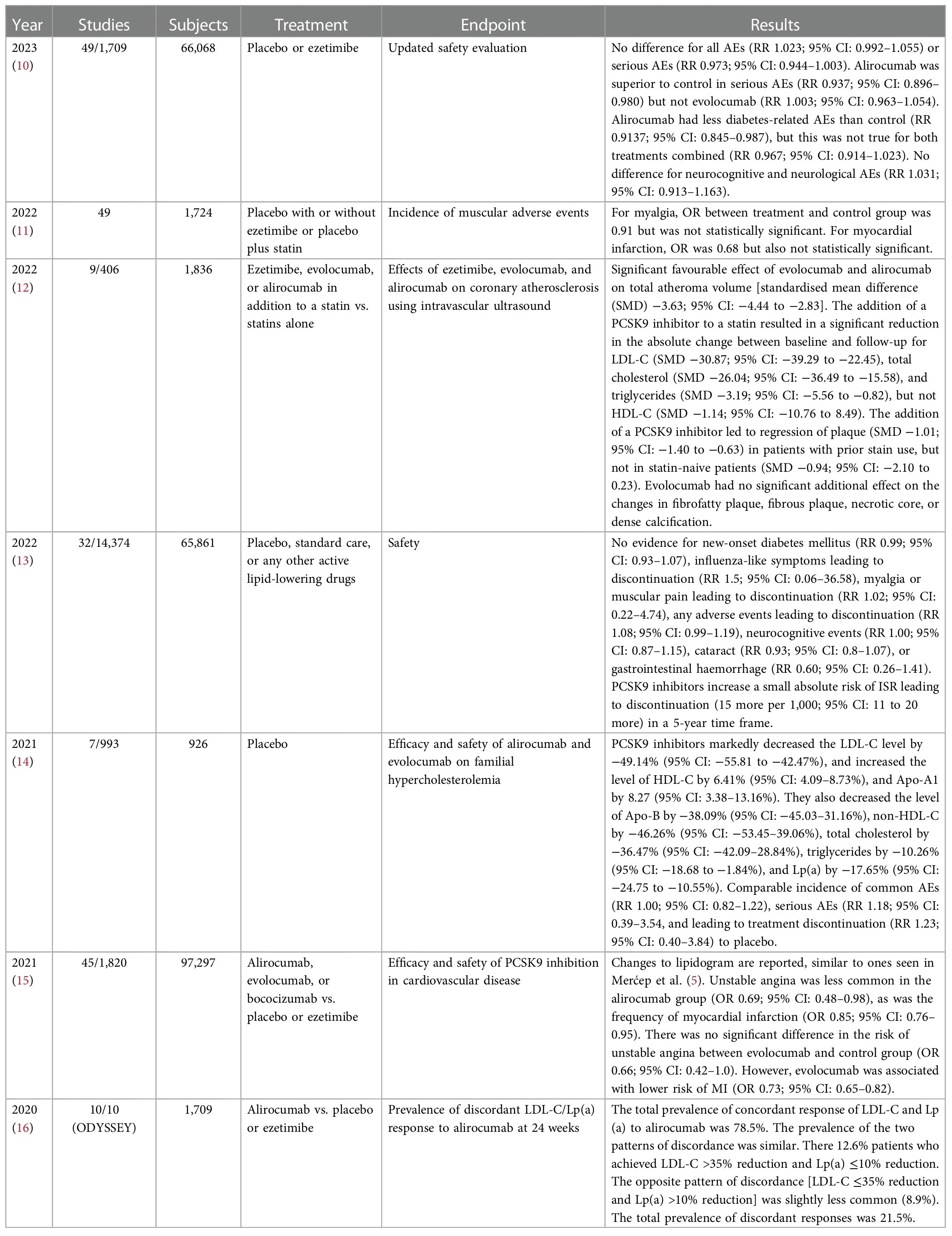
PCSK9 inhibitors significantly reduced cardiovascular events, heart attacks, and ischaemic strokes compared to statins (Table 1). However, these consistent benefits were not observed when compared with ezetimibe (10, 11). Alirocumab and evolocumab showed a reduction in cardiovascular disease, myocardial infarction, and stroke compared to placebo, with varying effects on mortality (15, 20, 21). PCSK9 inhibitors showed a greater reduction in LDL-C levels compared to ezetimibe, with no significant differences between doses (14–16). The risk of myocardial infarction, stroke, heart failure, diabetes mellitus, neurocognitive events, and death was comparable to placebo in both lipid-lowering trials and clinical outcome trials (17, 18). The combination of dual lipid-lowering therapy with PCSK9 inhibitors and ezetimibe led to a significant reduction in total atheroma volume (12). PCSK9 inhibitors did not increase the risk of diabetes or cataracts (13, 25, 30, 31). In the FOURIER study, evolocumab showed a 31% relative risk reduction in venous thromboembolism compared to placebo. The expected relative risks for cholesterol reduction with PCSK9 inhibitors were reported as 0.851, 0.810, and 0.770 for a 20%, 30%, and 40% reduction, respectively (28). Lowering LDL-C levels was associated with a lower risk of major cardiovascular events, myocardial infarction, stroke, and death overall across different interventions and subgroups (27).
The analysis showed no significant difference in overall or serious adverse events compared to the control group. Alirocumab showed superiority in reducing serious adverse events and had fewer diabetes-related events than the control group (21, 26). No significant differences were observed for evolocumab (22). There was also no significant difference in neurocognitive and neurological adverse events (23). The odds ratios for myalgia and myocardial infarction did not reach statistical significance. Both evolocumab and alirocumab had a favourable effect on total atheroma volume (24). PCSK9 inhibitors significantly reduced LDL-C levels and had a favourable effect on lipid profiles (19, 29). There was no evidence of new-onset diabetes, flu-like symptoms, or other adverse events leading to discontinuation of treatment (13). PCSK9 inhibitors did not increase the risk of injection site reactions over a 5-year period (13).
Cost-effectiveness of the PCSK9 inhibitor treatment
The comprehensive analysis of cost-effectiveness in different regions, including Germany, the United Kingdom, Canada, Spain, China, Saudi Arabia, and the Russian Federation, underlines the favourable economic profile of PCSK9 inhibitors, particularly evolocumab and alirocumab, in the context of cardiovascular risk management (Table 2) (32–39). Comparison with other lipid-lowering agents, including icosapent ethyl, fibrates, fenofibrate, and ezetimibe, consistently shows a more favourable cost–benefit ratio for PCSK9 inhibitors (32–39). These results suggest that the inclusion of evolocumab and alirocumab in treatment strategies not only holds promise for optimising clinical outcomes (CO) in high-risk cardiovascular patients, but is also consistent with cost-effective considerations, making them potentially valuable additions to therapeutic protocols.
Discussion
Drugs for the treatment of dyslipidaemia are among the most commonly used medicines. According to the National Ambulatory Medical Care Survey published by the Centres for Disease Control and Prevention in 2019, medications to treat dyslipidaemia were the second most frequently mentioned medications in primary care practices in the United States, surpassed only by analgesics, while atorvastatin was the second most frequently used prescription medication (40). For decades, statins were synonymous with the treatment of dyslipidaemia, but in recent years the new generation of lipid-lowering drugs has become more widely used as a result of new research findings and general awareness of the potential adverse effects of statins (although these are usually vastly overestimated). In second place in the treatment of dyslipidaemia are currently the PCSK9 inhibitors—alirocumab, evolocumab, and inclisiran, which is not strictly a PCSK9 inhibitor, but is often included in the same group of drugs. Numerous research papers have been published on the safety and efficacy of PCSK9 monoclonal antibodies, and all these papers have in common that they have demonstrated the efficacy in lipid lowering and the good safety profile of these drugs (41). Another important point that is often emphasised as a major advantage is their compliance, as they are administered once or twice a month. However, to date, no study has been published that demonstrates better compliance compared to standard daily oral statin treatment or combined treatment with statin + ezetimibe or bempedoic acid (42). In addition, recent results have confirmed the efficacy of PCSK9 inhibitors in reducing major cardiovascular events and have also shown the benefit of treatment with PCSK9 inhibitors in schematic stroke (43). Regarding the safety profile of PCSK9 inhibitors, most studies showed a very good safety profile; however, the targets were evaluated in the relatively short term so that potential long-term adverse effects could not yet be assessed. This brings us to the main problem in interpreting the previously published results on PCSK9 inhibition. In our study, we found that the number of published clinical trials is relatively low—106 compared to 62 meta-analyses—with new meta-analyses being published monthly, while there are currently only 76 active and recruiting clinical trials, based on the web source clinicaltrials.gov. Most trials focus on PCSK9 inhibition and serious cardiovascular events, but we can see a trend in pharmacology continuing in the lipid-lowering field—entirely new indications for PCSK9 inhibitors are being tested (44). On the other hand, published work to date has not yet shown promising results in patients with other risk factors for serious cardiovascular events, such as diabetes mellitus, chronic kidney disease, or other non-communicable diseases. The question might be: Have we jumped on the PCSK9 bandwagon too early? Why is there a sudden need for new potential indications for medications whose long-term side effects and interactions with the pathophysiology of other comorbidities are still unknown. Our patients not only have dyslipidaemia, but very often other risk factors that lead to serious cardiovascular events as well. One positive effect of the 21st century is the willingness of the medical community to publish real-world data on certain topics, and PCSK9 inhibition is no exception. There is an increasing number of publications based solely on real-world data confirming the results of clinical trials and meta-analyses of PCSK9 inhibitors (45–48).
An important issue that has not yet been mentioned is the cost-effectiveness of PCSK9 inhibitors. An important factor in treatment with PCSK9 inhibitors is their relatively high cost. The initial cost–benefit analyses all agreed that PCSK9 inhibitor therapy is not cost-effective, with reports ranging from developed countries to developing countries (49–51). Nevertheless, the price of evolocumab and alirocumab has fallen in recent years (52). However, even with this price reduction, some cost-effectiveness analyses have not shown positive results for the general use of PCSK9 inhibition. One of the most recent published analyses from the UK showed quality-adjusted life years (QALY) of 0.53 and 0.86 for evolocumab and alirocumab, respectively, at a cost of approximately £45,000. With a National Health Service willingness to pay £30,000/QALY, PCSK9 inhibitors do not appear to be cost-effective (33, 53). On the other hand, a Swedish analysis showed that PCSK9 inhibitors are cost-effective in the secondary prevention of myocardial infarction in combination therapy for very high-risk patients (54).
Conclusion
When we talk about PCSK9 inhibitors, we must all agree that they represent a revolutionary solution for lowering LDL cholesterol that the medical community awaited for decades after the introduction of statins. Finally, we now have clinical trial results and real-world data confirming the efficacy of the treatment regimen and the safety profile of evolocumab and alirocumab. For other novel treatment options based on PCSK9 inhibition, studies demonstrating the potential cardiovascular benefit or real-world data are still lacking. It must be mentioned that these new drugs are also expensive. When we talk about the costs and expenses of evolocumab and alirocumab, we can safely say that the cost-effectiveness of PSCK9 inhibitors is still very controversial, and the interpretation of the analysis results depends on the thresholds of the statutory health insurance funds. However, their benefit in high-risk patients is absolutely clear, regardless of the costs.
Author contributions
IM: Writing – review & editing. DS: Writing – original draft. PH: Writing – original draft. IP: Writing – review & editing. ŽR: Writing – review & editing.
Funding
The authors declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: executive summary. J Am Coll Cardiol. (2019) 73(24):3168–209. doi: 10.1016/j.jacc.2018.11.002
2. Teo KK, Rafiq T. Cardiovascular risk factors and prevention: a perspective from developing countries. Can J Cardiol. (2021) 37(5):733–43. doi: 10.1016/j.cjca.2021.02.009
3. Fredrickson DS, Lees RS. Editorial—a system for phenotyping hyperlipoproteinemia. Circulation. (1965) 31(3):321–7. doi: 10.1161/01.CIR.31.3.321
4. Chait A, Brunzell JD. Acquired hyperlipidemia (secondary dyslipoproteinemias). Endocrinol Metab Clin North Am. (1990) 19(2):259–78. doi: 10.1016/S0889-8529(18)30324-4
5. Merćep I, Strikić D, Slišković AM, Reiner Ž. New therapeutic approaches in treatment of dyslipidaemia—a narrative review. Pharmaceuticals. (2022) 15(7):839. doi: 10.3390/ph15070839
6. Merćep I, Friščić N, Strikić D, Reiner Ž. Advantages and disadvantages of inclisiran: a small interfering ribonucleic acid molecule targeting PCSK9—a narrative review. Cardiovasc Ther. (2022) 2022:1–6. doi: 10.1155/2022/8129513
7. Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. (2020) 41(1):111–88. doi: 10.1093/eurheartj/ehz455
8. Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Atherosclerosis. (2019) 290:140–205. doi: 10.1016/j.atherosclerosis.2019.08.014
9. Bytyçi I, Penson PE, Mikhailidis DP, Wong ND, Hernandez AV, Sahebkar A, et al. Prevalence of statin intolerance: a meta-analysis. Eur Heart J. (2022) 43(34):3213–23. doi: 10.1093/eurheartj/ehac015
10. Choi HD, Kim JH. An updated meta-analysis for safety evaluation of alirocumab and evolocumab as PCSK9 inhibitors. Cardiovasc Ther. (2023) 2023:1–11. doi: 10.1155/2023/7362551
11. Beltran RA, Zemeir KJ, Kimberling CR, Kneer MS, Mifflin MD, Broderick TL. Is a PCSK9 inhibitor right for your patient? A review of treatment data for individualized therapy. Int J Environ Res Public Health. (2022) 19(24):16899. doi: 10.3390/ijerph192416899
12. Liang D, Li C, Tu Y, Li Z, Zhang M. Additive effects of ezetimibe, evolocumab, and alirocumab on plaque burden and lipid content as assessed by intravascular ultrasound: a PRISMA-compliant meta-analysis. Medicine (Baltimore). (2022) 101(41):e31199. doi: 10.1097/MD.0000000000031199
13. Li J, Du H, Wang Y, Aertgeerts B, Guyatt G, Hao Q, et al. Safety of proprotein convertase subtilisin/kexin 9 inhibitors: a systematic review and meta-analysis. Heart. (2022) 108(16):1296–302. doi: 10.1136/heartjnl-2021-320556
14. Ge X, Zhu T, Zeng H, Yu X, Li J, Xie S, et al. A systematic review and meta-analysis of therapeutic efficacy and safety of alirocumab and evolocumab on familial hypercholesterolemia. Biomed Res Int. (2021) 2021:1–16. doi: 10.1155/2021/8032978
15. Geng Q, Li X, Sun Q, Wang Z. Efficacy and safety of PCSK9 inhibition in cardiovascular disease: a meta-analysis of 45 randomized controlled trials. Cardiol J. (2022) 29(4):574–81. doi: 10.5603/CJ.a2021.0110
16. Mahmood T, Minnier J, Ito MK, Li QH, Koren A, Kam IW, et al. Discordant responses of plasma low-density lipoprotein cholesterol and lipoprotein(a) to alirocumab: a pooled analysis from 10 ODYSSEY phase 3 studies. Eur J Prev Cardiol. (2021) 28(8):816–22. doi: 10.1177/2047487320915803
17. Sanz-Cuesta BE, Saver JL. Lipid-lowering therapy and hemorrhagic stroke risk. Stroke. (2021) 52(10):3142–50. doi: 10.1161/STROKEAHA.121.034576
18. Qin J, Liu L, Su XD, Wang BB, Fu BS, Cui JZ, et al. The effect of PCSK9 inhibitors on brain stroke prevention: a systematic review and meta-analysis. Nutr Metab Cardiovasc Dis. (2021) 31(8):2234–43. doi: 10.1016/j.numecd.2021.03.026
19. Farmakis I, Doundoulakis I, Pagiantza A, Zafeiropoulos S, Antza C, Karvounis H, et al. Lipoprotein(a) reduction with proprotein convertase subtilisin/kexin type 9 inhibitors: a systematic review and meta-analysis. J Cardiovasc Pharmacol. (2021) 77(3):397–407. doi: 10.1097/FJC.0000000000000963
20. Zhao Z, Hu X, Zhang Y, Liu D. Cardiovascular and safety events of PCSK9 inhibitors in statin-treated patients with cardiovascular risk: a systematic review and meta-analysis. J Pharm Pharm Sci. (2020) 23:422–36. doi: 10.18433/jpps31197
21. Schmidt AF, Pearce LS, Wilkins JT, Overington JP, Hingorani A, Casas JP. “PCSK9 monoclonal antibodies for the primary and secondary prevention of cardiovascular disease”. In: Casas JP, editor. Cochrane Database of Systematic Reviews. Chichester, UK: John Wiley & Sons, Ltd. (2020).
22. Benhuri B, Ueyama H, Takagi H, Briasoulis A, Kuno T. PCSK9 inhibitors and ezetimibe monotherapy in patients not receiving statins: a meta-analysis of randomized trials. Curr Vasc Pharmacol. (2021) 19(4):390–7. doi: 10.2174/1570161118666200807114559
23. van Bruggen FH, Nijhuis GBJ, Zuidema SU, Luijendijk H. Serious adverse events and deaths in PCSK9 inhibitor trials reported on ClinicalTrials.gov: a systematic review. Expert Rev Clin Pharmacol. (2020) 13(7):787–96. doi: 10.1080/17512433.2020.1787832
24. Masson W, Lobo M, Siniawski D, Molinero G, Masson G, Huerín M, et al. Role of non-statin lipid-lowering therapy in coronary atherosclerosis regression: a meta-analysis and meta-regression. Lipids Health Dis. (2020) 19(1):111. doi: 10.1186/s12944-020-01297-5
25. Chiu SW, Pratt CM, Feinn R, Chatterjee S. Proprotein convertase subtilisin/kexin type 9 inhibitors and ezetimibe on risk of new-onset diabetes: a systematic review and meta-analysis of large, double-blinded randomized controlled trials. J Cardiovasc Pharmacol Ther. (2020) 25(5):409–17. doi: 10.1177/1074248420924983
26. Guedeney P, Sorrentino S, Giustino G, Chapelle C, Laporte S, Claessen BE, et al. Indirect comparison of the efficacy and safety of alirocumab and evolocumab: a systematic review and network meta-analysis. Eur Heart J Cardiovasc Pharmacother. (2021) 7(3):225–35. doi: 10.1093/ehjcvp/pvaa024
27. Marston NA, Gurmu Y, Melloni GEM, Bonaca M, Gencer B, Sever PS, et al. The effect of PCSK9 (proprotein convertase subtilisin/kexin type 9) inhibition on the risk of venous thromboembolism. Circulation. (2020) 141(20):1600–7. doi: 10.1161/CIRCULATIONAHA.120.046397
28. Salvatore T, Morganti R, Marchioli R, De Caterina R. Cholesterol lowering and stroke: no longer room for pleiotropic effects of statins—confirmation from PCSK9 inhibitor studies. Am J Med. (2020) 133(1):95–9.e6. doi: 10.1016/j.amjmed.2019.06.029
29. Wang S, Xiu J, Liao W, Liao Y, Bin J. Relative effect of current intensive lipid-lowering drugs on cardiovascular outcomes in secondary prevention—a meta-analysis of 12 randomized trials. Circ J. (2019) 83(6):1356–67. doi: 10.1253/circj.CJ-18-1321
30. Masson W, Lobo M, Huerín M, Molinero G, Lobo L, Nogueira JP. Inhibidores de la proproteína convertasa plasmática subtilisina kexina tipo 9 y riesgo de cataratas: revisión sistemática y metaanálisis. Arch Soc Esp Oftalmol. (2019) 94(2):75–80. doi: 10.1016/j.oftal.2018.11.003
31. de Carvalho LSF, Campos AM, Sposito AC. Proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors and incident type 2 diabetes: a systematic review and meta-analysis with over 96,000 patient-years. Diabetes Care. (2018) 41(2):364–7. doi: 10.2337/dc17-1464
32. Michaeli DT, Michaeli JC, Boch T, Michaeli T. Cost-effectiveness of lipid-lowering therapies for cardiovascular prevention in Germany. Cardiovasc Drugs Ther. (2023) 37(4):683–94. doi: 10.1007/s10557-021-07310-y
33. Michaeli DT, Michaeli JC, Boch T, Michaeli T. Cost-effectiveness of icosapent ethyl, evolocumab, alirocumab, ezetimibe, or fenofibrate in combination with statins compared to statin monotherapy. Clin Drug Investig. (2022) 42(8):643–56. doi: 10.1007/s40261-022-01173-3
34. Grégoire J, Champsi S, Jobin M, Martinez L, Urbich M, Rogoza RM. Cost-effectiveness analysis of evolocumab in adult patients with atherosclerotic cardiovascular disease in Canada. Adv Ther. (2022) 39(7):3262–79. doi: 10.1007/s12325-022-02130-4
35. Imedio Cerezo B. Cost-effectiveness and cost-utility study of hypercholesterolemia treatment in Spain: evolocumab added to standard of care vs standard of care (2022). Available online at: http://hdl.handle.net/10230/52487 (accessed June 27, 2023).
36. Xie W, Song Y, Qin X, Jin P. Cost-effectiveness of evolocumab in adult patients with atherosclerotic cardiovascular disease from Chinese healthcare perspective. Adv Ther. (2023) 40(2):489–503. doi: 10.1007/s12325-022-02372-2
37. Xi X, Wang X, Xie W, Jia Y, Sanchez SZ, Martinez L, et al. Comparison of evolocumab and ezetimibe, both combined with statin therapy, for patients with recent acute coronary syndrome: a cost-effectiveness analysis from the Chinese healthcare perspective. Cardiovasc Drugs Ther. (2023) 37(5):905–16. doi: 10.1007/s10557-021-07276-x
38. Alghamdi A, Balkhi B, Altowaijri A, Al-shehri N, Ralph L, Marriott ER, et al. Cost-effectiveness analysis of evolocumab for the treatment of dyslipidemia in the Kingdom of Saudi Arabia. Pharmacoecon Open. (2022) 6(2):277–91. doi: 10.1007/s41669-021-00300-8
39. Bessonova TO, Mukhortova PA, Teryan RA, Bagdasarov AD, Musina NZ. Cost-effectiveness analysis of using atorvastatin, simvastatin, ezetimibe, alirocumab, evolocumab, inclisiran in adults with very high cardiovascular risk under the preferential drug provision program. FARMAKOEKONOMIKA. (2023) 16(1):17–34. doi: 10.17749/2070-4909/farmakoekonomika.2023.173
40. National Ambulatory Medical Care Survey: 2019 National Summary [Internet]. Available online at: https://www.cdc.gov/nchs/data/ahcd/namcs_summary/2019-namcs-web-tables-508.pdf (Accessed March 11, 2023).
41. Diaz R, Li QH, Bhatt DL, Bittner VA, Baccara-Dinet MT, Goodman SG, et al. Intensity of statin treatment after acute coronary syndrome, residual risk, and its modification by alirocumab: insights from the ODYSSEY OUTCOMES trial. Eur J Prev Cardiol. (2021) 28(1):33–43. doi: 10.1177/2047487320941987
42. Banach M, Penson PE, Farnier M, Fras Z, Latkovskis G, Laufs U, et al. Bempedoic acid in the management of lipid disorders and cardiovascular risk. 2023 position paper of the international lipid expert panel (ILEP). Prog Cardiovasc Dis. (2023) 79:2–11. doi: 10.1016/j.pcad.2023.03.001
43. Jukema JW, Zijlstra LE, Bhatt DL, Bittner VA, Diaz R, Drexel H, et al. Effect of alirocumab on stroke in ODYSSEY OUTCOMES. Circulation. (2019) 140(25):2054–62. doi: 10.1161/CIRCULATIONAHA.119.043826
44. Khademi F, Momtazi-borojeni AA, Reiner Ž, Banach M, Al-Rasadi KA, Sahebkar A. PCSK9 and infection: a potentially useful or dangerous association? J Cell Physiol. (2018) 233(4):2920–7. doi: 10.1002/jcp.26040
45. Gürgöze MT, Muller-Hansma AHG, Schreuder MM, Galema-Boers AMH, Boersma E, Roeters van Lennep JE. Adverse events associated with PCSK9 inhibitors: a real-world experience. Clin Pharmacol Ther. (2019) 105(2):496–504. doi: 10.1002/cpt.1193
46. Altschmiedová T, Todorovová V, Šnejdrlová M, Šatný M, Češka R. PCSK9 Inhibitors in real-world practice: analysis of data from 314 patients and 2 years of experience in a center of preventive cardiology. Curr Atheroscler Rep. (2022) 24(5):357–63. doi: 10.1007/s11883-022-01008-8
47. Uno-Eder K. Challenges with PCSK9 inhibitors use in Asia given real-world data implications. J Atheroscler Thromb. (2023) 30(9):1106–7. doi: 10.5551/jat.ED230
48. Zamora A, Masana L, Comas-Cufi M, Plana N, Vila À, García-Gil M, et al. Number of patients eligible for PCSK9 inhibitors based on real-world data from 2.5 million patients. Rev Esp Cardiol (Engl Ed). (2018) 71(12):1010–7. doi: 10.1016/j.rec.2018.03.003
49. Arrieta A, Hong JC, Khera R, Virani SS, Krumholz HM, Nasir K. Updated cost-effectiveness assessments of PCSK9 inhibitors from the perspectives of the health system and private payers. JAMA Cardiol. (2017) 2(12):1369. doi: 10.1001/jamacardio.2017.3655
50. Kodera S, Kiyosue A, Ando J, Akazawa H, Morita H, Watanabe M, et al. Cost-effectiveness analysis of cardiovascular disease treatment in Japan. Int Heart J. (2017) 58(6):847–52. doi: 10.1536/ihj.17-365
51. Civeira F, Pedro-Botet J. Cost-effectiveness evaluation of the use of PCSK9 inhibitors. Endocrinol Diabetes Nutr (Engl Ed). (2021) 68(6):369–71. doi: 10.1016/j.endien.2021.05.003
52. Pagliarulo N. Regeneron, Sanofi Cut PCSK9 List Price, Matching Earlier Move by Rival Amgen. Available online at: https://www.biopharmadive.com/news/regeneron-sanofi-cut-pcsk9-list-price-matching-earlier-move-by-rival-amge/548147/ (Accessed April 28, 2023).
53. Michaeli DT, Michaeli JC, Boch T, Michaeli T. Cost-effectiveness of cholesterol-lowering drugs for secondary cardiovascular prevention in the UK: ezetimibe, evolocumab, and alirocumab. Eur Heart J. (2022) 42(8):643–56. doi: 10.1093/eurheartj/ehac544.2367
54. Landmesser U, Lindgren P, Hagström E, van Hout B, Villa G, Pemberton-Ross P, et al. Cost-effectiveness of proprotein convertase subtilisin/kexin type 9 inhibition with evolocumab in patients with a history of myocardial infarction in Sweden. Eur Heart J Qual Care Clin Outcomes. (2022) 8(1):31–8. doi: 10.1093/ehjqcco/qcaa072
Keywords: PCSK9 inhibitors, cost-effectiveness, cardiovascular disease, dyslipidaemia treatment, statins
Citation: Mercep I, Strikic D, Hrabac P, Pecin I and Reiner Ž (2024) PCSK9 inhibition: from effectiveness to cost-effectiveness. Front. Cardiovasc. Med. 11:1339487. doi: 10.3389/fcvm.2024.1339487
Received: 16 November 2023; Accepted: 6 June 2024;
Published: 25 June 2024.
Edited by:
Mohamad Navab, UCLA Health System, United States© 2024 Mercep, Strikic, Hrabac, Pecin and Reiner. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dominik Strikic, c3RyaWtpYy5kb21pbmlrQGdtYWlsLmNvbQ==
 Iveta Mercep
Iveta Mercep Dominik Strikic
Dominik Strikic Pero Hrabac3
Pero Hrabac3 Željko Reiner
Željko Reiner