- Department of Cardiology, The Affiliated Hospital of Qingdao University, Qingdao, Shandong, China
Objective: Assessing the impact of lumbar disc herniation (LDH) on the plaque burden of coronary atherosclerosis is our objective.
Methods: In this study, a total of 212 patients (age 46–80 years) with unstable angina (UA) who underwent coronary angiography (CAG) in our hospital from January 2018 to July 2022 due to UA were included. Patients were divided into LDH group (n = 106) and no LDH group (n = 106). Gensini scores were calculated to assess the plaque burden of coronary. Logistic analysis was used to examine potential risk variables linked to the Gensini score. The association between lumbar disc lesions grading and coronary plaque burden was analysed by Spearman's correlation test. LDH patients with higher plaque burden (n = 56) were further divided into evolocumab treatment group (n = 28) and conventional treatment group (n = 28). Cox regression analysis were performed.
Results: Patients with LDH had higher Gensini scores (P < 0.01) and triglyceride (TG) levels (P = 0.04), but HDL-C (P = 0.01) levels were lower. LDH was found to be an independent risk factor for higher Gensini scores (OR = 2.38, P < 0.01) by logistic analysis. The Spearman's correlation test suggested that the degree of lumbar disc lesions was related to the Gensini score and the level of blood lipid. Cox regression analysis showed that evolocumab treatment could significantly reduce the composite MACE events (cardiac death, nonfatal myocardial infarction, nonfatal stroke, and readmission due to angina) (HR = 0.26, P = 0.04) in higher coronary plaque burden patients.
Conclusion: LDH is an independent risk factor for the higher coronary plaque burden. Evolocumab treatment significantly reduced the occurrence of cardiovascular events in LDH patients with higher plaque burden. Additionally, our data indicate that LDH is associated with increased blood lipid, which may contribute to the development of plaque burden.
1 Introduction
The relationship between lumbar disc herniation (LDH) and atherosclerosis has attracted increasing attention in recent years (1). Previous studies have shown that cardiovascular risk factors, particularly smoking, are significantly and independently associated with symptomatic LDH (2). Moreover, Yang et al. (3) demonstrated that the prevalence of cardiovascular risks (evaluated by checking the presence of metabolic syndrome) in patients with degenerative lumbar spinal disease was relatively higher compared to that in the general population. Moreover, Zhu et al. (4) found that frequent back pain (n = 39, 10.3% vs. n = 42, 5.9%, HR = 1.78) and daily back pain (n = 34, 11.8% vs. n = 42, 5.9%, HR = 2.13) were related to higher risk of coronary heart event compared to infrequent back pain. According to the research of Beckworth et al. (5), lumbar disc degeneration is related to higher prevalence of aortic atherosclerosis (n = 11, 22.45% vs. n = 62, 87.32%, P < 0.01) and severe aortic atherosclerosis (n = 4, 8.16% vs. n = 58, 81.69%, P < 0.01).
Recently, many cardiovascular risk factors were found to be related to the coronary plaque burden. Yang et al. (6) indicated that high-risk plaques were more common in patients with metabolic syndrome. Systemic lupus erythematosus (7) and severe obstructive sleep apnea (8) were also found to be associated with significant coronary artery plaque burden. Unfortunately, there are still no studies about the relationship between LDH and the plaque burden of coronary artery. To address this issue, the main goal of the present study was to evaluate the relationship between LDH and plaque burden in unstable angina (UA) patients.
2 Methods
2.1 Definitions
UA was defined based on 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain (9). LDH was defined as the displacement of the nucleus pulposus of the intervertebral disc through the annulus fibrosus, thereby causing pressure on the neural elements (10). The diagnosis methods including symptoms (back pain and associated leg symptoms), physical examination (the straight leg raise test, the contralateral straight leg raise test, the femoral nerve stretch test, and the bowstring sign) and MRI. The diagnosis of LDH was made by professional spinal surgeons. All patients included in the LDH group have two years or more history of lumbar disc herniation. Gensini score (11) is a widely used angiographic scoring system for quantifying the severity of cardiovascular atherosclerotic disease. We used Gensini score to evaluate coronary plaque burden in our study. The Pfirrmann grading system (12) and the grading system of migrated lumbar disc herniation (13) are both systems for grading the degree of lumbar disc lesions of patients according to the patients' lumbar MRI image. We used the two grading systems to evaluate the degree of LDH in our study. Evolocumab treatment was defined as receiving 140 mg of evolocumab once every two weeks or 420 mg of evolocumab once a month for at least six months. Dyslipidaemia was defined based on 2019 ESC/EAS Guidelines for the management of dyslipidaemias (14). End-stage heart failure was defined as New York Heart Association class III-IV, despite optimal medical and device therapy, intolerance or withdrawal of evidence-based heart failure medications such as beta blockers, angiotensin converting enzyme inhibitors due to hypotension, diuretic-refractory volume overload, or need for intravenous inotrope. Severe hepatic dysfunction was defined as an increase in bilirubin that exceeded 10 times the normal value, prothrombin activity < 40%, or the presence of hepatic encephalopathy. Severe renal insufficiency is defined as estimated glomerular filtration rate less than 30 ml/min·1.73 m2.
2.2 Study population
The study was approved by the Affiliated Hospital of Qingdao University research ethics committee (No: QYFYWZLL28122), and all patients gave written informed consent to participate. Present study enrolled 212 UA patients (aged 46–80 years). First, we consecutively enrolled patients with UA and LDH, who were hospitalized in our hospital between January 2018 and July 2022 and underwent coronary angiography (CAG) to LDH group (n = 106). Then, no LDH group (n = 106) was matched for age, sex and BMI, consisted of UA patients, who were hospitalized in our hospital between January 2018 and July 2022 and underwent CAG. All patients received standard medical therapy. Patients in LDH group who received evolocumab treatment were included in the evolocumab treatment group (n = 28), and patients in LDH group who did not receive evolocumab treatment were matched into the conventional treatment group (n = 28) based on Gensini score and baseline low-density lipoprotein cholesterol level. All patients included in the evolocumab treatment group and conventional treatment group received basic statin treatment and their Gensini scores were higher than the first tertile of the LDH group.The rest of the treatment drugs were used in accordance with the current guidelines, and there were no potential differences in medical therapy between the two groups. Exclusion criteria were as follows: (1) age more than 80 years, (2) a history of revascularization, (3) end-stage heart failure, (4) a history of myocardial infarction, and (5) severe liver and kidney dysfunction. Figure 1, shows the study flowchart.
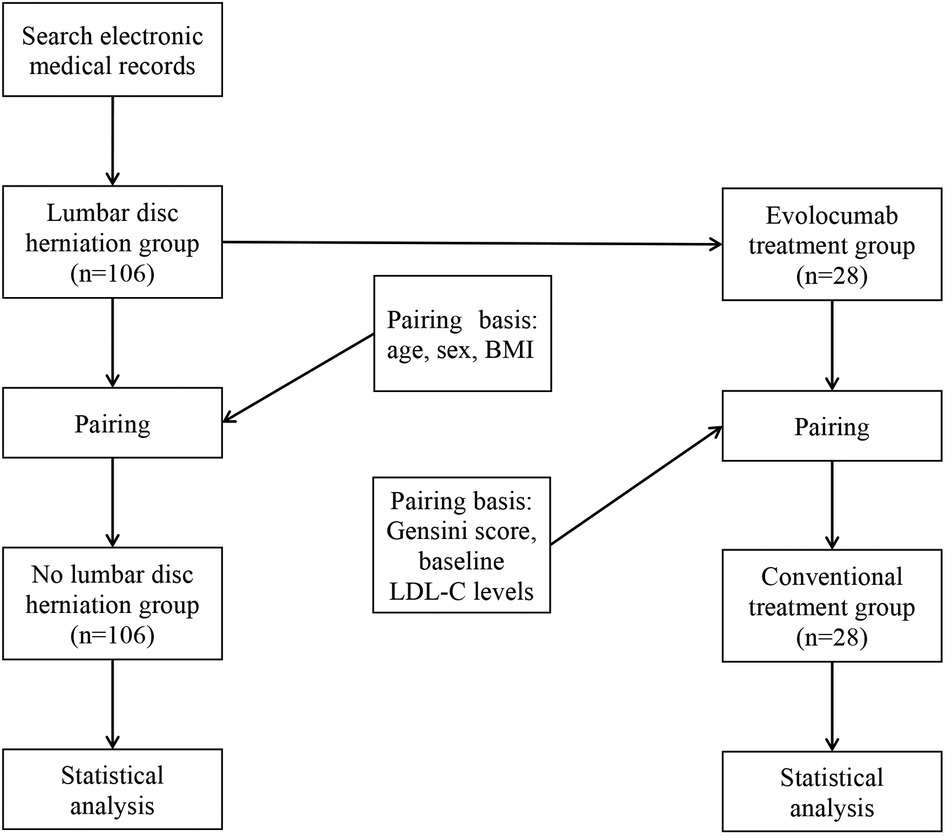
Figure 1. Study flowchart. BMI, weight and body mass index; LDL-C, low-density lipoprotein cholesterol.
2.3 PCSK9 inhibitor treatment
LDL receptors play a role in the removal of circulating LDL-C from blood. When the PCSK9 protein binds to the LDL receptor, it starts the process of degrading the receptor, thus increasing LDL-C levels. The PCSK9 inhibitor inhibits PCSK9 binding to LDL receptors, increase recycling LDL receptors, and indirectly lower circulating LDL-C levels by increasing LDL-C uptake (15). For patients who have not achieved their lipid targets with statins in combination with ezetimibe, the latest ESC/EAS guidelines for the management of dyslipidaemia recommend advocating the use of PCSK9 inhibitor (14).
2.4 Study endpoint
The follow-up time for subgroup analysis was 1 year. End event was defined as major adverse cardiovascular events (MACEs) including cardiac death, nonfatal myocardial infarction, nonfatal stroke, and readmission due to angina.
2.5 Statistical processing
The characteristics of the patients are presented as the mean ± SD or interquartile range for continuous variables and were compared by paired Student's t test if the data were normally distributed; otherwise, the paired Wilcoxon signed rank test was used. Categorical variables are presented as percentages and were compared by Pearson's chi-square test. The association between lumbar disc lesions grading and coronary plaque burden was analysed by Spearman's correlation test. Age, sex and weight and body mass index (BMI) were control variables to expel their influence on the correlation coefficients. Clinical characteristics were all initially tested with univariate logistic analysis, and all variables with a P value < 0.1 were considered for inclusion in the multivariate model to investigate potential risk variables linked to higher Gensini score. Forest plots were drawn based on logistic analysis. Cox regression analysis and survival curve were used to evaluate the impact of the indicators on the outcomes of patients. All statistical tests were two-tailed, and P < 0.05 was considered to be statistically significant. All statistical analysis were carried out using the SPSS 26.0 software.
3 Results
3.1 Patients characteristics
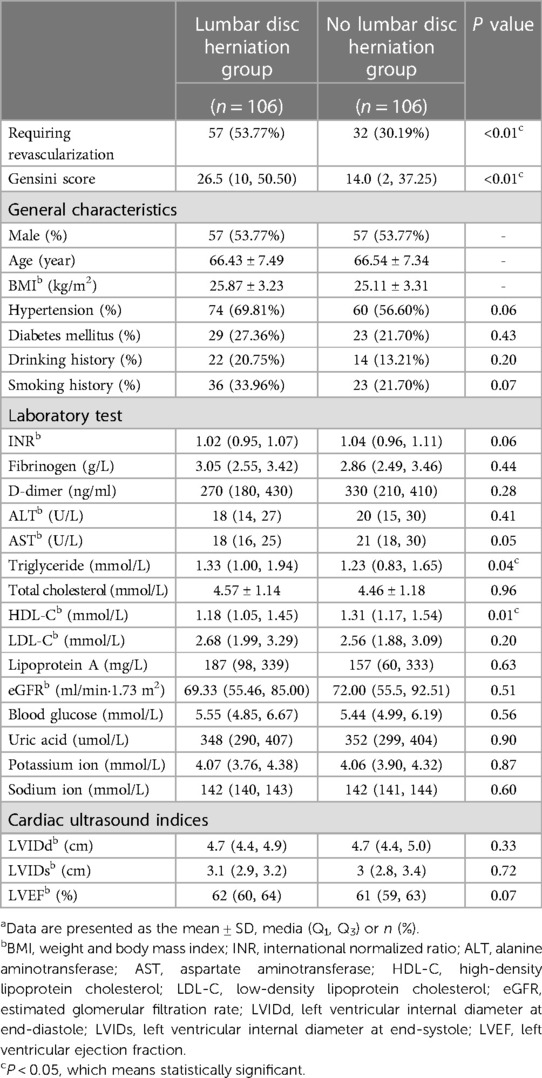
A total of 212 UA patients were assessed. Baseline clinical characteristics of patients are summarized in Table 1. General characteristics, total cholesterol, LDL-C, glucose, hepatic aminotransferases levels and cardiac ultrasound indices were similar between two groups.
As shown in Table 1, TG (median: 1.33 vs. 1.23 mmol/L, p = 0.04) levels were higher in the LDH group, while HDL-C (median: 1.18 vs. 1.31 mmol/L, p = 0.01) levels were lower. Our study suggested that the proportion of patients requiring coronary artery bypass graft surgery or percutaneous coronary intervention (57 vs. 32, p < 0.01) was higher in LDH group. The coronary plaque burden (median Gensini score: 26.5 vs. 14, p < 0.01) was also higher in LDH group.
Figure 2 showed with the increase of Gensini score (divided by tertiles), the proportion of LDH also increased (33.3%, 55.7%, 61.4%).
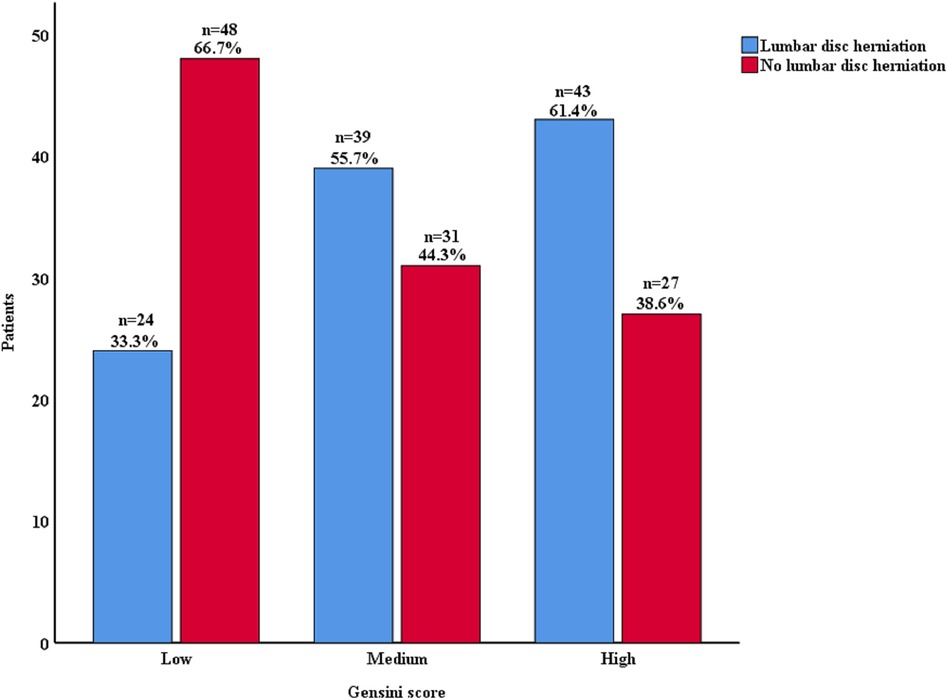
Figure 2. Lumbar disc herniation proportion according to Gensini score. Gensini score was divided by tertiles.
3.2 Logistic analysis
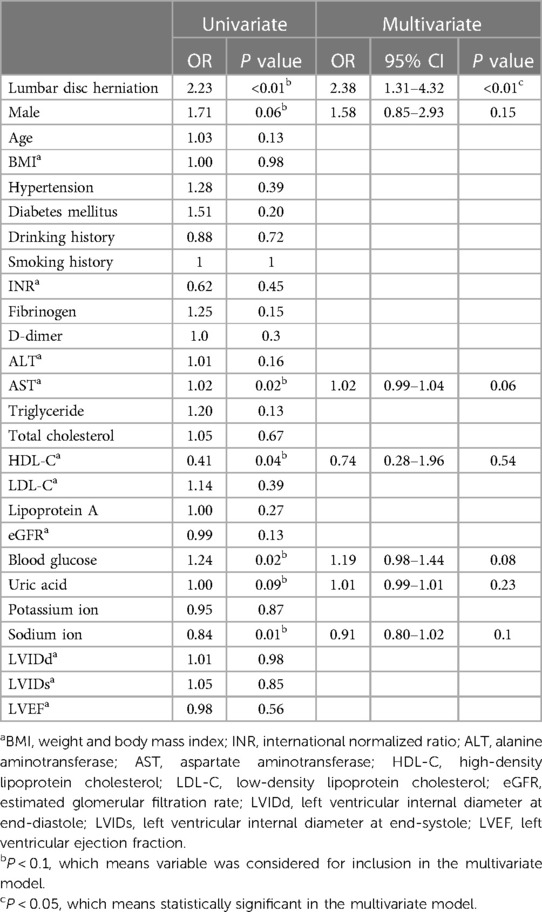
As shown in Table 2, Figures 3, 4, on multivariate model, LDH was found to be an independent risk factor for higher Gensini scores (OR = 2.38, 95% CI: 1.31–4.32, p < 0.01).
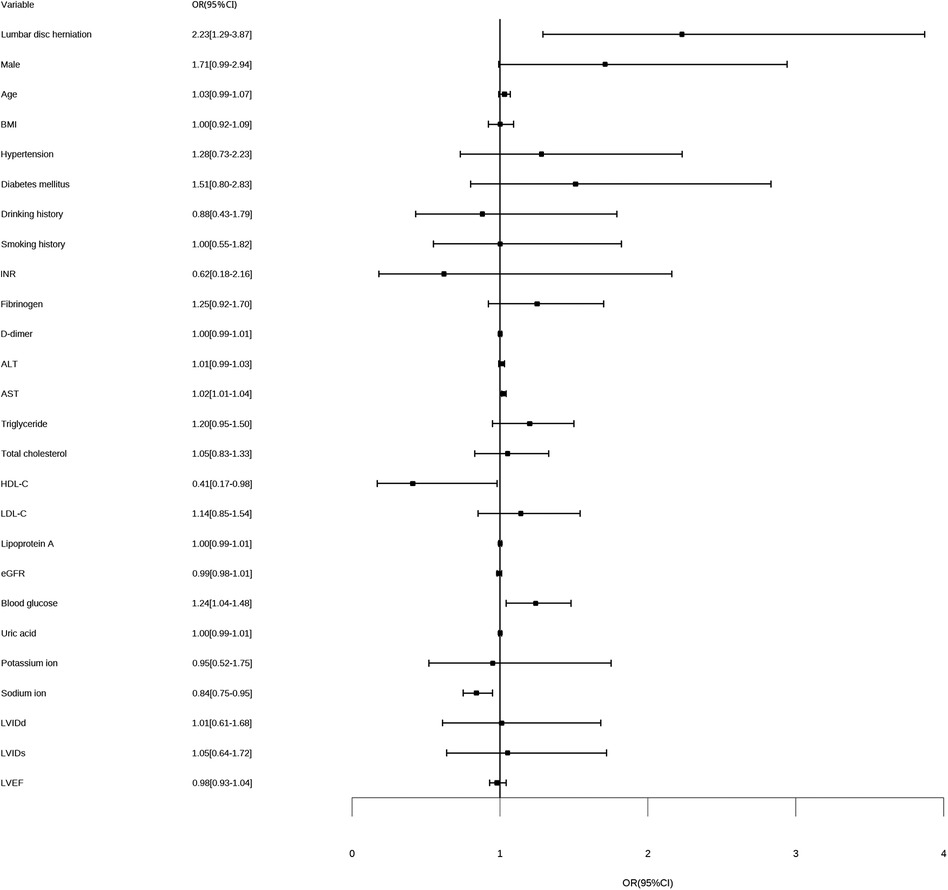
Figure 3. Forest plot for univariate logistic analysis. BMI, weight and body mass index; INR, international normalized ratio; ALT, alanine aminotransferase; AST, aspartate aminotransferase; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; eGFR, estimated glomerular filtration rate; LVIDd, left ventricular internal diameter at end-diastole; LVIDs, left ventricular internal diameter at end-systole; LVEF, left ventricular ejection fraction; OR, odds ratio for higher Gensini score.
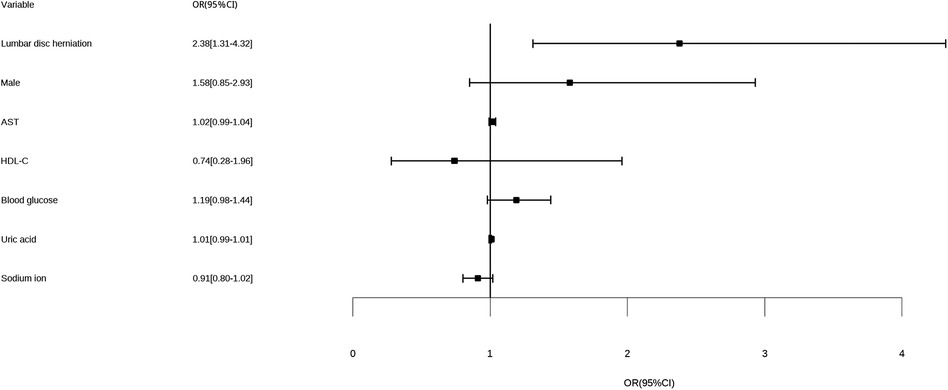
Figure 4. Forest plot for multivariate logistic analysis. AST, aspartate aminotransferase; HDL-C, high-density lipoprotein cholesterol; OR, odds ratio for higher Gensini score.
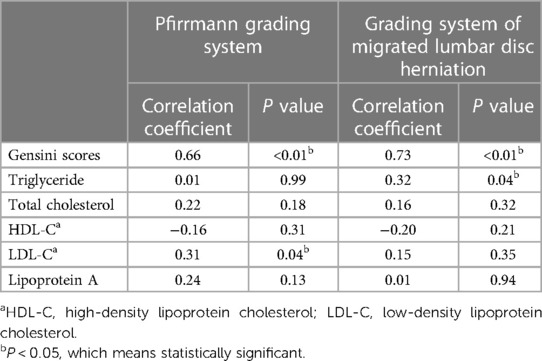
3.3 Correlation between the degree of lumbar disc lesions and blood lipid levels and Gensini score
Spearman's correlation test (Table 3) suggested that both the Pfirrmann grading system (correlation coefficient = 0.66, p < 0.01) and the grading system of migrated LDH (correlation coefficient = 0.73, p < 0.01) were positively correlated with the Gensini score. In addition, the Pfirrmann grading system was positively correlated with the LDL-C levels (correlation coefficient = 0.31, p = 0.04), while the grading system of migrated LDH was positively correlated with the TG levels (correlation coefficient = 0.32, p = 0.04).
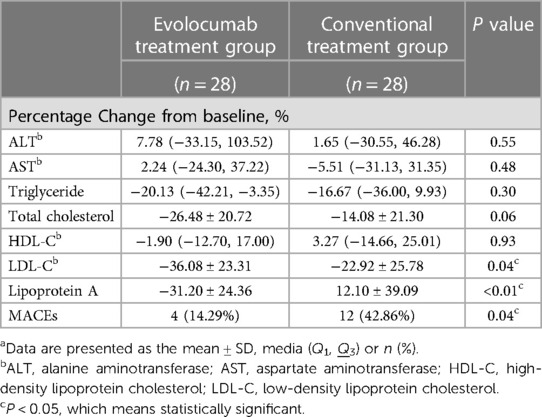
3.4 One year clinical outcomes
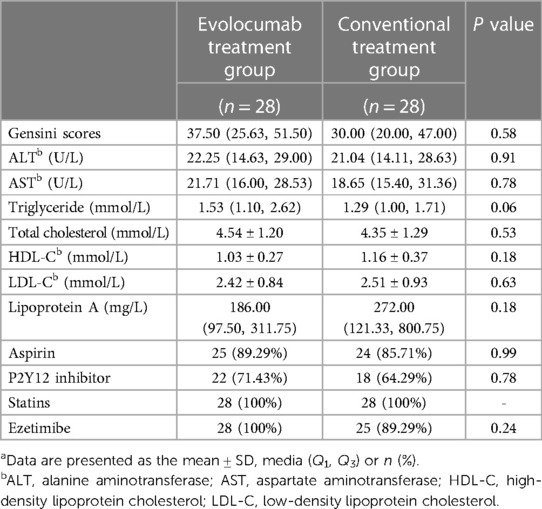
The baseline data of the 56 patients included in the evolocumab treatment group and the conventional treatment group were comparable (Table 4). As shown in Table 5, by 1-year follow-up, there were 42.86% (n = 12) composite MACEs in the conventional treatment group and 14.29% (n = 4) in the evolocumab treatment group (p = 0.04). The incidence of readmission due to angina, underwent nonfatal myocardial infarction, underwent nonfatal stroke, mortality were 21.42% (n = 6), 10.71% (n = 3), 7.14% (n = 2) and 3.57% (n = 1) in the conventional treatment group and 7.14% (n = 2), 3.57% (n = 1), 3.57% (n = 1) and 0% (n = 0) respectively in the evolocumab treatment group (all p > 0.05).
3.5 Subgroup analysis
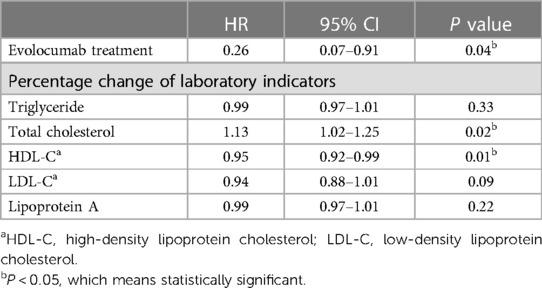
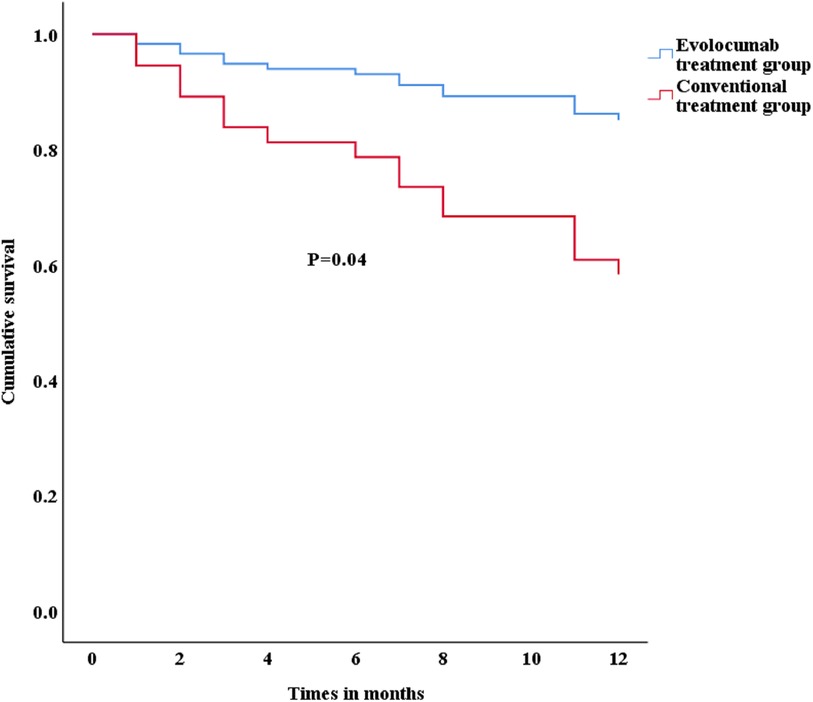
As shown in Table 5, the evolocumab treatment group presented significant reductions in LDL-C (mean: –36.08% VS. −22.92%, p = 0.04) and lipoprotein A (mean: −31.2% VS. 12.1%, p < 0.01). In addition, as shown in Table 6, the evolocumab treatment (HR = 0.26, 95%CI: 0.07–0.91, p = 0.04) significantly influenced the occurrence of MACEs, according to Cox regression analysis. The adjusted survival curve for Cox Proportional Hazards model (Figure 5) showed that patients treated with evolocumab had a better prognosis than those receiving conventional treatment.
4 Discussion
To our best knowledge, this is the first clinical research demonstrated that LDH remained as independent risk factor for coronary plaque burden. Moreover, evolocumab treatment significantly reduced the occurrence of MACEs in LDH patients with higher coronary plaque burden, suggesting LDH increases coronary plaque burden by affecting blood lipid. Although the pathophysiological mechanism is unclear, our data indicate a potential relationship between LDH and coronary plaque burden in UA patients.
4.1 Cardiovascular risk factors related to lumbar disc disease
The relationship between cardiovascular risk factors and LDH or degenerative lumbar disc disease attracted increasing attention in recent years. Colombini et al. (16) demonstrated that smoking was correlated with the prevalence of discopathies, osteochondrosis and both associated with LDH. Moreover, Steelman et al. (17) indicated the association between smoking and the development of degenerative disc disease. In addition, Rivinoja et al. (18) found that smoking during adolescence was correlated with hospitalization due to low back pain or sciatica, suggesting smoking as a predictor of LDH. Similar to the previous studies (5), our study indicated the prevelance of positive CAG results (57 vs. 32, p < 0.01) was higher in LDH patients. Moreover, our study found that the coronary plaque burden (median Gensini score: 26.5 vs. 14.0, p < 0.01) was also higher in LDH group.
4.2 Risk factors related to higher coronary plaque burden
Given the important role of coronary plaque burden in atherosclerotic cardiovascular disease risk stratification and management (19), the risk factors related to coronary plaque burden attracted increasing attention in recent years. Won et al. (20) suggested that serum hemoglobin level changes has an independent effect on coronary plaque volume. Akin et al. (21) indicated the coronary plaque burden was positively correlated with non-HDL-C and TG/HDL-C ratio. Moreover, Nafakhi et al. (22) demonstrated that pericardial fat volume independently associated with coronary atherosclerosis burden.
In our study, patients with LDH showed higher TG levels and Gensini scores and lower HDL-C levels. The result suggests LDH as a risk factor for higher coronary plaque burden. We hypothesis LDH increases coronary plaque burden by affecting blood lipid.
4.3 Impact of blood lipid levels on outcome
Previous studies by Yuan et al. (23) and Huang et al. (24) have shown that hyperlipidaemia is a risk factor for intervertebral disc degeneration. A study (25) that included 790 patients showed that total cholesterol levels, LDL-C levels, and TG levels were higher in patients with LDH. This may be related to blood lipids directly interfering with the death by pyroptosis of nucleus pulposus cells and damaging extracellular matrix metabolism (26). The latest ESC/EAS guidelines for the management of dyslipidaemias (14) have emphasized the importance of lipid-lowering treatment in reducing cardiovascular risk. Nelson et al. (27) and Nicholls et al. (28) demonstrated that evolocumab treatment can produce coronary plaque stabilization and regression. In this cohort, our results showed that evolocumab treatment significantly reduced occurrence of MACEs in the patients with higher plaque burden. Moreover, our data indicated that LDH is associated with increased blood lipid, which may contribute to the development of plaque burden.
4.4 Research significance
Our findings suggested that LDH was an independent risk factor for higher plaque burden in coronary, and blood lipid might play a key role. In LDH patients, controlling cardiovascular risk factors, especially blood lipid, is necessary to avoid coronary atherosclerosis. When considering surgery treatment in patients with LDH, comprehensive assessment of cardiovascular risk is required to avoid cardiovascular events in perioperative period.
4.5 Conclusion
LDH is an independent risk factor for the higher coronary plaque burden. Evolocumab treatment significantly reduces the occurrence of cardiovascular events in LDH patients with higher plaque burden. Our research suggests that LDH increases coronary plaque burden by affecting blood lipid.
4.6 Limitations
The current study has several limitations. First, it is a retrospective and observational study that could be skewed by confounding variables. Unmeasured factors could not be examined, although we looked at various aspects that potentially influence prognosis. Second, coronary plaque burden was evaluated by CAG, rather than intravascular ultrasound or optical coherence tomography. Due to the limitations of this trial, multicenter, large-sample clinical research is still needed.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Affiliated Hospital of Qingdao University research Ethics Committee. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
YW: Writing – original draft. JG: Writing – review & editing. HX: Writing – original draft. JL: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
This work was supported by Natural Science Foundation of Shandong Province (ZR2023MH083).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Kauppila L. Atherosclerosis and disc degeneration/low-back pain–a systematic review. Eur J Vasc Endovasc Surg. (2009) 37(6):661–70. doi: 10.1016/j.ejvs.2009.02.006
2. Jhawar B, Fuchs C, Colditz G, Stampfer M. Cardiovascular risk factors for physician-diagnosed lumbar disc herniation. Spine J. (2006) 6(6):684–91. doi: 10.1016/j.spinee.2006.04.016
3. Yang J, Lee B, Eum K, Suk K, Park J, Kim H, et al. Prevalence of gastrointestinal and cardiovascular risk in patients with degenerative lumbar spinal disease. Clin Orthop Surg. (2020) 12(3):343–52. doi: 10.4055/cios20021
4. Zhu K, Devine A, Dick IM, Prince RL. Association of back pain frequency with mortality, coronary heart events, mobility, and quality of life in elderly women. Spine (Phila Pa 1976). (2007) 32(18):2012–8. doi: 10.1097/BRS.0b013e318133fb82
5. Beckworth W, Holbrook J, Foster L, Ward L, Welle J. Atherosclerotic disease and its relationship to lumbar degenerative disk disease, facet arthritis, and stenosis with computed tomography angiography. PM & R. (2018) 10(4):331–7. doi: 10.1016/j.pmrj.2017.09.004
6. Yang X, Luo W, Han S, Zha L, Zhang J, Li X, et al. Prevalence of high-risk coronary plaques in patients with and without metabolic syndrome and the relationship with prognosis. BMC Cardiovasc Disord. (2020) 20(1):73. doi: 10.1186/s12872-020-01358-8
7. Carlucci P, Purmalek M, Dey A, Temesgen-Oyelakin Y, Sakhardande S, Joshi A, et al. Neutrophil subsets and their gene signature associate with vascular inflammation and coronary atherosclerosis in lupus. JCI Insight. (2018) 3(8):e99276. doi: 10.1172/jci.insight.99276
8. Mo L, Gupta V, Modi R, Munnur K, Cameron J, Seneviratne S, et al. Severe obstructive sleep apnea is associated with significant coronary artery plaque burden independent of traditional cardiovascular risk factors. Int J Cardiovasc Imaging. (2020) 36(2):347–55. doi: 10.1007/s10554-019-01710-w
9. Gulati M, Levy P, Mukherjee D, Amsterdam E, Bhatt D, Birtcher K, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: a report of the American college of cardiology/American heart association joint committee on clinical practice guidelines. Circulation. (2021) 144(22):e368–454. doi: 10.1161/CIR.0000000000001029
10. Zhang A, Xu A, Ansari K, Hardacker K, Anderson G, Alsoof D, et al. Lumbar disc herniation: diagnosis and management. Am J Med. (2023) 136(7):645–51. doi: 10.1016/j.amjmed.2023.03.024
11. Neeland I, Patel R, Eshtehardi P, Dhawan S, McDaniel M, Rab S, et al. Coronary angiographic scoring systems: an evaluation of their equivalence and validity. Am Heart J. (2012) 164(4):547–52.e1. doi: 10.1016/j.ahj.2012.07.007
12. Pfirrmann C, Metzdorf A, Zanetti M, Hodler J, Boos N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine. (2001) 26(17):1873–8. doi: 10.1097/00007632-200109010-00011
13. Ahn Y, Kim J, Yoo B, Jeong Y. A new grading system for migrated lumbar disc herniation on sagittal magnetic resonance imaging: an agreement study. J Clin Med. (2022) 11(7):1750. doi: 10.3390/jcm11071750
14. Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. (2020) 41(1):111–88. doi: 10.1093/eurheartj/ehz455
15. Hess C, Low Wang C, Hiatt W. PCSK9 inhibitors: mechanisms of action, metabolic effects, and clinical outcomes. Annu Rev Med. (2018) 69:133–45. doi: 10.1146/annurev-med-042716-091351
16. Colombini A, Brayda-Bruno M, Lombardi G, Croiset S, Vrech V, Maione V, et al. Foki polymorphism in the vitamin D receptor gene (VDR) and its association with lumbar spine pathologies in the Italian population: a case-control study. PloS one. (2014) 9(5):e97027. doi: 10.1371/journal.pone.0097027
17. Steelman T, Lewandowski L, Helgeson M, Wilson K, Olsen C, Gwinn D. Population-based risk factors for the development of degenerative disk disease. Clin Spine Surg. (2018) 31(8):E409–E12. doi: 10.1097/BSD.0000000000000682
18. Rivinoja A, Paananen M, Taimela S, Solovieva S, Okuloff A, Zitting P, et al. Sports, smoking, and overweight during adolescence as predictors of sciatica in adulthood: a 28-year follow-up study of a birth cohort. Am J Epidemiol. (2011) 173(8):890–7. doi: 10.1093/aje/kwq459
19. Dzaye O, Razavi A, Blaha M, Mortensen M. Evaluation of coronary stenosis versus plaque burden for atherosclerotic cardiovascular disease risk assessment and management. Curr Opin Cardiol. (2021) 36(6):769–75. doi: 10.1097/HCO.0000000000000911
20. Won K, Lee B, Heo R, Park H, Lin F, Hadamitzky M, et al. Longitudinal quantitative assessment of coronary atherosclerotic plaque burden related to serum hemoglobin levels. JACC Asia. (2022) 2(3):311–9. doi: 10.1016/j.jacasi.2021.10.010
21. Akin F, Altun İ, Ayca B, Kose N, Altun İ. Associations of non-HDL-C and triglyceride/HDL-C ratio with coronary plaque burden and plaque characteristics in young adults. Bosnian J Basic Med Sci. (2022) 22(6):1025–32. doi: 10.17305/bjbms.2022.7142
22. Nafakhi H, Al-Mosawi A, Alkhalil Q. Cardiovascular risk factors and pericardial fat volume as predictors of coronary atherosclerosis burden in postmenopausal women: a retrospective, single center study. Health Sci Rep. (2023) 6(3):e1155. doi: 10.1002/hsr2.1155
23. Yuan L, Huang Z, Han W, Chang R, Sun B, Zhu M, et al. The impact of dyslipidemia on lumbar intervertebral disc degeneration and vertebral endplate modic changes: a cross-sectional study of 1035 citizens in China. BMC Public Health. (2023) 23(1):1302. doi: 10.1186/s12889-023-16224-3
24. Huang Z, Chen J, Su Y, Guo M, Chen Y, Zhu Y, et al. Impact of dyslipidemia on the severity of symptomatic lumbar spine degeneration: a retrospective clinical study. Front Nutr. (2022) 9:1033375. doi: 10.3389/fnut.2022.1033375
25. Zhang Y, Zhao Y, Wang M, Si M, Li J, Hou Y, et al. Serum lipid levels are positively correlated with lumbar disc herniation–a retrospective study of 790 Chinese patients. Lipids Health Dis. (2016) 15:80. doi: 10.1186/s12944-016-0248-x
26. Yan J, Li S, Zhang Y, Deng Z, Wu J, Huang Z, et al. Viacholesterol induces pyroptosis and matrix degradation mSREBP1-driven endoplasmic Reticulum stress in intervertebral disc degeneration. Front Cell Dev Biol. (2021) 9:803132. doi: 10.3389/fcell.2021.803132
27. Nelson A, Puri R, Brennan D, Anderson T, Cho L, Ballantyne C, et al. C-reactive protein levels and plaque regression with evolocumab: insights from GLAGOV. Am J Prev Cardiol. (2020) 3:100091. doi: 10.1016/j.ajpc.2020.100091
Keywords: unstable angina, Gensini score, plaque burden, lumbar disc herniation, evolocumab treatment
Citation: Wang Y, Ge J, Xu H and Li J (2024) Lumbar disc herniation is an independent predictor of plaque burden in the patients with unstable angina. Front. Cardiovasc. Med. 11:1324456. doi: 10.3389/fcvm.2024.1324456
Received: 24 October 2023; Accepted: 22 January 2024;
Published: 9 February 2024.
Edited by:
Xi-Ming Yuan, Linköping University, SwedenReviewed by:
Leena Kauppila, Terveystalo Healthcare, FinlandSara Seitun, San Martino Polyclinic Hospital IRCCS, Italy
© 2024 Wang, Ge, Xu and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jian Li bGVlcmFiYml0eUAxMjYuY29t
†These authors have contributed equally to this work and share co-first authorship
Abbreviations ALT, alanine aminotransferase; AST, aspartate aminotransferase; BMI, weight and body mass index; CAG, coronary angiography; eGFR, estimated glomerular filtration rate; HDL-C, high-density lipoprotein cholesterol; INR, international normalized ratio; LDH, lumbar disc herniation; LDL-C, low-density lipoprotein cholesterol; LVEF, left ventricular ejection fraction; LVIDd, left ventricular internal diameter at end-diastole; LVIDs, left ventricular internal diameter at end-systole; TG, triglyceride; UA, unstable angina.
 Yongchao Wang
Yongchao Wang Junhua Ge
Junhua Ge Hao Xu
Hao Xu